Healthcare Operation Management: Infection Control, Risk and Errors
VerifiedAdded on 2020/04/15
|17
|5424
|90
Report
AI Summary
This report comprehensively examines healthcare operation management, focusing on infection control, risk management, and medical error prevention. The first section addresses infection control methods, data collection, training, and guidelines, including WHO recommendations and roles within the infection control department. The second section explores risk factors associated with surgical site infections, data sources, and the impact of infections on patients and hospitals. The third section delves into risk management, Maxwell's classification, medical error reporting, and the importance of quality improvement programs. The report presents data from physicians and nurses, analyzing the relationship between age, experience, and medical errors, as well as identifying common medical practices and error frequencies. The study uses semi-structured interviews and questionnaires to gather data, ensuring ethical considerations and confidentiality. The report concludes with a discussion of the causes and prevention of medical errors, emphasizing the need for validated processes, government regulations, and hospital policies to improve patient safety and healthcare outcomes.
Healthcare Operation Management
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Assignment task 1:
Q1.
Which are the methods you are well versed for infection control ?
Which are the methods your practiced to collect data and analyse it for infection
control ?
Have you undergone any specific training for infection control and if yes, can you
brief about the training?
Are you aware of the guidelines for infection control?
Whether our facility is following Government and WHO guidelines for infection
control ?
Describe in short roles and responsibilities of the head of infection control
department?
Is our facility made any written infection control policy ?
How much time you are spending on infection control programme ?
What are the commonly used disinfectants useful to prevent surgical site infections?
Which are the most common microorganisms responsible for surgical site infections?
Which is more efficient method for disinfection; local or systemic?
Q2.
Chief of General Surgery can provide data about risk factors associated with the patient.
Older age of the patient, treatment with immunosuppressive agents and malnutrition are
mainly responsible for occurrence of infection in patients. Chief of General surgery can also
provide input related to the operative procedure which are responsible for surgical site
infection (SSI). Factors related to operative procedure include hair removal, inappropriate use
of antimicrobial prophylaxis, duration of the operation and wound classification. Chief of
General Surgery can also give input related to the policies and procedures required for control
of surgical site infections. Information about operation room and isolation precautions can
also be obtained from Chief of General Surgery. Head of the pathology can provide
information about the extent and depth of infection. This information would be helpful in
assessing how old infection was? Input related to type of microorganism like gram positive
and gram negative can be obtained from head of pathology. Information about appearance of
incision can be obtained from head of pathology (Fuller, 2017).
Q3.
2
Q1.
Which are the methods you are well versed for infection control ?
Which are the methods your practiced to collect data and analyse it for infection
control ?
Have you undergone any specific training for infection control and if yes, can you
brief about the training?
Are you aware of the guidelines for infection control?
Whether our facility is following Government and WHO guidelines for infection
control ?
Describe in short roles and responsibilities of the head of infection control
department?
Is our facility made any written infection control policy ?
How much time you are spending on infection control programme ?
What are the commonly used disinfectants useful to prevent surgical site infections?
Which are the most common microorganisms responsible for surgical site infections?
Which is more efficient method for disinfection; local or systemic?
Q2.
Chief of General Surgery can provide data about risk factors associated with the patient.
Older age of the patient, treatment with immunosuppressive agents and malnutrition are
mainly responsible for occurrence of infection in patients. Chief of General surgery can also
provide input related to the operative procedure which are responsible for surgical site
infection (SSI). Factors related to operative procedure include hair removal, inappropriate use
of antimicrobial prophylaxis, duration of the operation and wound classification. Chief of
General Surgery can also give input related to the policies and procedures required for control
of surgical site infections. Information about operation room and isolation precautions can
also be obtained from Chief of General Surgery. Head of the pathology can provide
information about the extent and depth of infection. This information would be helpful in
assessing how old infection was? Input related to type of microorganism like gram positive
and gram negative can be obtained from head of pathology. Information about appearance of
incision can be obtained from head of pathology (Fuller, 2017).
Q3.
2
It has been estimated that approximately 38 % nosocomial infections occur due to surgical
site infections. SSI can occur in three forms like superficial SSI, deep incisional SSI and
organ or space SSS. Superficial, deep incisional and organ SSI can occur within one month,
upto one year and after one year respectively. Infection in the SSI mainly depends on the type
of surgery. Abdominal surgery can lead to infection due to mixed gram positive and gram
negative microorganisms, while extra abdominal surgery lead to infection due to S. aureus
and staphylococcoal infection. SSI can produce abscess formation in patients which is
associated with swelling, pain, redness and warmth. Cellulitis, bacteraemia and urinary tract
infection can occur in patients with SSI.
Surgical site infection can increase readmissions to the hospital. This can produce huge
financial burden on patients. Moreover, repeated hospital vissits can lead to reoccurrence of
infection in SSI patients. Hospital need to improve facilities for patient care hence there
might be augmentation in financial burden on the hospitals for improving healthcare
facilities. Hospital need to keep bed of patient with infection free for few days which can lead
to less revenue for the hospital. Surgeon would be in dilemma prior to surgery due to more
incidence of SSI (Shepard et al., 2013; Jenks et al., 2014).
Q4.
World Health Organisation (WHO) recommendations should be implemented for
infection control and for providing safe environment in the hospital.
Environmental safety Service Staff should be recruited.
More emphasis should be given for disinfecting surgical aids and hands during
surgery.
Meetings should be conducted among all the stakeholders on regular basis to prevent
occurrence of infection.
Validated room cleaning checklist should be implemented.
High touch areas should be given more attention for disinfection.
Personal protective equipment (PPE) should be kept outside operation theatre and
patients room. (Isaacson, 2012)
3
site infections. SSI can occur in three forms like superficial SSI, deep incisional SSI and
organ or space SSS. Superficial, deep incisional and organ SSI can occur within one month,
upto one year and after one year respectively. Infection in the SSI mainly depends on the type
of surgery. Abdominal surgery can lead to infection due to mixed gram positive and gram
negative microorganisms, while extra abdominal surgery lead to infection due to S. aureus
and staphylococcoal infection. SSI can produce abscess formation in patients which is
associated with swelling, pain, redness and warmth. Cellulitis, bacteraemia and urinary tract
infection can occur in patients with SSI.
Surgical site infection can increase readmissions to the hospital. This can produce huge
financial burden on patients. Moreover, repeated hospital vissits can lead to reoccurrence of
infection in SSI patients. Hospital need to improve facilities for patient care hence there
might be augmentation in financial burden on the hospitals for improving healthcare
facilities. Hospital need to keep bed of patient with infection free for few days which can lead
to less revenue for the hospital. Surgeon would be in dilemma prior to surgery due to more
incidence of SSI (Shepard et al., 2013; Jenks et al., 2014).
