Healthcare Financing in Low and Middle-Income Countries and UHC
VerifiedAdded on 2022/11/25
|15
|3895
|318
Report
AI Summary
This report investigates healthcare financing in Low and Middle-Income Countries (LMICs) and its significance in achieving Universal Health Coverage (UHC). It begins by emphasizing healthcare as a fundamental human right and the WHO's UHC program, which aims to ensure access to quality, affordable healthcare services without financial strain. The report outlines the objectives and components of UHC, highlighting the challenges faced by LMICs, such as corruption and reliance on out-of-pocket payments. It examines health financing methods, including government support, health insurance, and the laws of health economics. The report then delves into reforms that accelerate UHC progress, focusing on efficient healthcare financial systems, including pooling funds through voluntary and compulsory techniques. It also explores alternative financing methods like user fees and innovative financing methods, such as national and international-based approaches. The report concludes by assessing these financing mechanisms based on feasibility, equity, efficiency, and sustainability, underscoring the importance of effective evaluation for successful implementation.

Running header: Healthcare financing in LMICs and Achieving UHC 1
Healthcare financing in Low and Middle-Income Countries and
Achieving Universal Health Coverage
Name:
Institution:
Healthcare financing in Low and Middle-Income Countries and
Achieving Universal Health Coverage
Name:
Institution:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LMICs and UHC 2
Introduction
There is no doubt quality health, and affordable healthcare service is a fundamental
human right; thus, various governments are using multiple mechanisms and resources to ensure
the services are efficiently delivered. Consequently, the world health organization (WHO) has
adopted the universal health coverage program that seeks to ensure all persons and societies not
only access but also use the palliative, curative, and preventative healthcare services they need of
standard quality (WHO, 2019). Moreover, WHO advocates that the services should not impact
the user to any form financial stress. Notably, the UHC incorporates three objectives, which
include equity access to healthcare services, whereby everyone should access the service despite
the ability to pay (WHO, 2019). The second objective emphasizes on quality services that are
efficient to improve the general health of users, and the third seeks to protect the users from any
risks associated with finance. Notably, there are various components of UHC, which include
healthcare workforce, facilities, governance, communication networks, and financing.
Moreover, UHC not only advocates for individual treatment but also the general
population through various programs, such as public health campaigns (WHO, 2019). There are
two measures that aid in the evaluation and monitoring the progress towards UHC, which
include the proportion of a population that can access primary healthcare services and that
spends more than 10% of household income on healthcare services. Despite the UHC initiative,
at least half of the world population, especially in the low and middle-income countries (LMICs)
do not have full coverage of essential health services. Moreover, approximately 100 million
people are still subjected to poverty due to the increased cost of healthcare services (WHO,
2019). The WHO 2018 report exhibits that more than 800 million people, which accounts for
Introduction
There is no doubt quality health, and affordable healthcare service is a fundamental
human right; thus, various governments are using multiple mechanisms and resources to ensure
the services are efficiently delivered. Consequently, the world health organization (WHO) has
adopted the universal health coverage program that seeks to ensure all persons and societies not
only access but also use the palliative, curative, and preventative healthcare services they need of
standard quality (WHO, 2019). Moreover, WHO advocates that the services should not impact
the user to any form financial stress. Notably, the UHC incorporates three objectives, which
include equity access to healthcare services, whereby everyone should access the service despite
the ability to pay (WHO, 2019). The second objective emphasizes on quality services that are
efficient to improve the general health of users, and the third seeks to protect the users from any
risks associated with finance. Notably, there are various components of UHC, which include
healthcare workforce, facilities, governance, communication networks, and financing.
Moreover, UHC not only advocates for individual treatment but also the general
population through various programs, such as public health campaigns (WHO, 2019). There are
two measures that aid in the evaluation and monitoring the progress towards UHC, which
include the proportion of a population that can access primary healthcare services and that
spends more than 10% of household income on healthcare services. Despite the UHC initiative,
at least half of the world population, especially in the low and middle-income countries (LMICs)
do not have full coverage of essential health services. Moreover, approximately 100 million
people are still subjected to poverty due to the increased cost of healthcare services (WHO,
2019). The WHO 2018 report exhibits that more than 800 million people, which accounts for
LMICs and UHC 3
12% of the continent’s population allocate more than 10% of their respective household budgets
to cater to healthcare services.
Notably, in the year 2005 all the 192 member countries of the United Nations have an
agreement in achieving the UHC under the vision 2030 program (Reeves, Gourtsoyannis, Basu,
McCoy, McKee & Stuckler, 2015). However, LMICs healthcare systems are faced with various
challenges, such as corruption thus inhibiting the adoption and implementations of UHC.
Notably, only 20 LMICs have adopted a verifiable UHC program (Reeves, Gourtsoyannis, Basu,
McCoy, McKee & Stuckler, 2015). 2010 WHO report outlines various financial strategies that
will aid in achieving UHC, which include improving efficiency in taxation, implementing
innovative financial techniques, appropriate allocations of government budgets towards
healthcare, and increasing development assistance for health (Friebel, Molloy, Leatherman,
Dixon, Bauhoff, & Chalkidou, 2018). Moreover, the Lancet commission recommended that
UHC is only achievable by raising revenues through taxation. The primary source of government
funds is tax revenues in many countries; consequently, LMICs taxes account for 65% of the total
government revenues. Therefore, the following paper seeks to exhibit the healthcare financing in
LMICs and achieving the UHC. Moreover, the paper will discuss health financing alternatives
using a comparative healthcare system analysis
Health Financing
The adoption and implementation of the UHC are dependent on the healthcare funding
techniques used by the government. One of the factors that have experienced significant
development is the mode of payment of healthcare services whereby most industrialized or
developed countries tend to use the health insurance rather than personal payment (Tulchinsky &
Varavikova, 2014). However, the LMICs still use the traditional mechanisms, such as the out-of-
12% of the continent’s population allocate more than 10% of their respective household budgets
to cater to healthcare services.
Notably, in the year 2005 all the 192 member countries of the United Nations have an
agreement in achieving the UHC under the vision 2030 program (Reeves, Gourtsoyannis, Basu,
McCoy, McKee & Stuckler, 2015). However, LMICs healthcare systems are faced with various
challenges, such as corruption thus inhibiting the adoption and implementations of UHC.
