Strategies to Reduce Hospital Acquired Infections - Nursing Essay
VerifiedAdded on 2023/03/23
|12
|4096
|91
Essay
AI Summary
This essay addresses the increasing number of hospital-acquired infections (HAIs) by identifying and discussing two key strategies for their reduction, in response to a Nurse Unit Manager's (NUM) request. It emphasizes the significance of HAIs as a patient safety issue, highlighting their impact on morbidity, mortality, and healthcare costs within the Australian context, referencing the Australian Commission on Safety and Quality in Health Care and the Victorian Clinical Governance Framework. The essay focuses on evidence-based hand hygiene practices and appropriate antimicrobial stewardship as crucial interventions. It details actions for consumers, healthcare providers, healthcare organizations, government bodies, and educational institutions to improve hand hygiene compliance and antimicrobial prescribing. The ultimate goal is to reduce harm from HAIs through effective infection control and antimicrobial stewardship, supported by national guidelines and monitoring programs.

healthcare
associated
infection
A C T I O N G U I D E
1.2
associated
infection
A C T I O N G U I D E
1.2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
01 A U S T R A L I A N S A F E T Y A N D Q U A L I T Y G O A L S F O R H E A L T H C A R E
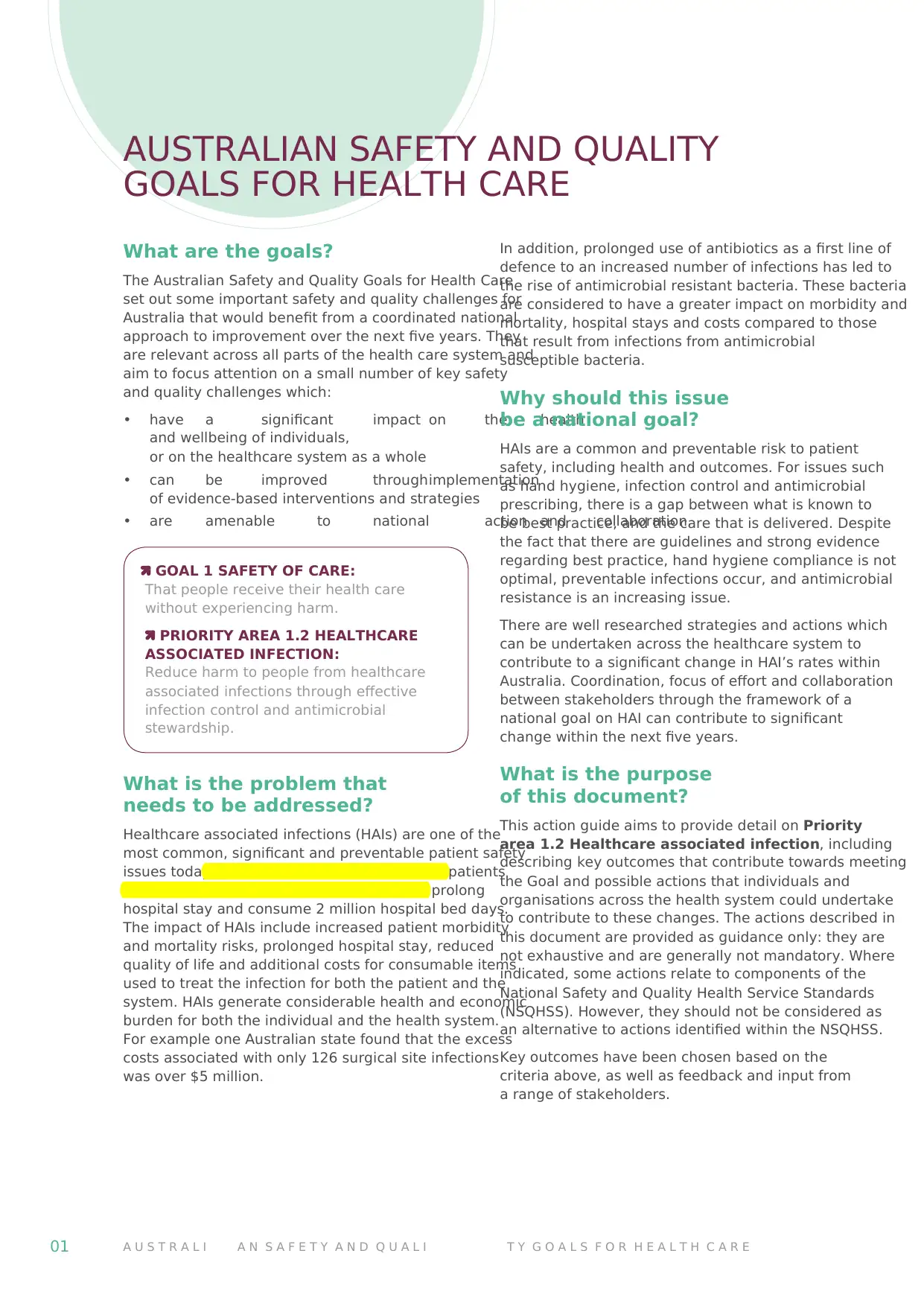
What are the goals?
