Comprehensive Report on Heart Failure: Causes, Symptoms, and Treatment
VerifiedAdded on 2023/01/09
|9
|1625
|35
Report
AI Summary
This report provides a comprehensive overview of heart failure, a chronic condition where the heart cannot pump enough blood to meet the body's needs. It explores the pathophysiology, detailing how factors like myocardial infarction and hypertension can impair heart muscle efficiency, leading to reduced contraction and reduced cardiac output. The report covers symptoms such as shortness of breath, fatigue, and irregular heartbeat, as well as potential complications. It also discusses various types of heart failure, including systolic and diastolic, and highlights risk factors such as high blood pressure and diabetes. The report emphasizes the importance of lifestyle changes, including diet, exercise, and stress management, alongside medical treatments to manage the condition. The report includes figures and references to support its findings.
Running head: Heart Failure 1
Heart Failure
Name
Institution
Heart Failure
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Heart Failure 2
Heart Failure
This is a chronic disorder in which the heart becomes incapable of pumping sufficient
blood and oxygen so as to meet the body needs. It is a s a result of damaged, stiffened or
weakened heart which in turn cannot keep up with the normal demands of pumping blood. The
body is highly reliant on the action of the heart to pump and deliver blood rich in oxygen and
nutrients to the body cells, therefore a weak or stiff heart cannot complete this function
efficiently. Although not all factors that leads to heart failure are changeable, the treatments
which are available are capable of improving the condition. This disease is very important
because it can result into kidney and liver damage, and valve problems, hence threatening the life
of an individual. One impact of this disease in the community is that it causes disruption on the
daily lives of individuals thereby making them less productive (Fry et al., 2016).
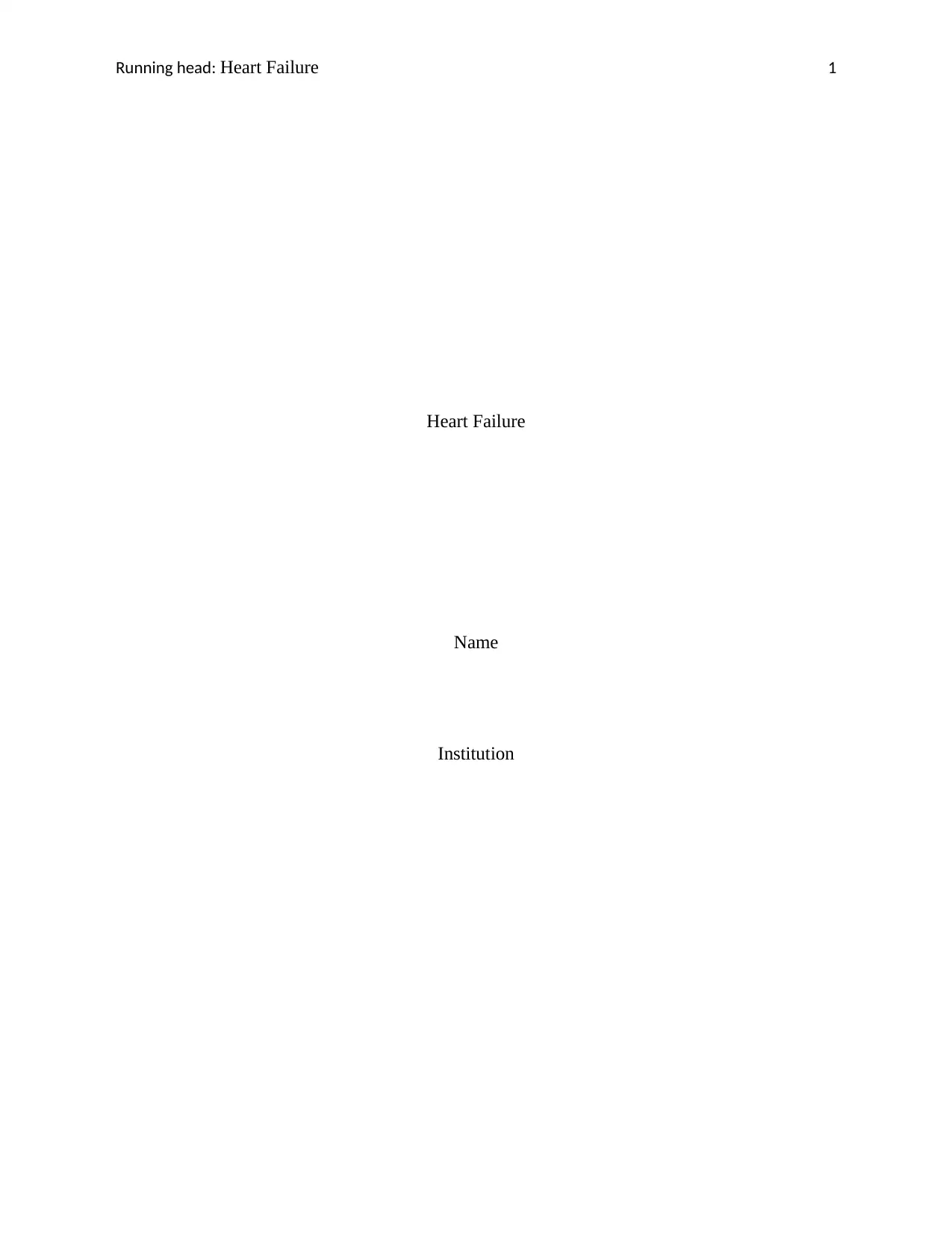
Figure 1: Heart rate of heart failure
Adapted from: https://www.medicographia.com/wp-content/uploads/2012/01/54.JPG
Heart Failure
This is a chronic disorder in which the heart becomes incapable of pumping sufficient
blood and oxygen so as to meet the body needs. It is a s a result of damaged, stiffened or
weakened heart which in turn cannot keep up with the normal demands of pumping blood. The
body is highly reliant on the action of the heart to pump and deliver blood rich in oxygen and
nutrients to the body cells, therefore a weak or stiff heart cannot complete this function
efficiently. Although not all factors that leads to heart failure are changeable, the treatments
which are available are capable of improving the condition. This disease is very important
because it can result into kidney and liver damage, and valve problems, hence threatening the life
of an individual. One impact of this disease in the community is that it causes disruption on the
daily lives of individuals thereby making them less productive (Fry et al., 2016).
