IT Healthcare Systems: EHR, Regulations, and Incentives
VerifiedAdded on 2022/10/04
|11
|2260
|155
Report
AI Summary
This report provides a comprehensive overview of the integration of Information Technology (IT) within healthcare systems. It explores the significant impact of IT on healthcare delivery, emphasizing the role of Electronic Health Records (EHRs) in enhancing patient care and achieving health equity. The report delves into the implications and uses of IT, highlighting its capacity to improve the safety, quality, and efficiency of healthcare services. It examines the applicable statutes and regulations governing EHRs in the United States, including the HITECH Act and the Meaningful Use program, which provide financial incentives for the adoption of certified EHR technology. The report discusses the benefits of EHRs, such as improved access to patient information, reduced medical errors, and enhanced patient-provider interaction. It also references real-world examples like Kaiser Permanente's EHR system and the Department of Veterans Affairs' system. Furthermore, it acknowledges the challenges and costs associated with EHR implementation, while underscoring IT's vital role in transforming healthcare and improving patient outcomes.

Running head: IT HEALTHCARE SYSTEMS 1
IT Healthcare Systems
Students Name
Institution Affiliation
IT Healthcare Systems
Students Name
Institution Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
IT HEALTHCARE SYSTEMS 2
Abstract
Globally, healthcare is changing rapidly. There is an increase in the elderly population, which
has improved the demand for services and the prerequisite to manage the healthcare plan.
Technology has become a significant influence both in payments and healthcare service delivery.
Info IT has the capacity to advance the safety, quality, and efficacy of the healthcare sector. The
essence of (EHR)electronic health records is to offer better care for patients and aid in achieving
health equity. The EHR provides a platform the supports the recording of patient’s information
to improve service delivery in the healthcare sector and allows the analysis of data for the
medical practitioners, the government, and other medical-related agencies. This paper will
discuss the implications and use of IT in the healthcare system; in addition, it will outline the
applicable statutes and regulations, penalties and incentives set to control electronic health
records in the United States
Introduction
For quality healthcare facilities delivery, the relevant stakeholders must integrate
complex information from different sources, which consequently Increases the ability of the
medical practitioners to access and use the correct data from the patients readily. Also,
accessibility of information by the patient is essential is promoting efficient and quality of care
as they can access data, which aids them better manage their disorder and connect with their
healthcare service providers. Information technology enables medical practitioners and other
healthcare stakeholders to access and acquire new information quickly (Bornstein, 2012). IT
offers a remarkable feature that provides a platform that disseminates information that is
accessible on a global level regarding the prices of healthcare services and commodities. The
platform allows the recording and analysis of patient data. The data can be retrieved and used in
Abstract
Globally, healthcare is changing rapidly. There is an increase in the elderly population, which
has improved the demand for services and the prerequisite to manage the healthcare plan.
Technology has become a significant influence both in payments and healthcare service delivery.
Info IT has the capacity to advance the safety, quality, and efficacy of the healthcare sector. The
essence of (EHR)electronic health records is to offer better care for patients and aid in achieving
health equity. The EHR provides a platform the supports the recording of patient’s information
to improve service delivery in the healthcare sector and allows the analysis of data for the
medical practitioners, the government, and other medical-related agencies. This paper will
discuss the implications and use of IT in the healthcare system; in addition, it will outline the
applicable statutes and regulations, penalties and incentives set to control electronic health
records in the United States
Introduction
For quality healthcare facilities delivery, the relevant stakeholders must integrate
complex information from different sources, which consequently Increases the ability of the
medical practitioners to access and use the correct data from the patients readily. Also,
accessibility of information by the patient is essential is promoting efficient and quality of care
as they can access data, which aids them better manage their disorder and connect with their
healthcare service providers. Information technology enables medical practitioners and other
healthcare stakeholders to access and acquire new information quickly (Bornstein, 2012). IT
offers a remarkable feature that provides a platform that disseminates information that is
accessible on a global level regarding the prices of healthcare services and commodities. The
platform allows the recording and analysis of patient data. The data can be retrieved and used in
IT HEALTHCARE SYSTEMS 3
the implementation of significant policies that impact the healthcare sector to prevent and treat
the spread of some conditions.
