Meeting the Needs of Service Users: Schizophrenia Case Study Analysis
VerifiedAdded on 2022/10/09
|16
|4068
|16
Case Study
AI Summary
This case study focuses on Marcia Jones, a 35-year-old woman diagnosed with schizophrenia. It examines her healthcare needs, treatment adherence, and the impact of her condition on her family. The case study delves into the application of Watson's Human Caring Theory and Orem's Theory of Self-Care Deficit Nursing to develop a comprehensive care plan. It explores assessment strategies, treatment settings, management options, and the importance of holistic care. The discussion includes the development of a care plan, reflection on its implementation, and a conclusion summarizing the key findings. The study highlights the challenges of schizophrenia, the significance of patient-centered care, and the role of healthcare professionals in supporting individuals with mental health conditions. The case study also emphasizes the importance of understanding the patient's environment, family dynamics, and cultural context to provide effective and personalized care.

Running head: CASE STUDY - SCHIZOPHRENIA
Case Study - Schizophrenia
Name of the student
Name of the university
Author’s name
Case Study - Schizophrenia
Name of the student
Name of the university
Author’s name
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CASE STUDY - SCHIZOPHRENIA
Table of Contents
Introduction......................................................................................................................................2
Discussion........................................................................................................................................3
Watson’s Human Caring Theory.................................................................................................4
Watson’s transpersonal care........................................................................................................4
Assessment of Schizophrenia..................................................................................................5
Choosing the treatment setting................................................................................................6
Options for management for schizophrenia.............................................................................7
Treatment adherence....................................................................................................................7
Holistic Management of Schizophrenia.......................................................................................8
Addressing the needs of the schizophrenia patients using Orem’s Theory.................................8
Recommendation.............................................................................................................................9
Care Plan........................................................................................................................................11
Reflection.......................................................................................................................................11
Conclusion.....................................................................................................................................12
References......................................................................................................................................14
Table of Contents
Introduction......................................................................................................................................2
Discussion........................................................................................................................................3
Watson’s Human Caring Theory.................................................................................................4
Watson’s transpersonal care........................................................................................................4
Assessment of Schizophrenia..................................................................................................5
Choosing the treatment setting................................................................................................6
Options for management for schizophrenia.............................................................................7
Treatment adherence....................................................................................................................7
Holistic Management of Schizophrenia.......................................................................................8
Addressing the needs of the schizophrenia patients using Orem’s Theory.................................8
Recommendation.............................................................................................................................9
Care Plan........................................................................................................................................11
Reflection.......................................................................................................................................11
Conclusion.....................................................................................................................................12
References......................................................................................................................................14
2CASE STUDY - SCHIZOPHRENIA
Question 1:
Answer 1:
Introduction
Schizophrenia is a serious long term disease of mental wellbeing. People who have
schizophrenia may seem to have lost touch with reality. Schizophrenia, though not as severe as
other mental illnesses, can be quite handicapping in the symptoms. Schizophrenia is correlated
with substantial health, social and economic problems, given its comparatively low frequency
(Sekar et al. 2016). Schizophrenia is diagnosed globally by about 1% of the population. In 2019
around the world, nearly 1.5 million people were diagnosed with schizophrenia. Schizophrenia is
one of the top 15 causes of disability worldwide, according to global statistics. About half of
people with schizophrenia experience mental and/or behavioral health issues in conjunction
(Sekar et al. 2016).
The following article is a case study about a person named Marcia Jones. She is a 35 year
old women married to her partner Ted who is 40 year old and she is a mother of three children
Florence, Mark and Anthony. Marcia Jones has a history of mental issue schizophrenia and that
is why she does not work outside of the home. The case study suggests that Marcia is able to
manage her condition whenever she takes her regular medications. Taking her regular mediations
allow her to manage the household chores and take care of two young children at home and
make sure that Florence gets to school on time and ready to learn. Ted Jones works as a
handyman, but his career is insecure and his family does not have much income. Thus, Ted has
Question 1:
Answer 1:
Introduction
Schizophrenia is a serious long term disease of mental wellbeing. People who have
schizophrenia may seem to have lost touch with reality. Schizophrenia, though not as severe as
other mental illnesses, can be quite handicapping in the symptoms. Schizophrenia is correlated
with substantial health, social and economic problems, given its comparatively low frequency
(Sekar et al. 2016). Schizophrenia is diagnosed globally by about 1% of the population. In 2019
around the world, nearly 1.5 million people were diagnosed with schizophrenia. Schizophrenia is
one of the top 15 causes of disability worldwide, according to global statistics. About half of
people with schizophrenia experience mental and/or behavioral health issues in conjunction
(Sekar et al. 2016).
