Leadership Role in Healthcare Change: A Critical Analysis, 2019
VerifiedAdded on 2023/03/31
|13
|3644
|413
Essay
AI Summary
This essay critically analyzes the role of leadership in facilitating change processes within healthcare organizations, focusing on performance improvement (PI) in therapeutic communication. It explores various leadership styles, such as transformational leadership, and change management theories, including Lewin's three-stage model, to address issues like ineffective communication between healthcare professionals and patients. The essay outlines the eight steps of performance improvement, emphasizing stakeholder accountability and continuous feedback. It also discusses the impact of workplace culture, barriers to change (e.g., resource limitations), and facilitators (e.g., commitment, supportive work culture). The importance of benchmarking best practices and strategies for motivating staff are examined, highlighting the registered nurse leader's role in promoting patient safety and quality care. Desklib offers more resources for students.

Running Head: HEALTHCARE
0
Building organizational capacity in healthcare
6/1/2019
0
Building organizational capacity in healthcare
6/1/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

HEALTHCARE
1
The essay brings about the discussion on the concept of leadership, and the role of the
leaders in context to healthcare organisations. Leadership is an essential element or important
phenomenon in any organisation as it determines an influence on the behaviour of the
individuals to attain goals. The role of a leader is crucial in the organisations to support
positive change in the organisational processes or practices. In addition, the essay will also
analyse the aspect and process of change within clinics or hospitals through the support of
managers or leaders.
The aim or objective behind the development of leadership and effectiveness in the
operations is to develop the capacity of the organisation at the public level. Moreover, the
discussion will also mention one aspect or health practice area that requires performance
requirement. This further states the application of change and leadership theory. The
assignment will therefore include the concepts of workplace culture, change management
practices, importance of benchmarking strategy, and others. Thus, it can be stated that the
essay will analyse the PI strategy of the health care organisations. Thus, the readers through
this essay will gain an understanding of the role of the leaders and their practices to assess
importance of benchmarking and the practices of change within institutions (Fortenberry &
McGoldrick, 2016).
To define and discuss the meaning of leadership in healthcare, it refers to the
behaviour of an individual for directing activities of a group towards a common goal. The
purpose of a leader is to influence the group activities and initiate positive change in the
organisation. Leadership theory is dynamic and evolves or changes over time, and the key
aspects of leadership is to assist group to cope with the change in the organisation (Foronda,
MacWilliams & McArthur, 2016).
In context to health care institutions, it has been found that leadership qualities and
strategies act as major processes, which determine the importance of workplace health
promotion. This is one of the aspects considered important on the health related work
practices, which aim to create a positive impact on the process of change. In healthcare
organisations, there are numerous professional groups, departments and speciality areas that
interact with each other. Therefore, these different groups might support or conflict with
each other. This is one major aspect that determine the significant role of the leader, as the
process of leadership capitalizes or incorporates the aspect of diversity as a whole, and
efficiently utilises the resources of the organisation (Berman, 2015).
1
The essay brings about the discussion on the concept of leadership, and the role of the
leaders in context to healthcare organisations. Leadership is an essential element or important
phenomenon in any organisation as it determines an influence on the behaviour of the
individuals to attain goals. The role of a leader is crucial in the organisations to support
positive change in the organisational processes or practices. In addition, the essay will also
analyse the aspect and process of change within clinics or hospitals through the support of
managers or leaders.
The aim or objective behind the development of leadership and effectiveness in the
operations is to develop the capacity of the organisation at the public level. Moreover, the
discussion will also mention one aspect or health practice area that requires performance
requirement. This further states the application of change and leadership theory. The
assignment will therefore include the concepts of workplace culture, change management
practices, importance of benchmarking strategy, and others. Thus, it can be stated that the
essay will analyse the PI strategy of the health care organisations. Thus, the readers through
this essay will gain an understanding of the role of the leaders and their practices to assess
importance of benchmarking and the practices of change within institutions (Fortenberry &
McGoldrick, 2016).
To define and discuss the meaning of leadership in healthcare, it refers to the
behaviour of an individual for directing activities of a group towards a common goal. The
purpose of a leader is to influence the group activities and initiate positive change in the
organisation. Leadership theory is dynamic and evolves or changes over time, and the key
aspects of leadership is to assist group to cope with the change in the organisation (Foronda,
MacWilliams & McArthur, 2016).
In context to health care institutions, it has been found that leadership qualities and
strategies act as major processes, which determine the importance of workplace health
promotion. This is one of the aspects considered important on the health related work
practices, which aim to create a positive impact on the process of change. In healthcare
organisations, there are numerous professional groups, departments and speciality areas that
interact with each other. Therefore, these different groups might support or conflict with
each other. This is one major aspect that determine the significant role of the leader, as the
process of leadership capitalizes or incorporates the aspect of diversity as a whole, and
efficiently utilises the resources of the organisation (Berman, 2015).

HEALTHCARE
2
Change in an important aspect in any organisation, and essential to be incorporated to
lead growth and success of the organisations. The role of a nurse leader is vital for the
effective implementation of change processes, in the healthcare practices. However, the
leadership change acts as a major challenge for the nurse leaders or specialists in the
healthcare. A number of leadership approaches can be adopted or implemented within
healthcare organisations, such as transformational leadership, conflict management, shared
leadership, collaborative leadership, and distributed leadership (Alligood, 2017).
