Case Study on Nursing Adults with Long Term Disease: HIV and TB
VerifiedAdded on 2023/06/15
|16
|4155
|288
Case Study
AI Summary
This case study presents the case of Mr. X, a 40-year-old businessperson diagnosed with HIV and subsequently with Tuberculosis (TB). The case details the progression of his conditions, the nursing assessments performed, and the treatment strategies employed. Initially, Mr. X was treated for TB with a focus on preventing the latent phase from becoming active. After successful TB treatment, antiretroviral therapy (ART) was initiated for HIV, with careful monitoring to avoid Immune Reconstitution Inflammatory Syndrome (IRIS). The case also explores the management of Oral candidiasis, another opportunistic infection, through topical and antifungal treatments. Throughout the treatment process, psychological support was provided to address the patient's depression. The case concludes with an evaluation of Mr. X's improved condition, highlighting the successful management of TB and the ongoing treatment of HIV. Desklib provides similar solved assignments for students.

Running Head: NURSING ADULTS WITH LONG TERM DISEASE
NURSING ADULTS WITH LONG TERM DISEASE
Name of the Student
Name of the University
Author’s Note
NURSING ADULTS WITH LONG TERM DISEASE
Name of the Student
Name of the University
Author’s Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING ADULTS WITH LONG TERM DISEASE
Essay:
Human Immunodeficiency Virus (HIV) is the virus that is responsible for causing
Acquired Immune Deficiency Syndrome (AIDS). It gradually damages and kills the T helper
cells, which are responsible for all adaptive immune responses of the body, and hence reduces
the immune system of the body (Lima and Melo 2012). This results in gradual destruction of the
ability of the body in fighting infection and certain types of cancers. HIV can be transmitted
through contaminated syringes or needles, sexual contact, transmission from an infected mother
to child during pregnancy or breast milk. Initially the affected individual will suffer from an
illness similar to influenza, which is followed by a latent, asymptomatic phase. HIV get
progressed to AIDS when the count of CD4 lymphocyte falls below 200 cell per ml of blood
(Gray and Cohn 2013). The characteristics ofAIDS include increased opportunistic infection
susceptibility and cell mediated immunity deficiency, which eventually lead to Cancer.
According to research,in U.K., about 88,769 that includes 315 children below the age of 15, have
been found to suffer from HIV and consequently are recieving specialist care (Wannheden et al.
2013). The total number of people receiving specialist care for HIV has grown steadily over the
last decade. There has been a sharp rise in the number of people accessing HIV care by 73%
between the periods of 2006 to 2015. One third of the HIV affected people in UK has reportedly
been the victim of social discrimination. The major victims are the health care workers. The fatal
effect of the HIV has given rise to various negative attitude like fear and anxiety in public
(Shankar et al. 2014).
The case study is about Mr. X, a 40 years old businessperson who resides in Bahia
situated in Brazil. For business purposes, he used to travel frequently to West Africa. In 2005,
Mr. X was diagnosed with HIV. He admitted to have licentious behavior with numerous African
Essay:
Human Immunodeficiency Virus (HIV) is the virus that is responsible for causing
Acquired Immune Deficiency Syndrome (AIDS). It gradually damages and kills the T helper
cells, which are responsible for all adaptive immune responses of the body, and hence reduces
the immune system of the body (Lima and Melo 2012). This results in gradual destruction of the
ability of the body in fighting infection and certain types of cancers. HIV can be transmitted
through contaminated syringes or needles, sexual contact, transmission from an infected mother
to child during pregnancy or breast milk. Initially the affected individual will suffer from an
illness similar to influenza, which is followed by a latent, asymptomatic phase. HIV get
progressed to AIDS when the count of CD4 lymphocyte falls below 200 cell per ml of blood
(Gray and Cohn 2013). The characteristics ofAIDS include increased opportunistic infection
susceptibility and cell mediated immunity deficiency, which eventually lead to Cancer.
According to research,in U.K., about 88,769 that includes 315 children below the age of 15, have
been found to suffer from HIV and consequently are recieving specialist care (Wannheden et al.
2013). The total number of people receiving specialist care for HIV has grown steadily over the
last decade. There has been a sharp rise in the number of people accessing HIV care by 73%
between the periods of 2006 to 2015. One third of the HIV affected people in UK has reportedly
been the victim of social discrimination. The major victims are the health care workers. The fatal
effect of the HIV has given rise to various negative attitude like fear and anxiety in public
(Shankar et al. 2014).
The case study is about Mr. X, a 40 years old businessperson who resides in Bahia
situated in Brazil. For business purposes, he used to travel frequently to West Africa. In 2005,
Mr. X was diagnosed with HIV. He admitted to have licentious behavior with numerous African
2NURSING ADULTS WITH LONG TERM DISEASE
sex workers along with maintaining a stable sexual relation with his wife. He was initially treated
in Mali for Chancroid. Mr. X started experiencing flu like symptoms along with
lymphadenopathy and splenomegaly after the fourth week of being diagnosed with Chancroid.
He reported even a loss of 12 kg of body weight. Soon he got severely ill and started
experiencing terrible clinical condition and hence had to be admitted in a health care center in
Mali.Laboratory test was performed and he was diagnosed with HIV 1 infection. In the following
days Mr. X also started experiencing various kinds of opportunistic infectious issues and was
diagnosed with Tuberculosis. A terrible decrease of his CD4-CD8 ratio to .16 (the normal value
lies between the range of 0.81-3.00) is recorded within 3 years.
The fact that Mr. X was suffering from opportunistic infection (OI) has resulted in
gradual damage of his immune system and eventually has taken the form of tuberculosis (TB).
Mycobacterium Tuberculosis bacteria cause the disease, Tuberculosis, which causes infection in
lung when inhaled by an individual.Though lungs are the primary parts of the body that is
infected by the bacteria, the bacteria gradually moves to other parts of the body through
bloodstream (Law et al. 2013). Both Having TB and HIV both was speeding up the decay of
immune system of the patient and thus latent TB eventually takes the form of active TB. Mr. X
was at a higher risk of death as the risk of death is double for individuals who are suffering from
both TB and HIV when compared to patients suffering only from HIV. Considering the fact that
Mr. X initially was not receiving antiretroviral treatment, within a span of two weeks the TB
which was in latent phase got converted to active phase.