The following article is a case study about a person named Marcia Jones. She is a 35 year
old women married to her partner Ted who is 40 year old and she is a mother of three children
Florence, Mark and Anthony. Marcia Jones has a history of mental issue schizophrenia and that
is why she does not work outside of the home. The case study suggests that Marcia is able to
manage her condition whenever she takes her regular medications. Taking her regular mediations
allow her to manage the household chores and take care of two young children at home and
make sure that Florence gets to school on time and ready to learn. Ted Jones works as a
handyman, but his career is insecure and his family does not have much income. Thus, Ted has
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CASE STUDY - SCHIZOPHRENIA
to work for long duration and due to this, he cannot always accommodate Marcia if she is not
comfortable at home. The case study states that whenever Marcia forgets to take her medicines,
she fails to manage her mental condition, thus, it makes her to struggle to manage the household
and her children.
The following article will discuss a healthcare plan based upon which a care plan will be
devised for Marcia. At the end of the article a reflective model will also be discussed regarding
the development of the care plan and implementing it to meet Marcia Jones’s healthcare needs.
Discussion
The care plan is a way to communicate the decisions of an ever-changing health care
professional (Gencbas, Bebis and Cicek 2018). The revised plan is passed on during the shift and
during the clinical rounds to the nursing staff as demands of the patient are addressed. Care plans
offer guidelines for personalized client service. A care plan is based on the particular diagnosis
list of each patient and should be structured according to the needs of the individual (Gencbas,
Bebis and Cicek 2018). Care plans promote documentation practice. The care plan will explain
in detail the changes to be made, which health care interventions to be carried out and what
guidance the patient or family members need. It is a guide for staff to look after the client. There
may be elements of the patient's care that team members with certain abilities must be delegated
(Gencbas, Bebis and Cicek 2018). There are five steps too effectively develop a care plan –
Assessment - Collect data from medical records, conduct a patient's physical examination,
determine ADL's, seek information on the health conditions of the patient and know more
signs and symptoms and pathophysiology.
to work for long duration and due to this, he cannot always accommodate Marcia if she is not
comfortable at home. The case study states that whenever Marcia forgets to take her medicines,
she fails to manage her mental condition, thus, it makes her to struggle to manage the household
and her children.
The following article will discuss a healthcare plan based upon which a care plan will be
devised for Marcia. At the end of the article a reflective model will also be discussed regarding
the development of the care plan and implementing it to meet Marcia Jones’s healthcare needs.
Discussion
The care plan is a way to communicate the decisions of an ever-changing health care
professional (Gencbas, Bebis and Cicek 2018). The revised plan is passed on during the shift and
during the clinical rounds to the nursing staff as demands of the patient are addressed. Care plans
offer guidelines for personalized client service. A care plan is based on the particular diagnosis
list of each patient and should be structured according to the needs of the individual (Gencbas,
Bebis and Cicek 2018). Care plans promote documentation practice. The care plan will explain
in detail the changes to be made, which health care interventions to be carried out and what
guidance the patient or family members need. It is a guide for staff to look after the client. There
may be elements of the patient's care that team members with certain abilities must be delegated
(Gencbas, Bebis and Cicek 2018). There are five steps too effectively develop a care plan –
Assessment - Collect data from medical records, conduct a patient's physical examination,
determine ADL's, seek information on the health conditions of the patient and know more
signs and symptoms and pathophysiology.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CASE STUDY - SCHIZOPHRENIA
Determination - The decision of the patient's problem(s)/nursing assessment (draw up a list
of the abnormal evaluation data, compare the abnormal evaluation data with possible nursing
conditions, agree on the diagnosis to be used.
Planning - Document outcomes / measurable goals and health strategies.
Implementation - Initiate the care plan
Evaluation - Determine what targets/outcomes is achieved.
Watson’s Human Caring Theory
The formulation of the Doctrine of Human Caring/Caring Science started more than 35
years ago by Jean Watson, the true legend of nursing; since then the theory has developed, and
yet the idea of creating a transpersonal caring-healing phase persists at the heart of both
recognizing and implementing in nursing practice. The philosophy of human care by Jean
Watson and the moment of compassion is partly based on the principles of transpersonal
psychology (Clark 2016).
