Decision-Making in Healthcare: Applying a Decision Tree Model
VerifiedAdded on 2023/03/31
|7
|1160
|495
Report
AI Summary
This report explores the application of a decision-tree model to address negative profitability trends within a healthcare organization's diagnostic imaging center. It emphasizes the importance of quantifying patient and diagnostic service quality to guide organizational decision-making. The report discusses the structure and principles of a decision tree model, illustrating its application with an example focused on improving diagnostic profitability through increased patient satisfaction. Several solutions are proposed to combat the negative trends, including the recruitment and allocation of a diagnostic team, staff training and education, modifying hospital schedules, and implementing routine auditing and feedback mechanisms. Each solution is analyzed for its potential short-term costs and long-term profitability benefits. The author concludes that the decision-tree model is a valuable tool for communicating strategies to the board of directors, quantifying probable outcomes, and facilitating data-driven decision-making within the healthcare organization.

Running head: HEALTHCARE DECISION-MAKING
HEALTHCARE DECISION-MAKING
Name of the Student:
Name of the University:
Author note:
HEALTHCARE DECISION-MAKING
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTHCARE DECISION-MAKING
Introduction
For mitigating shortcomings and deficits in the functioning of a healthcare organization,
quantifying the quality of the patient and diagnostic services provided by the same, must be
quantified into relevant outcomes or results which form the guiding principle for conductance of
collective organization decision-making (Jothi & Husain, 2015). The following paper will focus
on the usage of a decision-tree model for optimizing existing negative trends towards beneficial
profitability in a concerned healthcare organization.
Discussion
Decision-tree Model
For analyzing the current negative trends reflecting loss in profitability in a healthcare
organization, the quantitative model deemed to be effective for fulfilling the purpose is a
decision tree model. A decision tree is model of classification outlining observations and
assumptions with high likelihood of future occurrence in the form of possible alternatives and
decisions (Tang et al., 2019). A decision tree model acquires its title due to is characteristic
categorization of decisions being represented as branches emerging from a chosen problem. Each
branch represents a decision with further branches representing possible outcomes as a result of
the taking the decision. The primary principles outlining a decision tree model in a healthcare
model for example, will consisting of segmenting the stakeholders (nurses, patients), stratifying
the outcomes of each decision (high, medium, low risk) and predicting the results of future
occurrences underlying each decision (patient satisfaction: high or low) (Abdelaziz et al., 2018).
Introduction
For mitigating shortcomings and deficits in the functioning of a healthcare organization,
quantifying the quality of the patient and diagnostic services provided by the same, must be
quantified into relevant outcomes or results which form the guiding principle for conductance of
collective organization decision-making (Jothi & Husain, 2015). The following paper will focus
on the usage of a decision-tree model for optimizing existing negative trends towards beneficial
profitability in a concerned healthcare organization.
Discussion
Decision-tree Model
For analyzing the current negative trends reflecting loss in profitability in a healthcare
organization, the quantitative model deemed to be effective for fulfilling the purpose is a
decision tree model. A decision tree is model of classification outlining observations and
assumptions with high likelihood of future occurrence in the form of possible alternatives and
decisions (Tang et al., 2019). A decision tree model acquires its title due to is characteristic
categorization of decisions being represented as branches emerging from a chosen problem. Each
branch represents a decision with further branches representing possible outcomes as a result of
the taking the decision. The primary principles outlining a decision tree model in a healthcare
model for example, will consisting of segmenting the stakeholders (nurses, patients), stratifying
the outcomes of each decision (high, medium, low risk) and predicting the results of future
occurrences underlying each decision (patient satisfaction: high or low) (Abdelaziz et al., 2018).
