Systematic Review: Enhancing Medication Adherence in Heart Failure
VerifiedAdded on 2023/06/13
|9
|7032
|229
Literature Review
AI Summary
This systematic review examines interventions designed to improve medication adherence in patients with heart failure (CHF). The review included randomized controlled trials that assessed the impact of various strategies on medication adherence, measured through methods such as pill counts, electronic monitoring, and self-reported data. The study selection process involved searching databases like MEDLINE, CINAHL, Embase, and PsychInfo, resulting in the identification of 16 independent studies with a total of 3305 patients. Interventions ranged from simplifying medication regimens and patient education to healthcare provider monitoring and motivational techniques. The review assesses the risk of bias in included studies, focusing on selection, performance, attrition, and detection biases. While data pooling was not possible due to heterogeneity, the review provides a comprehensive analysis of the effectiveness of different adherence-enhancing interventions in CHF.
Advances in Heart Failure
Interventions to Enhance Adherence to Medications in
Patients With Heart Failure
A Systematic Review
Gerard J. Molloy, BSc, PhD; Ronan E. O’Carroll, BSc, PhD;
Miles D. Witham, BM, BCh, PhD, MRCP; Marion E.T. McMurdo, BM, BCh, FRCP, CBiol, FIBiol
Prognosis remains poor for patients with chronic heart
failure (CHF), despite improvements in the prevention
and treatment of heart failure over the last 25 years. Recent
estimates indicate that the median survival after a first
episode of heart failure is 2.3 years for men and 1.8 years for
women. 1 It is suggested that the improvements in outcomes
that have been achieved can be partly explained by increases
in prescribing rates of medications such as angiotensin-
converting enzyme inhibitors, 2 -blockers, 3 and spironolac-
tone 4 over this period. 1 Although the evidence on medication
efficacy for certain subgroups of patients with CHF is clear,
there are also compelling data showing that many of these
patients do not take their medications as prescribed by health
care providers. 5,6 This “nonadherence” to medication there-
fore remains a significant barrier to enhancing the effective-
ness of existing treatments.
Estimates for nonadherence to medications in CHF have
varied widely.5 One of the largest studies found that only 80%
of patients with a prescription for angiotensin-converting
enzyme inhibitors at hospital discharge completed the pre-
scription form 30 days after discharge, and this rate subse-
quently fell to 60% over 1 year. 7 Full adherence, defined as
filing enough prescriptions to have daily medication available
for 1 year, may be as low as 10% in CHF. 8 Poor adherence to
medication in CHF is associated with worse outcomes in
observational studies, including shorter event-free survival. 9
Therefore, strategies to enhance adherence provide a poten-
tially valuable strategy for improving survival, reducing
hospitalization and managing patient symptoms in CHF.
In this report, we provide an up-to-date review and analysis
of those studies that have developed and evaluated medica-
tion adherence interventions in CHF. Because CHF is typi-
cally symptomatic and includes medication with actions that
are discernible to the patient within hours of ingestion, for
example, diuretics and consequent diuresis, an examination
of interventions for this population in isolation from cardio-
vascular disease populations more generally is warranted
because some CVD patient populations can have asymptom-
atic conditions, for example, hypertension or hyperlipidemia
and medication regimens with little or no side effects. 10
Previous reviews 11 may have also set inclusion criteria that
may be too stringent for CHF populations, in which high
morbidity and mortality rates can make attrition rates for
medication adherence outcome measures appear abnormally
high over 1 year even in high-quality studies, for example,
⬎80% participant follow-up and ⬎6 month follow-up inclu-
sion criteria. 11 Therefore, potentially useful studies may have
been overlooked in previous reviews. The objective of this
systematic review was to identify and summarize the effec-
tiveness of intervention strategies to enhance adherence to
medications in heart failure populations.
Study Selection
The following inclusion criteria were used to identify appro-
priate published studies for the review:
(1) The study design was a randomized, controlled trial in
which an intervention group was compared with treat-
ment as usual or a clearly justified comparison group.
(2) The population of interest comprised adults (⬎18
years old) with a diagnosis of heart failure confirmed
by a physician.
(3) The intervention strategy clearly had a primary or
secondary aim to increase adherence to medication
prescribed for heart failure.
(4) Self-administered medication, that is, medication not
administered by a health care professional, was mea-
sured as an outcome by any of the following methods:
pill count, electronic monitoring, refill or prescription
records, and self-reported data.
A trial was included if it met all our inclusion criteria.
Reference Manager (version 11) software was used to iden-
tify and extract duplicate studies.
Literature Search
We performed a systematic review, using guidelines devel-
oped by the Cochrane Collaboration. The databases of the
Received August 24, 2011; accepted November 17, 2011.
From the Division of Psychology (G.J.M., R.E.O.), School of Natural Sciences, University of Stirling, Stirling, Scotland; and Ninewells Hospital and
Medical School (M.D.W., M.E.T.M.), Section of Ageing and Health, University of Dundee, Dundee, Scotland.
Correspondence to Gerard J. Molloy, BSc, PhD, Division of Psychology, School of Natural Sciences, Cottrell Bldg, University of Stirling, FK9 4LA,
Scotland. E-mail g.j.molloy@stir.ac.uk
(Circ Heart Fail. 2012;5:126-133.)
© 2012 American Heart Association, Inc.
Circ Heart Fail is available at http://circheartfailure.ahajournals.org DOI: 10.1161/CIRCHEARTFAILURE.111.964569
126
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Interventions to Enhance Adherence to Medications in
Patients With Heart Failure
A Systematic Review
Gerard J. Molloy, BSc, PhD; Ronan E. O’Carroll, BSc, PhD;
Miles D. Witham, BM, BCh, PhD, MRCP; Marion E.T. McMurdo, BM, BCh, FRCP, CBiol, FIBiol
Prognosis remains poor for patients with chronic heart
failure (CHF), despite improvements in the prevention
and treatment of heart failure over the last 25 years. Recent
estimates indicate that the median survival after a first
episode of heart failure is 2.3 years for men and 1.8 years for
women. 1 It is suggested that the improvements in outcomes
that have been achieved can be partly explained by increases
in prescribing rates of medications such as angiotensin-
converting enzyme inhibitors, 2 -blockers, 3 and spironolac-
tone 4 over this period. 1 Although the evidence on medication
efficacy for certain subgroups of patients with CHF is clear,
there are also compelling data showing that many of these
patients do not take their medications as prescribed by health
care providers. 5,6 This “nonadherence” to medication there-
fore remains a significant barrier to enhancing the effective-
ness of existing treatments.
Estimates for nonadherence to medications in CHF have
varied widely.5 One of the largest studies found that only 80%
of patients with a prescription for angiotensin-converting
enzyme inhibitors at hospital discharge completed the pre-
scription form 30 days after discharge, and this rate subse-
quently fell to 60% over 1 year. 7 Full adherence, defined as
filing enough prescriptions to have daily medication available
for 1 year, may be as low as 10% in CHF. 8 Poor adherence to
medication in CHF is associated with worse outcomes in
observational studies, including shorter event-free survival. 9
Therefore, strategies to enhance adherence provide a poten-
tially valuable strategy for improving survival, reducing
hospitalization and managing patient symptoms in CHF.
In this report, we provide an up-to-date review and analysis
of those studies that have developed and evaluated medica-
tion adherence interventions in CHF. Because CHF is typi-
cally symptomatic and includes medication with actions that
are discernible to the patient within hours of ingestion, for
example, diuretics and consequent diuresis, an examination
of interventions for this population in isolation from cardio-
vascular disease populations more generally is warranted
because some CVD patient populations can have asymptom-
atic conditions, for example, hypertension or hyperlipidemia
and medication regimens with little or no side effects. 10
Previous reviews 11 may have also set inclusion criteria that
may be too stringent for CHF populations, in which high
morbidity and mortality rates can make attrition rates for
medication adherence outcome measures appear abnormally
high over 1 year even in high-quality studies, for example,
⬎80% participant follow-up and ⬎6 month follow-up inclu-
sion criteria. 11 Therefore, potentially useful studies may have
been overlooked in previous reviews. The objective of this
systematic review was to identify and summarize the effec-
tiveness of intervention strategies to enhance adherence to
medications in heart failure populations.
Study Selection
The following inclusion criteria were used to identify appro-
priate published studies for the review:
(1) The study design was a randomized, controlled trial in
which an intervention group was compared with treat-
ment as usual or a clearly justified comparison group.
(2) The population of interest comprised adults (⬎18
years old) with a diagnosis of heart failure confirmed
by a physician.
(3) The intervention strategy clearly had a primary or
secondary aim to increase adherence to medication
prescribed for heart failure.
(4) Self-administered medication, that is, medication not
administered by a health care professional, was mea-
sured as an outcome by any of the following methods:
pill count, electronic monitoring, refill or prescription
records, and self-reported data.
A trial was included if it met all our inclusion criteria.
Reference Manager (version 11) software was used to iden-
tify and extract duplicate studies.
Literature Search
We performed a systematic review, using guidelines devel-
oped by the Cochrane Collaboration. The databases of the
Received August 24, 2011; accepted November 17, 2011.
From the Division of Psychology (G.J.M., R.E.O.), School of Natural Sciences, University of Stirling, Stirling, Scotland; and Ninewells Hospital and
Medical School (M.D.W., M.E.T.M.), Section of Ageing and Health, University of Dundee, Dundee, Scotland.
Correspondence to Gerard J. Molloy, BSc, PhD, Division of Psychology, School of Natural Sciences, Cottrell Bldg, University of Stirling, FK9 4LA,
Scotland. E-mail g.j.molloy@stir.ac.uk
(Circ Heart Fail. 2012;5:126-133.)
© 2012 American Heart Association, Inc.
Circ Heart Fail is available at http://circheartfailure.ahajournals.org DOI: 10.1161/CIRCHEARTFAILURE.111.964569
126
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Cochrane Central Register of Controlled Trials, MEDLINE,
Cumulative Index of Nursing and Allied Health Literature
(CINAHL), Embase, and PsychInfo were searched for full
published reports to the end of December 2010. All databases
were searched from their start date. The search strategy
incorporated relevant terms from recent Cochrane Reviews
on adherence to medication 11,12 and heart failure, 13 and a
highly sensitive search strategy developed by the Cochrane
group for maximizing the identification of randomized trials
was also applied in Medline. 14 The reference lists of all
selected articles and relevant review articles were also
searched for additional studies. Only studies/abstracts in
English were included because translation services were not
available to the authors for this review.
Data Extraction
Data were extracted from selected studies with the use of a
predefined form. Data were extracted by Dr Molloy. Risk of
bias was assessed independently by Drs Molloy and
O’Carroll, and discrepancies were resolved by discussing the
discrepant judgments. Details of information extracted are
provided in Tables 1 and 2. Study authors were contacted for
additional information.