According to research performed by WHO, about 78 percent patients suffering from both
HIV and TB are on antiretroviral therapy globally and 90 percent of patients are from Malawi,
Mozambique, Swaziland, Namibia and India (O’Cleirighet al. 2013). The fact that patients
sex workers along with maintaining a stable sexual relation with his wife. He was initially treated
in Mali for Chancroid. Mr. X started experiencing flu like symptoms along with
lymphadenopathy and splenomegaly after the fourth week of being diagnosed with Chancroid.
He reported even a loss of 12 kg of body weight. Soon he got severely ill and started
experiencing terrible clinical condition and hence had to be admitted in a health care center in
Mali.Laboratory test was performed and he was diagnosed with HIV 1 infection. In the following
days Mr. X also started experiencing various kinds of opportunistic infectious issues and was
diagnosed with Tuberculosis. A terrible decrease of his CD4-CD8 ratio to .16 (the normal value
lies between the range of 0.81-3.00) is recorded within 3 years.
The fact that Mr. X was suffering from opportunistic infection (OI) has resulted in
gradual damage of his immune system and eventually has taken the form of tuberculosis (TB).
Mycobacterium Tuberculosis bacteria cause the disease, Tuberculosis, which causes infection in
lung when inhaled by an individual.Though lungs are the primary parts of the body that is
infected by the bacteria, the bacteria gradually moves to other parts of the body through
bloodstream (Law et al. 2013). Both Having TB and HIV both was speeding up the decay of
immune system of the patient and thus latent TB eventually takes the form of active TB. Mr. X
was at a higher risk of death as the risk of death is double for individuals who are suffering from
both TB and HIV when compared to patients suffering only from HIV. Considering the fact that
Mr. X initially was not receiving antiretroviral treatment, within a span of two weeks the TB
which was in latent phase got converted to active phase.
According to research performed by WHO, about 78 percent patients suffering from both
HIV and TB are on antiretroviral therapy globally and 90 percent of patients are from Malawi,
Mozambique, Swaziland, Namibia and India (O’Cleirighet al. 2013). The fact that patients
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING ADULTS WITH LONG TERM DISEASE
suffering from both HIV and TB lacks in showing classic symptoms of pulmonary TB infection,
initially it was difficult to access that Mr. X is suffering from TB along with HIV. Being a
sufferer of sub clinical TB, the chest X-ray of Mr. X did not show TB symptoms initially.
Because of the fact that current availability of tools for sub clinical TB is less, especially for
patients with both TB and HIV, several HIV patients like Mr. X has to go through a fatal
condition due to the late detection of the disease. Before initiating thetreatment, the nursing
assessment is performed by taking account of a number of factors discussed here. Firstly, tests
are done to find out if Mr. X has symptoms of only TB or any other opportunistic infection along
with HIV. Secondly, all the existing treatments of Mr. X are taken into account. Thirdly, a
physiological counseling was conducted with the patient in order to understand the way in which
he is dealing with both HIV and Tuberculosis simultaneously. Finally, Tuberculosis Preventive
Treatment (TPT) was provided to Mr. X.
Considering the fact that patients infected with both HIV and TB have higher risk of
active TB development, crucial clinical management have in such situations (Mahnkeet al.
2012). The first step that had been taken once after it had been detected that Mr. X is suffering
from TB along with HIV was to put him on Tuberculosis Preventive Treatment (TPT) with once
daily usage of isoniazid 10 mg/kg (Maximum 600 mg) since prompt treatment of active TB will
reduce the TB related mortality and transmission risk. Mr. X was treated based on the drug with
proper bioavailability. The phases of treating Mr. X for TB comprised of initial phase and
continuation phase. The duration of initial phase was 2 to 3 months and that of the continuation
phase lasted for 4 to 5 months. After continuation of the treatment for about 5 months by a
regimen, which includes rifampicin throughout the treatment course, Mr. X was almost cured
and no sign of relapse of Tuberculosis is seen until now.
suffering from both HIV and TB lacks in showing classic symptoms of pulmonary TB infection,
initially it was difficult to access that Mr. X is suffering from TB along with HIV. Being a
sufferer of sub clinical TB, the chest X-ray of Mr. X did not show TB symptoms initially.
Because of the fact that current availability of tools for sub clinical TB is less, especially for
patients with both TB and HIV, several HIV patients like Mr. X has to go through a fatal
condition due to the late detection of the disease. Before initiating thetreatment, the nursing
assessment is performed by taking account of a number of factors discussed here. Firstly, tests
are done to find out if Mr. X has symptoms of only TB or any other opportunistic infection along
with HIV. Secondly, all the existing treatments of Mr. X are taken into account. Thirdly, a
physiological counseling was conducted with the patient in order to understand the way in which
he is dealing with both HIV and Tuberculosis simultaneously. Finally, Tuberculosis Preventive
Treatment (TPT) was provided to Mr. X.
Considering the fact that patients infected with both HIV and TB have higher risk of
active TB development, crucial clinical management have in such situations (Mahnkeet al.
2012). The first step that had been taken once after it had been detected that Mr. X is suffering
from TB along with HIV was to put him on Tuberculosis Preventive Treatment (TPT) with once
daily usage of isoniazid 10 mg/kg (Maximum 600 mg) since prompt treatment of active TB will
reduce the TB related mortality and transmission risk. Mr. X was treated based on the drug with
proper bioavailability. The phases of treating Mr. X for TB comprised of initial phase and
continuation phase. The duration of initial phase was 2 to 3 months and that of the continuation
phase lasted for 4 to 5 months. After continuation of the treatment for about 5 months by a
regimen, which includes rifampicin throughout the treatment course, Mr. X was almost cured
and no sign of relapse of Tuberculosis is seen until now.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING ADULTS WITH LONG TERM DISEASE
Because of the fact that Mr. X is suffering from active HIV, along with active TB,
initiation of antiretroviral Treatment (ART) was started just after completion of his TB treatment.