Carey S. Clark states that Transpersonal pertains to principles of a special bond,
partnership, subjective relevance and humanity shared. Transpersonal transmits a linkage further
than the self-image, recreating divine parameters that all human beings share with a deeper self,
others, nature and the solar system (Clark 2016).
Jean Watson's philosophy of human care seeks to move away from treatment-centricity
and focuses on "caring." The idea reflects on frameworks of behavior as well as nursing. This
claims that it is difficult to cure a human being as an object to be restored. The philosophical
elements of the philosophy of Watson include the cycle of Caritas, the relationship of
transpersonal care, caring moments and times, and modalities of caring-healing (Ozan and
Determination - The decision of the patient's problem(s)/nursing assessment (draw up a list
of the abnormal evaluation data, compare the abnormal evaluation data with possible nursing
conditions, agree on the diagnosis to be used.
Planning - Document outcomes / measurable goals and health strategies.
Implementation - Initiate the care plan
Evaluation - Determine what targets/outcomes is achieved.
Watson’s Human Caring Theory
The formulation of the Doctrine of Human Caring/Caring Science started more than 35
years ago by Jean Watson, the true legend of nursing; since then the theory has developed, and
yet the idea of creating a transpersonal caring-healing phase persists at the heart of both
recognizing and implementing in nursing practice. The philosophy of human care by Jean
Watson and the moment of compassion is partly based on the principles of transpersonal
psychology (Clark 2016).
Carey S. Clark states that Transpersonal pertains to principles of a special bond,
partnership, subjective relevance and humanity shared. Transpersonal transmits a linkage further
than the self-image, recreating divine parameters that all human beings share with a deeper self,
others, nature and the solar system (Clark 2016).
Jean Watson's philosophy of human care seeks to move away from treatment-centricity
and focuses on "caring." The idea reflects on frameworks of behavior as well as nursing. This
claims that it is difficult to cure a human being as an object to be restored. The philosophical
elements of the philosophy of Watson include the cycle of Caritas, the relationship of
transpersonal care, caring moments and times, and modalities of caring-healing (Ozan and
5CASE STUDY - SCHIZOPHRENIA
Okumuş 2017). With the assumption that these innovations would provide a remedy to Marcia
Jones ' issues, it was felt that it would be fitting to schedule nursing care based on that idea.
Watson’s transpersonal care
Mental illness is characterized as unreason, attributing a sense of an oppressed theme that
induced the rejection of the human psyche and the alienation of the individual in psychological
distress, defining the type of asylum commonly encountered in the field of mental health (Ferraz
et al. 2019). It is obvious why mental illness stays elusive in medicine to this day, that is, there is
no explanation to why this stigmatizing condition occurs and it is not clarified anywhere. The
mental disorder, though, is quickly recognized, because they are usually portrayed by people
who become sick habits outside those typically embraced by the community (Ferraz et al. 2019).
This shift from the hospital-centered to the psychosocial model is made possible by constructing
treatment and service environments in a series of phases through a complex process that includes
national, legal and moral guidance (Ferraz et al. 2019). This demonstrates the need for nurses to
focus on their work and expand their practical outlook, change the day-to-day practices of the
asylum and therapeutic environment so as to confine themselves to tasks such as medications,
baths and dressings, pursue greater approximation and contact with the subjects they care for
(Ferraz et al. 2019).
Assessment of Schizophrenia
The main focus of the current regulations is on aspects of schizophrenia treatment that
have seen major developments since the original guidelines were written. Such recommendations
do not extend in detail to any specific treatment situation and may include minor modifications
to suit the needs of patients in a particular setting.
Okumuş 2017). With the assumption that these innovations would provide a remedy to Marcia
Jones ' issues, it was felt that it would be fitting to schedule nursing care based on that idea.
Watson’s transpersonal care
Mental illness is characterized as unreason, attributing a sense of an oppressed theme that
induced the rejection of the human psyche and the alienation of the individual in psychological
distress, defining the type of asylum commonly encountered in the field of mental health (Ferraz
et al. 2019). It is obvious why mental illness stays elusive in medicine to this day, that is, there is
no explanation to why this stigmatizing condition occurs and it is not clarified anywhere. The
mental disorder, though, is quickly recognized, because they are usually portrayed by people
who become sick habits outside those typically embraced by the community (Ferraz et al. 2019).
This shift from the hospital-centered to the psychosocial model is made possible by constructing
treatment and service environments in a series of phases through a complex process that includes
national, legal and moral guidance (Ferraz et al. 2019). This demonstrates the need for nurses to
focus on their work and expand their practical outlook, change the day-to-day practices of the
asylum and therapeutic environment so as to confine themselves to tasks such as medications,
baths and dressings, pursue greater approximation and contact with the subjects they care for
(Ferraz et al. 2019).