Now, the discussion will further proceed to the assessment of one specific area of
health practice that requires performance improvement (PI) for implementing theories of
change and leadership. For gaining an understanding of the health practice area, ‘Therapeutic
Alliance’, or relationship is one of the important health-related practices (Birnbaum, 2017).
The term ‘therapeutic alliance’ is the relationship between the health care professional and
client or patient, and they work for initiating a positive change in the healthcare. It is a caring
relationship which support and lead to the patient’s safety and wellbeing. Therefore, nurse
leaders or health managers need to focus on developing essential skills to establish sound
relationship with the patients (Asiri et al., 2016).
Furthermore, the aspect of communication between the health professionals and client
is understood as a vital part of the therapeutic relationship. Therapeutic practice involves oral
communication of the public health professionals and nurses on one hand, and between the
patient and their support members on the other. However, it has been analysed that many
health care settings face the problem of effective communication between the health experts
and their clients. Therefore, ’lack of effective communication’ is one major issue which
requires performance improvement to lead change in the institutions (Foronda, MacWilliams &
McArthur, 2016).
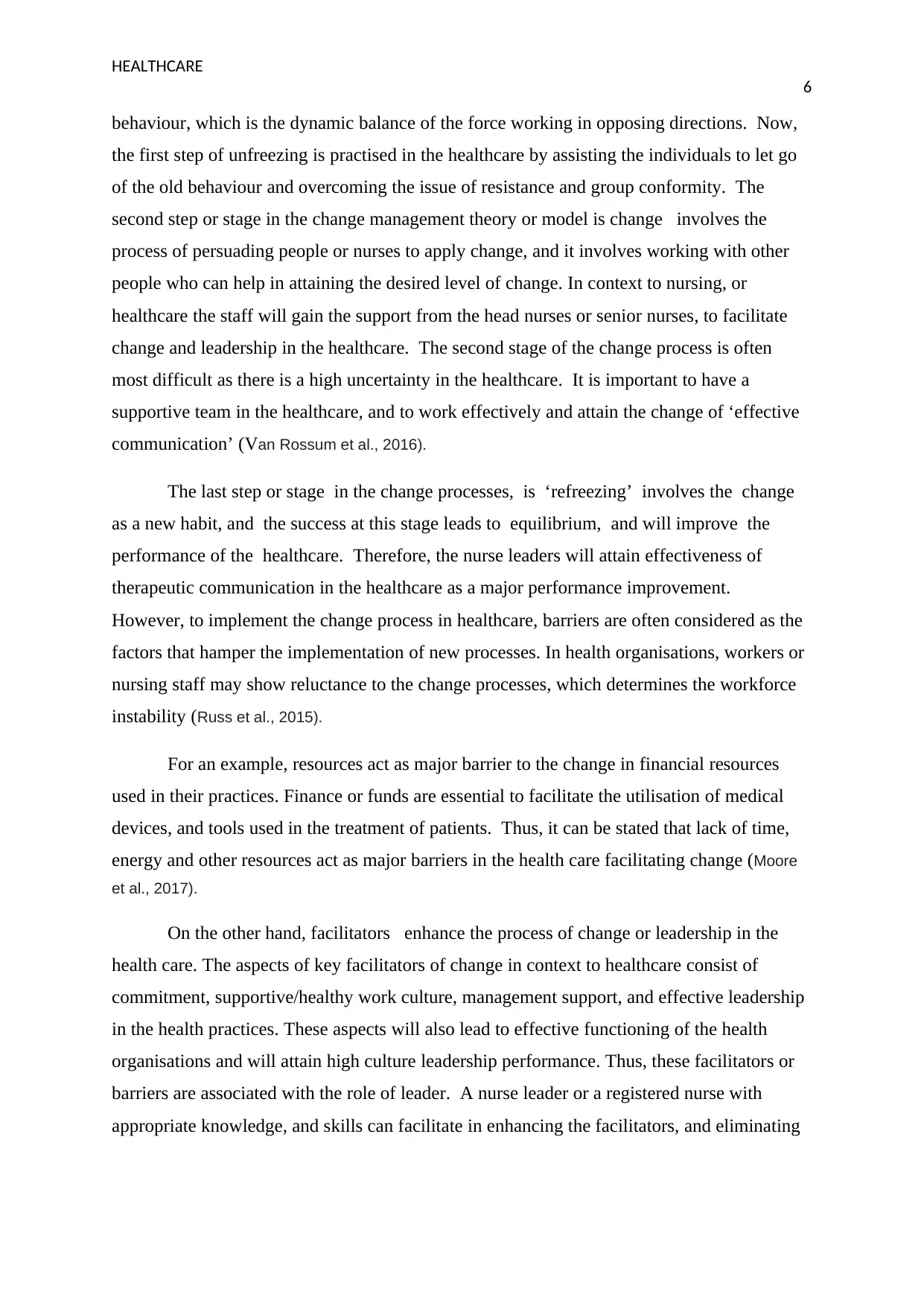
The strategy of performance improvement (PI) focuses upon enabling improvement in
the processes of providing health care facilities or services to the patients. The goal of PI is
observed to improve the clinical outcomes, enhancing the experience of patients, and
minimise the costs of healthcare. The below diagram, represents the eight steps or stages of
the performance improvement strategy which are applied to the healthcare for initiating the
change initiative, and attaining the health outcome of the patient (Pannick, Sevdalis &
Athanasiou, 2016).