Q4.
World Health Organisation (WHO) recommendations should be implemented for
infection control and for providing safe environment in the hospital.
Environmental safety Service Staff should be recruited.
More emphasis should be given for disinfecting surgical aids and hands during
surgery.
Meetings should be conducted among all the stakeholders on regular basis to prevent
occurrence of infection.
Validated room cleaning checklist should be implemented.
High touch areas should be given more attention for disinfection.
Personal protective equipment (PPE) should be kept outside operation theatre and
patients room. (Isaacson, 2012)
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Assignment task 2 :
Q1.
Risk management can be beneficial in reducing errors which can produce harm to the patients
and ultimately reduce financial burden on the patient. Hence, risk management can be
beneficial in improving overall quality of the patient care. Risk management can implement
coherent approach to improve patient care. Risk management can predict harm to the patient,
hence precautions can be taken to reduce this harm. Risk management can improve complete
procedure of care to the patient.
Q2.
Maxwell’s classification is based on different criterias like effectiveness, efficiency, relevance,
acceptability, access, and equity.
Effectiveness: Outpatient clinics have highly qualified staff well versed with medical procedures
and skills and implement suitable technology.
Efficiency: Outpatient clinics operate at low cost and produce optimum work with existing staff.
It maintains proper electronic record of patients which is helpful in improving efficiency of care
to the patients.
Acceptability: Outpatient clinics provide seats and lounges in the waiting room for the patients
and their relatives. Concerns of the patient and family members transfer effectively to clinicians
and feedback from the clinicians pass on to the patient and family members.
Relevance: In outpatient clinics, there is appropriate use of all the resources for improving health
of the patients.
Access: Outpatient clinics are easily accessible and care can be provided within stipulated
timeline without long duration waiting.
Equity: There is no discrimination of the patient based on factors like social, cultural,
financial and ethnic.
Q3.
Medical error reporting, its discussion and corrective measures for these errors are important
components of patient safety. In hospitals with multiple departments, medical errors are being
reported less often due to insecurity of loss of job.
4
Q1.
Risk management can be beneficial in reducing errors which can produce harm to the patients
and ultimately reduce financial burden on the patient. Hence, risk management can be
beneficial in improving overall quality of the patient care. Risk management can implement
coherent approach to improve patient care. Risk management can predict harm to the patient,
hence precautions can be taken to reduce this harm. Risk management can improve complete
procedure of care to the patient.
Q2.
Maxwell’s classification is based on different criterias like effectiveness, efficiency, relevance,
acceptability, access, and equity.
Effectiveness: Outpatient clinics have highly qualified staff well versed with medical procedures
and skills and implement suitable technology.
Efficiency: Outpatient clinics operate at low cost and produce optimum work with existing staff.
It maintains proper electronic record of patients which is helpful in improving efficiency of care
to the patients.
Acceptability: Outpatient clinics provide seats and lounges in the waiting room for the patients
and their relatives. Concerns of the patient and family members transfer effectively to clinicians
and feedback from the clinicians pass on to the patient and family members.
Relevance: In outpatient clinics, there is appropriate use of all the resources for improving health
of the patients.
Access: Outpatient clinics are easily accessible and care can be provided within stipulated
timeline without long duration waiting.
Equity: There is no discrimination of the patient based on factors like social, cultural,
financial and ethnic.
Q3.
Medical error reporting, its discussion and corrective measures for these errors are important
components of patient safety. In hospitals with multiple departments, medical errors are being
reported less often due to insecurity of loss of job.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Insufficient communication among medical staff of various departments. This might be due
to ban on use mobile phones in the hospital premises during official working hours.
Q4.
Additional characteristics include:
Highly qualified and trained management staff.
Acceptability of change in the process in the hospital during transformation.
Sustained quality improvement programme.
Implementation of changes according to the requirements of the global changes.
Implementation of effective communication system.
Healthcare staff and patient management.
Q5.
There is interaction between risk management and Donabedian’s, Maxwell’s classification of
quality. This interaction can be demonstrated by providing platform to fix the characteristics
of quality and planning measures to eliminate deficiencies to achieve quality. Risk
management is important aspect in the healthcare organisation because serious issues can
arise from the medical errors.
Effectiveness: Risk management can be helpful in understanding skill levels of staff,
equipments and modern technologies for meeting quality compliance. It can also be helpful in
achieving desired output for the patients and aim for the organisation. Risk management is
helpful in implementing required changes to avoid medical errors and implementing effective
quality.
Efficiency: Risk management make sure that there is cost effective and optimum utilization
of the resources for improving quality in healthcare organisation. Risk management also
ensures that there should not be unnecessary outcome of the intervention in the healthcare
facility.
Relevance : Risk management ensures that there is relevant data collected for assessing
health of patient. Moreover, it also ensures that appropriate intervention is provided to the
patient.
5
to ban on use mobile phones in the hospital premises during official working hours.
Q4.
Additional characteristics include:
Highly qualified and trained management staff.
Acceptability of change in the process in the hospital during transformation.
Sustained quality improvement programme.
Implementation of changes according to the requirements of the global changes.
Implementation of effective communication system.
Healthcare staff and patient management.
Q5.
There is interaction between risk management and Donabedian’s, Maxwell’s classification of
quality. This interaction can be demonstrated by providing platform to fix the characteristics
of quality and planning measures to eliminate deficiencies to achieve quality. Risk
management is important aspect in the healthcare organisation because serious issues can
arise from the medical errors.
Effectiveness: Risk management can be helpful in understanding skill levels of staff,
equipments and modern technologies for meeting quality compliance. It can also be helpful in
achieving desired output for the patients and aim for the organisation. Risk management is
helpful in implementing required changes to avoid medical errors and implementing effective
quality.
Efficiency: Risk management make sure that there is cost effective and optimum utilization
of the resources for improving quality in healthcare organisation. Risk management also
ensures that there should not be unnecessary outcome of the intervention in the healthcare
facility.
Relevance : Risk management ensures that there is relevant data collected for assessing
health of patient. Moreover, it also ensures that appropriate intervention is provided to the
patient.
5
Acceptability: In risk management there is provision for collection of responses form the
patient and these responses can be utilised for improvement in provision of healthcare
services to the patients and achieve complete satisfaction for the patients.
