NURSING ASSIGNMENT 13: Assessing and Managing HHS in Elderly Patients
VerifiedAdded on 2022/09/29
|16
|2676
|31
Report
AI Summary
This nursing assignment presents a comprehensive overview of Hyperosmolar Hyperglycemic Syndrome (HHS), focusing on the case of Mr. Stan Coombe, a 76-year-old patient with type 2 diabetes mellitus, pneumonia, and a urinary tract infection. The report begins with an introduction to HHS, detailing its characteristics and common causes, followed by an ISBAR handover providing a clear patient situation, background, assessment, and recommendations. The pathophysiology of HHS is explained, highlighting the mechanisms behind hyperglycemia and hyperosmolarity. The report then discusses multidisciplinary care, identifying the main problems, goals of care, and outlining both medical and nursing interventions. Medical care includes airway management, intravenous access, and aggressive fluid resuscitation, while nursing care emphasizes the importance of assessing precipitating factors, monitoring vital signs, and providing laboratory studies. The report concludes by emphasizing the need for prompt treatment, including intravenous fluids and insulin, to address dehydration and hyperglycemia. References to relevant medical literature are included to support the information presented.
NURSING ASSIGNMENT 1
NURSING ASSIGNMENT
By:
Professor’s Name:
College:
Course:
Date:
NURSING ASSIGNMENT
By:
Professor’s Name:
College:
Course:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT 2
Contents
Introduction...........................................................................................................................................3
ISBAR Handover.....................................................................................................................................4
Pathophysiology....................................................................................................................................6
Multidisciplinary care............................................................................................................................7
Main problems..................................................................................................................................7
Goals of care......................................................................................................................................8
Medical care......................................................................................................................................8
Nursing care.....................................................................................................................................10
Conclusion...........................................................................................................................................13
References...........................................................................................................................................14
Contents
Introduction...........................................................................................................................................3
ISBAR Handover.....................................................................................................................................4
Pathophysiology....................................................................................................................................6
Multidisciplinary care............................................................................................................................7
Main problems..................................................................................................................................7
Goals of care......................................................................................................................................8
Medical care......................................................................................................................................8
Nursing care.....................................................................................................................................10
Conclusion...........................................................................................................................................13
References...........................................................................................................................................14
NURSING ASSIGNMENT 3
Introduction
The hyperosmolar hyperglycaemic state is a diabetes mellitus (DM) metabolic complexity
described by serious hyperglycemia, hyperosmolar plasma, altered consciousness and
outrageous lack of hydration. Often, it occurs in type 2 DM, frequently in the setting of
physiologic pressure (Kitabchi, Umpierrez and Murphy 2015).
Hyperosmolar Hyperglycaemic was recently named hyperosmolar hyperglycaemic
nonketotic coma, however, the name was changed because less than 20% of patients with
HHS have coma.
The hyperosmolar hyperglycaemic syndrome is most regularly found in patients with type
2 DM with reduced fluid intake as seen in Mr. Stan Coombe who is experiencing increased
dehydration (Urden, Stacy and Lough 2017).
Regular manifestations of Hyperosmolar hyperglycaemic syndrome include blood glucose
levels more than 600 mg/dl, outrageous thirst, high blood pressure, perplexity or languor, dry
mouth, fever and skin that is dry and warm.
Introduction
The hyperosmolar hyperglycaemic state is a diabetes mellitus (DM) metabolic complexity
described by serious hyperglycemia, hyperosmolar plasma, altered consciousness and
outrageous lack of hydration. Often, it occurs in type 2 DM, frequently in the setting of
physiologic pressure (Kitabchi, Umpierrez and Murphy 2015).
Hyperosmolar Hyperglycaemic was recently named hyperosmolar hyperglycaemic
nonketotic coma, however, the name was changed because less than 20% of patients with
HHS have coma.
The hyperosmolar hyperglycaemic syndrome is most regularly found in patients with type
2 DM with reduced fluid intake as seen in Mr. Stan Coombe who is experiencing increased
dehydration (Urden, Stacy and Lough 2017).
Regular manifestations of Hyperosmolar hyperglycaemic syndrome include blood glucose
levels more than 600 mg/dl, outrageous thirst, high blood pressure, perplexity or languor, dry
mouth, fever and skin that is dry and warm.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING ASSIGNMENT 4
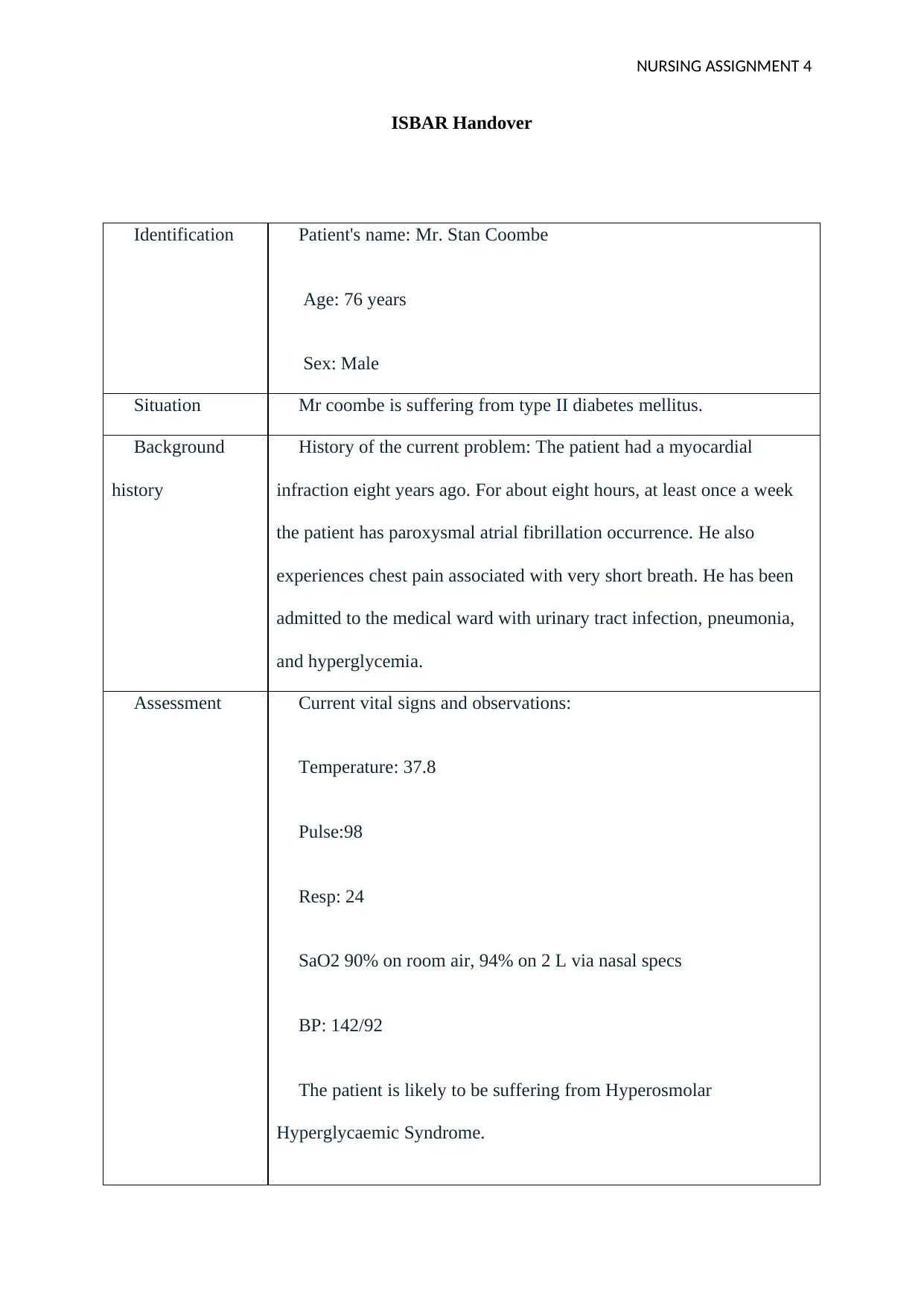
ISBAR Handover
Identification Patient's name: Mr. Stan Coombe
Age: 76 years
Sex: Male
Situation Mr coombe is suffering from type II diabetes mellitus.