Quality Assessment
As recommended by the Cochrane Reviewers Handbook, 14
we assessed study quality according to 4 main sources of
potential bias in the identified studies: (1) selection bias, (2)
performance bias, (3) attrition bias, and (4) and detection
bias. To do this, studies were assessed for adequate sequence
generation and allocation concealment (selection bias), the
presence of blinding in outcome assessment (performance
and detection bias), and whether reporting of losses to
follow-up and intention-to-treat analysis were specified (at-
trition bias). Selective reporting bias was not assessed be-
cause few studies had published protocols before completing
and reporting their studies, making assessing this aspect of
bias difficult in most cases. The overall quality assessment for
each study was summarized by using a risk-of-bias summary
figure, based on Cochrane review recommendations. 14
Analysis
Pooling of the data was not possible because of the hetero-
geneity of measurement and analysis between studies. We
grouped studies according to the main components included
in the interventions. This was based on categories specified in
a recent systematic review of interventions to enhance adher-
ence to lipid-lowering medication. 12
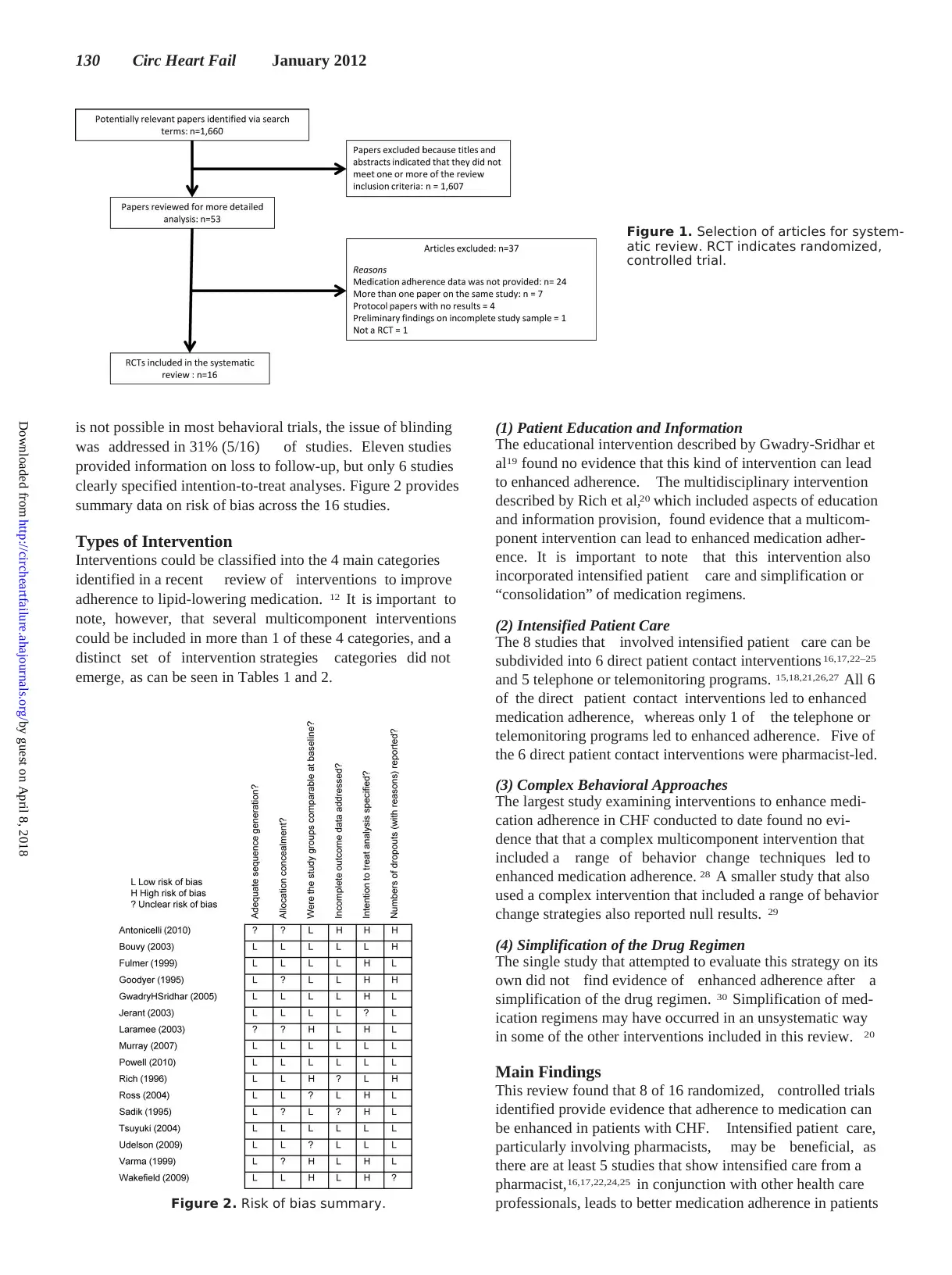
Selection of Trials
In total, the search strategies identified 1660 records (after
removal of duplicate records) of potential relevance from
searches of all 5 electronic databases (Figure 1). An inspec-
tion of study titles and the study abstracts revealed that more
than 95% of these did not meet the review inclusion criteria.
Fifty-three studies were retained for closer inspection, and
only 16 independent studies derived from these studies met
all the review inclusion criteria. The flow of studies through
the selection process is summarized in Figure 1.
Characteristics of Included Studies
Sixteen randomized, controlled trials were identified, con-
taining data on 3305 patients with CHF. The median total
sample size was 144 patients, with a range of 37–902. The
majority of studies (9/16) were conducted in the United
States. The average age of the study samples ranged from 55
years 15 to 85 years. 16 Male participation in trials ranged from
37%17 to 99%. 18 The median follow-up time was 6 months,
ranging from 2 weeks to 12 months, with 6 of 16 (38%) of
studies having follow-up times of less than 6 months. The
mean percentage of patients included at follow-up in the 13
studies that provided this data was 79.8%, with a range of
28 –100%. Adherence was measured by self-report in 5
studies, the medication event monitoring system in 5 studies,
tablet counts in 3 studies, and medication refill records in 3
studies. Because of the heterogeneity of measurement and
limitations in reporting, it was not possible to report a
summary of baseline rates of adherence for the reviewed
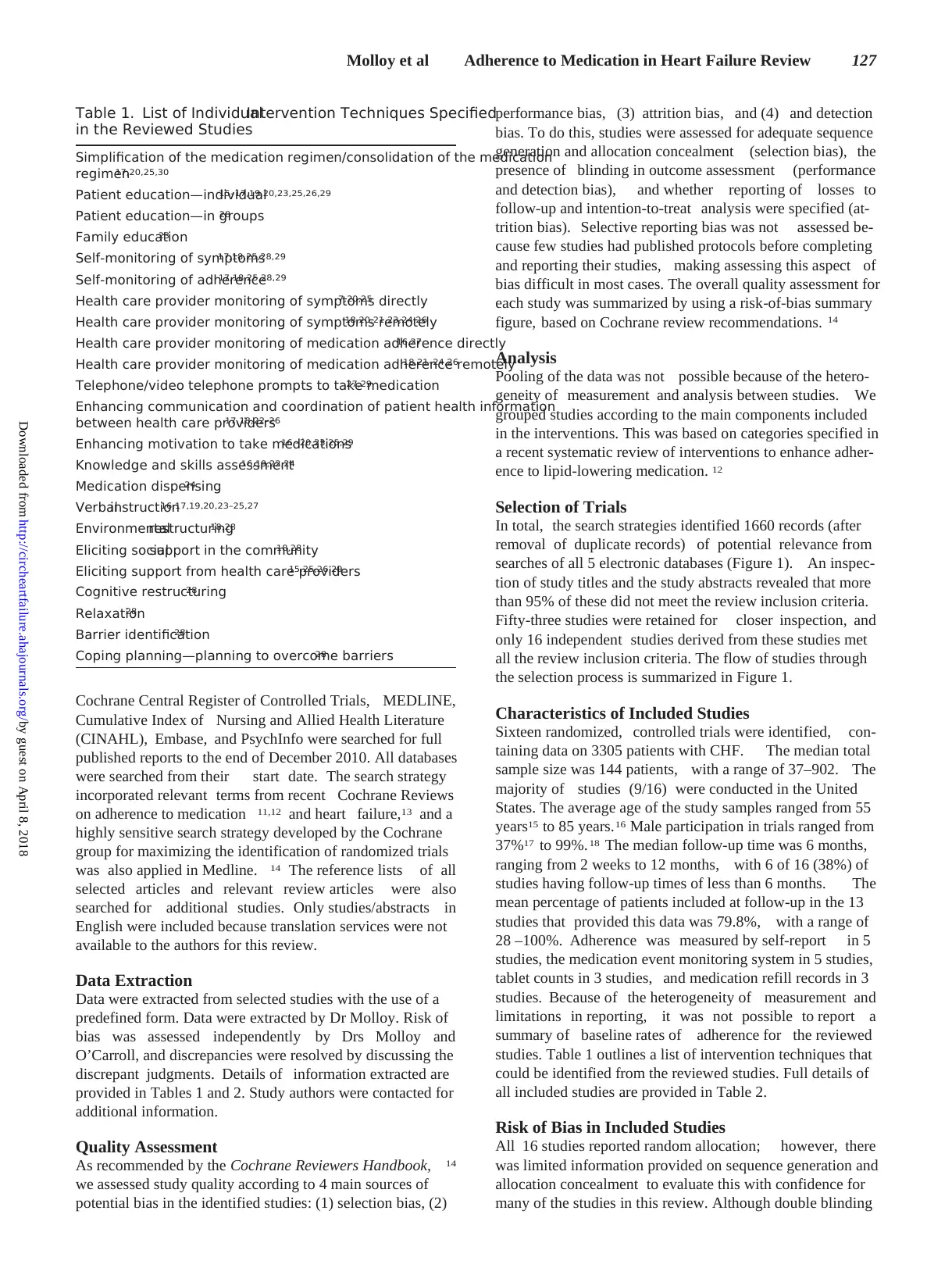
studies. Table 1 outlines a list of intervention techniques that
could be identified from the reviewed studies. Full details of
all included studies are provided in Table 2.
Risk of Bias in Included Studies
All 16 studies reported random allocation; however, there
was limited information provided on sequence generation and
allocation concealment to evaluate this with confidence for
many of the studies in this review. Although double blinding
Table 1. List of IndividualIntervention Techniques Specified
in the Reviewed Studies
Simplification of the medication regimen/consolidation of the medication
regimen17,20,25,30
Patient education—individual15–17,19,20,23,25,26,29
Patient education—in groups28
Family education23
Self-monitoring of symptoms17,18,25,28,29
Self-monitoring of adherence17,18,25,28,29
Health care provider monitoring of symptoms directly7,20,25
Health care provider monitoring of symptoms remotely18,20,21,23,24,26
Health care provider monitoring of medication adherence directly16,27
Health care provider monitoring of medication adherence remotely18,21–24,26
Telephone/video telephone prompts to take medication27,29
Enhancing communication and coordination of patient health information
between health care providers17,18,22–26
Enhancing motivation to take medications16 –20,23,25,29
Knowledge and skills assessment16,19,22,24
Medication dispensing24
Verbalinstruction16,17,19,20,23–25,27
Environmentalrestructuring18,28
Eliciting socialsupport in the community18,28
Eliciting support from health care providers15,25,26,29
Cognitive restructuring28
Relaxation28
Barrier identification28
Coping planning—planning to overcome barriers28
Molloy et al Adherence to Medication in Heart Failure Review 127
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Cumulative Index of Nursing and Allied Health Literature
(CINAHL), Embase, and PsychInfo were searched for full
published reports to the end of December 2010. All databases
were searched from their start date. The search strategy
incorporated relevant terms from recent Cochrane Reviews
on adherence to medication 11,12 and heart failure, 13 and a
highly sensitive search strategy developed by the Cochrane
group for maximizing the identification of randomized trials
was also applied in Medline. 14 The reference lists of all
selected articles and relevant review articles were also
searched for additional studies. Only studies/abstracts in
English were included because translation services were not
available to the authors for this review.