Access: Risk management assess reasons for not receiving appropriate intervention for
patients and its potential financial impact on the patient and hospital. Higher authorities in the
risk management department design strategies for improving access of appropriate healthcare
intervention to the patient. It would also be helpful in reducing adverse effects to the patients
due to less access to the healthcare interventions.
Equity: Risk management ensures that provision of medical services is devoid of bias and
these medical services should not vary based on social, financial and cultural aspects of the
patient. Risk management analyses rise of adverse effects due to unequal provision of
healthcare services. It also ensures provision of strategies to minimize these adverse effects.
6
patient and these responses can be utilised for improvement in provision of healthcare
services to the patients and achieve complete satisfaction for the patients.
Access: Risk management assess reasons for not receiving appropriate intervention for
patients and its potential financial impact on the patient and hospital. Higher authorities in the
risk management department design strategies for improving access of appropriate healthcare
intervention to the patient. It would also be helpful in reducing adverse effects to the patients
due to less access to the healthcare interventions.
Equity: Risk management ensures that provision of medical services is devoid of bias and
these medical services should not vary based on social, financial and cultural aspects of the
patient. Risk management analyses rise of adverse effects due to unequal provision of
healthcare services. It also ensures provision of strategies to minimize these adverse effects.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Assignment 3 :
Background/ Introduction:
Medial error can be categorised in two classes like error of execution and error of planning.
Error of execution include failure in administering planned medications and error of planning
include implementation of wrong plan to achieve desired outcome in the patient. Medical
errors are one of the most significant health problems. Since, long time medical errors are
responsible for the comprised patient safety. Medical errors not only affect patients but it also
affects family members. Staff also get affected due to medical errors because ethical issues
might arise due to medical errors, moreover staff might lose job due to medical errors.
Medical errors can produce huge financial burden on the hospitals for providing
supplementary health intervention and expenditure might also come through Lawsuit.
Medical errors and it consequences can be effectively managed by implementing regulated
healthcare services in the hospital. Effective reporting and management of the medical errors
can be regulated by making compulsion of licenses to the healthcare facilities and it should
be regulated by federal bodies. It is evident that majority of the medical errors do not occur
due to solely human errors, however defective process and systems in the organisation are
major contributors for the medical errors (Reason, 2001). Inadequate skill for the
implementation of processes and variable processes are also responsible for medical errors
(Kalra, 2011).
Potential outcomes of the medical errors mainly based on the type of patient like inpatient or
outpatient and procedure like surgery or medication. For the prevention of medical errors,
effective strategy need to be implemented. Medical error prevention strategy should include
validated processes and systems. These processes and systems should include prevention of
human errors and plan to compensate adverse events which would arise due to human errors.
Multiple strategies should be implemented like patient education, government regulations,
government investment and hospital policy. Medical errors can impact health, social and
economic wellbeing of the patient (Nguyen and Nguyen, 2016).
This study is designed not only to identify problems which can arise due to medical errors but
also solution would be provided to solve these problems. These solutions would be based on
the literature and validated methodologies. More attention would be given to the
identification of the errors and accurate reporting of the errors.
7
Background/ Introduction:
Medial error can be categorised in two classes like error of execution and error of planning.
Error of execution include failure in administering planned medications and error of planning
include implementation of wrong plan to achieve desired outcome in the patient. Medical
errors are one of the most significant health problems. Since, long time medical errors are
responsible for the comprised patient safety. Medical errors not only affect patients but it also
affects family members. Staff also get affected due to medical errors because ethical issues
might arise due to medical errors, moreover staff might lose job due to medical errors.
Medical errors can produce huge financial burden on the hospitals for providing
supplementary health intervention and expenditure might also come through Lawsuit.
Medical errors and it consequences can be effectively managed by implementing regulated
healthcare services in the hospital. Effective reporting and management of the medical errors
can be regulated by making compulsion of licenses to the healthcare facilities and it should
be regulated by federal bodies. It is evident that majority of the medical errors do not occur
due to solely human errors, however defective process and systems in the organisation are
major contributors for the medical errors (Reason, 2001). Inadequate skill for the
implementation of processes and variable processes are also responsible for medical errors
(Kalra, 2011).
Potential outcomes of the medical errors mainly based on the type of patient like inpatient or
outpatient and procedure like surgery or medication. For the prevention of medical errors,
effective strategy need to be implemented. Medical error prevention strategy should include
validated processes and systems. These processes and systems should include prevention of
human errors and plan to compensate adverse events which would arise due to human errors.
Multiple strategies should be implemented like patient education, government regulations,
government investment and hospital policy. Medical errors can impact health, social and
economic wellbeing of the patient (Nguyen and Nguyen, 2016).
This study is designed not only to identify problems which can arise due to medical errors but
also solution would be provided to solve these problems. These solutions would be based on
the literature and validated methodologies. More attention would be given to the
identification of the errors and accurate reporting of the errors.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Objectives:
To identify reasons for occurrence of medical errors in the healthcare facility.
To provide solution to prevent medical facility.
To implement validated and well researched method to identify reasons for medical
errors.
To provide solution to prevent medical errors based on evidence.
Data and inputs:
In this study, data was collected from 100 physicians and 200 nurses from the 50 hospitals.
Data will be collected by implementing semi-structured interviews because in this frame
work of interviews questions can be modified slightly based on the persons. Questionnaires
will be prepared for each aspects of data collection. This data was collected by sending
questionnaire through mail and response was received through mail. Ethical and
confidentiality consideration were made during data collection to prevent bias in the data.
These include identity and occupation of patient, physician and nurse were confidential. It
helped in giving honest response. Data provider should have knowledge about the medical
errors. Hence physicians and nurses were selected for the data collection. Patients were not
considered for the data collection because patient might not aware of the details of the
medical errors. Collected data was arranged in the Excel sheet. Both qualitative and
quantitative data was collected during the study.