Notably, only 20 LMICs have adopted a verifiable UHC program (Reeves, Gourtsoyannis, Basu,
McCoy, McKee & Stuckler, 2015). 2010 WHO report outlines various financial strategies that
will aid in achieving UHC, which include improving efficiency in taxation, implementing
innovative financial techniques, appropriate allocations of government budgets towards
healthcare, and increasing development assistance for health (Friebel, Molloy, Leatherman,
Dixon, Bauhoff, & Chalkidou, 2018). Moreover, the Lancet commission recommended that
UHC is only achievable by raising revenues through taxation. The primary source of government
funds is tax revenues in many countries; consequently, LMICs taxes account for 65% of the total
government revenues. Therefore, the following paper seeks to exhibit the healthcare financing in
LMICs and achieving the UHC. Moreover, the paper will discuss health financing alternatives
using a comparative healthcare system analysis
Health Financing
The adoption and implementation of the UHC are dependent on the healthcare funding
techniques used by the government. One of the factors that have experienced significant
development is the mode of payment of healthcare services whereby most industrialized or
developed countries tend to use the health insurance rather than personal payment (Tulchinsky &
Varavikova, 2014). However, the LMICs still use the traditional mechanisms, such as the out-of-
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LMICs and UHC 4
pocket (direct) payment, which hinders service delivery to the people due to increased rates of
corruption. Notably, every country tends to depend on government financial support for either
the general population or the marginalized groups, such as the elderly (Tulchinsky &
Varavikova, 2014). Moreover, government support is essential for healthcare services that
private insurance plans are unable or avoid to provide, such as special groups (infants, pregnant
women, and chronic conditions).
Health financing incorporates not only the techniques of raising money for healthcare but
also the allocation of funds thus there are various rules applicable in allocation funds in
healthcare known as laws of health economics, which include Sutton, Capone, and Roemer law,
among others (Tulchinsky & Varavikova, 2014). Sutton’s law advocates that healthcare services
are available based on the amount of financing; for instance, if more funds are directed towards
treatment services than preventative care, then treatments will be given more emphasis than