Data Extraction
Data were extracted from selected studies with the use of a
predefined form. Data were extracted by Dr Molloy. Risk of
bias was assessed independently by Drs Molloy and
O’Carroll, and discrepancies were resolved by discussing the
discrepant judgments. Details of information extracted are
provided in Tables 1 and 2. Study authors were contacted for
additional information.
Quality Assessment
As recommended by the Cochrane Reviewers Handbook, 14
we assessed study quality according to 4 main sources of
potential bias in the identified studies: (1) selection bias, (2)
performance bias, (3) attrition bias, and (4) and detection
bias. To do this, studies were assessed for adequate sequence
generation and allocation concealment (selection bias), the
presence of blinding in outcome assessment (performance
and detection bias), and whether reporting of losses to
follow-up and intention-to-treat analysis were specified (at-
trition bias). Selective reporting bias was not assessed be-
cause few studies had published protocols before completing
and reporting their studies, making assessing this aspect of
bias difficult in most cases. The overall quality assessment for
each study was summarized by using a risk-of-bias summary
figure, based on Cochrane review recommendations. 14
Analysis
Pooling of the data was not possible because of the hetero-
geneity of measurement and analysis between studies. We
grouped studies according to the main components included
in the interventions. This was based on categories specified in
a recent systematic review of interventions to enhance adher-
ence to lipid-lowering medication. 12
Selection of Trials
In total, the search strategies identified 1660 records (after
removal of duplicate records) of potential relevance from
searches of all 5 electronic databases (Figure 1). An inspec-
tion of study titles and the study abstracts revealed that more
than 95% of these did not meet the review inclusion criteria.
Fifty-three studies were retained for closer inspection, and
only 16 independent studies derived from these studies met
all the review inclusion criteria. The flow of studies through
the selection process is summarized in Figure 1.
Characteristics of Included Studies
Sixteen randomized, controlled trials were identified, con-
taining data on 3305 patients with CHF. The median total
sample size was 144 patients, with a range of 37–902. The
majority of studies (9/16) were conducted in the United
States. The average age of the study samples ranged from 55
years 15 to 85 years. 16 Male participation in trials ranged from
37%17 to 99%. 18 The median follow-up time was 6 months,
ranging from 2 weeks to 12 months, with 6 of 16 (38%) of
studies having follow-up times of less than 6 months. The
mean percentage of patients included at follow-up in the 13
studies that provided this data was 79.8%, with a range of
28 –100%. Adherence was measured by self-report in 5
studies, the medication event monitoring system in 5 studies,
tablet counts in 3 studies, and medication refill records in 3
studies. Because of the heterogeneity of measurement and
limitations in reporting, it was not possible to report a
summary of baseline rates of adherence for the reviewed
studies. Table 1 outlines a list of intervention techniques that
could be identified from the reviewed studies. Full details of
all included studies are provided in Table 2.
Risk of Bias in Included Studies
All 16 studies reported random allocation; however, there
was limited information provided on sequence generation and
allocation concealment to evaluate this with confidence for
many of the studies in this review. Although double blinding
Table 1. List of IndividualIntervention Techniques Specified
in the Reviewed Studies
Simplification of the medication regimen/consolidation of the medication
regimen17,20,25,30
Patient education—individual15–17,19,20,23,25,26,29
Patient education—in groups28
Family education23
Self-monitoring of symptoms17,18,25,28,29
Self-monitoring of adherence17,18,25,28,29
Health care provider monitoring of symptoms directly7,20,25
Health care provider monitoring of symptoms remotely18,20,21,23,24,26
Health care provider monitoring of medication adherence directly16,27
Health care provider monitoring of medication adherence remotely18,21–24,26
Telephone/video telephone prompts to take medication27,29
Enhancing communication and coordination of patient health information
between health care providers17,18,22–26
Enhancing motivation to take medications16 –20,23,25,29
Knowledge and skills assessment16,19,22,24
Medication dispensing24
Verbalinstruction16,17,19,20,23–25,27
Environmentalrestructuring18,28
Eliciting socialsupport in the community18,28
Eliciting support from health care providers15,25,26,29
Cognitive restructuring28
Relaxation28
Barrier identification28
Coping planning—planning to overcome barriers28
Molloy et al Adherence to Medication in Heart Failure Review 127
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
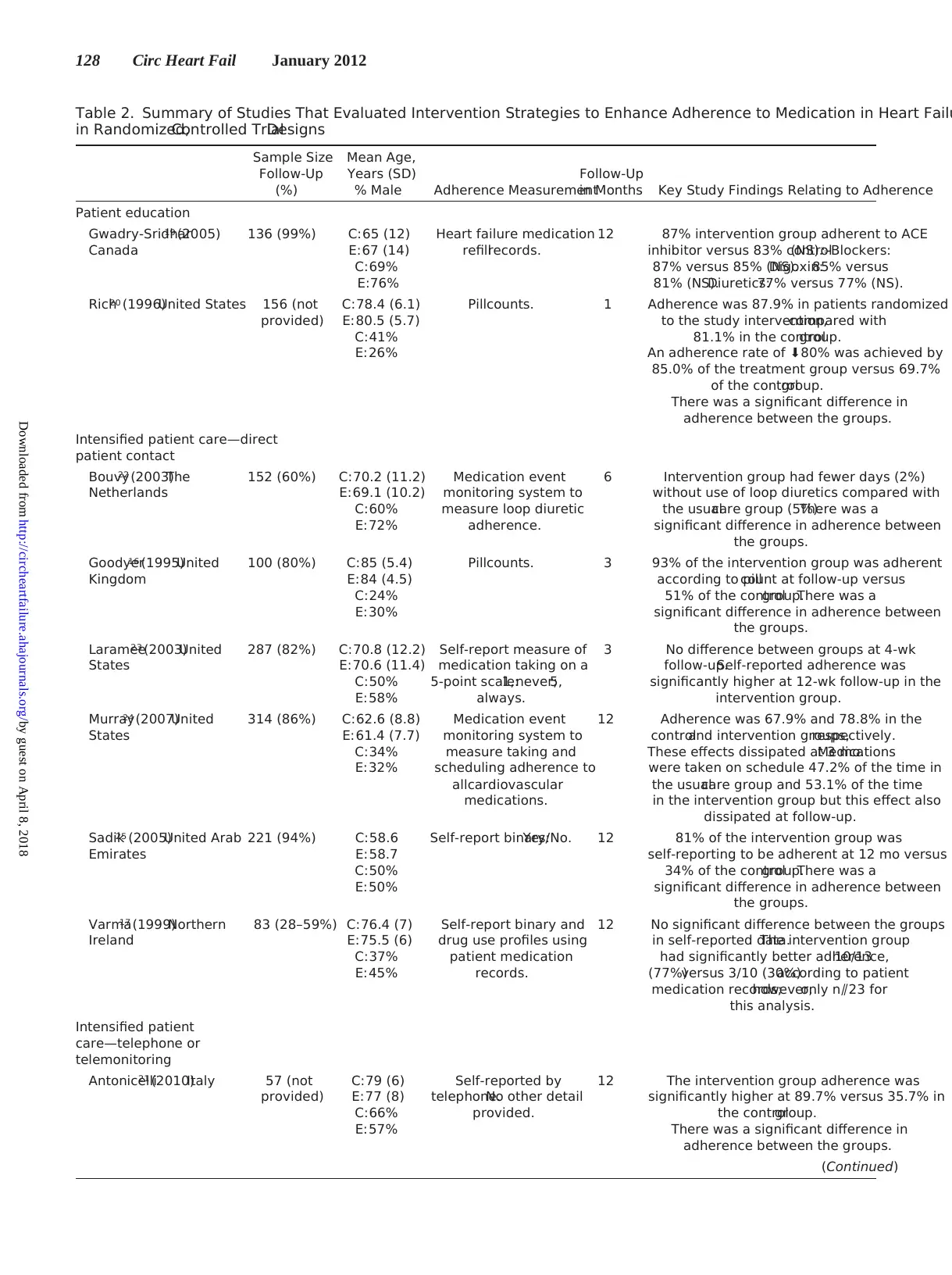
Table 2. Summary of Studies That Evaluated Intervention Strategies to Enhance Adherence to Medication in Heart Failu
in Randomized,Controlled TrialDesigns
Sample Size
Follow-Up
(%)
Mean Age,
Years (SD)
% Male Adherence Measurement
Follow-Up
in Months Key Study Findings Relating to Adherence
Patient education
Gwadry-Sridhar19 (2005)
Canada
136 (99%) C:65 (12)
E:67 (14)
C:69%
E:76%
Heart failure medication
refillrecords.
12 87% intervention group adherent to ACE
inhibitor versus 83% control(NS).-Blockers:
87% versus 85% (NS).Digoxin:85% versus
81% (NS).Diuretics:77% versus 77% (NS).
Rich20 (1996)United States 156 (not
provided)
C:78.4 (6.1)
E:80.5 (5.7)
C:41%
E:26%
Pillcounts. 1 Adherence was 87.9% in patients randomized
to the study intervention,compared with
81.1% in the controlgroup.
An adherence rate of ⬇80% was achieved by
85.0% of the treatment group versus 69.7%
of the controlgroup.
There was a significant difference in
adherence between the groups.
Intensified patient care—direct
patient contact
Bouvy22 (2003)The
Netherlands
152 (60%) C:70.2 (11.2)
E:69.1 (10.2)
C:60%
E:72%
Medication event
monitoring system to
measure loop diuretic
adherence.
6 Intervention group had fewer days (2%)
without use of loop diuretics compared with
the usualcare group (5%).There was a
significant difference in adherence between
the groups.
Goodyer16 (1995)United
Kingdom
100 (80%) C:85 (5.4)
E:84 (4.5)
C:24%
E:30%
Pillcounts. 3 93% of the intervention group was adherent
according to pillcount at follow-up versus
51% of the controlgroup.There was a
significant difference in adherence between
the groups.
Laramee23 (2003)United
States
287 (82%) C:70.8 (12.2)
E:70.6 (11.4)
C:50%
E:58%
Self-report measure of
medication taking on a
5-point scale:1,never;5,
always.
3 No difference between groups at 4-wk
follow-up.Self-reported adherence was
significantly higher at 12-wk follow-up in the
intervention group.
Murray24 (2007)United
States
314 (86%) C:62.6 (8.8)
E:61.4 (7.7)
C:34%
E:32%
Medication event
monitoring system to
measure taking and
scheduling adherence to
allcardiovascular
medications.
12 Adherence was 67.9% and 78.8% in the
controland intervention groups,respectively.
These effects dissipated at 3 mo.Medications
were taken on schedule 47.2% of the time in
the usualcare group and 53.1% of the time
in the intervention group but this effect also
dissipated at follow-up.