Following were the questions included in the questionnaires :
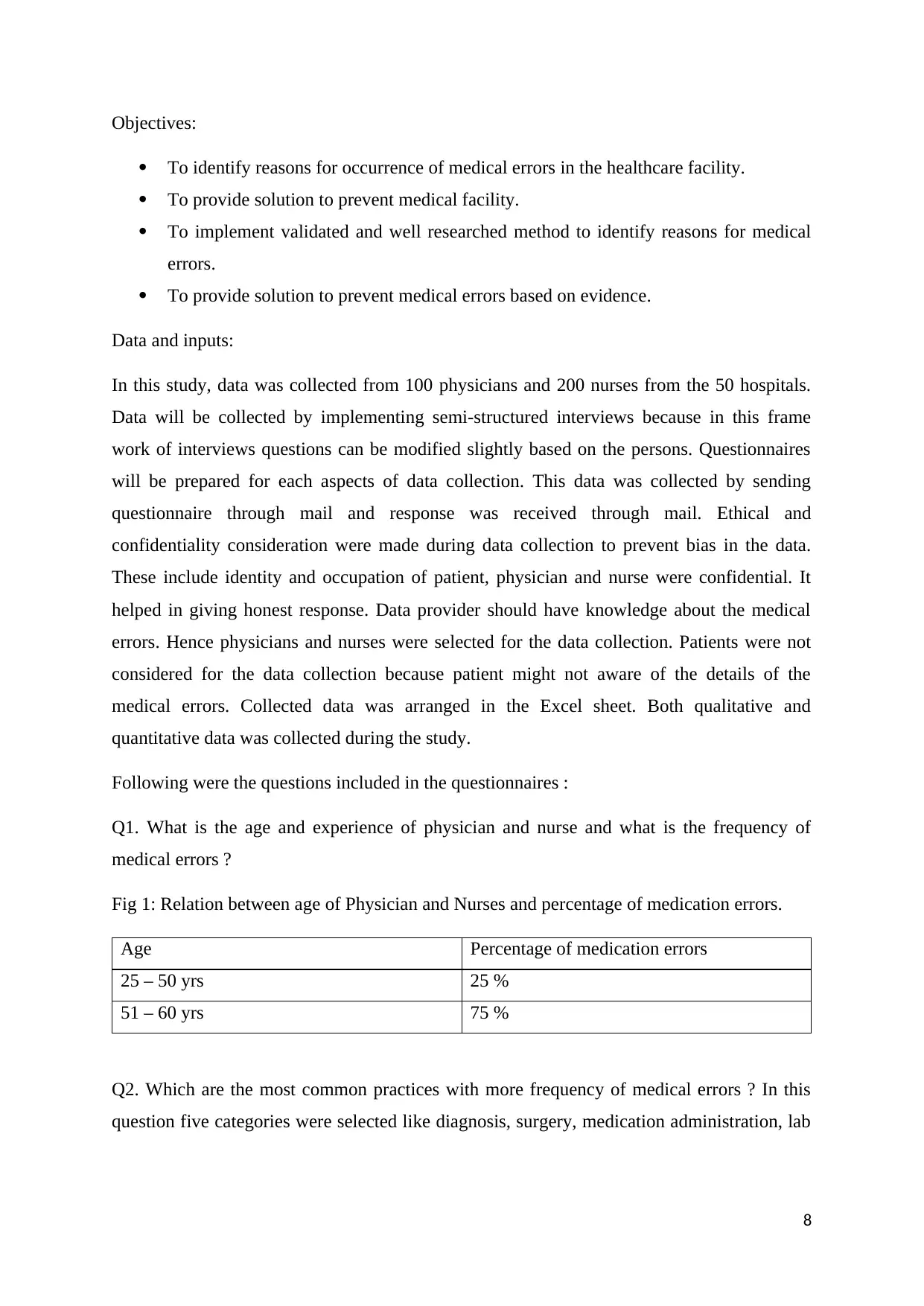
Q1. What is the age and experience of physician and nurse and what is the frequency of
medical errors ?
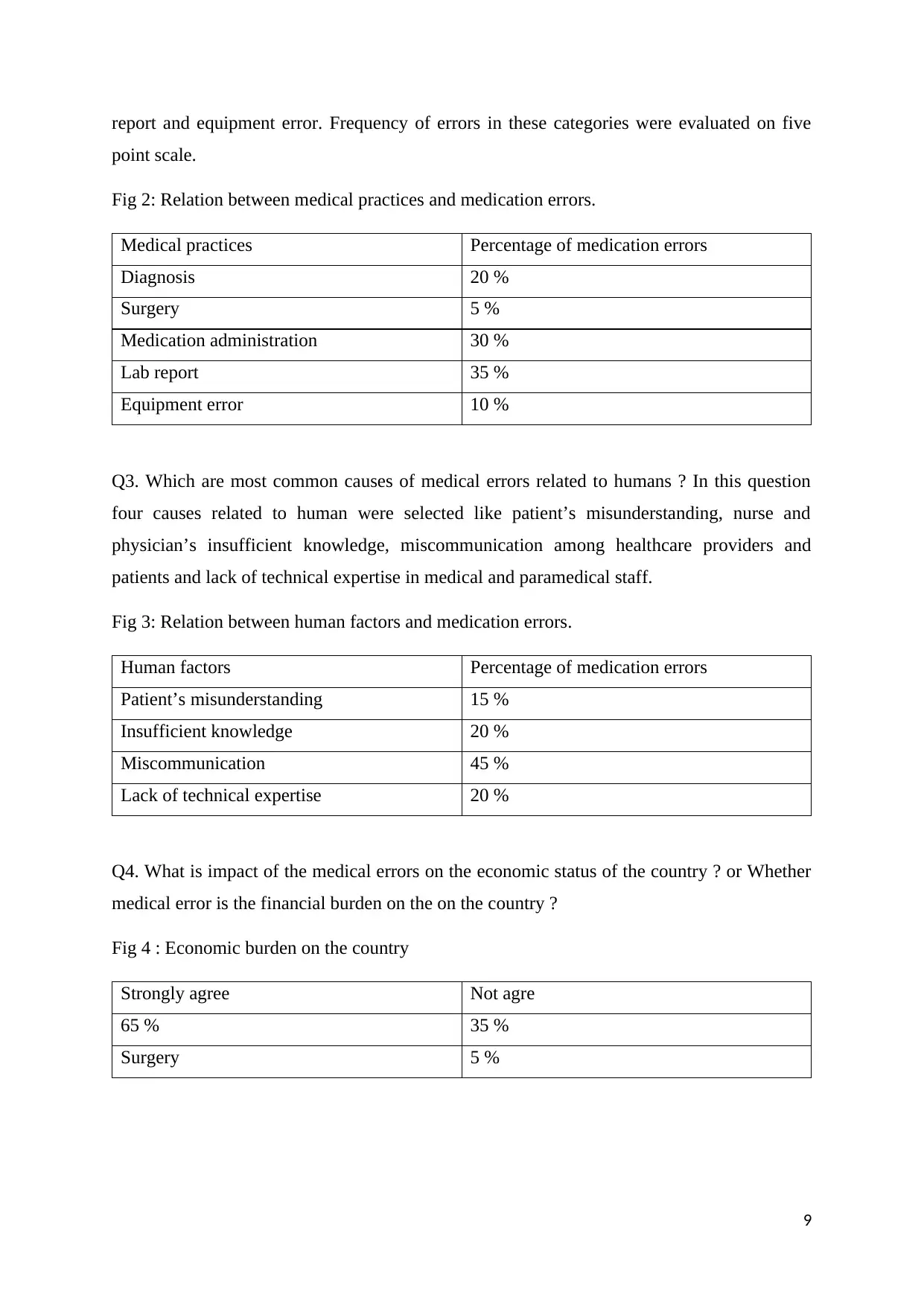
Fig 1: Relation between age of Physician and Nurses and percentage of medication errors.