Background
history
History of the current problem: The patient had a myocardial
infraction eight years ago. For about eight hours, at least once a week
the patient has paroxysmal atrial fibrillation occurrence. He also
experiences chest pain associated with very short breath. He has been
admitted to the medical ward with urinary tract infection, pneumonia,
and hyperglycemia.
Assessment Current vital signs and observations:
Temperature: 37.8
Pulse:98
Resp: 24
SaO2 90% on room air, 94% on 2 L via nasal specs
BP: 142/92
The patient is likely to be suffering from Hyperosmolar
Hyperglycaemic Syndrome.
ISBAR Handover
Identification Patient's name: Mr. Stan Coombe
Age: 76 years
Sex: Male
Situation Mr coombe is suffering from type II diabetes mellitus.
Background
history
History of the current problem: The patient had a myocardial
infraction eight years ago. For about eight hours, at least once a week
the patient has paroxysmal atrial fibrillation occurrence. He also
experiences chest pain associated with very short breath. He has been
admitted to the medical ward with urinary tract infection, pneumonia,
and hyperglycemia.
Assessment Current vital signs and observations:
Temperature: 37.8
Pulse:98
Resp: 24
SaO2 90% on room air, 94% on 2 L via nasal specs
BP: 142/92
The patient is likely to be suffering from Hyperosmolar
Hyperglycaemic Syndrome.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT 5
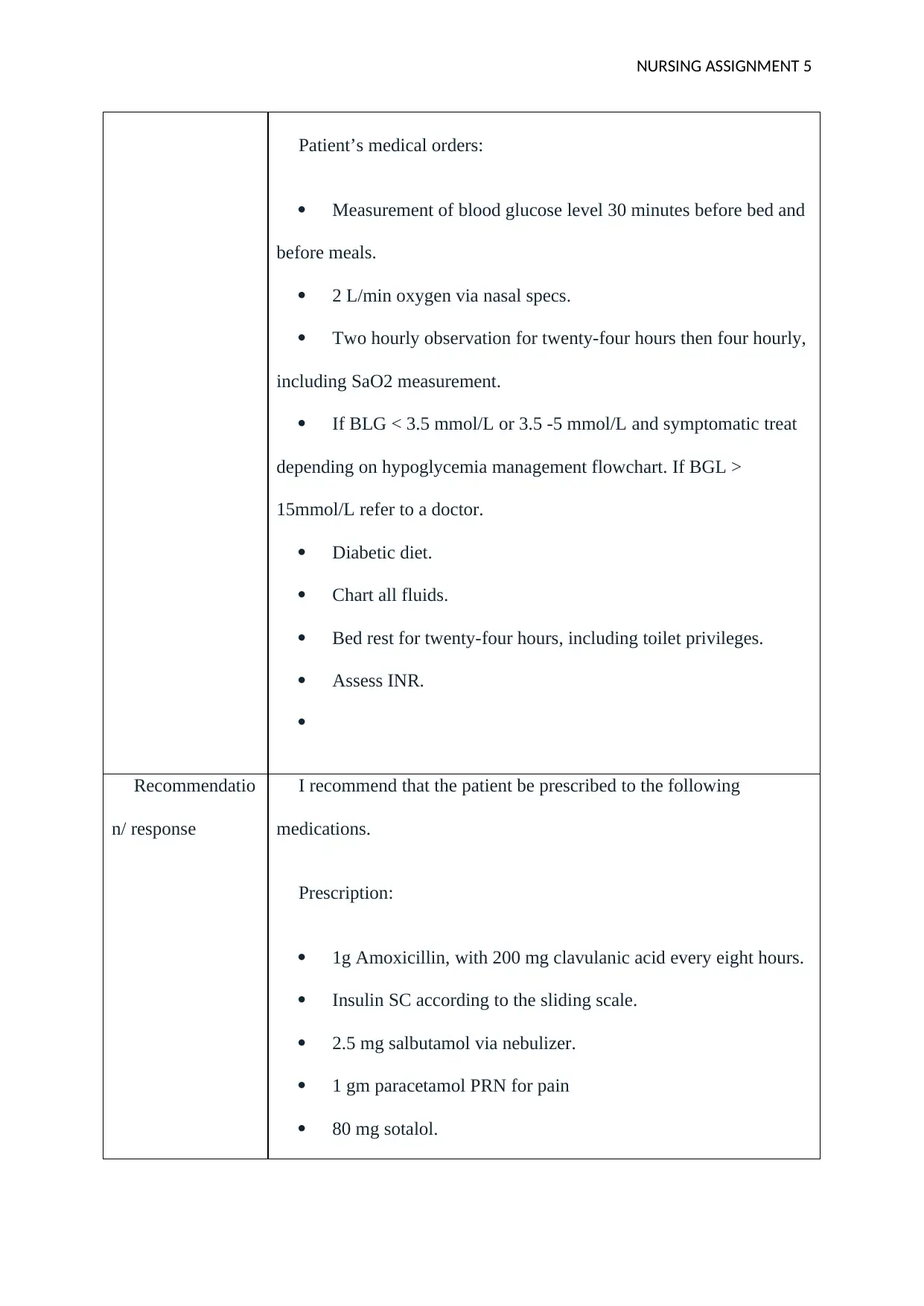
Patient’s medical orders:
Measurement of blood glucose level 30 minutes before bed and
before meals.
2 L/min oxygen via nasal specs.
Two hourly observation for twenty-four hours then four hourly,
including SaO2 measurement.
If BLG < 3.5 mmol/L or 3.5 -5 mmol/L and symptomatic treat
depending on hypoglycemia management flowchart. If BGL >
15mmol/L refer to a doctor.
Diabetic diet.
Chart all fluids.
Bed rest for twenty-four hours, including toilet privileges.
Assess INR.
Recommendatio
n/ response
I recommend that the patient be prescribed to the following
medications.
Prescription:
1g Amoxicillin, with 200 mg clavulanic acid every eight hours.
Insulin SC according to the sliding scale.
2.5 mg salbutamol via nebulizer.
1 gm paracetamol PRN for pain
80 mg sotalol.
Patient’s medical orders:
Measurement of blood glucose level 30 minutes before bed and
before meals.