2HEALTHCARE DECISION-MAKING
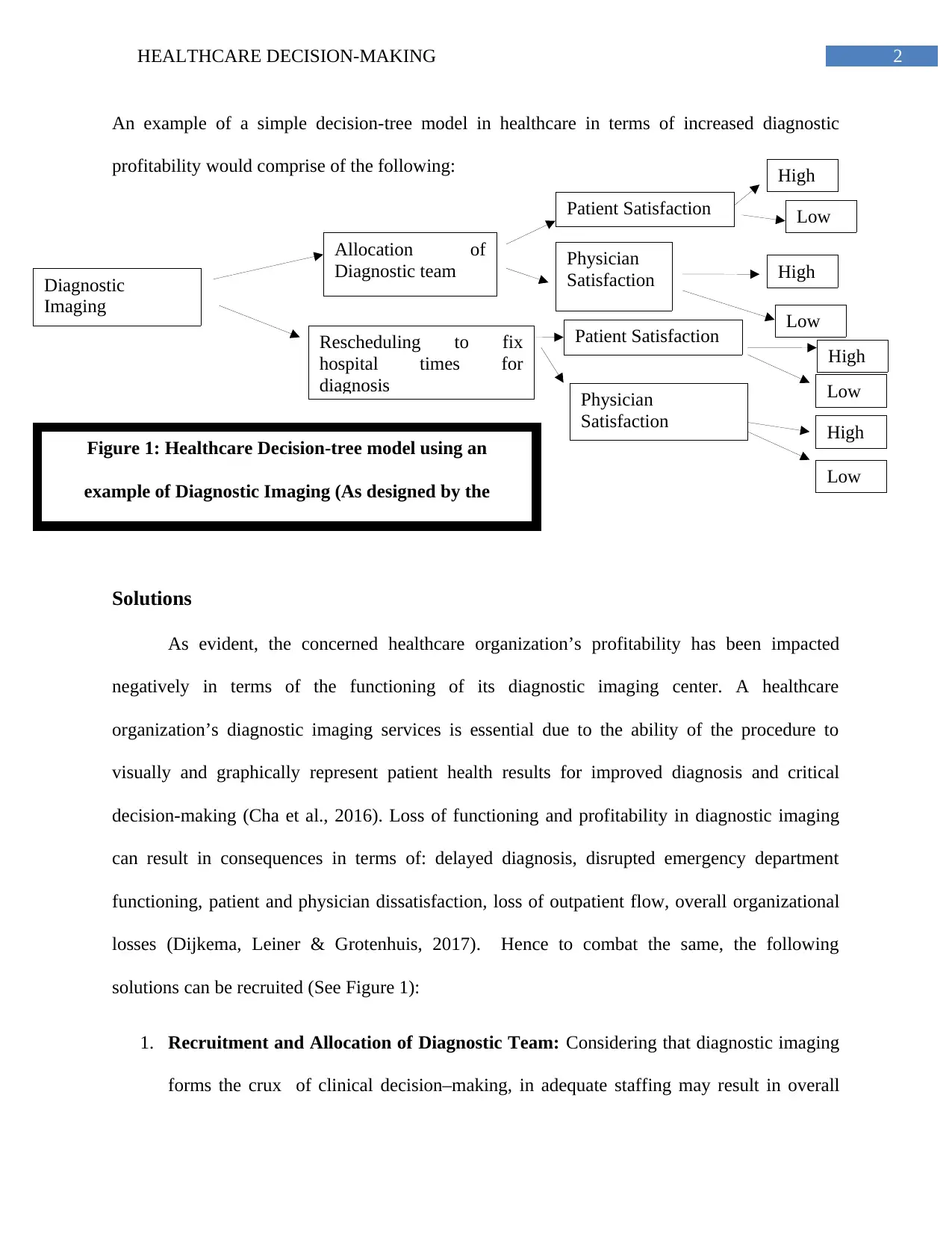
An example of a simple decision-tree model in healthcare in terms of increased diagnostic
profitability would comprise of the following:
Solutions
As evident, the concerned healthcare organization’s profitability has been impacted
negatively in terms of the functioning of its diagnostic imaging center. A healthcare
organization’s diagnostic imaging services is essential due to the ability of the procedure to
visually and graphically represent patient health results for improved diagnosis and critical
decision-making (Cha et al., 2016). Loss of functioning and profitability in diagnostic imaging
can result in consequences in terms of: delayed diagnosis, disrupted emergency department
functioning, patient and physician dissatisfaction, loss of outpatient flow, overall organizational
losses (Dijkema, Leiner & Grotenhuis, 2017). Hence to combat the same, the following
solutions can be recruited (See Figure 1):
1. Recruitment and Allocation of Diagnostic Team: Considering that diagnostic imaging
forms the crux of clinical decision–making, in adequate staffing may result in overall
Diagnostic
Imaging
Allocation of
Diagnostic team
Rescheduling to fix
hospital times for
diagnosis
Patient Satisfaction
Physician
Satisfaction
Patient Satisfaction
Physician
Satisfaction
High
Low
High
Low
High
Low
High
Low
Figure 1: Healthcare Decision-tree model using an
example of Diagnostic Imaging (As designed by the
author)
An example of a simple decision-tree model in healthcare in terms of increased diagnostic
profitability would comprise of the following:
Solutions
As evident, the concerned healthcare organization’s profitability has been impacted
negatively in terms of the functioning of its diagnostic imaging center. A healthcare
organization’s diagnostic imaging services is essential due to the ability of the procedure to
visually and graphically represent patient health results for improved diagnosis and critical
decision-making (Cha et al., 2016). Loss of functioning and profitability in diagnostic imaging
can result in consequences in terms of: delayed diagnosis, disrupted emergency department
functioning, patient and physician dissatisfaction, loss of outpatient flow, overall organizational
losses (Dijkema, Leiner & Grotenhuis, 2017). Hence to combat the same, the following
solutions can be recruited (See Figure 1):
1. Recruitment and Allocation of Diagnostic Team: Considering that diagnostic imaging
forms the crux of clinical decision–making, in adequate staffing may result in overall
Diagnostic
Imaging
Allocation of
Diagnostic team
Rescheduling to fix