Age Percentage of medication errors
25 – 50 yrs 25 %
51 – 60 yrs 75 %
Q2. Which are the most common practices with more frequency of medical errors ? In this
question five categories were selected like diagnosis, surgery, medication administration, lab
8
To identify reasons for occurrence of medical errors in the healthcare facility.
To provide solution to prevent medical facility.
To implement validated and well researched method to identify reasons for medical
errors.
To provide solution to prevent medical errors based on evidence.
Data and inputs:
In this study, data was collected from 100 physicians and 200 nurses from the 50 hospitals.
Data will be collected by implementing semi-structured interviews because in this frame
work of interviews questions can be modified slightly based on the persons. Questionnaires
will be prepared for each aspects of data collection. This data was collected by sending
questionnaire through mail and response was received through mail. Ethical and
confidentiality consideration were made during data collection to prevent bias in the data.
These include identity and occupation of patient, physician and nurse were confidential. It
helped in giving honest response. Data provider should have knowledge about the medical
errors. Hence physicians and nurses were selected for the data collection. Patients were not
considered for the data collection because patient might not aware of the details of the
medical errors. Collected data was arranged in the Excel sheet. Both qualitative and
quantitative data was collected during the study.
Following were the questions included in the questionnaires :
Q1. What is the age and experience of physician and nurse and what is the frequency of
medical errors ?
Fig 1: Relation between age of Physician and Nurses and percentage of medication errors.
Age Percentage of medication errors
25 – 50 yrs 25 %
51 – 60 yrs 75 %
Q2. Which are the most common practices with more frequency of medical errors ? In this
question five categories were selected like diagnosis, surgery, medication administration, lab
8
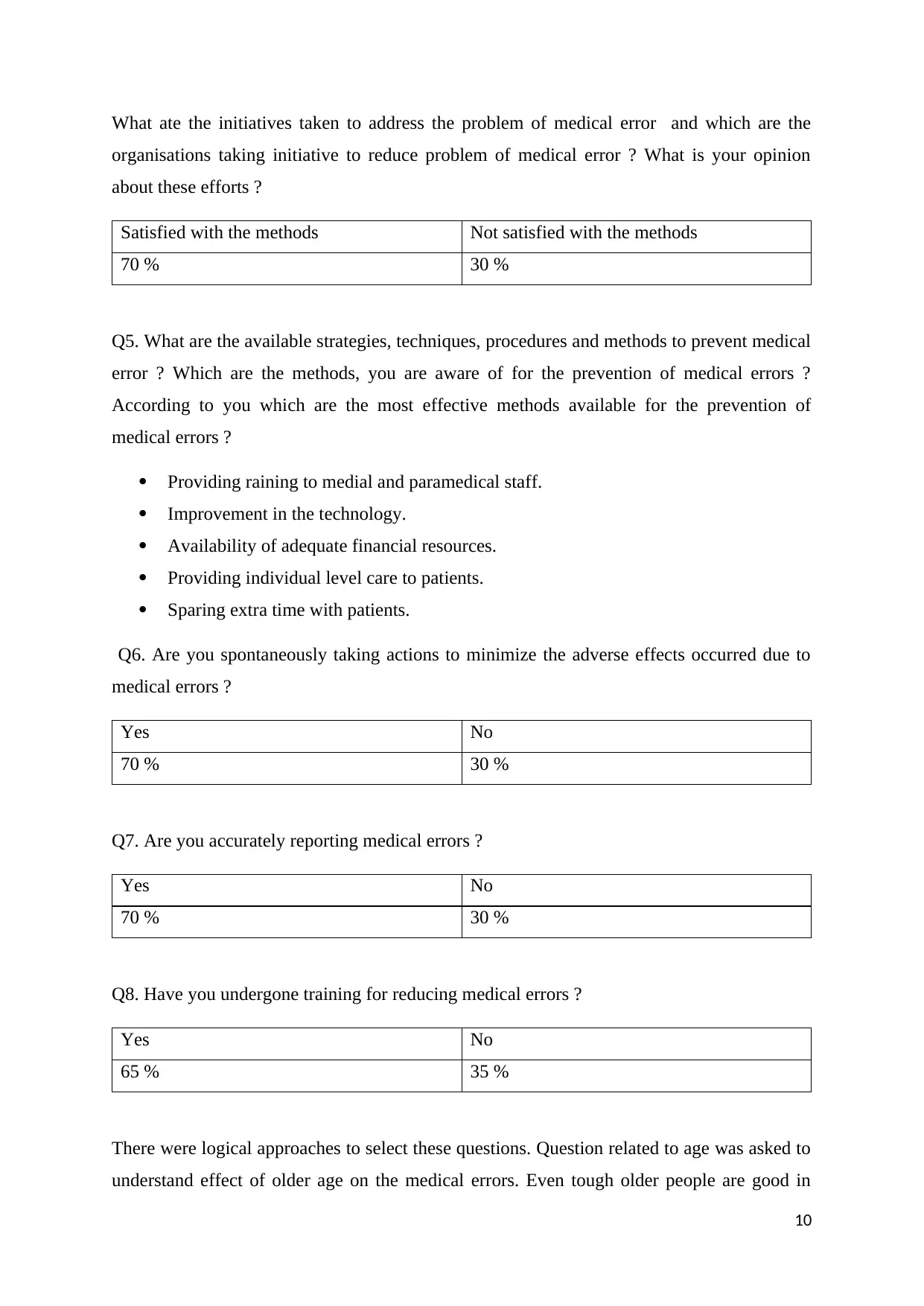
report and equipment error. Frequency of errors in these categories were evaluated on five
point scale.
Fig 2: Relation between medical practices and medication errors.
