Holmesglen Diploma of Nursing: HLTENN005 Workbook Assessment Task 4/5
VerifiedAdded on 2023/03/23
|22
|4677
|58
Homework Assignment
AI Summary
This document presents a completed workbook assessment for the HLTENN005 unit, focusing on contributing to nursing care for a person with complex needs. The scenario centers on Jessica Fong, a 30-year-old patient who sustained multiple injuries in a motor vehicle accident, including a closed head injury, fractured tibia and fibula, and a perforated bowel requiring a laparotomy and loop ileostomy. The assessment covers various aspects of nursing care, including post-operative management, neurological and neurovascular observations, ileostomy and stoma care, nasogastric tube (NGT) feeding, and addressing the patient's physical, emotional, and psychosocial needs. The student answers questions related to nursing interventions, maintaining patient dignity, assessing and managing complications associated with the ileostomy, and providing education to the patient. Additionally, the assessment includes the rationale for nursing interventions like head elevation, managing anxiety, and ensuring regular mouth care for patients with NGT feeds. The student demonstrates understanding of the conditions for assessment, equipment and resources required and post-operative orders given to the patient. The student is expected to answer all questions fully with explanations related to the scenario given.
CRS170
Revision 101
July 2017
Page 1 of 22
Assessment Task 4/5: Workbook Assessment
Student Version: Knowledge
Student information
Student name: . Student ID: .
Section A – Program/Course details
Qualification code: HLT54115 Qualification title: Diploma of Nursing
Unit code: HLTENN005 Unit title: Contribute to nursing care for
a person with complex needs
Section B – Assessment task details
Assessment number: 4/5 Semester/Year: Semester 1 2019
Due date: To be provided by your
Assessor.
Duration of assessment: 2 tutorials
Assessment task
results:
This assessment task will be marked as:
☒ Ungraded result: Satisfactory or Not Satisfactory
☐ Other (eg points): Graded once deemed satisfactory
Section C – Instructions to students
Task instructions:
Worksheet will be completed over two tutorials.
Students will need to access resources on Brightspace such as readings and PowerPoints to work on
worksheet outside of tutorials.
Students MUST answer all questions fully (explanations relating specifically to the scenario is required).
Answers for the worksheet will be covered in the tutorials.
Completed worksheets will be returned to the session teacher.
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 1 of 22
Assessment Task 4/5: Workbook Assessment
Student Version: Knowledge
Student information
Student name: . Student ID: .
Section A – Program/Course details
Qualification code: HLT54115 Qualification title: Diploma of Nursing
Unit code: HLTENN005 Unit title: Contribute to nursing care for
a person with complex needs
Section B – Assessment task details
Assessment number: 4/5 Semester/Year: Semester 1 2019
Due date: To be provided by your
Assessor.
Duration of assessment: 2 tutorials
Assessment task
results:
This assessment task will be marked as:
☒ Ungraded result: Satisfactory or Not Satisfactory
☐ Other (eg points): Graded once deemed satisfactory
Section C – Instructions to students
Task instructions:
Worksheet will be completed over two tutorials.
Students will need to access resources on Brightspace such as readings and PowerPoints to work on
worksheet outside of tutorials.
Students MUST answer all questions fully (explanations relating specifically to the scenario is required).
Answers for the worksheet will be covered in the tutorials.
Completed worksheets will be returned to the session teacher.
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 2 of 22
Section D – Conditions for assessment
Conditions:
Student to complete and attach Assessment Submission Cover Sheet to the completed Assessment Task.
Equipment/resources students must supply: Equipment/resources to be provided by the RTO:
Recommended text:
Koutoukidis, G, Stainton, K, & Hughson, J. (2017).Tabbner’s Nursing Care Theory and Practice (7th ed,).
Sydney, Australia: Elsevier.
Tiziani A, 2013 Havard’s Nursing Guide to Drugs (10th
ed.). Mosby Elsevier
Pens
Assessment paper
Resources on Brightspace and face to face
discussion facilitated by a teacher.
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 2 of 22
Section D – Conditions for assessment
Conditions:
Student to complete and attach Assessment Submission Cover Sheet to the completed Assessment Task.
Equipment/resources students must supply: Equipment/resources to be provided by the RTO:
Recommended text:
Koutoukidis, G, Stainton, K, & Hughson, J. (2017).Tabbner’s Nursing Care Theory and Practice (7th ed,).