Figure 1: Heart rate of heart failure
Adapted from: https://www.medicographia.com/wp-content/uploads/2012/01/54.JPG
Heart Failure 3
Pathophysiology of Heart Failure
Since heart failure can be due to myocardial infarction, hypertension, and amyloidosis,
the main pathophysiology is a decrease in the efficiency of the muscles of the heart which causes
an overload or damage. With time, these overloads lead to the reduced force of contraction
within the ventricles. The over-stretching of the heart muscles reduces the capacity of the heart to
cross-link the myosin and actin filaments. According to Savarese and Lund (2017), heart failure
can result from any auxiliary or practical cardiovascular turmoil which debilitates the capacity of
the ventricle to fill with or eject blood. Heart failure is as a result of effects on the cardiac output.
Kemp and Conte (2012) argue that low stroke volume may lead to the failure of the diastole or
systole while high output may lead to low systemic vascular resistance, peripheral shunting and
hyperthyroidism. The essential functions of the heart are secured by the integration of its
electrical and mechanical functions and therefore changes in the structure of the heart such as
valvular dysfunction may result into an overload of heart pressure or volume. The factors that
affect the cardiac output include the preload which is the volume of blood or amount of fiber
which stretches in the ventricles at the end of the diastole, afterload which is the resistance
against which the ventricle must pump, contractility which is the heart muscle’s ability to
contract and relate to the strength of contraction (Mathews, & Schweighardt, 2017). In order to
uphold normal cardiac output, several compensatory mechanisms play the role of compensatory
enlargement in the form of cardiac hypertrophy and cardiac dilation. The compensatory
mechanisms may restore the cardiac output to near normal, however, if excessive, they may
worsen the heart failure due to vasoconstriction and excessive tachycardia. The Starling’s Law
portrays the connection among preload and cardiovascular yield by expressing that the more
prominent the heart muscle filaments are extended as a result of increments in volume, the more
Pathophysiology of Heart Failure
Since heart failure can be due to myocardial infarction, hypertension, and amyloidosis,
the main pathophysiology is a decrease in the efficiency of the muscles of the heart which causes
an overload or damage. With time, these overloads lead to the reduced force of contraction
within the ventricles. The over-stretching of the heart muscles reduces the capacity of the heart to
cross-link the myosin and actin filaments. According to Savarese and Lund (2017), heart failure
can result from any auxiliary or practical cardiovascular turmoil which debilitates the capacity of
the ventricle to fill with or eject blood. Heart failure is as a result of effects on the cardiac output.