Medical practices Percentage of medication errors
Diagnosis 20 %
Surgery 5 %
Medication administration 30 %
Lab report 35 %
Equipment error 10 %
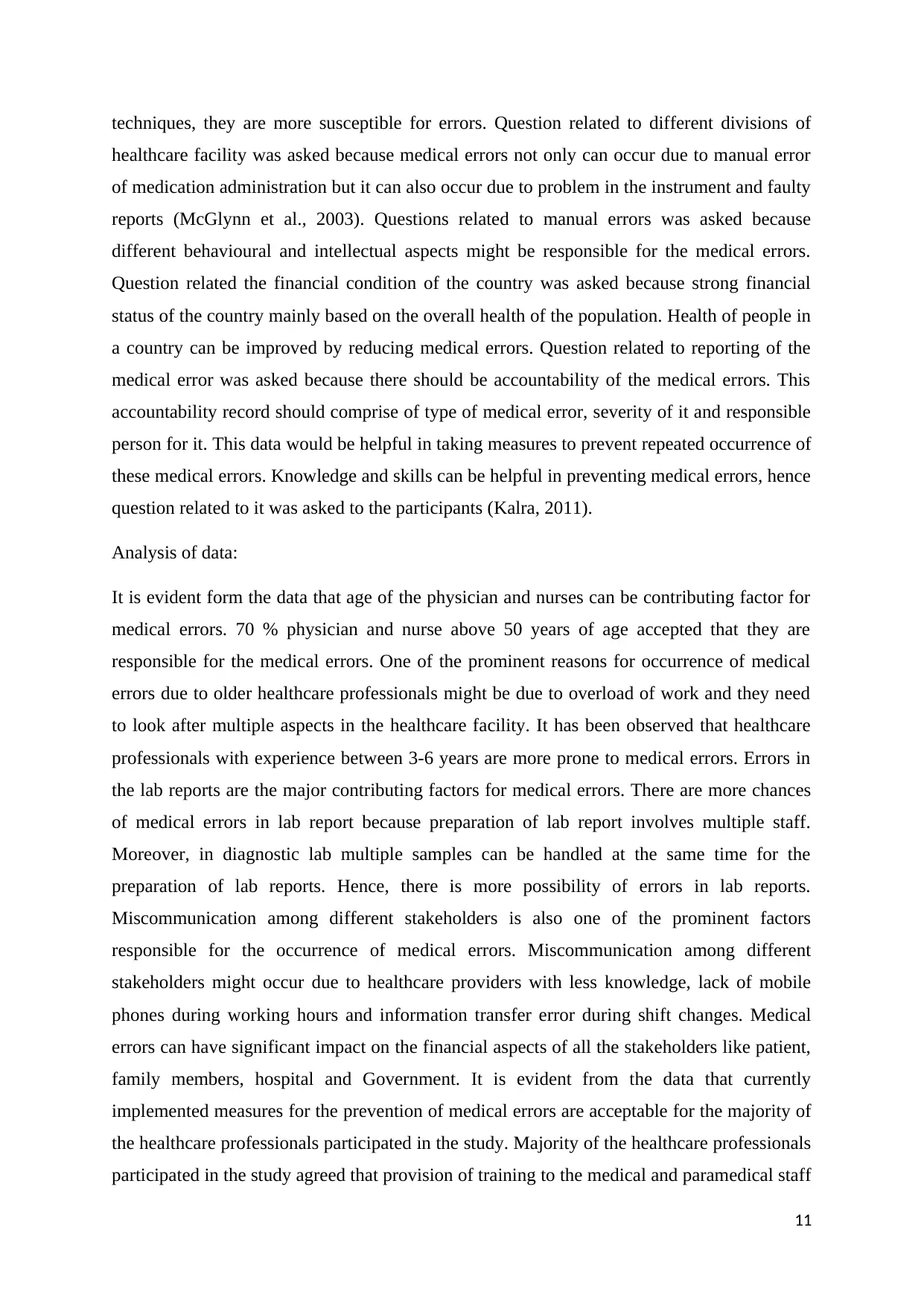
Q3. Which are most common causes of medical errors related to humans ? In this question
four causes related to human were selected like patient’s misunderstanding, nurse and
physician’s insufficient knowledge, miscommunication among healthcare providers and
patients and lack of technical expertise in medical and paramedical staff.
Fig 3: Relation between human factors and medication errors.
Human factors Percentage of medication errors
Patient’s misunderstanding 15 %
Insufficient knowledge 20 %
Miscommunication 45 %
Lack of technical expertise 20 %
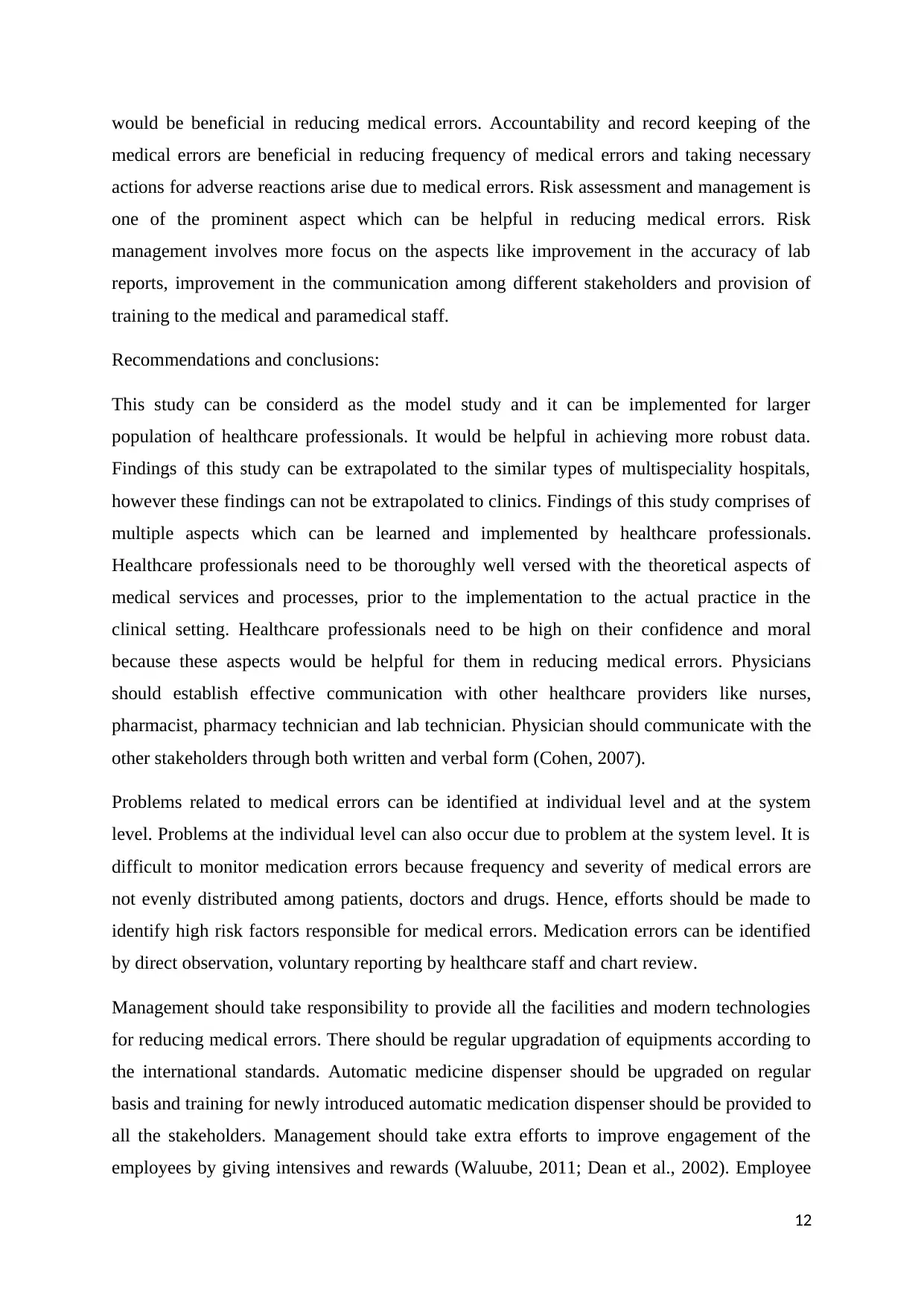
Q4. What is impact of the medical errors on the economic status of the country ? or Whether
medical error is the financial burden on the on the country ?