The Australian Safety and Quality Goals for Health Care
set out some important safety and quality challenges for
Australia that would benefit from a coordinated national
approach to improvement over the next five years. They
are relevant across all parts of the health care system and
aim to focus attention on a small number of key safety
and quality challenges which:
• have a significant impact on the health
and wellbeing of individuals,
or on the healthcare system as a whole
• can be improved throughimplementation
of evidence-based interventions and strategies
• are amenable to national action and collaboration.
GOAL 1 SAFETY OF CARE:
That people receive their health care
without experiencing harm.
PRIORITY AREA 1.2 HEALTHCARE
ASSOCIATED INFECTION:
Reduce harm to people from healthcare
associated infections through effective
infection control and antimicrobial
stewardship.
What is the problem that
needs to be addressed?
Healthcare associated infections (HAIs) are one of the
most common, significant and preventable patient safety
issues today. Each year in Australian 180,000 patients
suffer healthcare associated infections that prolong
hospital stay and consume 2 million hospital bed days.
The impact of HAIs include increased patient morbidity
and mortality risks, prolonged hospital stay, reduced
quality of life and additional costs for consumable items
used to treat the infection for both the patient and the
system. HAIs generate considerable health and economic
burden for both the individual and the health system.
For example one Australian state found that the excess
costs associated with only 126 surgical site infections
was over $5 million.
In addition, prolonged use of antibiotics as a first line of
defence to an increased number of infections has led to
the rise of antimicrobial resistant bacteria. These bacteria
are considered to have a greater impact on morbidity and
mortality, hospital stays and costs compared to those
that result from infections from antimicrobial
susceptible bacteria.
Why should this issue
be a national goal?
HAIs are a common and preventable risk to patient
safety, including health and outcomes. For issues such
as hand hygiene, infection control and antimicrobial
prescribing, there is a gap between what is known to
be best practice, and the care that is delivered. Despite
the fact that there are guidelines and strong evidence
regarding best practice, hand hygiene compliance is not
optimal, preventable infections occur, and antimicrobial
resistance is an increasing issue.
There are well researched strategies and actions which
can be undertaken across the healthcare system to
contribute to a significant change in HAI’s rates within
Australia. Coordination, focus of effort and collaboration
between stakeholders through the framework of a
national goal on HAI can contribute to significant
change within the next five years.
What is the purpose
of this document?
This action guide aims to provide detail on Priority
area 1.2 Healthcare associated infection, including
describing key outcomes that contribute towards meeting
the Goal and possible actions that individuals and
organisations across the health system could undertake
to contribute to these changes. The actions described in
this document are provided as guidance only: they are
not exhaustive and are generally not mandatory. Where
indicated, some actions relate to components of the
National Safety and Quality Health Service Standards
(NSQHSS). However, they should not be considered as
an alternative to actions identified within the NSQHSS.
Key outcomes have been chosen based on the
criteria above, as well as feedback and input from
a range of stakeholders.
AUSTRALIAN SAFETY AND QUALITY
GOALS FOR HEALTH CARE
What are the goals?