Kemp and Conte (2012) argue that low stroke volume may lead to the failure of the diastole or
systole while high output may lead to low systemic vascular resistance, peripheral shunting and
hyperthyroidism. The essential functions of the heart are secured by the integration of its
electrical and mechanical functions and therefore changes in the structure of the heart such as
valvular dysfunction may result into an overload of heart pressure or volume. The factors that
affect the cardiac output include the preload which is the volume of blood or amount of fiber
which stretches in the ventricles at the end of the diastole, afterload which is the resistance
against which the ventricle must pump, contractility which is the heart muscle’s ability to
contract and relate to the strength of contraction (Mathews, & Schweighardt, 2017). In order to
uphold normal cardiac output, several compensatory mechanisms play the role of compensatory
enlargement in the form of cardiac hypertrophy and cardiac dilation. The compensatory
mechanisms may restore the cardiac output to near normal, however, if excessive, they may
worsen the heart failure due to vasoconstriction and excessive tachycardia. The Starling’s Law
portrays the connection among preload and cardiovascular yield by expressing that the more
prominent the heart muscle filaments are extended as a result of increments in volume, the more
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Heart Failure 4
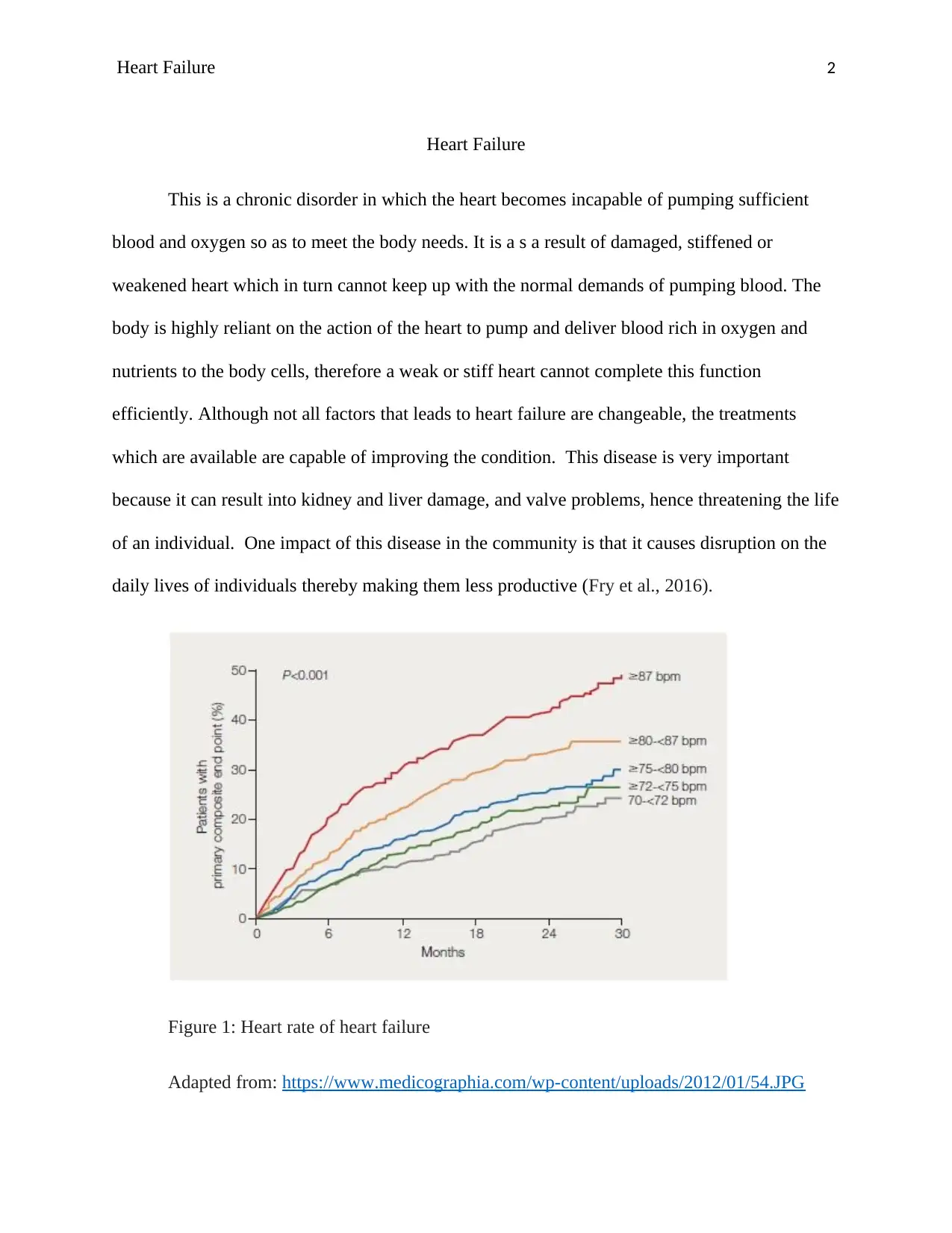
prominent their ensuing power of compression yet just to a limited extent. Past that point, strands
get over-extended and the power of compression is diminished (Arques, and Ambrosi, 2011).
This is accomplished by expanding the dimension of sarcomeres in the enlarged heart just as
expanding the myocardial contractility which endeavors to keep up the stroke volume. Heart
failure causes depression of ventricular function curve which may lead to compensation due to
the stretching of myocardial fibres. According to Tanai and Frantz (2011), stretching results into
dilatation which happens when the left ventricle does not to eject its normal end diastolic
volume. It is important to note that failing ventricle requires higher end-diastolic volume so as to
achieve the same cardiac output that normal ventricle achieves with lower ventricular volumes.
Figure 2: Pathophysiology of heart failure.
Adapted from: https://www.researchgate.net/profile/Rudolf_De_Boer2/publication/263320761/
figure/fig1/AS:296515248640003@1447706152851/Pathophysiology-of-heart-failure-which-is-
reflected-by-different-biomarkers.png
prominent their ensuing power of compression yet just to a limited extent. Past that point, strands
get over-extended and the power of compression is diminished (Arques, and Ambrosi, 2011).
