Healthcare Case Study: HAIs, Hand Hygiene, and Change Implementation
VerifiedAdded on 2022/12/15
|12
|2961
|52
Case Study
AI Summary
This case study analyzes the prevalence of hospital acquired infections (HAIs) in Intensive Care Units (ICUs), focusing on the role of hand hygiene in infection control. The author, drawing on their experience as a nursing in-charge in India, highlights the significance of HAIs as a major threat to patient safety, particularly in vulnerable populations. The study emphasizes the importance of hand hygiene protocols, referencing WHO guidelines, and explores the application of Kurt Lewin's Change Model to implement effective change management strategies. The case study details the unfreezing, changing, and refreezing stages of the model, providing practical recommendations for educating nursing professionals, providing necessary support, and reinforcing new practices to reduce HAIs and improve healthcare outcomes. The outcome measurement will be done post 3 months of refreezing the change. The paper concludes with a call for training, education, and the potential use of bundle approaches for comprehensive infection prevention.

Running head: HEALTHCARE
HEALTHCARE
Name of the Student
Name of University
Author’s note
HEALTHCARE
Name of the Student
Name of University
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
HEALTHCARE
Introduction
Intensive Care Unit (ICU) can be stressful and a growing body of evidences suggest the
increase in work load among the nursing professionals working in the ICU settings increase the
vulnerability of error along with chances of mortality and morbidity among healthcare
professionals (Van Mol et al., 2015). The following case study is based on my previous work-
experience on India where I use work as nursing-in-charge in ICU and CCU. The paper will
focus one of the alarming threat population in ICU, hospital acquired infections (HAIs). This will
be followed by the importance of hand hygiene in decreasing the chances of HAIs and how this
change can be implemented under the healthcare settings. The paper will help to understand the
importance of the effective change management towards introducing a fresh change in practice.
The quality initiative
Hospital Acquired Infections (HAIs)
During my six years of working experience in India as a nursing in-charge in the ICU and
CCU unit, I have seen that one of the fatal threats to the patients in the ICU and the CCU units
are vulnerability towards developing hospital acquired infections (HAIs) or nosocomial
infection. HAIs or healthcare associated infections (HCAIs) are defined as those infections that
people develop during the stay in the hospital. These are the infections that develop within first
48 hours following hospitalization or within the 30days of stay in the hospital after receiving the
healthcare(Haque et al., 2018). According to the data published by the US Center for Disease
Control and Prevention, approximately 1.7 million hospitalized patients develop HCAIs per year
while being admitted in the hospital for some other health issues among these, at least 98,000
HEALTHCARE
Introduction
Intensive Care Unit (ICU) can be stressful and a growing body of evidences suggest the
increase in work load among the nursing professionals working in the ICU settings increase the
vulnerability of error along with chances of mortality and morbidity among healthcare
professionals (Van Mol et al., 2015). The following case study is based on my previous work-
experience on India where I use work as nursing-in-charge in ICU and CCU. The paper will
focus one of the alarming threat population in ICU, hospital acquired infections (HAIs). This will
be followed by the importance of hand hygiene in decreasing the chances of HAIs and how this
change can be implemented under the healthcare settings. The paper will help to understand the
importance of the effective change management towards introducing a fresh change in practice.
The quality initiative
Hospital Acquired Infections (HAIs)
During my six years of working experience in India as a nursing in-charge in the ICU and
CCU unit, I have seen that one of the fatal threats to the patients in the ICU and the CCU units
are vulnerability towards developing hospital acquired infections (HAIs) or nosocomial
infection. HAIs or healthcare associated infections (HCAIs) are defined as those infections that
people develop during the stay in the hospital. These are the infections that develop within first
48 hours following hospitalization or within the 30days of stay in the hospital after receiving the
healthcare(Haque et al., 2018). According to the data published by the US Center for Disease
Control and Prevention, approximately 1.7 million hospitalized patients develop HCAIs per year
while being admitted in the hospital for some other health issues among these, at least 98,000
2
HEALTHCARE
(one out of 17 patients) die due to HCAIs. In the developing countries like India, ten out of 100
patients develop HACIs. This number is double in comparison to the developed countries like
Europe or US. The percentage is higher among the patients who are admitted in the ICUs. The
ICU patients are either critically ill or are immune-compromised making them vulnerable to
develop HCAIs (Haque et al., 2018).