The Australian Safety and Quality Goals for Health Care
set out some important safety and quality challenges for
Australia that would benefit from a coordinated national
approach to improvement over the next five years. They
are relevant across all parts of the health care system and
aim to focus attention on a small number of key safety
and quality challenges which:
• have a significant impact on the health
and wellbeing of individuals,
or on the healthcare system as a whole
• can be improved throughimplementation
of evidence-based interventions and strategies
• are amenable to national action and collaboration.
GOAL 1 SAFETY OF CARE:
That people receive their health care
without experiencing harm.
PRIORITY AREA 1.2 HEALTHCARE
ASSOCIATED INFECTION:
Reduce harm to people from healthcare
associated infections through effective
infection control and antimicrobial
stewardship.
What is the problem that
needs to be addressed?
Healthcare associated infections (HAIs) are one of the
most common, significant and preventable patient safety
issues today. Each year in Australian 180,000 patients
suffer healthcare associated infections that prolong
hospital stay and consume 2 million hospital bed days.
The impact of HAIs include increased patient morbidity
and mortality risks, prolonged hospital stay, reduced
quality of life and additional costs for consumable items
used to treat the infection for both the patient and the
system. HAIs generate considerable health and economic
burden for both the individual and the health system.
For example one Australian state found that the excess
costs associated with only 126 surgical site infections
was over $5 million.
In addition, prolonged use of antibiotics as a first line of
defence to an increased number of infections has led to
the rise of antimicrobial resistant bacteria. These bacteria
are considered to have a greater impact on morbidity and
mortality, hospital stays and costs compared to those
that result from infections from antimicrobial
susceptible bacteria.
Why should this issue
be a national goal?
HAIs are a common and preventable risk to patient
safety, including health and outcomes. For issues such
as hand hygiene, infection control and antimicrobial
prescribing, there is a gap between what is known to
be best practice, and the care that is delivered. Despite
the fact that there are guidelines and strong evidence
regarding best practice, hand hygiene compliance is not
optimal, preventable infections occur, and antimicrobial
resistance is an increasing issue.
There are well researched strategies and actions which
can be undertaken across the healthcare system to
contribute to a significant change in HAI’s rates within
Australia. Coordination, focus of effort and collaboration
between stakeholders through the framework of a
national goal on HAI can contribute to significant
change within the next five years.
What is the purpose
of this document?
This action guide aims to provide detail on Priority
area 1.2 Healthcare associated infection, including
describing key outcomes that contribute towards meeting
the Goal and possible actions that individuals and
organisations across the health system could undertake
to contribute to these changes. The actions described in
this document are provided as guidance only: they are
not exhaustive and are generally not mandatory. Where
indicated, some actions relate to components of the
National Safety and Quality Health Service Standards
(NSQHSS). However, they should not be considered as
an alternative to actions identified within the NSQHSS.
Key outcomes have been chosen based on the
criteria above, as well as feedback and input from
a range of stakeholders.
