Healthcare Reimbursement Challenges and Strategies at Sinai Hospital
VerifiedAdded on 2022/09/27
|11
|2129
|47
Report
AI Summary
This report provides an analysis of healthcare reimbursement and revenue cycle management at Sinai Hospital of Baltimore, a small private hospital. The report identifies challenges related to insurance verification, claims processing, and revenue collection. It examines the impact of various hospital departments on the reimbursement process, including billing, coding, and patient care. The report discusses the significance of managed care contracts, patient satisfaction, and the role of electronic health records. It covers various healthcare reimbursement methods, including fee-for-service and prospective payment systems, and highlights the importance of coding compliance and ethical considerations. The report concludes by emphasizing the need for healthcare professionals to monitor reimbursement methods and address the cost of liability. The report also cites several references related to healthcare reimbursement and revenue cycle management.
1
Healthcare reimbursement
Institution:
Name:
Date:
1
Healthcare reimbursement
Institution:
Name:
Date:
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Introduction
Sinai Hospital of Baltimore is a ten roomed hospital that was established in 1866 to cater
to the needs of Jewish patients and medical specialists. It is a private hospital based in the
northwest of Baltimore County. They have one superintendent, administrator, cashier, six
nursing staff, one occupational therapist, and three call Centre reps, a cafeteria and maintenance
workforce. Sinai Hospital is a small medical facility with approximately 50 beds for
rehabilitation and long term care plan. The facility is encountering reimbursement and revenue
collection challenges.
Healthcare reimbursement.
Reimbursement is referred to as the circulation of finance in a health care system. The act
is a medical and managerial role, which contribute to capturing, management and gathering
payments from the patients. It is accounting for all operations of a patient. Revenue circulation is
supposed to ensure that patient's account balance is nil. The process begins when calls for an
appointment that ends when all the things are collected. Hospital's workforce is mandated to
ensure they capture patients’ details well, including full name, cellphone contact, and scheme
cover details (Souliotis et al., 2016). Various stages need to be considered from the start to
ensure that everything is well set. Failing to capture insurance cover details during setting up of
appointments, for instance, might lead to time wastage and money when it’s determined that a
patient’s health-care cover is not acknowledged.
Patients are found to take extra financial costs amount obligation to cater to their health
charges through various medical insurance that patients have to select. These vary in several of
co-insurance and co-payments, alongside the annual maximums of the spend expenditure for
2
Introduction
Sinai Hospital of Baltimore is a ten roomed hospital that was established in 1866 to cater
to the needs of Jewish patients and medical specialists. It is a private hospital based in the
northwest of Baltimore County. They have one superintendent, administrator, cashier, six
nursing staff, one occupational therapist, and three call Centre reps, a cafeteria and maintenance
workforce. Sinai Hospital is a small medical facility with approximately 50 beds for
rehabilitation and long term care plan. The facility is encountering reimbursement and revenue
collection challenges.
Healthcare reimbursement.
Reimbursement is referred to as the circulation of finance in a health care system. The act
is a medical and managerial role, which contribute to capturing, management and gathering
payments from the patients. It is accounting for all operations of a patient. Revenue circulation is
supposed to ensure that patient's account balance is nil. The process begins when calls for an
appointment that ends when all the things are collected. Hospital's workforce is mandated to
ensure they capture patients’ details well, including full name, cellphone contact, and scheme
cover details (Souliotis et al., 2016). Various stages need to be considered from the start to
ensure that everything is well set. Failing to capture insurance cover details during setting up of
appointments, for instance, might lead to time wastage and money when it’s determined that a
patient’s health-care cover is not acknowledged.
Patients are found to take extra financial costs amount obligation to cater to their health
charges through various medical insurance that patients have to select. These vary in several of
co-insurance and co-payments, alongside the annual maximums of the spend expenditure for
2
3
patients and their families (Green, 2018). If the insurance confirmation procedures are not
completed, some of the issues that will be encountered are that patent’s claim is denied, improper
collection of co-payments, collection of wrong forms, which takes place some weeks after the
patient is attended. Insurance confirmation is a starting point, and it's the most crucial point, to
request disbursement from the insurance cover for the facility. Furthermore, if this practice is not
well documented it will end up in denial of the claim or the delayed payments for an extent of
one to three months beyond the recommended payment turnaround period of two weeks to two
months.