Assessment of Schizophrenia
The main focus of the current regulations is on aspects of schizophrenia treatment that
have seen major developments since the original guidelines were written. Such recommendations
do not extend in detail to any specific treatment situation and may include minor modifications
to suit the needs of patients in a particular setting.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CASE STUDY - SCHIZOPHRENIA
For the management of schizophrenia suffered by Marcia Jones there are certain steps are
to be taken. There is a need for a thorough assessment of Marcia Jones and his / her caregivers.
A comprehensive history and physical and mental health assessments are the foundation of this
test. Steps should be taken to collect data from all angles, in particular from the family. Since
such a treatment plan is much more dependable. Schizophrenia diagnosis is ideally rendered as
per current clinical guidelines whenever possible. It should address all the other aspects
including the symptoms characteristics, symptom frequency, comorbid medical and
psychological problems, and in particular comorbid drug abuse, risks of harm to themselves,
level of operation and the social and cultural climate of the individual. The diagnosis will cover
all other areas. A strong fear level along with a thorough evaluation will help detect certain
patients with abuse/dependence on comorbid drugs. Caregivers ' evaluations will focus on things
like their knowledge and experience of the condition, the conduct and conviction towards
treatment, the effect of the disease on them and their social and personal belongings.
It's essential to keep in mind that evaluation is a continuous operation. As the therapy
continues certain aspects such as medication responsiveness, side effects, commitment to
treatment, the influence of the immediate environment of the individual, medical evaluations,
other health-care needs, ease of access and interaction with the treatment; team may need to be
assessed independently. The care plan design includes agreeing on the environment of the
procedure, the procedures to be used and the issues to be treated. During the planning of the
treatment plan, patients, carers and staff involved in the care may be contacted. Treatment
arrangements shall be focused on requirements, realistic, practicable and adjustable. These
should be re-evaluated and updated constantly, if needed.
For the management of schizophrenia suffered by Marcia Jones there are certain steps are
to be taken. There is a need for a thorough assessment of Marcia Jones and his / her caregivers.
A comprehensive history and physical and mental health assessments are the foundation of this
test. Steps should be taken to collect data from all angles, in particular from the family. Since
such a treatment plan is much more dependable. Schizophrenia diagnosis is ideally rendered as
per current clinical guidelines whenever possible. It should address all the other aspects
including the symptoms characteristics, symptom frequency, comorbid medical and
psychological problems, and in particular comorbid drug abuse, risks of harm to themselves,
level of operation and the social and cultural climate of the individual. The diagnosis will cover
all other areas. A strong fear level along with a thorough evaluation will help detect certain
patients with abuse/dependence on comorbid drugs. Caregivers ' evaluations will focus on things
like their knowledge and experience of the condition, the conduct and conviction towards
treatment, the effect of the disease on them and their social and personal belongings.
It's essential to keep in mind that evaluation is a continuous operation. As the therapy
continues certain aspects such as medication responsiveness, side effects, commitment to
treatment, the influence of the immediate environment of the individual, medical evaluations,
other health-care needs, ease of access and interaction with the treatment; team may need to be
assessed independently. The care plan design includes agreeing on the environment of the
procedure, the procedures to be used and the issues to be treated. During the planning of the
treatment plan, patients, carers and staff involved in the care may be contacted. Treatment
arrangements shall be focused on requirements, realistic, practicable and adjustable. These
should be re-evaluated and updated constantly, if needed.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY - SCHIZOPHRENIA
Choosing the treatment setting
When selecting a treatment facility, the basic principle is to provide services in the least
restrictive environment, which nonetheless satisfies patient and caregiver needs. The most
common treatment environments would be either ambulatory hospitals or inpatient wards.
Wherever possible, patients admitted to the hospital setting should have family caregivers
accompanying them. In the case that hospital care services are not open, it may be appropriate to
alert the patient and/or relatives about such a need and encourage access to the nearest available
medical facility.
Options for management for schizophrenia
Schizophrenia treatment options can be generally categorized as antipsychotic,
electroconvulsive (ECT), adjunctive and psychosocial treatments.