2 L/min oxygen via nasal specs.
Two hourly observation for twenty-four hours then four hourly,
including SaO2 measurement.
If BLG < 3.5 mmol/L or 3.5 -5 mmol/L and symptomatic treat
depending on hypoglycemia management flowchart. If BGL >
15mmol/L refer to a doctor.
Diabetic diet.
Chart all fluids.
Bed rest for twenty-four hours, including toilet privileges.
Assess INR.
Recommendatio
n/ response
I recommend that the patient be prescribed to the following
medications.
Prescription:
1g Amoxicillin, with 200 mg clavulanic acid every eight hours.
Insulin SC according to the sliding scale.
2.5 mg salbutamol via nebulizer.
1 gm paracetamol PRN for pain
80 mg sotalol.
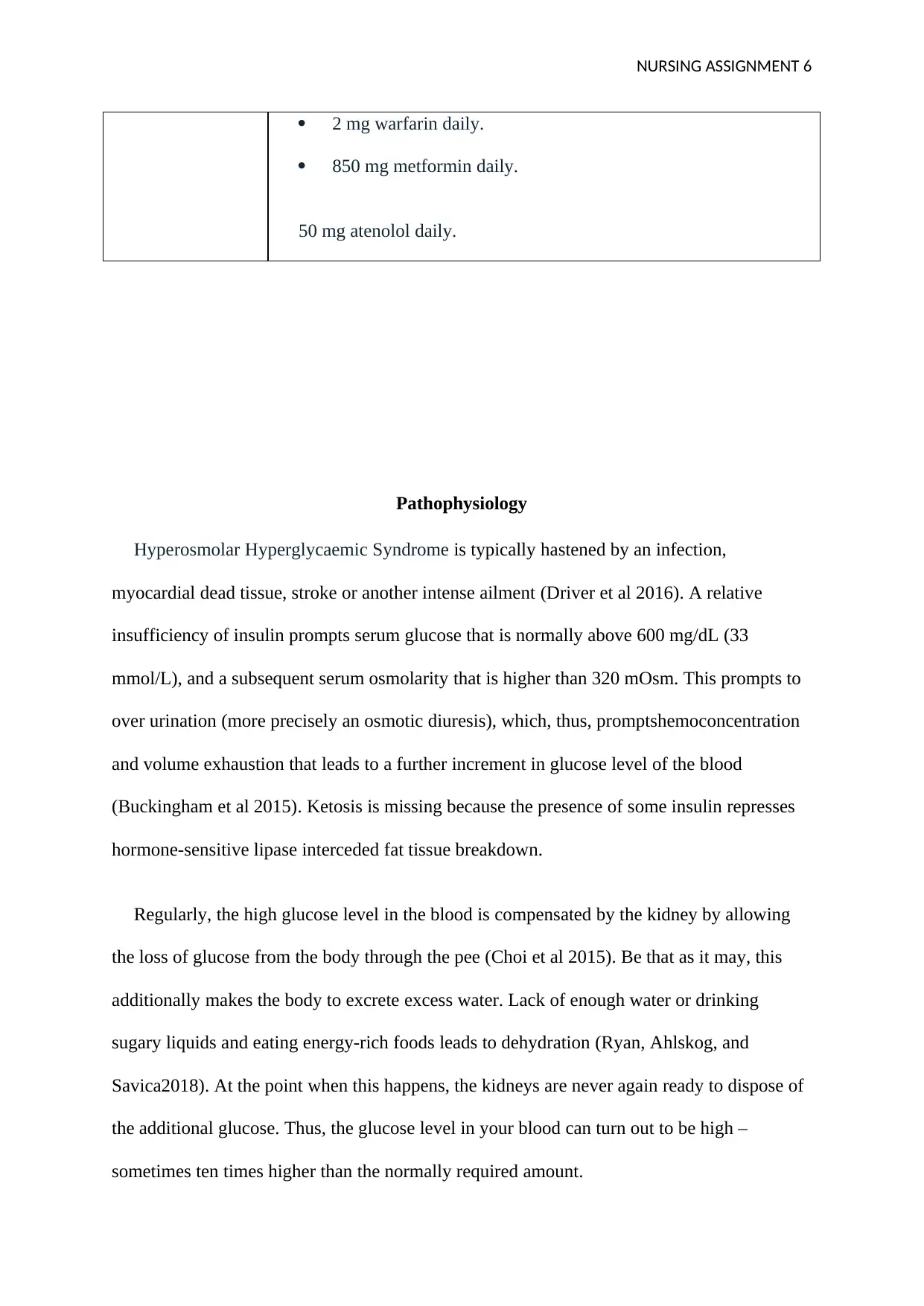
NURSING ASSIGNMENT 6
2 mg warfarin daily.
850 mg metformin daily.
50 mg atenolol daily.
Pathophysiology
Hyperosmolar Hyperglycaemic Syndrome is typically hastened by an infection,
myocardial dead tissue, stroke or another intense ailment (Driver et al 2016). A relative
insufficiency of insulin prompts serum glucose that is normally above 600 mg/dL (33
mmol/L), and a subsequent serum osmolarity that is higher than 320 mOsm. This prompts to
over urination (more precisely an osmotic diuresis), which, thus, promptshemoconcentration
and volume exhaustion that leads to a further increment in glucose level of the blood
(Buckingham et al 2015). Ketosis is missing because the presence of some insulin represses
hormone-sensitive lipase interceded fat tissue breakdown.
Regularly, the high glucose level in the blood is compensated by the kidney by allowing
the loss of glucose from the body through the pee (Choi et al 2015). Be that as it may, this
additionally makes the body to excrete excess water. Lack of enough water or drinking
sugary liquids and eating energy-rich foods leads to dehydration (Ryan, Ahlskog, and
Savica2018). At the point when this happens, the kidneys are never again ready to dispose of
the additional glucose. Thus, the glucose level in your blood can turn out to be high –
sometimes ten times higher than the normally required amount.
2 mg warfarin daily.
850 mg metformin daily.
50 mg atenolol daily.
Pathophysiology
Hyperosmolar Hyperglycaemic Syndrome is typically hastened by an infection,
myocardial dead tissue, stroke or another intense ailment (Driver et al 2016). A relative
insufficiency of insulin prompts serum glucose that is normally above 600 mg/dL (33
mmol/L), and a subsequent serum osmolarity that is higher than 320 mOsm. This prompts to
over urination (more precisely an osmotic diuresis), which, thus, promptshemoconcentration
and volume exhaustion that leads to a further increment in glucose level of the blood
(Buckingham et al 2015). Ketosis is missing because the presence of some insulin represses
hormone-sensitive lipase interceded fat tissue breakdown.