prevention. Capone’s law advocates that allocation of funds is based on the interest of providers
rather than the general public. Finally, the ability for incentives to control both hospital bed
supply and utilization tends influences Roemer's law of allocation.
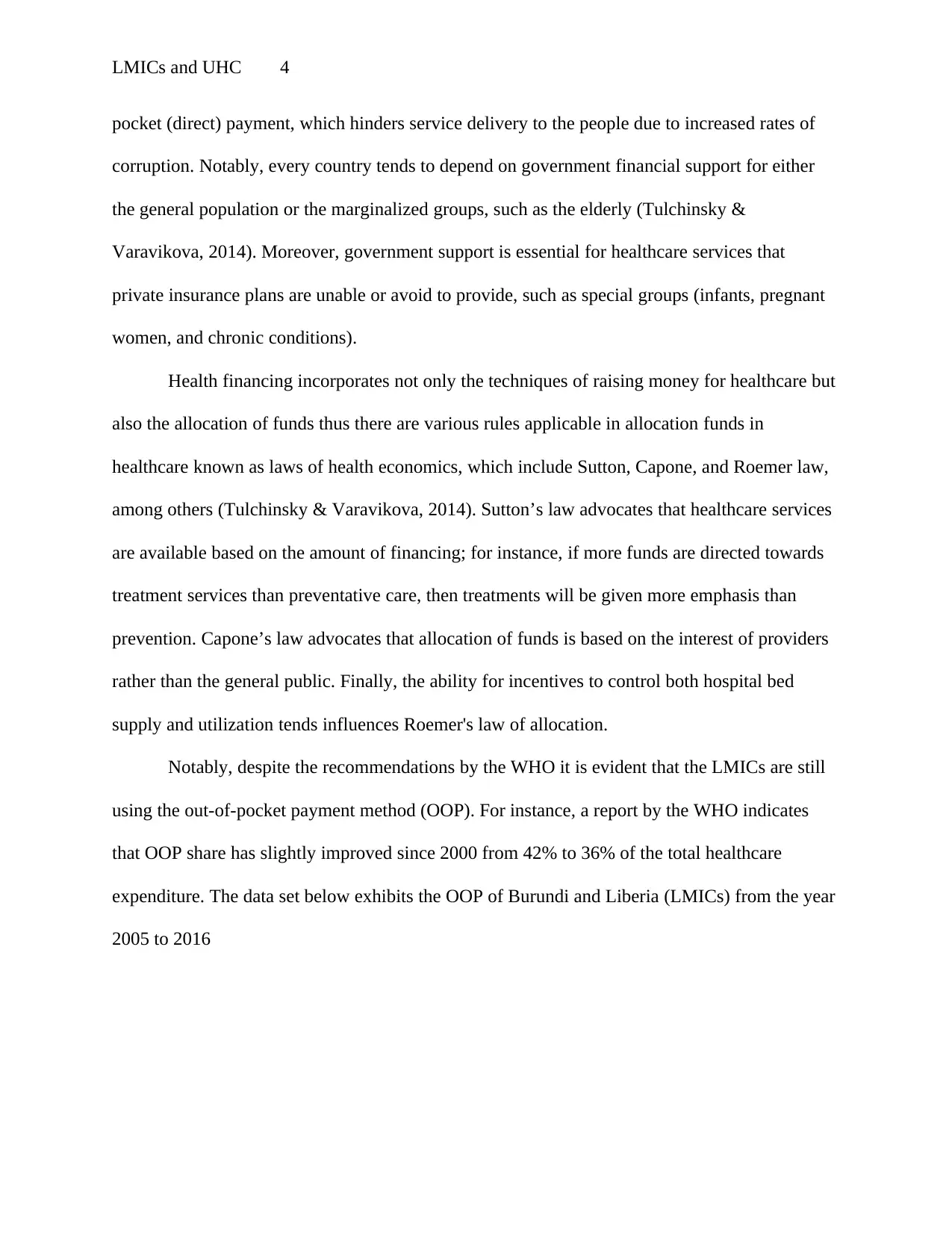
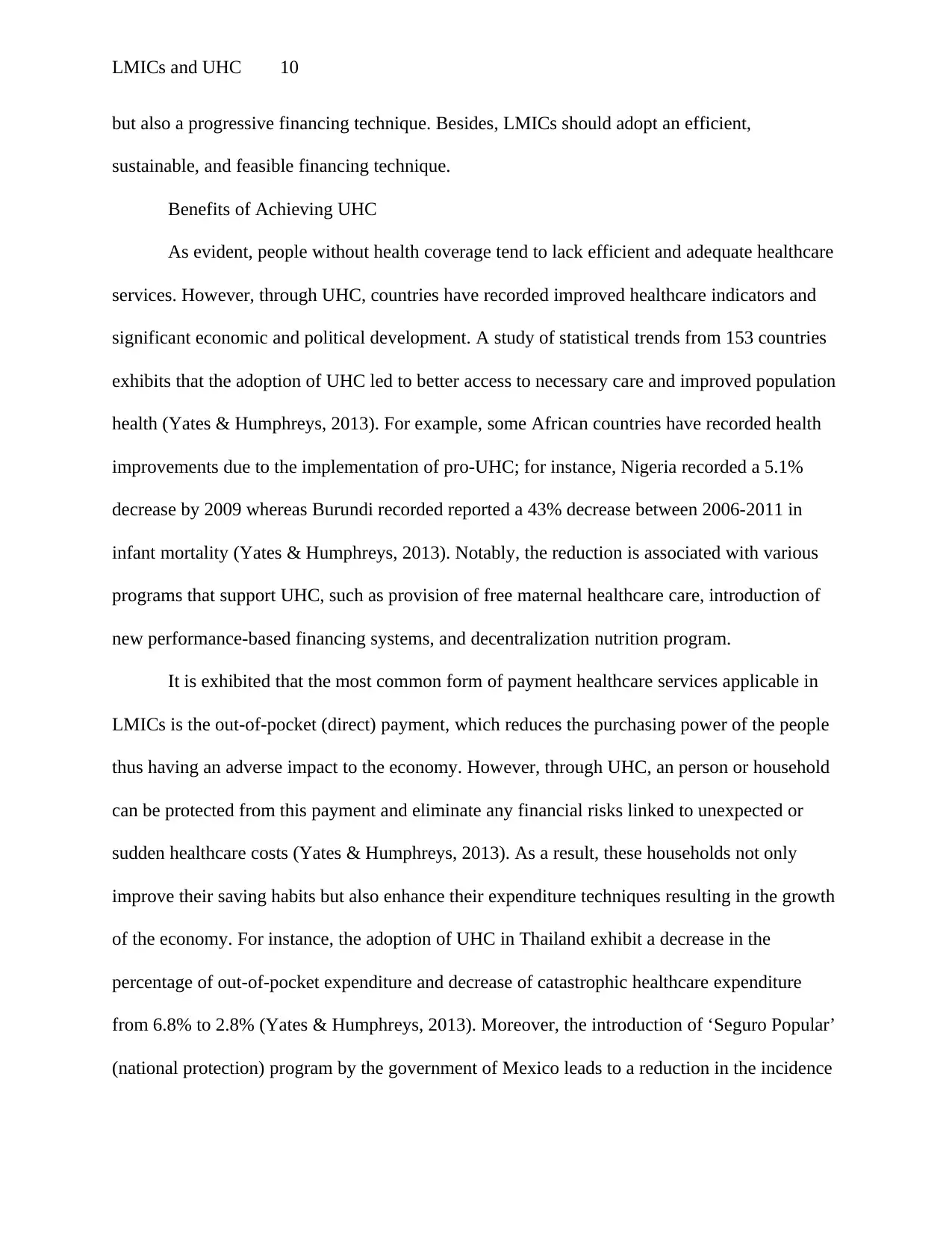
Notably, despite the recommendations by the WHO it is evident that the LMICs are still
using the out-of-pocket payment method (OOP). For instance, a report by the WHO indicates
that OOP share has slightly improved since 2000 from 42% to 36% of the total healthcare
expenditure. The data set below exhibits the OOP of Burundi and Liberia (LMICs) from the year
2005 to 2016
pocket (direct) payment, which hinders service delivery to the people due to increased rates of
corruption. Notably, every country tends to depend on government financial support for either
the general population or the marginalized groups, such as the elderly (Tulchinsky &
Varavikova, 2014). Moreover, government support is essential for healthcare services that
private insurance plans are unable or avoid to provide, such as special groups (infants, pregnant
women, and chronic conditions).
Health financing incorporates not only the techniques of raising money for healthcare but
also the allocation of funds thus there are various rules applicable in allocation funds in
healthcare known as laws of health economics, which include Sutton, Capone, and Roemer law,
among others (Tulchinsky & Varavikova, 2014). Sutton’s law advocates that healthcare services
are available based on the amount of financing; for instance, if more funds are directed towards
treatment services than preventative care, then treatments will be given more emphasis than
prevention. Capone’s law advocates that allocation of funds is based on the interest of providers
rather than the general public. Finally, the ability for incentives to control both hospital bed
supply and utilization tends influences Roemer's law of allocation.
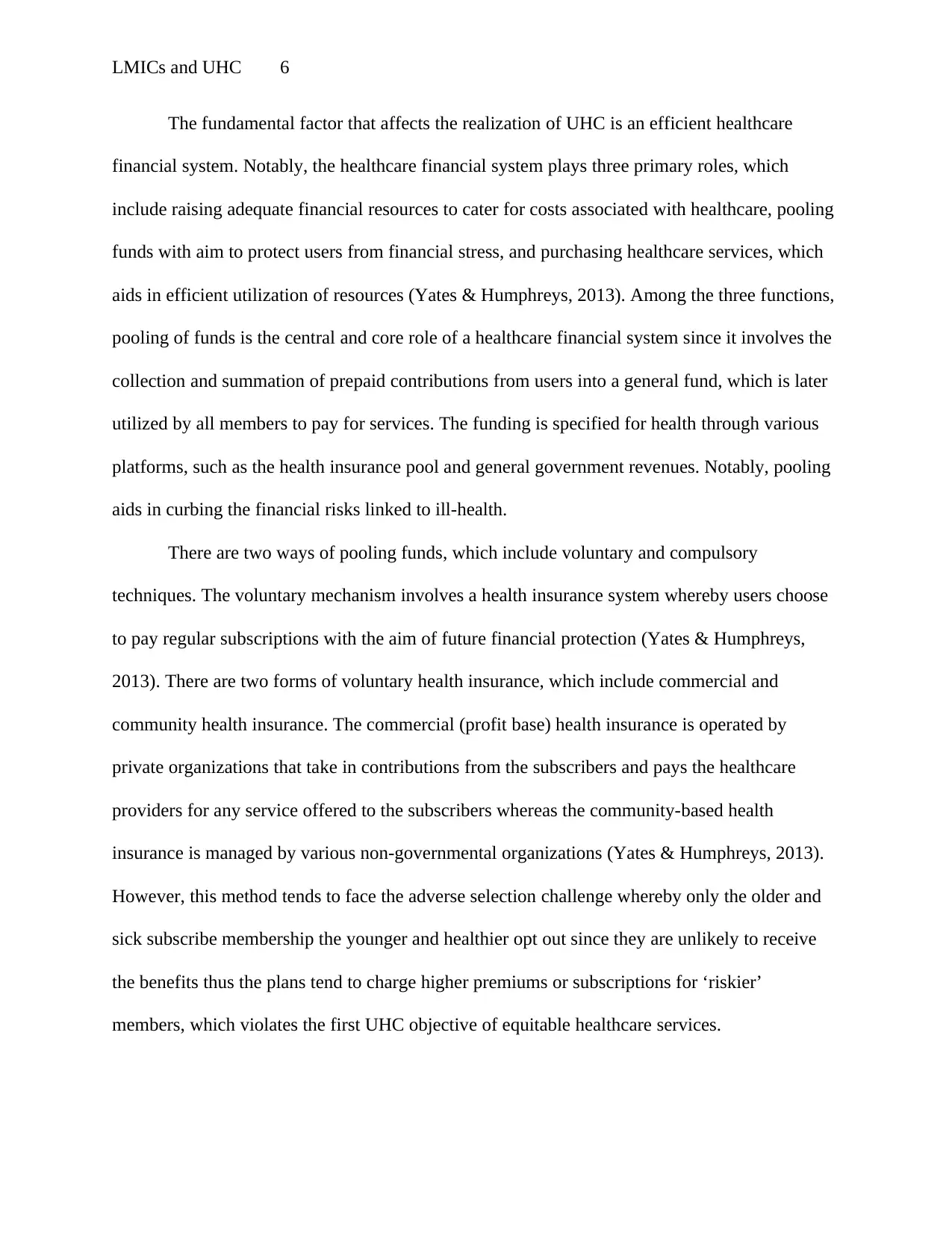
Notably, despite the recommendations by the WHO it is evident that the LMICs are still
using the out-of-pocket payment method (OOP). For instance, a report by the WHO indicates
that OOP share has slightly improved since 2000 from 42% to 36% of the total healthcare
expenditure. The data set below exhibits the OOP of Burundi and Liberia (LMICs) from the year
2005 to 2016
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LMICs and UHC 5
(WHO, Global
Health Expenditure Data, 2018)
The graph below exhibits an increase
in OOP in LMICs across the
12- year period.