HAIs, threats and role of nurses
The HACIs increase the threat of spreading drug resistance micro-organisms mainly
multi-drug resistant (MDR) micro-organisms like carbapenem resistant enterobacteriaceae. The
spread of MDR infections leads to poor patients’ outcome while increasing the time of stay in the
hospital and increasing the cost of care (Swaminathan et al., 2017). In India or in other
developed countries there are no proper infrastructure for effective infection control and
prevention and thus contributing to further increase in the chances of the disease development
and spread of infection. Although hospital affiliations is not mandatory in India, autonomous
bodies like the National Accreditation Board of Hospitals and the National Health Mission’s
National Health Systems Resource Centre have introduced special programmes on effective
prevention of infections. However, surveillance programs are not comprehensive in reducing the
threat of HAIs (Swaminathan et al,. 2017). According to the study conducted by Khan, Ahmad
and Mehboob (2015) over middle and low income countries, the main source of the HAIs are the
nursing professionals. It is the nurses who spent majority of the time with the patients under the
healthcare settings. The contamination is spread through the touch of the infected hands
(unsterilized hands) leading to the development of different types of HAIs like the bloodstream
infection (BSI), ventilator-associated infection (VAP), surgical site infections (SSI) and urinary
tract infection (UTI).
HEALTHCARE
(one out of 17 patients) die due to HCAIs. In the developing countries like India, ten out of 100
patients develop HACIs. This number is double in comparison to the developed countries like
Europe or US. The percentage is higher among the patients who are admitted in the ICUs. The
ICU patients are either critically ill or are immune-compromised making them vulnerable to
develop HCAIs (Haque et al., 2018).
HAIs, threats and role of nurses
The HACIs increase the threat of spreading drug resistance micro-organisms mainly
multi-drug resistant (MDR) micro-organisms like carbapenem resistant enterobacteriaceae. The
spread of MDR infections leads to poor patients’ outcome while increasing the time of stay in the
