Reflection's Role in Healthcare: Critical Incident Analysis
VerifiedAdded on 2023/01/18
|13
|4292
|56
Report
AI Summary
This report delves into the significance of reflective practices within healthcare services. It begins by defining reflection and its importance, followed by an examination of different reflective models, including Kolb's and Gibbs' models, highlighting their advantages and disadvantages. The report then discusses the application of reflection in practice, illustrated through a critical incident analysis using Gibbs' reflective model. This includes a description of the incident, feelings experienced, evaluation, analysis, conclusion, and an action plan. Additionally, the report analyzes the role of consent in maintaining patient dignity, with an emphasis on verbal and non-verbal communication and references to the NMC Code. The goal is to understand how effective communication skills enable healthcare practitioners to provide accurate and appropriate information to patients. The report concludes with an emphasis on how reflective practices can lead to improved quality of care and professional development.
Reflection
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
1. Introduction..................................................................................................................................1
2. What is Reflection?......................................................................................................................1
3. Reflection in practice...................................................................................................................6
CONCLUSION..............................................................................................................................10
REFERENCES..............................................................................................................................12
1. Introduction..................................................................................................................................1
2. What is Reflection?......................................................................................................................1
3. Reflection in practice...................................................................................................................6
CONCLUSION..............................................................................................................................10
REFERENCES..............................................................................................................................12
1. Introduction
Reflective practices defines a way of studying the own experiences for improving
manner, in which a person works (Clifford, 2019). This practice is mainly used by health
practitioners who always seek to improve their working procedures, in order to become more
proactive as well as qualified professionals (Richard, Gagnon and Careau, 2019). The present
study is going to examine the importance of reflection in healthcare services, with a support of
literature review. Here, an understanding of self-awareness and reflection, with impact of
reflection on practices of practitioners, as well as factors which support for improvement of same
is also described. A discussion is made by using different models of reflection with specific
advantages and disadvantages. Along with this, purpose of using reflection and how it helps in
achievement of a goal, is also explained. Furthermore, to understand role of reflection in
improving the quality of services, an illustration is given that described a critical incident and
how clinical staff deals with same, by using Gibb's reflective model. Another task includes an
analysis is done on consent for maintaining the dignity of patients, with insight of verbal and
non-verbal communication. For this process NMC Code is taken that describes the professional
standards of nurses and associated members in HSC sector. This would help in evaluating how
good communication skills enables a health practitioner in providing the specific and right
information to others.
2. What is Reflection?
Reflection can be defined as a process of reviewing, analysis as well as evaluating the
own experience actively, by drawing upon a number of theoretical concepts to make future
actions (Linsley, Kane and Barker, 2019). In context with health and social care sector, reflective
practices provide an insight what a person has done in previous situations and learned from
experience, to improve quality of services in future. By closely linking with the concept of
learning from own experience, a person can think what had done and what happened, so that
decision can be taken for future improvement in services (Field and Brown, 2019). As concept of
reflective thinking is like general 'thinking', but it requires the conscious efforts for developing
an insight about an incident. So, reviewing the process how health caregivers have managed
makes them able to develop pre-planned actions for handling same situation, if it occurs in the
future.
1
Reflective practices defines a way of studying the own experiences for improving
manner, in which a person works (Clifford, 2019). This practice is mainly used by health
practitioners who always seek to improve their working procedures, in order to become more
proactive as well as qualified professionals (Richard, Gagnon and Careau, 2019). The present
study is going to examine the importance of reflection in healthcare services, with a support of
literature review. Here, an understanding of self-awareness and reflection, with impact of
reflection on practices of practitioners, as well as factors which support for improvement of same
is also described. A discussion is made by using different models of reflection with specific
advantages and disadvantages. Along with this, purpose of using reflection and how it helps in
achievement of a goal, is also explained. Furthermore, to understand role of reflection in
improving the quality of services, an illustration is given that described a critical incident and
how clinical staff deals with same, by using Gibb's reflective model. Another task includes an
analysis is done on consent for maintaining the dignity of patients, with insight of verbal and
non-verbal communication. For this process NMC Code is taken that describes the professional
standards of nurses and associated members in HSC sector. This would help in evaluating how
good communication skills enables a health practitioner in providing the specific and right
information to others.
2. What is Reflection?
Reflection can be defined as a process of reviewing, analysis as well as evaluating the
own experience actively, by drawing upon a number of theoretical concepts to make future
actions (Linsley, Kane and Barker, 2019). In context with health and social care sector, reflective
practices provide an insight what a person has done in previous situations and learned from
experience, to improve quality of services in future. By closely linking with the concept of
learning from own experience, a person can think what had done and what happened, so that
decision can be taken for future improvement in services (Field and Brown, 2019). As concept of
reflective thinking is like general 'thinking', but it requires the conscious efforts for developing
an insight about an incident. So, reviewing the process how health caregivers have managed
makes them able to develop pre-planned actions for handling same situation, if it occurs in the
future.