Regularly, the high glucose level in the blood is compensated by the kidney by allowing
the loss of glucose from the body through the pee (Choi et al 2015). Be that as it may, this
additionally makes the body to excrete excess water. Lack of enough water or drinking
sugary liquids and eating energy-rich foods leads to dehydration (Ryan, Ahlskog, and
Savica2018). At the point when this happens, the kidneys are never again ready to dispose of
the additional glucose. Thus, the glucose level in your blood can turn out to be high –
sometimes ten times higher than the normally required amount.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING ASSIGNMENT 7
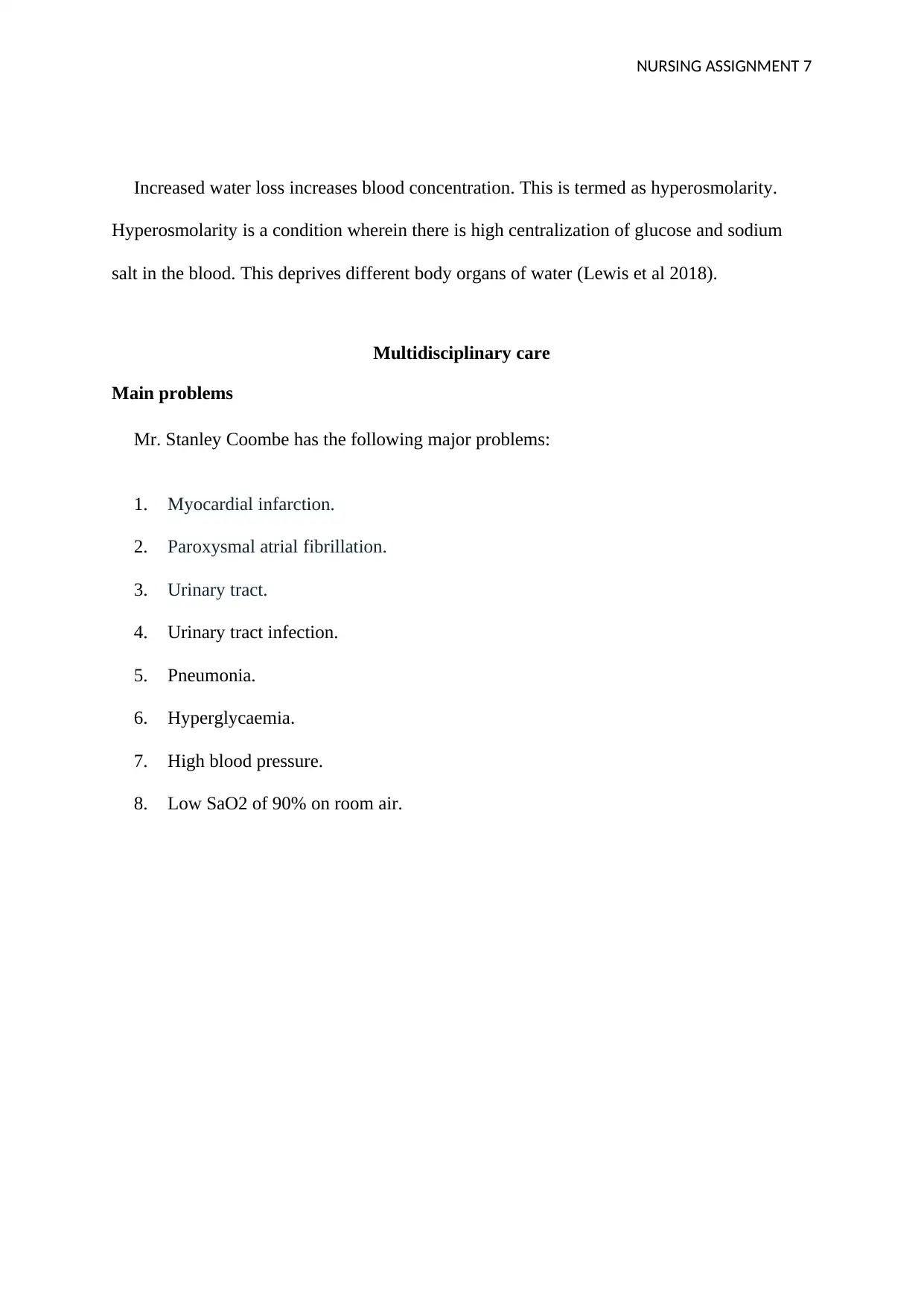
Increased water loss increases blood concentration. This is termed as hyperosmolarity.
Hyperosmolarity is a condition wherein there is high centralization of glucose and sodium
salt in the blood. This deprives different body organs of water (Lewis et al 2018).
Multidisciplinary care
Main problems
Mr. Stanley Coombe has the following major problems:
1. Myocardial infarction.
2. Paroxysmal atrial fibrillation.
3. Urinary tract.
4. Urinary tract infection.
5. Pneumonia.
6. Hyperglycaemia.
7. High blood pressure.
8. Low SaO2 of 90% on room air.
Increased water loss increases blood concentration. This is termed as hyperosmolarity.
Hyperosmolarity is a condition wherein there is high centralization of glucose and sodium
salt in the blood. This deprives different body organs of water (Lewis et al 2018).
Multidisciplinary care
Main problems
Mr. Stanley Coombe has the following major problems:
1. Myocardial infarction.
2. Paroxysmal atrial fibrillation.
3. Urinary tract.
4. Urinary tract infection.
5. Pneumonia.
6. Hyperglycaemia.
7. High blood pressure.
8. Low SaO2 of 90% on room air.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT 8
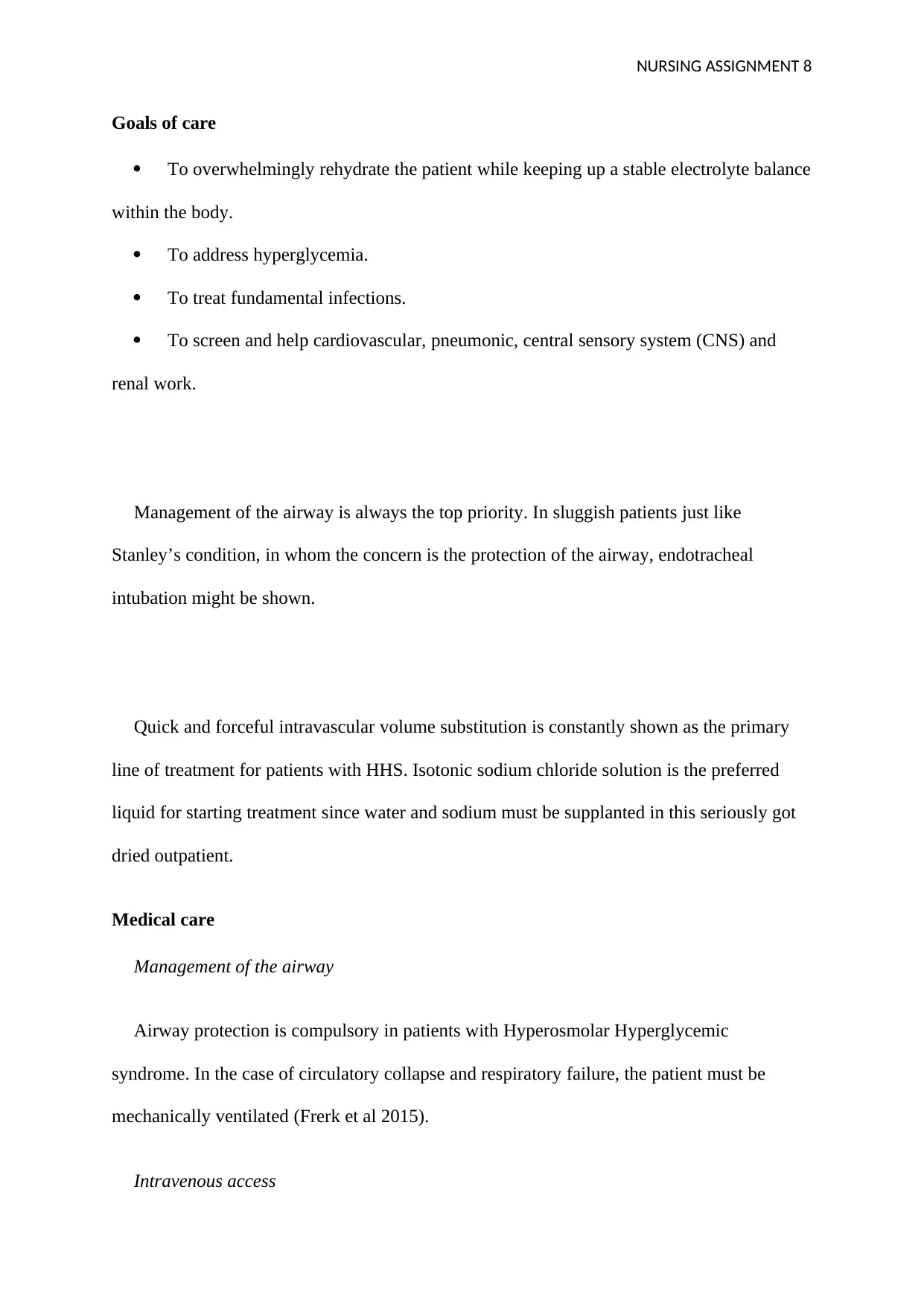
Goals of care
To overwhelmingly rehydrate the patient while keeping up a stable electrolyte balance
within the body.