The reason behind this is that HIV and TB treatment should not be preferably started
simultaneously (Walker et al. 2015). The major reasons behind this are firstly, to avoid
interactions of antiretroviral (ARV) drugs with TB drugs. Secondly, over lapping of toxicities
may also occur if both the treatments are done simultaneously. Thirdly, if the both treatments are
not done simultaneously, there remains no risk of Immune Reconstitution Inflammatory
Syndrome (IRIS) and increased adherence (Chimbindi,Bärnighausen and Newell 2014).
Fourthly, avoiding the treatment of both the diseases simultaneously will minimize the confusion
of the patient of what drug to take and when. Finally, simplification of patient management is
another reason behind it.
Monitoring of ART is very crucial once the patient initially gets started with it since there
remains a chance of the occurrence of Immune Reconstitution Inflammatory Syndrome (IRIS)
(Schuster, Bornovalova and Hunt 2012). This is the reason behind the fact that Mr. X had been
kept under strict monitoring. Sometimes, it was often noticed that a patient was developing IRIS
even after a few days of improvement. The chief reason behind the occurrence of IRIS are low
CD4 count and initiation of ART in early stages of TB treatment (Daftary 2012). In spite of the
fact that Mr. X reportedly has a low CD4 count, he is not suffering from IRIS since his treatment
is done under crucial monitoring.
It was observed that Mr. X, during the treatment got severely depressed due to his illness.
Thus, an additional support of an eminent psychologist is required in order to motivate him.
Throughout the whole process, it can be evaluated that the condition of Mr. X as a patient has
majorly improved in the past 7 months. When he was admitted in the health care center, he was
Because of the fact that Mr. X is suffering from active HIV, along with active TB,
initiation of antiretroviral Treatment (ART) was started just after completion of his TB treatment.
The reason behind this is that HIV and TB treatment should not be preferably started
simultaneously (Walker et al. 2015). The major reasons behind this are firstly, to avoid
interactions of antiretroviral (ARV) drugs with TB drugs. Secondly, over lapping of toxicities
may also occur if both the treatments are done simultaneously. Thirdly, if the both treatments are
not done simultaneously, there remains no risk of Immune Reconstitution Inflammatory
Syndrome (IRIS) and increased adherence (Chimbindi,Bärnighausen and Newell 2014).
Fourthly, avoiding the treatment of both the diseases simultaneously will minimize the confusion
of the patient of what drug to take and when. Finally, simplification of patient management is
another reason behind it.
Monitoring of ART is very crucial once the patient initially gets started with it since there
remains a chance of the occurrence of Immune Reconstitution Inflammatory Syndrome (IRIS)
(Schuster, Bornovalova and Hunt 2012). This is the reason behind the fact that Mr. X had been
kept under strict monitoring. Sometimes, it was often noticed that a patient was developing IRIS
even after a few days of improvement. The chief reason behind the occurrence of IRIS are low
CD4 count and initiation of ART in early stages of TB treatment (Daftary 2012). In spite of the
fact that Mr. X reportedly has a low CD4 count, he is not suffering from IRIS since his treatment
is done under crucial monitoring.
It was observed that Mr. X, during the treatment got severely depressed due to his illness.
Thus, an additional support of an eminent psychologist is required in order to motivate him.
Throughout the whole process, it can be evaluated that the condition of Mr. X as a patient has
majorly improved in the past 7 months. When he was admitted in the health care center, he was
5NURSING ADULTS WITH LONG TERM DISEASE
suffering from active HIV and Active Tuberculosis. He was cured of TB within a span of about 6
month and the disease, till now is showing no sign of relapsing. In spite of the fact that HIV is an
incurable disease, Mr. X is in a much better condition than what he was before being admitted in
the health care home.
Another major problem from which Mr. X was suffering is Oral candidiasis. Nursing
assessment of Mr. X disclosed several symptoms of the mentioned disease. He reported that for
the past few months he was having a feeling of discomfort and sensation of burning in his mouth
and throat along with an altered sense of taste, which he reported to be very poor. He also had
creamy white spots in his mouth and throat that can be removed by lightly scrapping on the spot.
Other issues like cracking, soreness, redness and swelling in the corner of the mouth was also
reported by him.
The first step of Oropharyngeal candidiasis diagnosis of Mr. X was clinical examination
of his mouth. In order to confirm the disease a sore was scraped and was checked under
microscope. However, since the presence of the disease was unclear from the clinical
examination label test including smear and culture is done. After the confirmation of the disease,
immediate treatment of oropharyngeal candidiasis of Mr. X was started. Considering the fact
that, though oral therapy is one of the most effective first line treatment, Mr. X was given
topical treatment since it is safer and convenient for mild to moderate diseases.
Topical oral treatment include a regular mouth rinse schedule and lozenges or troches.
The medication given to Mr. X was Clotrimazole troches and nystatin (Mycostanin) pastille. He
was suggested to intake Clotrimazole troches of dosage 10mg daily for 5 times in the mouth.2
Nystatin (Mycostanin) pastille tablets of 50 mg was also taken by him daily 4 to 5 times. It was
informed to Mr. X that the tablets needs to be sucked slowly and should not be swallowed or
suffering from active HIV and Active Tuberculosis. He was cured of TB within a span of about 6
month and the disease, till now is showing no sign of relapsing. In spite of the fact that HIV is an
incurable disease, Mr. X is in a much better condition than what he was before being admitted in
the health care home.
Another major problem from which Mr. X was suffering is Oral candidiasis. Nursing
assessment of Mr. X disclosed several symptoms of the mentioned disease. He reported that for
the past few months he was having a feeling of discomfort and sensation of burning in his mouth
and throat along with an altered sense of taste, which he reported to be very poor. He also had
creamy white spots in his mouth and throat that can be removed by lightly scrapping on the spot.
Other issues like cracking, soreness, redness and swelling in the corner of the mouth was also
reported by him.