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

The concept of reflection can be understood in a better way by using different models as
explained below –
Kolb's Reflective Model:
This model was given by David Kolb, which includes four stages to reflect experience of
a person related to past behaviour. It would help in highlighting the main actions and conclude
the ideas which have been used to resolve an issue (Brennan, 2019). In this regard, through Kolb
model, medical practitioners can reflect what they have learned from entire experience, as per
each model -
Concrete experience – This stage assists a practitioner to review the most critical
situation, in order to recognise what actions have been taken (Richard, Gagnon and Careau,
2019). By reflecting systematically, the entire journey from initial to end, they can learn
something new and can make ideas how to better improve that situation, if it occurs in future
2
explained below –
Kolb's Reflective Model:
This model was given by David Kolb, which includes four stages to reflect experience of
a person related to past behaviour. It would help in highlighting the main actions and conclude
the ideas which have been used to resolve an issue (Brennan, 2019). In this regard, through Kolb
model, medical practitioners can reflect what they have learned from entire experience, as per
each model -
Concrete experience – This stage assists a practitioner to review the most critical
situation, in order to recognise what actions have been taken (Richard, Gagnon and Careau,
2019). By reflecting systematically, the entire journey from initial to end, they can learn
something new and can make ideas how to better improve that situation, if it occurs in future
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
again, by existing skill and practice. At this stage, a person in healthcare sector, can make notes
of related situation to describe what has seen, how they feel and what thinks about same.
Reflective observation – It is second main stage of Kolb’s reflective model, which states
that by written down the description in first stage about own experience, now, it individual needs
to reflect detailed manner what has actually happened in that situation (Job, Yan Wong and
Anstey, 2019). This description includes what have been worked and which action or ideas have
been failed. It also helps in analysing why such critical incident has been happened and what
other persons response for the same. Through this process, they can realise what has going well
and own contribution for resolving the situation.
Abstract conceptualisation – It is another main stage, where personal contribution can be
realised, which arise questions what a person has done well or differently from others. Initially,
individuals need to find the different ways that would be taken for dealing with critical situations
(Ellis, 2019). Through this process, they can also think up effective strategies from own
experience to face or deal with similar situation in future. Along with this, to realise all these
things, they are also required to make a healthy discussion under a group, so that better ideas can
be generated for resolving critical incidents in a better way.
Active experimentation – It is the last phase of reflective model, which states to
practising the more effective or new way by acquiring theoretical and practical knowledge from
past experience (Richard, Gagnon and Careau, 2019). By taking own reflections and ideas about
improvements, practitioners can develop new strategies and make minds how the same will help
in dealing with situations. So, experiencing own ideas within active experimentation stage,
makes a person realising the new “concrete experiences”.
Thus, utilising the Kolb’s reflective model, health practitioners can make new ideas to
improve quality of services, which would help in well-being of a person more effectively.
Gibbs Reflective Theory:
This theory of reflection was developed by Gibbs in 1988. It is based on six-stage
approach whose core principles are quite similar to Kolb's reflective model, that helps in
reflecting own thoughts and feelings after an experience (Clifford, 2019). In context with health
and social care sector, this model can be applied more easily because some critical incidences are
mostly happened to occur again and again. So, using Gibb's model, health practitioners find it
3
of related situation to describe what has seen, how they feel and what thinks about same.
Reflective observation – It is second main stage of Kolb’s reflective model, which states
that by written down the description in first stage about own experience, now, it individual needs
to reflect detailed manner what has actually happened in that situation (Job, Yan Wong and
Anstey, 2019). This description includes what have been worked and which action or ideas have
been failed. It also helps in analysing why such critical incident has been happened and what
other persons response for the same. Through this process, they can realise what has going well
and own contribution for resolving the situation.
Abstract conceptualisation – It is another main stage, where personal contribution can be
realised, which arise questions what a person has done well or differently from others. Initially,
individuals need to find the different ways that would be taken for dealing with critical situations
(Ellis, 2019). Through this process, they can also think up effective strategies from own
experience to face or deal with similar situation in future. Along with this, to realise all these
things, they are also required to make a healthy discussion under a group, so that better ideas can
be generated for resolving critical incidents in a better way.
Active experimentation – It is the last phase of reflective model, which states to
practising the more effective or new way by acquiring theoretical and practical knowledge from
past experience (Richard, Gagnon and Careau, 2019). By taking own reflections and ideas about
improvements, practitioners can develop new strategies and make minds how the same will help
in dealing with situations. So, experiencing own ideas within active experimentation stage,
makes a person realising the new “concrete experiences”.
Thus, utilising the Kolb’s reflective model, health practitioners can make new ideas to
improve quality of services, which would help in well-being of a person more effectively.
