HLTENN008: Applying Legal and Ethical Parameters to Nursing
VerifiedAdded on 2023/06/09
|12
|4865
|452
Homework Assignment
AI Summary
This assignment provides a detailed exploration of legal and ethical parameters in nursing practice, focusing on key definitions, theoretical concepts, and legal terms relevant to the field. It covers ethics, bioethics, and nursing ethics, along with ethical theories like consequentialism and deontological ethics. The assignment also explains various legal terms such as civil law, common law, statute law, precedent, law of torts, negligence, assault, battery, legal capacity, intellectual capacity, clinical incapacity, false imprisonment, defamation, vicarious liability, defendant, plaintiff, harassment, expert witness, and coronial inquests. Furthermore, it describes the Australian court hierarchy and identifies sources for accessing Australian legislation. The assignment addresses requirements for valid consent, differences between implied and expressed consent, the functions of the coroner, and professional aspects breached in specific nursing scenarios, including vicarious liability and the importance of obtaining patient consent. It also outlines legal requirements for writing nursing reports, emphasizing regulatory guidelines and ethical principles.
Attention Students:
This is an editable word document.
This word copy of assessment is for student to work offline. Please DO NOT
upload this document in Student Hub. You can copy and paste answers
from this word document to your online assessment.
Assessments
Student : Theresa Smith - S1814604
Course : Diploma of Nursing
Course
Offer : 18VDONB6
Course
Unit : HLTENN008 Apply legal and ethical parameters to nursing
practice
Assessm
ent type : Theory Assessment
1. Define the following terms:
1.1
Ethics: Ethics is the prescribed and accepted code of behaviour in the nursing
field.
1.2
Bioethics: Bioethics refers to the study of ethical concerns emerging from
advances in nursing policy and practice.
1.3
Nursing ethics: This is a branch of applied of ethics which mainly studies activities
in nursing field.
Reference: Armstrong, A. E. (2006). Towards a strong virtue ethics for nursing
practice. Nursing Philosophy, 7(3), 110-124.
2. Different ethical theories exist and theories can be applied
to different situations to inform our thinking and support
decision making. Describe the following theoretical concepts
related to ethical conduct (in 25-40 words each).
2.1
Consequentialism: In normative ethical theories, Consequentialism asserts that the
consequences of an individual’s behaviour are the final basis for any judgement
about the wrongness or the rightness of their behaviour.
2.2
Deontological (duty-based) ethics: This is an approach to ethics which
This is an editable word document.
This word copy of assessment is for student to work offline. Please DO NOT
upload this document in Student Hub. You can copy and paste answers
from this word document to your online assessment.
Assessments
Student : Theresa Smith - S1814604
Course : Diploma of Nursing
Course
Offer : 18VDONB6
Course
Unit : HLTENN008 Apply legal and ethical parameters to nursing
practice
Assessm
ent type : Theory Assessment
1. Define the following terms:
1.1
Ethics: Ethics is the prescribed and accepted code of behaviour in the nursing
field.
1.2
Bioethics: Bioethics refers to the study of ethical concerns emerging from
advances in nursing policy and practice.
1.3
Nursing ethics: This is a branch of applied of ethics which mainly studies activities
in nursing field.
Reference: Armstrong, A. E. (2006). Towards a strong virtue ethics for nursing
practice. Nursing Philosophy, 7(3), 110-124.
2. Different ethical theories exist and theories can be applied
to different situations to inform our thinking and support
decision making. Describe the following theoretical concepts
related to ethical conduct (in 25-40 words each).
2.1
Consequentialism: In normative ethical theories, Consequentialism asserts that the
consequences of an individual’s behaviour are the final basis for any judgement
about the wrongness or the rightness of their behaviour.
2.2
Deontological (duty-based) ethics: This is an approach to ethics which
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
concentrates on the wrongness or the rightness themselves as opposed to the
wrongness or the rightness of the consequences of the particular actions.
References: Alexander, L., & Moore, M. (2007). Deontological ethics.
3. You must use correct common legal terms associated with
nursing practice, and correctly interpret their meaning
irrespective of the area in which you are working. Describe
the following legal terms and types of law:
3.1
Civil law: Civil law requires nurses involved in malpractices such as wrongful
discharge to be impelled to compensate individuals affected by their actions.
3.2
Common law: Common law is derived from social mores or principles and consists
of wide, interpretive dogmas based on systematic reasoning, common sense and
traditional justice.
3.3
Statute law: Statute law refers to legislation passed by either State Parliament or
Federal Parliament touching on an issue revolving around the nursing field.
3.4
Precedent: In nursing, Precedent refers to an action, a verdict or a ruling which
might be used as an example to be adhered in the future.
3.5
Law of torts: In common law, torts are malpractices committed by a nurse such as
invasion of privacy and make the victim to suffer either physically or mentally.
3.6
Negligence: This can be described as a nurse’s failure to take reasonable steps or
care to curb an injury or a loss to a patient making him or her suffer unnecessarily.
3.7
Assault: This is an intentional or an unlawful direct of force to a patient instigated
by a nurse meant to create fear or threat. An example is threatening them verbally
or pretending to hit them.
3.8
Battery: This occurs when a nurse intentionally causes harm to someone. It is a
criminal offense and can lead to civil lawsuit.
3.9
Legal capacity: This is a nurse’s ability to make a binding contract, make decisions
of a legal nature or sue another person.
3.10
Intellectual capacity: The Intellectual Capacity Act 2005 (MCA) provided nurses
attending to patients with impaired capacity to make decisions or rationalize a
framework within which to work to alleviate their conditions.
3.11
Clinical incapacity: Clinical incapacity to make treatment decisions refers to the
medical judgement of a qualified nurse who determines an individual is not able
to: comprehend his or her medical conditions or the substantial benefits and perils
of proposed treatment and its alternatives.
3.12
wrongness or the rightness of the consequences of the particular actions.
References: Alexander, L., & Moore, M. (2007). Deontological ethics.
3. You must use correct common legal terms associated with
nursing practice, and correctly interpret their meaning
irrespective of the area in which you are working. Describe
the following legal terms and types of law:
3.1
Civil law: Civil law requires nurses involved in malpractices such as wrongful
discharge to be impelled to compensate individuals affected by their actions.