hospital times for
diagnosis
Patient Satisfaction
Physician
Satisfaction
Patient Satisfaction
Physician
Satisfaction
High
Low
High
Low
High
Low
High
Low
Figure 1: Healthcare Decision-tree model using an
example of Diagnostic Imaging (As designed by the
author)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTHCARE DECISION-MAKING
delayed functioning for every department of the organization. Hence additional workers
may be recruited, delegated into specific teams (radiography, computer tomography etc.)
followed by a separate diagnostic communication channel relaying information to the
emergency department on a priority basis. This will result in increased profits in terms of
reduced delays, quicker diagnosis, patient satisfaction and increased patient flow
(Venderink et al., 2017).
2. Staff Training and Education Framework: Implementation of a training and
educational plan by diagnostic technicians will result in long term benefits in terms of
improved equipment usage by staff, hastened diagnostic imaging and improvements in
physician decision-making and patient satisfaction. However, short term losses in terms
of expenditures in recruiting training personnel and equipment may be yield difficult-to-
achieve financial targets in the organization’s break even report (Gregory et al., 2016).
3. Modifying Hospital Schedules: Rescheduling the hospital schedules to incorporate
specific times for diagnostic imaging services will allow improved and organized patient
flow and reallocation of staff functioning as per the specified timings. This will result in
long term profits in terms of increased pre-diagnostic preparation time for staff and
patients resulting in faster diagnostics and clinical decision-making. While rescheduling
timings may yield staff and patient confusion and resistance to change, communicating
such changes prior to actual implementation may mitigate these difficulties (Lugu et al.,
2016).
4. Routine Auditing and Feedback: Considering optimum diagnostic imaging services is
strongly associated with patient and physician satisfaction, obtaining feedback will assist
in future profitability and improvements by recognizing preferences of both these
delayed functioning for every department of the organization. Hence additional workers
may be recruited, delegated into specific teams (radiography, computer tomography etc.)
followed by a separate diagnostic communication channel relaying information to the
emergency department on a priority basis. This will result in increased profits in terms of
reduced delays, quicker diagnosis, patient satisfaction and increased patient flow
(Venderink et al., 2017).