hospital and increasing the cost of care (Swaminathan et al., 2017). In India or in other
developed countries there are no proper infrastructure for effective infection control and
prevention and thus contributing to further increase in the chances of the disease development
and spread of infection. Although hospital affiliations is not mandatory in India, autonomous
bodies like the National Accreditation Board of Hospitals and the National Health Mission’s
National Health Systems Resource Centre have introduced special programmes on effective
prevention of infections. However, surveillance programs are not comprehensive in reducing the
threat of HAIs (Swaminathan et al,. 2017). According to the study conducted by Khan, Ahmad
and Mehboob (2015) over middle and low income countries, the main source of the HAIs are the
nursing professionals. It is the nurses who spent majority of the time with the patients under the
healthcare settings. The contamination is spread through the touch of the infected hands
(unsterilized hands) leading to the development of different types of HAIs like the bloodstream
infection (BSI), ventilator-associated infection (VAP), surgical site infections (SSI) and urinary
tract infection (UTI).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
HEALTHCARE
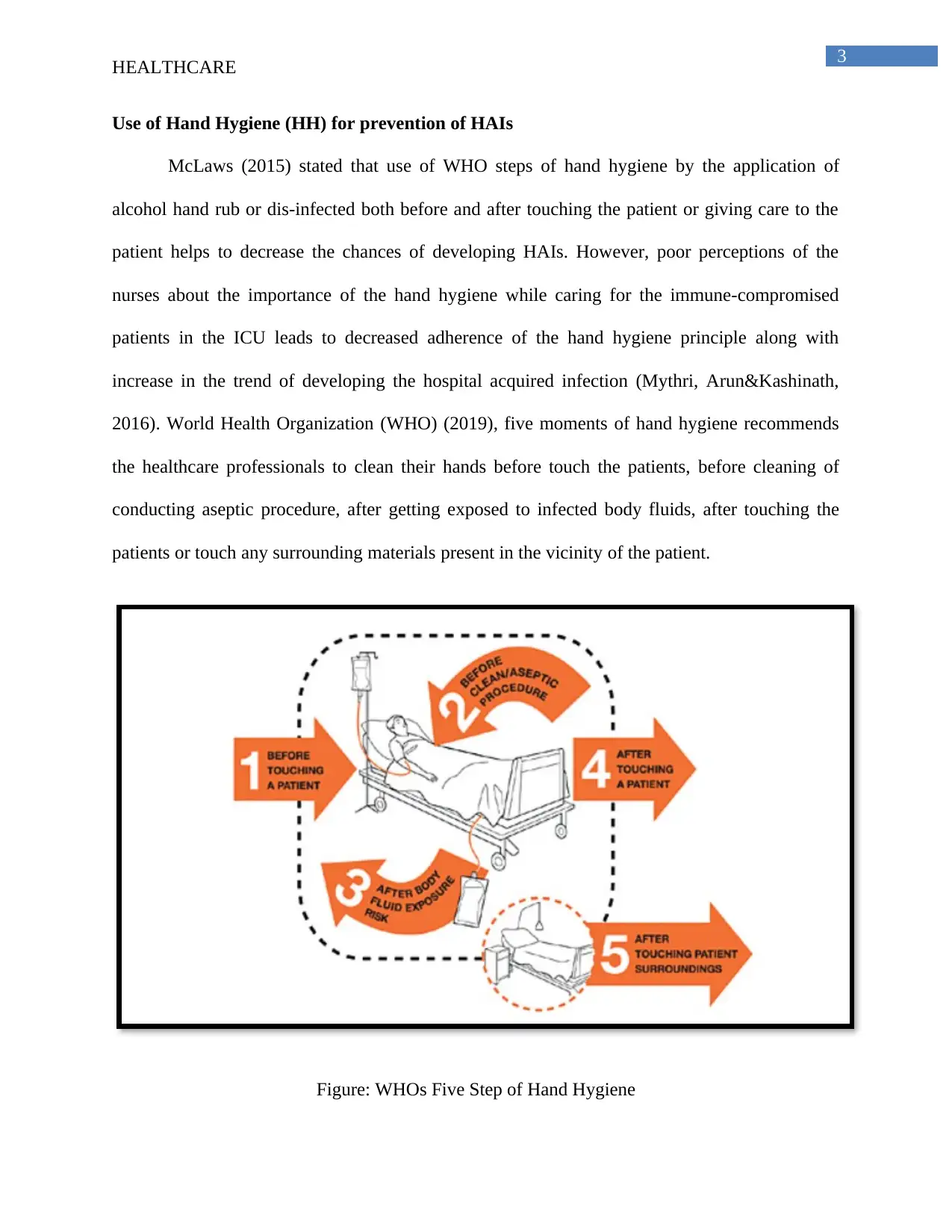
Use of Hand Hygiene (HH) for prevention of HAIs
McLaws (2015) stated that use of WHO steps of hand hygiene by the application of
alcohol hand rub or dis-infected both before and after touching the patient or giving care to the
patient helps to decrease the chances of developing HAIs. However, poor perceptions of the
nurses about the importance of the hand hygiene while caring for the immune-compromised
patients in the ICU leads to decreased adherence of the hand hygiene principle along with
increase in the trend of developing the hospital acquired infection (Mythri, Arun&Kashinath,
2016). World Health Organization (WHO) (2019), five moments of hand hygiene recommends
the healthcare professionals to clean their hands before touch the patients, before cleaning of
conducting aseptic procedure, after getting exposed to infected body fluids, after touching the
patients or touch any surrounding materials present in the vicinity of the patient.