Treatment adherence
Adherence is described as “the degree to which the action of patients corresponds with
the therapeutic order in terms of daily hospital appointments, taking drugs, maintaining diets,
implementing lifestyle changes”. Evidence suggests that approximately half of schizophrenic
patients do not comply with treatment recommendations, approximately one-third miss their
clinical appointments, and 20-60% of patients drop out of treatment (Fiszdon, Kurtz, Choi, Bell
and Martino 2016). Factors commonly correlated with non-adherence involve inadequate
understanding, negative attitude or subjective drug reaction, misuse of comorbid drugs and weak
clinical relationship. Clinicians must make efforts to reduce compliance rates for the medication
and non-adherence to treatment. Some of the prevalent clinician-related factors involve
inadequate clinician-patient/caregiver coordination, weak clinical partnership, and non-
collaborative decision making. Therefore, to improve overall performance, physicians need to
Choosing the treatment setting
When selecting a treatment facility, the basic principle is to provide services in the least
restrictive environment, which nonetheless satisfies patient and caregiver needs. The most
common treatment environments would be either ambulatory hospitals or inpatient wards.
Wherever possible, patients admitted to the hospital setting should have family caregivers
accompanying them. In the case that hospital care services are not open, it may be appropriate to
alert the patient and/or relatives about such a need and encourage access to the nearest available
medical facility.
Options for management for schizophrenia
Schizophrenia treatment options can be generally categorized as antipsychotic,
electroconvulsive (ECT), adjunctive and psychosocial treatments.
Treatment adherence
Adherence is described as “the degree to which the action of patients corresponds with
the therapeutic order in terms of daily hospital appointments, taking drugs, maintaining diets,
implementing lifestyle changes”. Evidence suggests that approximately half of schizophrenic
patients do not comply with treatment recommendations, approximately one-third miss their
clinical appointments, and 20-60% of patients drop out of treatment (Fiszdon, Kurtz, Choi, Bell
and Martino 2016). Factors commonly correlated with non-adherence involve inadequate
understanding, negative attitude or subjective drug reaction, misuse of comorbid drugs and weak
clinical relationship. Clinicians must make efforts to reduce compliance rates for the medication
and non-adherence to treatment. Some of the prevalent clinician-related factors involve
inadequate clinician-patient/caregiver coordination, weak clinical partnership, and non-
collaborative decision making. Therefore, to improve overall performance, physicians need to
8CASE STUDY - SCHIZOPHRENIA
focus on better coordination and strengthen therapeutic cooperation with the patient and the
families. Each time physicians experience insufficient compliance with prescription or therapy,
each effort is needed to understand the reasons behind the same (Fiszdon, Kurtz, Choi, Bell and
Martino 2016).
Reasonable non-adherence evaluation needs to cover cultural, financial, biological and
pharmacological backgrounds assessment. Concerns between patients / caregivers need to be
addressed through proper psycho-education and pharmacological treatment modification. The
use of depot procedures and the use of formulas that exit the mouth under observation will
increase compliance with medication. There is also evidence that cognitive-behavioral methods
and positive coaching have beneficial effects.
Holistic Management of Schizophrenia
Holistic treatment of schizophrenia requires conventional pharmacological intervention,
complementary medical intervention, psychological intervention and other psychosocial aspects
such as housing, healthcare, vocational training, jobs, relationships, intimacy, fitness, general
well-being, alcohol, substance abuse, suicide prevention, depression, leisure, culture, aggressive
behaviour (Ganguly and Moustafa 2019).
Addressing the needs of the schizophrenia patients using Orem’s Theory
The hypothesis of self-care deficit nursing is a grand postulation of nursing, formulated
by Dorothea Orem around 1959 and 2001 (Younas 2017). It is especially used for the recovery
or primary healthcare environments, wherein the patient is expected to become as flexible as
possible. The principle is also known as the Orem's nursing model (Younas 2017). The risk of
morbidity or death associated with poor physical health, which requires an important nursing
focus on better coordination and strengthen therapeutic cooperation with the patient and the
families. Each time physicians experience insufficient compliance with prescription or therapy,
each effort is needed to understand the reasons behind the same (Fiszdon, Kurtz, Choi, Bell and
Martino 2016).
Reasonable non-adherence evaluation needs to cover cultural, financial, biological and
pharmacological backgrounds assessment. Concerns between patients / caregivers need to be
addressed through proper psycho-education and pharmacological treatment modification. The
use of depot procedures and the use of formulas that exit the mouth under observation will
increase compliance with medication. There is also evidence that cognitive-behavioral methods
and positive coaching have beneficial effects.