The first step of Oropharyngeal candidiasis diagnosis of Mr. X was clinical examination
of his mouth. In order to confirm the disease a sore was scraped and was checked under
microscope. However, since the presence of the disease was unclear from the clinical
examination label test including smear and culture is done. After the confirmation of the disease,
immediate treatment of oropharyngeal candidiasis of Mr. X was started. Considering the fact
that, though oral therapy is one of the most effective first line treatment, Mr. X was given
topical treatment since it is safer and convenient for mild to moderate diseases.
Topical oral treatment include a regular mouth rinse schedule and lozenges or troches.
The medication given to Mr. X was Clotrimazole troches and nystatin (Mycostanin) pastille. He
was suggested to intake Clotrimazole troches of dosage 10mg daily for 5 times in the mouth.2
Nystatin (Mycostanin) pastille tablets of 50 mg was also taken by him daily 4 to 5 times. It was
informed to Mr. X that the tablets needs to be sucked slowly and should not be swallowed or
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING ADULTS WITH LONG TERM DISEASE
chewed as a whole. Mr. X followed the instructions given to him thoroughly during his
treatment.
Despite the fact that mouth rinses are less effective and remains in contact with the
internal portion of the mouth for a very short time, mouth rinses were also suggested to the
patient since he had issues with sore and very dry mouth. Mr. X was instructed to to use the moth
rinses for at least four times a day and swilled around the rinse for a long amount of time in the
mouth and then swallow it.
Considering the fact that Mr. X was suffering from fungal infection, he was treated with
three antifungal drugs. The name of the first drug is Nizoral which is taken for acidic food or
drinks (Cassone and Cauda 2012). The other two medications includes Sporanox which has great
potential to interact with HIV medicines) and Diflucan for later use.
Common side effects of the oral drugs given to Mr. X were nausea, belly pain and
vomiting. Other side effects includes drowsiness, dizziness, headaches, changed taste sensation
and rashes (Patel et al. 2012). Apart from these side effects, serious issues like liver toxicity
though very rare may happen (Kwamin et al. 2013). However, in case of Mr. X, no side effects
mild or severe, has been seen.
After treating the student for half a month, major improve of his fungal infection was
noticed. In order to prevent the reoccurrence of the fungal infection, the patient was educated and
thoroughly observed. After each meal, it was observed that whether Mr. X is brushing his teeth
or not. The brush provided had soft bristles in order to avoid oral trauma (Armstrong-James,
Meintjes and Brown 2014). Secondly, Mr. X was asked to wash his mouth thoroughly before
using the liquid medications or lozenges. Thirdly, no hot or spicy food are served to him since he
chewed as a whole. Mr. X followed the instructions given to him thoroughly during his
treatment.
Despite the fact that mouth rinses are less effective and remains in contact with the
internal portion of the mouth for a very short time, mouth rinses were also suggested to the
patient since he had issues with sore and very dry mouth. Mr. X was instructed to to use the moth
rinses for at least four times a day and swilled around the rinse for a long amount of time in the
mouth and then swallow it.
Considering the fact that Mr. X was suffering from fungal infection, he was treated with
three antifungal drugs. The name of the first drug is Nizoral which is taken for acidic food or
drinks (Cassone and Cauda 2012). The other two medications includes Sporanox which has great
potential to interact with HIV medicines) and Diflucan for later use.
Common side effects of the oral drugs given to Mr. X were nausea, belly pain and
vomiting. Other side effects includes drowsiness, dizziness, headaches, changed taste sensation
and rashes (Patel et al. 2012). Apart from these side effects, serious issues like liver toxicity
though very rare may happen (Kwamin et al. 2013). However, in case of Mr. X, no side effects
mild or severe, has been seen.
After treating the student for half a month, major improve of his fungal infection was
noticed. In order to prevent the reoccurrence of the fungal infection, the patient was educated and
thoroughly observed. After each meal, it was observed that whether Mr. X is brushing his teeth
or not. The brush provided had soft bristles in order to avoid oral trauma (Armstrong-James,
Meintjes and Brown 2014). Secondly, Mr. X was asked to wash his mouth thoroughly before
using the liquid medications or lozenges. Thirdly, no hot or spicy food are served to him since he
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ADULTS WITH LONG TERM DISEASE
was suffering from the oral disease. Fourthly, no sugar containing food and alcohol was provided
to him since alcohol is converted to sugar and sugar helps in the growth of Candida. Milk and
yogurt was provided to him since it contains acidophilus bacteria that are friendly bacteria and
helps the body to fight against Candida. Limited amount of garlic pills were provided to him
since large amount of garlic, though helpful to reduce fungal infections, may interfere with his
HIV medications (Pappas et al. 2015).
After the complition of his treatment, Mr. X was totally cured of oropharyngeal
candidiasis. Initially, when he was detected to have oropharyngeal candidiasis, he was suffering
from issues like burning sensation in the mouth and throat, major discomfort and with an altered
sense of poor taste as mentioned earlier. He also had creamy white spots in his mouth and throat
that can be removed by lightly scrapping on the spot. Other issues like cracking, soreness,
redness and swelling in the corner of the mouth was also reported by him. All these issues were
solved at the end of the medication. However, before discharging, Mr. X was suggested to
continue with the mouth rinses daily for four times in order to prevent the re occurrence of the
disease. He was also suggested to maintain the food habits that he used to follow in the health
care home even after being discharged.
From the essay, it can be concluded that in spite of the fact that AIDS is an incurable
disease and it had become more powerful due to tuberculosis in case of Mr. X, fight for survival
should not be stopped. Despite the fact that HIV is incurable, hazardous effects of the disease can
be reduce largely by taking proper medical support. Tuberculosis, even when it is in an active
stage can be cured with the help of Tuberculosis Preventive Treatment (TPT). Unfortunately,
patients like Mr. X who are suffering from HIV goes through several psychological issues along
with their already existing physical agony. The social discrimination which includes being
was suffering from the oral disease. Fourthly, no sugar containing food and alcohol was provided
to him since alcohol is converted to sugar and sugar helps in the growth of Candida. Milk and
yogurt was provided to him since it contains acidophilus bacteria that are friendly bacteria and
helps the body to fight against Candida. Limited amount of garlic pills were provided to him
since large amount of garlic, though helpful to reduce fungal infections, may interfere with his
HIV medications (Pappas et al. 2015).