2
Change in an important aspect in any organisation, and essential to be incorporated to
lead growth and success of the organisations. The role of a nurse leader is vital for the
effective implementation of change processes, in the healthcare practices. However, the
leadership change acts as a major challenge for the nurse leaders or specialists in the
healthcare. A number of leadership approaches can be adopted or implemented within
healthcare organisations, such as transformational leadership, conflict management, shared
leadership, collaborative leadership, and distributed leadership (Alligood, 2017).
Now, the discussion will further proceed to the assessment of one specific area of
health practice that requires performance improvement (PI) for implementing theories of
change and leadership. For gaining an understanding of the health practice area, ‘Therapeutic
Alliance’, or relationship is one of the important health-related practices (Birnbaum, 2017).
The term ‘therapeutic alliance’ is the relationship between the health care professional and
client or patient, and they work for initiating a positive change in the healthcare. It is a caring
relationship which support and lead to the patient’s safety and wellbeing. Therefore, nurse
leaders or health managers need to focus on developing essential skills to establish sound
relationship with the patients (Asiri et al., 2016).
Furthermore, the aspect of communication between the health professionals and client
is understood as a vital part of the therapeutic relationship. Therapeutic practice involves oral
communication of the public health professionals and nurses on one hand, and between the
patient and their support members on the other. However, it has been analysed that many
health care settings face the problem of effective communication between the health experts
and their clients. Therefore, ’lack of effective communication’ is one major issue which
requires performance improvement to lead change in the institutions (Foronda, MacWilliams &
McArthur, 2016).
The strategy of performance improvement (PI) focuses upon enabling improvement in
the processes of providing health care facilities or services to the patients. The goal of PI is
observed to improve the clinical outcomes, enhancing the experience of patients, and
minimise the costs of healthcare. The below diagram, represents the eight steps or stages of
the performance improvement strategy which are applied to the healthcare for initiating the
change initiative, and attaining the health outcome of the patient (Pannick, Sevdalis &
Athanasiou, 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

HEALTHCARE
3
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

HEALTHCARE
4
The aspect of performance improvement initiatives are considered important, they
must identify the problem at first and then take appropriate steps to solve them. There are
eight steps in the process of performance improvement for taking the initiative of change
management. These steps consist of prioritizing opportunities, which includes identifying the
issues or m problems in context to the healthcare improvement plan (Foronda, MacWilliams,&
McArthur, 2016).
Dedicated leadership include acquiring support from the senior members to
incorporate or practice change in the health practices. Identifying the root causes involves
identifying actual, or current processes that lack effectiveness in the practices, and making
the change accordingly (Riley, 2015). The next step or stage in the process of the performance
improvement includes, committing to the work plan and goals, communicating change
effectively through using systematic planning. It further includes carrying out smart rollout,
and holding accountability of all the stakeholders, and adjusting the new processes and
protocols as per the work in monitoring performance (Silver et al., 2016).
In the above-mentioned steps of performance improvement strategy the step of
stakeholder’s accountability is considered important, as they role of front line nurses is
significant to the change process. The last step of adjust as needed can be termed as feedback
to monitor the change in protocols or processes at all the levels. In this aspect, the health
professionals or specialist undertake the responsibility of establishing mechanisms for
gaining suggestions from the stakeholders for making any additional changes or
improvements (Nudurupati et al., 2015).
The role of a RN i.e. registered nurse leader is vital in the practice of performance
improvement as nurses can prevent the harm to their patients. They ensure patient safety and
continuity of quality care, which is essential to lead effective communication in the
healthcare. Moreover, nurses maintain the documentation to record the pertinent details such
as the assessment, findings, health history of patient, tests, treatment, and outcomes. It has
been found through research that proper documentation promotes effective communication in
the healthcare. It is due to the reason that proper documentation of the patient details reduces
the possibility of errors or mistakes by the health specialists or nurse (El-Jardali & Fadlallah,
2017).
It therefore helps in improving the communication between the specialist and client.
This further improves the coordination of the nurses with their patients, and develops
4
The aspect of performance improvement initiatives are considered important, they
must identify the problem at first and then take appropriate steps to solve them. There are
eight steps in the process of performance improvement for taking the initiative of change
management. These steps consist of prioritizing opportunities, which includes identifying the
issues or m problems in context to the healthcare improvement plan (Foronda, MacWilliams,&
McArthur, 2016).
Dedicated leadership include acquiring support from the senior members to
incorporate or practice change in the health practices. Identifying the root causes involves
identifying actual, or current processes that lack effectiveness in the practices, and making
the change accordingly (Riley, 2015). The next step or stage in the process of the performance
improvement includes, committing to the work plan and goals, communicating change
effectively through using systematic planning. It further includes carrying out smart rollout,
and holding accountability of all the stakeholders, and adjusting the new processes and
protocols as per the work in monitoring performance (Silver et al., 2016).