To address hyperglycemia.
To treat fundamental infections.
To screen and help cardiovascular, pneumonic, central sensory system (CNS) and
renal work.
Management of the airway is always the top priority. In sluggish patients just like
Stanley’s condition, in whom the concern is the protection of the airway, endotracheal
intubation might be shown.
Quick and forceful intravascular volume substitution is constantly shown as the primary
line of treatment for patients with HHS. Isotonic sodium chloride solution is the preferred
liquid for starting treatment since water and sodium must be supplanted in this seriously got
dried outpatient.
Medical care
Management of the airway
Airway protection is compulsory in patients with Hyperosmolar Hyperglycemic
syndrome. In the case of circulatory collapse and respiratory failure, the patient must be
mechanically ventilated (Frerk et al 2015).
Intravenous access
Goals of care
To overwhelmingly rehydrate the patient while keeping up a stable electrolyte balance
within the body.
To address hyperglycemia.
To treat fundamental infections.
To screen and help cardiovascular, pneumonic, central sensory system (CNS) and
renal work.
Management of the airway is always the top priority. In sluggish patients just like
Stanley’s condition, in whom the concern is the protection of the airway, endotracheal
intubation might be shown.
Quick and forceful intravascular volume substitution is constantly shown as the primary
line of treatment for patients with HHS. Isotonic sodium chloride solution is the preferred
liquid for starting treatment since water and sodium must be supplanted in this seriously got
dried outpatient.
Medical care
Management of the airway
Airway protection is compulsory in patients with Hyperosmolar Hyperglycemic
syndrome. In the case of circulatory collapse and respiratory failure, the patient must be
mechanically ventilated (Frerk et al 2015).
Intravenous access
NURSING ASSIGNMENT 9
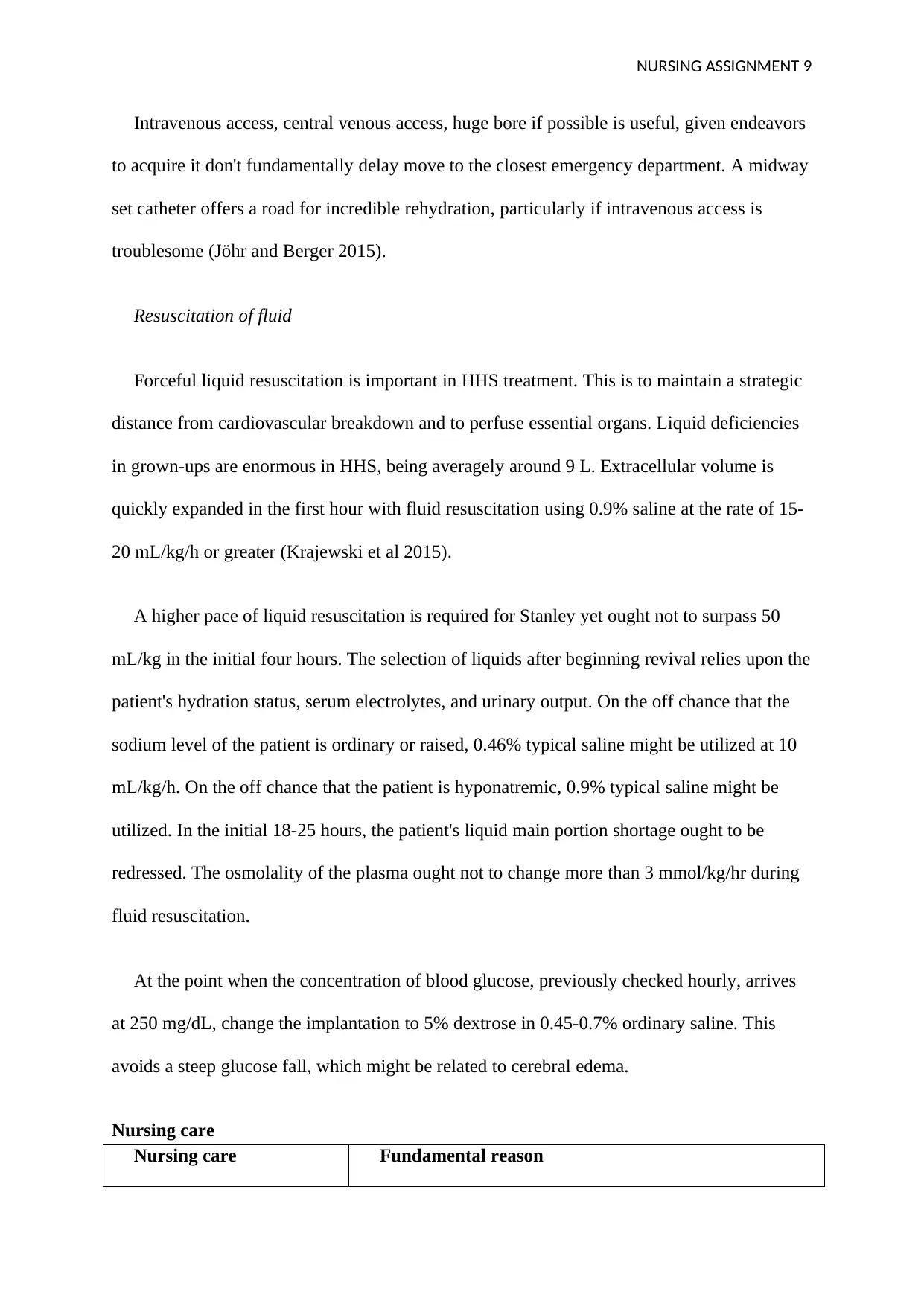
Intravenous access, central venous access, huge bore if possible is useful, given endeavors
to acquire it don't fundamentally delay move to the closest emergency department. A midway
set catheter offers a road for incredible rehydration, particularly if intravenous access is
troublesome (Jöhr and Berger 2015).