This is accomplished by expanding the dimension of sarcomeres in the enlarged heart just as
expanding the myocardial contractility which endeavors to keep up the stroke volume. Heart
failure causes depression of ventricular function curve which may lead to compensation due to
the stretching of myocardial fibres. According to Tanai and Frantz (2011), stretching results into
dilatation which happens when the left ventricle does not to eject its normal end diastolic
volume. It is important to note that failing ventricle requires higher end-diastolic volume so as to
achieve the same cardiac output that normal ventricle achieves with lower ventricular volumes.
Figure 2: Pathophysiology of heart failure.
Adapted from: https://www.researchgate.net/profile/Rudolf_De_Boer2/publication/263320761/
figure/fig1/AS:296515248640003@1447706152851/Pathophysiology-of-heart-failure-which-is-
reflected-by-different-biomarkers.png
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Heart Failure 5
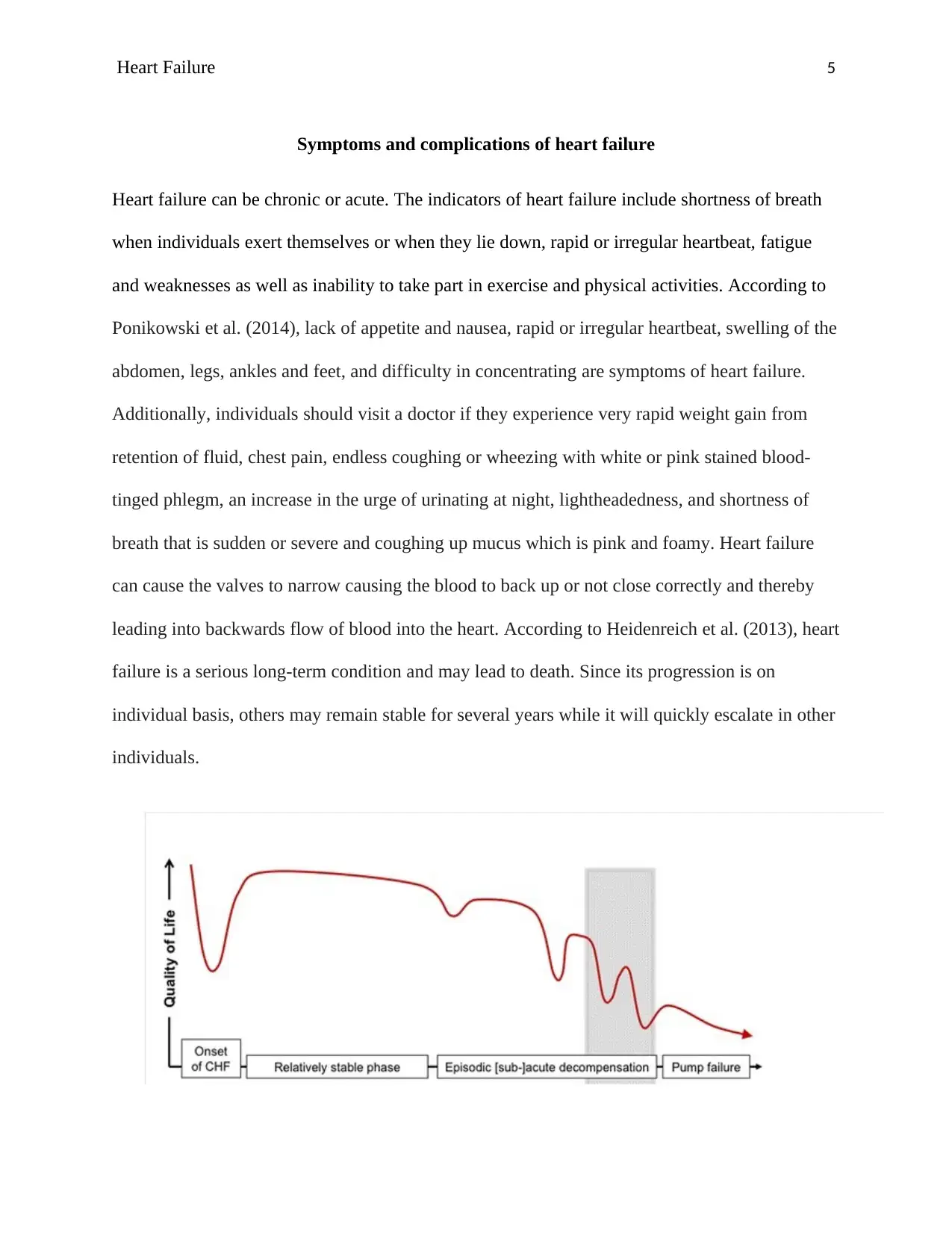
Symptoms and complications of heart failure
Heart failure can be chronic or acute. The indicators of heart failure include shortness of breath
when individuals exert themselves or when they lie down, rapid or irregular heartbeat, fatigue
and weaknesses as well as inability to take part in exercise and physical activities. According to
Ponikowski et al. (2014), lack of appetite and nausea, rapid or irregular heartbeat, swelling of the
abdomen, legs, ankles and feet, and difficulty in concentrating are symptoms of heart failure.