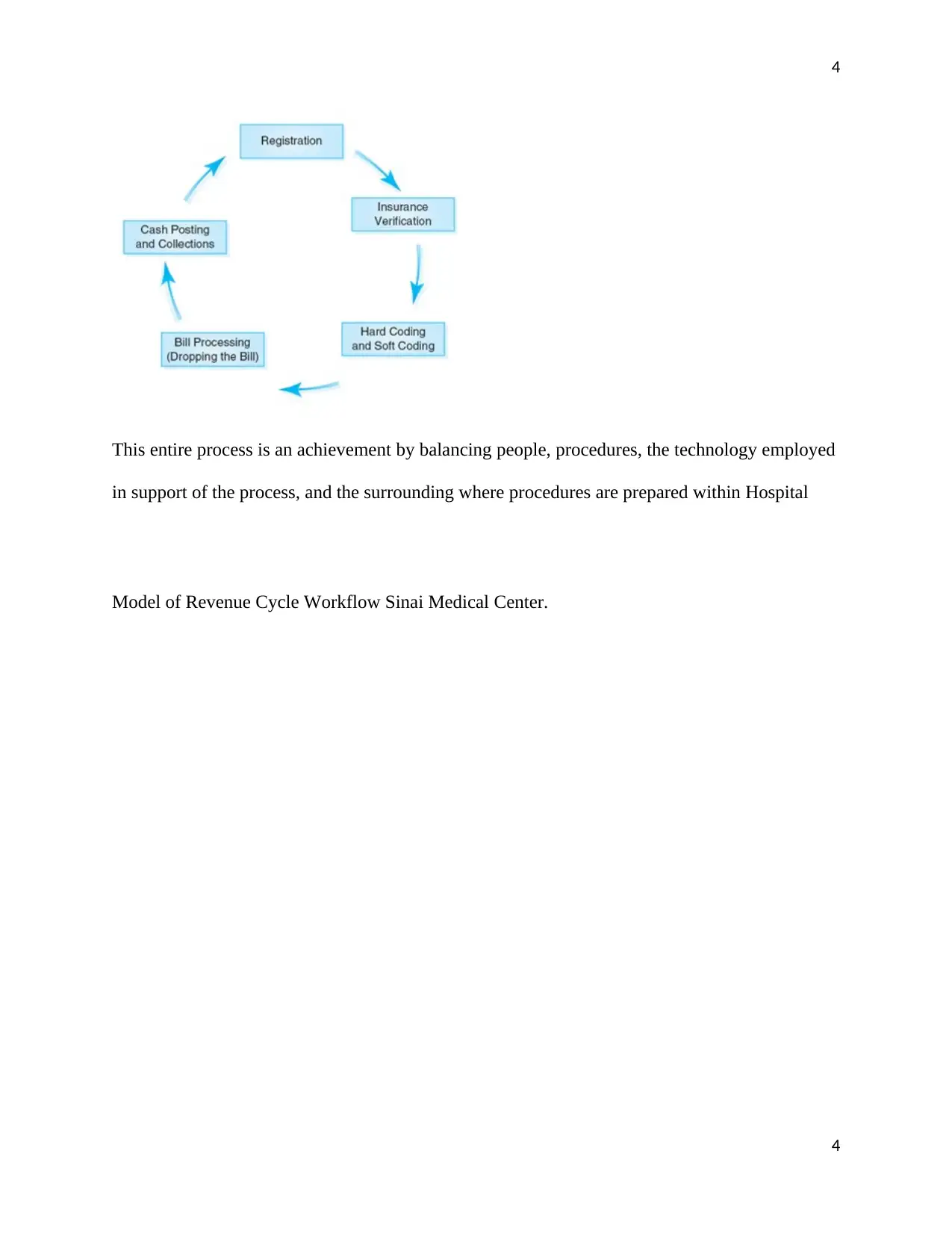
Revenue collection is a crucial component for the reimbursement procedures of medical
facilities. There are various measures of the process that are responsible for their roles and these
roles combine into the overall objective of delivering blameless claims for the services provided
at the medical setting (Glaser, 2010). The initial section of the revenue process is the front-end,
which consist of paying negotiation that takes place without the experience of the patient,
admission element that involves preparing patient for outpatient and inpatient services,
registering, verifying insurance, obtaining prior authorization, and patient financial advice.
