Palliative Care: Healthcare Variation Strategies, Case Study Analysis
VerifiedAdded on 2023/01/18
|9
|2239
|37
Report
AI Summary
This report delves into the complexities of palliative care within the context of healthcare variation, emphasizing the crucial role of nursing strategies. Focusing on a case study of Mrs. Brown, a retiree experiencing acute breathlessness and other symptoms, the report highlights the importance of pain management and emotional/communication support as high-priority interventions. It explores the concept of pain management, including acute and chronic pain, desired patient outcomes, and various nursing interventions such as comprehensive pain examinations and the use of relaxation techniques. The report also examines the significance of emotional and communication support for patients and their families. The report provides an overview of the prevalence of palliative care, the importance of symptom management, and the benefits of integrating palliative care to enhance the quality of life for patients with life-threatening illnesses.

Running head: HEALTHCARE VARIATION 1
Healthcare Variation (Palliative Care)
Student’s Name
Institutional Affiliation
Healthcare Variation (Palliative Care)
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE VARIATION 2
Introduction
Palliative care involves the specialized and comprehensive care offered by an
interdisciplinary team that constitutes GPs, DNs, and CNSs who play significant roles towards
supporting patients and families that live with life-threatening conditions. The significant
concern is on pain and symptom management, advanced care, information sharing, spiritual
support, psychosocial, and coordination of care (Quill & Abernethy, 2013). Notably, about
68% of the Medicare costs in Australia are connected to individuals experiencing chronic
conditions (Maddocks, Lovell, Booth, Man & Higginson, 2017).Palliative care or end of life
care is expected to minimize the disease symptoms that may lead the patients towards suffering
even though it is not expected to cure the illnesses (Maddocks, Lovell, Booth, Man & Higginson,
2017). Based on the case study, Mrs. Brown is a retiree who resides with her husband who is a
part-timer and she experiences acute breathlessness. In this case, the GP has a responsibility to
take Mrs. Brown through palliative approach as she experiences depression, panic attacks, and
also she is poorly nourished. While direct caregivers and health professionals have an ideal
responsibility to assist the patients, two high priority nursing strategies are considered to manage
Mrs. Brown through the palliative approach.
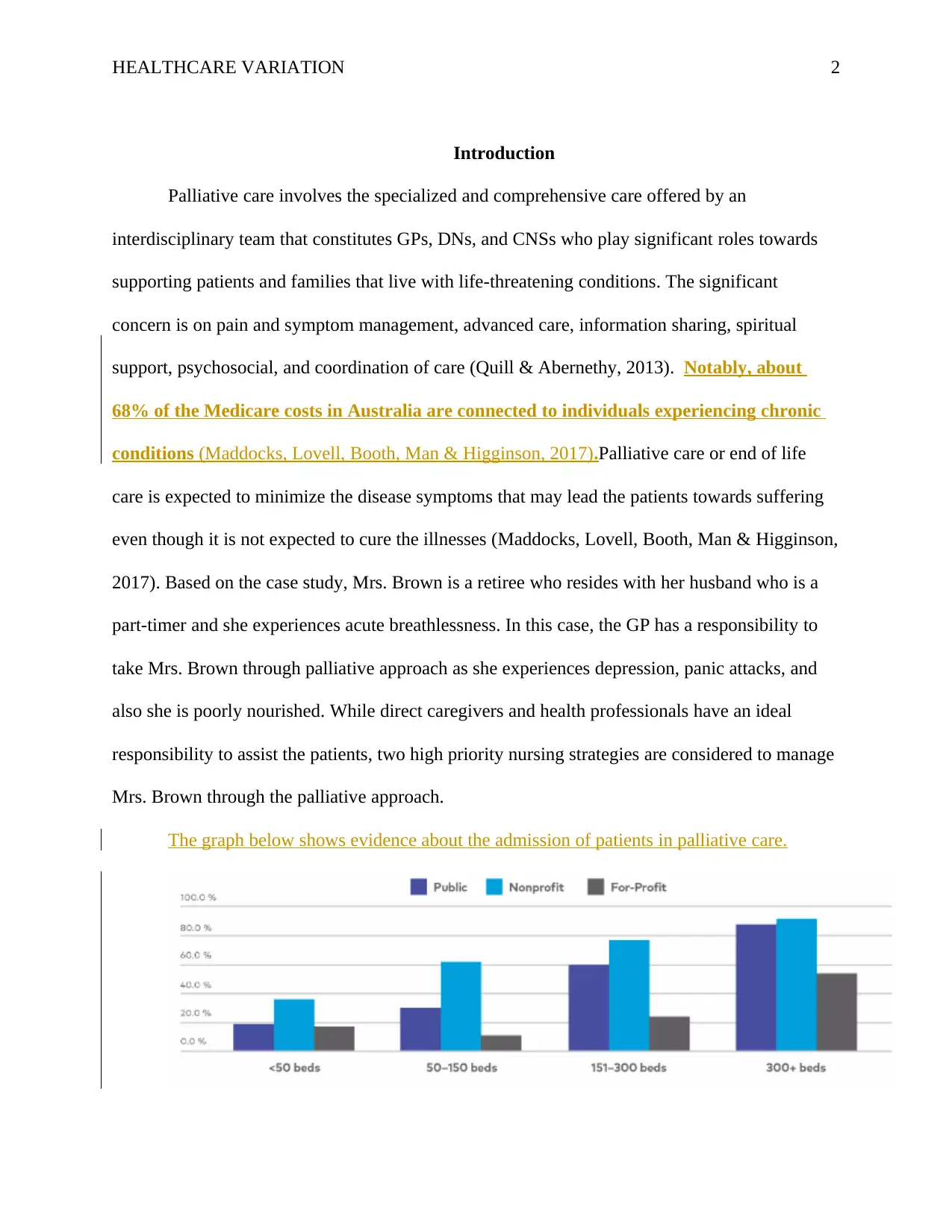
The graph below shows evidence about the admission of patients in palliative care.
Introduction
Palliative care involves the specialized and comprehensive care offered by an
interdisciplinary team that constitutes GPs, DNs, and CNSs who play significant roles towards
supporting patients and families that live with life-threatening conditions. The significant