After the complition of his treatment, Mr. X was totally cured of oropharyngeal
candidiasis. Initially, when he was detected to have oropharyngeal candidiasis, he was suffering
from issues like burning sensation in the mouth and throat, major discomfort and with an altered
sense of poor taste as mentioned earlier. He also had creamy white spots in his mouth and throat
that can be removed by lightly scrapping on the spot. Other issues like cracking, soreness,
redness and swelling in the corner of the mouth was also reported by him. All these issues were
solved at the end of the medication. However, before discharging, Mr. X was suggested to
continue with the mouth rinses daily for four times in order to prevent the re occurrence of the
disease. He was also suggested to maintain the food habits that he used to follow in the health
care home even after being discharged.
From the essay, it can be concluded that in spite of the fact that AIDS is an incurable
disease and it had become more powerful due to tuberculosis in case of Mr. X, fight for survival
should not be stopped. Despite the fact that HIV is incurable, hazardous effects of the disease can
be reduce largely by taking proper medical support. Tuberculosis, even when it is in an active
stage can be cured with the help of Tuberculosis Preventive Treatment (TPT). Unfortunately,
patients like Mr. X who are suffering from HIV goes through several psychological issues along
with their already existing physical agony. The social discrimination which includes being
8NURSING ADULTS WITH LONG TERM DISEASE
avoided or abused by friends and family, as in the case of Mr. X, creates a major stress in the
mind of the patient. Not only tuberculosis, Mr. X was also suffering from oropharyngeal
candidiasis. Though he was in a moderate stage of the oral disease, the disease could have
reached a severe stage if not treated properly. Because of the fact that Mr. X had thoroughly
followed all the instructions given to him he was able to recover within a span of a month.
However, Mr. X needs to follow all the instructions given to him in order to prevent the re
occurrence of the disease. Thus, it can be said that, Mr. X is completely cured of both
Tuberculosis and oropharyngeal candidiasis. . Finally, it can be said, though incurable, being
diagnosed with HIV does not means the end of one’s life. Examples of several individuals are
there who are leading a joyful life and dealing with the fatal disease simultaneously.
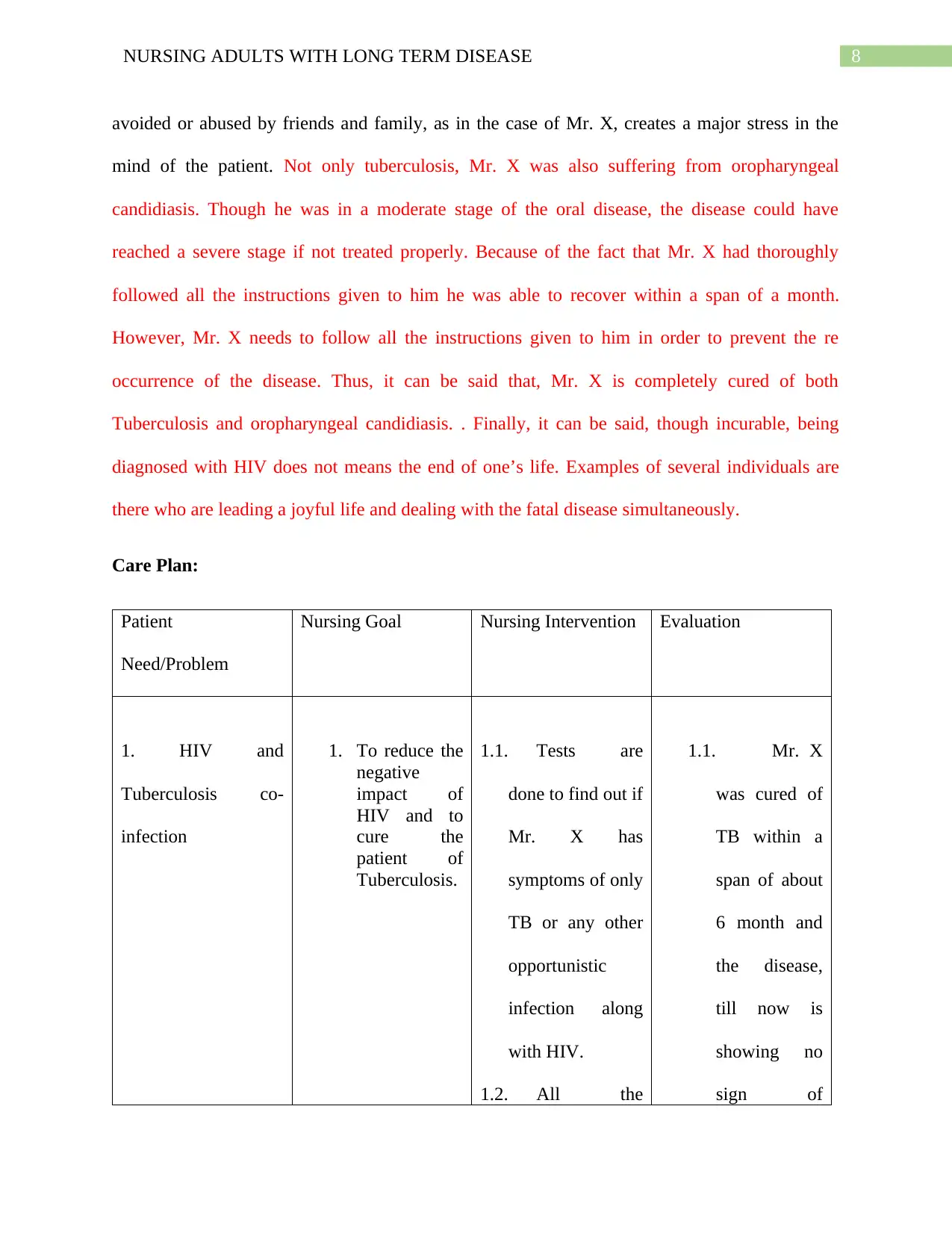
Care Plan:
Patient
Need/Problem
Nursing Goal Nursing Intervention Evaluation
1. HIV and
Tuberculosis co-
infection
1. To reduce the
negative
impact of
HIV and to
cure the
patient of
Tuberculosis.