Figure: WHOs Five Step of Hand Hygiene
HEALTHCARE
Use of Hand Hygiene (HH) for prevention of HAIs
McLaws (2015) stated that use of WHO steps of hand hygiene by the application of
alcohol hand rub or dis-infected both before and after touching the patient or giving care to the
patient helps to decrease the chances of developing HAIs. However, poor perceptions of the
nurses about the importance of the hand hygiene while caring for the immune-compromised
patients in the ICU leads to decreased adherence of the hand hygiene principle along with
increase in the trend of developing the hospital acquired infection (Mythri, Arun&Kashinath,
2016). World Health Organization (WHO) (2019), five moments of hand hygiene recommends
the healthcare professionals to clean their hands before touch the patients, before cleaning of
conducting aseptic procedure, after getting exposed to infected body fluids, after touching the
patients or touch any surrounding materials present in the vicinity of the patient.
Figure: WHOs Five Step of Hand Hygiene
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
HEALTHCARE
(Source: WHO, 2019)
Kingston, O'Connell and Dunne (2016) stated that proper compliance of the hand hygiene
procedure as stated by WHO helps to decrease HAIs at a significant rate. Sundal et al. (2017)
havehowever argued that increasing the nurses or the healthcare professionals’ compliance with
hand hygience procedures remains a significant challenge under the hospital settings. In order to
decrease the chances of the HAIs it is important to educate the nursing professionals to abide by
the guidelines of the WHO’s five step of the hand hygiene protocol. Identifying the nurses’
performance in hand hygiene is the first step towards developing teaching methods in order to
improve and to sustain their moment-specific compliance. Regular feedbacks along with
education and training of the nursing professionals under the hospital settings are important in
order to initiate the change management.
Implementation of change management
Kingston, O'Connell and Dunne (2016) stated that use of multimodal approach for the
effective adherence or implementation of hand hygiene (HH) intervention strategies whether
guided by WHO or through any other tested multimodal framework promotes only moderate
improvements in the compliance of HH. Kingston, O'Connell and Dunne (2016) recommended
that effective change management principle must be implemented in order to increase the
compliance of HH under the hospital settings.
Kurt Lewin’s Change Model (KLCM)
Thus in order to bring a positive change under the healthcare settings, I will make use of
the Kurt Lewin’s Change management Model. Kurt Lewin’s Change Model (KLCM) involves
three steps that include unfreezing, changing and then refreezing. This model is practical and
HEALTHCARE
(Source: WHO, 2019)
Kingston, O'Connell and Dunne (2016) stated that proper compliance of the hand hygiene
procedure as stated by WHO helps to decrease HAIs at a significant rate. Sundal et al. (2017)
havehowever argued that increasing the nurses or the healthcare professionals’ compliance with
hand hygience procedures remains a significant challenge under the hospital settings. In order to
decrease the chances of the HAIs it is important to educate the nursing professionals to abide by
the guidelines of the WHO’s five step of the hand hygiene protocol. Identifying the nurses’
performance in hand hygiene is the first step towards developing teaching methods in order to
improve and to sustain their moment-specific compliance. Regular feedbacks along with
education and training of the nursing professionals under the hospital settings are important in
order to initiate the change management.
Implementation of change management
Kingston, O'Connell and Dunne (2016) stated that use of multimodal approach for the
effective adherence or implementation of hand hygiene (HH) intervention strategies whether
guided by WHO or through any other tested multimodal framework promotes only moderate
improvements in the compliance of HH. Kingston, O'Connell and Dunne (2016) recommended
that effective change management principle must be implemented in order to increase the
compliance of HH under the hospital settings.
Kurt Lewin’s Change Model (KLCM)
Thus in order to bring a positive change under the healthcare settings, I will make use of
the Kurt Lewin’s Change management Model. Kurt Lewin’s Change Model (KLCM) involves
three steps that include unfreezing, changing and then refreezing. This model is practical and
5
HEALTHCARE
simple and thus can be effective under the healthcare settings of the low or middle income
countries that suffer from lack of adequate funding. According to Lewin, the process of change
entails generation of need for change and then progressing towards the new practice approach
and then solidifying the new practice approach as the inherent norm of the system(Cummings,
Bridgman & Brown, 2016). Hassan (2018) stated that this model is widely used and serves as the
basis for many modern change models. Hassan (2018) further stated that under the healthcare
settings, the change management mode of Lewin is prove to be effective in order to bring a
positive change under the healthcare settings.