concern is on pain and symptom management, advanced care, information sharing, spiritual
support, psychosocial, and coordination of care (Quill & Abernethy, 2013). Notably, about
68% of the Medicare costs in Australia are connected to individuals experiencing chronic
conditions (Maddocks, Lovell, Booth, Man & Higginson, 2017).Palliative care or end of life
care is expected to minimize the disease symptoms that may lead the patients towards suffering
even though it is not expected to cure the illnesses (Maddocks, Lovell, Booth, Man & Higginson,
2017). Based on the case study, Mrs. Brown is a retiree who resides with her husband who is a
part-timer and she experiences acute breathlessness. In this case, the GP has a responsibility to
take Mrs. Brown through palliative approach as she experiences depression, panic attacks, and
also she is poorly nourished. While direct caregivers and health professionals have an ideal
responsibility to assist the patients, two high priority nursing strategies are considered to manage
Mrs. Brown through the palliative approach.
The graph below shows evidence about the admission of patients in palliative care.

HEALTHCARE VARIATION 3
Figure 1: Demonstrates the prevalence of patients on palliative care in public, nonprofit,
and for-profit health facilities in Australia (Indian Journal of Palliative Care 2012).
Two High Priority Nursing Strategies (Pain Management, Emotional and
Communication Support)
Symptom management is the most crucial activity that must be prioritized while
providing care to a patient. Symptoms change from a single person to another based on the
specific diagnosis or health problems (Dumanovsky, Augustin, Rogers, Lettang, Meier &
Morrison, 2016). In this case, the GP needs to listen to Mrs. Brown carefully, observe and also,
assess her changes to find the potential nursing priority strategies to incorporate in palliative
approach. Mrs. Brown encounters various symptoms in palliative care that indicates a high
degree of discomforts such as breathlessness, depression, panic attacks, chronic morning coughs
that has white sputum, rhinorrhoea, and poor nourishing. In this case, the nursing priority
strategies that can be considered in Mrs. Brown’s case are chronic pain management and
emotional and communication support. Pain management is a crucial nursing strategy in
palliative care that integrates various protocols for pain relief. From a holistic perspective of pain
management, the GP will attend the physical needs by providing adequate doses of analgesia,
narcotics, timely scheduling, and the co-analgesics use that can help relieve pain. On the other
hand, emotional and communication support is a nursing priority strategy whereby professionals
offering patients the palliative care needs to be sensitive. In this case, the health professional
should be sensitive to Mrs. Brown as she experiences panic attacks, depression, and sleep
problems that cause her health to deteriorate. This nursing strategy priority can be categorized as
emotional and social as it will guide Mrs. Brown and the family towards coping skills.