1.1. Tests are
done to find out if
Mr. X has
symptoms of only
TB or any other
opportunistic
infection along
with HIV.
1.2. All the
1.1. Mr. X
was cured of
TB within a
span of about
6 month and
the disease,
till now is
showing no
sign of
avoided or abused by friends and family, as in the case of Mr. X, creates a major stress in the
mind of the patient. Not only tuberculosis, Mr. X was also suffering from oropharyngeal
candidiasis. Though he was in a moderate stage of the oral disease, the disease could have
reached a severe stage if not treated properly. Because of the fact that Mr. X had thoroughly
followed all the instructions given to him he was able to recover within a span of a month.
However, Mr. X needs to follow all the instructions given to him in order to prevent the re
occurrence of the disease. Thus, it can be said that, Mr. X is completely cured of both
Tuberculosis and oropharyngeal candidiasis. . Finally, it can be said, though incurable, being
diagnosed with HIV does not means the end of one’s life. Examples of several individuals are
there who are leading a joyful life and dealing with the fatal disease simultaneously.
Care Plan:
Patient
Need/Problem
Nursing Goal Nursing Intervention Evaluation
1. HIV and
Tuberculosis co-
infection
1. To reduce the
negative
impact of
HIV and to
cure the
patient of
Tuberculosis.
1.1. Tests are
done to find out if
Mr. X has
symptoms of only
TB or any other
opportunistic
infection along
with HIV.
1.2. All the
1.1. Mr. X
was cured of
TB within a
span of about
6 month and
the disease,
till now is
showing no
sign of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
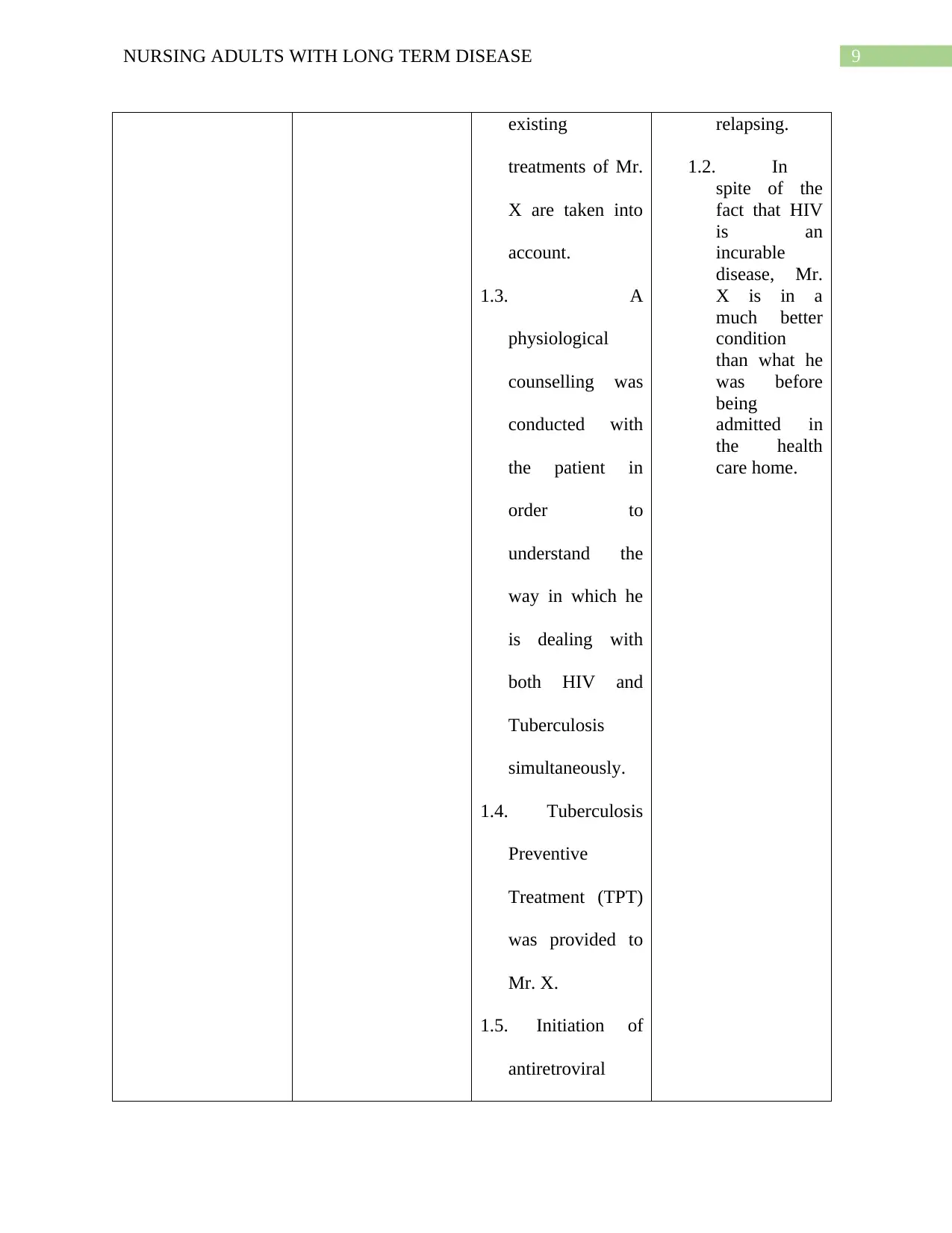
9NURSING ADULTS WITH LONG TERM DISEASE
existing
treatments of Mr.
X are taken into
account.
1.3. A
physiological
counselling was
conducted with
the patient in
order to
understand the
way in which he
is dealing with
both HIV and
Tuberculosis
simultaneously.
1.4. Tuberculosis
Preventive
Treatment (TPT)
was provided to
Mr. X.
1.5. Initiation of
antiretroviral
relapsing.