In the cycle, the medical staff will provide essential support and services required for
admission the services needed for the admission, and ensure that required essential documents is
available. This section handles the bills, post-payment, adjusting any claim that was rejected due
to faults, appealing all denials that are not correct, and supplying any extra documentation
required as well as making corrections.
3
patients and their families (Green, 2018). If the insurance confirmation procedures are not
completed, some of the issues that will be encountered are that patent’s claim is denied, improper
collection of co-payments, collection of wrong forms, which takes place some weeks after the
patient is attended. Insurance confirmation is a starting point, and it's the most crucial point, to
request disbursement from the insurance cover for the facility. Furthermore, if this practice is not
well documented it will end up in denial of the claim or the delayed payments for an extent of
one to three months beyond the recommended payment turnaround period of two weeks to two
months.
Revenue collection is a crucial component for the reimbursement procedures of medical
facilities. There are various measures of the process that are responsible for their roles and these
roles combine into the overall objective of delivering blameless claims for the services provided
at the medical setting (Glaser, 2010). The initial section of the revenue process is the front-end,
which consist of paying negotiation that takes place without the experience of the patient,
admission element that involves preparing patient for outpatient and inpatient services,
registering, verifying insurance, obtaining prior authorization, and patient financial advice.
In the cycle, the medical staff will provide essential support and services required for
admission the services needed for the admission, and ensure that required essential documents is
available. This section handles the bills, post-payment, adjusting any claim that was rejected due
to faults, appealing all denials that are not correct, and supplying any extra documentation
required as well as making corrections.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
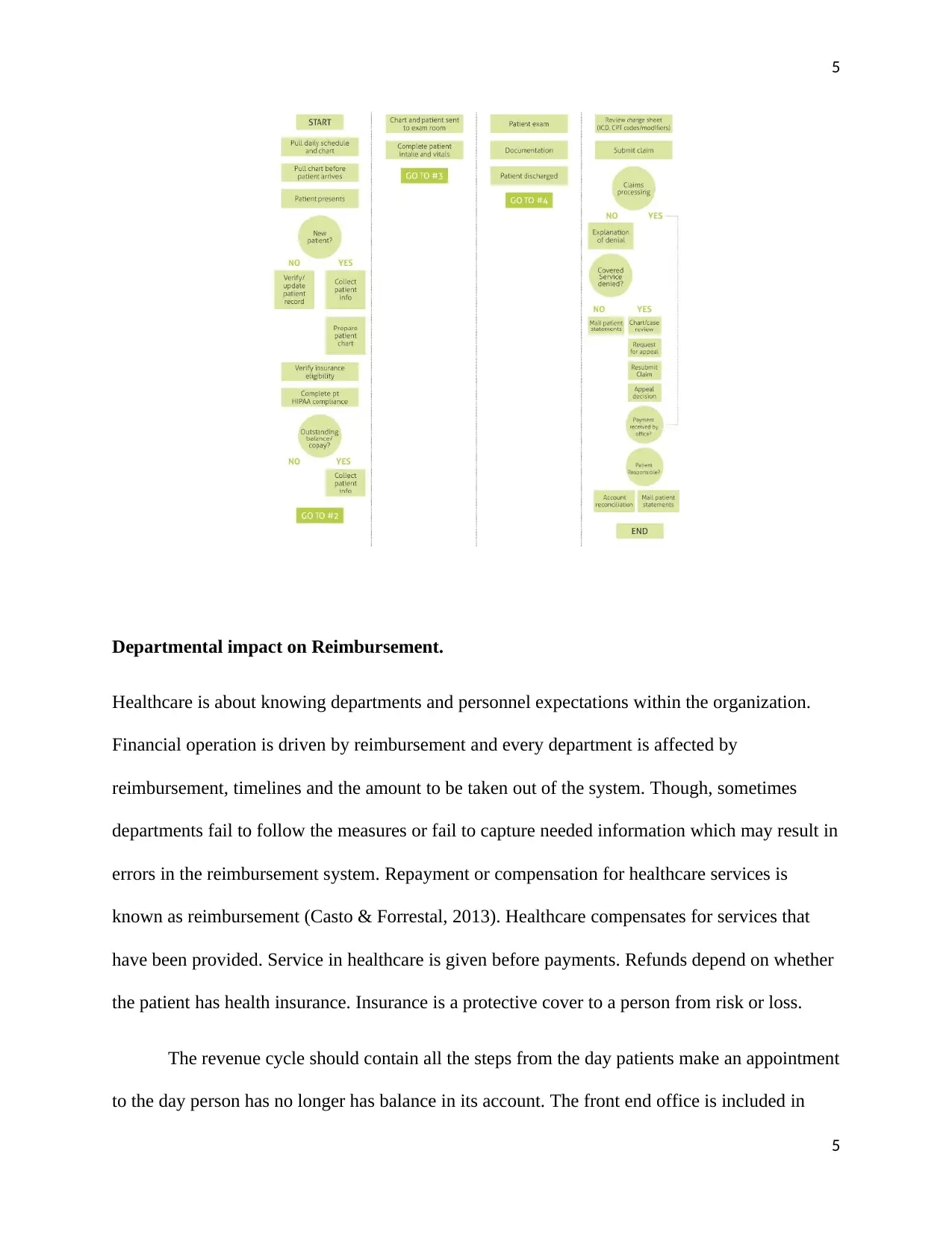