Resuscitation of fluid
Forceful liquid resuscitation is important in HHS treatment. This is to maintain a strategic
distance from cardiovascular breakdown and to perfuse essential organs. Liquid deficiencies
in grown-ups are enormous in HHS, being averagely around 9 L. Extracellular volume is
quickly expanded in the first hour with fluid resuscitation using 0.9% saline at the rate of 15-
20 mL/kg/h or greater (Krajewski et al 2015).
A higher pace of liquid resuscitation is required for Stanley yet ought not to surpass 50
mL/kg in the initial four hours. The selection of liquids after beginning revival relies upon the
patient's hydration status, serum electrolytes, and urinary output. On the off chance that the
sodium level of the patient is ordinary or raised, 0.46% typical saline might be utilized at 10
mL/kg/h. On the off chance that the patient is hyponatremic, 0.9% typical saline might be
utilized. In the initial 18-25 hours, the patient's liquid main portion shortage ought to be
redressed. The osmolality of the plasma ought not to change more than 3 mmol/kg/hr during
fluid resuscitation.
At the point when the concentration of blood glucose, previously checked hourly, arrives
at 250 mg/dL, change the implantation to 5% dextrose in 0.45-0.7% ordinary saline. This
avoids a steep glucose fall, which might be related to cerebral edema.
Nursing care
Nursing care Fundamental reason
Intravenous access, central venous access, huge bore if possible is useful, given endeavors
to acquire it don't fundamentally delay move to the closest emergency department. A midway
set catheter offers a road for incredible rehydration, particularly if intravenous access is
troublesome (Jöhr and Berger 2015).
Resuscitation of fluid
Forceful liquid resuscitation is important in HHS treatment. This is to maintain a strategic
distance from cardiovascular breakdown and to perfuse essential organs. Liquid deficiencies
in grown-ups are enormous in HHS, being averagely around 9 L. Extracellular volume is
quickly expanded in the first hour with fluid resuscitation using 0.9% saline at the rate of 15-
20 mL/kg/h or greater (Krajewski et al 2015).
A higher pace of liquid resuscitation is required for Stanley yet ought not to surpass 50
mL/kg in the initial four hours. The selection of liquids after beginning revival relies upon the
patient's hydration status, serum electrolytes, and urinary output. On the off chance that the
sodium level of the patient is ordinary or raised, 0.46% typical saline might be utilized at 10
mL/kg/h. On the off chance that the patient is hyponatremic, 0.9% typical saline might be
utilized. In the initial 18-25 hours, the patient's liquid main portion shortage ought to be
redressed. The osmolality of the plasma ought not to change more than 3 mmol/kg/hr during
fluid resuscitation.
At the point when the concentration of blood glucose, previously checked hourly, arrives
at 250 mg/dL, change the implantation to 5% dextrose in 0.45-0.7% ordinary saline. This
avoids a steep glucose fall, which might be related to cerebral edema.
Nursing care
Nursing care Fundamental reason
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING ASSIGNMENT 10
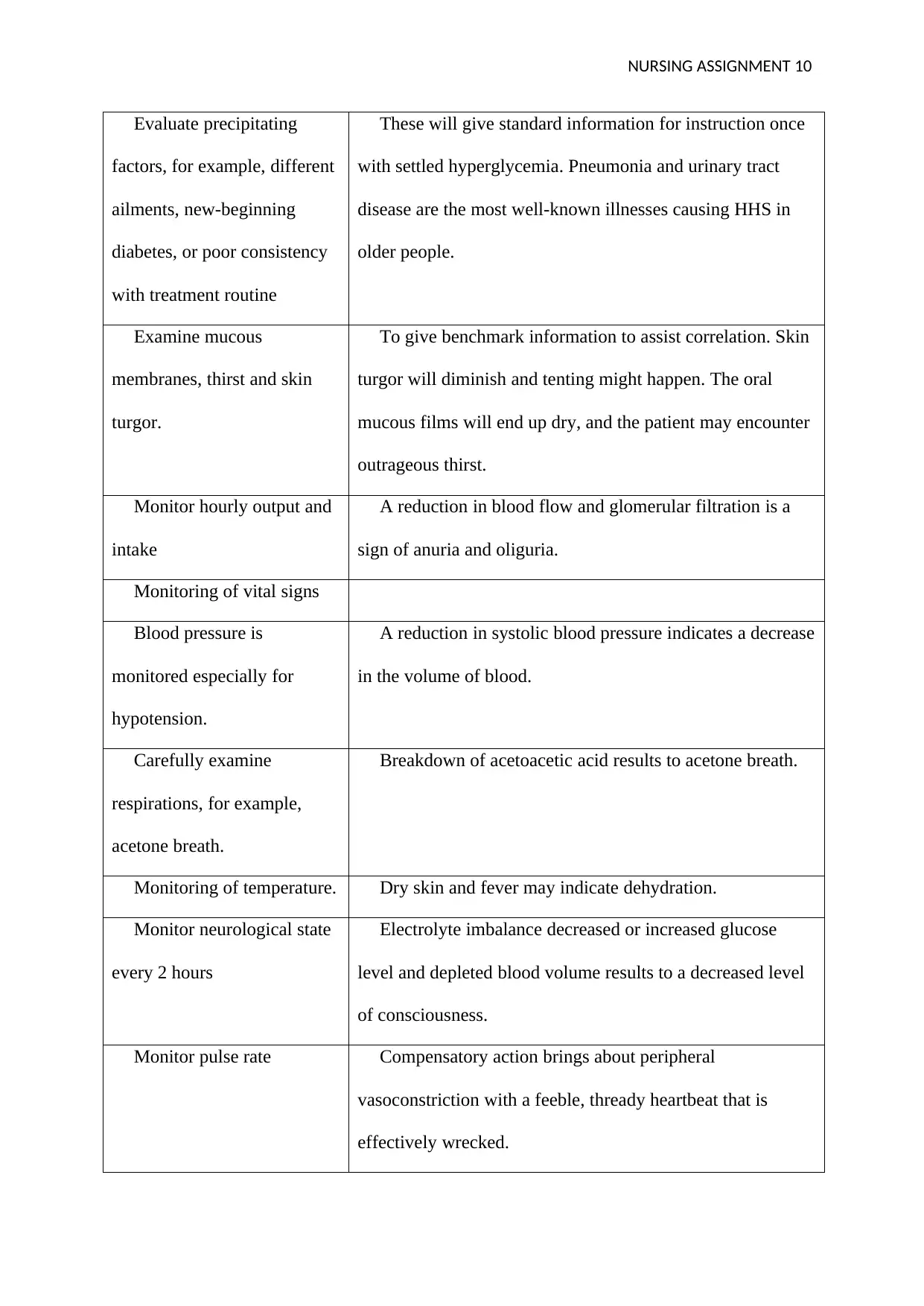
Evaluate precipitating
factors, for example, different
ailments, new-beginning
diabetes, or poor consistency
with treatment routine
These will give standard information for instruction once
with settled hyperglycemia. Pneumonia and urinary tract
disease are the most well-known illnesses causing HHS in
older people.