In the above-mentioned steps of performance improvement strategy the step of
stakeholder’s accountability is considered important, as they role of front line nurses is
significant to the change process. The last step of adjust as needed can be termed as feedback
to monitor the change in protocols or processes at all the levels. In this aspect, the health
professionals or specialist undertake the responsibility of establishing mechanisms for
gaining suggestions from the stakeholders for making any additional changes or
improvements (Nudurupati et al., 2015).
The role of a RN i.e. registered nurse leader is vital in the practice of performance
improvement as nurses can prevent the harm to their patients. They ensure patient safety and
continuity of quality care, which is essential to lead effective communication in the
healthcare. Moreover, nurses maintain the documentation to record the pertinent details such
as the assessment, findings, health history of patient, tests, treatment, and outcomes. It has
been found through research that proper documentation promotes effective communication in
the healthcare. It is due to the reason that proper documentation of the patient details reduces
the possibility of errors or mistakes by the health specialists or nurse (El-Jardali & Fadlallah,
2017).
It therefore helps in improving the communication between the specialist and client.
This further improves the coordination of the nurses with their patients, and develops

HEALTHCARE
5
understanding and trust. It facilitates the process of therapeutic communication and helps in
the healing of the treatment. Besides, this a nurse leader or manager educates or informs the
patient about their illness, process of treatment, medications and the aspect of self-care
contributing to positive health outcomes (Defenbaugh & Chikotas, 2016). Therefore, it
determines an important role of the nurse leaders in taking the initiative for the performance
improvement in context to therapeutic communication. Nurses in a healthcare setting ensure
effective care and treatment to their patients through practising effective communication
(Korlén et al., 2017).
To determine the application of leadership, in the healthcare, in context to
performance improvement transformational leadership is an appropriate practice.
Transformational leadership style or approach in nursing refers to the aspect or process,
whereby a leader identifies the needed change, and creates a vision to guide or support the
team members to execute change within organisation or system. Therefore, it has been
analysed that nurse leaders through practising transformational leadership can facilitate
change in the health care, and help their patients overcome with their health problems
(Boamah et al., 2018).
Now, it has been understood that effective leadership approach is essential to bring
and facilitate change in the healthcare however there is an important role of workplace
culture. Physical aspects of healthcare organisation, such as cleanliness, air quality, safety
concerns are some of the major parts of the work culture. These aspects determine the
healthy environment. It has been found through research that workplace culture of health
care is interconnected with the change and leadership. As organisational culture is viewed as
the key element in the large system transformation, therefore the health leaders need to focus
on developing a positive culture (Fischer, 2016).
A positive environment in the hospitals clinics or healthcare will enable their staff or
nurse leaders to facilitate change in the organisation. In context to the above discussed
aspect of area of healthcare practice, i.e. ‘therapeutic communication’ and will therefore
improve the health condition of the people. Thus, nurse leaders are stated as the change
agent in the nursing, and they guide or facilitate change (Gausvik et al., 2015).
Change management process and management theories of nursing consist of Kurt
Lewin’s model, which is a three-staged model of change. The steps in the model include
unfreezing-change-refreezing. The element of behaviour is described by Lewin, as the
5
understanding and trust. It facilitates the process of therapeutic communication and helps in
the healing of the treatment. Besides, this a nurse leader or manager educates or informs the
patient about their illness, process of treatment, medications and the aspect of self-care
contributing to positive health outcomes (Defenbaugh & Chikotas, 2016). Therefore, it
determines an important role of the nurse leaders in taking the initiative for the performance
improvement in context to therapeutic communication. Nurses in a healthcare setting ensure
effective care and treatment to their patients through practising effective communication
(Korlén et al., 2017).
To determine the application of leadership, in the healthcare, in context to
performance improvement transformational leadership is an appropriate practice.
Transformational leadership style or approach in nursing refers to the aspect or process,
whereby a leader identifies the needed change, and creates a vision to guide or support the
team members to execute change within organisation or system. Therefore, it has been
analysed that nurse leaders through practising transformational leadership can facilitate
change in the health care, and help their patients overcome with their health problems
(Boamah et al., 2018).
Now, it has been understood that effective leadership approach is essential to bring
and facilitate change in the healthcare however there is an important role of workplace
culture. Physical aspects of healthcare organisation, such as cleanliness, air quality, safety
concerns are some of the major parts of the work culture. These aspects determine the
healthy environment. It has been found through research that workplace culture of health
care is interconnected with the change and leadership. As organisational culture is viewed as
the key element in the large system transformation, therefore the health leaders need to focus
on developing a positive culture (Fischer, 2016).
A positive environment in the hospitals clinics or healthcare will enable their staff or
nurse leaders to facilitate change in the organisation. In context to the above discussed
aspect of area of healthcare practice, i.e. ‘therapeutic communication’ and will therefore
improve the health condition of the people. Thus, nurse leaders are stated as the change
agent in the nursing, and they guide or facilitate change (Gausvik et al., 2015).