Sadik25 (2005)United Arab
Emirates
221 (94%) C:58.6
E:58.7
C:50%
E:50%
Self-report binary:Yes/No. 12 81% of the intervention group was
self-reporting to be adherent at 12 mo versus
34% of the controlgroup.There was a
significant difference in adherence between
the groups.
Varma17 (1999)Northern
Ireland
83 (28–59%) C:76.4 (7)
E:75.5 (6)
C:37%
E:45%
Self-report binary and
drug use profiles using
patient medication
records.
12 No significant difference between the groups
in self-reported data.The intervention group
had significantly better adherence,10/13
(77%)versus 3/10 (30%)according to patient
medication records;however,only n⫽23 for
this analysis.
Intensified patient
care—telephone or
telemonitoring
Antonicelli21 (2010)Italy 57 (not
provided)
C:79 (6)
E:77 (8)
C:66%
E:57%
Self-reported by
telephone.No other detail
provided.
12 The intervention group adherence was
significantly higher at 89.7% versus 35.7% in
the controlgroup.
There was a significant difference in
adherence between the groups.
(Continued)
128 Circ Heart Fail January 2012
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
in Randomized,Controlled TrialDesigns
Sample Size
Follow-Up
(%)
Mean Age,
Years (SD)
% Male Adherence Measurement
Follow-Up
in Months Key Study Findings Relating to Adherence
Patient education
Gwadry-Sridhar19 (2005)
Canada
136 (99%) C:65 (12)
E:67 (14)
C:69%
E:76%
Heart failure medication
refillrecords.
12 87% intervention group adherent to ACE
inhibitor versus 83% control(NS).-Blockers:
87% versus 85% (NS).Digoxin:85% versus
81% (NS).Diuretics:77% versus 77% (NS).
Rich20 (1996)United States 156 (not
provided)
C:78.4 (6.1)
E:80.5 (5.7)
C:41%
E:26%
Pillcounts. 1 Adherence was 87.9% in patients randomized
to the study intervention,compared with
81.1% in the controlgroup.
An adherence rate of ⬇80% was achieved by
85.0% of the treatment group versus 69.7%
of the controlgroup.
There was a significant difference in
adherence between the groups.
Intensified patient care—direct
patient contact
Bouvy22 (2003)The
Netherlands
152 (60%) C:70.2 (11.2)
E:69.1 (10.2)
C:60%
E:72%
Medication event
monitoring system to
measure loop diuretic
adherence.
6 Intervention group had fewer days (2%)
without use of loop diuretics compared with
the usualcare group (5%).There was a
significant difference in adherence between
the groups.
Goodyer16 (1995)United
Kingdom
100 (80%) C:85 (5.4)
E:84 (4.5)
C:24%
E:30%
Pillcounts. 3 93% of the intervention group was adherent
according to pillcount at follow-up versus
51% of the controlgroup.There was a
significant difference in adherence between
the groups.
Laramee23 (2003)United
States
287 (82%) C:70.8 (12.2)
E:70.6 (11.4)
C:50%
E:58%
Self-report measure of
medication taking on a
5-point scale:1,never;5,
always.
3 No difference between groups at 4-wk
follow-up.Self-reported adherence was
significantly higher at 12-wk follow-up in the
intervention group.
Murray24 (2007)United
States
314 (86%) C:62.6 (8.8)
E:61.4 (7.7)
C:34%
E:32%
Medication event
monitoring system to
measure taking and
scheduling adherence to
allcardiovascular
medications.
12 Adherence was 67.9% and 78.8% in the
controland intervention groups,respectively.
These effects dissipated at 3 mo.Medications
were taken on schedule 47.2% of the time in
the usualcare group and 53.1% of the time
in the intervention group but this effect also
dissipated at follow-up.
Sadik25 (2005)United Arab
Emirates
221 (94%) C:58.6
E:58.7
C:50%
E:50%
Self-report binary:Yes/No. 12 81% of the intervention group was
self-reporting to be adherent at 12 mo versus
34% of the controlgroup.There was a
significant difference in adherence between
the groups.
Varma17 (1999)Northern
Ireland
83 (28–59%) C:76.4 (7)
E:75.5 (6)
C:37%
E:45%
Self-report binary and
drug use profiles using
patient medication
records.
12 No significant difference between the groups
in self-reported data.The intervention group
had significantly better adherence,10/13
(77%)versus 3/10 (30%)according to patient
medication records;however,only n⫽23 for
this analysis.
Intensified patient
care—telephone or
telemonitoring
Antonicelli21 (2010)Italy 57 (not
provided)
C:79 (6)
E:77 (8)
C:66%
E:57%
Self-reported by
telephone.No other detail
provided.
12 The intervention group adherence was
significantly higher at 89.7% versus 35.7% in
the controlgroup.
There was a significant difference in
adherence between the groups.
(Continued)
128 Circ Heart Fail January 2012
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
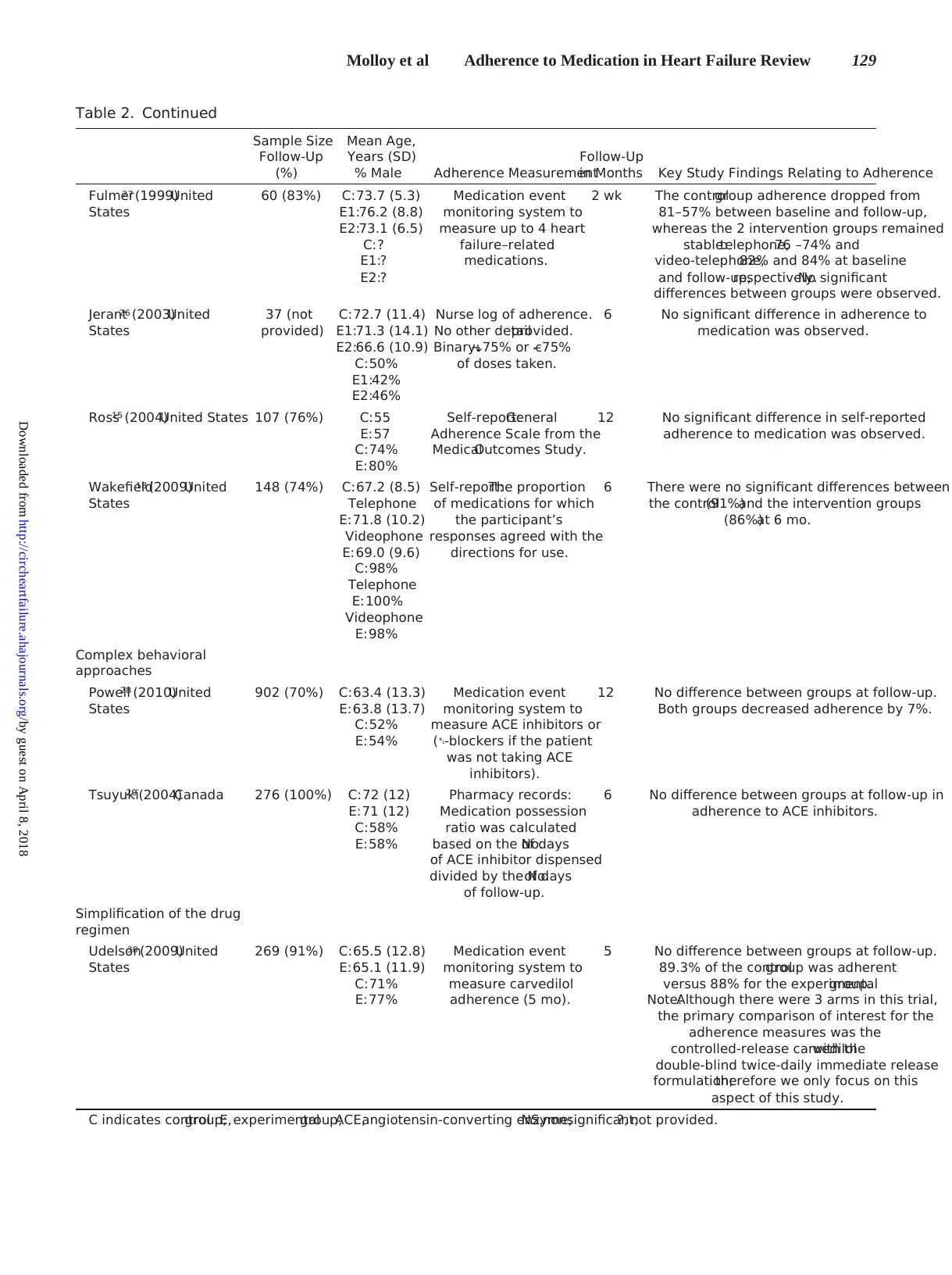
Table 2. Continued
Sample Size
Follow-Up
(%)
Mean Age,
Years (SD)
% Male Adherence Measurement
Follow-Up
in Months Key Study Findings Relating to Adherence
Fulmer27 (1999)United
States
60 (83%) C:73.7 (5.3)
E1:76.2 (8.8)
E2:73.1 (6.5)
C:?
E1:?
E2:?
Medication event
monitoring system to
measure up to 4 heart
failure–related
medications.
2 wk The controlgroup adherence dropped from
81–57% between baseline and follow-up,
whereas the 2 intervention groups remained
stable:telephone,76 –74% and
video-telephone,82% and 84% at baseline
and follow-up,respectively.No significant
differences between groups were observed.
Jerant26 (2003)United
States
37 (not
provided)
C:72.7 (11.4)
E1:71.3 (14.1)
E2:66.6 (10.9)
C:50%
E1:42%
E2:46%
Nurse log of adherence.
No other detailprovided.
Binary:⬎75% or ⱕ75%
of doses taken.
6 No significant difference in adherence to
medication was observed.
Ross15 (2004)United States 107 (76%) C:55
E:57
C:74%
E:80%
Self-report:General
Adherence Scale from the
MedicalOutcomes Study.
12 No significant difference in self-reported
adherence to medication was observed.
Wakefield18 (2009)United
States
148 (74%) C:67.2 (8.5)
Telephone
E:71.8 (10.2)
Videophone
E:69.0 (9.6)
C:98%
Telephone
E:100%
Videophone
E:98%
Self-report:The proportion
of medications for which
the participant’s
responses agreed with the
directions for use.
6 There were no significant differences between
the control(91%)and the intervention groups
(86%)at 6 mo.
Complex behavioral
approaches
Powell28 (2010)United
States
902 (70%) C:63.4 (13.3)
E:63.8 (13.7)
C:52%
E:54%
Medication event
monitoring system to
measure ACE inhibitors or
(-blockers if the patient
was not taking ACE
inhibitors).
12 No difference between groups at follow-up.
Both groups decreased adherence by 7%.
Tsuyuki29 (2004)Canada 276 (100%) C:72 (12)
E:71 (12)
C:58%
E:58%
Pharmacy records:
Medication possession
ratio was calculated
based on the No.of days
of ACE inhibitor dispensed
divided by the No.of days
of follow-up.
6 No difference between groups at follow-up in
adherence to ACE inhibitors.
Simplification of the drug
regimen
Udelson30 (2009)United
States
269 (91%) C:65.5 (12.8)
E:65.1 (11.9)
C:71%
E:77%
Medication event
monitoring system to
measure carvedilol
adherence (5 mo).
5 No difference between groups at follow-up.
89.3% of the controlgroup was adherent
versus 88% for the experimentalgroup.