Quality of healthcare has improved through the incorporation of IT in the healthcare
sector. Quality of care is delivered by offering correct patient records and allows medical
practitioners to comprehend the medical history of their patients (Slight et al., 2015). With a
comprehensive medical history, the medical practitioners can offer perfect remedies to the
patients’ problems hence reducing the instances of over-prescriptions that may be fatal to the
patients. The system guarantees patients' safety, decreases medical errors, and has improved the
interaction between patients and medical practitioners.
At least 96 percent of the healthcare providers in the US use certified EHR technology as
mandated by the HITECH 2009. The healthcare sector through the IT for Economic and Clinic
Health Act is allocated more than $35 billion government funding to encourage the
implementation of IT through EHR program (Slight et al., 2015). Incorporation of EHR in the
sector will help the medical practitioners evade medical errors, cut down on needless costs,
reduce bookkeeping, and consequently advance the quality of healthcare throughout the country
(Wright, Henkin, Feblowitz, McCoy, Bates & Sittig, 2013). Medicaid and Medicare EHR
programs offer financial incentives to qualified specialists who are in a position to prove
meaningful use of the certified EHR technology.
Meaningful Use Certified EHR Technology
Meaningful use signifies that the interested medical personals must demonstrate that they
are incorporating certified electronic health records in approaches that can be quantified in
quantity or quality. The main intention of meaningful use was to enhance the collaboration
the implementation of significant policies that impact the healthcare sector to prevent and treat
the spread of some conditions.
Quality of healthcare has improved through the incorporation of IT in the healthcare
sector. Quality of care is delivered by offering correct patient records and allows medical
practitioners to comprehend the medical history of their patients (Slight et al., 2015). With a
comprehensive medical history, the medical practitioners can offer perfect remedies to the
patients’ problems hence reducing the instances of over-prescriptions that may be fatal to the
patients. The system guarantees patients' safety, decreases medical errors, and has improved the
interaction between patients and medical practitioners.
At least 96 percent of the healthcare providers in the US use certified EHR technology as
mandated by the HITECH 2009. The healthcare sector through the IT for Economic and Clinic
Health Act is allocated more than $35 billion government funding to encourage the
implementation of IT through EHR program (Slight et al., 2015). Incorporation of EHR in the
sector will help the medical practitioners evade medical errors, cut down on needless costs,
reduce bookkeeping, and consequently advance the quality of healthcare throughout the country
(Wright, Henkin, Feblowitz, McCoy, Bates & Sittig, 2013). Medicaid and Medicare EHR
programs offer financial incentives to qualified specialists who are in a position to prove
meaningful use of the certified EHR technology.
Meaningful Use Certified EHR Technology
Meaningful use signifies that the interested medical personals must demonstrate that they
are incorporating certified electronic health records in approaches that can be quantified in
quantity or quality. The main intention of meaningful use was to enhance the collaboration
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
IT HEALTHCARE SYSTEMS 4
between public and clinical healthcare, improve patient-centered preventive care and promote the
continued development of robust, and controlled exchanges of data (Slight et al., 2015). The
American Recovery and Reinvestment Act of 2009 indicates that there are three necessary
approaches to define meaningful use including;
1. The incorporation of certified EHR in a meaningful way, for example, in
e-prescribing.
2. The incorporation of certified EHR of health data to enhance the quality of
healthcare services.
3. The incoporation of certified EHR technology to offer quality measures as
well as other measures.
Medical specialists that are qualified for the Medicare EHR incentive program includea
the doctors of medicine and osteopathy, chiropractors, dentists, optometrists, and podiatrists
(Appari, Eric & Anthony, 2013). Medicaid HER incentive program encompassed qualified
professionals including doctors, nurses, midwives, and dentists. The two programs exclude
medical social workers, physical therapists, psychologists, occupational therapists, and
dieticians.
The named medical practitioners who wish to be qualified for the Medicaid EHR
incentive program must have a at least 30 percent Medicaid patient volume under their care. The
pediatricians are required to have at least of 20 percent of the patient’s capacity (Slight et al.,
2015). Or they practice predominately in federally fit healthcare or rural healthcare facilities with
a 30 percent minimum patient level associated with needy people.
between public and clinical healthcare, improve patient-centered preventive care and promote the
continued development of robust, and controlled exchanges of data (Slight et al., 2015). The
American Recovery and Reinvestment Act of 2009 indicates that there are three necessary
approaches to define meaningful use including;
1. The incorporation of certified EHR in a meaningful way, for example, in
e-prescribing.