This entire process is an achievement by balancing people, procedures, the technology employed
in support of the process, and the surrounding where procedures are prepared within Hospital
Model of Revenue Cycle Workflow Sinai Medical Center.
4
This entire process is an achievement by balancing people, procedures, the technology employed
in support of the process, and the surrounding where procedures are prepared within Hospital
Model of Revenue Cycle Workflow Sinai Medical Center.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Departmental impact on Reimbursement.
Healthcare is about knowing departments and personnel expectations within the organization.
Financial operation is driven by reimbursement and every department is affected by
reimbursement, timelines and the amount to be taken out of the system. Though, sometimes
departments fail to follow the measures or fail to capture needed information which may result in
errors in the reimbursement system. Repayment or compensation for healthcare services is
known as reimbursement (Casto & Forrestal, 2013). Healthcare compensates for services that
have been provided. Service in healthcare is given before payments. Refunds depend on whether
the patient has health insurance. Insurance is a protective cover to a person from risk or loss.
The revenue cycle should contain all the steps from the day patients make an appointment
to the day person has no longer has balance in its account. The front end office is included in
5
Departmental impact on Reimbursement.
Healthcare is about knowing departments and personnel expectations within the organization.
Financial operation is driven by reimbursement and every department is affected by
reimbursement, timelines and the amount to be taken out of the system. Though, sometimes
departments fail to follow the measures or fail to capture needed information which may result in
errors in the reimbursement system. Repayment or compensation for healthcare services is
known as reimbursement (Casto & Forrestal, 2013). Healthcare compensates for services that
have been provided. Service in healthcare is given before payments. Refunds depend on whether
the patient has health insurance. Insurance is a protective cover to a person from risk or loss.