Examine mucous
membranes, thirst and skin
turgor.
To give benchmark information to assist correlation. Skin
turgor will diminish and tenting might happen. The oral
mucous films will end up dry, and the patient may encounter
outrageous thirst.
Monitor hourly output and
intake
A reduction in blood flow and glomerular filtration is a
sign of anuria and oliguria.
Monitoring of vital signs
Blood pressure is
monitored especially for
hypotension.
A reduction in systolic blood pressure indicates a decrease
in the volume of blood.
Carefully examine
respirations, for example,
acetone breath.
Breakdown of acetoacetic acid results to acetone breath.
Monitoring of temperature. Dry skin and fever may indicate dehydration.
Monitor neurological state
every 2 hours
Electrolyte imbalance decreased or increased glucose
level and depleted blood volume results to a decreased level
of consciousness.
Monitor pulse rate Compensatory action brings about peripheral
vasoconstriction with a feeble, thready heartbeat that is
effectively wrecked.
Evaluate precipitating
factors, for example, different
ailments, new-beginning
diabetes, or poor consistency
with treatment routine
These will give standard information for instruction once
with settled hyperglycemia. Pneumonia and urinary tract
disease are the most well-known illnesses causing HHS in
older people.
Examine mucous
membranes, thirst and skin
turgor.
To give benchmark information to assist correlation. Skin
turgor will diminish and tenting might happen. The oral
mucous films will end up dry, and the patient may encounter
outrageous thirst.
Monitor hourly output and
intake
A reduction in blood flow and glomerular filtration is a
sign of anuria and oliguria.
Monitoring of vital signs
Blood pressure is
monitored especially for
hypotension.
A reduction in systolic blood pressure indicates a decrease
in the volume of blood.
Carefully examine
respirations, for example,
acetone breath.
Breakdown of acetoacetic acid results to acetone breath.
Monitoring of temperature. Dry skin and fever may indicate dehydration.
Monitor neurological state
every 2 hours
Electrolyte imbalance decreased or increased glucose
level and depleted blood volume results to a decreased level
of consciousness.
Monitor pulse rate Compensatory action brings about peripheral
vasoconstriction with a feeble, thready heartbeat that is
effectively wrecked.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT 11
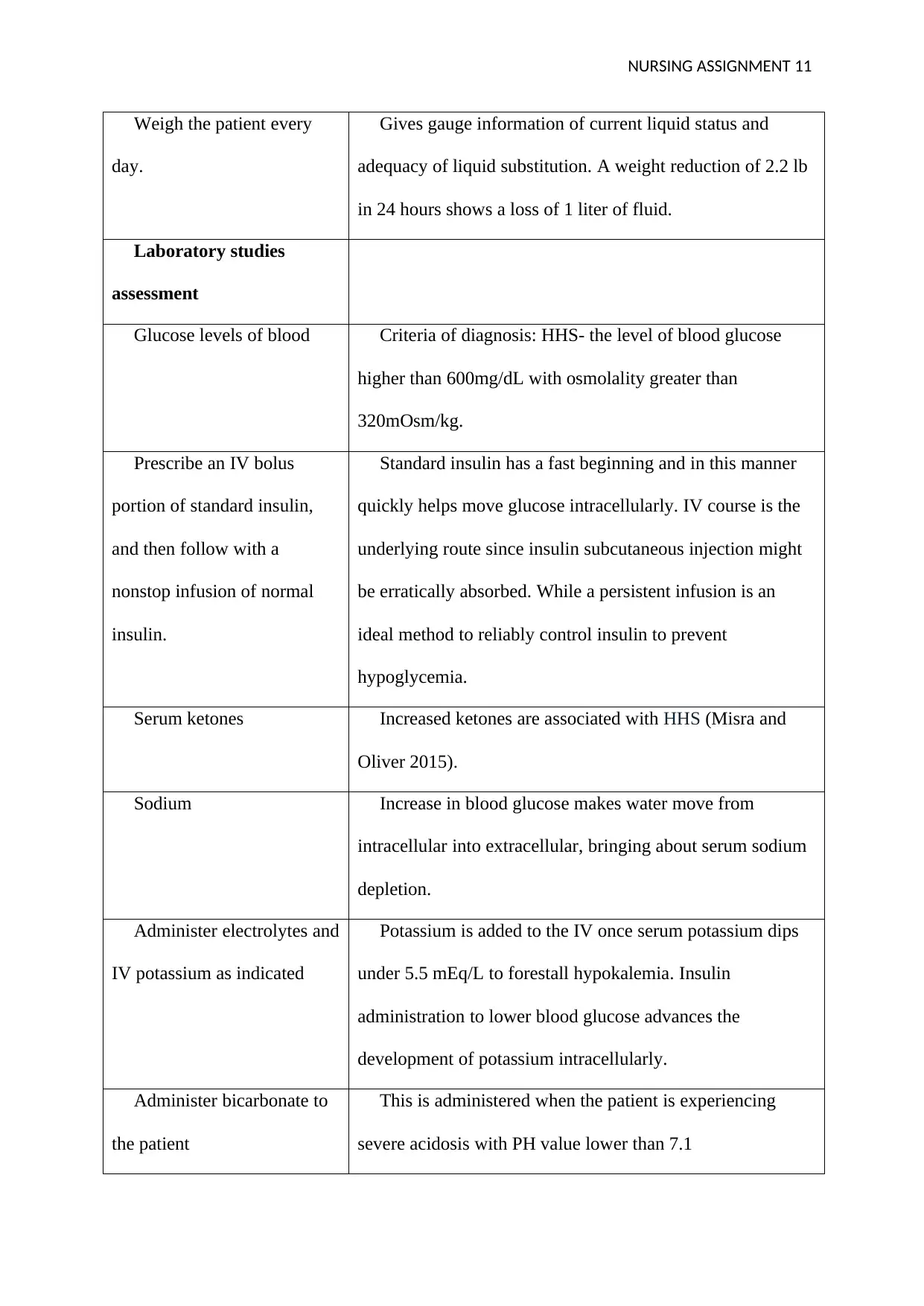
Weigh the patient every
day.
Gives gauge information of current liquid status and
adequacy of liquid substitution. A weight reduction of 2.2 lb
in 24 hours shows a loss of 1 liter of fluid.
Laboratory studies
assessment
Glucose levels of blood Criteria of diagnosis: HHS- the level of blood glucose
higher than 600mg/dL with osmolality greater than
320mOsm/kg.
Prescribe an IV bolus
portion of standard insulin,
and then follow with a
nonstop infusion of normal
insulin.
Standard insulin has a fast beginning and in this manner
quickly helps move glucose intracellularly. IV course is the
underlying route since insulin subcutaneous injection might
be erratically absorbed. While a persistent infusion is an
ideal method to reliably control insulin to prevent
hypoglycemia.
Serum ketones Increased ketones are associated with HHS (Misra and
Oliver 2015).
Sodium Increase in blood glucose makes water move from
intracellular into extracellular, bringing about serum sodium
depletion.