Gibbs Reflective Theory:
This theory of reflection was developed by Gibbs in 1988. It is based on six-stage
approach whose core principles are quite similar to Kolb's reflective model, that helps in
reflecting own thoughts and feelings after an experience (Clifford, 2019). In context with health
and social care sector, this model can be applied more easily because some critical incidences are
mostly happened to occur again and again. So, using Gibb's model, health practitioners find it
3
easy to use, it focuses on the experience and learning from the incident, thoughts about situation,
what was happened good or bad, then analyse whole situation and make action plan for the
future. This is the best method for a student like myself to use as it is so easy to use, and with
new experiences, a lot of my feelings will be in forefront of any case I deal with as its all new
experiences. Gibb’s theory 6 stages can be described in following way –
Description of experience – This stage reflects a situation in detail manner, where what
was happened in the beginning and why it was occurred is discussed. Through this prospectus, a
number of aspects that are relevant for such an event can be revealed (Linsley, Kane and Barker,
2019). It includes circumstances that creates the situation, who were involved in dealing with
same, what actions they had taken etc. Therefore, by recognising these things medical
practitioners can judge a situation better way.
Feelings about experience – Here, at this stage, health professionals can explore their
feelings and thoughts that they have felt during the past events. It includes how such an event
impact on their experience. For example – a serious case where a person is injured a lot and there
was no senior medical professional present, then how remaining staff has tacked the situation
and feel, can be recognised. In this situation, mostly staff feel conscious and nervous about
actions they have been used to deal with injured (Field and Brown, 2019). If treatment they are
going to take is risky for treatment of injured person, or they confidently do the same. Thus,
reflecting in such a manner, a person can ascertain own confidence level and make improvement
to handle similar kind of situation in future, more effectively.
Evaluation of experience – At this stage, level of extremeness can be evaluated about the
previous situation, after describing the above two phases (Taylor and Guerin, 2019). Here, health
practitioners can analysed how they have responded towards challenging situation, including
effectiveness or ineffectiveness about experience got from the same. Through this process, they
can also evaluate contribution of own and other associated persons, to evaluate who was worked
more. If a situation was handled more efficiently, then it reveals that quality of work was much
good. This would motivate practitioners to deal with future challenging situations more patiently
and confidently (Brennan, 2019). On the other hand, if practitioners failed to handle previous
cases due to some wrong actions then they can evaluate the reasons behind same and develop
better plan.
4
what was happened good or bad, then analyse whole situation and make action plan for the
future. This is the best method for a student like myself to use as it is so easy to use, and with
new experiences, a lot of my feelings will be in forefront of any case I deal with as its all new
experiences. Gibb’s theory 6 stages can be described in following way –
Description of experience – This stage reflects a situation in detail manner, where what
was happened in the beginning and why it was occurred is discussed. Through this prospectus, a
number of aspects that are relevant for such an event can be revealed (Linsley, Kane and Barker,
2019). It includes circumstances that creates the situation, who were involved in dealing with
same, what actions they had taken etc. Therefore, by recognising these things medical
practitioners can judge a situation better way.
Feelings about experience – Here, at this stage, health professionals can explore their
feelings and thoughts that they have felt during the past events. It includes how such an event
impact on their experience. For example – a serious case where a person is injured a lot and there
was no senior medical professional present, then how remaining staff has tacked the situation
and feel, can be recognised. In this situation, mostly staff feel conscious and nervous about
actions they have been used to deal with injured (Field and Brown, 2019). If treatment they are
going to take is risky for treatment of injured person, or they confidently do the same. Thus,
reflecting in such a manner, a person can ascertain own confidence level and make improvement
to handle similar kind of situation in future, more effectively.
Evaluation of experience – At this stage, level of extremeness can be evaluated about the
previous situation, after describing the above two phases (Taylor and Guerin, 2019). Here, health
practitioners can analysed how they have responded towards challenging situation, including
effectiveness or ineffectiveness about experience got from the same. Through this process, they
can also evaluate contribution of own and other associated persons, to evaluate who was worked
more. If a situation was handled more efficiently, then it reveals that quality of work was much
good. This would motivate practitioners to deal with future challenging situations more patiently
and confidently (Brennan, 2019). On the other hand, if practitioners failed to handle previous
cases due to some wrong actions then they can evaluate the reasons behind same and develop
better plan.