2. Staff Training and Education Framework: Implementation of a training and
educational plan by diagnostic technicians will result in long term benefits in terms of
improved equipment usage by staff, hastened diagnostic imaging and improvements in
physician decision-making and patient satisfaction. However, short term losses in terms
of expenditures in recruiting training personnel and equipment may be yield difficult-to-
achieve financial targets in the organization’s break even report (Gregory et al., 2016).
3. Modifying Hospital Schedules: Rescheduling the hospital schedules to incorporate
specific times for diagnostic imaging services will allow improved and organized patient
flow and reallocation of staff functioning as per the specified timings. This will result in
long term profits in terms of increased pre-diagnostic preparation time for staff and
patients resulting in faster diagnostics and clinical decision-making. While rescheduling
timings may yield staff and patient confusion and resistance to change, communicating
such changes prior to actual implementation may mitigate these difficulties (Lugu et al.,
2016).
4. Routine Auditing and Feedback: Considering optimum diagnostic imaging services is
strongly associated with patient and physician satisfaction, obtaining feedback will assist
in future profitability and improvements by recognizing preferences of both these
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTHCARE DECISION-MAKING
stakeholders. Routine auditing procedures will produce long term profitability in terms of
prompt identification and management of imaging and equipment errors as compared to
long term financial losses due to aggravation of erroneous staff and machinery
functioning. Redirecting organizational financial resources to yield novel auditing and
feedback frameworks may however yield short term losses (Bajre et al., 2017).
Summary: Personal Improvement
To conclude, the decision-tree proved to be beneficial in communicating with the board
of directors on the strategies with which the negative trend in the profitability of the healthcare
organization’s diagnostic imaging centre. The decision-tree model was helpful since it assisted in
quantifying and summarizing probable outcomes of a decision into concise values, which further
compelled the usage of organizational data and the resultant ease in communication to the board
of directors. Hence, the decision-tree model proves to be helpful in future qualitative and
quantitative assessments of the healthcare organization.
stakeholders. Routine auditing procedures will produce long term profitability in terms of
prompt identification and management of imaging and equipment errors as compared to
long term financial losses due to aggravation of erroneous staff and machinery
functioning. Redirecting organizational financial resources to yield novel auditing and
feedback frameworks may however yield short term losses (Bajre et al., 2017).
Summary: Personal Improvement
To conclude, the decision-tree proved to be beneficial in communicating with the board
of directors on the strategies with which the negative trend in the profitability of the healthcare
organization’s diagnostic imaging centre. The decision-tree model was helpful since it assisted in
quantifying and summarizing probable outcomes of a decision into concise values, which further
compelled the usage of organizational data and the resultant ease in communication to the board
of directors. Hence, the decision-tree model proves to be helpful in future qualitative and
quantitative assessments of the healthcare organization.
5HEALTHCARE DECISION-MAKING
References
Abdelaziz, A., Elhoseny, M., Salama, A. S., & Riad, A. M. (2018). A machine learning model
for improving healthcare services on cloud computing environment. Measurement, 119,
117-128.
Bajre, M. K., Pennington, M., Woznitza, N., Beardmore, C., Radhakrishnan, M., Harris, R., &
McCrone, P. (2017). Expanding the role of radiographers in reporting suspected lung
cancer: a cost-effectiveness analysis using a decision tree model. Radiography, 23(4),
273-278.
Cha, M. J., Lee, K. S., Kim, H. S., Lee, S. W., Jeong, C. J., Kim, E. Y., & Lee, H. Y. (2016).
Improvement in imaging diagnosis technique and modalities for solitary pulmonary
nodules: from ground-glass opacity nodules to part-solid and solid nodules. Expert review
of respiratory medicine, 10(3), 261-278.