Additionally, individuals should visit a doctor if they experience very rapid weight gain from
retention of fluid, chest pain, endless coughing or wheezing with white or pink stained blood-
tinged phlegm, an increase in the urge of urinating at night, lightheadedness, and shortness of
breath that is sudden or severe and coughing up mucus which is pink and foamy. Heart failure
can cause the valves to narrow causing the blood to back up or not close correctly and thereby
leading into backwards flow of blood into the heart. According to Heidenreich et al. (2013), heart
failure is a serious long-term condition and may lead to death. Since its progression is on
individual basis, others may remain stable for several years while it will quickly escalate in other
individuals.
Symptoms and complications of heart failure
Heart failure can be chronic or acute. The indicators of heart failure include shortness of breath
when individuals exert themselves or when they lie down, rapid or irregular heartbeat, fatigue
and weaknesses as well as inability to take part in exercise and physical activities. According to
Ponikowski et al. (2014), lack of appetite and nausea, rapid or irregular heartbeat, swelling of the
abdomen, legs, ankles and feet, and difficulty in concentrating are symptoms of heart failure.
Additionally, individuals should visit a doctor if they experience very rapid weight gain from
retention of fluid, chest pain, endless coughing or wheezing with white or pink stained blood-
tinged phlegm, an increase in the urge of urinating at night, lightheadedness, and shortness of
breath that is sudden or severe and coughing up mucus which is pink and foamy. Heart failure
can cause the valves to narrow causing the blood to back up or not close correctly and thereby
leading into backwards flow of blood into the heart. According to Heidenreich et al. (2013), heart