2. The incorporation of certified EHR of health data to enhance the quality of
healthcare services.
3. The incoporation of certified EHR technology to offer quality measures as
well as other measures.
Medical specialists that are qualified for the Medicare EHR incentive program includea
the doctors of medicine and osteopathy, chiropractors, dentists, optometrists, and podiatrists
(Appari, Eric & Anthony, 2013). Medicaid HER incentive program encompassed qualified
professionals including doctors, nurses, midwives, and dentists. The two programs exclude
medical social workers, physical therapists, psychologists, occupational therapists, and
dieticians.
The named medical practitioners who wish to be qualified for the Medicaid EHR
incentive program must have a at least 30 percent Medicaid patient volume under their care. The
pediatricians are required to have at least of 20 percent of the patient’s capacity (Slight et al.,
2015). Or they practice predominately in federally fit healthcare or rural healthcare facilities with
a 30 percent minimum patient level associated with needy people.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
IT HEALTHCARE SYSTEMS 5
Incentives payments for qualified practitioners are founded on a practitioner as an
individual and not the practice in general. Every qualified practitioner in practice should show
meaningful use of the certified EHR to be qualified for the incentive payment (Slight et al.,
2015). The number of individual incentive payments is not supposed to be more than one in
every year, irrespective of the number of practices or regions in which the practitioner operates.
Qualified practitioners are not supposed to take part in both the Medicaid and Medicare
incentive programs. The professionals are required to choose which plan of benefit to their
services (Appari et al., 2013). They can, however, change the program after they have been
offered their first incentive. After selecting the Medicaid incentive program, the practitioners are
also supposed to select a state where they would like to get the payments regardless of whether
they offer services across many states (Appari et al., 2013). After eligibility, the practitioners are
registered for the incentive programs.
The eligible practitioners are required to register for the incentive programs through the
online CMS registration system. They are eligible to register before they get a certified EHR
system in place and even before they have a registration record in the Medicare (PECOS)
Provider Enrollment, Chain, And Ownership System that is needed for all Medicare qualified
practitioners (Appari et al., 2013). Not all regions are eligible to take part in the Medicaid
electronic incentive program; therefore, the provides should be sure to check the status of their
state from the CMS website.
Providing certified EHR technology is key to being considered for incentive payments.
Therefore, the practitioners should select a technology that has been certified and tested by the
Coordinator Authorized Testing and Certification Body (ONC-ATCB) (Bowes, 2014).
Practitioners with an already established electronic health record should ensure the software is
Incentives payments for qualified practitioners are founded on a practitioner as an
individual and not the practice in general. Every qualified practitioner in practice should show
meaningful use of the certified EHR to be qualified for the incentive payment (Slight et al.,
2015). The number of individual incentive payments is not supposed to be more than one in
every year, irrespective of the number of practices or regions in which the practitioner operates.
Qualified practitioners are not supposed to take part in both the Medicaid and Medicare
incentive programs. The professionals are required to choose which plan of benefit to their
services (Appari et al., 2013). They can, however, change the program after they have been
offered their first incentive. After selecting the Medicaid incentive program, the practitioners are
also supposed to select a state where they would like to get the payments regardless of whether
they offer services across many states (Appari et al., 2013). After eligibility, the practitioners are
registered for the incentive programs.
The eligible practitioners are required to register for the incentive programs through the
online CMS registration system. They are eligible to register before they get a certified EHR
system in place and even before they have a registration record in the Medicare (PECOS)
Provider Enrollment, Chain, And Ownership System that is needed for all Medicare qualified
practitioners (Appari et al., 2013). Not all regions are eligible to take part in the Medicaid
electronic incentive program; therefore, the provides should be sure to check the status of their
state from the CMS website.
Providing certified EHR technology is key to being considered for incentive payments.
Therefore, the practitioners should select a technology that has been certified and tested by the
Coordinator Authorized Testing and Certification Body (ONC-ATCB) (Bowes, 2014).