Dijkema, E. J., Leiner, T., & Grotenhuis, H. B. (2017). Diagnosis, imaging and clinical
management of aortic coarctation. Heart, 103(15), 1148-1155.
Gregory, S., Kuntz, K., Sainfort, F., & Kharbanda, A. (2016). Cost-effectiveness of integrating a
clinical decision rule and staged imaging protocol for diagnosis of appendicitis. Value in
Health, 19(1), 28-35.
Jothi, N., & Husain, W. (2015). Data mining in healthcare–a review. Procedia Computer
Science, 72, 306-313.
References
Abdelaziz, A., Elhoseny, M., Salama, A. S., & Riad, A. M. (2018). A machine learning model
for improving healthcare services on cloud computing environment. Measurement, 119,
117-128.
Bajre, M. K., Pennington, M., Woznitza, N., Beardmore, C., Radhakrishnan, M., Harris, R., &
McCrone, P. (2017). Expanding the role of radiographers in reporting suspected lung
cancer: a cost-effectiveness analysis using a decision tree model. Radiography, 23(4),
273-278.
Cha, M. J., Lee, K. S., Kim, H. S., Lee, S. W., Jeong, C. J., Kim, E. Y., & Lee, H. Y. (2016).
Improvement in imaging diagnosis technique and modalities for solitary pulmonary
nodules: from ground-glass opacity nodules to part-solid and solid nodules. Expert review
of respiratory medicine, 10(3), 261-278.
Dijkema, E. J., Leiner, T., & Grotenhuis, H. B. (2017). Diagnosis, imaging and clinical
management of aortic coarctation. Heart, 103(15), 1148-1155.
Gregory, S., Kuntz, K., Sainfort, F., & Kharbanda, A. (2016). Cost-effectiveness of integrating a
clinical decision rule and staged imaging protocol for diagnosis of appendicitis. Value in
Health, 19(1), 28-35.
Jothi, N., & Husain, W. (2015). Data mining in healthcare–a review. Procedia Computer
Science, 72, 306-313.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HEALTHCARE DECISION-MAKING
Lungu, A., Swift, A. J., Capener, D., Kiely, D., Hose, R., & Wild, J. M. (2016). Diagnosis of
pulmonary hypertension from magnetic resonance imaging–based computational models
and decision tree analysis. Pulmonary circulation, 6(2), 181-190.
Tang, V., Siu, P. K. Y., Choy, K. L., Lam, H. Y., Ho, G. T. S., Lee, C. K. M., & Tsang, Y. P.
(2019). An adaptive clinical decision support system for serving the elderly with chronic
diseases in healthcare industry. Expert Systems, e12369.
Venderink, W., Govers, T. M., de Rooij, M., Fütterer, J. J., & Sedelaar, J. M. (2017). Cost-
effectiveness comparison of imaging-guided prostate biopsy techniques: systematic
transrectal ultrasound, direct in-bore MRI, and image fusion. American Journal of
Roentgenology, 208(5), 1058-1063.
Lungu, A., Swift, A. J., Capener, D., Kiely, D., Hose, R., & Wild, J. M. (2016). Diagnosis of
pulmonary hypertension from magnetic resonance imaging–based computational models
and decision tree analysis. Pulmonary circulation, 6(2), 181-190.
Tang, V., Siu, P. K. Y., Choy, K. L., Lam, H. Y., Ho, G. T. S., Lee, C. K. M., & Tsang, Y. P.
(2019). An adaptive clinical decision support system for serving the elderly with chronic
diseases in healthcare industry. Expert Systems, e12369.
Venderink, W., Govers, T. M., de Rooij, M., Fütterer, J. J., & Sedelaar, J. M. (2017). Cost-
effectiveness comparison of imaging-guided prostate biopsy techniques: systematic
transrectal ultrasound, direct in-bore MRI, and image fusion. American Journal of
Roentgenology, 208(5), 1058-1063.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