Year 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016
0
50
100
150
200
250
Household out-of-pocket payment
Burundi Liberia
(WHO, Global Health Expenditure Data, 2018)
Health Financing Reforms that Accelerate Progress of UHC in LMICs
Year Burundi Liberia
200
5
33.09579 60.48296
200
6
44.07598 55.00419
200
7
51.23849 83.77617
200
8
53.52701 72.79213
200
9
58.12128 82.84348
201
0
64.62142 89.71262
201
1
57.35658 105.87
201
2
45.14991 104.6166
201
3
44.13011 119.0681
201
4
60.48588 143.8365
201
5
60.94413 151.512
201
6
59.28656 148.9604
(WHO, Global
Health Expenditure Data, 2018)
The graph below exhibits an increase
in OOP in LMICs across the
12- year period.
Year 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016
0
50
100
150
200
250
Household out-of-pocket payment
Burundi Liberia
(WHO, Global Health Expenditure Data, 2018)
Health Financing Reforms that Accelerate Progress of UHC in LMICs
Year Burundi Liberia
200
5
33.09579 60.48296
200
6
44.07598 55.00419
200
7
51.23849 83.77617
200
8
53.52701 72.79213
200
9
58.12128 82.84348
201
0
64.62142 89.71262
201
1
57.35658 105.87
201
2
45.14991 104.6166
201
3
44.13011 119.0681
201
4
60.48588 143.8365
201
5
60.94413 151.512
201
6
59.28656 148.9604
LMICs and UHC 6
The fundamental factor that affects the realization of UHC is an efficient healthcare
financial system. Notably, the healthcare financial system plays three primary roles, which
include raising adequate financial resources to cater for costs associated with healthcare, pooling
funds with aim to protect users from financial stress, and purchasing healthcare services, which
aids in efficient utilization of resources (Yates & Humphreys, 2013). Among the three functions,
pooling of funds is the central and core role of a healthcare financial system since it involves the
collection and summation of prepaid contributions from users into a general fund, which is later
utilized by all members to pay for services. The funding is specified for health through various
platforms, such as the health insurance pool and general government revenues. Notably, pooling
aids in curbing the financial risks linked to ill-health.
There are two ways of pooling funds, which include voluntary and compulsory
techniques. The voluntary mechanism involves a health insurance system whereby users choose
to pay regular subscriptions with the aim of future financial protection (Yates & Humphreys,
2013). There are two forms of voluntary health insurance, which include commercial and
community health insurance. The commercial (profit base) health insurance is operated by
private organizations that take in contributions from the subscribers and pays the healthcare
providers for any service offered to the subscribers whereas the community-based health
insurance is managed by various non-governmental organizations (Yates & Humphreys, 2013).
However, this method tends to face the adverse selection challenge whereby only the older and
sick subscribe membership the younger and healthier opt out since they are unlikely to receive
the benefits thus the plans tend to charge higher premiums or subscriptions for ‘riskier’
members, which violates the first UHC objective of equitable healthcare services.
The fundamental factor that affects the realization of UHC is an efficient healthcare
financial system. Notably, the healthcare financial system plays three primary roles, which
include raising adequate financial resources to cater for costs associated with healthcare, pooling
funds with aim to protect users from financial stress, and purchasing healthcare services, which
aids in efficient utilization of resources (Yates & Humphreys, 2013). Among the three functions,
pooling of funds is the central and core role of a healthcare financial system since it involves the
collection and summation of prepaid contributions from users into a general fund, which is later
utilized by all members to pay for services. The funding is specified for health through various
platforms, such as the health insurance pool and general government revenues. Notably, pooling
aids in curbing the financial risks linked to ill-health.
There are two ways of pooling funds, which include voluntary and compulsory
techniques. The voluntary mechanism involves a health insurance system whereby users choose
to pay regular subscriptions with the aim of future financial protection (Yates & Humphreys,
2013). There are two forms of voluntary health insurance, which include commercial and
community health insurance. The commercial (profit base) health insurance is operated by
private organizations that take in contributions from the subscribers and pays the healthcare
providers for any service offered to the subscribers whereas the community-based health
insurance is managed by various non-governmental organizations (Yates & Humphreys, 2013).
However, this method tends to face the adverse selection challenge whereby only the older and
sick subscribe membership the younger and healthier opt out since they are unlikely to receive
the benefits thus the plans tend to charge higher premiums or subscriptions for ‘riskier’
members, which violates the first UHC objective of equitable healthcare services.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LMICs and UHC 7
On the other hand, the compulsory technique depends on mandatory subscriptions to
provide an equitable healthcare financing system and only operated by the government. There
are two ways applicable in this technique, which include general taxation and charges and
mandatory contributions to health insurance (Yates & Humphreys, 2013). General taxation
involves sourcing of funds from all government taxes and fees, such as direct taxes and indirect
taxes (import duties). The mandatory contributions, also known as social health insurance, are
derived from compulsory deductions from employees’ wages and remunerations. Notably, the
deductions are proportional to the wages of the employee, thus making the scheme more
equitable compared to the voluntary method.
Alternative Financing Methods
Notably, there are various proposed alternative financing methods that the LMICs can
use to fund UHC. The WHO recommends two alternative methods, which include user fees and
innovative financing methods (WHO, Alternative financing methods, 2019). User fees technique
is one of the conventional adopted financing methods by many countries, which involves direct
charges to users for healthcare services. Moreover, the mechanism is widely implemented
because the contributions aid in guiding demand to cost-effective healthcare at adequate levels;
besides, the techniques improves equity if revenues generated from fees are channeled towards
healthcare needs of the poor thus supporting the UHC (WHO, Alternative financing methods,
2019). However, opposers of the technique argue that the allocation is not guaranteed, hence it
needs exemption policies or other forms of regulations of financial protection otherwise user fees
will exclude the poor from the market for healthcare.
In addition to user fees, other financing mechanisms are being experimented by various
countries across the globe, which are known as innovative financing methods. Notably, the
On the other hand, the compulsory technique depends on mandatory subscriptions to
provide an equitable healthcare financing system and only operated by the government. There
are two ways applicable in this technique, which include general taxation and charges and
mandatory contributions to health insurance (Yates & Humphreys, 2013). General taxation
involves sourcing of funds from all government taxes and fees, such as direct taxes and indirect
taxes (import duties). The mandatory contributions, also known as social health insurance, are
derived from compulsory deductions from employees’ wages and remunerations. Notably, the
deductions are proportional to the wages of the employee, thus making the scheme more
equitable compared to the voluntary method.