Fig 4 : Economic burden on the country
Strongly agree Not agre
65 % 35 %
Surgery 5 %
9
point scale.
Fig 2: Relation between medical practices and medication errors.
Medical practices Percentage of medication errors
Diagnosis 20 %
Surgery 5 %
Medication administration 30 %
Lab report 35 %
Equipment error 10 %
Q3. Which are most common causes of medical errors related to humans ? In this question
four causes related to human were selected like patient’s misunderstanding, nurse and
physician’s insufficient knowledge, miscommunication among healthcare providers and
patients and lack of technical expertise in medical and paramedical staff.
Fig 3: Relation between human factors and medication errors.
Human factors Percentage of medication errors
Patient’s misunderstanding 15 %
Insufficient knowledge 20 %
Miscommunication 45 %
Lack of technical expertise 20 %
Q4. What is impact of the medical errors on the economic status of the country ? or Whether
medical error is the financial burden on the on the country ?
Fig 4 : Economic burden on the country
Strongly agree Not agre
65 % 35 %
Surgery 5 %
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
What ate the initiatives taken to address the problem of medical error and which are the
organisations taking initiative to reduce problem of medical error ? What is your opinion
about these efforts ?
Satisfied with the methods Not satisfied with the methods
70 % 30 %
Q5. What are the available strategies, techniques, procedures and methods to prevent medical
error ? Which are the methods, you are aware of for the prevention of medical errors ?
According to you which are the most effective methods available for the prevention of
medical errors ?
Providing raining to medial and paramedical staff.
Improvement in the technology.
Availability of adequate financial resources.
Providing individual level care to patients.
Sparing extra time with patients.
Q6. Are you spontaneously taking actions to minimize the adverse effects occurred due to
medical errors ?
Yes No
70 % 30 %
Q7. Are you accurately reporting medical errors ?
Yes No
70 % 30 %
Q8. Have you undergone training for reducing medical errors ?
Yes No
65 % 35 %
There were logical approaches to select these questions. Question related to age was asked to
understand effect of older age on the medical errors. Even tough older people are good in
10
organisations taking initiative to reduce problem of medical error ? What is your opinion
about these efforts ?
Satisfied with the methods Not satisfied with the methods
70 % 30 %
Q5. What are the available strategies, techniques, procedures and methods to prevent medical
error ? Which are the methods, you are aware of for the prevention of medical errors ?
According to you which are the most effective methods available for the prevention of
medical errors ?
Providing raining to medial and paramedical staff.
Improvement in the technology.
Availability of adequate financial resources.
Providing individual level care to patients.
Sparing extra time with patients.
Q6. Are you spontaneously taking actions to minimize the adverse effects occurred due to
medical errors ?
Yes No
70 % 30 %
Q7. Are you accurately reporting medical errors ?
Yes No
70 % 30 %
Q8. Have you undergone training for reducing medical errors ?
Yes No
65 % 35 %
There were logical approaches to select these questions. Question related to age was asked to
understand effect of older age on the medical errors. Even tough older people are good in
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
techniques, they are more susceptible for errors. Question related to different divisions of
healthcare facility was asked because medical errors not only can occur due to manual error
of medication administration but it can also occur due to problem in the instrument and faulty
reports (McGlynn et al., 2003). Questions related to manual errors was asked because
different behavioural and intellectual aspects might be responsible for the medical errors.
Question related the financial condition of the country was asked because strong financial
status of the country mainly based on the overall health of the population. Health of people in
a country can be improved by reducing medical errors. Question related to reporting of the
medical error was asked because there should be accountability of the medical errors. This
accountability record should comprise of type of medical error, severity of it and responsible
person for it. This data would be helpful in taking measures to prevent repeated occurrence of
these medical errors. Knowledge and skills can be helpful in preventing medical errors, hence
question related to it was asked to the participants (Kalra, 2011).
Analysis of data:
It is evident form the data that age of the physician and nurses can be contributing factor for
medical errors. 70 % physician and nurse above 50 years of age accepted that they are
responsible for the medical errors. One of the prominent reasons for occurrence of medical
errors due to older healthcare professionals might be due to overload of work and they need
to look after multiple aspects in the healthcare facility. It has been observed that healthcare
professionals with experience between 3-6 years are more prone to medical errors. Errors in
the lab reports are the major contributing factors for medical errors. There are more chances
of medical errors in lab report because preparation of lab report involves multiple staff.
Moreover, in diagnostic lab multiple samples can be handled at the same time for the
preparation of lab reports. Hence, there is more possibility of errors in lab reports.