Note:Although there were 3 arms in this trial,
the primary comparison of interest for the
adherence measures was the
controlled-release carvedilolwith the
double-blind twice-daily immediate release
formulation;therefore we only focus on this
aspect of this study.
C indicates controlgroup;E,experimentalgroup;ACE,angiotensin-converting enzyme;NS,nonsignificant;?, not provided.
Molloy et al Adherence to Medication in Heart Failure Review 129
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Sample Size
Follow-Up
(%)
Mean Age,
Years (SD)
% Male Adherence Measurement
Follow-Up
in Months Key Study Findings Relating to Adherence
Fulmer27 (1999)United
States
60 (83%) C:73.7 (5.3)
E1:76.2 (8.8)
E2:73.1 (6.5)
C:?
E1:?
E2:?
Medication event
monitoring system to
measure up to 4 heart
failure–related
medications.
2 wk The controlgroup adherence dropped from
81–57% between baseline and follow-up,
whereas the 2 intervention groups remained
stable:telephone,76 –74% and
video-telephone,82% and 84% at baseline
and follow-up,respectively.No significant
differences between groups were observed.
Jerant26 (2003)United
States
37 (not
provided)
C:72.7 (11.4)
E1:71.3 (14.1)
E2:66.6 (10.9)
C:50%
E1:42%
E2:46%
Nurse log of adherence.
No other detailprovided.
Binary:⬎75% or ⱕ75%
of doses taken.
6 No significant difference in adherence to
medication was observed.
Ross15 (2004)United States 107 (76%) C:55
E:57
C:74%
E:80%
Self-report:General
Adherence Scale from the
MedicalOutcomes Study.
12 No significant difference in self-reported
adherence to medication was observed.
Wakefield18 (2009)United
States
148 (74%) C:67.2 (8.5)
Telephone
E:71.8 (10.2)
Videophone
E:69.0 (9.6)
C:98%
Telephone
E:100%
Videophone
E:98%
Self-report:The proportion
of medications for which
the participant’s
responses agreed with the
directions for use.
6 There were no significant differences between
the control(91%)and the intervention groups
(86%)at 6 mo.
Complex behavioral
approaches
Powell28 (2010)United
States
902 (70%) C:63.4 (13.3)
E:63.8 (13.7)
C:52%
E:54%
Medication event
monitoring system to
measure ACE inhibitors or
(-blockers if the patient
was not taking ACE
inhibitors).
12 No difference between groups at follow-up.
Both groups decreased adherence by 7%.
Tsuyuki29 (2004)Canada 276 (100%) C:72 (12)
E:71 (12)
C:58%
E:58%
Pharmacy records:
Medication possession
ratio was calculated
based on the No.of days
of ACE inhibitor dispensed
divided by the No.of days
of follow-up.
6 No difference between groups at follow-up in
adherence to ACE inhibitors.
Simplification of the drug
regimen
Udelson30 (2009)United
States
269 (91%) C:65.5 (12.8)
E:65.1 (11.9)
C:71%
E:77%
Medication event
monitoring system to
measure carvedilol
adherence (5 mo).
5 No difference between groups at follow-up.
89.3% of the controlgroup was adherent
versus 88% for the experimentalgroup.
Note:Although there were 3 arms in this trial,
the primary comparison of interest for the
adherence measures was the
controlled-release carvedilolwith the
double-blind twice-daily immediate release
formulation;therefore we only focus on this
aspect of this study.
C indicates controlgroup;E,experimentalgroup;ACE,angiotensin-converting enzyme;NS,nonsignificant;?, not provided.
Molloy et al Adherence to Medication in Heart Failure Review 129
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
is not possible in most behavioral trials, the issue of blinding
was addressed in 31% (5/16) of studies. Eleven studies
provided information on loss to follow-up, but only 6 studies
clearly specified intention-to-treat analyses. Figure 2 provides
summary data on risk of bias across the 16 studies.
Types of Intervention
Interventions could be classified into the 4 main categories
identified in a recent review of interventions to improve
adherence to lipid-lowering medication. 12 It is important to
note, however, that several multicomponent interventions
could be included in more than 1 of these 4 categories, and a
distinct set of intervention strategies categories did not
emerge, as can be seen in Tables 1 and 2.
(1) Patient Education and Information
The educational intervention described by Gwadry-Sridhar et
al 19 found no evidence that this kind of intervention can lead
to enhanced adherence. The multidisciplinary intervention
described by Rich et al,20 which included aspects of education
and information provision, found evidence that a multicom-
ponent intervention can lead to enhanced medication adher-
ence. It is important to note that this intervention also
incorporated intensified patient care and simplification or
“consolidation” of medication regimens.
(2) Intensified Patient Care
The 8 studies that involved intensified patient care can be
subdivided into 6 direct patient contact interventions 16,17,22–25
and 5 telephone or telemonitoring programs. 15,18,21,26,27 All 6
of the direct patient contact interventions led to enhanced
medication adherence, whereas only 1 of the telephone or
telemonitoring programs led to enhanced adherence. Five of
the 6 direct patient contact interventions were pharmacist-led.
(3) Complex Behavioral Approaches
The largest study examining interventions to enhance medi-
cation adherence in CHF conducted to date found no evi-
dence that that a complex multicomponent intervention that
included a range of behavior change techniques led to
enhanced medication adherence. 28 A smaller study that also
used a complex intervention that included a range of behavior
change strategies also reported null results. 29
(4) Simplification of the Drug Regimen
The single study that attempted to evaluate this strategy on its
own did not find evidence of enhanced adherence after a
simplification of the drug regimen. 30 Simplification of med-
ication regimens may have occurred in an unsystematic way
in some of the other interventions included in this review. 20
Main Findings
This review found that 8 of 16 randomized, controlled trials
identified provide evidence that adherence to medication can
be enhanced in patients with CHF. Intensified patient care,
particularly involving pharmacists, may be beneficial, as
there are at least 5 studies that show intensified care from a
pharmacist, 16,17,22,24,25 in conjunction with other health care
professionals, leads to better medication adherence in patients
Figure 1. Selection of articles for system-
atic review. RCT indicates randomized,
controlled trial.
Figure 2. Risk of bias summary.
130 Circ Heart Fail January 2012
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
was addressed in 31% (5/16) of studies. Eleven studies
provided information on loss to follow-up, but only 6 studies
clearly specified intention-to-treat analyses. Figure 2 provides
summary data on risk of bias across the 16 studies.
Types of Intervention
Interventions could be classified into the 4 main categories
identified in a recent review of interventions to improve
adherence to lipid-lowering medication. 12 It is important to
note, however, that several multicomponent interventions
could be included in more than 1 of these 4 categories, and a
distinct set of intervention strategies categories did not
emerge, as can be seen in Tables 1 and 2.
(1) Patient Education and Information
The educational intervention described by Gwadry-Sridhar et
al 19 found no evidence that this kind of intervention can lead
to enhanced adherence. The multidisciplinary intervention
described by Rich et al,20 which included aspects of education
and information provision, found evidence that a multicom-
ponent intervention can lead to enhanced medication adher-
ence. It is important to note that this intervention also
incorporated intensified patient care and simplification or
“consolidation” of medication regimens.
(2) Intensified Patient Care
The 8 studies that involved intensified patient care can be
subdivided into 6 direct patient contact interventions 16,17,22–25
and 5 telephone or telemonitoring programs. 15,18,21,26,27 All 6
of the direct patient contact interventions led to enhanced
medication adherence, whereas only 1 of the telephone or
telemonitoring programs led to enhanced adherence. Five of
the 6 direct patient contact interventions were pharmacist-led.
(3) Complex Behavioral Approaches
The largest study examining interventions to enhance medi-
cation adherence in CHF conducted to date found no evi-
dence that that a complex multicomponent intervention that
included a range of behavior change techniques led to
enhanced medication adherence. 28 A smaller study that also
used a complex intervention that included a range of behavior
change strategies also reported null results. 29
(4) Simplification of the Drug Regimen
The single study that attempted to evaluate this strategy on its
own did not find evidence of enhanced adherence after a
simplification of the drug regimen. 30 Simplification of med-
ication regimens may have occurred in an unsystematic way
in some of the other interventions included in this review. 20
Main Findings
This review found that 8 of 16 randomized, controlled trials
identified provide evidence that adherence to medication can
be enhanced in patients with CHF. Intensified patient care,
particularly involving pharmacists, may be beneficial, as
there are at least 5 studies that show intensified care from a
pharmacist, 16,17,22,24,25 in conjunction with other health care
professionals, leads to better medication adherence in patients
Figure 1. Selection of articles for system-
atic review. RCT indicates randomized,
controlled trial.
Figure 2. Risk of bias summary.
130 Circ Heart Fail January 2012
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from

with CHF. There is emerging evidence that patient education
and self-management training alone is not effective in en-
hancing adherence to medication. 19,28,29 The overall conclu-
sion of the methodological quality of the 16 trials included in
this review indicate that there is limited high-quality evidence
evaluating the effectiveness of specific adherence-enhancing
interventions in patients with CHF and that the findings of
many of the existing randomized, controlled trials should be
interpreted with caution. The heterogeneity in intervention
techniques and measurement methodology observed between
the studies in this review means that a conclusive literature on
enhancing adherence to medication in heart failure has yet to
emerge. This mirrors findings from other related broader
reviews in a range of clinical conditions. 11,12
Our assessment of the sample characteristics also revealed
that the patients enrolled into these studies were not repre-
sentative of the patients with CHF seen in clinical practice in
terms of age and sex profile. This indicates that selection
biases are operating in recruitment in this area of research,
which limits the generalizability of these findings. The
relatively short and variable follow-up times seen across
these 16 studies also show that there are limited data on the
sustainability of both the intervention strategies and the
intervention effects in those studies that found significantly
enhanced adherence. Five of the reports included23–26,29
incorporated a health economics evaluation with varying
degrees of sophistication; therefore the cost implications of
most of the intervention strategies are unknown. However, 2
of these studies26,29 reported significant health care cost
reductions as a consequence of the interventions. This raises
the possibility that medication-enhancing interventions can
reduce health care costs, which may be particularly important
in new health care funding environments, for example,
accountable care organizations in the United States or the
Quality Outcomes Framework in the United Kingdom.
Although a number of studies in this review did include
interventions that used information technology, specifically
telemonitoring of patients with CHF, 13 this area of research
has yet to evaluate the role or potential of electronic patient
records or new developments in handheld communication
devices and social media to enhance adherence to medication
in heart failure. Future work should attempt to investigate the
potential of these new technologies in motivating, enabling,
and prompting patients with heart failure to take their
medications as prescribed.
Limitations
The most obvious limitation in this review was that quanti-
tative meta-analysis was not possible. A recent meta-analysis
of 33 studies 31 testing adherence-enhancing interventions for
older adults estimated that effect sizes were likely to be in the
small to medium range, with a summary standardized mean
difference of 0.33 in medication adherence observed between
control and intervention groups. Only 1 of the studies in the
published meta-analysis is included in our review. 20 Until
there is greater consistency of measurement and analysis
across studies, we cannot know whether similar effects can be
achieved in CHF populations. Future investigators should
therefore assume that intervention effects will not be larger
than the small to medium range when conducting sample size
calculations for new studies.