Figure 1: Demonstrates the prevalence of patients on palliative care in public, nonprofit,
and for-profit health facilities in Australia (Indian Journal of Palliative Care 2012).
Two High Priority Nursing Strategies (Pain Management, Emotional and
Communication Support)
Symptom management is the most crucial activity that must be prioritized while
providing care to a patient. Symptoms change from a single person to another based on the
specific diagnosis or health problems (Dumanovsky, Augustin, Rogers, Lettang, Meier &
Morrison, 2016). In this case, the GP needs to listen to Mrs. Brown carefully, observe and also,
assess her changes to find the potential nursing priority strategies to incorporate in palliative
approach. Mrs. Brown encounters various symptoms in palliative care that indicates a high
degree of discomforts such as breathlessness, depression, panic attacks, chronic morning coughs
that has white sputum, rhinorrhoea, and poor nourishing. In this case, the nursing priority
strategies that can be considered in Mrs. Brown’s case are chronic pain management and
emotional and communication support. Pain management is a crucial nursing strategy in
palliative care that integrates various protocols for pain relief. From a holistic perspective of pain
management, the GP will attend the physical needs by providing adequate doses of analgesia,
narcotics, timely scheduling, and the co-analgesics use that can help relieve pain. On the other
hand, emotional and communication support is a nursing priority strategy whereby professionals
offering patients the palliative care needs to be sensitive. In this case, the health professional
should be sensitive to Mrs. Brown as she experiences panic attacks, depression, and sleep
problems that cause her health to deteriorate. This nursing strategy priority can be categorized as
emotional and social as it will guide Mrs. Brown and the family towards coping skills.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE VARIATION 4
Specifically, supportive communication is crucial for caregivers, patients, and family members
as they can communicate effectively about the process of death (Tracy & Morrison, 2013). This
kind of topic results in discomfort and it is challenging for both the patients and families to
engage in such conversations. In this case, health professionals have an obligation to support the
family towards understanding that death is inevitable. Pain management and emotional and
communication support can work effectively in regard to Mrs. Brown’s case to support her
physically, emotionally, and socially.
Selected Strategy for Physical Symptom (Pain Management)
Of the two selected nursing priority strategies, pain management is selected for a physical
symptom. In this category, there is the acute and chronic pain that have different impacts on a
patient (Manjiani, Paul, Kunnumpurath, Kaye & Vadivelu, 2014). To start with the acute pain, it
involves the unpleasant experience that arises from the potential tissue damages that may occur
suddenly or slowly until the duration of about 6 months. Chronic pain involves an unpleasant
experience that may prolong beyond the unpredictable time of more than 6 months. Acute and
chronic pain connects to chronic physical disability or injuring agents that appear chemically or
emotionally (Hui, Kim, Park, Zhang, Strasser, Cherny & Bruera, 2015). Based on the case study,
acute or chronic pain is evident as Mrs. Brown experiences restlessness, panic attacks, prolonged
cough, and depression that leads her to appear poorly nourished. In this case, the desired patient
outcomes that Mrs. Brown will report when pain is controlled follow the prescriptions, verbalize
ways that guarantee pain relief, and depict the use of relaxation techniques as guided by the GP.
On the other hand, the desired outcome in the family is to ensure cooperation while taking Mrs.
Brown through palliative care.
Specifically, supportive communication is crucial for caregivers, patients, and family members
as they can communicate effectively about the process of death (Tracy & Morrison, 2013). This
kind of topic results in discomfort and it is challenging for both the patients and families to
engage in such conversations. In this case, health professionals have an obligation to support the
family towards understanding that death is inevitable. Pain management and emotional and
communication support can work effectively in regard to Mrs. Brown’s case to support her
physically, emotionally, and socially.