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
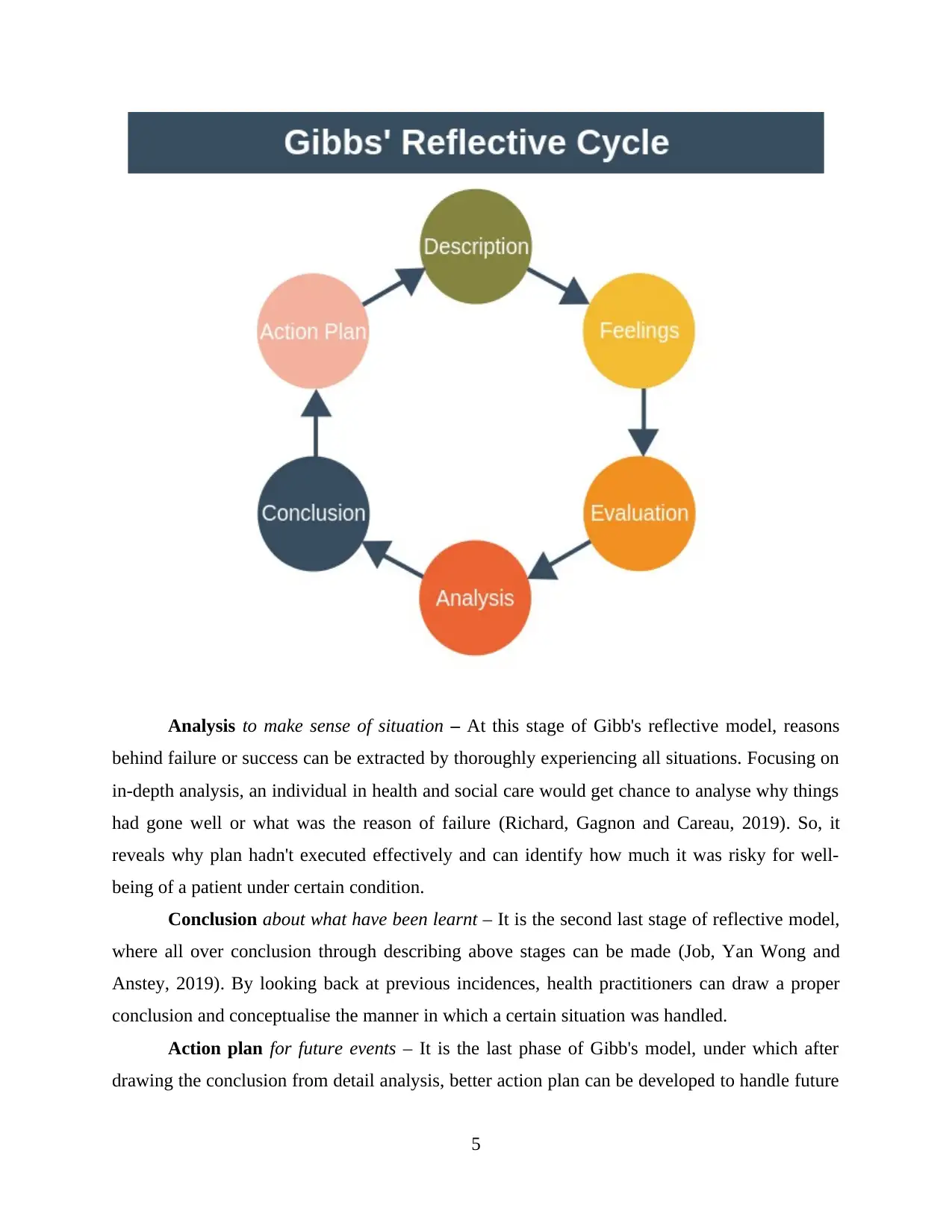
Analysis to make sense of situation – At this stage of Gibb's reflective model, reasons
behind failure or success can be extracted by thoroughly experiencing all situations. Focusing on
in-depth analysis, an individual in health and social care would get chance to analyse why things
had gone well or what was the reason of failure (Richard, Gagnon and Careau, 2019). So, it
reveals why plan hadn't executed effectively and can identify how much it was risky for well-
being of a patient under certain condition.
Conclusion about what have been learnt – It is the second last stage of reflective model,
where all over conclusion through describing above stages can be made (Job, Yan Wong and
Anstey, 2019). By looking back at previous incidences, health practitioners can draw a proper
conclusion and conceptualise the manner in which a certain situation was handled.
Action plan for future events – It is the last phase of Gibb's model, under which after
drawing the conclusion from detail analysis, better action plan can be developed to handle future
5
behind failure or success can be extracted by thoroughly experiencing all situations. Focusing on
in-depth analysis, an individual in health and social care would get chance to analyse why things
had gone well or what was the reason of failure (Richard, Gagnon and Careau, 2019). So, it
reveals why plan hadn't executed effectively and can identify how much it was risky for well-
being of a patient under certain condition.
Conclusion about what have been learnt – It is the second last stage of reflective model,
where all over conclusion through describing above stages can be made (Job, Yan Wong and
Anstey, 2019). By looking back at previous incidences, health practitioners can draw a proper
conclusion and conceptualise the manner in which a certain situation was handled.
Action plan for future events – It is the last phase of Gibb's model, under which after
drawing the conclusion from detail analysis, better action plan can be developed to handle future
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
situations (Ellis, 2019). This plan will include strategies and procedures that can be taken to
improve quality of healthcare services for minimising risk and well-being of a patient.
Rationale behind using the reflection
In healthcare sector, reflective practices is essential to analyse how practitioners have
behaved in a particular situation and way they have dealt with same. Through this process, they
can review under what condition a specific event has occurred and how their experience match
with preconceived ideas to resolve same (Job, Yan Wong and Anstey, 2019). Along with this,
through which approaches they can better handled such situation, can also be developed. This
practice make staff of healthcare association to learn from actions and being capable to deal with
future situations more effectively.