1.2. In
spite of the
fact that HIV
is an
incurable
disease, Mr.
X is in a
much better
condition
than what he
was before
being
admitted in
the health
care home.
existing
treatments of Mr.
X are taken into
account.
1.3. A
physiological
counselling was
conducted with
the patient in
order to
understand the
way in which he
is dealing with
both HIV and
Tuberculosis
simultaneously.
1.4. Tuberculosis
Preventive
Treatment (TPT)
was provided to
Mr. X.
1.5. Initiation of
antiretroviral
relapsing.
1.2. In
spite of the
fact that HIV
is an
incurable
disease, Mr.
X is in a
much better
condition
than what he
was before
being
admitted in
the health
care home.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
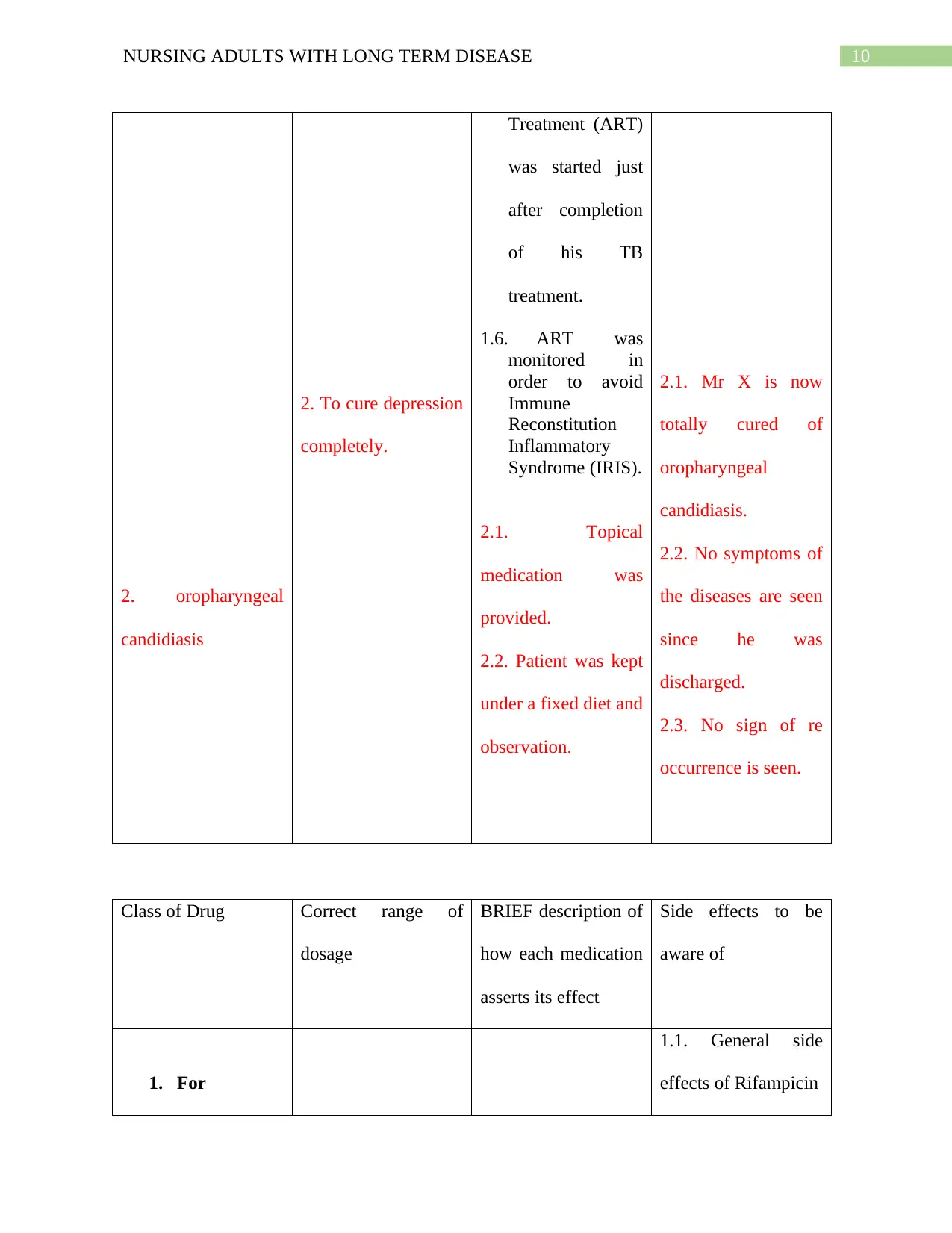
10NURSING ADULTS WITH LONG TERM DISEASE
2. oropharyngeal
candidiasis
2. To cure depression
completely.
Treatment (ART)
was started just
after completion
of his TB
treatment.
1.6. ART was
monitored in
order to avoid
Immune
Reconstitution
Inflammatory
Syndrome (IRIS).
2.1. Topical
medication was
provided.
2.2. Patient was kept
under a fixed diet and
observation.
2.1. Mr X is now
totally cured of
oropharyngeal
candidiasis.
2.2. No symptoms of
the diseases are seen
since he was
discharged.
2.3. No sign of re
occurrence is seen.
Class of Drug Correct range of
dosage
BRIEF description of
how each medication
asserts its effect
Side effects to be
aware of
1. For
1.1. General side
effects of Rifampicin
2. oropharyngeal
candidiasis
2. To cure depression
completely.
Treatment (ART)
was started just
after completion
of his TB
treatment.
1.6. ART was
monitored in
order to avoid
Immune
Reconstitution
Inflammatory
Syndrome (IRIS).
2.1. Topical
medication was
provided.
2.2. Patient was kept
under a fixed diet and
observation.
2.1. Mr X is now
totally cured of
oropharyngeal
candidiasis.
2.2. No symptoms of
the diseases are seen
since he was
discharged.
2.3. No sign of re
occurrence is seen.