The limited number of studies identified that describe a
heterogeneous range of interventions prevent us from draw-
ing firm conclusions on many types of adherence promoting
strategies for patients with CHF. For example, the null
findings for the one study 30 in this review that compared
once-daily dosing with twice-daily dosing should be consid-
ered in light of the limitations of that particular study and the
considerable evidence in other conditions that simplifying
medication regimens is associated with better adherence. 32
There was also limited detail provided on the contexts in
which interventions were delivered. This makes it difficult to
know where and when effective interventions to enhance
adherence to medication are best delivered.
Implications for Research
Adherence to medication and other aspects of self-care for a
debilitating symptomatic chronic illness such as CHF is a
complex behavior with multifactorial determinants, 6,33 in-
cluding a range of individual and social-environment fac-
tors.34,35 Although earlier studies have reviewed the broader
issues of adherence to health professionals’ self-care recom-
mendation in CHF, 5 this review focused on those interven-
tions that specifically address medication adherence for 3 key
reasons. First, the association between medication adherence
and health outcomes is more precisely described, 2,4 whereas
the benefits of other aspects of adherence to CHF self-care
cannot be estimated with the same degree of precision
because of measurement and study design limitations that are
inherent in studying these phenomena, for example, weighing
oneself daily and limiting sodium intake. Second, adherence
to medication is a very different behavioral phenomenon 36
than other aspects of adherence to self-care in heart failure
that is likely to have different determinants. Finally,
intervention strategies to enhance adherence to medication
are likely to be of a different form than many other aspects
of adherence to self-care, given the unique barriers and
facilitators to this behavior. 5,33 Therefore, there is clearly
scope to develop a focus for further investigation into
adherence to medication in heart failure as opposed to more
generalized management of self-care in heart failure. 5
Four of the studies included in this review 18,21,28,30 have
been published since the Cochrane review of interventions for
enhancing medication adherence,11 and only 1 of the studies25
included in the present review was included in that Cochrane
review. Another more recent relevant review on improving
adherence to cardiovascular medication 10 included only 4
studies from the present review. 16,24,27,30
Many of the reviewed studies provided limited information
on the content of the study interventions. This prevents the
development of a cumulative body of research or even simple
replication of individual studies. The increasing emphasis on
publishing detailed protocol reports in advance of the study
commencement has reduced this problem in more recent
studies. This area of research would, however, be greatly
strengthened by the development of a taxonomy of behavior
change techniques for medication adherence– enhancing in-
terventions to standardize the content, classification, and
Molloy et al Adherence to Medication in Heart Failure Review 131
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
and self-management training alone is not effective in en-
hancing adherence to medication. 19,28,29 The overall conclu-
sion of the methodological quality of the 16 trials included in
this review indicate that there is limited high-quality evidence
evaluating the effectiveness of specific adherence-enhancing
interventions in patients with CHF and that the findings of
many of the existing randomized, controlled trials should be
interpreted with caution. The heterogeneity in intervention
techniques and measurement methodology observed between
the studies in this review means that a conclusive literature on
enhancing adherence to medication in heart failure has yet to
emerge. This mirrors findings from other related broader
reviews in a range of clinical conditions. 11,12
Our assessment of the sample characteristics also revealed
that the patients enrolled into these studies were not repre-
sentative of the patients with CHF seen in clinical practice in
terms of age and sex profile. This indicates that selection
biases are operating in recruitment in this area of research,
which limits the generalizability of these findings. The
relatively short and variable follow-up times seen across
these 16 studies also show that there are limited data on the
sustainability of both the intervention strategies and the
intervention effects in those studies that found significantly
enhanced adherence. Five of the reports included23–26,29
incorporated a health economics evaluation with varying
degrees of sophistication; therefore the cost implications of
most of the intervention strategies are unknown. However, 2
of these studies26,29 reported significant health care cost
reductions as a consequence of the interventions. This raises
the possibility that medication-enhancing interventions can
reduce health care costs, which may be particularly important
in new health care funding environments, for example,
accountable care organizations in the United States or the
Quality Outcomes Framework in the United Kingdom.
Although a number of studies in this review did include
interventions that used information technology, specifically
telemonitoring of patients with CHF, 13 this area of research
has yet to evaluate the role or potential of electronic patient
records or new developments in handheld communication
devices and social media to enhance adherence to medication
in heart failure. Future work should attempt to investigate the
potential of these new technologies in motivating, enabling,
and prompting patients with heart failure to take their
medications as prescribed.
Limitations
The most obvious limitation in this review was that quanti-
tative meta-analysis was not possible. A recent meta-analysis
of 33 studies 31 testing adherence-enhancing interventions for
older adults estimated that effect sizes were likely to be in the
small to medium range, with a summary standardized mean
difference of 0.33 in medication adherence observed between
control and intervention groups. Only 1 of the studies in the
published meta-analysis is included in our review. 20 Until
there is greater consistency of measurement and analysis
across studies, we cannot know whether similar effects can be
achieved in CHF populations. Future investigators should
therefore assume that intervention effects will not be larger
than the small to medium range when conducting sample size
calculations for new studies.
The limited number of studies identified that describe a
heterogeneous range of interventions prevent us from draw-
ing firm conclusions on many types of adherence promoting
strategies for patients with CHF. For example, the null
findings for the one study 30 in this review that compared
once-daily dosing with twice-daily dosing should be consid-
ered in light of the limitations of that particular study and the
considerable evidence in other conditions that simplifying
medication regimens is associated with better adherence. 32
There was also limited detail provided on the contexts in
which interventions were delivered. This makes it difficult to
know where and when effective interventions to enhance
adherence to medication are best delivered.
Implications for Research
Adherence to medication and other aspects of self-care for a
debilitating symptomatic chronic illness such as CHF is a
complex behavior with multifactorial determinants, 6,33 in-
cluding a range of individual and social-environment fac-
tors.34,35 Although earlier studies have reviewed the broader
issues of adherence to health professionals’ self-care recom-
mendation in CHF, 5 this review focused on those interven-
tions that specifically address medication adherence for 3 key
reasons. First, the association between medication adherence
and health outcomes is more precisely described, 2,4 whereas
the benefits of other aspects of adherence to CHF self-care
cannot be estimated with the same degree of precision
because of measurement and study design limitations that are
inherent in studying these phenomena, for example, weighing
oneself daily and limiting sodium intake. Second, adherence
to medication is a very different behavioral phenomenon 36
than other aspects of adherence to self-care in heart failure
that is likely to have different determinants. Finally,
intervention strategies to enhance adherence to medication
are likely to be of a different form than many other aspects
of adherence to self-care, given the unique barriers and
facilitators to this behavior. 5,33 Therefore, there is clearly
scope to develop a focus for further investigation into
adherence to medication in heart failure as opposed to more
generalized management of self-care in heart failure. 5
Four of the studies included in this review 18,21,28,30 have
been published since the Cochrane review of interventions for
enhancing medication adherence,11 and only 1 of the studies25
included in the present review was included in that Cochrane
review. Another more recent relevant review on improving
adherence to cardiovascular medication 10 included only 4
studies from the present review. 16,24,27,30
Many of the reviewed studies provided limited information
on the content of the study interventions. This prevents the
development of a cumulative body of research or even simple
replication of individual studies. The increasing emphasis on
publishing detailed protocol reports in advance of the study
commencement has reduced this problem in more recent
studies. This area of research would, however, be greatly
strengthened by the development of a taxonomy of behavior
change techniques for medication adherence– enhancing in-
terventions to standardize the content, classification, and
Molloy et al Adherence to Medication in Heart Failure Review 131
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

description of intervention strategies. The value of such
taxonomies is gaining increasing recognition in other areas of
behavioral science that focus on the role self-care in promot-
ing health. 37 Because the content and context of many
adherence-enhancing interventions is not clearly specified in
standardized terminology and theory from behavioral science
is often absent, the approaches to intervention development in
this area can be likened to developing antihypertensive
medications without any understanding of the pharmacology
of the medication, the physiology of systemic blood pressure
control, or the pathophysiology of hypertension. 38
Implications for Practice
There is clearly scope to significantly improve outcomes in
heart failure by enhancing adherence to those existing med-
ications that are known to reduce morbidity and mortality
from heart failure. CHF medication regimens have become
increasingly complex as new treatments have emerged, 6
which provides a challenge for patients with CHF to manage.
Practitioners should consider that developing effective meth-
ods to increase patient adherence to existing medications with
known efficacy could have far greater health benefits than
providing new treatments that may not be followed. 11 The
reviewed studies do provide evidence that enhanced adher-
ence to medications can be achieved in heart failure patients
and that the role of pharmacists may be particularly impor-
tant, in particular, direct communication between patient,
pharmacists, and other health care providers.22,24,25 This
review also suggests that patient education about CHF or
self-management training alone may not be effective. Overall
it is clear, however, that formal recommendations on the best
approaches to enhance adherence to medication in CHF
cannot be derived from the existing studies. New studies with
more clearly justified and specified methodology are required
to generate a cumulative body of findings that could be used
to inform clinical practice. In particular, more explicit use of
behavioral sciences in developing adherence interventions in
CHF is clearly warranted.
Conclusions
It may be possible to improve adherence to medication in
patients with CHF by using a range of strategies; however,
the specification of effective techniques requires greater
clarity in this literature. There is currently limited high-
quality evidence on the effectiveness of interventions that aim
to enhance adherence to medication in typical heart failure
patients, and further research is needed to identify the
optimum strategies for implementation in clinical practice.
Disclosures
None.
References
1. Jhund PS, Macintyre K, Simpson CR, Lewsey JD, Stewart S, Redpath A,
Chalmers JW, Capewell S, McMurray JJ. Long-term trends in first hos-
pitalization for heart failure and subsequent survival between 1986 and
2003: a population study of 5.1 million people. Circulation. 2009;119:
515–523.
2. SOLVD Investigators. Effect of enalapril on survival in patients with
reduced left ventricular ejection fractions and congestive heart failure: the
SOLVD Investigators. N Engl J Med. 1991;325:293–302.
3. Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM,
Shusterman NH. The effect of carvedilol on morbidity and mortality in
patients with chronic heart failure: US Carvedilol Heart Failure Study
Group. N Engl J Med. 1996;334:1349 –1355.
4. Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky
J, Wittes J. The effect of spironolactone on morbidity and mortality in
patients with severe heart failure: Randomized Aldactone Evaluation
Study Investigators. N Engl J Med. 1999;341:709 –717.
5. van der Wal MH, Jaarsma T. Adherence in heart failure in the elderly:
problem and possible solutions. Int J Cardiol. 2008;125:203–208.
6. Hauptman PJ. Medication adherence in heart failure. Heart Fail Rev.
2008;13:99 –106.
7. Butler J, Arbogast PG, Daugherty J, Jain MK, Ray WA, Griffin MR.
Outpatient utilization of angiotensin-converting enzyme inhibitors among
heart failure patients after hospital discharge. J Am Coll Cardiol. 2004;
43:2036 –2043.
8. Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Avorn J. Noncompliance
with congestive heart failure therapy in the elderly. Arch Intern Med.
1994;154:433– 437.
9. Wu JR, Moser DK, De Jong MJ, Rayens MK, Chung ML, Riegel B,
Lennie TA. Defining an evidence-based cutpoint for medication
adherence in heart failure. Am Heart J. 2009;157:285–291.