The revenue cycle should contain all the steps from the day patients make an appointment
to the day person has no longer has balance in its account. The front end office is included in
5
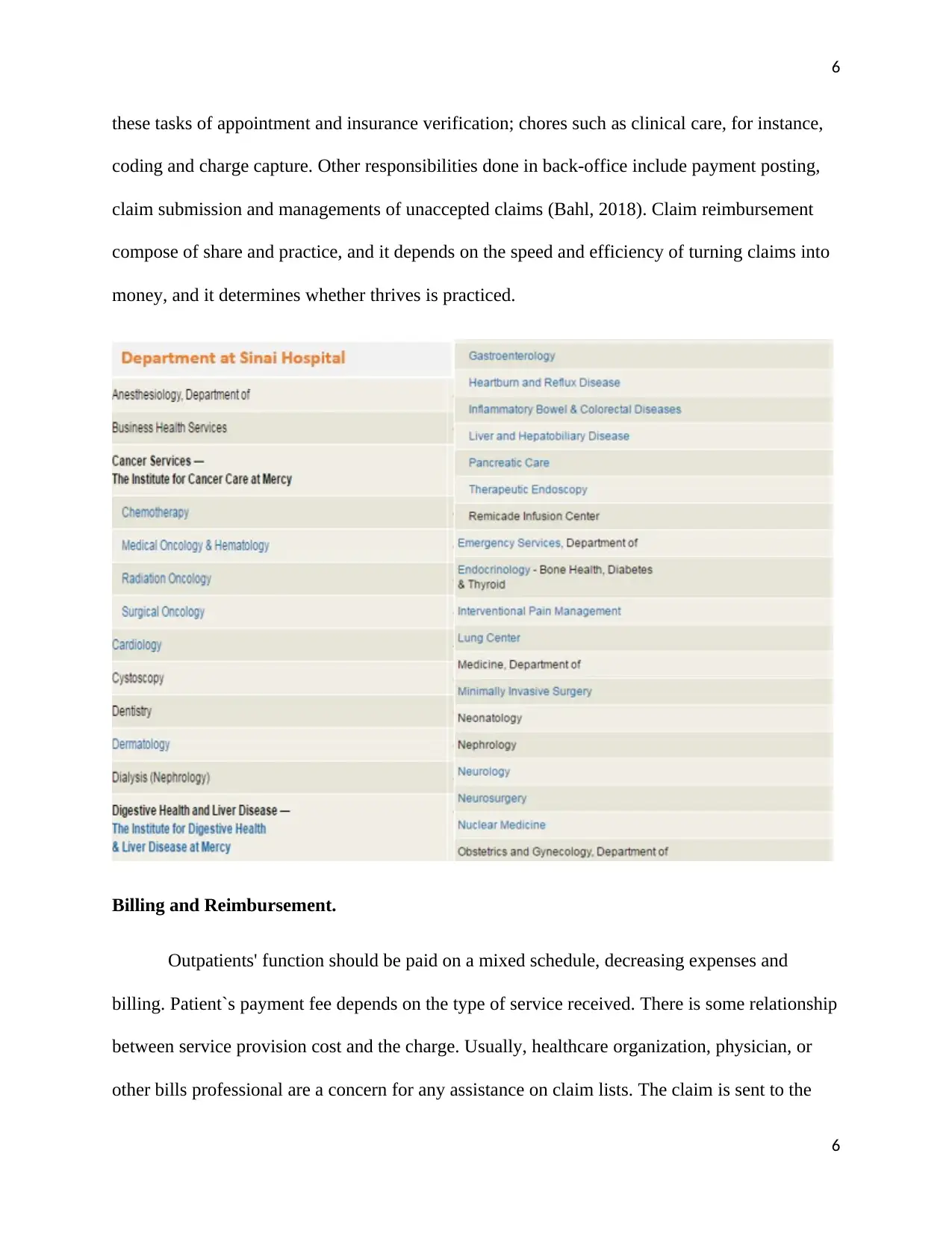
6
these tasks of appointment and insurance verification; chores such as clinical care, for instance,
coding and charge capture. Other responsibilities done in back-office include payment posting,
claim submission and managements of unaccepted claims (Bahl, 2018). Claim reimbursement
compose of share and practice, and it depends on the speed and efficiency of turning claims into
money, and it determines whether thrives is practiced.