3.2
Common law: Common law is derived from social mores or principles and consists
of wide, interpretive dogmas based on systematic reasoning, common sense and
traditional justice.
3.3
Statute law: Statute law refers to legislation passed by either State Parliament or
Federal Parliament touching on an issue revolving around the nursing field.
3.4
Precedent: In nursing, Precedent refers to an action, a verdict or a ruling which
might be used as an example to be adhered in the future.
3.5
Law of torts: In common law, torts are malpractices committed by a nurse such as
invasion of privacy and make the victim to suffer either physically or mentally.
3.6
Negligence: This can be described as a nurse’s failure to take reasonable steps or
care to curb an injury or a loss to a patient making him or her suffer unnecessarily.
3.7
Assault: This is an intentional or an unlawful direct of force to a patient instigated
by a nurse meant to create fear or threat. An example is threatening them verbally
or pretending to hit them.
3.8
Battery: This occurs when a nurse intentionally causes harm to someone. It is a
criminal offense and can lead to civil lawsuit.
3.9
Legal capacity: This is a nurse’s ability to make a binding contract, make decisions
of a legal nature or sue another person.
3.10
Intellectual capacity: The Intellectual Capacity Act 2005 (MCA) provided nurses
attending to patients with impaired capacity to make decisions or rationalize a
framework within which to work to alleviate their conditions.
3.11
Clinical incapacity: Clinical incapacity to make treatment decisions refers to the
medical judgement of a qualified nurse who determines an individual is not able
to: comprehend his or her medical conditions or the substantial benefits and perils
of proposed treatment and its alternatives.
3.12
False imprisonment: In the nursing field, false imprisonment takes place whenever
a person (who does not have legal authority or justification) keeps a patient
involuntarily or against his will in a nursing home, hospital, or other health
institution or facility, or even in an ambulance.
3.13
Defamation: This happens when a healthcare practitioner say a nurse publishes a
false statement which lowers the reputation of an individual before the right-
thinking society members. For such a published statement to be deemed
defamatory, it must meet particular legislative requirements that of course vary
from a country to another.
3.14
Vicarious liability: This refers to a condition when a person is held answerable for
the omissions or actions of another individual. In a nursing context, a nurse can be
held responsible for the actions or omissions of other nurses working under them,
provided that they happened under their directions as employers.
3.15
Defendant: In nursing criminal cases, a defendant refers to a person accused of an
offense. A defendant can either be an individual or an organization.
3.16
Plaintiff: In nursing criminal cases, a plaintiff is a person who files a case against
the defendant in a court of law.
3.17
Harassment: Harassment in the field of nursing takes place when a health
practitioner aggressively pressurizes or intimidates another person say the patient
or a co-worker.
3.18
Expert witness: This is a person whose level of specialization skills or knowledge in
nursing matters inhibits or disqualifies them from presenting their viewpoints
about the facts of a case during legal proceedings.
3.19
Coronial inquests: In nursing, Coronial inquests refer to public hearings held to
scrutinize the circumstances and cause revolving around the demise of a patient in
unnatural or unusual circumstances. Inquests are normally done by magistrates
acting as coroners.
References: Avery, G. (2016). Law and Ethics in Nursing and Healthcare: An
Introduction. SAGE.
Rodger, D. (2018). Law and Ethics in Nursing and Healthcare: An
Introduction.
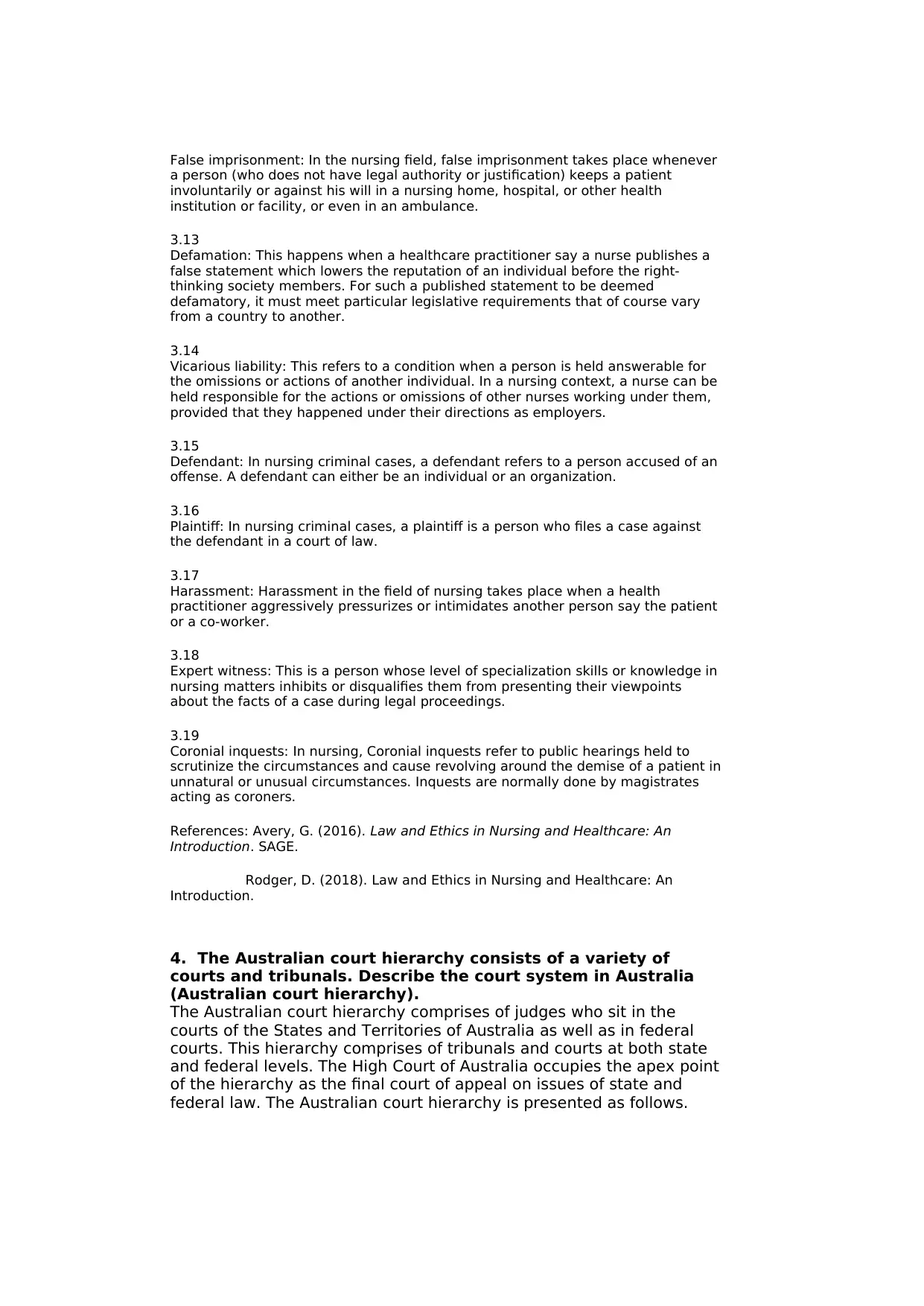
4. The Australian court hierarchy consists of a variety of
courts and tribunals. Describe the court system in Australia
(Australian court hierarchy).