Unfreezing
This is the first step of KLCM. It states that before change can be implemented, an
atmosphere must be created that is ready to welcome the new change. As people will naturally
resist adopting with the new change, the goal during unfreezing stage will be to create awareness
about the change or educate the people about the importance of the change. This will help to
improve the acceptability of the change while eliminating the hindrance that comes in the way of
implementing new change(Hassan, 2018). Ocasio, Laamanen and Vaara(2018) stated that
communication is crucial during the unfreezing stage. Effective communication helps the staffs
or the employees to get informed about the change and its importance under the work place
settings. In case of implementation of WHO’s five step of the HH procedure under the hospital
settings, among the nurses, the first step that must be undertaken include educating the nursing
professionals about the importance of the HH procedure and how it can aid in improving the
overall quality of care by reducing the chances of HAIs. Farhoudiet al. (2016)stated that
education of the nursing professionals under the healthcare settings by physicians helps to
increase the level of awareness among the nursing professionals. It also helps to increase the
HEALTHCARE
simple and thus can be effective under the healthcare settings of the low or middle income
countries that suffer from lack of adequate funding. According to Lewin, the process of change
entails generation of need for change and then progressing towards the new practice approach
and then solidifying the new practice approach as the inherent norm of the system(Cummings,
Bridgman & Brown, 2016). Hassan (2018) stated that this model is widely used and serves as the
basis for many modern change models. Hassan (2018) further stated that under the healthcare
settings, the change management mode of Lewin is prove to be effective in order to bring a
positive change under the healthcare settings.
Unfreezing
This is the first step of KLCM. It states that before change can be implemented, an
atmosphere must be created that is ready to welcome the new change. As people will naturally
resist adopting with the new change, the goal during unfreezing stage will be to create awareness
about the change or educate the people about the importance of the change. This will help to
improve the acceptability of the change while eliminating the hindrance that comes in the way of
implementing new change(Hassan, 2018). Ocasio, Laamanen and Vaara(2018) stated that
communication is crucial during the unfreezing stage. Effective communication helps the staffs
or the employees to get informed about the change and its importance under the work place
settings. In case of implementation of WHO’s five step of the HH procedure under the hospital
settings, among the nurses, the first step that must be undertaken include educating the nursing
professionals about the importance of the HH procedure and how it can aid in improving the
overall quality of care by reducing the chances of HAIs. Farhoudiet al. (2016)stated that
education of the nursing professionals under the healthcare settings by physicians helps to
increase the level of awareness among the nursing professionals. It also helps to increase the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
HEALTHCARE
understanding among the nurses and the doctors thus helping to implement effective
collaboration. The educational program must be designed with the help of power-point
presentations and with the help of posters.
Changing
After the people become well aware about the importance of change, the said change can
be effectively implemented. According to Lewin, a change can be defined as a process where the
organization must experience the transition or move into the new state. Thus this step is also
known as transitioning or moving step that can be marked by proper implementation of the
change. It is under this process, that the change becomes real. However, this time is marked with
fear and uncertainity and thus it is a hardest step to overcome. Proper support and
communication are keys for attaining success in this stage (Hassan, 2018). Thus for the
implementation of the change in practice among the nursing professionals working in the ICU or
the CCU units, proper support must be given for successful implementation of the change. Here
support can be highlighted like proper supply of the hand rub, soaps or antiseptic at the bedside
of the patients so that the nurses might not miss out the process of hand sanitization. This will be
followed by installation of posters at the entry of at the bed side of the patients in the ICU. The
posters will showcases the steps to be conducted to abide hand hygiene. This will help to
implement the change in a successful manner. Sadule-Rios and Aguilera (2017) are of the
opinion that lack of proper resources at the bed side and lack of proper guidance are the two
principal factors behind the lack of adherence of the HH among the nurses. Proper support,
monitoring the gaps in performance and arranging training needs accordingly will help to bring
positive change under health care settings.