failure is a serious long-term condition and may lead to death. Since its progression is on
individual basis, others may remain stable for several years while it will quickly escalate in other
individuals.
Heart Failure 6
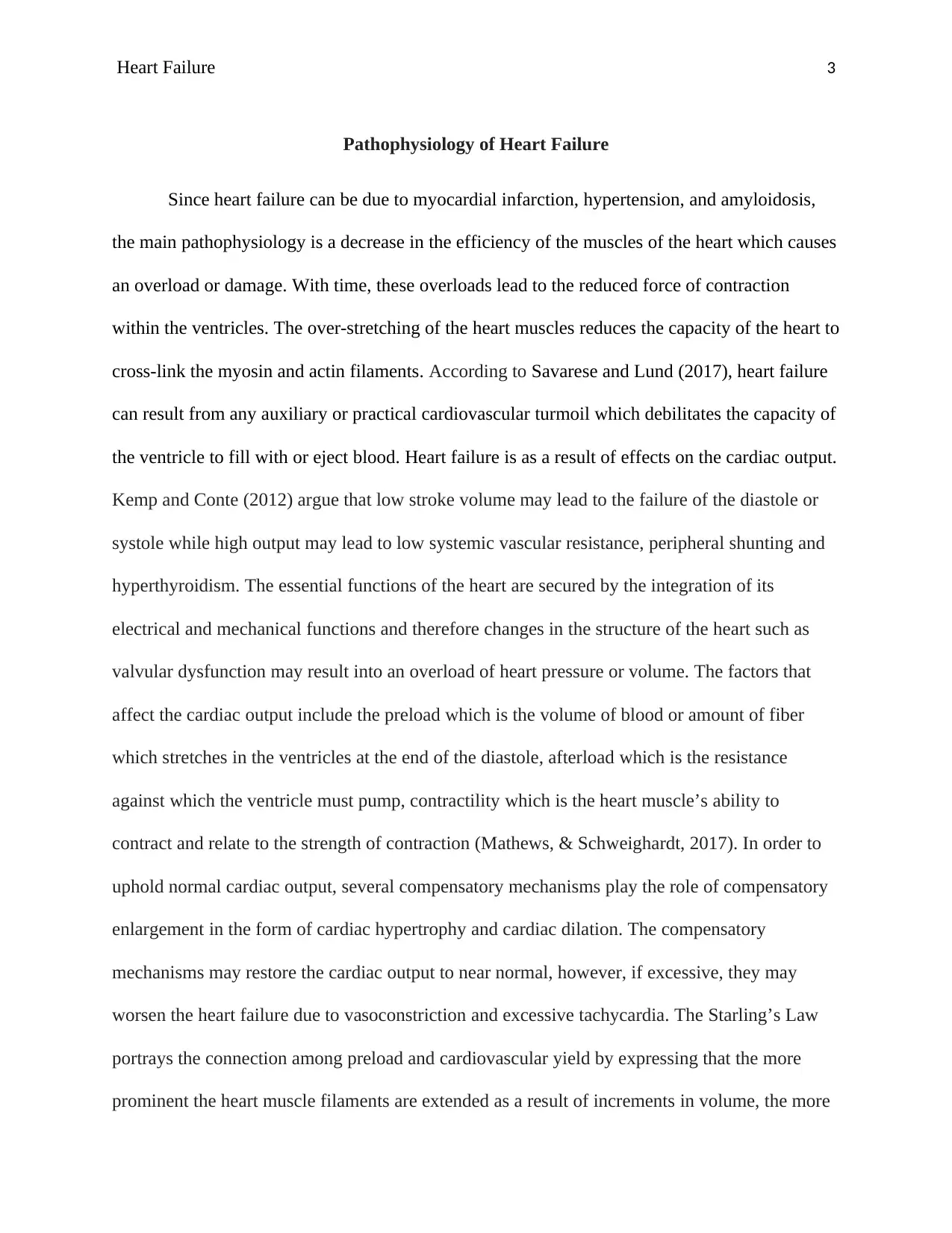
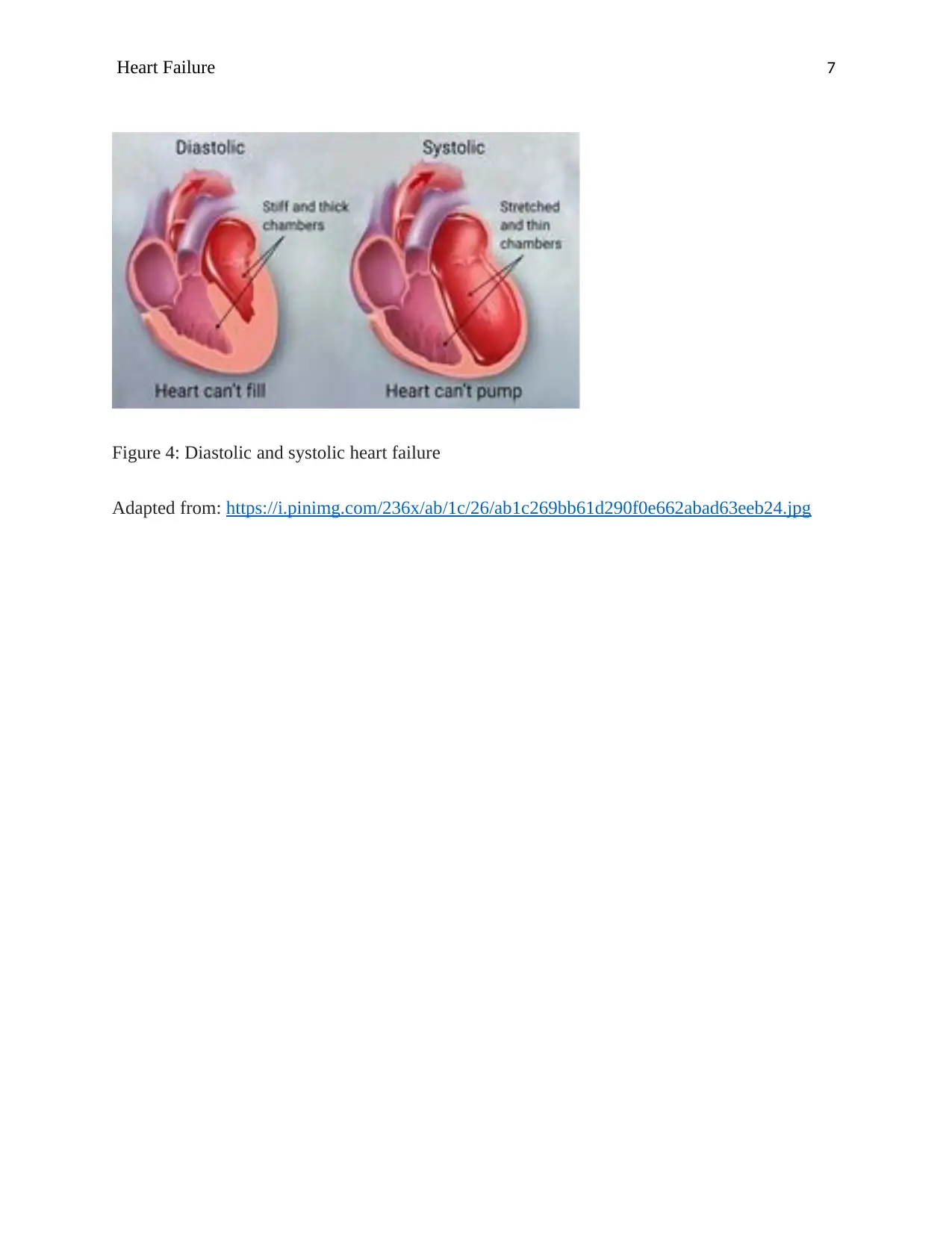
Figure 3: Progression of heart failure
Adapted from: https://www.radiometer.co.uk/-/media/radiometer/corporate/images/page/
products/heart-failure-illustration-1.jpg?la=en-GB
Precis
Heart failure is a condition that stems from the damage of heart muscles, making them
weak and unable to properly pump blood. Heart failure damages can also be as a result of lasting
illnesses like high blood pressure, diabetes, heart diseases or even heart attack. There are
different types of heart failure, these include systolic, left-sided, right-sided and diastolic heart
failures. It is also essential to note that heart failure can also be caused by cardiomyopathy. The
heart failure risk factors are high blood pressure, obesity, diabetes, certain medications as well as
coronary artery diseases. Additionally, people with heart failure may also risk congenital heart
defects, sleep apnea, irregular heartbeat, use of tobacco as well as use of alcohol. To help control
or eliminate the risk factors associated with heart failure, individuals must be willing to make
tremendous changes in their lifestyles. These include staying physically active, learning how to
reduce and manage stress, eating healthy foods and quitting smoking. Furthermore, individuals
with hear failure should limit alcohol, caffeine and consume less salt. People thought to be
having heart failure undergo through blood and breathing tests, echocardiogram,
electrocardiogram, and x-ray scans so as to create a full diagnosis.