3. Reflection in practice
Critical incident
Reflective practice can be considered to promote personal and professional development
skills, where a person by analysing own past experience can construct a path to achieve good
result in future (Richard, Gagnon and Careau, 2019). As a health practitioner, I have also faced a
lot of cases that increase my experience and improve my performance. One of the major
incident, where breakthrough my experience is revealed by using Gibb's reflective model -
Description of incident
When I was placed firstly as a nurse in the hospital rehabilitation ward where main role is
to support patients gain their strength and mobility to be discharged from hospital, to reduce
stress and calm their anxiety during treatment. First case have seen by me was a patient who was
suffered from dementia and kept into the rehabilitation ward against his will, because consent
form was signed by family member. So, to address the needs of this patient and keep in hospital
who wants to leave, I have analysed that whole staff have effective communication skills, that
helps in collaborate with each other. When I was told to make sure the patient does not fall out of
bed as she wanted to escape from the bed, as she had prior incident of falls and was not able to
stand without support of equipment and carer, she had dementia and asked me when she would
be discharged and needed constant reassurance that she would be discharged from the hospital
soon, the situation was so awkward and patient started crying due to high level of anxiety and
distress.
Feeling –
6
improve quality of healthcare services for minimising risk and well-being of a patient.
Rationale behind using the reflection
In healthcare sector, reflective practices is essential to analyse how practitioners have
behaved in a particular situation and way they have dealt with same. Through this process, they
can review under what condition a specific event has occurred and how their experience match
with preconceived ideas to resolve same (Job, Yan Wong and Anstey, 2019). Along with this,
through which approaches they can better handled such situation, can also be developed. This
practice make staff of healthcare association to learn from actions and being capable to deal with
future situations more effectively.
3. Reflection in practice
Critical incident
Reflective practice can be considered to promote personal and professional development
skills, where a person by analysing own past experience can construct a path to achieve good
result in future (Richard, Gagnon and Careau, 2019). As a health practitioner, I have also faced a
lot of cases that increase my experience and improve my performance. One of the major
incident, where breakthrough my experience is revealed by using Gibb's reflective model -
Description of incident
When I was placed firstly as a nurse in the hospital rehabilitation ward where main role is
to support patients gain their strength and mobility to be discharged from hospital, to reduce
stress and calm their anxiety during treatment. First case have seen by me was a patient who was
suffered from dementia and kept into the rehabilitation ward against his will, because consent
form was signed by family member. So, to address the needs of this patient and keep in hospital
who wants to leave, I have analysed that whole staff have effective communication skills, that
helps in collaborate with each other. When I was told to make sure the patient does not fall out of
bed as she wanted to escape from the bed, as she had prior incident of falls and was not able to
stand without support of equipment and carer, she had dementia and asked me when she would
be discharged and needed constant reassurance that she would be discharged from the hospital
soon, the situation was so awkward and patient started crying due to high level of anxiety and
distress.
Feeling –
6
I was feeling very inadequate to deal with such a situation and slightly felt unsure how to
convince her, as she had dementia was my first case where I felt almost we were keeping her
against her will in the hospital. It also increased my anxiety level and feel little bit less confident
to work more in the ward (Ellis, 2019). However, colleagues and senior staff have supported me
to handle the situation but it didn't make me confident to stay long time with the patient because
she calmed down only for a few minutes but again fought to get out. My feeling was what if it
was me, would I like it if I was kept somewhere against my will. I was very uncomfortable.
Evaluation –
As my role is to give support to health carers and nurses that were administering the
medication and other diagnostic process, therefore, to manage these duties other nursing staff
have supported me a lot (Taylor and Guerin, 2019). Through information sharing and good
communication among team, has encouraged me to accept this challenging role and give efforts
to perform well.
Analysis
I have analysed from above situation that if a patient especially having any kind of
neurological disorder, is kept against their will, then consent form is essential. Under this
condition, it is also necessary for medical practitioners to have effective communication skills, to
keep patient within rehabilitation ward in safe manner.