HEALTHCARE
understanding among the nurses and the doctors thus helping to implement effective
collaboration. The educational program must be designed with the help of power-point
presentations and with the help of posters.
Changing
After the people become well aware about the importance of change, the said change can
be effectively implemented. According to Lewin, a change can be defined as a process where the
organization must experience the transition or move into the new state. Thus this step is also
known as transitioning or moving step that can be marked by proper implementation of the
change. It is under this process, that the change becomes real. However, this time is marked with
fear and uncertainity and thus it is a hardest step to overcome. Proper support and
communication are keys for attaining success in this stage (Hassan, 2018). Thus for the
implementation of the change in practice among the nursing professionals working in the ICU or
the CCU units, proper support must be given for successful implementation of the change. Here
support can be highlighted like proper supply of the hand rub, soaps or antiseptic at the bedside
of the patients so that the nurses might not miss out the process of hand sanitization. This will be
followed by installation of posters at the entry of at the bed side of the patients in the ICU. The
posters will showcases the steps to be conducted to abide hand hygiene. This will help to
implement the change in a successful manner. Sadule-Rios and Aguilera (2017) are of the
opinion that lack of proper resources at the bed side and lack of proper guidance are the two
principal factors behind the lack of adherence of the HH among the nurses. Proper support,
monitoring the gaps in performance and arranging training needs accordingly will help to bring
positive change under health care settings.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
HEALTHCARE
Refreezing
This is the final step of change management model and deals with reinforcing and
stabilizing the new change in the operational system. This step is important for ensuring that
people do not revert back to the old norms. In order to re-inforce the change, one of the widely
acknowledged approach I giving rewards and recognition (Hassan, 2018). Saccoet al. (2015) are
of the opinion that nurses work under stressful job environment with no fixed duty hours. The
increase in the patients load, the requirement of the use of proper communication sills when
interacting with the patients and following doctor’s prescription stringently increase the job
stress and thus creating job-related burnout. For refreezing the change, the job burnout must be
reduced and this will motivate more nurses to spontaneously adapt the new change. This can be
done by giving rewards and recognition. Rewards and recognition helps to motivate the nurses
thus reducing job burnout and increasing the chance of solidifying the change in practice(Van
Mol et al., 2015).
Measurement of the outcome
The measurement of the outcome of change implemented under the healthcare settings
will be done post 3 months of refreezing the change. The change will be assessed by reporting
the the number the cases of HAIs that has occurred 3 moths post refreezing of the HH approach
among the nursing professionals under ICU settings. The data will be compared with the baseline
data.
Conclusion and Recommendation
Thus from the above discussion it can be concluded that KLCM principle can be prove to
be effective in introducing change in practice. The change in practice of use of WHO’s 5 step of
HEALTHCARE
Refreezing
This is the final step of change management model and deals with reinforcing and
stabilizing the new change in the operational system. This step is important for ensuring that
people do not revert back to the old norms. In order to re-inforce the change, one of the widely
acknowledged approach I giving rewards and recognition (Hassan, 2018). Saccoet al. (2015) are
of the opinion that nurses work under stressful job environment with no fixed duty hours. The
increase in the patients load, the requirement of the use of proper communication sills when
interacting with the patients and following doctor’s prescription stringently increase the job
stress and thus creating job-related burnout. For refreezing the change, the job burnout must be
reduced and this will motivate more nurses to spontaneously adapt the new change. This can be
done by giving rewards and recognition. Rewards and recognition helps to motivate the nurses
thus reducing job burnout and increasing the chance of solidifying the change in practice(Van
Mol et al., 2015).
Measurement of the outcome
The measurement of the outcome of change implemented under the healthcare settings
will be done post 3 months of refreezing the change. The change will be assessed by reporting
the the number the cases of HAIs that has occurred 3 moths post refreezing of the HH approach
among the nursing professionals under ICU settings. The data will be compared with the baseline
data.
Conclusion and Recommendation
Thus from the above discussion it can be concluded that KLCM principle can be prove to
be effective in introducing change in practice. The change in practice of use of WHO’s 5 step of
8
HEALTHCARE
HH under the hospital settings will help to reduce the chances of HAIs and thereby helping to
reduce the cost of care while improving the quality outcome. Training and education of the
nurses are principle keys towards implementation of the change.