Alternative Financing Methods
Notably, there are various proposed alternative financing methods that the LMICs can
use to fund UHC. The WHO recommends two alternative methods, which include user fees and
innovative financing methods (WHO, Alternative financing methods, 2019). User fees technique
is one of the conventional adopted financing methods by many countries, which involves direct
charges to users for healthcare services. Moreover, the mechanism is widely implemented
because the contributions aid in guiding demand to cost-effective healthcare at adequate levels;
besides, the techniques improves equity if revenues generated from fees are channeled towards
healthcare needs of the poor thus supporting the UHC (WHO, Alternative financing methods,
2019). However, opposers of the technique argue that the allocation is not guaranteed, hence it
needs exemption policies or other forms of regulations of financial protection otherwise user fees
will exclude the poor from the market for healthcare.
In addition to user fees, other financing mechanisms are being experimented by various
countries across the globe, which are known as innovative financing methods. Notably, the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LMICs and UHC 8
innovative financing techniques are driven by multiple factors, such as rising demand for
healthcare services, rapid technological advancements, the increased cost of care, and limits of
the traditional tax base (WHO, Alternative financing methods, 2019). There are two types of
innovative financing methods, which include national and international bases. Some of the
national base methods include state and national lotteries dedicated to healthcare, private-public
partnerships between the state and private sector to co-fund healthcare, and hypothetical taxes,
such as the ‘sin taxes’ for alcohol and tobacco. On the other hand, international based
mechanisms include the International Finance Facility (IFF), which front-load development
assistance through selling government bonds secure by future aids flows. Other methods include
debt for health swaps whereby both the government and private financial institutions are
involved in the conversion of the debt, and capital markets to develop new healthcare products.
Assessment of Financing Mechanisms
Notably, the adoption and implementation of any financing mechanism require adequate
and efficient evaluation. There are four factors used in the evaluation of financing mechanisms,
which include feasibility, equity, efficiency, and sustainability (McIntyre, 2007). Feasibility aids
in assessing if the implementation will be successful by incorporating various factors, such as
stakeholders’ support to the technique, and adequate administrative capacities, such as
information system and actuarial expertise. On the other hand, the sustainability of a financing
technique exhibits the long-term stability and potential for generating revenue (McIntyre, 2007).
Notably, in case the revenue generated by the method shows frequent cycles and fluctuations,
then the technique is regarded as unreliable thus, it is discarded and replaced with a mechanism
that generates more predictable revenue. Generally, sustainability seeks to exhibit if the system
innovative financing techniques are driven by multiple factors, such as rising demand for
healthcare services, rapid technological advancements, the increased cost of care, and limits of
the traditional tax base (WHO, Alternative financing methods, 2019). There are two types of
innovative financing methods, which include national and international bases. Some of the
national base methods include state and national lotteries dedicated to healthcare, private-public
partnerships between the state and private sector to co-fund healthcare, and hypothetical taxes,
such as the ‘sin taxes’ for alcohol and tobacco. On the other hand, international based
mechanisms include the International Finance Facility (IFF), which front-load development
assistance through selling government bonds secure by future aids flows. Other methods include
debt for health swaps whereby both the government and private financial institutions are
involved in the conversion of the debt, and capital markets to develop new healthcare products.
Assessment of Financing Mechanisms
Notably, the adoption and implementation of any financing mechanism require adequate
and efficient evaluation. There are four factors used in the evaluation of financing mechanisms,
which include feasibility, equity, efficiency, and sustainability (McIntyre, 2007). Feasibility aids
in assessing if the implementation will be successful by incorporating various factors, such as
stakeholders’ support to the technique, and adequate administrative capacities, such as
information system and actuarial expertise. On the other hand, the sustainability of a financing
technique exhibits the long-term stability and potential for generating revenue (McIntyre, 2007).
Notably, in case the revenue generated by the method shows frequent cycles and fluctuations,
then the technique is regarded as unreliable thus, it is discarded and replaced with a mechanism
that generates more predictable revenue. Generally, sustainability seeks to exhibit if the system
LMICs and UHC 9
can maintain or expand the current level of funding in the long-term and adapt to the changing
healthcare needs.
The efficiency of a financing technique is the ability of the mechanism to generate a
relatively large amount of funding, which consolidates multiple funding techniques that generate
a limited amount of funds (McIntyre, 2007). Moreover, an efficient financing mechanism seeks
to lower both the cost of fund collection and administration, thus allocating more funds to the
provision of healthcare services. Notably, there are two forms of financial efficiency, which
include allocative and technical efficiency (McIntyre, 2007). Allocative efficiency is the
allocation of resources to various level of care whereby funds are channeled towards services
dealing with the essential ill-health in the society, thus giving priority to the cost-effective
interventions. On the other hand, technical allocative is the provision of resources to all
healthcare services while minimizing the cost of each without tampering with the quality of care.
Equity assesses if users can contribute to healthcare funding and benefit from the
services according to their need for care. Moreover, equity ensures that none of the households is
impoverished by its demand for medical services or any unplanned healthcare costs. Notably,
equity discourages the regressive financing mechanism whereby all users contribute a similar
amount towards health care funding rather advocates for a progressive mechanism whereby the
all users contribute money proportional to their level of income (McIntyre, 2007). As a result, the
high-income earners in the society tend to contribute a larger proportion of their income (wages
and renumerations) than the low-income earners. Moreover, progressive funding mechanism is
considered as a pivot in the redistribution of resources in the country (McIntyre, 2007).
Generally, an equitable financing system incorporates cross-subsidies from both the rich to poor
and healthy to ill. Therefore, to achieve the UHC, the LMICs should adopt not only an equitable
can maintain or expand the current level of funding in the long-term and adapt to the changing
healthcare needs.
The efficiency of a financing technique is the ability of the mechanism to generate a
relatively large amount of funding, which consolidates multiple funding techniques that generate
a limited amount of funds (McIntyre, 2007). Moreover, an efficient financing mechanism seeks
to lower both the cost of fund collection and administration, thus allocating more funds to the
provision of healthcare services. Notably, there are two forms of financial efficiency, which
include allocative and technical efficiency (McIntyre, 2007). Allocative efficiency is the
allocation of resources to various level of care whereby funds are channeled towards services
dealing with the essential ill-health in the society, thus giving priority to the cost-effective
interventions. On the other hand, technical allocative is the provision of resources to all
healthcare services while minimizing the cost of each without tampering with the quality of care.