Billing and Reimbursement.
Outpatients' function should be paid on a mixed schedule, decreasing expenses and
billing. Patient`s payment fee depends on the type of service received. There is some relationship
between service provision cost and the charge. Usually, healthcare organization, physician, or
other bills professional are a concern for any assistance on claim lists. The claim is sent to the
6
these tasks of appointment and insurance verification; chores such as clinical care, for instance,
coding and charge capture. Other responsibilities done in back-office include payment posting,
claim submission and managements of unaccepted claims (Bahl, 2018). Claim reimbursement
compose of share and practice, and it depends on the speed and efficiency of turning claims into
money, and it determines whether thrives is practiced.
Billing and Reimbursement.
Outpatients' function should be paid on a mixed schedule, decreasing expenses and
billing. Patient`s payment fee depends on the type of service received. There is some relationship
between service provision cost and the charge. Usually, healthcare organization, physician, or
other bills professional are a concern for any assistance on claim lists. The claim is sent to the
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
health agency and is known as submitting a claim. Health stipulation is within government
policy and regulation; the third party pays claims. Physicians mostly use this method of billing.
Specific payments made by the patients for each service received is known as Self-Pay fee. The
guarantors or patients pay by themselves to the service providers such as clinics, physicians or
hospitals. The patients get reimbursements to cover health benefits from a government agency or
health insurance.
Marketing and Reimbursement.
Managed cared contract is an important element in the managing of revenue. Contracts
which are managed can be utilized effectively as a reliable source of increasing revenue in an
organization. Reliable managed care contracts not only increase the revenue but also increase
patients' satisfaction since patients are convinced by the excellent treatment and services (Bahl,
2018). The availability of managed care contracts is essential as it carries the relevant insurance
payment schedule, which may be negotiated.
Convincing a patient in managed care requires proper preparedness, good relationship,
and negotiating skills. Some of the strategies used in negotiating about managed care contract
include: analyzing contracts, influencing, knowing what you want and negotiating and precisely
what you require. Organization requires to build good contract negotiating skills that will enable
them to win the customer and easily reach an acceptable agreement.
Patient care is essential health care sector; it is necessary to satisfy the customer and
make them feel happy. Even though most doctors work on improving their medical skills, they
7
health agency and is known as submitting a claim. Health stipulation is within government
policy and regulation; the third party pays claims. Physicians mostly use this method of billing.
Specific payments made by the patients for each service received is known as Self-Pay fee. The
guarantors or patients pay by themselves to the service providers such as clinics, physicians or
hospitals. The patients get reimbursements to cover health benefits from a government agency or
health insurance.
Marketing and Reimbursement.
Managed cared contract is an important element in the managing of revenue. Contracts
which are managed can be utilized effectively as a reliable source of increasing revenue in an
organization. Reliable managed care contracts not only increase the revenue but also increase
patients' satisfaction since patients are convinced by the excellent treatment and services (Bahl,
2018). The availability of managed care contracts is essential as it carries the relevant insurance
payment schedule, which may be negotiated.
Convincing a patient in managed care requires proper preparedness, good relationship,
and negotiating skills. Some of the strategies used in negotiating about managed care contract
include: analyzing contracts, influencing, knowing what you want and negotiating and precisely
what you require. Organization requires to build good contract negotiating skills that will enable
them to win the customer and easily reach an acceptable agreement.
Patient care is essential health care sector; it is necessary to satisfy the customer and
make them feel happy. Even though most doctors work on improving their medical skills, they
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
also need to learn ways of strengthening their patient care skill (Mindel & Mathiassen, 2015).
Customer is key to any business and determines the level of success. Excellent customer care
skills include handling complaints and concerns from customers. Most health organization has
put more efforts into improving its healthcare system, which requires a collaborative relationship
between all health departments.
Health organization are mandated to maintain documentation and provide a reliable
report from a certified electronic health record system to access all the quality measure data.