Administer electrolytes and
IV potassium as indicated
Potassium is added to the IV once serum potassium dips
under 5.5 mEq/L to forestall hypokalemia. Insulin
administration to lower blood glucose advances the
development of potassium intracellularly.
Administer bicarbonate to
the patient
This is administered when the patient is experiencing
severe acidosis with PH value lower than 7.1
Weigh the patient every
day.
Gives gauge information of current liquid status and
adequacy of liquid substitution. A weight reduction of 2.2 lb
in 24 hours shows a loss of 1 liter of fluid.
Laboratory studies
assessment
Glucose levels of blood Criteria of diagnosis: HHS- the level of blood glucose
higher than 600mg/dL with osmolality greater than
320mOsm/kg.
Prescribe an IV bolus
portion of standard insulin,
and then follow with a
nonstop infusion of normal
insulin.
Standard insulin has a fast beginning and in this manner
quickly helps move glucose intracellularly. IV course is the
underlying route since insulin subcutaneous injection might
be erratically absorbed. While a persistent infusion is an
ideal method to reliably control insulin to prevent
hypoglycemia.
Serum ketones Increased ketones are associated with HHS (Misra and
Oliver 2015).
Sodium Increase in blood glucose makes water move from
intracellular into extracellular, bringing about serum sodium
depletion.
Administer electrolytes and
IV potassium as indicated
Potassium is added to the IV once serum potassium dips
under 5.5 mEq/L to forestall hypokalemia. Insulin
administration to lower blood glucose advances the
development of potassium intracellularly.
Administer bicarbonate to
the patient
This is administered when the patient is experiencing
severe acidosis with PH value lower than 7.1
NURSING ASSIGNMENT 12
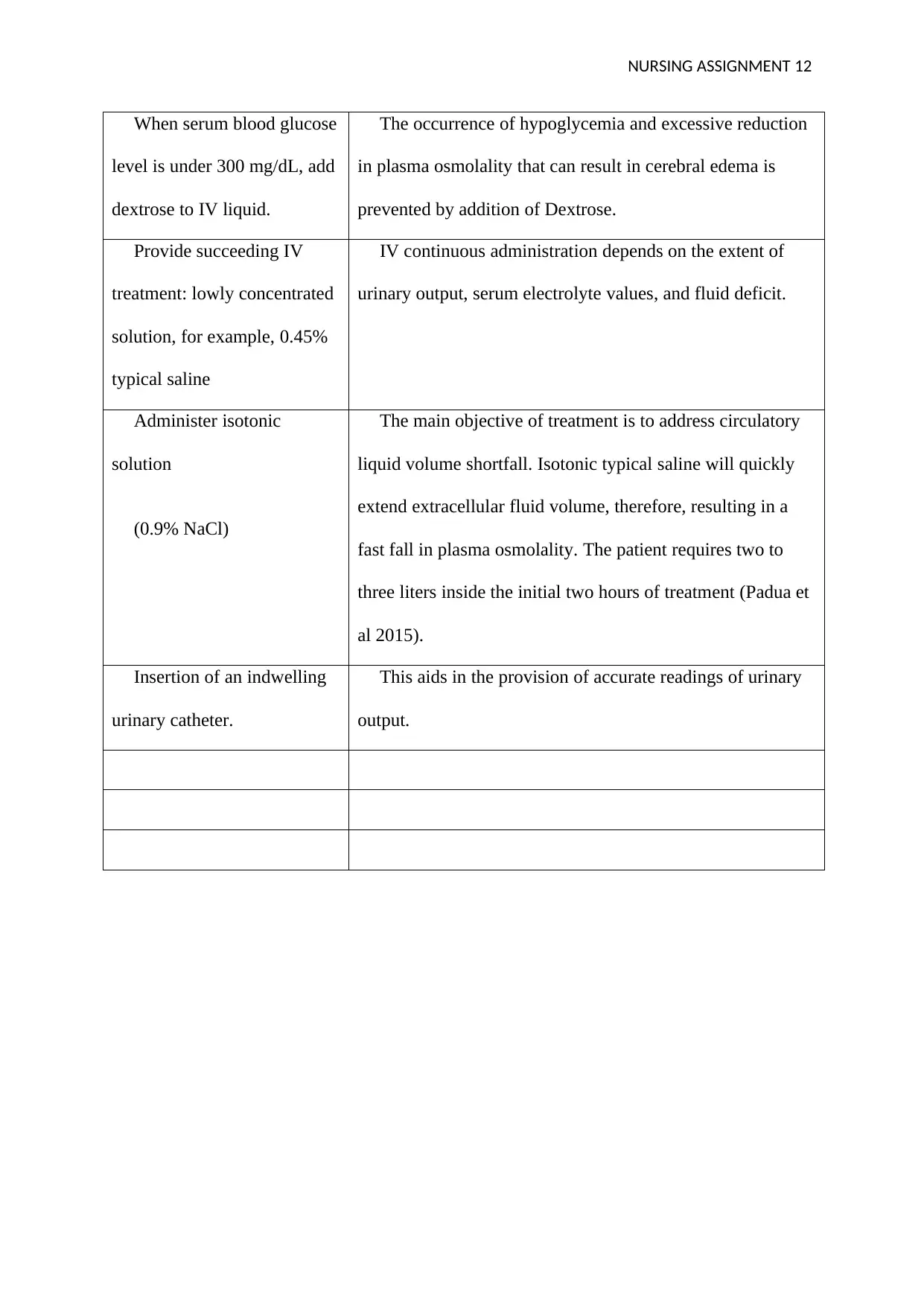
When serum blood glucose
level is under 300 mg/dL, add
dextrose to IV liquid.
The occurrence of hypoglycemia and excessive reduction
in plasma osmolality that can result in cerebral edema is
prevented by addition of Dextrose.
Provide succeeding IV
treatment: lowly concentrated
solution, for example, 0.45%
typical saline
IV continuous administration depends on the extent of
urinary output, serum electrolyte values, and fluid deficit.
Administer isotonic
solution
(0.9% NaCl)
The main objective of treatment is to address circulatory
liquid volume shortfall. Isotonic typical saline will quickly
extend extracellular fluid volume, therefore, resulting in a
fast fall in plasma osmolality. The patient requires two to
three liters inside the initial two hours of treatment (Padua et
al 2015).
Insertion of an indwelling
urinary catheter.
This aids in the provision of accurate readings of urinary
output.
When serum blood glucose
level is under 300 mg/dL, add
dextrose to IV liquid.
The occurrence of hypoglycemia and excessive reduction
in plasma osmolality that can result in cerebral edema is
prevented by addition of Dextrose.
Provide succeeding IV
treatment: lowly concentrated
solution, for example, 0.45%
typical saline
IV continuous administration depends on the extent of
urinary output, serum electrolyte values, and fluid deficit.
Administer isotonic
solution
(0.9% NaCl)
The main objective of treatment is to address circulatory
liquid volume shortfall. Isotonic typical saline will quickly
extend extracellular fluid volume, therefore, resulting in a
fast fall in plasma osmolality. The patient requires two to
three liters inside the initial two hours of treatment (Padua et
al 2015).
Insertion of an indwelling
urinary catheter.
This aids in the provision of accurate readings of urinary
output.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