Figure 3: Progression of heart failure
Adapted from: https://www.radiometer.co.uk/-/media/radiometer/corporate/images/page/
products/heart-failure-illustration-1.jpg?la=en-GB
Precis
Heart failure is a condition that stems from the damage of heart muscles, making them
weak and unable to properly pump blood. Heart failure damages can also be as a result of lasting
illnesses like high blood pressure, diabetes, heart diseases or even heart attack. There are
different types of heart failure, these include systolic, left-sided, right-sided and diastolic heart
failures. It is also essential to note that heart failure can also be caused by cardiomyopathy. The
heart failure risk factors are high blood pressure, obesity, diabetes, certain medications as well as
coronary artery diseases. Additionally, people with heart failure may also risk congenital heart
defects, sleep apnea, irregular heartbeat, use of tobacco as well as use of alcohol. To help control
or eliminate the risk factors associated with heart failure, individuals must be willing to make
tremendous changes in their lifestyles. These include staying physically active, learning how to
reduce and manage stress, eating healthy foods and quitting smoking. Furthermore, individuals
with hear failure should limit alcohol, caffeine and consume less salt. People thought to be
having heart failure undergo through blood and breathing tests, echocardiogram,
electrocardiogram, and x-ray scans so as to create a full diagnosis.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Heart Failure 7
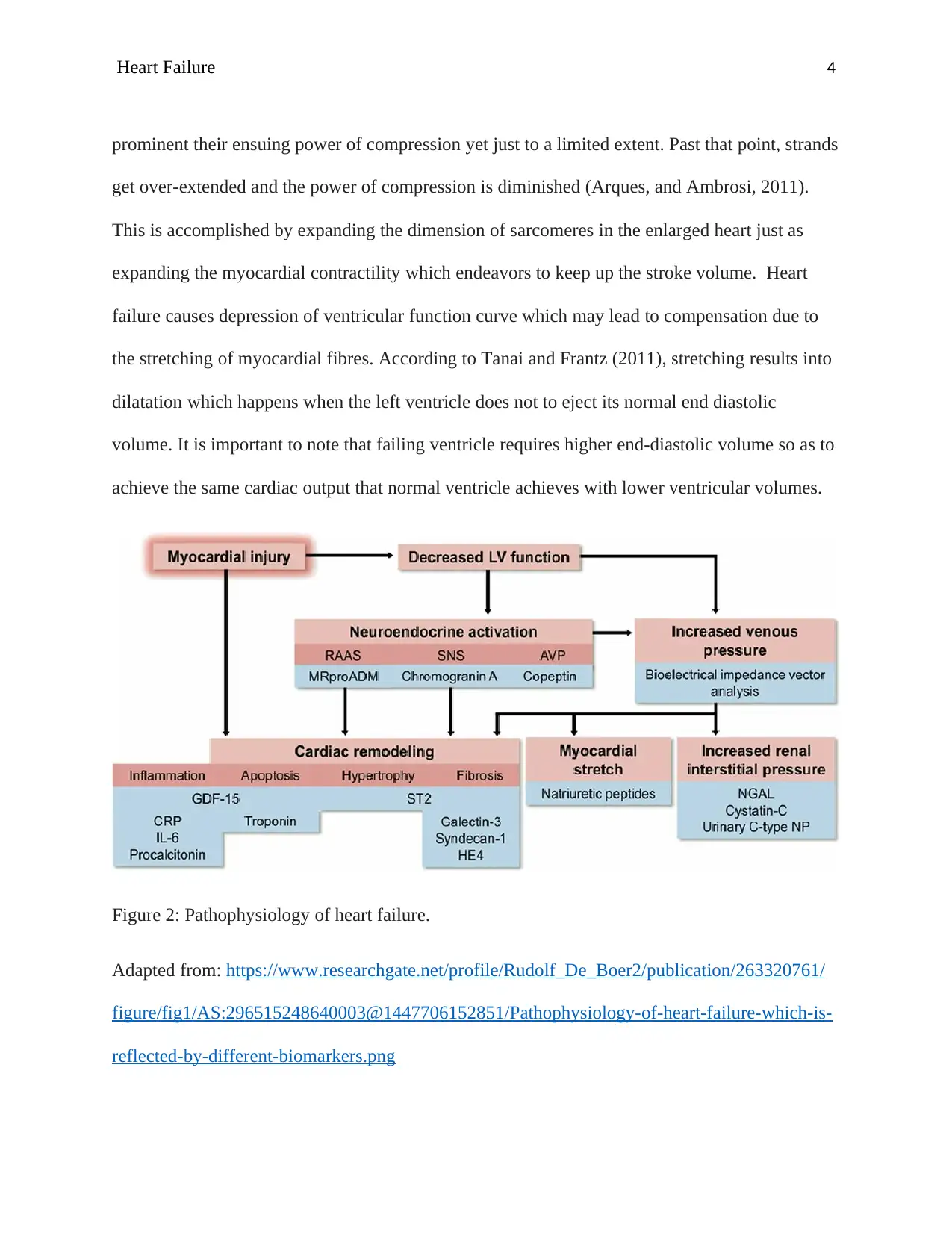
Figure 4: Diastolic and systolic heart failure
Adapted from: https://i.pinimg.com/236x/ab/1c/26/ab1c269bb61d290f0e662abad63eeb24.jpg
Figure 4: Diastolic and systolic heart failure
Adapted from: https://i.pinimg.com/236x/ab/1c/26/ab1c269bb61d290f0e662abad63eeb24.jpg
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Heart Failure 8
References
Arques, S., & Ambrosi, P. (2011). Human serum albumin in the clinical syndrome of heart
failure. Journal of cardiac failure, 17(6), 451-458.
Fry, M., McLachlan, S., Purdy, S., Sanders, T., Kadam, U. T., & Chew-Graham, C. A. (2016).
The implications of living with heart failure; the impact on everyday life, family support,
co-morbidities and access to healthcare: a secondary qualitative analysis. BMC family
practice, 17(1), 139. https://doi.org/10.1186/s12875-016-0537-5
Kemp, C. D., & Conte, J. V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-371. https://doi.org/10.1016/j.carpath.2011.11.007
Mathews, J. L., & Schweighardt, A. (2017). The Role of Natriuretic Peptides in the