These systems should be an audit to determine their reliability (O’Donnell et al., 2013). The
program also prevents improper payments; system audits assist in curbing irregular payment.
However, there has been an attempt to fraud and abuse electronic health record through
misrepresentation of services, altering of billing system, and recording false information in the
system health record. Other ethical issues include people impersonating others, for example,
using someone identity, including someone who is not eligible for a policy and failure to remove
a non-eligible person from a system.
Conclusion
In conclusion, Healthcare Reimbursement entails information about healthcare payment
systems from one authoritative source. The system checks the financial systems in a daily health
care environment and providing a fundamental understanding of public funding programs, health
insurance and the kind of services offered to the patients. Administrators and health care
personnel frequently learn payment systems (Acemoglu & Finkelstein, 2008). Coding
compliance and clinical Coding has information about today`s approval code sets; it also
describes then relations between coded data, accordance and reimbursement with the guidelines
and regulation of private and the payers. Private and commercial health care insurance and the
8
also need to learn ways of strengthening their patient care skill (Mindel & Mathiassen, 2015).
Customer is key to any business and determines the level of success. Excellent customer care
skills include handling complaints and concerns from customers. Most health organization has
put more efforts into improving its healthcare system, which requires a collaborative relationship
between all health departments.
Health organization are mandated to maintain documentation and provide a reliable
report from a certified electronic health record system to access all the quality measure data.
These systems should be an audit to determine their reliability (O’Donnell et al., 2013). The
program also prevents improper payments; system audits assist in curbing irregular payment.
However, there has been an attempt to fraud and abuse electronic health record through
misrepresentation of services, altering of billing system, and recording false information in the
system health record. Other ethical issues include people impersonating others, for example,
using someone identity, including someone who is not eligible for a policy and failure to remove
a non-eligible person from a system.
Conclusion
In conclusion, Healthcare Reimbursement entails information about healthcare payment
systems from one authoritative source. The system checks the financial systems in a daily health
care environment and providing a fundamental understanding of public funding programs, health
insurance and the kind of services offered to the patients. Administrators and health care
personnel frequently learn payment systems (Acemoglu & Finkelstein, 2008). Coding
compliance and clinical Coding has information about today`s approval code sets; it also
describes then relations between coded data, accordance and reimbursement with the guidelines
and regulation of private and the payers. Private and commercial health care insurance and the
8
9
entailment understanding of health care insurance policy are explained by Voluntary Healthcare
Insurance Plans.
In healthcare, there are multiple methods of reimbursement to physicians, hospital, health
providers, depending on the nature of service provided to patients. Reimbursement occurs after,
provision of health care following reimbursement (Harrington, 2019). There are significant types
of payment methods episode of care and fee for care reimbursement based on the unit of
payment (Vian, 2008. The most basic reimbursement methods include managed care, surveying
fee-for-service, prospective and global payments systems.
Health care professionals should monitor health care methods of reimbursement. The
major problem for the residence is the cost of liability. Whenever the issue is significant, the
inadequate reimbursement for minor service is not addressed. Many physicians find it hard to
cover their practices due to the lowering of medical reimbursement rates by state.
9
entailment understanding of health care insurance policy are explained by Voluntary Healthcare
Insurance Plans.
In healthcare, there are multiple methods of reimbursement to physicians, hospital, health
providers, depending on the nature of service provided to patients. Reimbursement occurs after,
provision of health care following reimbursement (Harrington, 2019). There are significant types
of payment methods episode of care and fee for care reimbursement based on the unit of
payment (Vian, 2008. The most basic reimbursement methods include managed care, surveying
fee-for-service, prospective and global payments systems.
Health care professionals should monitor health care methods of reimbursement. The
major problem for the residence is the cost of liability. Whenever the issue is significant, the
inadequate reimbursement for minor service is not addressed. Many physicians find it hard to
cover their practices due to the lowering of medical reimbursement rates by state.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
References.