Practitioners with an already established electronic health record should ensure the software is
IT HEALTHCARE SYSTEMS 6
tested by the ONC-ATCB, especially for the Medicaid and mediocre electronic health record
incentive programs.
An electronic health record requires significant inputs for it to be fully functional to the
extent that it meets the needs of its consumers. For instance, Kaiser Permanente Health Connect,
a Kaiser's comprehensive EHR system, used at least $3 billion in the integration of the system
(Bornstein, 2012). The system has been of great importance to the organization allowing all the
paper medical records to be integrated into one electronic health system making it one of the
major private EHR across the globe. The program has been in operation since the year 2005 and
has undergone major changes to ensure efficiency in service delivery to the patient. Currently,
the system serves over 12 million patients in 39 hospitals (Wager, Lee & Glaser, 2017). The
healthcare provider is also seeking advanced information technology to integrate into the
healthcare sector to aid in cost accounting (Lehmann, O’Connor, Shorte & Johnson, 2015). The
move is driven by the need to understand the cost, which has become critical to healthcare
providers. Unlike the privately operating system, the Department of Veterans Affairs (VA) uses
a homegrown EHR that has existed for the past 30 years (Lehmann et al., 2015). The VA system
is operable with the department of the defense system and the two-share information; however,
the system has interoperability challenges, which prompted the need for a new system that has
additional capabilities for the VA (Collen & Ball, 2015).
The HITECH proposed a five-year timeline that began in 2011, requiring the healthcare
providers to establish meaningful use of EHR technology (Reisman, 2017). The program has
widely been used since the passing of its legislation; however, it still faces significant barriers,
including a lack of cooperation among stakeholders, excessive regulations, among others. The
major obstacle faced by the program is its financial cost (Menachemi & Collum, 2011). Even
tested by the ONC-ATCB, especially for the Medicaid and mediocre electronic health record
incentive programs.
An electronic health record requires significant inputs for it to be fully functional to the
extent that it meets the needs of its consumers. For instance, Kaiser Permanente Health Connect,
a Kaiser's comprehensive EHR system, used at least $3 billion in the integration of the system
(Bornstein, 2012). The system has been of great importance to the organization allowing all the
paper medical records to be integrated into one electronic health system making it one of the
major private EHR across the globe. The program has been in operation since the year 2005 and
has undergone major changes to ensure efficiency in service delivery to the patient. Currently,
the system serves over 12 million patients in 39 hospitals (Wager, Lee & Glaser, 2017). The
healthcare provider is also seeking advanced information technology to integrate into the
healthcare sector to aid in cost accounting (Lehmann, O’Connor, Shorte & Johnson, 2015). The
move is driven by the need to understand the cost, which has become critical to healthcare
providers. Unlike the privately operating system, the Department of Veterans Affairs (VA) uses
a homegrown EHR that has existed for the past 30 years (Lehmann et al., 2015). The VA system
is operable with the department of the defense system and the two-share information; however,
the system has interoperability challenges, which prompted the need for a new system that has
additional capabilities for the VA (Collen & Ball, 2015).
The HITECH proposed a five-year timeline that began in 2011, requiring the healthcare
providers to establish meaningful use of EHR technology (Reisman, 2017). The program has
widely been used since the passing of its legislation; however, it still faces significant barriers,
including a lack of cooperation among stakeholders, excessive regulations, among others. The
major obstacle faced by the program is its financial cost (Menachemi & Collum, 2011). Even
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
IT HEALTHCARE SYSTEMS 7
with the potential for incentive payments, the cost of implementing the program remains a
significant barrier to its implementation. According to Michigan Center for Effective IT
adoption, the program required at least $15,000-$ 70, 000 upfront and yearly charges for
application based on whether it is a server or web-supported (Collen & Ball, 2015). Besides, the
program requires numerous modified interfaces to make them interoperable with other
organizations and providers.
Conclusion
Information technology is vital in healthcare service delivery; however, as evidenced by
the Kaiser's comprehensive HER system, a lot needs to be done to ensure that the system fully
integrates all the required elements and offers efficient services to the patients. Meaningful use
program was a critical plan to incorporate EHRs into the healthcare system; however, the
providers had to meet slew if requirements to prove the meaningful use. The integration of IT
will help in transforming healthcare and improve the safety of the patient through leveraging IT
to improve the accuracy, efficiency, and effectiveness of the healthcare system.
with the potential for incentive payments, the cost of implementing the program remains a
significant barrier to its implementation. According to Michigan Center for Effective IT
adoption, the program required at least $15,000-$ 70, 000 upfront and yearly charges for
application based on whether it is a server or web-supported (Collen & Ball, 2015). Besides, the
program requires numerous modified interfaces to make them interoperable with other
organizations and providers.