The Australian court hierarchy comprises of judges who sit in the
courts of the States and Territories of Australia as well as in federal
courts. This hierarchy comprises of tribunals and courts at both state
and federal levels. The High Court of Australia occupies the apex point
of the hierarchy as the final court of appeal on issues of state and
federal law. The Australian court hierarchy is presented as follows.
a person (who does not have legal authority or justification) keeps a patient
involuntarily or against his will in a nursing home, hospital, or other health
institution or facility, or even in an ambulance.
3.13
Defamation: This happens when a healthcare practitioner say a nurse publishes a
false statement which lowers the reputation of an individual before the right-
thinking society members. For such a published statement to be deemed
defamatory, it must meet particular legislative requirements that of course vary
from a country to another.
3.14
Vicarious liability: This refers to a condition when a person is held answerable for
the omissions or actions of another individual. In a nursing context, a nurse can be
held responsible for the actions or omissions of other nurses working under them,
provided that they happened under their directions as employers.
3.15
Defendant: In nursing criminal cases, a defendant refers to a person accused of an
offense. A defendant can either be an individual or an organization.
3.16
Plaintiff: In nursing criminal cases, a plaintiff is a person who files a case against
the defendant in a court of law.
3.17
Harassment: Harassment in the field of nursing takes place when a health
practitioner aggressively pressurizes or intimidates another person say the patient
or a co-worker.
3.18
Expert witness: This is a person whose level of specialization skills or knowledge in
nursing matters inhibits or disqualifies them from presenting their viewpoints
about the facts of a case during legal proceedings.
3.19
Coronial inquests: In nursing, Coronial inquests refer to public hearings held to
scrutinize the circumstances and cause revolving around the demise of a patient in
unnatural or unusual circumstances. Inquests are normally done by magistrates
acting as coroners.
References: Avery, G. (2016). Law and Ethics in Nursing and Healthcare: An
Introduction. SAGE.
Rodger, D. (2018). Law and Ethics in Nursing and Healthcare: An
Introduction.
4. The Australian court hierarchy consists of a variety of
courts and tribunals. Describe the court system in Australia
(Australian court hierarchy).
The Australian court hierarchy comprises of judges who sit in the
courts of the States and Territories of Australia as well as in federal
courts. This hierarchy comprises of tribunals and courts at both state
and federal levels. The High Court of Australia occupies the apex point
of the hierarchy as the final court of appeal on issues of state and
federal law. The Australian court hierarchy is presented as follows.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References: Mack, K., & Roach Anleu, S. (2012). Entering the
Australian judiciary: Gender and court hierarchy. Law & Policy, 34(3),
313-347.
5. Identify and describe 2 (two) sources you could refer to in
accessing information related to Australian legislation and
Australian judiciary: Gender and court hierarchy. Law & Policy, 34(3),
313-347.
5. Identify and describe 2 (two) sources you could refer to in
accessing information related to Australian legislation and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
supporting documentation.
I would refer to the Constitution of the Commonwealth of Australia
and the Infosheet document containing the Australian Acts of
Parliament. These two sources have been sanctioned in a series of
referendums as having legislative significance for Australia.
Reference: Aroney, N. (2009). The constitution of a federal
commonwealth: The making and meaning of the Australian
constitution. Cambridge University Press.
6. For a patient's consent to be valid a number of criteria will
need to be met. Briefly describe 2 (two) requirements of
obtaining a valid consent.
For a patient’s consent to be deemed valid it must be informed and
voluntary and the individual consenting should have the capacity to
reason and make decisions. He or she must be able to understand the
information presented to them and use it to make informed decisions.
Again, the person should do so without coercion or any other form of
external stimuli.
Reference: Ramlaul, A., & Vosper, M. (2013). Patient Centered Care in
Medical Imaging and Radiotherapy E-Book. Elsevier Health Sciences.
7. Explain the difference between implied consent and
expressed consent (in 30-40 words).
Expressed consent takes place when a patient communicates his or
her permission directly and clearly. This can include signing medical
waivers to give consent for a certain treatment or making clear verbal
statements. On the other hand, implied consent is relayed through
actions thus unlike the former it is hard to prove in a legal context. It
can be done by nodding or by rolling up your sleeve to receive an
injection.
Reference: Cowdrey, M. L., & Drew, M. (2015). Basic Law for the Allied
Health Professions. Jones & Bartlett Learning.
8. Briefly describe the functions of the coroner in relation to a
healthcare event (in 30-40 words).
Coroners investigate particular forms of demises in attempt to
determine the identity of the dead person, circumstances, place, date
and medical cause of death. He or she may also order an inquest into
the manner or the main cause of demise within his jurisdiction.
Reference: Moore, J. (2014). Coroners’ recommendations about
healthcare-related deaths as a potential tool for improving patient
safety and quality of care. NZ Med J, 127(1398), 35-53.
9. When is it required to give evidence to the coroner and
what types of evidence could you provide?