10. Glynn L, Fahey T. Cardiovascular medication: improving adherence. Clin
Evid (Online). 2011. Available at http://clinicalevidence.bmj.com.
11. Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for
enhancing medication adherence. Cochrane Database Syst Rev. 2008;2:
CD000011.
12. Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to
lipid lowering medication. Cochrane Database Syst Rev. 2010;
CD004371.
13. Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D,
Stewart S, Cleland JG. Structured telephone support or telemonitoring
programmes for patients with chronic heart failure. Cochrane Database
Syst Rev. 2010;8:CD007228.
14. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of
Interventions. Chichester, UK: The Cochrane Collaboration and John
Wiley & Sons Ltd; 2008.
15. Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a
web-based online medical record with electronic communication capa-
bilities to patients with congestive heart failure: randomized trial. J Med
Internet Res. 2004;6:e12.
16. Goodyer LI, Miskelly F, Milligan P. Does encouraging good compliance
improve patients’ clinical condition in heart failure? Br J Clin Pract.
1995;49:173–176.
17. Varma S, McElnay JC, Hughes CM, Passmore AP, Varma M. Pharma-
ceutical care of patients with congestive heart failure: interventions and
outcomes. Pharmacotherapy. 1999;19:860 – 869.
18. Wakefield BJ, Holman JE, Ray A, Scherubel M, Burns TL, Kienzle MG,
Rosenthal GE. Outcomes of a home telehealth intervention for patients
with heart failure. J Telemed Telecare. 2009;15:46 –50.
19. Gwadry-Sridhar FH, Arnold JM, Zhang Y, Brown JE, Marchiori G,
Guyatt G. Pilot study to determine the impact of a multidisciplinary
educational intervention in patients hospitalized with heart failure. Am
Heart J. 2005;150:982e1–982e9.
20. Rich MW, Gray DB, Beckham V, Wittenberg C, Luther P. Effect of a
multidisciplinary intervention on medication compliance in elderly
patients with congestive heart failure. Am J Med. 1996;101:270 –276.
21. Antonicelli R, Mazzanti I, Abbatecola AM, Parati G. Impact of home
patient telemonitoring on use of beta-blockers in congestive heart failure.
Drugs Aging. 2010;27:801– 805.
22. Bouvy ML, Heerdink ER, Urquhart J, Grobbee DE, Hoes AW, Leufkens
HG. Effect of a pharmacist-led intervention on diuretic compliance in
heart failure patients: a randomized controlled study. J Card Fail. 2003;
9:404 – 411.
23. Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case man-
agement in a heterogeneous congestive heart failure population: a ran-
domized controlled trial. Arch Intern Med. 2003;163:809 – 817.
24. Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, Stroupe KT,
Wu J, Clark D, Smith F, Gradus-Pizlo I, Weinberger M, Brater DC.
Pharmacist intervention to improve medication adherence in heart failure:
a randomized trial. Ann Intern Med. 2007;146:714 –725.
25. Sadik A, Yousif M, McElnay JC. Pharmaceutical care of patients with
heart failure. Br J Clin Pharmacol. 2005;60:183–193.
26. Jerant AF, Azari R, Martinez C, Nesbitt TS. A randomized trial of
telenursing to reduce hospitalization for heart failure: patient-centered
132 Circ Heart Fail January 2012
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
taxonomies is gaining increasing recognition in other areas of
behavioral science that focus on the role self-care in promot-
ing health. 37 Because the content and context of many
adherence-enhancing interventions is not clearly specified in
standardized terminology and theory from behavioral science
is often absent, the approaches to intervention development in
this area can be likened to developing antihypertensive
medications without any understanding of the pharmacology
of the medication, the physiology of systemic blood pressure
control, or the pathophysiology of hypertension. 38
Implications for Practice
There is clearly scope to significantly improve outcomes in
heart failure by enhancing adherence to those existing med-
ications that are known to reduce morbidity and mortality
from heart failure. CHF medication regimens have become
increasingly complex as new treatments have emerged, 6
which provides a challenge for patients with CHF to manage.
Practitioners should consider that developing effective meth-
ods to increase patient adherence to existing medications with
known efficacy could have far greater health benefits than
providing new treatments that may not be followed. 11 The
reviewed studies do provide evidence that enhanced adher-
ence to medications can be achieved in heart failure patients
and that the role of pharmacists may be particularly impor-
tant, in particular, direct communication between patient,
pharmacists, and other health care providers.22,24,25 This
review also suggests that patient education about CHF or
self-management training alone may not be effective. Overall
it is clear, however, that formal recommendations on the best
approaches to enhance adherence to medication in CHF
cannot be derived from the existing studies. New studies with
more clearly justified and specified methodology are required
to generate a cumulative body of findings that could be used
to inform clinical practice. In particular, more explicit use of
behavioral sciences in developing adherence interventions in
CHF is clearly warranted.
Conclusions
It may be possible to improve adherence to medication in
patients with CHF by using a range of strategies; however,
the specification of effective techniques requires greater
clarity in this literature. There is currently limited high-
quality evidence on the effectiveness of interventions that aim
to enhance adherence to medication in typical heart failure
patients, and further research is needed to identify the
optimum strategies for implementation in clinical practice.
Disclosures
None.
References
1. Jhund PS, Macintyre K, Simpson CR, Lewsey JD, Stewart S, Redpath A,
Chalmers JW, Capewell S, McMurray JJ. Long-term trends in first hos-
pitalization for heart failure and subsequent survival between 1986 and
2003: a population study of 5.1 million people. Circulation. 2009;119:
515–523.
2. SOLVD Investigators. Effect of enalapril on survival in patients with
reduced left ventricular ejection fractions and congestive heart failure: the
SOLVD Investigators. N Engl J Med. 1991;325:293–302.
3. Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM,
Shusterman NH. The effect of carvedilol on morbidity and mortality in
patients with chronic heart failure: US Carvedilol Heart Failure Study
Group. N Engl J Med. 1996;334:1349 –1355.
4. Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky
J, Wittes J. The effect of spironolactone on morbidity and mortality in
patients with severe heart failure: Randomized Aldactone Evaluation
Study Investigators. N Engl J Med. 1999;341:709 –717.
5. van der Wal MH, Jaarsma T. Adherence in heart failure in the elderly:
problem and possible solutions. Int J Cardiol. 2008;125:203–208.
6. Hauptman PJ. Medication adherence in heart failure. Heart Fail Rev.
2008;13:99 –106.
7. Butler J, Arbogast PG, Daugherty J, Jain MK, Ray WA, Griffin MR.
Outpatient utilization of angiotensin-converting enzyme inhibitors among
heart failure patients after hospital discharge. J Am Coll Cardiol. 2004;
43:2036 –2043.
8. Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Avorn J. Noncompliance
with congestive heart failure therapy in the elderly. Arch Intern Med.
1994;154:433– 437.
9. Wu JR, Moser DK, De Jong MJ, Rayens MK, Chung ML, Riegel B,
Lennie TA. Defining an evidence-based cutpoint for medication
adherence in heart failure. Am Heart J. 2009;157:285–291.
10. Glynn L, Fahey T. Cardiovascular medication: improving adherence. Clin
Evid (Online). 2011. Available at http://clinicalevidence.bmj.com.
11. Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for
enhancing medication adherence. Cochrane Database Syst Rev. 2008;2:
CD000011.
12. Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to
lipid lowering medication. Cochrane Database Syst Rev. 2010;
CD004371.
13. Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D,
Stewart S, Cleland JG. Structured telephone support or telemonitoring
programmes for patients with chronic heart failure. Cochrane Database
Syst Rev. 2010;8:CD007228.
14. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of
Interventions. Chichester, UK: The Cochrane Collaboration and John
Wiley & Sons Ltd; 2008.
15. Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a
web-based online medical record with electronic communication capa-
bilities to patients with congestive heart failure: randomized trial. J Med
Internet Res. 2004;6:e12.
16. Goodyer LI, Miskelly F, Milligan P. Does encouraging good compliance
improve patients’ clinical condition in heart failure? Br J Clin Pract.
1995;49:173–176.
17. Varma S, McElnay JC, Hughes CM, Passmore AP, Varma M. Pharma-
ceutical care of patients with congestive heart failure: interventions and
outcomes. Pharmacotherapy. 1999;19:860 – 869.
18. Wakefield BJ, Holman JE, Ray A, Scherubel M, Burns TL, Kienzle MG,
Rosenthal GE. Outcomes of a home telehealth intervention for patients
with heart failure. J Telemed Telecare. 2009;15:46 –50.
19. Gwadry-Sridhar FH, Arnold JM, Zhang Y, Brown JE, Marchiori G,
Guyatt G. Pilot study to determine the impact of a multidisciplinary
educational intervention in patients hospitalized with heart failure. Am
Heart J. 2005;150:982e1–982e9.
20. Rich MW, Gray DB, Beckham V, Wittenberg C, Luther P. Effect of a
multidisciplinary intervention on medication compliance in elderly
patients with congestive heart failure. Am J Med. 1996;101:270 –276.
21. Antonicelli R, Mazzanti I, Abbatecola AM, Parati G. Impact of home
patient telemonitoring on use of beta-blockers in congestive heart failure.
Drugs Aging. 2010;27:801– 805.
22. Bouvy ML, Heerdink ER, Urquhart J, Grobbee DE, Hoes AW, Leufkens
HG. Effect of a pharmacist-led intervention on diuretic compliance in
heart failure patients: a randomized controlled study. J Card Fail. 2003;
9:404 – 411.
23. Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case man-
agement in a heterogeneous congestive heart failure population: a ran-
domized controlled trial. Arch Intern Med. 2003;163:809 – 817.
24. Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, Stroupe KT,
Wu J, Clark D, Smith F, Gradus-Pizlo I, Weinberger M, Brater DC.
Pharmacist intervention to improve medication adherence in heart failure:
a randomized trial. Ann Intern Med. 2007;146:714 –725.
25. Sadik A, Yousif M, McElnay JC. Pharmaceutical care of patients with
heart failure. Br J Clin Pharmacol. 2005;60:183–193.
26. Jerant AF, Azari R, Martinez C, Nesbitt TS. A randomized trial of
telenursing to reduce hospitalization for heart failure: patient-centered
132 Circ Heart Fail January 2012
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

outcomes and nursing indicators. Home Health Care Serv Q. 2003;
22:1–20.
27. Fulmer TT, Feldman PH, Kim TS, Carty B, Beers M, Molina M, Putnam
M. An intervention study to enhance medication compliance in
community-dwelling elderly individuals. J Gerontol Nurs. 1999;25:6 –14.
28. Powell LH, Calvin JE Jr, Richardson D, Janssen I, Mendes de Leon CF,
Flynn KJ, Grady KL, Rucker-Whitaker CS, Eaton C, Avery E; HART
Investigators. Self-management counseling in patients with heart failure:
the Heart Failure Adherence and Retention Randomized Behavioral Trial.
JAMA. 2010;304:1331–1338.
29. Tsuyuki RT, Fradette M, Johnson JA, Bungard TJ, Eurich DT, Ashton T,
Gordon W, Ikuta R, Kornder J, Mackay E, Manyari D, O’Reilly K,
Semchuk W. A multicenter disease management program for hospitalized
patients with heart failure. J Card Fail. 2004;10:473– 480.