Conclusion
Information technology is vital in healthcare service delivery; however, as evidenced by
the Kaiser's comprehensive HER system, a lot needs to be done to ensure that the system fully
integrates all the required elements and offers efficient services to the patients. Meaningful use
program was a critical plan to incorporate EHRs into the healthcare system; however, the
providers had to meet slew if requirements to prove the meaningful use. The integration of IT
will help in transforming healthcare and improve the safety of the patient through leveraging IT
to improve the accuracy, efficiency, and effectiveness of the healthcare system.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
IT HEALTHCARE SYSTEMS 8
References
Reisman, M. (2017). EHRs: the challenge of making electronic data usable and
interoperable. Pharmacy and Therapeutics, 42(9), 572.
Menachemi, N., & Collum, T. H. (2011). Benefits and drawbacks of electronic health record
systems. Risk management and healthcare policy, 4, 47.
Bornstein, S. (2012). An integrated EHR at Northern California Kaiser Permanente. Applied
clinical informatics, 3(03), 318-325.
Collen, M. F., & Ball, M. J. (Eds.). (2015). The history of medical informatics in the United
States. Springer.
Wager, K. A., Lee, F. W., & Glaser, J. P. (2017). Health care information systems: a practical
approach for health care management. John Wiley & Sons.
Bowes III, W. A. (2014). Impacts of EHR certification and meaningful use implementation on an
integrated delivery network. In AMIA Annual Symposium Proceedings (Vol. 2014, p.
325). American Medical Informatics Association.
Wright, A., Henkin, S., Feblowitz, J., McCoy, A. B., Bates, D. W., & Sittig, D. F. (2013). Early
results of the meaningful use program for electronic health records. New England
Journal of Medicine, 368(8), 779-780.
Slight, S. P., Berner, E. S., Galanter, W., Huff, S., Lambert, B. L., Lannon, C., ... & Payne, T. H.
(2015). Meaningful use of electronic health records: experiences from the field and future
opportunities. JMIR medical informatics, 3(3), e30.
References
Reisman, M. (2017). EHRs: the challenge of making electronic data usable and
interoperable. Pharmacy and Therapeutics, 42(9), 572.
Menachemi, N., & Collum, T. H. (2011). Benefits and drawbacks of electronic health record
systems. Risk management and healthcare policy, 4, 47.
Bornstein, S. (2012). An integrated EHR at Northern California Kaiser Permanente. Applied
clinical informatics, 3(03), 318-325.
Collen, M. F., & Ball, M. J. (Eds.). (2015). The history of medical informatics in the United
States. Springer.
Wager, K. A., Lee, F. W., & Glaser, J. P. (2017). Health care information systems: a practical
approach for health care management. John Wiley & Sons.
Bowes III, W. A. (2014). Impacts of EHR certification and meaningful use implementation on an
integrated delivery network. In AMIA Annual Symposium Proceedings (Vol. 2014, p.
325). American Medical Informatics Association.
Wright, A., Henkin, S., Feblowitz, J., McCoy, A. B., Bates, D. W., & Sittig, D. F. (2013). Early
results of the meaningful use program for electronic health records. New England
Journal of Medicine, 368(8), 779-780.
Slight, S. P., Berner, E. S., Galanter, W., Huff, S., Lambert, B. L., Lannon, C., ... & Payne, T. H.
(2015). Meaningful use of electronic health records: experiences from the field and future
opportunities. JMIR medical informatics, 3(3), e30.

IT HEALTHCARE SYSTEMS 9
Appari, A., Eric Johnson, M., & Anthony, D. L. (2013). Meaningful use of electronic health
record systems and process quality of care: evidence from a panel data analysis of US
acute‐care hospitals. Health services research, 48(2pt1), 354-375.