I might be required to provide evidence to the coroner especially if the
type of death which has occurred does not fall precisely within the
category of deaths the coroner has perfected on investigating and
also when it has occurred outside his jurisdiction. In such cases then I
will be prompted to provide relevant information that will assist the
I would refer to the Constitution of the Commonwealth of Australia
and the Infosheet document containing the Australian Acts of
Parliament. These two sources have been sanctioned in a series of
referendums as having legislative significance for Australia.
Reference: Aroney, N. (2009). The constitution of a federal
commonwealth: The making and meaning of the Australian
constitution. Cambridge University Press.
6. For a patient's consent to be valid a number of criteria will
need to be met. Briefly describe 2 (two) requirements of
obtaining a valid consent.
For a patient’s consent to be deemed valid it must be informed and
voluntary and the individual consenting should have the capacity to
reason and make decisions. He or she must be able to understand the
information presented to them and use it to make informed decisions.
Again, the person should do so without coercion or any other form of
external stimuli.
Reference: Ramlaul, A., & Vosper, M. (2013). Patient Centered Care in
Medical Imaging and Radiotherapy E-Book. Elsevier Health Sciences.
7. Explain the difference between implied consent and
expressed consent (in 30-40 words).
Expressed consent takes place when a patient communicates his or
her permission directly and clearly. This can include signing medical
waivers to give consent for a certain treatment or making clear verbal
statements. On the other hand, implied consent is relayed through
actions thus unlike the former it is hard to prove in a legal context. It
can be done by nodding or by rolling up your sleeve to receive an
injection.
Reference: Cowdrey, M. L., & Drew, M. (2015). Basic Law for the Allied
Health Professions. Jones & Bartlett Learning.
8. Briefly describe the functions of the coroner in relation to a
healthcare event (in 30-40 words).
Coroners investigate particular forms of demises in attempt to
determine the identity of the dead person, circumstances, place, date
and medical cause of death. He or she may also order an inquest into
the manner or the main cause of demise within his jurisdiction.
Reference: Moore, J. (2014). Coroners’ recommendations about
healthcare-related deaths as a potential tool for improving patient
safety and quality of care. NZ Med J, 127(1398), 35-53.
9. When is it required to give evidence to the coroner and
what types of evidence could you provide?
I might be required to provide evidence to the coroner especially if the
type of death which has occurred does not fall precisely within the
category of deaths the coroner has perfected on investigating and
also when it has occurred outside his jurisdiction. In such cases then I
will be prompted to provide relevant information that will assist the
coroner in the investigation process. Also, as a nurse I can be
summoned to give evidence concerning the care given before the
death.
Reference: Freckelton, I., & Ranson, D. (2006). Death investigation
and the coroner's inquest.
10. You noticed that the nurse allocated to take care of
residents on the west wing is not attending to the call bell
requests made by residents. You asked the nurse why the call
bells are not answered. The nurse asked you to ignore it.
Describe 2 (two) professional aspects breached by the nurse
in this scenario (in 30-40 words).
Due to the nurse’s negligence, it can be said that he or she is
breaching the professional duty of care due to the failure to take
reasonable care or steps to prevent injury or suffering of the patients.
Besides, the nurse is breaching the ethical professional aspect of his
or her work by failing to observe the nursing standards of care.
Reference: Ulrich, C. M., Taylor, C., Soeken, K., O’Donnell, P., Farrar,
A., Danis, M., & Grady, C. (2010). Everyday ethics: ethical issues and
stress in nursing practice. Journal of advanced nursing, 66(11), 2510-
2519.
11. The registered nurse asked a student nurse to assist a
resident with shaving. The student nurse is asked to perform
the task without anyone supervising her. Applying the
concept of vicarious liability, explain who will be held
responsible for the actions or omissions of the student nurse?
Will that be the student nurses herself or the registered
nurse? (in 30-40 words).
As described earlier, vicarious liability takes effect when the
subordinate becomes answerable for the activities of another party
whom they had full ability and capability to control the actions of a
violator. So in this case scenario, the registered nurse will be held
responsible for the actions or omissions of the student nurse.
Reference: Booth, J. W. (2007). An Update on Vicarious Liability for
Certified Nurse‐Midwives/Certified Midwives. Journal of midwifery &
women's health, 52(2), 153-157.
12. You are asked by the registered nurse to provide oral
care to a resident. When should you obtain consent from the
resident to proceed with the care? (in 20-30 words).
Despite the prior request by the registered nurse to provide oral care,
it is important to inform the patient and request for her participation
in the healthcare decision, the nature of the decision as well as
reasonable alternatives to be proposed.
Reference:
Reference: Collins, J. W., Wolf, L., Bell, J., & Evanoff, B. (2004). An
evaluation of a “best practices” musculoskeletal injury prevention
program in nursing homes. Injury Prevention, 10(4), 206-211.
13. Identify and outline 2 (two) legal requirements you must
apply when writing nursing reports.
summoned to give evidence concerning the care given before the
death.
Reference: Freckelton, I., & Ranson, D. (2006). Death investigation
and the coroner's inquest.
10. You noticed that the nurse allocated to take care of
residents on the west wing is not attending to the call bell
requests made by residents. You asked the nurse why the call
bells are not answered. The nurse asked you to ignore it.
Describe 2 (two) professional aspects breached by the nurse
in this scenario (in 30-40 words).
Due to the nurse’s negligence, it can be said that he or she is
breaching the professional duty of care due to the failure to take
reasonable care or steps to prevent injury or suffering of the patients.
Besides, the nurse is breaching the ethical professional aspect of his
or her work by failing to observe the nursing standards of care.
Reference: Ulrich, C. M., Taylor, C., Soeken, K., O’Donnell, P., Farrar,
A., Danis, M., & Grady, C. (2010). Everyday ethics: ethical issues and
stress in nursing practice. Journal of advanced nursing, 66(11), 2510-
2519.
11. The registered nurse asked a student nurse to assist a
resident with shaving. The student nurse is asked to perform
the task without anyone supervising her. Applying the
concept of vicarious liability, explain who will be held
responsible for the actions or omissions of the student nurse?
Will that be the student nurses herself or the registered
nurse? (in 30-40 words).