Sydney, Australia: Elsevier.
Tiziani A, 2013 Havard’s Nursing Guide to Drugs (10th
ed.). Mosby Elsevier
Pens
Assessment paper
Resources on Brightspace and face to face
discussion facilitated by a teacher.
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
CRS170
Revision 101
July 2017
Page 3 of 22
Student Instructions
Read the following Scenario and answer the questions using the information provided below.
Scenario:
Jessica Fong is an active thirty (30) year old who was involved in a motor vehicle accident. She has
sustained a closed head injury, and a fractured right tibia and fibula, which required an ORIF (open
reduction and internal fixation). Her other injury is a perforated bowel. She has had a laparotomy and loop
ileostomy formation. Jessica has a NG tube (Nasogastric tube) inserted prior to surgery, it remains insitu for
nasogastric feeds to meet her nutritional needs.
Medical history: No significant medical history. Allergy to strawberries causes abdominal pain and
diarrhoea.
You undertake a systems assessment of Jessica at the commencement of your care. These are your
assessment findings:
CNS: Alert, orientated, obeys commands. Slightly drowsy as she is post anaesthesia. Pupils size 3 and
reactive to light bilaterally. Full function and movement to both arms and left leg, right leg injured. No
complaints of pain due to analgesia given intra operatively.
CVS: Temp. 36.7C, HR 88 bpm regular. Colour, god well perfused. Peripheries warm. IV(Intravenous)
cannula site intact.
Resp: Air entry L(left)=R (right). RR 18rpm. SaO2 = 97% on room air
Renal: Has not passed urine since return to ward one (1) hour ago. Pre-operative urinalysis NAD (No
abnormalities detected), SG (Specific Gravity) 1.010, Ph (acid-alkali balance) 5.5
GIT: Ileostomy bag 75mls rose coloured fluid. Stoma red. Abdomen soft, no distention.
Endocrine: BGL (Blood glucose level) = 6.5 mmols
Musculoskeletal: Neurovascular assessment – left leg full range of movement and sensation. Right leg,
Jessica is able to wriggle her toes, no other movement due to operation site. Has full sensation on right leg.
Both legs pedal and tibial pulses strong. Capillary refill under 2 seconds both feet. Legs warm and well
perfused.
Skin: No redness or loss of skin integrity
Social: Divorced, has sole custody for her seven (7) year old daughter. Has no contact with ex-husband
and receives no financial help for their daughter. She works full time in a pharmacy and has limited child
care assistance from her parents who also both work. She is very anxious about the impact of her injuries
on her ability to return to work and care for her daughter.
Post-operative orders:
RPAO (routine post anaesthetic observations)
Neurologic and neurovascular observations 4/24 prn
Nurse with head elevated to 40%
RIB (rest in bed) until surgical and physiotherapy review in 24 (twenty-four) hrs. Mobilise with a
walking frame after review.
Abdominal wound dressing remains intact until surgical review.
Ileostomy and stoma care prn (as necessary) as per protocol
NGT (Nasogastric tube) gravity feeds 50mL/hour of Osmolite
NBM (Nil by mouth) until bowel sounds return.
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 3 of 22
Student Instructions
Read the following Scenario and answer the questions using the information provided below.
Scenario:
Jessica Fong is an active thirty (30) year old who was involved in a motor vehicle accident. She has
sustained a closed head injury, and a fractured right tibia and fibula, which required an ORIF (open
reduction and internal fixation). Her other injury is a perforated bowel. She has had a laparotomy and loop
ileostomy formation. Jessica has a NG tube (Nasogastric tube) inserted prior to surgery, it remains insitu for
nasogastric feeds to meet her nutritional needs.
Medical history: No significant medical history. Allergy to strawberries causes abdominal pain and
diarrhoea.
You undertake a systems assessment of Jessica at the commencement of your care. These are your
assessment findings:
CNS: Alert, orientated, obeys commands. Slightly drowsy as she is post anaesthesia. Pupils size 3 and
reactive to light bilaterally. Full function and movement to both arms and left leg, right leg injured. No
complaints of pain due to analgesia given intra operatively.
CVS: Temp. 36.7C, HR 88 bpm regular. Colour, god well perfused. Peripheries warm. IV(Intravenous)
cannula site intact.