AUSTRALIAN SAFETY AND QUALITY
GOALS FOR HEALTH CARE
A C T I O N G U I D E I H E A L T H C A R E A S S O C I A T E D I N F E C T I O N 02
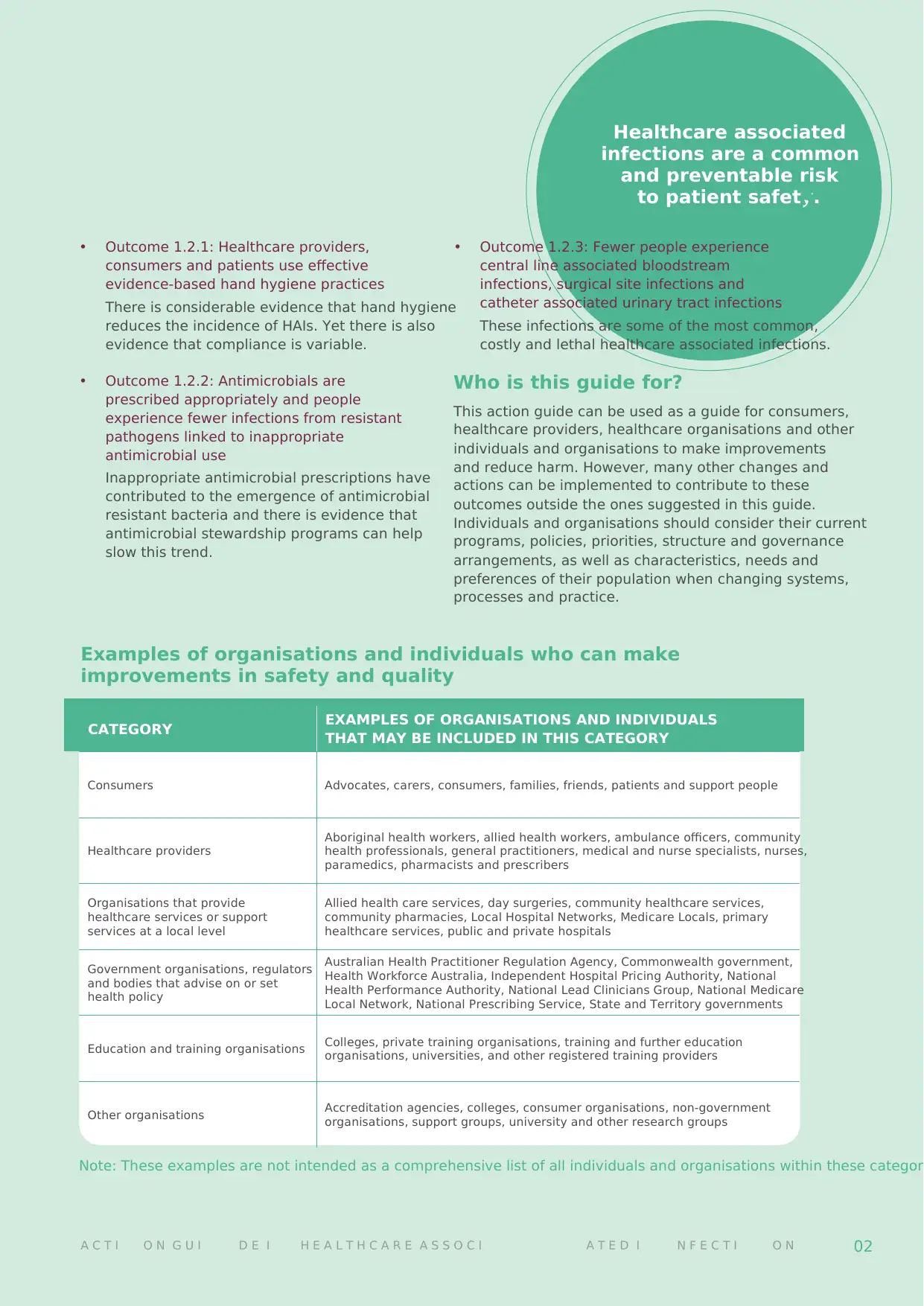
CATEGORY EXAMPLES OF ORGANISATIONS AND INDIVIDUALS
THAT MAY BE INCLUDED IN THIS CATEGORY
Consumers Advocates, carers, consumers, families, friends, patients and support people
Healthcare providers
Aboriginal health workers, allied health workers, ambulance officers, community
health professionals, general practitioners, medical and nurse specialists, nurses,
paramedics, pharmacists and prescribers
Organisations that provide
healthcare services or support
services at a local level
Allied health care services, day surgeries, community healthcare services,
community pharmacies, Local Hospital Networks, Medicare Locals, primary
healthcare services, public and private hospitals
Government organisations, regulators
and bodies that advise on or set
health policy
Australian Health Practitioner Regulation Agency, Commonwealth government,
Health Workforce Australia, Independent Hospital Pricing Authority, National
Health Performance Authority, National Lead Clinicians Group, National Medicare
Local Network, National Prescribing Service, State and Territory governments
Education and training organisations Colleges, private training organisations, training and further education
organisations, universities, and other registered training providers
Other organisations Accreditation agencies, colleges, consumer organisations, non-government
organisations, support groups, university and other research groups
Examples of organisations and individuals who can make
improvements in safety and quality
Healthcare associated
infections are a common
and preventable risk
to patient safety.