As described earlier, vicarious liability takes effect when the
subordinate becomes answerable for the activities of another party
whom they had full ability and capability to control the actions of a
violator. So in this case scenario, the registered nurse will be held
responsible for the actions or omissions of the student nurse.
Reference: Booth, J. W. (2007). An Update on Vicarious Liability for
Certified Nurse‐Midwives/Certified Midwives. Journal of midwifery &
women's health, 52(2), 153-157.
12. You are asked by the registered nurse to provide oral
care to a resident. When should you obtain consent from the
resident to proceed with the care? (in 20-30 words).
Despite the prior request by the registered nurse to provide oral care,
it is important to inform the patient and request for her participation
in the healthcare decision, the nature of the decision as well as
reasonable alternatives to be proposed.
Reference:
Reference: Collins, J. W., Wolf, L., Bell, J., & Evanoff, B. (2004). An
evaluation of a “best practices” musculoskeletal injury prevention
program in nursing homes. Injury Prevention, 10(4), 206-211.
13. Identify and outline 2 (two) legal requirements you must
apply when writing nursing reports.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Apply a clear comprehension of regulatory or legal
guidelines/acts as they impact on nursing practices.
Apply code of conduct, ethics and Division/Enrolled 2 nursing
competency principles in nursing practice.
References : Page, A. (Ed.). (2004). Keeping patients safe:
Transforming the work environment of nurses. National Academies
Press.
14. Whom would you seek clarification from for concerns
relating to requests for tests and referrals for your residents
in the workplace? Identify 2 (two) personnel who could assist
you.
I would seek help from:
Head of the nursing staff
Service directors
These two personnel are tasked with leadership functions of decision
making and governance within any healthcare organization.
Reference: Harris, M. D. (2005). Handbook of home health care
administration. Jones & Bartlett Learning.
15. With reference to, there are different legal and ethical
considerations underpinning nursing practice and this may
vary between States and Territories. Various legal and ethical
considerations relevant to the nursing profession are
identified below. Explain how these are applied in nursing
practice in your State/Territory (in 40-50 words each).
Contemporary ethical concepts and principles in nursing:
15.1
Autonomy: In Australia, both nurses and patients are allowed to make their own
decisions. Professionals have the mandate and freedom to make decisions and act
in accordance with their professional knowledge base. They are also expected to
respect their patients’ autonomy.
15.2
Beneficence: In healthcare, this refers to an act of kindness, charity, and charity
with an implication of doing good to other people including moral commitment. In
my state, nurses are expected to do actions which promote good. This involves
doing what is deemed best for the client.
15.3
Non-maleficence: This involves a legal and an ethical obligation to avoid causing
harm to others. Nurses are thus expected to act in ways that cannot cause
impairment or inflict evil to their patients. Particularly, they should not lead to
intentional or avoidable harm.
15.4
Justice: This ethical principle requires Australian nurses to fairly, equally, justly
give each person what he or she is due. They are supposed to treat every
individual impartially with favouritism, bias or prejudice. They should do so
regardless of economic status, citizenship, sexual orientation or ethnicity of the
other party.
15.5
Rights: Nurses are obliged to adhere to the various rights of healthcare
guidelines/acts as they impact on nursing practices.
Apply code of conduct, ethics and Division/Enrolled 2 nursing
competency principles in nursing practice.
References : Page, A. (Ed.). (2004). Keeping patients safe:
Transforming the work environment of nurses. National Academies
Press.
14. Whom would you seek clarification from for concerns
relating to requests for tests and referrals for your residents
in the workplace? Identify 2 (two) personnel who could assist
you.
I would seek help from:
Head of the nursing staff
Service directors
These two personnel are tasked with leadership functions of decision
making and governance within any healthcare organization.
Reference: Harris, M. D. (2005). Handbook of home health care
administration. Jones & Bartlett Learning.
15. With reference to, there are different legal and ethical
considerations underpinning nursing practice and this may
vary between States and Territories. Various legal and ethical
considerations relevant to the nursing profession are
identified below. Explain how these are applied in nursing
practice in your State/Territory (in 40-50 words each).
Contemporary ethical concepts and principles in nursing:
15.1
Autonomy: In Australia, both nurses and patients are allowed to make their own
decisions. Professionals have the mandate and freedom to make decisions and act
in accordance with their professional knowledge base. They are also expected to
respect their patients’ autonomy.
15.2
Beneficence: In healthcare, this refers to an act of kindness, charity, and charity
with an implication of doing good to other people including moral commitment. In
my state, nurses are expected to do actions which promote good. This involves
doing what is deemed best for the client.
15.3
Non-maleficence: This involves a legal and an ethical obligation to avoid causing
harm to others. Nurses are thus expected to act in ways that cannot cause
impairment or inflict evil to their patients. Particularly, they should not lead to
intentional or avoidable harm.
15.4
Justice: This ethical principle requires Australian nurses to fairly, equally, justly
give each person what he or she is due. They are supposed to treat every
individual impartially with favouritism, bias or prejudice. They should do so
regardless of economic status, citizenship, sexual orientation or ethnicity of the
other party.
15.5
Rights: Nurses are obliged to adhere to the various rights of healthcare
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
administration which include right dose, right documentation, right time and
frequency, right history assessment, right drug, right route, right approach and
right to privacy. They are expected by the concerned legal authorities to treat
their clients with care and observe their rights.
15.6
Veracity: This principle is based on the virtue of truth telling. Veracity is grounded
in respect for people and the ideology of autonomy. Nurses while in their lines of
duty are expected to always tell nothing but the truth regardless of what the
consequences might be.
References: ABA, A. B. A. (2007). Guidance to nurses and midwives regarding
ethical conduct of nursing and midwifery research.
16. Various pieces of legislation are enacted in each
State/Territory underpinning nursing practice. Identify the
legislation relevant to your State/Territory relating to the
following and describe how these pieces of legislation impact
your nursing practice (in 40-50 words each):
16.1
Health Practitioner Regulation National Law Act: This legislation is related to the
Health Practitioner Regulation National Law (NSW) which summarizes the core
obligations of registered health specialists and students. As a nursing student in
this jurisdiction I have the obligation to ensure a comprehensive professional
development and duly adherence to the requirements of the legislation.