Resp: Air entry L(left)=R (right). RR 18rpm. SaO2 = 97% on room air
Renal: Has not passed urine since return to ward one (1) hour ago. Pre-operative urinalysis NAD (No
abnormalities detected), SG (Specific Gravity) 1.010, Ph (acid-alkali balance) 5.5
GIT: Ileostomy bag 75mls rose coloured fluid. Stoma red. Abdomen soft, no distention.
Endocrine: BGL (Blood glucose level) = 6.5 mmols
Musculoskeletal: Neurovascular assessment – left leg full range of movement and sensation. Right leg,
Jessica is able to wriggle her toes, no other movement due to operation site. Has full sensation on right leg.
Both legs pedal and tibial pulses strong. Capillary refill under 2 seconds both feet. Legs warm and well
perfused.
Skin: No redness or loss of skin integrity
Social: Divorced, has sole custody for her seven (7) year old daughter. Has no contact with ex-husband
and receives no financial help for their daughter. She works full time in a pharmacy and has limited child
care assistance from her parents who also both work. She is very anxious about the impact of her injuries
on her ability to return to work and care for her daughter.
Post-operative orders:
RPAO (routine post anaesthetic observations)
Neurologic and neurovascular observations 4/24 prn
Nurse with head elevated to 40%
RIB (rest in bed) until surgical and physiotherapy review in 24 (twenty-four) hrs. Mobilise with a
walking frame after review.
Abdominal wound dressing remains intact until surgical review.
Ileostomy and stoma care prn (as necessary) as per protocol
NGT (Nasogastric tube) gravity feeds 50mL/hour of Osmolite
NBM (Nil by mouth) until bowel sounds return.
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CRS170
Revision 101
July 2017
Page 4 of 22
Element 1: Perform nursing interventions to assist a person with complex needs
1.11.2 Perform nursing interventions based on the person’s predetermined plan of care
Question
1.1a
Jessica sustained a closed head injury and is to be nursed
with her head elevated by 40 (forty) degrees. Explain why
this is important.
Satisfactory response
Yes ☐ No ☐
Answer:
Head injury leads to alteration of pressure in the cranium, cerebral perfusion pressure
and the blood flow to the cerebrum. Closed head injury increases the intracranial
pressure and elevation of the head at 40 degrees therefore decreases the intracranial
pressure building up and the cerebral perfusion pressure as well.
……………………………………………………………………………………………………
……………………………………………………………………………………………………
……………………………………………………………………………………………………
…………………………………………………………………………………………………
Teacher Comment:
Question
1.1b
If Jessica’s neurological observations deteriorate for
example her conscious level decreasing, pupil’s unequal
and reacting sluggishly. What complication could this
indicate?
Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
……An increase in Intracranial Pressure.
………………………………………………………………………………………………………
…………………………………………………………………………………………………
Teacher Comment:
Question
1.1c
Why is it of neurological importance to manage Jessica’s
anxiety, pain and continence needs? Satisfactory response
Yes ☐ No ☐
Answer:
……To manage Jessica’s stress. Anxiety can lead to urinary incontinence hence
management of continence needs is required for a neurological impaired disorder.
Management of pain is done to make Jessica comfortable.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………..
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 4 of 22
Element 1: Perform nursing interventions to assist a person with complex needs
1.11.2 Perform nursing interventions based on the person’s predetermined plan of care
Question
1.1a
Jessica sustained a closed head injury and is to be nursed
with her head elevated by 40 (forty) degrees. Explain why
this is important.
Satisfactory response
Yes ☐ No ☐
Answer:
Head injury leads to alteration of pressure in the cranium, cerebral perfusion pressure
and the blood flow to the cerebrum. Closed head injury increases the intracranial
pressure and elevation of the head at 40 degrees therefore decreases the intracranial
pressure building up and the cerebral perfusion pressure as well.
……………………………………………………………………………………………………
……………………………………………………………………………………………………
……………………………………………………………………………………………………
…………………………………………………………………………………………………
Teacher Comment:
Question
1.1b
If Jessica’s neurological observations deteriorate for
example her conscious level decreasing, pupil’s unequal
and reacting sluggishly. What complication could this
indicate?
Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
……An increase in Intracranial Pressure.