Holistic Management of Schizophrenia
Holistic treatment of schizophrenia requires conventional pharmacological intervention,
complementary medical intervention, psychological intervention and other psychosocial aspects
such as housing, healthcare, vocational training, jobs, relationships, intimacy, fitness, general
well-being, alcohol, substance abuse, suicide prevention, depression, leisure, culture, aggressive
behaviour (Ganguly and Moustafa 2019).
Addressing the needs of the schizophrenia patients using Orem’s Theory
The hypothesis of self-care deficit nursing is a grand postulation of nursing, formulated
by Dorothea Orem around 1959 and 2001 (Younas 2017). It is especially used for the recovery
or primary healthcare environments, wherein the patient is expected to become as flexible as
possible. The principle is also known as the Orem's nursing model (Younas 2017). The risk of
morbidity or death associated with poor physical health, which requires an important nursing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CASE STUDY - SCHIZOPHRENIA
approach, has risen in people with schizophrenia. Dorothy Orem's Theory of Self-Care Deficit
Nursing (SCDNT), which focuses on people as whole who use their environment for the sake of
wellbeing, has made a substantial contribution to nursing. Understanding patient expectations
through various conceptual perspectives allow nurses to align higher quality, evidence-based
treatment with the experiences, desires and values of patients while taking into consideration the
effect of wider socio-political contexts (Wazni and Gifford 2017).
People experiencing schizophrenia have particular self-care criteria across the condition
and so need different self-care precautions to protect them from poor physical health, elevated
morbidity and premature death (Wazni and Gifford 2017). Orem's SCDNT acknowledges that
habits are learned during the self-care process and that mental disorder causes deviations from
normality, thus, the analysis of the individual needs of people for better physical health is
important (Wazni and Gifford 2017). The interpretive theory stresses that the social world is
built empirically on personal beliefs that can be seen only from the perspective of an individual.
Using the conceptual framework inside the SCDNT to understand the complex health
requirements of schizophrenic patients helps nurses to understand the realities of patients as
viewed by the patients itself that may vary from what society considers “natural”. It enables the
study of any obstacle and self-care challenges that may be focused on social or cultural factors,
in addition to mental disorder, and helps to incorporate individual therapy adapted to their social,
economic and environmental circumstances (Wazni and Gifford 2017).
Recommendation
In addition to detailed advice on drugs and psychiatric health and to tackle common
problems within this community, including smoking cessation, drug abuse treatment and weight
approach, has risen in people with schizophrenia. Dorothy Orem's Theory of Self-Care Deficit
Nursing (SCDNT), which focuses on people as whole who use their environment for the sake of
wellbeing, has made a substantial contribution to nursing. Understanding patient expectations
through various conceptual perspectives allow nurses to align higher quality, evidence-based
treatment with the experiences, desires and values of patients while taking into consideration the
effect of wider socio-political contexts (Wazni and Gifford 2017).
People experiencing schizophrenia have particular self-care criteria across the condition
and so need different self-care precautions to protect them from poor physical health, elevated
morbidity and premature death (Wazni and Gifford 2017). Orem's SCDNT acknowledges that
habits are learned during the self-care process and that mental disorder causes deviations from
normality, thus, the analysis of the individual needs of people for better physical health is
important (Wazni and Gifford 2017). The interpretive theory stresses that the social world is
built empirically on personal beliefs that can be seen only from the perspective of an individual.
Using the conceptual framework inside the SCDNT to understand the complex health
requirements of schizophrenic patients helps nurses to understand the realities of patients as
viewed by the patients itself that may vary from what society considers “natural”. It enables the
study of any obstacle and self-care challenges that may be focused on social or cultural factors,
in addition to mental disorder, and helps to incorporate individual therapy adapted to their social,
economic and environmental circumstances (Wazni and Gifford 2017).
Recommendation
In addition to detailed advice on drugs and psychiatric health and to tackle common
problems within this community, including smoking cessation, drug abuse treatment and weight
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10CASE STUDY - SCHIZOPHRENIA
loss, for the first time, the schizophrenia Patients Outcomes Research Team (PORT) has
composed of new guidelines for treatments. It would be essential for the social worker and the
rest of the multi-disciplinary team to act upon this mentioned recommendation for the
management of Marcia Jones. The PORT authors limit their recommendations to those
interventions that have been tested in randomized controlled trials (Kreyenbuhl, Buchanan,
Dickerson and Dixon 2010).
The PORT analysis advises the use of certain antipsychotic, with the exception of
Clozaril (Clozapine) and Olanzapine (Zyprexa), since these medications are most likely
to provoke important growth in weight and other metabolic adverse effects (Kreyenbuhl,
Buchanan, Dickerson and Dixon 2010).