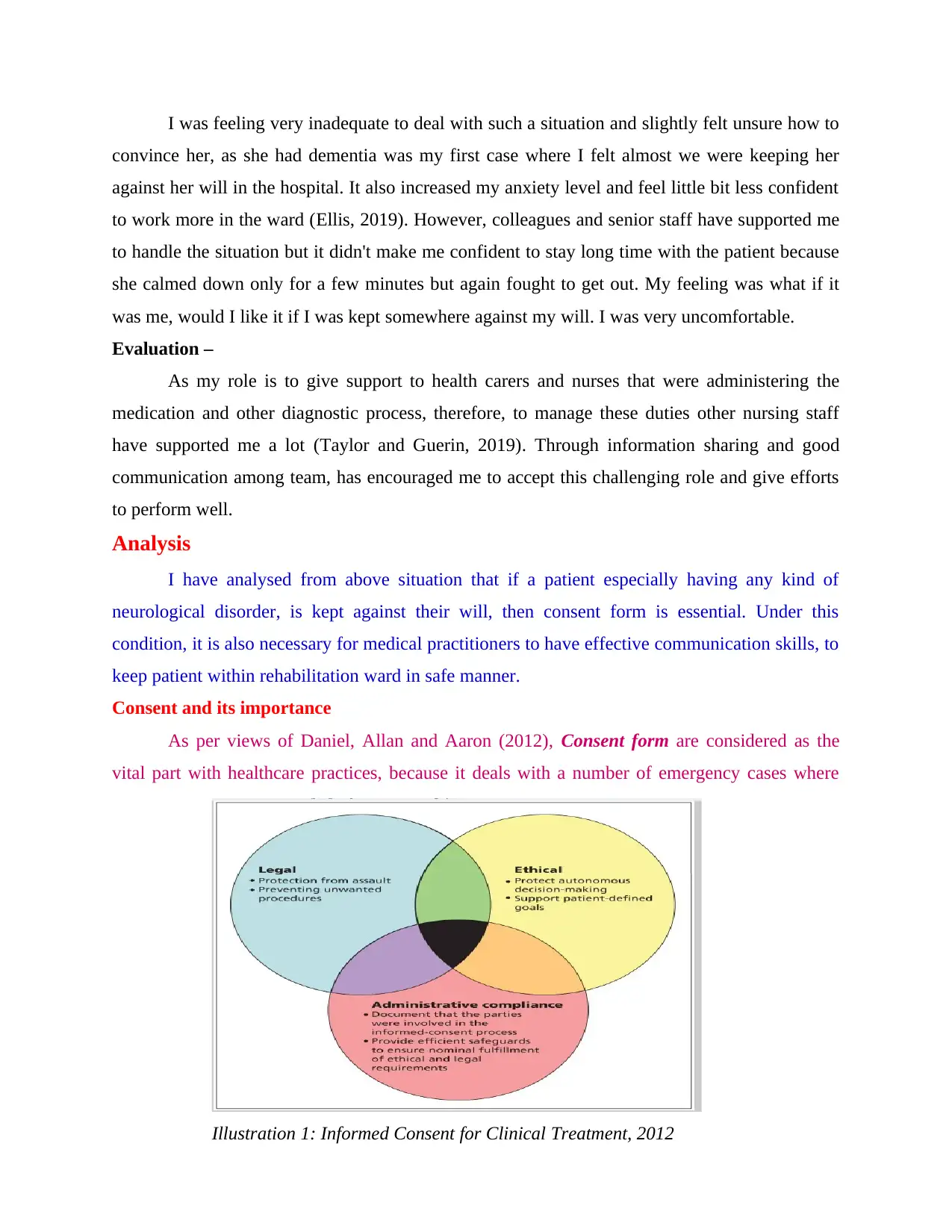
Consent and its importance
As per views of Daniel, Allan and Aaron (2012), Consent form are considered as the
vital part with healthcare practices, because it deals with a number of emergency cases where
7
Illustration 1: Informed Consent for Clinical Treatment, 2012
convince her, as she had dementia was my first case where I felt almost we were keeping her
against her will in the hospital. It also increased my anxiety level and feel little bit less confident
to work more in the ward (Ellis, 2019). However, colleagues and senior staff have supported me
to handle the situation but it didn't make me confident to stay long time with the patient because
she calmed down only for a few minutes but again fought to get out. My feeling was what if it
was me, would I like it if I was kept somewhere against my will. I was very uncomfortable.
Evaluation –
As my role is to give support to health carers and nurses that were administering the
medication and other diagnostic process, therefore, to manage these duties other nursing staff
have supported me a lot (Taylor and Guerin, 2019). Through information sharing and good
communication among team, has encouraged me to accept this challenging role and give efforts
to perform well.
Analysis
I have analysed from above situation that if a patient especially having any kind of
neurological disorder, is kept against their will, then consent form is essential. Under this
condition, it is also necessary for medical practitioners to have effective communication skills, to
keep patient within rehabilitation ward in safe manner.
Consent and its importance
As per views of Daniel, Allan and Aaron (2012), Consent form are considered as the
vital part with healthcare practices, because it deals with a number of emergency cases where
7
Illustration 1: Informed Consent for Clinical Treatment, 2012
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
any step can create a risk for a patient's life. In such a condition, it is essential for healthcare
professionals to obtain a signed consent form by family members of patient so that any decision
taken on the behalf of well-being of patient, can be legal (Informed Consent for Clinical
Treatment, 2012). As per the case analysis, where I have evaluated that how patients against their
will are kept safely in hospitals, when consent form is signed by their family members. Through
this case scenario, first time I was aware with concept of consent form and why it is necessary.
Informed consent refers to be vital document therefore, where to perform all surgical, treatment
and aesthetic procedures, can be taken by informing the patient's family members. It beholds the
ethical principle related to patient dignity and respect including human rights as well, where if
family members are known what procedures are going to be taken for patients surgery or any
other test, then it facilitates a good decision power to health practitioners (Richard, Gagnon and
Careau, 2019). In context with legitimation, signing the consent form also taken is essential from
legal point of view, where family members will not allow to take any legal action in case of
patient death or any risk condition after signing the form (Taylor and Guerin, 2019). This
document includes a detailed information about critical condition of patient, necessary treatment
procedures, consequences, alternative options for treatment, potential risks and benefits etc.