Change management process and management theories of nursing consist of Kurt
Lewin’s model, which is a three-staged model of change. The steps in the model include
unfreezing-change-refreezing. The element of behaviour is described by Lewin, as the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE
6
behaviour, which is the dynamic balance of the force working in opposing directions. Now,
the first step of unfreezing is practised in the healthcare by assisting the individuals to let go
of the old behaviour and overcoming the issue of resistance and group conformity. The
second step or stage in the change management theory or model is change involves the
process of persuading people or nurses to apply change, and it involves working with other
people who can help in attaining the desired level of change. In context to nursing, or
healthcare the staff will gain the support from the head nurses or senior nurses, to facilitate
change and leadership in the healthcare. The second stage of the change process is often
most difficult as there is a high uncertainty in the healthcare. It is important to have a
supportive team in the healthcare, and to work effectively and attain the change of ‘effective
communication’ (Van Rossum et al., 2016).
The last step or stage in the change processes, is ‘refreezing’ involves the change
as a new habit, and the success at this stage leads to equilibrium, and will improve the
performance of the healthcare. Therefore, the nurse leaders will attain effectiveness of
therapeutic communication in the healthcare as a major performance improvement.
However, to implement the change process in healthcare, barriers are often considered as the
factors that hamper the implementation of new processes. In health organisations, workers or
nursing staff may show reluctance to the change processes, which determines the workforce
instability (Russ et al., 2015).
For an example, resources act as major barrier to the change in financial resources
used in their practices. Finance or funds are essential to facilitate the utilisation of medical
devices, and tools used in the treatment of patients. Thus, it can be stated that lack of time,
energy and other resources act as major barriers in the health care facilitating change (Moore
et al., 2017).
On the other hand, facilitators enhance the process of change or leadership in the
health care. The aspects of key facilitators of change in context to healthcare consist of
commitment, supportive/healthy work culture, management support, and effective leadership
in the health practices. These aspects will also lead to effective functioning of the health
organisations and will attain high culture leadership performance. Thus, these facilitators or
barriers are associated with the role of leader. A nurse leader or a registered nurse with
appropriate knowledge, and skills can facilitate in enhancing the facilitators, and eliminating
6
behaviour, which is the dynamic balance of the force working in opposing directions. Now,
the first step of unfreezing is practised in the healthcare by assisting the individuals to let go
of the old behaviour and overcoming the issue of resistance and group conformity. The
second step or stage in the change management theory or model is change involves the
process of persuading people or nurses to apply change, and it involves working with other
people who can help in attaining the desired level of change. In context to nursing, or
healthcare the staff will gain the support from the head nurses or senior nurses, to facilitate
change and leadership in the healthcare. The second stage of the change process is often
most difficult as there is a high uncertainty in the healthcare. It is important to have a
supportive team in the healthcare, and to work effectively and attain the change of ‘effective
communication’ (Van Rossum et al., 2016).
The last step or stage in the change processes, is ‘refreezing’ involves the change
as a new habit, and the success at this stage leads to equilibrium, and will improve the
performance of the healthcare. Therefore, the nurse leaders will attain effectiveness of
therapeutic communication in the healthcare as a major performance improvement.
However, to implement the change process in healthcare, barriers are often considered as the
factors that hamper the implementation of new processes. In health organisations, workers or
nursing staff may show reluctance to the change processes, which determines the workforce
instability (Russ et al., 2015).
For an example, resources act as major barrier to the change in financial resources
used in their practices. Finance or funds are essential to facilitate the utilisation of medical
devices, and tools used in the treatment of patients. Thus, it can be stated that lack of time,
energy and other resources act as major barriers in the health care facilitating change (Moore
et al., 2017).
On the other hand, facilitators enhance the process of change or leadership in the
health care. The aspects of key facilitators of change in context to healthcare consist of
commitment, supportive/healthy work culture, management support, and effective leadership
in the health practices. These aspects will also lead to effective functioning of the health
organisations and will attain high culture leadership performance. Thus, these facilitators or
barriers are associated with the role of leader. A nurse leader or a registered nurse with
appropriate knowledge, and skills can facilitate in enhancing the facilitators, and eliminating
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

HEALTHCARE
7
the barriers to overcome deficiencies in the treatment process and implement change in the
health institutes (Pannick, S., Sevdalis, N., & Athanasiou, 2016).
In consideration to the change processes and management concepts in the healthcare,
the concept of benchmarking is important. Benchmarking refers to the process of comparing
the business processes of one firm to the best practices of other businesses in the industry.
Benchmarks can be assigned to the best industry standards of an organisation, and their
comparison to others. To implement the process of change in respect to the given area of
performance improvement, i.e. ‘therapeutic communication’ health organisations require the
combined efforts of the nursing staff, RN, or head nurse, and the managers or leaders.
therefore, their engagement is considered vital to support the process of change (Willis et al.,
2016).These are the key stakeholders of healthcare that includes patients, physicians,
employers, insurance companies, pharmaceutical firms, and government.
Stakeholder engagement process of strategy is therefore, used by the healthcare to
motivate and enhance their level of involvement to facilitate performance improvement at all
the stages. For attaining the aim of inclusion and encouragement of all the stakeholders in the
performance improvement, stakeholder mapping can be done by the health managers
(Purushotham et al., 2018).