………………………………………………………………………………………………………
…………………………………………………………………………………………………
Teacher Comment:
Question
1.1c
Why is it of neurological importance to manage Jessica’s
anxiety, pain and continence needs? Satisfactory response
Yes ☐ No ☐
Answer:
……To manage Jessica’s stress. Anxiety can lead to urinary incontinence hence
management of continence needs is required for a neurological impaired disorder.
Management of pain is done to make Jessica comfortable.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………..
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 5 of 22
1.3 Undertake nursing interventions demonstrating respect for the person’s dignity and cultural diversity.
Question 1.2 Jessica is at bedrest for 24hrs and is reliant on you for her
personal hygiene, continence and pressure care needs. She
is a young independent person, explain three (3) strategies
you would employ to maintain her dignity and respect her
individuality.
Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
…Ensuring that she remains covered while providing her care needs. By doing so it
protects her physical privacy.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Protecting Jessica’s personal information by avoiding sharing personal information about
Jessica beyond what is necessary for the members of the care team.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………
Assisting Jessica with personal grooming , this will make her retain pride in her
appearance.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 5 of 22
1.3 Undertake nursing interventions demonstrating respect for the person’s dignity and cultural diversity.
Question 1.2 Jessica is at bedrest for 24hrs and is reliant on you for her
personal hygiene, continence and pressure care needs. She
is a young independent person, explain three (3) strategies
you would employ to maintain her dignity and respect her
individuality.
Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
…Ensuring that she remains covered while providing her care needs. By doing so it
protects her physical privacy.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Protecting Jessica’s personal information by avoiding sharing personal information about
Jessica beyond what is necessary for the members of the care team.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………
Assisting Jessica with personal grooming , this will make her retain pride in her
appearance.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
CRS170
Revision 101
July 2017
Page 6 of 22
………………………………………………………………………………………………………
………………………………………………………………………………………………………
……………………………………………………………………………………………………
1.3 Encourage the person to assist by undertaking aspects of their own care during care interventions
Jessica may be going home with her ileostomy bag before she has her reversal surgery. You are going to
assess her ileostomy and at the same time educate Jessica regarding self-management.
Question
1.3a
Discuss assessments you would make regarding the following,
include Jessica’s involvement in your answer. Satisfactory response
Yes ☐ No ☐
Answer:
Peri-stomal skin:
……………………………………………………………………………………………………I
will remove Jessica’s pouching system
……………………………………………………………………………………………
Assess Jessica in both her sitting and lying positions.
…………………………………………………………………………………………………
…………………………………………………………………………………………………
…
Stoma:
…I will assess for the state and colour of the stoma by feeling surrounding stoma site
gently for tenderness.
I will then ask Jessica to cough and feel the cough impulse to assess for parastomal
hernia.
I will then gently digitate the stoma to check patency and assess the stoma.
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 6 of 22
………………………………………………………………………………………………………
………………………………………………………………………………………………………
……………………………………………………………………………………………………
1.3 Encourage the person to assist by undertaking aspects of their own care during care interventions
Jessica may be going home with her ileostomy bag before she has her reversal surgery. You are going to
assess her ileostomy and at the same time educate Jessica regarding self-management.
Question
1.3a
Discuss assessments you would make regarding the following,
include Jessica’s involvement in your answer. Satisfactory response
Yes ☐ No ☐
Answer:
Peri-stomal skin:
……………………………………………………………………………………………………I
will remove Jessica’s pouching system
……………………………………………………………………………………………
Assess Jessica in both her sitting and lying positions.
…………………………………………………………………………………………………
…………………………………………………………………………………………………
…
Stoma:
…I will assess for the state and colour of the stoma by feeling surrounding stoma site
gently for tenderness.
I will then ask Jessica to cough and feel the cough impulse to assess for parastomal
hernia.
I will then gently digitate the stoma to check patency and assess the stoma.
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CRS170
Revision 101
July 2017
Page 7 of 22
………………………………………………………………………………………………………
…………………………………………………………………………………………………
…………………………………………………………………………………………………
…………………………………………………………………………………………
Stoma bag:
……………………………………………………………………………………………………I
will start in the in centre of the stoma and assess outward ending with the
surrounding tissue..