Pathophysiology and Treatment of Heart Failure. In Emerging Applications,
Perspectives, and Discoveries in Cardiovascular Research (pp. 1-16). IGI Global.
Ponikowski, P., Anker, S. D., AlHabib, K. F., Cowie, M. R., Force, T. L., Hu, S., ... & Samal, U.
C. (2014). Heart failure: preventing disease and death worldwide. ESC Heart
Failure, 1(1), 4-25.
Tanai, E., & Frantz, S. (2011). Pathophysiology of heart failure. Comprehensive
physiology, 6(1), 187-214. https://doi.org/10.1002/cphy.c140055
Heidenreich, P. A., Albert, N. M., Allen, L. A., Bluemke, D. A., Butler, J., Fonarow, G. C., ... &
Nichol, G. (2013). Forecasting the impact of heart failure in the United States: a policy
statement from the American Heart Association. Circulation: Heart Failure, 6(3), 606-
619.
References
Arques, S., & Ambrosi, P. (2011). Human serum albumin in the clinical syndrome of heart
failure. Journal of cardiac failure, 17(6), 451-458.
Fry, M., McLachlan, S., Purdy, S., Sanders, T., Kadam, U. T., & Chew-Graham, C. A. (2016).
The implications of living with heart failure; the impact on everyday life, family support,
co-morbidities and access to healthcare: a secondary qualitative analysis. BMC family
practice, 17(1), 139. https://doi.org/10.1186/s12875-016-0537-5
Kemp, C. D., & Conte, J. V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-371. https://doi.org/10.1016/j.carpath.2011.11.007
Mathews, J. L., & Schweighardt, A. (2017). The Role of Natriuretic Peptides in the
Pathophysiology and Treatment of Heart Failure. In Emerging Applications,
Perspectives, and Discoveries in Cardiovascular Research (pp. 1-16). IGI Global.
Ponikowski, P., Anker, S. D., AlHabib, K. F., Cowie, M. R., Force, T. L., Hu, S., ... & Samal, U.
C. (2014). Heart failure: preventing disease and death worldwide. ESC Heart
Failure, 1(1), 4-25.
Tanai, E., & Frantz, S. (2011). Pathophysiology of heart failure. Comprehensive
physiology, 6(1), 187-214. https://doi.org/10.1002/cphy.c140055
Heidenreich, P. A., Albert, N. M., Allen, L. A., Bluemke, D. A., Butler, J., Fonarow, G. C., ... &
Nichol, G. (2013). Forecasting the impact of heart failure in the United States: a policy
statement from the American Heart Association. Circulation: Heart Failure, 6(3), 606-
619.

Heart Failure 9
Savarese, G., & Lund, L. H. (2017). Global public health burden of heart failure. Cardiac failure
review, 3(1), 7.
Savarese, G., & Lund, L. H. (2017). Global public health burden of heart failure. Cardiac failure
review, 3(1), 7.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