Selected Strategy for Physical Symptom (Pain Management)
Of the two selected nursing priority strategies, pain management is selected for a physical
symptom. In this category, there is the acute and chronic pain that have different impacts on a
patient (Manjiani, Paul, Kunnumpurath, Kaye & Vadivelu, 2014). To start with the acute pain, it
involves the unpleasant experience that arises from the potential tissue damages that may occur
suddenly or slowly until the duration of about 6 months. Chronic pain involves an unpleasant
experience that may prolong beyond the unpredictable time of more than 6 months. Acute and
chronic pain connects to chronic physical disability or injuring agents that appear chemically or
emotionally (Hui, Kim, Park, Zhang, Strasser, Cherny & Bruera, 2015). Based on the case study,
acute or chronic pain is evident as Mrs. Brown experiences restlessness, panic attacks, prolonged
cough, and depression that leads her to appear poorly nourished. In this case, the desired patient
outcomes that Mrs. Brown will report when pain is controlled follow the prescriptions, verbalize
ways that guarantee pain relief, and depict the use of relaxation techniques as guided by the GP.
On the other hand, the desired outcome in the family is to ensure cooperation while taking Mrs.
Brown through palliative care.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE VARIATION 5
Gutgsell et al (2013) argues that various nursing interventions involved in pain
management programme include performing a comprehensive pain examination that includes
location, traits, frequency, severity, quality, duration, and onset. At this point, this step will offer
baseline data whereby a realistic strategy can be established while considering the verbal and
behavioral aspects that relate to the degree of pain experienced by a patient. Pain is also
connected to many elements that may interact to increase the degree of pain felt by the patient
(Towler, Molassiotis & Brearley, 2013). Moreover, it is important to examine the patient’s pain
views as well as behavioral responses. This step in palliative care recognizes the pain control
techniques and patient’s demands. In this case, health professionals will need to realize Mrs.
Brown’s needs and methods to contain panic attacks, depression, and breathlessness. The next
step in pain management involves encouraging Mrs. Brown and her family by explaining to them
the importance of taking narcotic drugs. Notably, in case Mrs. Brown is provided with inaccurate
information based on drugs use, she may experience oversedation that impairs the efforts of pain
control. Pain management also involves verifying the patient’s current and previous narcotic and
analgesic drug use that provides insight about what failed in the past medications that can
influence the therapy plan (Burns & McIlfatrick, 2015). Notably, Mrs. Brown had been admitted
in the hospital three times in the previous years hence it is important to take note of the previous
medications. It is also important to identify the signs and symptoms of pain to ensure the nurse
identifies the effective comfort conditions that will help control Mrs. Brown’s troubling issues of
panic attacks and breathlessness. Relaxation techniques will be required to send the patient into
meditation to minimize the sedative impacts of sedative drugs (Van Mechelen, Aertgeerts, De
Ceulaer, Thoonsen, Vermandere, Warmenhoven & De Lepeleire, 2013). Through meditation,
Mrs. Brown will fight depression and improve her nourishment. The medications will be
Gutgsell et al (2013) argues that various nursing interventions involved in pain
management programme include performing a comprehensive pain examination that includes
location, traits, frequency, severity, quality, duration, and onset. At this point, this step will offer
baseline data whereby a realistic strategy can be established while considering the verbal and
behavioral aspects that relate to the degree of pain experienced by a patient. Pain is also
connected to many elements that may interact to increase the degree of pain felt by the patient
(Towler, Molassiotis & Brearley, 2013). Moreover, it is important to examine the patient’s pain
views as well as behavioral responses. This step in palliative care recognizes the pain control
techniques and patient’s demands. In this case, health professionals will need to realize Mrs.
Brown’s needs and methods to contain panic attacks, depression, and breathlessness. The next
step in pain management involves encouraging Mrs. Brown and her family by explaining to them
the importance of taking narcotic drugs. Notably, in case Mrs. Brown is provided with inaccurate
information based on drugs use, she may experience oversedation that impairs the efforts of pain
control. Pain management also involves verifying the patient’s current and previous narcotic and
analgesic drug use that provides insight about what failed in the past medications that can
influence the therapy plan (Burns & McIlfatrick, 2015). Notably, Mrs. Brown had been admitted
in the hospital three times in the previous years hence it is important to take note of the previous
medications. It is also important to identify the signs and symptoms of pain to ensure the nurse
identifies the effective comfort conditions that will help control Mrs. Brown’s troubling issues of
panic attacks and breathlessness. Relaxation techniques will be required to send the patient into
meditation to minimize the sedative impacts of sedative drugs (Van Mechelen, Aertgeerts, De
Ceulaer, Thoonsen, Vermandere, Warmenhoven & De Lepeleire, 2013). Through meditation,
Mrs. Brown will fight depression and improve her nourishment. The medications will be
HEALTHCARE VARIATION 6
beneficial as they can help retain low pain levels. Lastly, Mrs. Brown will have to manage the
dosage and the medications administered to enhance her quality of life. This nursing priority
strategy will support Mrs. Brown physically and palliative care will be effective as it enhances a
patient’s quality of life.