…………………………………………………………………………………………………
…………………………………………………………………………………………………
………………………………………………………………………………………………
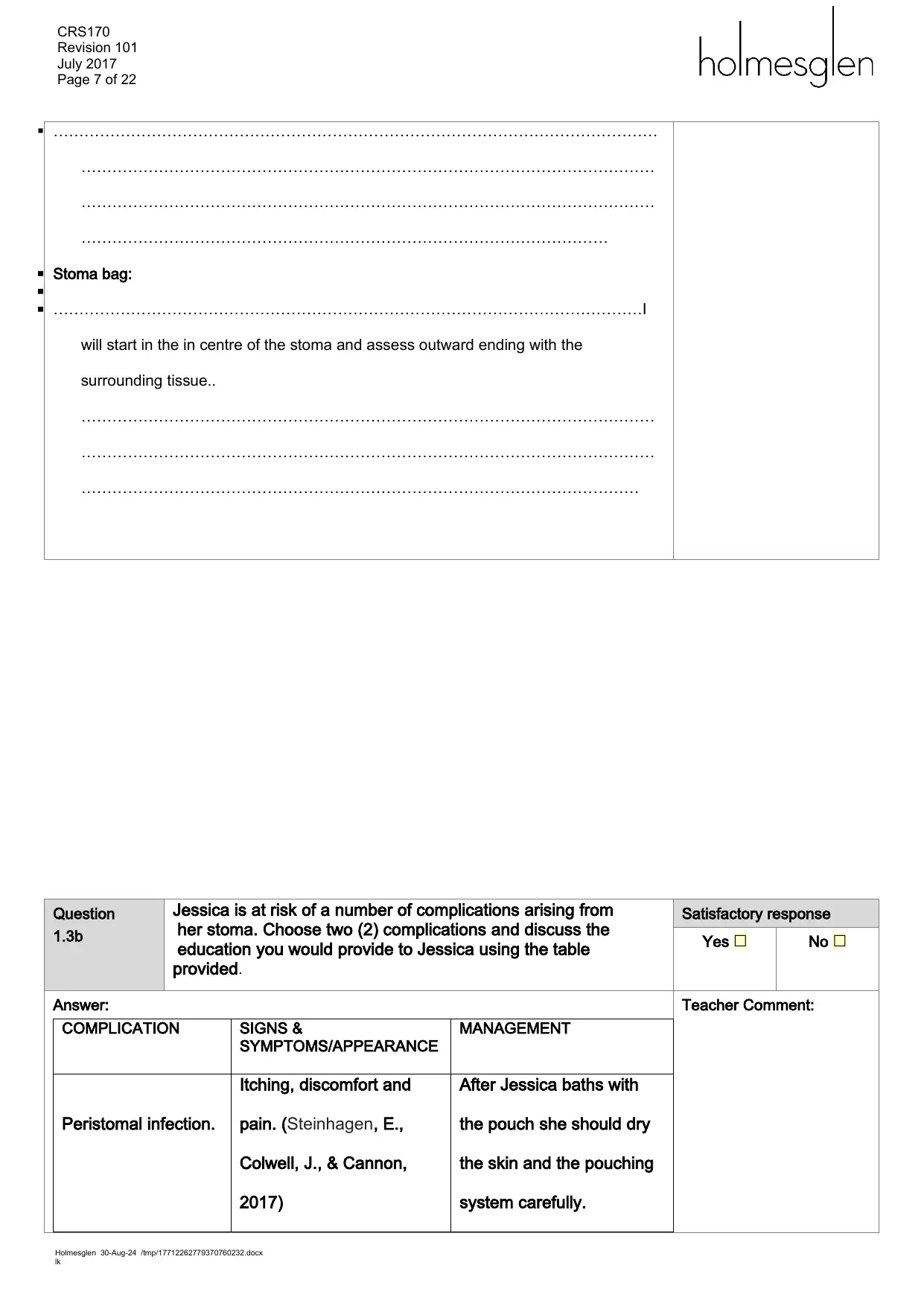
Question
1.3b
Jessica is at risk of a number of complications arising from
her stoma. Choose two (2) complications and discuss the
education you would provide to Jessica using the table
provided.
Satisfactory response
Yes ☐ No ☐
Answer:
COMPLICATION SIGNS &
SYMPTOMS/APPEARANCE
MANAGEMENT
Peristomal infection.
Itching, discomfort and
pain. (Steinhagen, E.,
Colwell, J., & Cannon,
2017)
After Jessica baths with
the pouch she should dry
the skin and the pouching
system carefully.