A number of standards act as major benchmarks in the healthcare to improve the
overall performance, and achieve health outcomes. For an example, the benchmark of hand
washing compliance has been set by WHO for every health care organisation, to ensure
better health facilities. In context to the chosen area for the improvement, in healthcare, i.e.
communication it has been analysed that ‘communication standards’ acts as benchmark for
the healthcare (Shahid et al., 2019).
In healthcare organisations, the role of nurse leaders or nurse managers is considered
crucial for the effective change in the healthcare. The nurse leader plays an important role in
creating a sustainable change in the healthcare. To define the term, sustainable change refers
to the process when an organisation or health care has attained change, and shifts from the
process of efforts to change, leading to the new way of doing work, or carrying out health
practices. To mention the essential elements or components of sustainable change includes
communication between nurse and patients, and human, social, economic, and
environmental. Therefore, healthcare must focus upon involving the different aspects of
change, and incorporating effective utilisation of different resources. These four
7
the barriers to overcome deficiencies in the treatment process and implement change in the
health institutes (Pannick, S., Sevdalis, N., & Athanasiou, 2016).
In consideration to the change processes and management concepts in the healthcare,
the concept of benchmarking is important. Benchmarking refers to the process of comparing
the business processes of one firm to the best practices of other businesses in the industry.
Benchmarks can be assigned to the best industry standards of an organisation, and their
comparison to others. To implement the process of change in respect to the given area of
performance improvement, i.e. ‘therapeutic communication’ health organisations require the
combined efforts of the nursing staff, RN, or head nurse, and the managers or leaders.
therefore, their engagement is considered vital to support the process of change (Willis et al.,
2016).These are the key stakeholders of healthcare that includes patients, physicians,
employers, insurance companies, pharmaceutical firms, and government.
Stakeholder engagement process of strategy is therefore, used by the healthcare to
motivate and enhance their level of involvement to facilitate performance improvement at all
the stages. For attaining the aim of inclusion and encouragement of all the stakeholders in the
performance improvement, stakeholder mapping can be done by the health managers
(Purushotham et al., 2018).
A number of standards act as major benchmarks in the healthcare to improve the
overall performance, and achieve health outcomes. For an example, the benchmark of hand
washing compliance has been set by WHO for every health care organisation, to ensure
better health facilities. In context to the chosen area for the improvement, in healthcare, i.e.
communication it has been analysed that ‘communication standards’ acts as benchmark for
the healthcare (Shahid et al., 2019).
In healthcare organisations, the role of nurse leaders or nurse managers is considered
crucial for the effective change in the healthcare. The nurse leader plays an important role in
creating a sustainable change in the healthcare. To define the term, sustainable change refers
to the process when an organisation or health care has attained change, and shifts from the
process of efforts to change, leading to the new way of doing work, or carrying out health
practices. To mention the essential elements or components of sustainable change includes
communication between nurse and patients, and human, social, economic, and
environmental. Therefore, healthcare must focus upon involving the different aspects of
change, and incorporating effective utilisation of different resources. These four

HEALTHCARE
8
components determine the effectiveness of the health managers achieving the sustainability
of change, in respect to the performance improvement.
From the research on the effective use of performance improvement strategy i.e. PI it
has been found that these are used in almost every organisation. Specifically, organisations
who want to progress towards betterment of the performance of the work processes, mainly
involves the use of PI strategy. An example is ‘Quality improvement’ is another major area
of the health practices, which requires the use of performance improvement strategy. It has
been analysed that the use of change management theories and PI strategy is beneficial at all
different levels, i.e. personal, group, and organisational level.
At organisational level, it will enhance the management of the healthcare, which in
turn benefits the patients. At personal level, health managers or nurse leaders implementing
the PI strategy will be able to improve or establish effective skills and competencies for
providing care and treatment to the patients or people. On the other hand, to discuss the
relationship and effectiveness of the use of PI strategy, it has been found that it also promotes
the coordination, and collaboration of the team members in the healthcare. It is essential for
the team members to work together and ensure great support for attaining the goal of
effective communication, leading to positive health outcomes (Rizk et al., 2015).
To conclude the above discussion it has been analysed that the healthcare
organisations must emphasize the use of effective communication in their health practices. In
health organisations, the nurse leaders or managers play a vital role in ensuring the attainment
of positive health outcomes. The assignment has discussed about an important aspect of the
performance improvement, i.e. therapeutic communication amongst the health specialist and
patients. Nurse leaders are vital for incorporating the change and leadership in the
organisation. Amongst, different theories, the style of transformational leadership have been
found to be effective in the healthcare to facilitate change. Transformational leaders or nurse
leaders engage all the stakeholders such as patients, clinicians towards supporting change in
the healthcare. The discussion also mentioned the meaning and importance of benchmarking
in the healthcare practices, as they determine the attainment of health outcomes of the
patients. The concept of change management and the aspects of facilitators and barriers has
been also described in the discussion using the Lewin’s theory or model of change. Thus,
from the above analysis of the discussion it has been found that the leader plays a vital role in
the performance improvement in context to healthcare practices. Furthermore, it has been
8
components determine the effectiveness of the health managers achieving the sustainability
of change, in respect to the performance improvement.