When patients initially responded to treatment due to having several options, many
experienced a relapse of symptoms. The PORT team suggests any first or second-
generation antipsychotics other than clozapine and specifically states that treatment
should be administered at the lowest appropriate levels to avoid complication
(Kreyenbuhl, Buchanan, Dickerson and Dixon 2010).
The PORT analysis advises that intermittent maintenance therapy — an approach to
prevent antipsychotics before illnesses come back or deteriorate — be allocated only for
patients who feel obliged to continue to take an antipsychotic, as well as those who
cannot endorse the adverse effects (Kreyenbuhl, Buchanan, Dickerson and Dixon 2010).
Psycho-social therapies are known as being an integral part of schizophrenia treatment.
Numerous psychosocial approaches include family counseling, cognitive behavioral
therapy, social skills instruction, clinical remediation, adult engagement services, group
therapy, career recovery, case management, use of community mental health networks
loss, for the first time, the schizophrenia Patients Outcomes Research Team (PORT) has
composed of new guidelines for treatments. It would be essential for the social worker and the
rest of the multi-disciplinary team to act upon this mentioned recommendation for the
management of Marcia Jones. The PORT authors limit their recommendations to those
interventions that have been tested in randomized controlled trials (Kreyenbuhl, Buchanan,
Dickerson and Dixon 2010).
The PORT analysis advises the use of certain antipsychotic, with the exception of
Clozaril (Clozapine) and Olanzapine (Zyprexa), since these medications are most likely
to provoke important growth in weight and other metabolic adverse effects (Kreyenbuhl,
Buchanan, Dickerson and Dixon 2010).
When patients initially responded to treatment due to having several options, many
experienced a relapse of symptoms. The PORT team suggests any first or second-
generation antipsychotics other than clozapine and specifically states that treatment
should be administered at the lowest appropriate levels to avoid complication
(Kreyenbuhl, Buchanan, Dickerson and Dixon 2010).
The PORT analysis advises that intermittent maintenance therapy — an approach to
prevent antipsychotics before illnesses come back or deteriorate — be allocated only for
patients who feel obliged to continue to take an antipsychotic, as well as those who
cannot endorse the adverse effects (Kreyenbuhl, Buchanan, Dickerson and Dixon 2010).
Psycho-social therapies are known as being an integral part of schizophrenia treatment.
Numerous psychosocial approaches include family counseling, cognitive behavioral
therapy, social skills instruction, clinical remediation, adult engagement services, group