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 7 of 22
………………………………………………………………………………………………………
…………………………………………………………………………………………………
…………………………………………………………………………………………………
…………………………………………………………………………………………
Stoma bag:
……………………………………………………………………………………………………I
will start in the in centre of the stoma and assess outward ending with the
surrounding tissue..
…………………………………………………………………………………………………
…………………………………………………………………………………………………
………………………………………………………………………………………………
Question
1.3b
Jessica is at risk of a number of complications arising from
her stoma. Choose two (2) complications and discuss the
education you would provide to Jessica using the table
provided.
Satisfactory response
Yes ☐ No ☐
Answer:
COMPLICATION SIGNS &
SYMPTOMS/APPEARANCE
MANAGEMENT
Peristomal infection.
Itching, discomfort and
pain. (Steinhagen, E.,
Colwell, J., & Cannon,
2017)
After Jessica baths with
the pouch she should dry
the skin and the pouching
system carefully.
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 8 of 22
Stoma trauma. A visible cut, and a bright
red bleeding.
Manage the visible cut
while observing the
the aseptic techniques
to prevent infection.
1.4 Consider the person’s physical, emotional and psychosocial needs when performing nursing
interventions.
Question
1.4a
Jessica is very anxious and distressed about having an
ileostomy. State three (3) reasons for her anxiety Satisfactory response
Yes ☐ No ☐
Answer:
1.
………………………………………………………………………………………………………
Jessica’s main fear and anxiety can be on the change of the diet she is to take due to the
procedure he has undergone lately.
……………………………………………………………………………………………………
2. She might also be scared of the status of then stoma. “what if her stoma
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 8 of 22
Stoma trauma. A visible cut, and a bright
red bleeding.
Manage the visible cut
while observing the
the aseptic techniques
to prevent infection.
1.4 Consider the person’s physical, emotional and psychosocial needs when performing nursing
interventions.
Question
1.4a
Jessica is very anxious and distressed about having an
ileostomy. State three (3) reasons for her anxiety Satisfactory response
Yes ☐ No ☐
Answer:
1.
………………………………………………………………………………………………………
Jessica’s main fear and anxiety can be on the change of the diet she is to take due to the
procedure he has undergone lately.
……………………………………………………………………………………………………
2. She might also be scared of the status of then stoma. “what if her stoma
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
CRS170
Revision 101
July 2017
Page 9 of 22
leaks?”………………………………………………………………………………………………
………………………………………………………………………………………………………
3.According to Liao & Qin, (2014.), it was said that in as much as the individual with
stoma has to cope with some sensitive issues such as faecal incontinence, he/she may
also experience changes to their body image, sexual functioning, isolated socially, stigma
decreased mood and embarrassment.
………………………………………………………………………………………………………
……………………………………………………………………………………………………
Element 2. Contribute to the nursing care of people with common disorders and conditions
2.1 Provide nursing care to the person appropriate to the management of complex conditions
Question
2.1a
Jessica had her Nasogastric tube (NGT) inserted prior to her
abdominal surgery, provide a reason for this procedure being
performed specifically pre-operatively.
Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
Inserting a nasogastric tubing helps in gaining access to the stomach and its contents
and it can be performed to drain the Gastric contents prior to abdominal surgery.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
……………………………………………………………………………………………………
Teacher Comment:
Question
2.1b
Would a NGT (Nasogastric tube) usually be contraindicated for
this person? If so, explain the reason. Satisfactory response
Yes ☐ No ☐
Answer:
……………………………………………………………………………………………………
…YES, it would be contra indicated, increase in hospital stay and complication rates are
observed in patients who receive nasogastric decompression compared to those
without NG tube (Wang et al.,2015).
.……………………………………………………………………………………………………
………………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 9 of 22
leaks?”………………………………………………………………………………………………
………………………………………………………………………………………………………
3.According to Liao & Qin, (2014.), it was said that in as much as the individual with
stoma has to cope with some sensitive issues such as faecal incontinence, he/she may
also experience changes to their body image, sexual functioning, isolated socially, stigma
decreased mood and embarrassment.