Equity assesses if users can contribute to healthcare funding and benefit from the
services according to their need for care. Moreover, equity ensures that none of the households is
impoverished by its demand for medical services or any unplanned healthcare costs. Notably,
equity discourages the regressive financing mechanism whereby all users contribute a similar
amount towards health care funding rather advocates for a progressive mechanism whereby the
all users contribute money proportional to their level of income (McIntyre, 2007). As a result, the
high-income earners in the society tend to contribute a larger proportion of their income (wages
and renumerations) than the low-income earners. Moreover, progressive funding mechanism is
considered as a pivot in the redistribution of resources in the country (McIntyre, 2007).
Generally, an equitable financing system incorporates cross-subsidies from both the rich to poor
and healthy to ill. Therefore, to achieve the UHC, the LMICs should adopt not only an equitable
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LMICs and UHC 10
but also a progressive financing technique. Besides, LMICs should adopt an efficient,
sustainable, and feasible financing technique.
Benefits of Achieving UHC
As evident, people without health coverage tend to lack efficient and adequate healthcare
services. However, through UHC, countries have recorded improved healthcare indicators and
significant economic and political development. A study of statistical trends from 153 countries
exhibits that the adoption of UHC led to better access to necessary care and improved population
health (Yates & Humphreys, 2013). For example, some African countries have recorded health
improvements due to the implementation of pro-UHC; for instance, Nigeria recorded a 5.1%
decrease by 2009 whereas Burundi recorded reported a 43% decrease between 2006-2011 in
infant mortality (Yates & Humphreys, 2013). Notably, the reduction is associated with various
programs that support UHC, such as provision of free maternal healthcare care, introduction of
new performance-based financing systems, and decentralization nutrition program.
It is exhibited that the most common form of payment healthcare services applicable in
LMICs is the out-of-pocket (direct) payment, which reduces the purchasing power of the people
thus having an adverse impact to the economy. However, through UHC, an person or household
can be protected from this payment and eliminate any financial risks linked to unexpected or
sudden healthcare costs (Yates & Humphreys, 2013). As a result, these households not only
improve their saving habits but also enhance their expenditure techniques resulting in the growth
of the economy. For instance, the adoption of UHC in Thailand exhibit a decrease in the
percentage of out-of-pocket expenditure and decrease of catastrophic healthcare expenditure