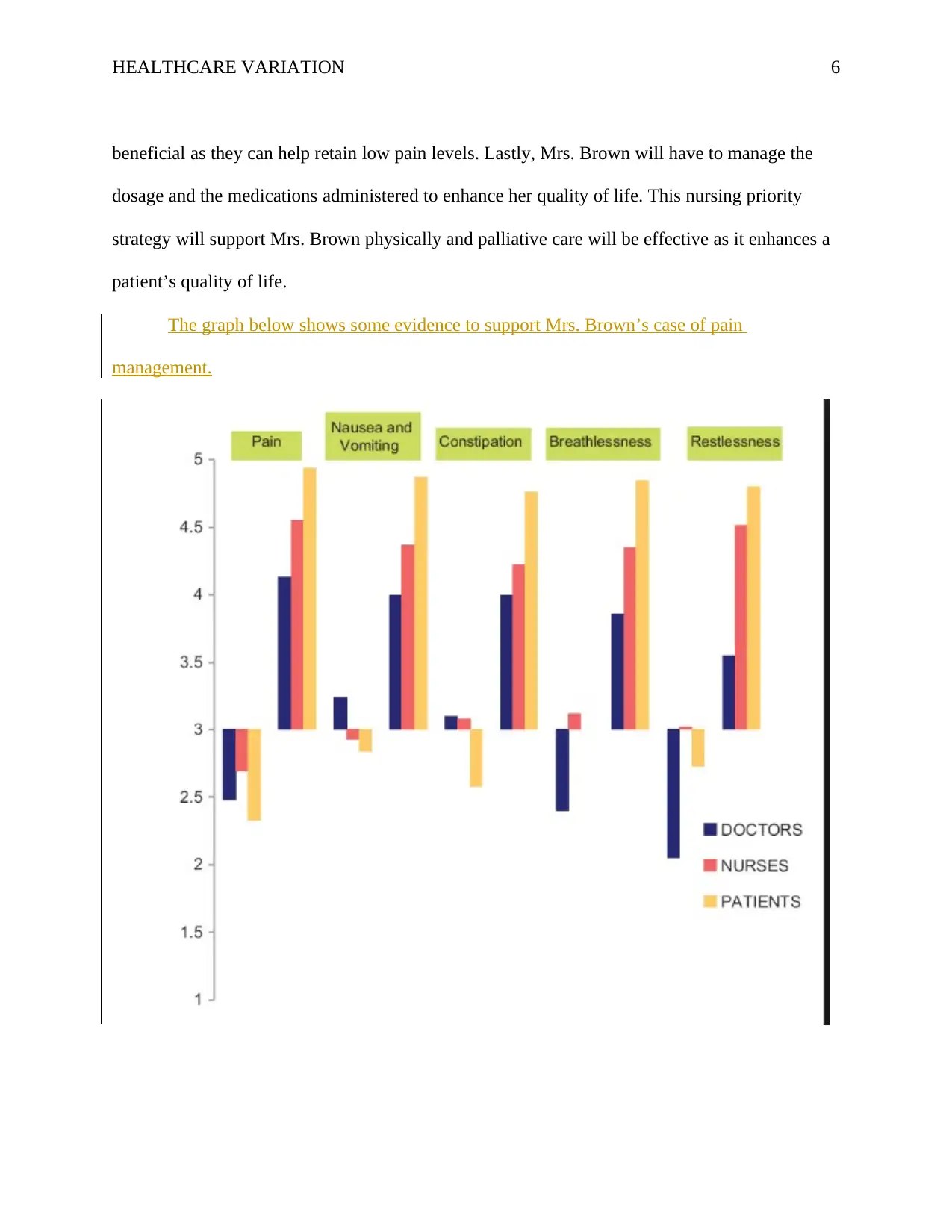
The graph below shows some evidence to support Mrs. Brown’s case of pain
management.
beneficial as they can help retain low pain levels. Lastly, Mrs. Brown will have to manage the
dosage and the medications administered to enhance her quality of life. This nursing priority
strategy will support Mrs. Brown physically and palliative care will be effective as it enhances a
patient’s quality of life.