From the research on the effective use of performance improvement strategy i.e. PI it
has been found that these are used in almost every organisation. Specifically, organisations
who want to progress towards betterment of the performance of the work processes, mainly
involves the use of PI strategy. An example is ‘Quality improvement’ is another major area
of the health practices, which requires the use of performance improvement strategy. It has
been analysed that the use of change management theories and PI strategy is beneficial at all
different levels, i.e. personal, group, and organisational level.
At organisational level, it will enhance the management of the healthcare, which in
turn benefits the patients. At personal level, health managers or nurse leaders implementing
the PI strategy will be able to improve or establish effective skills and competencies for
providing care and treatment to the patients or people. On the other hand, to discuss the
relationship and effectiveness of the use of PI strategy, it has been found that it also promotes
the coordination, and collaboration of the team members in the healthcare. It is essential for
the team members to work together and ensure great support for attaining the goal of
effective communication, leading to positive health outcomes (Rizk et al., 2015).
To conclude the above discussion it has been analysed that the healthcare
organisations must emphasize the use of effective communication in their health practices. In
health organisations, the nurse leaders or managers play a vital role in ensuring the attainment
of positive health outcomes. The assignment has discussed about an important aspect of the
performance improvement, i.e. therapeutic communication amongst the health specialist and
patients. Nurse leaders are vital for incorporating the change and leadership in the
organisation. Amongst, different theories, the style of transformational leadership have been
found to be effective in the healthcare to facilitate change. Transformational leaders or nurse
leaders engage all the stakeholders such as patients, clinicians towards supporting change in
the healthcare. The discussion also mentioned the meaning and importance of benchmarking
in the healthcare practices, as they determine the attainment of health outcomes of the
patients. The concept of change management and the aspects of facilitators and barriers has
been also described in the discussion using the Lewin’s theory or model of change. Thus,
from the above analysis of the discussion it has been found that the leader plays a vital role in
the performance improvement in context to healthcare practices. Furthermore, it has been
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

HEALTHCARE
9
also understood that the patients must undertake the responsibility of the care for their health
and must ensure effective participation in the process of communication.
9
also understood that the patients must undertake the responsibility of the care for their health
and must ensure effective participation in the process of communication.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

HEALTHCARE
10
References
Alligood, M. R. (2017). Nursing Theorists and Their Work-E-Book. United States: Elsevier
Health Sciences.
Asiri, S. A., Rohrer, W. W., Al-Surimi, K., Da’ar, O. O. & Ahmed, A. (2016). The
association of leadership styles and empowerment with nurses’ organizational
commitment in an acute health care setting: a cross-sectional study. BMC nursing,
15(1), 38.
Berman, E. (2015). Performance and productivity in public and non-profit organizations.
United Kingdom: Routledge.
Birnbaum, S. (2017). Therapeutic communication in mental health nursing: Aesthetic and
metaphoric processes in the engagement with challenging patients. United Kingdom:
Routledge.
Boamah, S. A., Laschinger, H. K. S., Wong, C. & Clarke, S. (2018). Effect of
transformational leadership on job satisfaction and patient safety outcomes. Nursing
outlook, 66(2), 180-189.
Defenbaugh, N. & Chikotas, N. E. (2016). The outcome of inter-professional education:
Integrating communication studies into a standardized patient experience for
advanced practice nursing students. Nurse education in practice, 16(1), 176-181.
El-Jardali, F. & Fadlallah, R. (2017). A review of national policies and strategies to improve
quality of health care and patient safety: a case study from Lebanon and Jordan. BMC
health services research, 17(1), 568.
Fischer, S. A. (2016). Transformational leadership in nursing: a concept analysis. Journal of
Advanced Nursing, 72(11), 2644-2653.
Foronda, C., MacWilliams, B. & McArthur, E. (2016). Inter-professional communication in
healthcare: an integrative review. Nurse education in practice, 19, 36-40.
Fortenberry Jr, J. L. & McGoldrick, P. J. (2016). Internal marketing: A pathway for
healthcare facilities to improve the patient experience. International Journal of
Healthcare Management, 9(1), 28-33.
10
References
Alligood, M. R. (2017). Nursing Theorists and Their Work-E-Book. United States: Elsevier
Health Sciences.
Asiri, S. A., Rohrer, W. W., Al-Surimi, K., Da’ar, O. O. & Ahmed, A. (2016). The
association of leadership styles and empowerment with nurses’ organizational
commitment in an acute health care setting: a cross-sectional study. BMC nursing,
15(1), 38.
Berman, E. (2015). Performance and productivity in public and non-profit organizations.
United Kingdom: Routledge.
Birnbaum, S. (2017). Therapeutic communication in mental health nursing: Aesthetic and
metaphoric processes in the engagement with challenging patients. United Kingdom:
Routledge.
Boamah, S. A., Laschinger, H. K. S., Wong, C. & Clarke, S. (2018). Effect of
transformational leadership on job satisfaction and patient safety outcomes. Nursing
outlook, 66(2), 180-189.
Defenbaugh, N. & Chikotas, N. E. (2016). The outcome of inter-professional education:
Integrating communication studies into a standardized patient experience for
advanced practice nursing students. Nurse education in practice, 16(1), 176-181.
El-Jardali, F. & Fadlallah, R. (2017). A review of national policies and strategies to improve
quality of health care and patient safety: a case study from Lebanon and Jordan. BMC
health services research, 17(1), 568.