Lehmann, C. U., O’Connor, K. G., Shorte, V. A., & Johnson, T. D. (2015). Use of electronic
health record systems by office-based pediatricians. Pediatrics, 135(1), e7-e15.
Appari, A., Eric Johnson, M., & Anthony, D. L. (2013). Meaningful use of electronic health
record systems and process quality of care: evidence from a panel data analysis of US
acute‐care hospitals. Health services research, 48(2pt1), 354-375.
Lehmann, C. U., O’Connor, K. G., Shorte, V. A., & Johnson, T. D. (2015). Use of electronic
health record systems by office-based pediatricians. Pediatrics, 135(1), e7-e15.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
IT HEALTHCARE SYSTEMS 10
Appendices
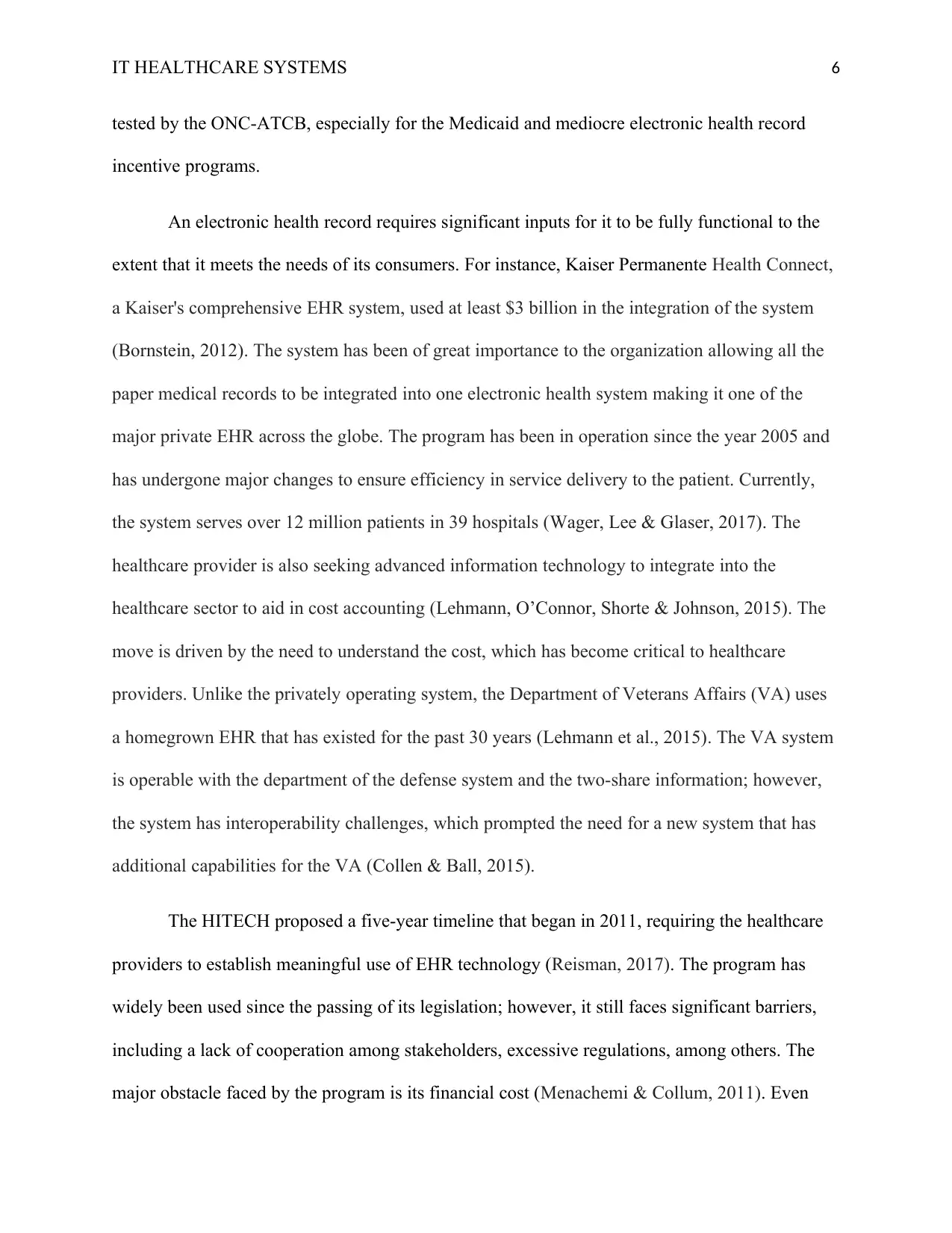
1. Obtained from centers for (Medicare & Medicaid services, 2019)
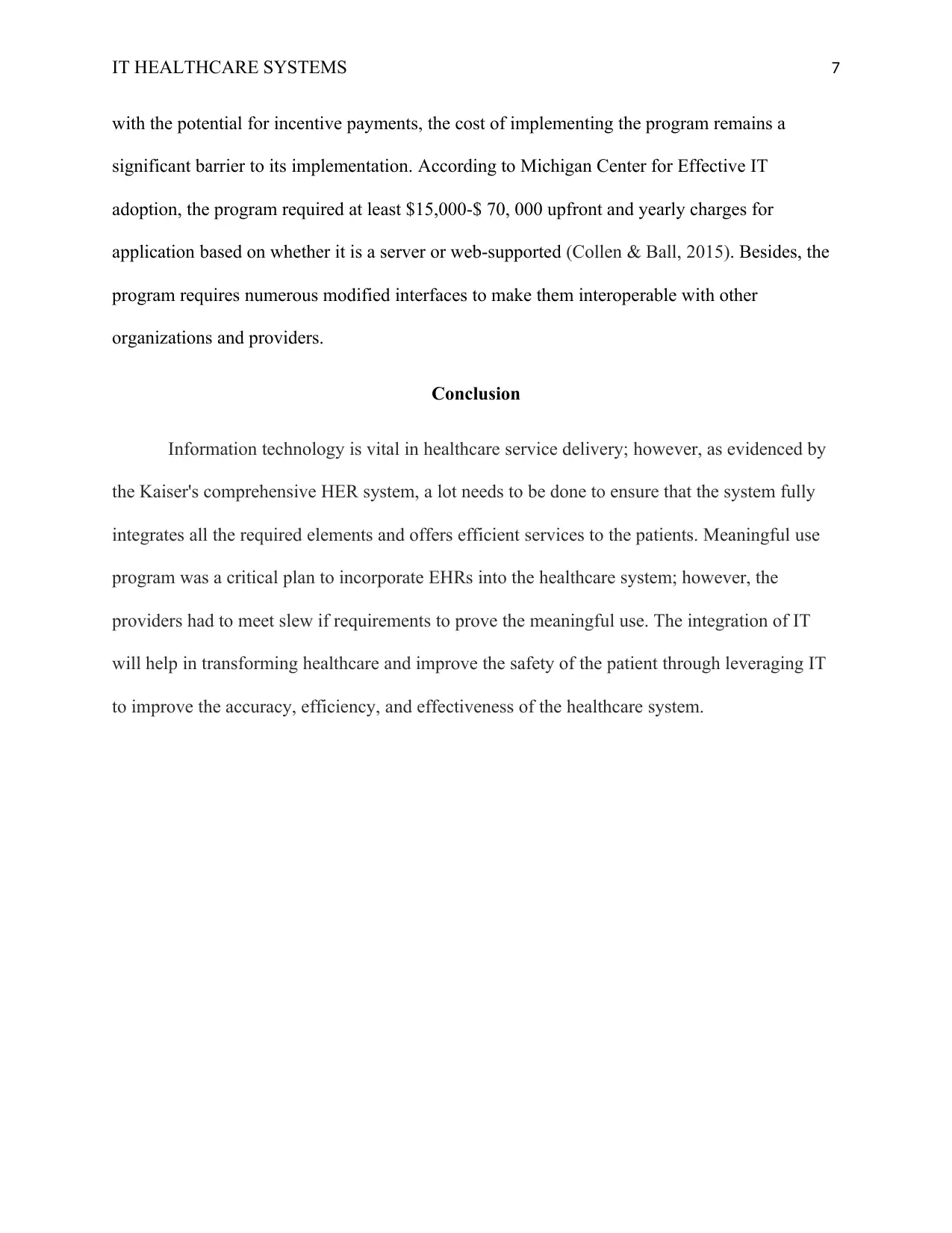
2. Obtained from centers for (Medicare & Medicaid services, 2019)