Apart from using Kurt Lewin's three-step change model, bundle approach can also be
used for the effective prevention of the HAIs. However, bundle approach is a relatively new
concept that is being revolutionizing in the ICU having high risk patients. The proper application
of the bundle approach can be prove to be helpful under the healthcare settings of the low and the
middle income countries. However,, focus must also be given on the very basic of the bundle
approach that is development, assessment and implementation of the new change in the health
care practice in order to make the overall approach cost-effective(Mathur, 2018).
HEALTHCARE
HH under the hospital settings will help to reduce the chances of HAIs and thereby helping to
reduce the cost of care while improving the quality outcome. Training and education of the
nurses are principle keys towards implementation of the change.
Apart from using Kurt Lewin's three-step change model, bundle approach can also be
used for the effective prevention of the HAIs. However, bundle approach is a relatively new
concept that is being revolutionizing in the ICU having high risk patients. The proper application
of the bundle approach can be prove to be helpful under the healthcare settings of the low and the
middle income countries. However,, focus must also be given on the very basic of the bundle
approach that is development, assessment and implementation of the new change in the health
care practice in order to make the overall approach cost-effective(Mathur, 2018).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
HEALTHCARE
References
Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps:
Rethinking Kurt Lewin’s legacy for change management. Human relations, 69(1), 33-60.
Farhoudi, F., SanaeiDashti, A., HoshangiDavani, M., Ghalebi, N., Sajadi, G., &Taghizadeh, R.
(2016). Impact of WHO hand hygiene improvement program implementation: a quasi-
experimental trial. BioMed research international, 2016.
Haque, M., Sartelli, M., McKimm, J. &Bakar, M.A., (2018).Health care-associated infections–an
overview. Infection and drug resistance, 11, p.2321.
Hassan, A. T. (2018). Organizational Change Management: A Literature Review. Available at
SSRN 3135770.
Khan, H.A., Ahmad, A. &Mehboob, R., (2015).Nosocomial infections and their control
strategies. Asian pacific journal of tropical biomedicine, 5(7), pp.509-514.
Kingston, L., O'Connell, N.H. & Dunne, C.P., (2016). Hand hygiene-related clinical trials
reported since 2010: a systematic review. Journal of Hospital Infection, 92(4), pp.309-
320.
Mathur, P. (2018). Prevention of healthcare-associated infections in low-and middle-income
Countries: The'bundle approach'. Indian journal of medical microbiology, 36(2), 155.
McLaws, M.L., (2015). The relationship between hand hygiene and health care-associated
infection: it’s complicated. Infection and drug resistance, 8, p.7.
HEALTHCARE
References
Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps:
Rethinking Kurt Lewin’s legacy for change management. Human relations, 69(1), 33-60.
Farhoudi, F., SanaeiDashti, A., HoshangiDavani, M., Ghalebi, N., Sajadi, G., &Taghizadeh, R.
(2016). Impact of WHO hand hygiene improvement program implementation: a quasi-
experimental trial. BioMed research international, 2016.
Haque, M., Sartelli, M., McKimm, J. &Bakar, M.A., (2018).Health care-associated infections–an
overview. Infection and drug resistance, 11, p.2321.
Hassan, A. T. (2018). Organizational Change Management: A Literature Review. Available at
SSRN 3135770.
Khan, H.A., Ahmad, A. &Mehboob, R., (2015).Nosocomial infections and their control
strategies. Asian pacific journal of tropical biomedicine, 5(7), pp.509-514.
Kingston, L., O'Connell, N.H. & Dunne, C.P., (2016). Hand hygiene-related clinical trials
reported since 2010: a systematic review. Journal of Hospital Infection, 92(4), pp.309-
320.
Mathur, P. (2018). Prevention of healthcare-associated infections in low-and middle-income
Countries: The'bundle approach'. Indian journal of medical microbiology, 36(2), 155.