16.2
Health (drugs and poisons) legislation: This legislation relates to Health (Drugs and
Poisons) Regulation 1996 – Queensland that provides standards and control to
reduce the risks associated with scheduled poisons and medicines. It provides
regulation over manufacturing, supply, selling, handling, labelling, and storage of
scheduled poisons and medicines.
16.3
Mental health legislation: This legislation relates to the Mental Health Legislation
and Human Rights which takes effect in each Australian State and Territory. This
legislation protects persons with mental disorders and ensures consistent
enhancement of Mental Health Care. As a nursing professional I have the
responsibility to take care of mentally impaired persons both within and without
my jurisdiction.
16.4
Carers recognition legislation or official policies: This one relates to the Carer
Recognition Act 2010 Guidelines that aims to augment awareness and recognition
of the role carers assume in offering everyday healthcare to individuals with
mental illness, mental conditions, disability, as well as those who are frail aged. As
a healthcare practitioner, this legislation requires me to recognize the role other
experts in combating the aforementioned maladies.
16.5
Anti-discrimination legislation: This relates to the Australia's anti-discrimination law
which fights against unlawful discrimination of persons based on their race, sex,
age, intersex status, and disability in particular areas of public life like
employment and education. This legislation obliges me to view every person as
important regardless of their special status or attributes.
16.6
frequency, right history assessment, right drug, right route, right approach and
right to privacy. They are expected by the concerned legal authorities to treat
their clients with care and observe their rights.
15.6
Veracity: This principle is based on the virtue of truth telling. Veracity is grounded
in respect for people and the ideology of autonomy. Nurses while in their lines of
duty are expected to always tell nothing but the truth regardless of what the
consequences might be.
References: ABA, A. B. A. (2007). Guidance to nurses and midwives regarding
ethical conduct of nursing and midwifery research.
16. Various pieces of legislation are enacted in each
State/Territory underpinning nursing practice. Identify the
legislation relevant to your State/Territory relating to the
following and describe how these pieces of legislation impact
your nursing practice (in 40-50 words each):
16.1
Health Practitioner Regulation National Law Act: This legislation is related to the
Health Practitioner Regulation National Law (NSW) which summarizes the core
obligations of registered health specialists and students. As a nursing student in
this jurisdiction I have the obligation to ensure a comprehensive professional
development and duly adherence to the requirements of the legislation.
16.2
Health (drugs and poisons) legislation: This legislation relates to Health (Drugs and
Poisons) Regulation 1996 – Queensland that provides standards and control to
reduce the risks associated with scheduled poisons and medicines. It provides
regulation over manufacturing, supply, selling, handling, labelling, and storage of
scheduled poisons and medicines.
16.3
Mental health legislation: This legislation relates to the Mental Health Legislation
and Human Rights which takes effect in each Australian State and Territory. This
legislation protects persons with mental disorders and ensures consistent
enhancement of Mental Health Care. As a nursing professional I have the
responsibility to take care of mentally impaired persons both within and without
my jurisdiction.
16.4
Carers recognition legislation or official policies: This one relates to the Carer
Recognition Act 2010 Guidelines that aims to augment awareness and recognition
of the role carers assume in offering everyday healthcare to individuals with
mental illness, mental conditions, disability, as well as those who are frail aged. As
a healthcare practitioner, this legislation requires me to recognize the role other
experts in combating the aforementioned maladies.
16.5
Anti-discrimination legislation: This relates to the Australia's anti-discrimination law
which fights against unlawful discrimination of persons based on their race, sex,
age, intersex status, and disability in particular areas of public life like
employment and education. This legislation obliges me to view every person as
important regardless of their special status or attributes.
16.6
Children and young people legislation: This legislation relates to the Children and
Young Persons (Care and Protection) Act 1998 which provides that young people
are in need of care and protection. The Director-General of the jurisdiction is
obliged to do whatever it takes to promote and safeguard the welfare, well-being,
and safety of the young person or child. As a nursing professional I will work hand
in hand with the Director-General to ensure this legislature is adhered to without
blemish.
16.7
Working with children legislation: This legislation relates to Working with Children
Act 2005 ('the Act') whose purpose is to check persons working with children. It is
also dutiful for the Working with Children Check, that aids decide whether people
are appropriate to work in child-related employment. This legislature enables to
comprehend that subjecting children to laborious activities may make them prone
to some ailments.
16.8
Workplace health and safety (WHS) legislation: This legislation relates to the Work
Health and Safety Act 2011which sets regulations to enhance work safety and
health of workers in Australia. The responsible regulators set out legal duties and
responsibilities to be followed by employers and business owners. As a nursing
practitioner, this legislature allows me to acknowledge the work of WHO in
campaigning for proper working environments devoid of risks or hazards.
References: Berman, A., Snyder, S. J., Kozier, B., Erb, G. L., Levett-Jones, T.,
Dwyer, T., ... & Parker, B. (2014). Kozier & Erb's Fundamentals of Nursing
Australian Edition (Vol. 3). Pearson Higher Education AU.
17. The owner of an aged care facility released the photos
and videos of a resident who had dementia without prior
consent. The resident's family filed a petition in court against
the organisation asking for compensation. What type of
penalties should a Nurse expect if found to be in breach of the
privacy act 1988 (in 30-40 words).
The nurse found at the breach of privacy might be subjected to
various penalties which differ in regards to the seriousness of the
breach. They include: dollar or Pecuniary penalties where an
individual can be forced to pay some money as a fine or an
incarceration especially when the act was intentional.
Reference: Barry, J., & Hardiker, N. (2012). Advancing nursing practice
through social media: a global perspective. OJIN: The Online Journal of
Issues in Nursing, 17(3).
18. Various clinical situations will leave you in an ethical
dilemma. Identify what ethical principles are in conflict with
regards to the following ethical dilemmas (in 30-40 words
each):
18.1
Abortion: A major ethical dilemma occurs in the question of abortion when the
woman requests for the process while it is against the principles of nursing to do
anything which can harm either the foetus or the mother. The nurse is thus left
wondering whether to help the woman abort or defile the Non-maleficence
Young Persons (Care and Protection) Act 1998 which provides that young people
are in need of care and protection. The Director-General of the jurisdiction is
obliged to do whatever it takes to promote and safeguard the welfare, well-being,
and safety of the young person or child. As a nursing professional I will work hand
in hand with the Director-General to ensure this legislature is adhered to without
blemish.