………………………………………………………………………………………………………
……………………………………………………………………………………………………
Element 2. Contribute to the nursing care of people with common disorders and conditions
2.1 Provide nursing care to the person appropriate to the management of complex conditions
Question
2.1a
Jessica had her Nasogastric tube (NGT) inserted prior to her
abdominal surgery, provide a reason for this procedure being
performed specifically pre-operatively.
Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
Inserting a nasogastric tubing helps in gaining access to the stomach and its contents
and it can be performed to drain the Gastric contents prior to abdominal surgery.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
……………………………………………………………………………………………………
Teacher Comment:
Question
2.1b
Would a NGT (Nasogastric tube) usually be contraindicated for
this person? If so, explain the reason. Satisfactory response
Yes ☐ No ☐
Answer:
……………………………………………………………………………………………………
…YES, it would be contra indicated, increase in hospital stay and complication rates are
observed in patients who receive nasogastric decompression compared to those
without NG tube (Wang et al.,2015).
.……………………………………………………………………………………………………
………………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CRS170
Revision 101
July 2017
Page 10 of 22
NGT gravity feeds 50mL/hour of Osmolite has been ordered for Jessica.
Question
2.1c
How will you confirm nasogastric tube placement prior to
commencing nasogastric feeds?
Outline how you will deliver the feed after checking the tube
placement.
Satisfactory response
Yes ☐ No ☐
Answer:
Tube placement check:
………………………………………………………………………………………………………
ICorrect positioning of the NG tude can confirmed by the use of Chest X-Ray, the view
should be adequate with upper oesophagus down to below the diaphragm.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Delivery of feed:
……………………………………………………………………………………………………
According to Gale Encyclopedia of Nursing and Allied Health, (2016), the food can be
given by gravity, or by a pump.
Gravity requires the use of a syringe.
3 to 5 ml of air is therefore pulled into the syringe,
The syringe is then connected to the end of the tube,
A stethoscope is put in the nurses’s ears its end over the top of the stomach at a position
that is just below the center of the ribs.
The air is then pushed into the NG tube
Food contents are now pulled into the syringe and Jessica is fed.
The last thing after the feeding is over is flushing the tubing.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 10 of 22
NGT gravity feeds 50mL/hour of Osmolite has been ordered for Jessica.
Question
2.1c
How will you confirm nasogastric tube placement prior to
commencing nasogastric feeds?
Outline how you will deliver the feed after checking the tube
placement.
Satisfactory response
Yes ☐ No ☐
Answer:
Tube placement check:
………………………………………………………………………………………………………
ICorrect positioning of the NG tude can confirmed by the use of Chest X-Ray, the view
should be adequate with upper oesophagus down to below the diaphragm.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Delivery of feed:
……………………………………………………………………………………………………
According to Gale Encyclopedia of Nursing and Allied Health, (2016), the food can be
given by gravity, or by a pump.
Gravity requires the use of a syringe.
3 to 5 ml of air is therefore pulled into the syringe,
The syringe is then connected to the end of the tube,
A stethoscope is put in the nurses’s ears its end over the top of the stomach at a position
that is just below the center of the ribs.
The air is then pushed into the NG tube
Food contents are now pulled into the syringe and Jessica is fed.
The last thing after the feeding is over is flushing the tubing.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 11 of 22
………………………………………………………………………………………………………
………………………………………………………………………………………………………
…………………………………………………………………………………………………
Question
2.1d
Explain why regular mouthcare is important for a person having
nasogastric feeds. Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
……Regular Mouthcare improves the oral and dental hygiene and this can help prevent
bad breath. Effective oral care done to Jessica can help reduce ingection and
promotes health as well.
………………………………………………………………………………………………
…
……………………………………………………………………………………………………….
Teacher Comment:
2.2 Observe, report and document the person’s reactions and responses to the provided care management
and medication
Question 2.2 Jessica’s SpO2 drops to 87% on room air (RA). The doctor has
prescribed 6L/min of oxygen therapy via a Hudson face mask.
You have applied the oxygen therapy.
Provide three (3) immediate nursing interventions you may
initiate at this time for Jessica.
Satisfactory response
Yes ☐ No ☐
Answer:
1.……Position Jessica with her head elevated in a semi-Fowler’s position.
………………………………………………………………………………………………………
………………………………………………………………………………………………………I
2…I will turn Jessica every two hours while monitoring the oxygen saturation closely after
turning.