therapy, career recovery, case management, use of community mental health networks
11CASE STUDY - SCHIZOPHRENIA
and crisis response systems have been shown to be effective in schizophrenia
management.
To minimize the risk of physiological side effects and clinical morbidity and mortality,
patients should be recommended to change their lifestyle and nutrition. These include
physical exercises, dietary changes and nicotine abstinence etc.
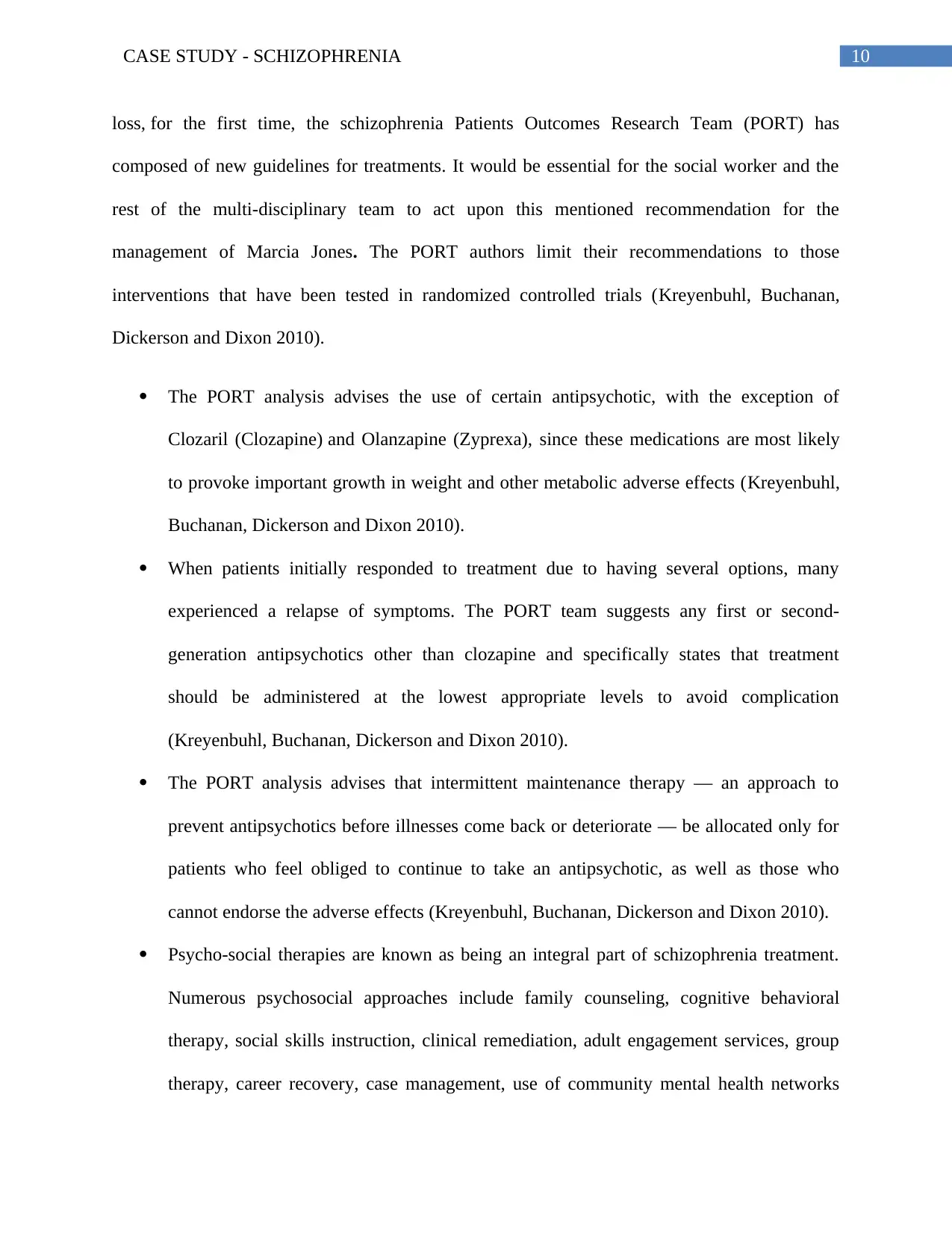
Care Plan
Nursing Assessment Nursing Diagnosis Expected Outcome Intervention Evaluation
Non-realistic
thought
Disorientation
Unable to focus
for a long period
of time
Impaired judgment
Disordered
thought systems
leading to poor
judgment
Disturbance
in cognitive
functioning and
behaviours
Marcia Jones will
be immediately free
of injury
Anxiety will
decrease
Keep focus and
attention to perform
a task or operations
Treatment or
interventions such
as intermittent
maintenance
therapy, Psycho-
social therapies
and antipsychotic
will be initiated.
Following this
treatment will enable
Marcia Jones to
manage her condition
and will also help in
prevent the re-
occurrence of the
condition.
Question 2:
Answer 2:
Reflection
The following reflection will be done based upon the Gibb’s reflective cycle (Husebø,
O'Regan and Nestel 2015). Marcia Jones is 35 year old women married to her partner Ted who is
40 year old and she is a mother of three children Florence, Mark and Anthony. Marcia Jones has
and crisis response systems have been shown to be effective in schizophrenia
management.
To minimize the risk of physiological side effects and clinical morbidity and mortality,
patients should be recommended to change their lifestyle and nutrition. These include
physical exercises, dietary changes and nicotine abstinence etc.
Care Plan
Nursing Assessment Nursing Diagnosis Expected Outcome Intervention Evaluation
Non-realistic
thought
Disorientation
Unable to focus
for a long period
of time
Impaired judgment
Disordered
thought systems
leading to poor
judgment
Disturbance
in cognitive
functioning and
behaviours
Marcia Jones will
be immediately free
of injury
Anxiety will
decrease
Keep focus and
attention to perform
a task or operations
Treatment or
interventions such
as intermittent
maintenance
therapy, Psycho-
social therapies
and antipsychotic
will be initiated.
Following this
treatment will enable
Marcia Jones to
manage her condition
and will also help in
prevent the re-
occurrence of the
condition.
Question 2:
Answer 2:
Reflection
The following reflection will be done based upon the Gibb’s reflective cycle (Husebø,
O'Regan and Nestel 2015). Marcia Jones is 35 year old women married to her partner Ted who is
40 year old and she is a mother of three children Florence, Mark and Anthony. Marcia Jones has
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