Therefore, getting these information, family members and other relatives of patients can make
their mind about where to give treatment, if such a procedure would help in preventing the
patient or not. While, healthcare practitioners also can provide services more effectively by
getting the support of them. For this purpose, as per 4, 7 and 8 code of NMC, to obtain informed
consent healthcare practitioners are required to need to make proper communication with patient
and their family members, before taking out any actions. This would help in getting support of
them, for proper treatment of patients. Once consent is obtained, hospitals and the staff can
perform all necessary action to treat the patient. The consent form creates trust and positive
relationship between health care givers, patient and their family members by ensuring them good
and high quality of understanding. In addition to this, with the help of consent form the hospital
does not get any kind of negative blame if there is any problem can arise while providing
treatment to the patients.
Skills which are required to get valid consent
8
professionals to obtain a signed consent form by family members of patient so that any decision
taken on the behalf of well-being of patient, can be legal (Informed Consent for Clinical
Treatment, 2012). As per the case analysis, where I have evaluated that how patients against their
will are kept safely in hospitals, when consent form is signed by their family members. Through
this case scenario, first time I was aware with concept of consent form and why it is necessary.
Informed consent refers to be vital document therefore, where to perform all surgical, treatment
and aesthetic procedures, can be taken by informing the patient's family members. It beholds the
ethical principle related to patient dignity and respect including human rights as well, where if
family members are known what procedures are going to be taken for patients surgery or any
other test, then it facilitates a good decision power to health practitioners (Richard, Gagnon and
Careau, 2019). In context with legitimation, signing the consent form also taken is essential from
legal point of view, where family members will not allow to take any legal action in case of
patient death or any risk condition after signing the form (Taylor and Guerin, 2019). This
document includes a detailed information about critical condition of patient, necessary treatment
procedures, consequences, alternative options for treatment, potential risks and benefits etc.
Therefore, getting these information, family members and other relatives of patients can make
their mind about where to give treatment, if such a procedure would help in preventing the
patient or not. While, healthcare practitioners also can provide services more effectively by
getting the support of them. For this purpose, as per 4, 7 and 8 code of NMC, to obtain informed
consent healthcare practitioners are required to need to make proper communication with patient
and their family members, before taking out any actions. This would help in getting support of
them, for proper treatment of patients. Once consent is obtained, hospitals and the staff can
perform all necessary action to treat the patient. The consent form creates trust and positive
relationship between health care givers, patient and their family members by ensuring them good
and high quality of understanding. In addition to this, with the help of consent form the hospital
does not get any kind of negative blame if there is any problem can arise while providing
treatment to the patients.
Skills which are required to get valid consent
8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
For gaining valid consents, it is essential for health practitioners to possess effective
verbal and non-verbal communication skills. These skills are considered as the key part of
relationship between health practitioners and patients during treatment procedure. As per NMC
code 7, it is essential for health practitioners to use proper languages while making
communications with patients, colleagues and other visitors, that they can understand properly.
Through verbal and non-verbal communication skills, health practitioners can easily take valid
consent of patient or relatives, for providing entire information about treatment in ethical way
(Linsley, Kane and Barker, 2019). Having proper communication with patient and relative ones,
health practitioners can inform them about treatment procedures, risks and time that will be taken
for recovery of health, for proper well-being. This would help patients in making decisions to
take such a treatment and give approval accordingly, so that ethics can be maintained. Similarly,
as per NMC code 8, it also depicts that health practitioners must maintain effective
communications with colleagues, so that work can be done through better cooperation. This
would aid to provide effective quality of work with proper care to patients.
Reflective Conclusion –
It has been concluded from this case that patient safety is considered as the heart of
services, where to provide proper care and medical service, it is essential for hospitals to get
consent form signed either by patient or their family members. Through the described situation, I
have analysed that to deal with patient who are kept against their willing in hospitals,
communication skills are necessary to develop. By developing this skill, I can contribute more
efforts and support to other health practitioners to calm down aggressive behaviour of patients
during treatment (Field and Brown, 2019). Along with this, it has been summarised that gaining
consent is legal obligations because it helps in people from assault and prevent them unwanted
procedures. Similarly, it also taken as ethical obligations because it protect autonomous decision
making as well as support the patient defined goals also. Through gaining consent form, medical
professionals can take effective decisions before taking any treatment procedure for well-being
of patients, by providing them entire information. Along with this, as per administrative
compliance, it is essential for healthcare professionals to obtain consent documents which
governs the involvement of associated parties within informed-consent process. In addition to
9
verbal and non-verbal communication skills. These skills are considered as the key part of
relationship between health practitioners and patients during treatment procedure. As per NMC
code 7, it is essential for health practitioners to use proper languages while making
communications with patients, colleagues and other visitors, that they can understand properly.