McLaws, M.L., (2015). The relationship between hand hygiene and health care-associated
infection: it’s complicated. Infection and drug resistance, 8, p.7.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
HEALTHCARE
Mythri, H., Arun, A., &Kashinath, K. R. (2016).Perception and Practice Regarding Infection
Control Measures among Healthcare Workers in District Government Hospital of
Tumkur, India. Indian Journal of Public Health Research & Development, 7(1).
Ocasio, W., Laamanen, T., &Vaara, E. (2018). Communication and attention dynamics: An
attention‐based view of strategic change. Strategic Management Journal, 39(1), 155-167.
Sacco, T. L., Ciurzynski, S. M., Harvey, M. E., & Ingersoll, G. L. (2015). Compassion
satisfaction and compassion fatigue among critical care nurses. Critical care nurse, 35(4),
32-42.
Sadule-Rios, N., & Aguilera, G. (2017). Nurses’ perceptions of reasons for persistent low rates in
hand hygiene compliance. Intensive and Critical Care Nursing, 42, 17-21.
Sundal, J. S., Aune, A. G., Storvig, E., Aasland, J. K., Fjeldsæter, K. L., &Torjuul, K. (2017).
The hand hygiene compliance of student nurses during clinical placements. Journal of
clinical nursing, 26(23-24), 4646-4653.
Swaminathan, S., Prasad, J., Dhariwal, A. C., Guleria, R., Misra, M. C., Malhotra, R., ...&Ohri,
V. (2017). Strengthening infection prevention and control and systematic surveillance of
healthcare associated infections in India. bmj, 358, j3768.
Van Mol, M. M., Kompanje, E. J., Benoit, D. D., Bakker, J., &Nijkamp, M. D. (2015). The
prevalence of compassion fatigue and burnout among healthcare professionals in
intensive care units: a systematic review. PloS one, 10(8), e0136955.
HEALTHCARE
Mythri, H., Arun, A., &Kashinath, K. R. (2016).Perception and Practice Regarding Infection
Control Measures among Healthcare Workers in District Government Hospital of
Tumkur, India. Indian Journal of Public Health Research & Development, 7(1).
Ocasio, W., Laamanen, T., &Vaara, E. (2018). Communication and attention dynamics: An
attention‐based view of strategic change. Strategic Management Journal, 39(1), 155-167.
Sacco, T. L., Ciurzynski, S. M., Harvey, M. E., & Ingersoll, G. L. (2015). Compassion
satisfaction and compassion fatigue among critical care nurses. Critical care nurse, 35(4),
32-42.
Sadule-Rios, N., & Aguilera, G. (2017). Nurses’ perceptions of reasons for persistent low rates in
hand hygiene compliance. Intensive and Critical Care Nursing, 42, 17-21.
Sundal, J. S., Aune, A. G., Storvig, E., Aasland, J. K., Fjeldsæter, K. L., &Torjuul, K. (2017).
The hand hygiene compliance of student nurses during clinical placements. Journal of
clinical nursing, 26(23-24), 4646-4653.
Swaminathan, S., Prasad, J., Dhariwal, A. C., Guleria, R., Misra, M. C., Malhotra, R., ...&Ohri,
V. (2017). Strengthening infection prevention and control and systematic surveillance of
healthcare associated infections in India. bmj, 358, j3768.
Van Mol, M. M., Kompanje, E. J., Benoit, D. D., Bakker, J., &Nijkamp, M. D. (2015). The
prevalence of compassion fatigue and burnout among healthcare professionals in
intensive care units: a systematic review. PloS one, 10(8), e0136955.
11
HEALTHCARE
World Health Organization.(WHO).(2019). My 5 Moments for Hand Hygiene. Access date: 27th
June 2019. Retrieved from: https://www.who.int/infection-prevention/campaigns/clean-
hands/5moments/en/
HEALTHCARE
World Health Organization.(WHO).(2019). My 5 Moments for Hand Hygiene. Access date: 27th
June 2019. Retrieved from: https://www.who.int/infection-prevention/campaigns/clean-
hands/5moments/en/
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