The graph below shows some evidence to support Mrs. Brown’s case of pain
management.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

HEALTHCARE VARIATION 7
Figure 2: Demonstrates various conditions such as pain nausea and vomiting,
constipation, breathlessness, and restlessness that are experienced by patients in the end of life
(Murtagh, Bausewein, Verne, Groeneveld, Kaloki & Higginson, 2014).
Conclusion
In the past decades, the healthcare system seeks to provide various options to support
patients in effortless dying experience. Therefore, medical treatments integrate palliative care
whose goal is to improve the patient’s quality of life by employing a holistic approach that is
designed to minimize pain and symptoms that patients experience while they suffer from life-
threatening illness. In this case, emotional and communication support, pain management, and
spiritual support are nursing high priority strategies that are integrated into palliative care. Based
on the case study, Mrs. Brown experiences a life-threatening illness hence she is taken through
palliative care using the pain management, emotional and communication support as nursing
priority strategies. Palliative care aims to improve the quality of life of a patient through support
from family and medications [provided by health professionals.
Figure 2: Demonstrates various conditions such as pain nausea and vomiting,
constipation, breathlessness, and restlessness that are experienced by patients in the end of life
(Murtagh, Bausewein, Verne, Groeneveld, Kaloki & Higginson, 2014).
Conclusion
In the past decades, the healthcare system seeks to provide various options to support
patients in effortless dying experience. Therefore, medical treatments integrate palliative care
whose goal is to improve the patient’s quality of life by employing a holistic approach that is
designed to minimize pain and symptoms that patients experience while they suffer from life-
threatening illness. In this case, emotional and communication support, pain management, and
spiritual support are nursing high priority strategies that are integrated into palliative care. Based
on the case study, Mrs. Brown experiences a life-threatening illness hence she is taken through
palliative care using the pain management, emotional and communication support as nursing
priority strategies. Palliative care aims to improve the quality of life of a patient through support
from family and medications [provided by health professionals.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE VARIATION 8
References
Burns, M., & McIlfatrick, S. (2015). Palliative care in dementia: literature review of nurses'
knowledge and attitudes towards pain assessment. International journal of palliative
nursing, 21(8), 400-407.
Dumanovsky, T., Augustin, R., Rogers, M., Lettang, K., Meier, D. E., & Morrison, R. S. (2016).
The growth of palliative care in US hospitals: a status report. Journal of palliative
medicine, 19(1), 8-15.
Gutgsell, K. J., Schluchter, M., Margevicius, S., DeGolia, P. A., McLaughlin, B., Harris, M., &
Wiencek, C. (2013). Music therapy reduces pain in palliative care patients: a randomized
controlled trial. Journal of Pain and Symptom Management, 45(5), 822-831.
Hui, D., Kim, Y. J., Park, J. C., Zhang, Y., Strasser, F., Cherny, N., & Bruera, E. (2015).
Integration of oncology and palliative care: a systematic review. The oncologist, 20(1),
77-83.
Indian Journal of Palliative Care. (2012, May 1). Study of nurses' knowledge about palliative
care: A quantitative cross-sectional survey Prem V, Karvannan H, Kumar SP,
Karthikbabu S, Syed N, Sisodia V, Jaykumar S Indian J Palliat Care. Retrieved from
http://www.jpalliativecare.com/article.asp?issn=0973-
1075;year=2012;volume=18;issue=2;spage=122;epage=127;aulast=Prem
Maddocks, M., Lovell, N., Booth, S., Man, W. D., & Higginson, I. J. (2017). Palliative care and
management of troublesome symptoms for people with chronic obstructive pulmonary
disease. The Lancet, 390(10098), 988-1002.
References
Burns, M., & McIlfatrick, S. (2015). Palliative care in dementia: literature review of nurses'
knowledge and attitudes towards pain assessment. International journal of palliative
nursing, 21(8), 400-407.