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 11 of 22
………………………………………………………………………………………………………
………………………………………………………………………………………………………
…………………………………………………………………………………………………
Question
2.1d
Explain why regular mouthcare is important for a person having
nasogastric feeds. Satisfactory response
Yes ☐ No ☐
Answer:
………………………………………………………………………………………………………
……Regular Mouthcare improves the oral and dental hygiene and this can help prevent
bad breath. Effective oral care done to Jessica can help reduce ingection and
promotes health as well.
………………………………………………………………………………………………
…
……………………………………………………………………………………………………….
Teacher Comment:
2.2 Observe, report and document the person’s reactions and responses to the provided care management
and medication
Question 2.2 Jessica’s SpO2 drops to 87% on room air (RA). The doctor has
prescribed 6L/min of oxygen therapy via a Hudson face mask.
You have applied the oxygen therapy.
Provide three (3) immediate nursing interventions you may
initiate at this time for Jessica.
Satisfactory response
Yes ☐ No ☐
Answer:
1.……Position Jessica with her head elevated in a semi-Fowler’s position.
………………………………………………………………………………………………………
………………………………………………………………………………………………………I
2…I will turn Jessica every two hours while monitoring the oxygen saturation closely after
turning.
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
CRS170
Revision 101
July 2017
Page 12 of 22
………………………………………………………………………………………………………
………………………………………………………………………………………………………
…………………………………………………………………………………………….
………………………………………………………………………………………………………
……… 3.Maintaining the oxygen administration device as stated by the by the physician
treating Jessica. This maintains the oxygen saturation equal to or above 90%. .
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………
.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
……………………………………………………………………………………………………
2.3 Refer promptly to the registered nurse any reactions, responses or variations from the normal or
unexpected outcomes, including concern for the deteriorating patient.
Question 2.3a Jessica has been on oxygen therapy for four (4) hours,
periodically the oxygen has been removed to assess her ability
to maintain her SpO2 on RA, they drop below 90% when the
oxygen is removed. You report your findings to the RN and
Doctor.
It is decided to continue oxygen therapy for Jessica. What are
(two) 2 further nursing interventions you would initiate for long
term oxygen therapy?
Satisfactory response
Yes ☐ No ☐
Answer:
1.Reduce the work of breathing for Jessica by adopting a sitting position that will help her
breathe with ease. Such allowing her sit on the chair with a table in front of her,
then I will advise her to place her arms on the table and allow her relax her arms
and shoulders, instruct her to place her feet on the floor and breath as normal.
………………………………………………………………………………………………
……
………………………………………………………………………………………………………
2.Administer oxygen while Jessica is at rest and when asleep at 2L/min via the nasal
cannula.
………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
Revision 101
July 2017
Page 12 of 22
………………………………………………………………………………………………………
………………………………………………………………………………………………………
…………………………………………………………………………………………….
………………………………………………………………………………………………………
……… 3.Maintaining the oxygen administration device as stated by the by the physician
treating Jessica. This maintains the oxygen saturation equal to or above 90%. .
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………
.
………………………………………………………………………………………………………
………………………………………………………………………………………………………
………………………………………………………………………………………………………
……………………………………………………………………………………………………
2.3 Refer promptly to the registered nurse any reactions, responses or variations from the normal or
unexpected outcomes, including concern for the deteriorating patient.
Question 2.3a Jessica has been on oxygen therapy for four (4) hours,
periodically the oxygen has been removed to assess her ability
to maintain her SpO2 on RA, they drop below 90% when the
oxygen is removed. You report your findings to the RN and
Doctor.
It is decided to continue oxygen therapy for Jessica. What are
(two) 2 further nursing interventions you would initiate for long
term oxygen therapy?
Satisfactory response
Yes ☐ No ☐
Answer:
1.Reduce the work of breathing for Jessica by adopting a sitting position that will help her
breathe with ease. Such allowing her sit on the chair with a table in front of her,
then I will advise her to place her arms on the table and allow her relax her arms
and shoulders, instruct her to place her feet on the floor and breath as normal.
………………………………………………………………………………………………
……
………………………………………………………………………………………………………
2.Administer oxygen while Jessica is at rest and when asleep at 2L/min via the nasal
cannula.
………………………………………………………………………………………………
Teacher Comment:
Holmesglen 30-Aug-24 /tmp/17712262779370760232.docx
lk
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