16.7
Working with children legislation: This legislation relates to Working with Children
Act 2005 ('the Act') whose purpose is to check persons working with children. It is
also dutiful for the Working with Children Check, that aids decide whether people
are appropriate to work in child-related employment. This legislature enables to
comprehend that subjecting children to laborious activities may make them prone
to some ailments.
16.8
Workplace health and safety (WHS) legislation: This legislation relates to the Work
Health and Safety Act 2011which sets regulations to enhance work safety and
health of workers in Australia. The responsible regulators set out legal duties and
responsibilities to be followed by employers and business owners. As a nursing
practitioner, this legislature allows me to acknowledge the work of WHO in
campaigning for proper working environments devoid of risks or hazards.
References: Berman, A., Snyder, S. J., Kozier, B., Erb, G. L., Levett-Jones, T.,
Dwyer, T., ... & Parker, B. (2014). Kozier & Erb's Fundamentals of Nursing
Australian Edition (Vol. 3). Pearson Higher Education AU.
17. The owner of an aged care facility released the photos
and videos of a resident who had dementia without prior
consent. The resident's family filed a petition in court against
the organisation asking for compensation. What type of
penalties should a Nurse expect if found to be in breach of the
privacy act 1988 (in 30-40 words).
The nurse found at the breach of privacy might be subjected to
various penalties which differ in regards to the seriousness of the
breach. They include: dollar or Pecuniary penalties where an
individual can be forced to pay some money as a fine or an
incarceration especially when the act was intentional.
Reference: Barry, J., & Hardiker, N. (2012). Advancing nursing practice
through social media: a global perspective. OJIN: The Online Journal of
Issues in Nursing, 17(3).
18. Various clinical situations will leave you in an ethical
dilemma. Identify what ethical principles are in conflict with
regards to the following ethical dilemmas (in 30-40 words
each):
18.1
Abortion: A major ethical dilemma occurs in the question of abortion when the
woman requests for the process while it is against the principles of nursing to do
anything which can harm either the foetus or the mother. The nurse is thus left
wondering whether to help the woman abort or defile the Non-maleficence
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
principle.
18.2
Tissue transplantation and organ donation: Ethical questions have risen since
some people exploit the poor with intent of selling some of their body organs.
Patients sometimes die since the processes of tissue transplant take a lot of time.
In either way justice is not done to the patient who has entrusted his or her life to
the nurses.
18.3
Reproductive technology: Artificial insemination, gamete intrafallopian transfer
(GIFT), and intracytoplasmic sperm injection (ICSI) are some of the common
reproductive technologies. These processes are very risky and thus they are in
conflict with the principle of Non-maleficence.
18.4
Euthanasia and assisted suicide: Patients or their family members may through
decisions ask for a mercy killing which involves taking away life. The nurse in
charge is left in an ethical dilemma since this act involves immorality but at the
same time cannot against the principle of Autonomy which allows patients to make
decisions freely.
18.5
Restraint: There are five types of restraint namely mechanical, psychological,
technological, physical, and chemical. All of them are not universal remedies and
can present significant risks to patients. Thus, they also contradict the principle of
efficiency and Non-maleficence.
18.6
Open disclosure: Healthcare practitioners have been slow to implement the
practice of OD owing to the strong ethical issues associated. OD involves
uncertainty, errors, concerning how much and what to disclose. Hence OD
contradicts and conflicts with the principle of veracity.
18.7
Mandatory reporting: Ethical dilemmas arise when executives demand for
mandatory reporting of incompetent behaviour. A nurse might be reluctant to
report a malpractice of another nurse due to individual interests or relations. But
such an act will again comprise the principle of veracity.
18.8
Quality of life: Beneficence principle is always highly compromised when it comes
to the discussion of Quality of Life. This principle requires nurses to bring
satisfaction to the patient no matter what while Quality of Life from its definition
implies that it might bring about some bad experience of living.
18.9
Conscientious objection: a fundamental right or freedom of conscience is
conflicted since doctors and other health practitioners are said to have no right to
conscientious objection in liberal democracies. Their freedom to act in harmony
with their deeply held convictions is highly curtailed.
18.10
Abuse, e.g. elder abuse: The essential goal of ethics related to elder abuse is to
thwart preventable suffering and to sustain Quality Of Life. Ethical dilemmas take
place when there is a conflict of principles among persons. The Principle of
Autonomy is thus compromised in this case.
18.11
Consent: Sometimes patients might be at a condition which cannot allow them to
18.2
Tissue transplantation and organ donation: Ethical questions have risen since
some people exploit the poor with intent of selling some of their body organs.
Patients sometimes die since the processes of tissue transplant take a lot of time.
In either way justice is not done to the patient who has entrusted his or her life to
the nurses.
18.3
Reproductive technology: Artificial insemination, gamete intrafallopian transfer
(GIFT), and intracytoplasmic sperm injection (ICSI) are some of the common
reproductive technologies. These processes are very risky and thus they are in
conflict with the principle of Non-maleficence.
18.4
Euthanasia and assisted suicide: Patients or their family members may through
decisions ask for a mercy killing which involves taking away life. The nurse in
charge is left in an ethical dilemma since this act involves immorality but at the
same time cannot against the principle of Autonomy which allows patients to make
decisions freely.
18.5
Restraint: There are five types of restraint namely mechanical, psychological,
technological, physical, and chemical. All of them are not universal remedies and
can present significant risks to patients. Thus, they also contradict the principle of
efficiency and Non-maleficence.
18.6
Open disclosure: Healthcare practitioners have been slow to implement the
practice of OD owing to the strong ethical issues associated. OD involves
uncertainty, errors, concerning how much and what to disclose. Hence OD
contradicts and conflicts with the principle of veracity.
18.7
Mandatory reporting: Ethical dilemmas arise when executives demand for
mandatory reporting of incompetent behaviour. A nurse might be reluctant to
report a malpractice of another nurse due to individual interests or relations. But
such an act will again comprise the principle of veracity.