Class of Drug Correct range of
dosage
BRIEF description of
how each medication
asserts its effect
Side effects to be
aware of
1. For
1.1. General side
effects of Rifampicin
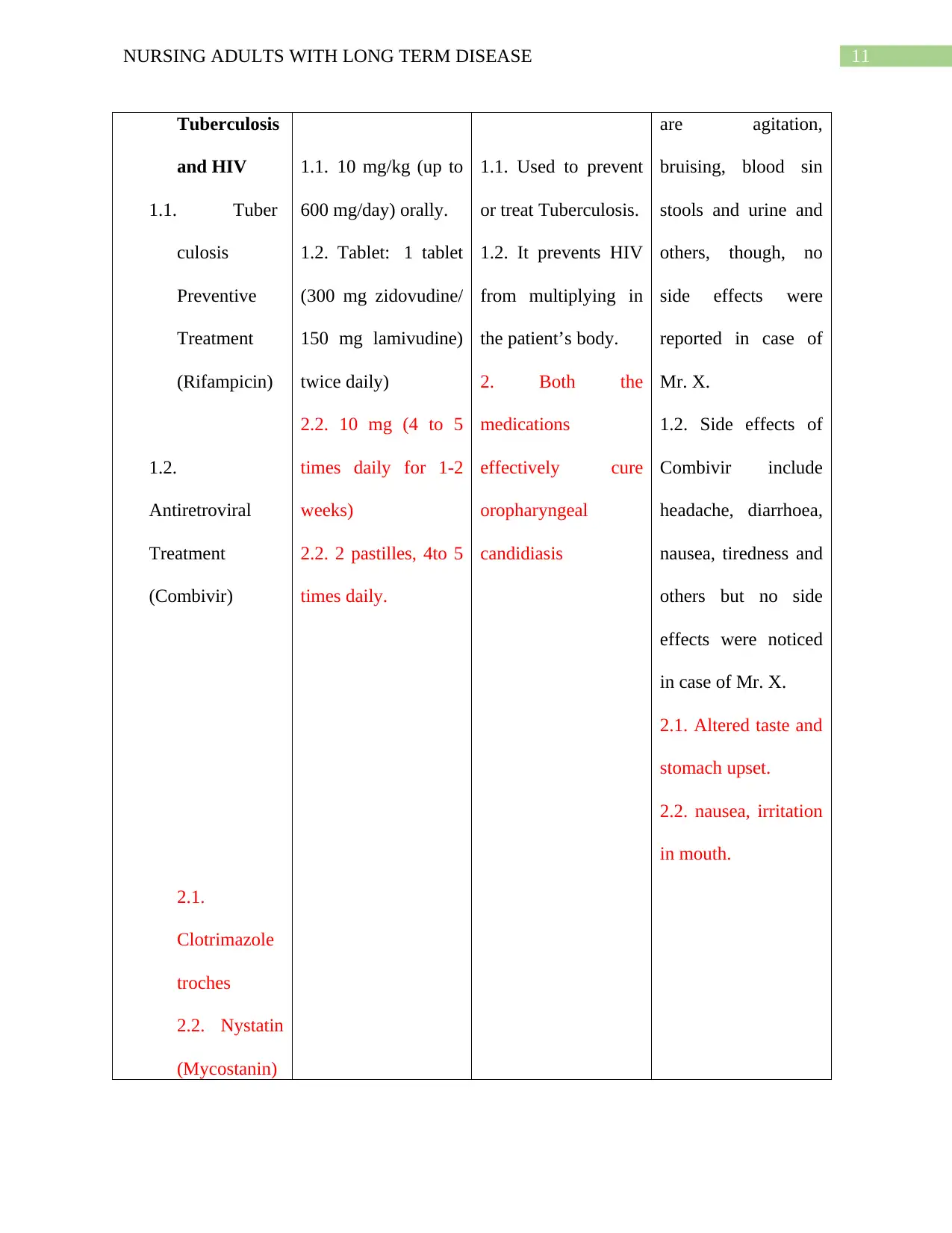
11NURSING ADULTS WITH LONG TERM DISEASE
Tuberculosis
and HIV
1.1. Tuber
culosis
Preventive
Treatment
(Rifampicin)
1.2.
Antiretroviral
Treatment
(Combivir)
2.1.
Clotrimazole
troches
2.2. Nystatin
(Mycostanin)
1.1. 10 mg/kg (up to
600 mg/day) orally.
1.2. Tablet: 1 tablet
(300 mg zidovudine/
150 mg lamivudine)
twice daily)
2.2. 10 mg (4 to 5
times daily for 1-2
weeks)
2.2. 2 pastilles, 4to 5
times daily.
1.1. Used to prevent
or treat Tuberculosis.
1.2. It prevents HIV
from multiplying in
the patient’s body.
2. Both the
medications
effectively cure
oropharyngeal
candidiasis
are agitation,
bruising, blood sin
stools and urine and
others, though, no
side effects were
reported in case of
Mr. X.
1.2. Side effects of
Combivir include
headache, diarrhoea,
nausea, tiredness and
others but no side
effects were noticed
in case of Mr. X.
2.1. Altered taste and
stomach upset.
2.2. nausea, irritation
in mouth.
Tuberculosis
and HIV
1.1. Tuber
culosis
Preventive
Treatment
(Rifampicin)
1.2.
Antiretroviral
Treatment
(Combivir)
2.1.
Clotrimazole
troches
2.2. Nystatin
(Mycostanin)
1.1. 10 mg/kg (up to
600 mg/day) orally.
1.2. Tablet: 1 tablet
(300 mg zidovudine/
150 mg lamivudine)
twice daily)
2.2. 10 mg (4 to 5
times daily for 1-2
weeks)
2.2. 2 pastilles, 4to 5
times daily.
1.1. Used to prevent
or treat Tuberculosis.
1.2. It prevents HIV
from multiplying in
the patient’s body.
2. Both the
medications
effectively cure
oropharyngeal
candidiasis
are agitation,
bruising, blood sin
stools and urine and
others, though, no
side effects were
reported in case of
Mr. X.
1.2. Side effects of
Combivir include
headache, diarrhoea,
nausea, tiredness and
others but no side
effects were noticed
in case of Mr. X.
2.1. Altered taste and
stomach upset.
2.2. nausea, irritation
in mouth.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