from 6.8% to 2.8% (Yates & Humphreys, 2013). Moreover, the introduction of ‘Seguro Popular’
(national protection) program by the government of Mexico leads to a reduction in the incidence
but also a progressive financing technique. Besides, LMICs should adopt an efficient,
sustainable, and feasible financing technique.
Benefits of Achieving UHC
As evident, people without health coverage tend to lack efficient and adequate healthcare
services. However, through UHC, countries have recorded improved healthcare indicators and
significant economic and political development. A study of statistical trends from 153 countries
exhibits that the adoption of UHC led to better access to necessary care and improved population
health (Yates & Humphreys, 2013). For example, some African countries have recorded health
improvements due to the implementation of pro-UHC; for instance, Nigeria recorded a 5.1%
decrease by 2009 whereas Burundi recorded reported a 43% decrease between 2006-2011 in
infant mortality (Yates & Humphreys, 2013). Notably, the reduction is associated with various
programs that support UHC, such as provision of free maternal healthcare care, introduction of
new performance-based financing systems, and decentralization nutrition program.
It is exhibited that the most common form of payment healthcare services applicable in
LMICs is the out-of-pocket (direct) payment, which reduces the purchasing power of the people
thus having an adverse impact to the economy. However, through UHC, an person or household
can be protected from this payment and eliminate any financial risks linked to unexpected or
sudden healthcare costs (Yates & Humphreys, 2013). As a result, these households not only
improve their saving habits but also enhance their expenditure techniques resulting in the growth
of the economy. For instance, the adoption of UHC in Thailand exhibit a decrease in the
percentage of out-of-pocket expenditure and decrease of catastrophic healthcare expenditure
from 6.8% to 2.8% (Yates & Humphreys, 2013). Moreover, the introduction of ‘Seguro Popular’
(national protection) program by the government of Mexico leads to a reduction in the incidence
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LMICs and UHC 11
of catastrophic expenditure from 3.1% to 2% and a decrease in impoverishment because of
health expenditure from 3.3% to 0.8% between 2000 and 2010.
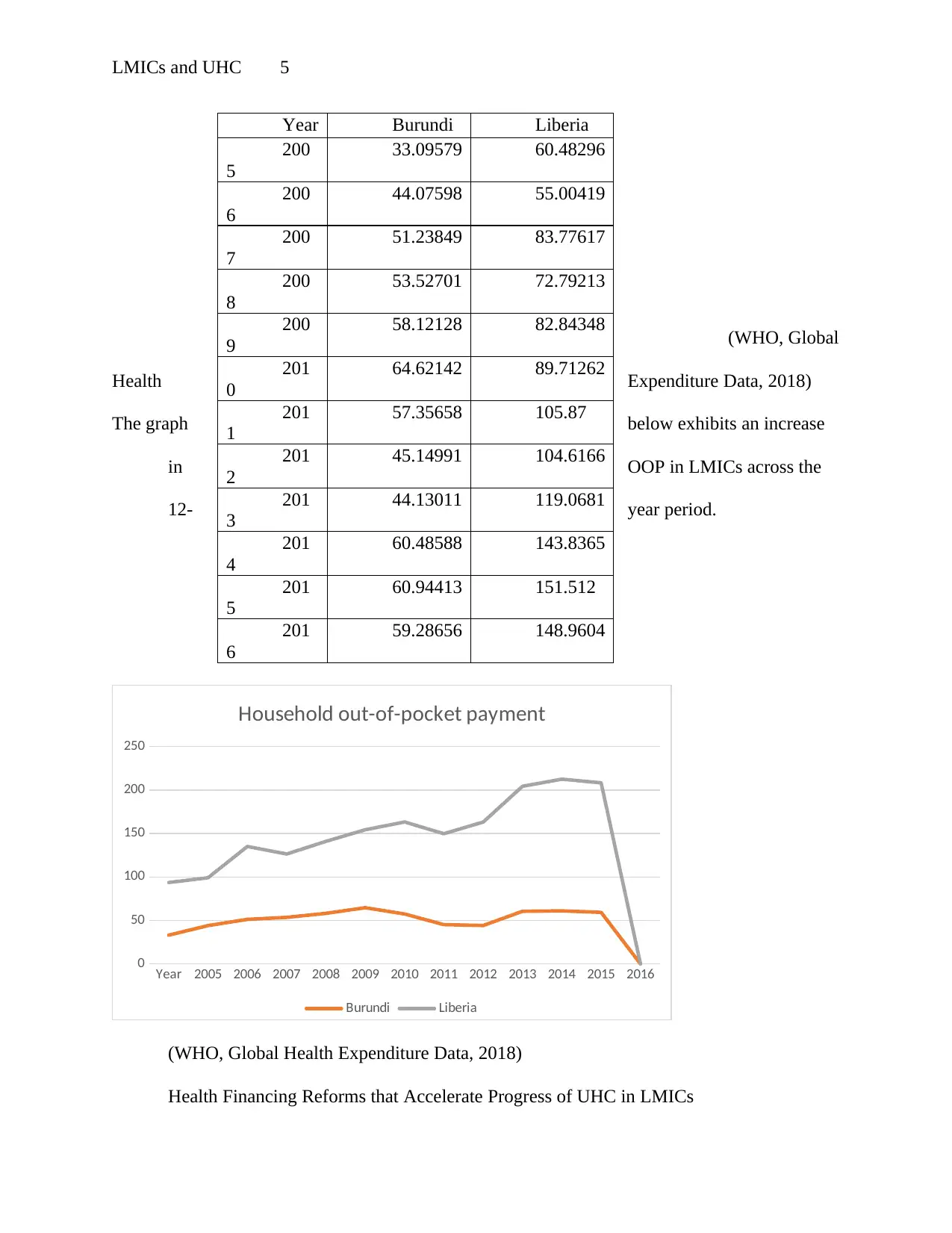
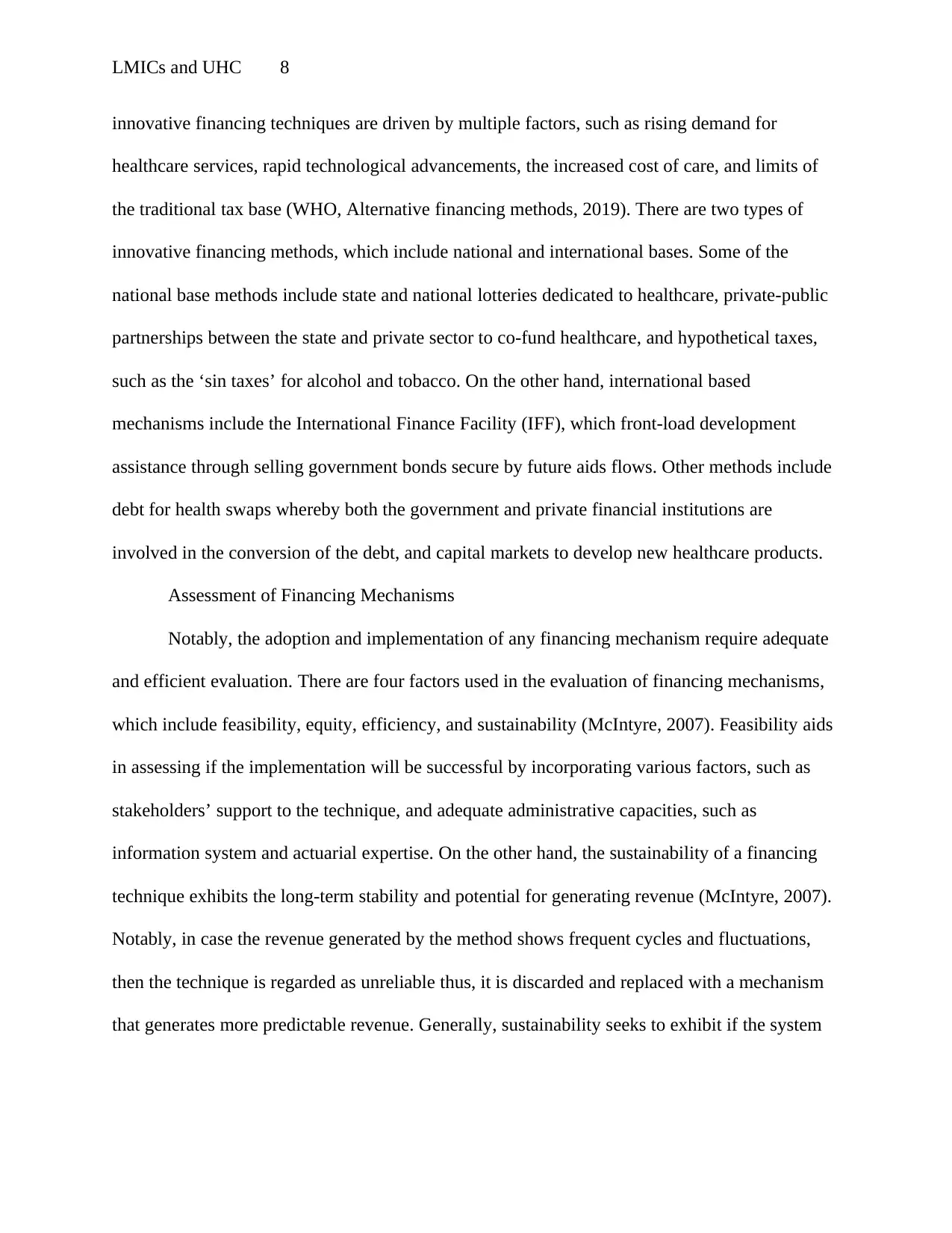
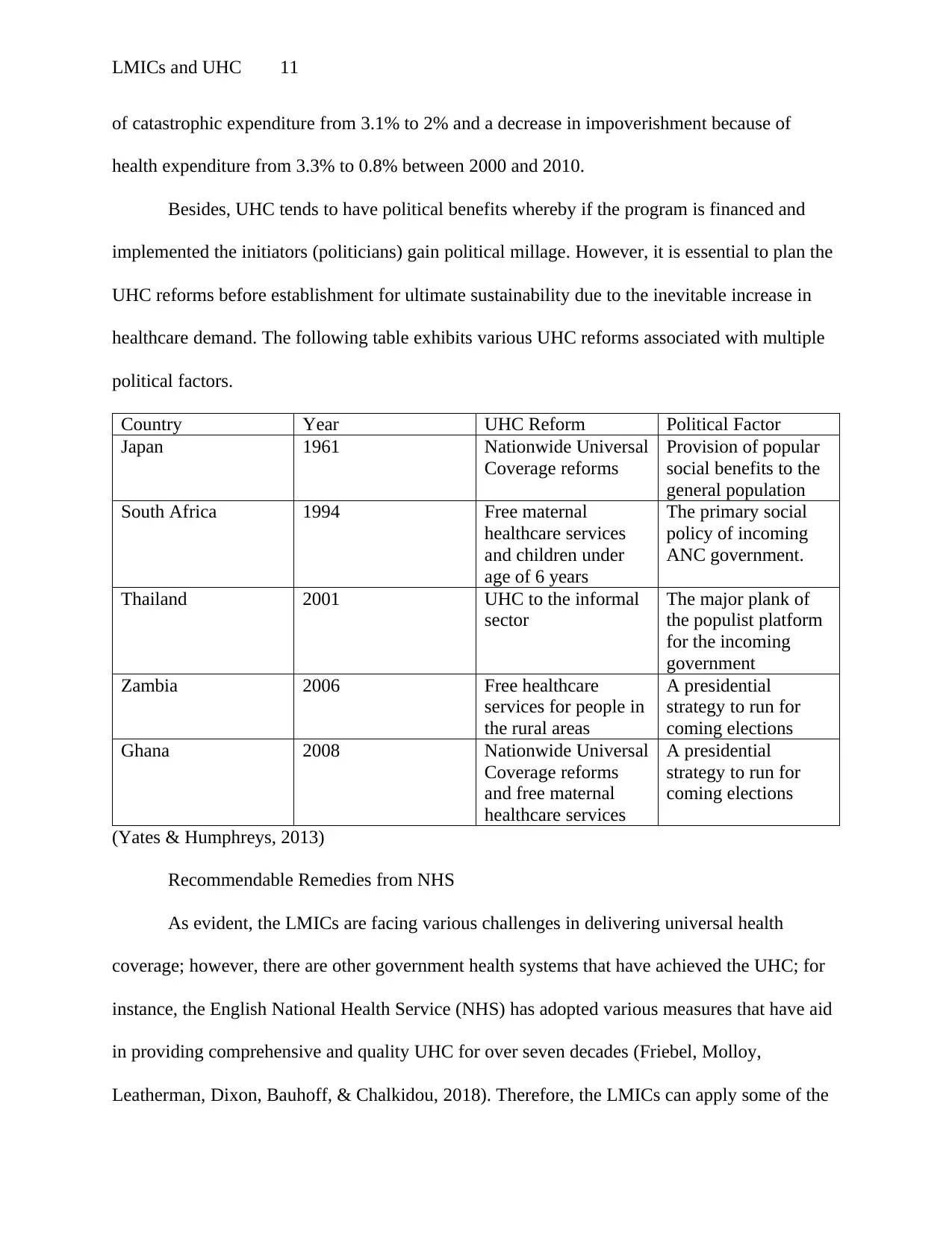
Besides, UHC tends to have political benefits whereby if the program is financed and
implemented the initiators (politicians) gain political millage. However, it is essential to plan the
UHC reforms before establishment for ultimate sustainability due to the inevitable increase in
healthcare demand. The following table exhibits various UHC reforms associated with multiple
political factors.