30. Udelson JE, Pressler SJ, Sackner-Bernstein J, Massaro J, Ordronneau P,
Lukas MA, Hauptman PJ. Adherence with once daily versus twice daily
carvedilol in patients with heart failure: the Compliance And Quality of
Life Study Comparing Once-Daily Controlled-Release Carvedilol CR and
Twice-Daily Immediate-Release Carvedilol IR in Patients with Heart
Failure (CASPER) Trial. J Card Fail. 2009;15:385–393.
31. Conn VS, Hafdahl AR, Cooper PS, Ruppar TM, Mehr DR, Russell CL.
Interventions to improve medication adherence among older adults: meta-
analysis of adherence outcomes among randomized controlled trials.
Gerontologist. 2009;49:447– 462.
32. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations
between dose regimens and medication compliance. Clin Ther. 2001;23:
1296 –1310.
33. van der Wal MH, Jaarsma T, Moser DK, Veeger NJ, van Gilst WH, van
Veldhuisen DJ. Compliance in heart failure patients: the importance of
knowledge and beliefs. Eur Heart J. 2006;27:434 – 440.
34. Molloy GJ, Johnston DW, Witham MD. Family caregiving and con-
gestive heart failure: review and analysis. Eur J Heart Fail. 2005;7:
592– 603.
35. Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support
and self-care of patients with heart failure. Ann Behav Med. 2008;35:
70 –79.
36. Horowitz CR, Rein SB, Leventhal H. A story of maladies, miscon-
ceptions and mishaps: effective management of heart failure. Soc Sci
Med. 2004;58:631– 643.
37. Abraham C, Michie S. A taxonomy of behavior change techniques used
in interventions. Health Psychol. 2008;27:379 –387.
38. Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N. Changing the
behavior of healthcare professionals: the use of theory in promoting the
uptake of research findings. J Clin Epidemiol. 2005;58:107–112.
KEY WORDS: heart failure 䡲 medication adherence 䡲 behavior change 䡲
compliance
Molloy et al Adherence to Medication in Heart Failure Review 133
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
22:1–20.
27. Fulmer TT, Feldman PH, Kim TS, Carty B, Beers M, Molina M, Putnam
M. An intervention study to enhance medication compliance in
community-dwelling elderly individuals. J Gerontol Nurs. 1999;25:6 –14.
28. Powell LH, Calvin JE Jr, Richardson D, Janssen I, Mendes de Leon CF,
Flynn KJ, Grady KL, Rucker-Whitaker CS, Eaton C, Avery E; HART
Investigators. Self-management counseling in patients with heart failure:
the Heart Failure Adherence and Retention Randomized Behavioral Trial.
JAMA. 2010;304:1331–1338.
29. Tsuyuki RT, Fradette M, Johnson JA, Bungard TJ, Eurich DT, Ashton T,
Gordon W, Ikuta R, Kornder J, Mackay E, Manyari D, O’Reilly K,
Semchuk W. A multicenter disease management program for hospitalized
patients with heart failure. J Card Fail. 2004;10:473– 480.
30. Udelson JE, Pressler SJ, Sackner-Bernstein J, Massaro J, Ordronneau P,
Lukas MA, Hauptman PJ. Adherence with once daily versus twice daily
carvedilol in patients with heart failure: the Compliance And Quality of
Life Study Comparing Once-Daily Controlled-Release Carvedilol CR and
Twice-Daily Immediate-Release Carvedilol IR in Patients with Heart
Failure (CASPER) Trial. J Card Fail. 2009;15:385–393.
31. Conn VS, Hafdahl AR, Cooper PS, Ruppar TM, Mehr DR, Russell CL.
Interventions to improve medication adherence among older adults: meta-
analysis of adherence outcomes among randomized controlled trials.
Gerontologist. 2009;49:447– 462.
32. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations
between dose regimens and medication compliance. Clin Ther. 2001;23:
1296 –1310.
33. van der Wal MH, Jaarsma T, Moser DK, Veeger NJ, van Gilst WH, van
Veldhuisen DJ. Compliance in heart failure patients: the importance of
knowledge and beliefs. Eur Heart J. 2006;27:434 – 440.
34. Molloy GJ, Johnston DW, Witham MD. Family caregiving and con-
gestive heart failure: review and analysis. Eur J Heart Fail. 2005;7:
592– 603.
35. Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support
and self-care of patients with heart failure. Ann Behav Med. 2008;35:
70 –79.
36. Horowitz CR, Rein SB, Leventhal H. A story of maladies, miscon-
ceptions and mishaps: effective management of heart failure. Soc Sci
Med. 2004;58:631– 643.
37. Abraham C, Michie S. A taxonomy of behavior change techniques used
in interventions. Health Psychol. 2008;27:379 –387.
38. Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N. Changing the
behavior of healthcare professionals: the use of theory in promoting the
uptake of research findings. J Clin Epidemiol. 2005;58:107–112.
KEY WORDS: heart failure 䡲 medication adherence 䡲 behavior change 䡲
compliance
Molloy et al Adherence to Medication in Heart Failure Review 133
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
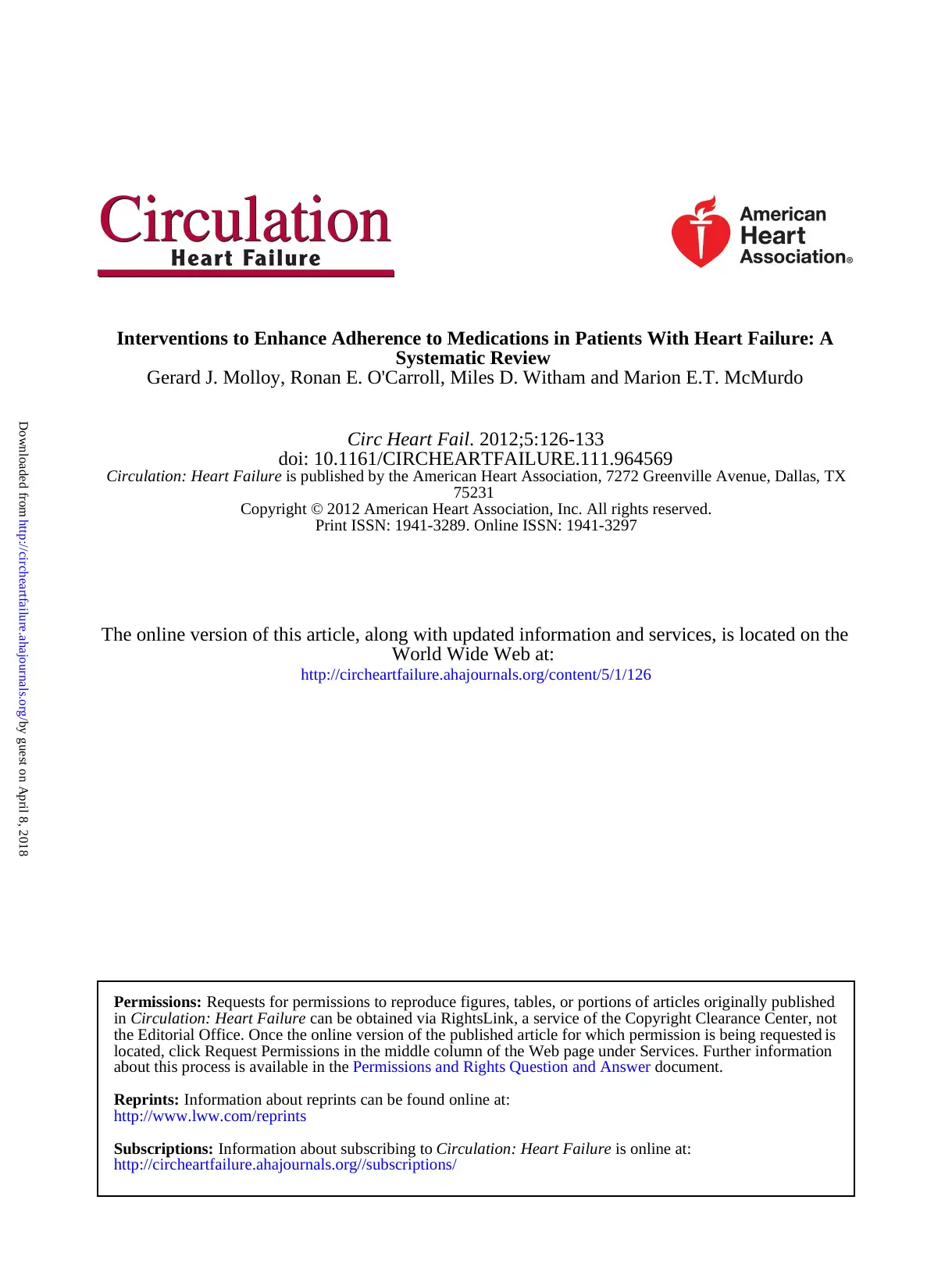
Gerard J. Molloy, Ronan E. O'Carroll, Miles D. Witham and Marion E.T. McMurdo
Systematic Review
Interventions to Enhance Adherence to Medications in Patients With Heart Failure: A
Print ISSN: 1941-3289. Online ISSN: 1941-3297
Copyright © 2012 American Heart Association, Inc. All rights reserved.
75231
is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TXCirculation: Heart Failure
doi: 10.1161/CIRCHEARTFAILURE.111.964569
2012;5:126-133Circ Heart Fail.
http://circheartfailure.ahajournals.org/content/5/1/126
World Wide Web at:
The online version of this article, along with updated information and services, is located on the
http://circheartfailure.ahajournals.org//subscriptions/
is online at:Circulation: Heart FailureInformation about subscribing toSubscriptions:
http://www.lww.com/reprints
Information about reprints can be found online at:Reprints:
document.Permissions and Rights Question and Answerabout this process is available in the
located, click Request Permissions in the middle column of the Web page under Services. Further information
isthe Editorial Office. Once the online version of the published article for which permission is being requested
can be obtained via RightsLink, a service of the Copyright Clearance Center, notCirculation: Heart Failurein Requests for permissions to reproduce figures, tables, or portions of articles originally publishedPermissions:
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
Systematic Review
Interventions to Enhance Adherence to Medications in Patients With Heart Failure: A
Print ISSN: 1941-3289. Online ISSN: 1941-3297
Copyright © 2012 American Heart Association, Inc. All rights reserved.
75231
is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TXCirculation: Heart Failure
doi: 10.1161/CIRCHEARTFAILURE.111.964569
2012;5:126-133Circ Heart Fail.
http://circheartfailure.ahajournals.org/content/5/1/126
World Wide Web at:
The online version of this article, along with updated information and services, is located on the
http://circheartfailure.ahajournals.org//subscriptions/
is online at:Circulation: Heart FailureInformation about subscribing toSubscriptions:
http://www.lww.com/reprints
Information about reprints can be found online at:Reprints:
document.Permissions and Rights Question and Answerabout this process is available in the
located, click Request Permissions in the middle column of the Web page under Services. Further information
isthe Editorial Office. Once the online version of the published article for which permission is being requested
can be obtained via RightsLink, a service of the Copyright Clearance Center, notCirculation: Heart Failurein Requests for permissions to reproduce figures, tables, or portions of articles originally publishedPermissions:
by guest on April 8, 2018http://circheartfailure.ahajournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