Acemoglu, D., & Finkelstein, A. (2008). Input and technology choices in regulated industries:
Evidence from the health care sector. Journal of Political Economy, 116(5), 837-880.
Bahl, T. (2018). Enhancement of revenue cycle management: case in change
management (Doctoral dissertation, University of Pittsburgh, S., & Cierkens, K. (2008).
Legal aspects of E-HEALTH. Studies in health technology and informatics, 141, 47-56.
Casto, A. B., & Forrestal, E. (2013). Principles of healthcare reimbursement. American Health
Information Management Association.
Cavagnero, E. (2008). Health sector reforms in Argentina and the performance of the health
financing system. Health policy, 88(1), 88-99.
Green, M. (2018). Understanding health insurance: A guide to billing and reimbursement.
Cengage Learning.
Glaser, J. (2010). HITECH lays the foundation for more ambitious outcomes-based
reimbursement. Am J Manag Care, 16(12 Suppl HIT), SP19-SP23.
Harrington, M. K. (2019). Health Care Finance and the Mechanics of Insurance and
Reimbursement. Jones & Bartlett Learning.
Mindel, V., & Mathiassen, L. (2015, January). Contextualist inquiry into hospital revenue cycle
transformation: Bridging research and practice. In 2015 48th Hawaii International
Conference on System Sciences (pp. 2960-2969). IEEE.
10
References.
Acemoglu, D., & Finkelstein, A. (2008). Input and technology choices in regulated industries:
Evidence from the health care sector. Journal of Political Economy, 116(5), 837-880.
Bahl, T. (2018). Enhancement of revenue cycle management: case in change
management (Doctoral dissertation, University of Pittsburgh, S., & Cierkens, K. (2008).
Legal aspects of E-HEALTH. Studies in health technology and informatics, 141, 47-56.
Casto, A. B., & Forrestal, E. (2013). Principles of healthcare reimbursement. American Health
Information Management Association.
Cavagnero, E. (2008). Health sector reforms in Argentina and the performance of the health
financing system. Health policy, 88(1), 88-99.
Green, M. (2018). Understanding health insurance: A guide to billing and reimbursement.
Cengage Learning.
Glaser, J. (2010). HITECH lays the foundation for more ambitious outcomes-based
reimbursement. Am J Manag Care, 16(12 Suppl HIT), SP19-SP23.
Harrington, M. K. (2019). Health Care Finance and the Mechanics of Insurance and
Reimbursement. Jones & Bartlett Learning.
Mindel, V., & Mathiassen, L. (2015, January). Contextualist inquiry into hospital revenue cycle
transformation: Bridging research and practice. In 2015 48th Hawaii International
Conference on System Sciences (pp. 2960-2969). IEEE.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
O’Donnell, A. N., Williams, M., & Kilbourne, A. M. (2013). Overcoming roadblocks: current
and emerging reimbursement strategies for integrated mental health services in primary
care. Journal of general internal medicine, 28(12), 1667-1672.
Souliotis, K., Golna, C., Tountas, Y., Siskou, O., Kaitelidou, D., & Liaropoulos, L. (2016).
Informal payments in the Greek health sector amid the financial crisis: old habits die last.
The European Journal of Health Economics, 17(2), 159-170.
Vian, T. (2008). Review of corruption in the health sector: theory, methods and
interventions. Health policy and planning, 23(2), 83-94.
11
O’Donnell, A. N., Williams, M., & Kilbourne, A. M. (2013). Overcoming roadblocks: current
and emerging reimbursement strategies for integrated mental health services in primary
care. Journal of general internal medicine, 28(12), 1667-1672.
Souliotis, K., Golna, C., Tountas, Y., Siskou, O., Kaitelidou, D., & Liaropoulos, L. (2016).
Informal payments in the Greek health sector amid the financial crisis: old habits die last.
The European Journal of Health Economics, 17(2), 159-170.
Vian, T. (2008). Review of corruption in the health sector: theory, methods and
interventions. Health policy and planning, 23(2), 83-94.
11
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