Country Year UHC Reform Political Factor
Japan 1961 Nationwide Universal
Coverage reforms
Provision of popular
social benefits to the
general population
South Africa 1994 Free maternal
healthcare services
and children under
age of 6 years
The primary social
policy of incoming
ANC government.
Thailand 2001 UHC to the informal
sector
The major plank of
the populist platform
for the incoming
government
Zambia 2006 Free healthcare
services for people in
the rural areas
A presidential
strategy to run for
coming elections
Ghana 2008 Nationwide Universal
Coverage reforms
and free maternal
healthcare services
A presidential
strategy to run for
coming elections
(Yates & Humphreys, 2013)
Recommendable Remedies from NHS
As evident, the LMICs are facing various challenges in delivering universal health
coverage; however, there are other government health systems that have achieved the UHC; for
instance, the English National Health Service (NHS) has adopted various measures that have aid
in providing comprehensive and quality UHC for over seven decades (Friebel, Molloy,
Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). Therefore, the LMICs can apply some of the
of catastrophic expenditure from 3.1% to 2% and a decrease in impoverishment because of
health expenditure from 3.3% to 0.8% between 2000 and 2010.
Besides, UHC tends to have political benefits whereby if the program is financed and
implemented the initiators (politicians) gain political millage. However, it is essential to plan the
UHC reforms before establishment for ultimate sustainability due to the inevitable increase in
healthcare demand. The following table exhibits various UHC reforms associated with multiple
political factors.
Country Year UHC Reform Political Factor
Japan 1961 Nationwide Universal
Coverage reforms
Provision of popular
social benefits to the
general population
South Africa 1994 Free maternal
healthcare services
and children under
age of 6 years
The primary social
policy of incoming
ANC government.
Thailand 2001 UHC to the informal
sector
The major plank of
the populist platform
for the incoming
government
Zambia 2006 Free healthcare
services for people in
the rural areas
A presidential
strategy to run for
coming elections
Ghana 2008 Nationwide Universal
Coverage reforms
and free maternal
healthcare services
A presidential
strategy to run for
coming elections
(Yates & Humphreys, 2013)
Recommendable Remedies from NHS
As evident, the LMICs are facing various challenges in delivering universal health
coverage; however, there are other government health systems that have achieved the UHC; for
instance, the English National Health Service (NHS) has adopted various measures that have aid
in providing comprehensive and quality UHC for over seven decades (Friebel, Molloy,
Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). Therefore, the LMICs can apply some of the
LMICs and UHC 12
measures, which include prevention, priority setting, target setting and monitoring for enhanced
performance, providing integrated and coordinated care, investing in people, and regulation of
quality. For example, the NHS has implemented various measures to aid in primary disease
prevention, such as raising the minimum age for purchase and consumption of tobacco and
alcohol products and imposing the minimum unit pricing for alcohol (Friebel, Molloy,
Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). As a result, smoking-related diseases have
reduced, thus reducing the expenditure related to these diseases and increases finance allocation
in providing other health services.
Moreover, the NHS has adopted the priority setting measure whereby the government
uses evidence-based guidance and recommendations to the adoption of cost-effective care in
various sectors, such as medicine, treatment of specific conditions, and safe staffing levels for
providers (Friebel, Molloy, Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). Besides, NHS
collects large data sets that aids in monitoring the quality of care and performance of providers;
for instance, by introducing the national performance targets in conjunction with providers has
resulted in a reduction in healthcare-associated infections. The NHS has adopted a Care Quality
Commission (CQC) for both medical professionals and providers that monitors, regulates, and
inspects the health and social services provided. Furthermore, to ensure the health care systems
are equipped with adequate and efficient skills, the NHS has adopted advanced medical training
and technologies (Friebel, Molloy, Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). As
evident, the above measures have aid in achieving UHC in other countries; thus, the LMICs
should adopt and implement the measures.
measures, which include prevention, priority setting, target setting and monitoring for enhanced
performance, providing integrated and coordinated care, investing in people, and regulation of
quality. For example, the NHS has implemented various measures to aid in primary disease
prevention, such as raising the minimum age for purchase and consumption of tobacco and
alcohol products and imposing the minimum unit pricing for alcohol (Friebel, Molloy,
Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). As a result, smoking-related diseases have
reduced, thus reducing the expenditure related to these diseases and increases finance allocation
in providing other health services.
Moreover, the NHS has adopted the priority setting measure whereby the government
uses evidence-based guidance and recommendations to the adoption of cost-effective care in
various sectors, such as medicine, treatment of specific conditions, and safe staffing levels for
providers (Friebel, Molloy, Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). Besides, NHS
collects large data sets that aids in monitoring the quality of care and performance of providers;
for instance, by introducing the national performance targets in conjunction with providers has
resulted in a reduction in healthcare-associated infections. The NHS has adopted a Care Quality
Commission (CQC) for both medical professionals and providers that monitors, regulates, and
inspects the health and social services provided. Furthermore, to ensure the health care systems
are equipped with adequate and efficient skills, the NHS has adopted advanced medical training
and technologies (Friebel, Molloy, Leatherman, Dixon, Bauhoff, & Chalkidou, 2018). As
evident, the above measures have aid in achieving UHC in other countries; thus, the LMICs
should adopt and implement the measures.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