18.8
Quality of life: Beneficence principle is always highly compromised when it comes
to the discussion of Quality of Life. This principle requires nurses to bring
satisfaction to the patient no matter what while Quality of Life from its definition
implies that it might bring about some bad experience of living.
18.9
Conscientious objection: a fundamental right or freedom of conscience is
conflicted since doctors and other health practitioners are said to have no right to
conscientious objection in liberal democracies. Their freedom to act in harmony
with their deeply held convictions is highly curtailed.
18.10
Abuse, e.g. elder abuse: The essential goal of ethics related to elder abuse is to
thwart preventable suffering and to sustain Quality Of Life. Ethical dilemmas take
place when there is a conflict of principles among persons. The Principle of
Autonomy is thus compromised in this case.
18.11
Consent: Sometimes patients might be at a condition which cannot allow them to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
make any type of consent. In such as case then the nurse might be impelled to do
what he or she feels is right for the patient devoid of their consent. This act
conflicts the patient’s right to make decisions or the principle of Autonomy.
18.12
Artificially prolonging life: Decisions whether to prolong or withdraw life are often
complex since there are so many issues surrounding life and death. Needless to
say, nurses ability autonomy to make decisions whether to prolong life or not are
highly abridged.
18.13
Refusal and withdrawal of treatment: Specialists are mandated to safeguard the
patient’s good and circumvent any injury to the patient. The principles of
beneficence and nonmaleficence give ethical keystone to withdrawing or
withholding treatment in a number of ways.
18.14
Stem cell research, e.g. embryonic stem cell research: When it comes to
embryonic stem cell research, it is not possible to reverence both moral principles.
In order to take embryonic stem cells, the premature embryo has to be smashed.
This implies wiping out a potential human life.
18.15
'Not for resuscitation' orders: Each patient regardless of their condition has
autonomy and, even though a patient might make decisions based on end-of-life
healthcare which other people think are erroneous, it is each patient’s freedom to
make those decisions for themselves. A “Do Not Resuscitate” order is a medical
doctor request that requests healthcare professional that a patient is not to
receive any, or only inadequate, resuscitative efforts in the event the patient’s
heart stops beating or the patient stops breathing.
18.16
Cultural and religious matters: There are over and over again religious and cultural
deliberations whenever caring for an individual after passing away. No two cultural
or religious sets are precisely similar, and there are frequently different factions.
Cultural factors strappingly manipulate family’s’ and patients' decisions at the end
of life.
Reference: Wells, S., Quash, B., & Eklund, R. (2017). Introducing Christian Ethics.
John Wiley & Sons.
19. There are different legal and ethical considerations
underpinning nursing practice and this may vary between
States and Territories. Various legal and ethical
considerations relevant to the nursing profession are
identified below. Explain how these are applied in nursing
practice in your State/Territory (in 40-50 words each).
Life and death issues:
19.1
Power of attorney: In Australia, the power of attorneys allows nurses delegate
management of affairs to people they trust.
19.2
Living wills and advanced directives: These are legal documents which an
individual specifies what should be done to him or her if they are no longer able to
what he or she feels is right for the patient devoid of their consent. This act
conflicts the patient’s right to make decisions or the principle of Autonomy.
18.12
Artificially prolonging life: Decisions whether to prolong or withdraw life are often
complex since there are so many issues surrounding life and death. Needless to
say, nurses ability autonomy to make decisions whether to prolong life or not are
highly abridged.
18.13
Refusal and withdrawal of treatment: Specialists are mandated to safeguard the
patient’s good and circumvent any injury to the patient. The principles of
beneficence and nonmaleficence give ethical keystone to withdrawing or
withholding treatment in a number of ways.
18.14
Stem cell research, e.g. embryonic stem cell research: When it comes to
embryonic stem cell research, it is not possible to reverence both moral principles.
In order to take embryonic stem cells, the premature embryo has to be smashed.
This implies wiping out a potential human life.
18.15
'Not for resuscitation' orders: Each patient regardless of their condition has
autonomy and, even though a patient might make decisions based on end-of-life
healthcare which other people think are erroneous, it is each patient’s freedom to
make those decisions for themselves. A “Do Not Resuscitate” order is a medical
doctor request that requests healthcare professional that a patient is not to
receive any, or only inadequate, resuscitative efforts in the event the patient’s
heart stops beating or the patient stops breathing.
18.16
Cultural and religious matters: There are over and over again religious and cultural
deliberations whenever caring for an individual after passing away. No two cultural
or religious sets are precisely similar, and there are frequently different factions.
Cultural factors strappingly manipulate family’s’ and patients' decisions at the end
of life.
Reference: Wells, S., Quash, B., & Eklund, R. (2017). Introducing Christian Ethics.
John Wiley & Sons.
19. There are different legal and ethical considerations
underpinning nursing practice and this may vary between
States and Territories. Various legal and ethical
considerations relevant to the nursing profession are
identified below. Explain how these are applied in nursing
practice in your State/Territory (in 40-50 words each).
Life and death issues:
19.1
Power of attorney: In Australia, the power of attorneys allows nurses delegate
management of affairs to people they trust.
19.2
Living wills and advanced directives: These are legal documents which an
individual specifies what should be done to him or her if they are no longer able to
make any decision for themselves say due to sickness or something.
19.3
Guardianship: This takes place when an individual is lawfully selected by the
Victorian Civil and Administrative Tribunal (VCAT) to make specific daily life
decisions for another individual who, due to disability (including dementia), lacks
decision-making capability for a decision that needs to be made.
Reference: Curtis, K., & Ramsden, C. (2015). Emergency and trauma care for
nurses and paramedics. Elsevier Health Sciences.
19.3
Guardianship: This takes place when an individual is lawfully selected by the
Victorian Civil and Administrative Tribunal (VCAT) to make specific daily life
decisions for another individual who, due to disability (including dementia), lacks
decision-making capability for a decision that needs to be made.
Reference: Curtis, K., & Ramsden, C. (2015). Emergency and trauma care for
nurses and paramedics. Elsevier Health Sciences.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