Dumanovsky, T., Augustin, R., Rogers, M., Lettang, K., Meier, D. E., & Morrison, R. S. (2016).
The growth of palliative care in US hospitals: a status report. Journal of palliative
medicine, 19(1), 8-15.
Gutgsell, K. J., Schluchter, M., Margevicius, S., DeGolia, P. A., McLaughlin, B., Harris, M., &
Wiencek, C. (2013). Music therapy reduces pain in palliative care patients: a randomized
controlled trial. Journal of Pain and Symptom Management, 45(5), 822-831.
Hui, D., Kim, Y. J., Park, J. C., Zhang, Y., Strasser, F., Cherny, N., & Bruera, E. (2015).
Integration of oncology and palliative care: a systematic review. The oncologist, 20(1),
77-83.
Indian Journal of Palliative Care. (2012, May 1). Study of nurses' knowledge about palliative
care: A quantitative cross-sectional survey Prem V, Karvannan H, Kumar SP,
Karthikbabu S, Syed N, Sisodia V, Jaykumar S Indian J Palliat Care. Retrieved from
http://www.jpalliativecare.com/article.asp?issn=0973-
1075;year=2012;volume=18;issue=2;spage=122;epage=127;aulast=Prem
Maddocks, M., Lovell, N., Booth, S., Man, W. D., & Higginson, I. J. (2017). Palliative care and
management of troublesome symptoms for people with chronic obstructive pulmonary
disease. The Lancet, 390(10098), 988-1002.
HEALTHCARE VARIATION 9
Manjiani, D., Paul, D. B., Kunnumpurath, S., Kaye, A. D., & Vadivelu, N. (2014). Availability
and utilization of opioids for pain management: global issues. Ochsner Journal, 14(2),
208-215.
Murtagh, F. E., Bausewein, C., Verne, J., Groeneveld, E. I., Kaloki, Y. E., & Higginson, I. J.
(2014). How many people need palliative care? A study developing and comparing
methods for population-based estimates. Palliative medicine, 28(1), 49-58.
Quill, T. E., & Abernethy, A. P. (2013). Generalist plus specialist palliative care—creating a
more sustainable model. New England Journal of Medicine, 368(13), 1173-1175.
Towler, P., Molassiotis, A., & Brearley, S. G. (2013). What is the evidence for the use of
acupuncture as an intervention for symptom management in cancer supportive and
palliative care: an integrative overview of reviews. Supportive Care in Cancer, 21(10),
2913-2923.
Tracy, B., & Morrison, R. S. (2013). Pain management in older adults. Clinical
therapeutics, 35(11), 1659-1668.
Van Mechelen, W., Aertgeerts, B., De Ceulaer, K., Thoonsen, B., Vermandere, M.,
Warmenhoven, F.,& De Lepeleire, J. (2013). Defining the palliative care patient: a
systematic review. Palliative Medicine, 27(3), 197-208.
Manjiani, D., Paul, D. B., Kunnumpurath, S., Kaye, A. D., & Vadivelu, N. (2014). Availability
and utilization of opioids for pain management: global issues. Ochsner Journal, 14(2),
208-215.
Murtagh, F. E., Bausewein, C., Verne, J., Groeneveld, E. I., Kaloki, Y. E., & Higginson, I. J.
(2014). How many people need palliative care? A study developing and comparing
methods for population-based estimates. Palliative medicine, 28(1), 49-58.
Quill, T. E., & Abernethy, A. P. (2013). Generalist plus specialist palliative care—creating a
more sustainable model. New England Journal of Medicine, 368(13), 1173-1175.
Towler, P., Molassiotis, A., & Brearley, S. G. (2013). What is the evidence for the use of
acupuncture as an intervention for symptom management in cancer supportive and
palliative care: an integrative overview of reviews. Supportive Care in Cancer, 21(10),
2913-2923.
Tracy, B., & Morrison, R. S. (2013). Pain management in older adults. Clinical
therapeutics, 35(11), 1659-1668.
Van Mechelen, W., Aertgeerts, B., De Ceulaer, K., Thoonsen, B., Vermandere, M.,
Warmenhoven, F.,& De Lepeleire, J. (2013). Defining the palliative care patient: a
systematic review. Palliative Medicine, 27(3), 197-208.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