Appendices
1. Obtained from centers for (Medicare & Medicaid services, 2019)
2. Obtained from centers for (Medicare & Medicaid services, 2019)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
IT HEALTHCARE SYSTEMS 11
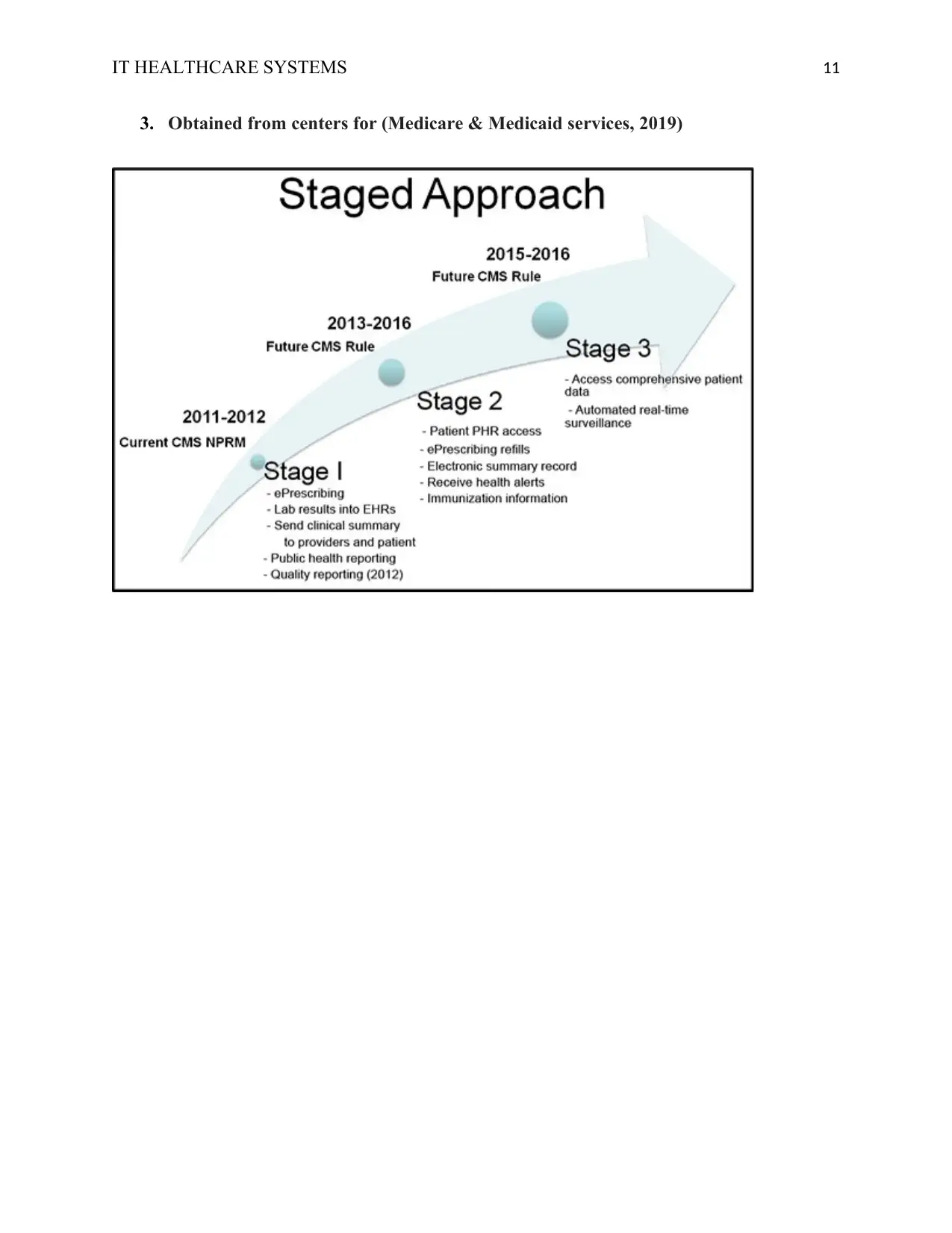
3. Obtained from centers for (Medicare & Medicaid services, 2019)
3. Obtained from centers for (Medicare & Medicaid services, 2019)
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