Fischer, S. A. (2016). Transformational leadership in nursing: a concept analysis. Journal of
Advanced Nursing, 72(11), 2644-2653.
Foronda, C., MacWilliams, B. & McArthur, E. (2016). Inter-professional communication in
healthcare: an integrative review. Nurse education in practice, 19, 36-40.
Fortenberry Jr, J. L. & McGoldrick, P. J. (2016). Internal marketing: A pathway for
healthcare facilities to improve the patient experience. International Journal of
Healthcare Management, 9(1), 28-33.

HEALTHCARE
11
Gausvik, C., Lautar, A., Miller, L., Pallerla, H. & Schlaudecker, J. (2015). Structured nursing
communication on interdisciplinary acute care teams improves perceptions of safety,
efficiency, understanding of care plan and teamwork as well as job
satisfaction. Journal of multidisciplinary healthcare, 8, 33.
Korlén, S., Essén, A., Lindgren, P., Amer-Wahlin, I. & von Thiele Schwarz, U. (2017).
Managerial strategies to make incentives meaningful and motivating. Journal of
health organization and management, 31(2), 126-141.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M. & Wolf, A. (2017). Barriers and
facilitators to the implementation of person‐centred care in different healthcare
contexts. Scandinavian journal of caring sciences, 31(4), 662-673.
Nudurupati, S. S., Bhattacharya, A., Lascelles, D. & Caton, N. (2015). Strategic sourcing
with multi-stakeholders through value co-creation: evidence from global health care
company. International Journal of Production Economics, 166, 248-257.
Pannick, S., Sevdalis, N. & Athanasiou, T. (2016). Beyond clinical engagement: a pragmatic
model for quality improvement interventions, aligning clinical and managerial
priorities. BMJ Qual Saf, 25(9), 716-725.
Purushotham, S., Meng, C., Che, Z. & Liu, Y. (2018). Benchmarking deep learning models
on large healthcare datasets. Journal of biomedical informatics, 83, 112-134.
Riley, J. B. (2015). Communication in nursing. United States: Elsevier Health Sciences.
Rizk, M. K., Sawhney, M. S., Cohen, J., Pike, I. M., Adler, D. G., Dominitz, J. A. & Wani, S.
(2015). Quality indicators common to all GI endoscopic procedures. The American
journal of gastroenterology, 110(1), 48.
Russ, S. J., Sevdalis, N., Moorthy, K., Mayer, E. K., Rout, S., Caris, J. & Darzi, A. (2015). A
qualitative evaluation of the barriers and facilitators toward implementation of the
WHO surgical safety checklist across hospitals in England: lessons from the “Surgical
Checklist Implementation Project”. Annals of surgery, 261(1), 81-91.
Shahid, S., Ekberg, S., Holloway, M., Jacka, C., Yates, P., Garvey, G., & Thompson, S. C.
(2019). Experiential learning to increase palliative care competence among the
11
Gausvik, C., Lautar, A., Miller, L., Pallerla, H. & Schlaudecker, J. (2015). Structured nursing
communication on interdisciplinary acute care teams improves perceptions of safety,
efficiency, understanding of care plan and teamwork as well as job
satisfaction. Journal of multidisciplinary healthcare, 8, 33.
Korlén, S., Essén, A., Lindgren, P., Amer-Wahlin, I. & von Thiele Schwarz, U. (2017).
Managerial strategies to make incentives meaningful and motivating. Journal of
health organization and management, 31(2), 126-141.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M. & Wolf, A. (2017). Barriers and
facilitators to the implementation of person‐centred care in different healthcare
contexts. Scandinavian journal of caring sciences, 31(4), 662-673.
Nudurupati, S. S., Bhattacharya, A., Lascelles, D. & Caton, N. (2015). Strategic sourcing
with multi-stakeholders through value co-creation: evidence from global health care
company. International Journal of Production Economics, 166, 248-257.
Pannick, S., Sevdalis, N. & Athanasiou, T. (2016). Beyond clinical engagement: a pragmatic
model for quality improvement interventions, aligning clinical and managerial
priorities. BMJ Qual Saf, 25(9), 716-725.
Purushotham, S., Meng, C., Che, Z. & Liu, Y. (2018). Benchmarking deep learning models
on large healthcare datasets. Journal of biomedical informatics, 83, 112-134.
Riley, J. B. (2015). Communication in nursing. United States: Elsevier Health Sciences.
Rizk, M. K., Sawhney, M. S., Cohen, J., Pike, I. M., Adler, D. G., Dominitz, J. A. & Wani, S.
(2015). Quality indicators common to all GI endoscopic procedures. The American
journal of gastroenterology, 110(1), 48.
Russ, S. J., Sevdalis, N., Moorthy, K., Mayer, E. K., Rout, S., Caris, J. & Darzi, A. (2015). A
qualitative evaluation of the barriers and facilitators toward implementation of the
WHO surgical safety checklist across hospitals in England: lessons from the “Surgical
Checklist Implementation Project”. Annals of surgery, 261(1), 81-91.
Shahid, S., Ekberg, S., Holloway, M., Jacka, C., Yates, P., Garvey, G., & Thompson, S. C.
(2019). Experiential learning to increase palliative care competence among the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