Through verbal and non-verbal communication skills, health practitioners can easily take valid
consent of patient or relatives, for providing entire information about treatment in ethical way
(Linsley, Kane and Barker, 2019). Having proper communication with patient and relative ones,
health practitioners can inform them about treatment procedures, risks and time that will be taken
for recovery of health, for proper well-being. This would help patients in making decisions to
take such a treatment and give approval accordingly, so that ethics can be maintained. Similarly,
as per NMC code 8, it also depicts that health practitioners must maintain effective
communications with colleagues, so that work can be done through better cooperation. This
would aid to provide effective quality of work with proper care to patients.
Reflective Conclusion –
It has been concluded from this case that patient safety is considered as the heart of
services, where to provide proper care and medical service, it is essential for hospitals to get
consent form signed either by patient or their family members. Through the described situation, I
have analysed that to deal with patient who are kept against their willing in hospitals,
communication skills are necessary to develop. By developing this skill, I can contribute more
efforts and support to other health practitioners to calm down aggressive behaviour of patients
during treatment (Field and Brown, 2019). Along with this, it has been summarised that gaining
consent is legal obligations because it helps in people from assault and prevent them unwanted
procedures. Similarly, it also taken as ethical obligations because it protect autonomous decision
making as well as support the patient defined goals also. Through gaining consent form, medical
professionals can take effective decisions before taking any treatment procedure for well-being
of patients, by providing them entire information. Along with this, as per administrative
compliance, it is essential for healthcare professionals to obtain consent documents which
governs the involvement of associated parties within informed-consent process. In addition to
9

this, gaining consent form also provides efficient safeguards, for ensuring that nominal
fulfilments have been taken about ethical and legal requirements.
Action Plan –
For improvement of my performance, I would like to engage more in such cases where it
almost difficult to handle the patient's mood and influence them to take therapies. For such a
role, I would work more on verbal and non-verbal communication skills that enables me to deal
with difficult situations more easily. Along with this, I would also work more on analysing the
importance of consent form, which is essential to provide effective treatment.
CONCLUSION
To improve quality of healthcare services, reflection is essential that provides a way to
handle complex situations. By reflecting on different situations, health practitioners can evaluate
if actions taken was appropriate or not. This would help in preparing better action plan for
improving services. Within healthcare, reflective practice has defined as an active and dynamic
action-based ethical set of skills which is used to deal with complex, real and difficult situations.
So, utilising this type of practices in nursing field, a person can increase its self-awareness and
creative thinking skills, that refers to be key component of emotional intelligence. This would
help in encouraging the active engagement in healthcare services by identifying a situation where
an individual is encountered with the most drastic situation that could not be handled. For this
purpose, to review what a person has done in past experience, a number of models can be
utilised. It includes Kolb's learning model that helps in evaluating what has been learnt from past
experience and where learning skills are needed to be improved, for performing better in future.
While Gibb's reflective model helps in conducting a deep analysis over past performances and
revealing what has gone well and what's not. This would help in analysing own performance and
evaluating where need to work more, so that risk can be minimised if same situations will occur
in future. From this report, importance of patient informed also analysed, where family member
of the patients understand about various risk, its alternatives as well as possible benefits they get
in return of any treatment they get. Each and every patient have right to know the information
about procedure as well as treatment which they get. Therefore, for health practitioners before
taking any decisions related to patient's treatment procedure, need to take approval of their
family members through consent form.
10
fulfilments have been taken about ethical and legal requirements.
Action Plan –
For improvement of my performance, I would like to engage more in such cases where it
almost difficult to handle the patient's mood and influence them to take therapies. For such a
role, I would work more on verbal and non-verbal communication skills that enables me to deal
with difficult situations more easily. Along with this, I would also work more on analysing the
importance of consent form, which is essential to provide effective treatment.
CONCLUSION
To improve quality of healthcare services, reflection is essential that provides a way to
handle complex situations. By reflecting on different situations, health practitioners can evaluate
if actions taken was appropriate or not. This would help in preparing better action plan for
improving services. Within healthcare, reflective practice has defined as an active and dynamic
action-based ethical set of skills which is used to deal with complex, real and difficult situations.
So, utilising this type of practices in nursing field, a person can increase its self-awareness and
creative thinking skills, that refers to be key component of emotional intelligence. This would
help in encouraging the active engagement in healthcare services by identifying a situation where
an individual is encountered with the most drastic situation that could not be handled. For this
purpose, to review what a person has done in past experience, a number of models can be
utilised. It includes Kolb's learning model that helps in evaluating what has been learnt from past
experience and where learning skills are needed to be improved, for performing better in future.
While Gibb's reflective model helps in conducting a deep analysis over past performances and
revealing what has gone well and what's not. This would help in analysing own performance and
evaluating where need to work more, so that risk can be minimised if same situations will occur
in future. From this report, importance of patient informed also analysed, where family member
of the patients understand about various risk, its alternatives as well as possible benefits they get
in return of any treatment they get. Each and every patient have right to know the information
about procedure as well as treatment which they get. Therefore, for health practitioners before
taking any decisions related to patient's treatment procedure, need to take approval of their
family members through consent form.
10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