Miscommunication among different stakeholders is also one of the prominent factors
responsible for the occurrence of medical errors. Miscommunication among different
stakeholders might occur due to healthcare providers with less knowledge, lack of mobile
phones during working hours and information transfer error during shift changes. Medical
errors can have significant impact on the financial aspects of all the stakeholders like patient,
family members, hospital and Government. It is evident from the data that currently
implemented measures for the prevention of medical errors are acceptable for the majority of
the healthcare professionals participated in the study. Majority of the healthcare professionals
participated in the study agreed that provision of training to the medical and paramedical staff
11
healthcare facility was asked because medical errors not only can occur due to manual error
of medication administration but it can also occur due to problem in the instrument and faulty
reports (McGlynn et al., 2003). Questions related to manual errors was asked because
different behavioural and intellectual aspects might be responsible for the medical errors.
Question related the financial condition of the country was asked because strong financial
status of the country mainly based on the overall health of the population. Health of people in
a country can be improved by reducing medical errors. Question related to reporting of the
medical error was asked because there should be accountability of the medical errors. This
accountability record should comprise of type of medical error, severity of it and responsible
person for it. This data would be helpful in taking measures to prevent repeated occurrence of
these medical errors. Knowledge and skills can be helpful in preventing medical errors, hence
question related to it was asked to the participants (Kalra, 2011).
Analysis of data:
It is evident form the data that age of the physician and nurses can be contributing factor for
medical errors. 70 % physician and nurse above 50 years of age accepted that they are
responsible for the medical errors. One of the prominent reasons for occurrence of medical
errors due to older healthcare professionals might be due to overload of work and they need
to look after multiple aspects in the healthcare facility. It has been observed that healthcare
professionals with experience between 3-6 years are more prone to medical errors. Errors in
the lab reports are the major contributing factors for medical errors. There are more chances
of medical errors in lab report because preparation of lab report involves multiple staff.
Moreover, in diagnostic lab multiple samples can be handled at the same time for the
preparation of lab reports. Hence, there is more possibility of errors in lab reports.
Miscommunication among different stakeholders is also one of the prominent factors
responsible for the occurrence of medical errors. Miscommunication among different
stakeholders might occur due to healthcare providers with less knowledge, lack of mobile
phones during working hours and information transfer error during shift changes. Medical
errors can have significant impact on the financial aspects of all the stakeholders like patient,
family members, hospital and Government. It is evident from the data that currently
implemented measures for the prevention of medical errors are acceptable for the majority of
the healthcare professionals participated in the study. Majority of the healthcare professionals
participated in the study agreed that provision of training to the medical and paramedical staff
11
would be beneficial in reducing medical errors. Accountability and record keeping of the
medical errors are beneficial in reducing frequency of medical errors and taking necessary
actions for adverse reactions arise due to medical errors. Risk assessment and management is
one of the prominent aspect which can be helpful in reducing medical errors. Risk
management involves more focus on the aspects like improvement in the accuracy of lab
reports, improvement in the communication among different stakeholders and provision of
training to the medical and paramedical staff.
Recommendations and conclusions:
This study can be considerd as the model study and it can be implemented for larger
population of healthcare professionals. It would be helpful in achieving more robust data.
Findings of this study can be extrapolated to the similar types of multispeciality hospitals,
however these findings can not be extrapolated to clinics. Findings of this study comprises of
multiple aspects which can be learned and implemented by healthcare professionals.
Healthcare professionals need to be thoroughly well versed with the theoretical aspects of
medical services and processes, prior to the implementation to the actual practice in the
clinical setting. Healthcare professionals need to be high on their confidence and moral
because these aspects would be helpful for them in reducing medical errors. Physicians
should establish effective communication with other healthcare providers like nurses,
pharmacist, pharmacy technician and lab technician. Physician should communicate with the
other stakeholders through both written and verbal form (Cohen, 2007).
Problems related to medical errors can be identified at individual level and at the system
level. Problems at the individual level can also occur due to problem at the system level. It is
difficult to monitor medication errors because frequency and severity of medical errors are
not evenly distributed among patients, doctors and drugs. Hence, efforts should be made to
identify high risk factors responsible for medical errors. Medication errors can be identified
by direct observation, voluntary reporting by healthcare staff and chart review.
Management should take responsibility to provide all the facilities and modern technologies
for reducing medical errors. There should be regular upgradation of equipments according to
the international standards. Automatic medicine dispenser should be upgraded on regular
basis and training for newly introduced automatic medication dispenser should be provided to
all the stakeholders. Management should take extra efforts to improve engagement of the
employees by giving intensives and rewards (Waluube, 2011; Dean et al., 2002). Employee
12
medical errors are beneficial in reducing frequency of medical errors and taking necessary
actions for adverse reactions arise due to medical errors. Risk assessment and management is
one of the prominent aspect which can be helpful in reducing medical errors. Risk
management involves more focus on the aspects like improvement in the accuracy of lab
reports, improvement in the communication among different stakeholders and provision of
training to the medical and paramedical staff.
Recommendations and conclusions:
This study can be considerd as the model study and it can be implemented for larger
population of healthcare professionals. It would be helpful in achieving more robust data.
Findings of this study can be extrapolated to the similar types of multispeciality hospitals,
however these findings can not be extrapolated to clinics. Findings of this study comprises of
multiple aspects which can be learned and implemented by healthcare professionals.
Healthcare professionals need to be thoroughly well versed with the theoretical aspects of
medical services and processes, prior to the implementation to the actual practice in the
clinical setting. Healthcare professionals need to be high on their confidence and moral
because these aspects would be helpful for them in reducing medical errors. Physicians
should establish effective communication with other healthcare providers like nurses,
pharmacist, pharmacy technician and lab technician. Physician should communicate with the
other stakeholders through both written and verbal form (Cohen, 2007).
Problems related to medical errors can be identified at individual level and at the system
level. Problems at the individual level can also occur due to problem at the system level. It is
difficult to monitor medication errors because frequency and severity of medical errors are
not evenly distributed among patients, doctors and drugs. Hence, efforts should be made to
identify high risk factors responsible for medical errors. Medication errors can be identified
by direct observation, voluntary reporting by healthcare staff and chart review.
Management should take responsibility to provide all the facilities and modern technologies
for reducing medical errors. There should be regular upgradation of equipments according to
the international standards. Automatic medicine dispenser should be upgraded on regular
basis and training for newly introduced automatic medication dispenser should be provided to
all the stakeholders. Management should take extra efforts to improve engagement of the
employees by giving intensives and rewards (Waluube, 2011; Dean et al., 2002). Employee
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