• Outcome 1.2.1: Healthcare providers,
consumers and patients use effective
evidence-based hand hygiene practices
There is considerable evidence that hand hygiene
reduces the incidence of HAIs. Yet there is also
evidence that compliance is variable.
• Outcome 1.2.2: Antimicrobials are
prescribed appropriately and people
experience fewer infections from resistant
pathogens linked to inappropriate
antimicrobial use
Inappropriate antimicrobial prescriptions have
contributed to the emergence of antimicrobial
resistant bacteria and there is evidence that
antimicrobial stewardship programs can help
slow this trend.
• Outcome 1.2.3: Fewer people experience
central line associated bloodstream
infections, surgical site infections and
catheter associated urinary tract infections
These infections are some of the most common,
costly and lethal healthcare associated infections.
Who is this guide for?
This action guide can be used as a guide for consumers,
healthcare providers, healthcare organisations and other
individuals and organisations to make improvements
and reduce harm. However, many other changes and
actions can be implemented to contribute to these
outcomes outside the ones suggested in this guide.
Individuals and organisations should consider their current
programs, policies, priorities, structure and governance
arrangements, as well as characteristics, needs and
preferences of their population when changing systems,
processes and practice.
Note: These examples are not intended as a comprehensive list of all individuals and organisations within these categor
CATEGORY EXAMPLES OF ORGANISATIONS AND INDIVIDUALS
THAT MAY BE INCLUDED IN THIS CATEGORY
Consumers Advocates, carers, consumers, families, friends, patients and support people
Healthcare providers
Aboriginal health workers, allied health workers, ambulance officers, community
health professionals, general practitioners, medical and nurse specialists, nurses,
paramedics, pharmacists and prescribers
Organisations that provide
healthcare services or support
services at a local level
Allied health care services, day surgeries, community healthcare services,
community pharmacies, Local Hospital Networks, Medicare Locals, primary
healthcare services, public and private hospitals
Government organisations, regulators
and bodies that advise on or set
health policy
Australian Health Practitioner Regulation Agency, Commonwealth government,
Health Workforce Australia, Independent Hospital Pricing Authority, National
Health Performance Authority, National Lead Clinicians Group, National Medicare
Local Network, National Prescribing Service, State and Territory governments
Education and training organisations Colleges, private training organisations, training and further education
organisations, universities, and other registered training providers
Other organisations Accreditation agencies, colleges, consumer organisations, non-government
organisations, support groups, university and other research groups
Examples of organisations and individuals who can make
improvements in safety and quality
Healthcare associated
infections are a common
and preventable risk
to patient safety.
• Outcome 1.2.1: Healthcare providers,
consumers and patients use effective
evidence-based hand hygiene practices
There is considerable evidence that hand hygiene
reduces the incidence of HAIs. Yet there is also
evidence that compliance is variable.
• Outcome 1.2.2: Antimicrobials are
prescribed appropriately and people
experience fewer infections from resistant
pathogens linked to inappropriate
antimicrobial use
Inappropriate antimicrobial prescriptions have
contributed to the emergence of antimicrobial
resistant bacteria and there is evidence that
antimicrobial stewardship programs can help
slow this trend.
• Outcome 1.2.3: Fewer people experience
central line associated bloodstream
infections, surgical site infections and
catheter associated urinary tract infections
These infections are some of the most common,
costly and lethal healthcare associated infections.
Who is this guide for?
This action guide can be used as a guide for consumers,
healthcare providers, healthcare organisations and other
individuals and organisations to make improvements
and reduce harm. However, many other changes and
actions can be implemented to contribute to these
outcomes outside the ones suggested in this guide.
Individuals and organisations should consider their current
programs, policies, priorities, structure and governance
arrangements, as well as characteristics, needs and
preferences of their population when changing systems,
processes and practice.
Note: These examples are not intended as a comprehensive list of all individuals and organisations within these categor
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
03 A U S T R A L I A N S A F E T Y A N D Q U A L I T Y G O A L S F O R H E A L T H C A R E
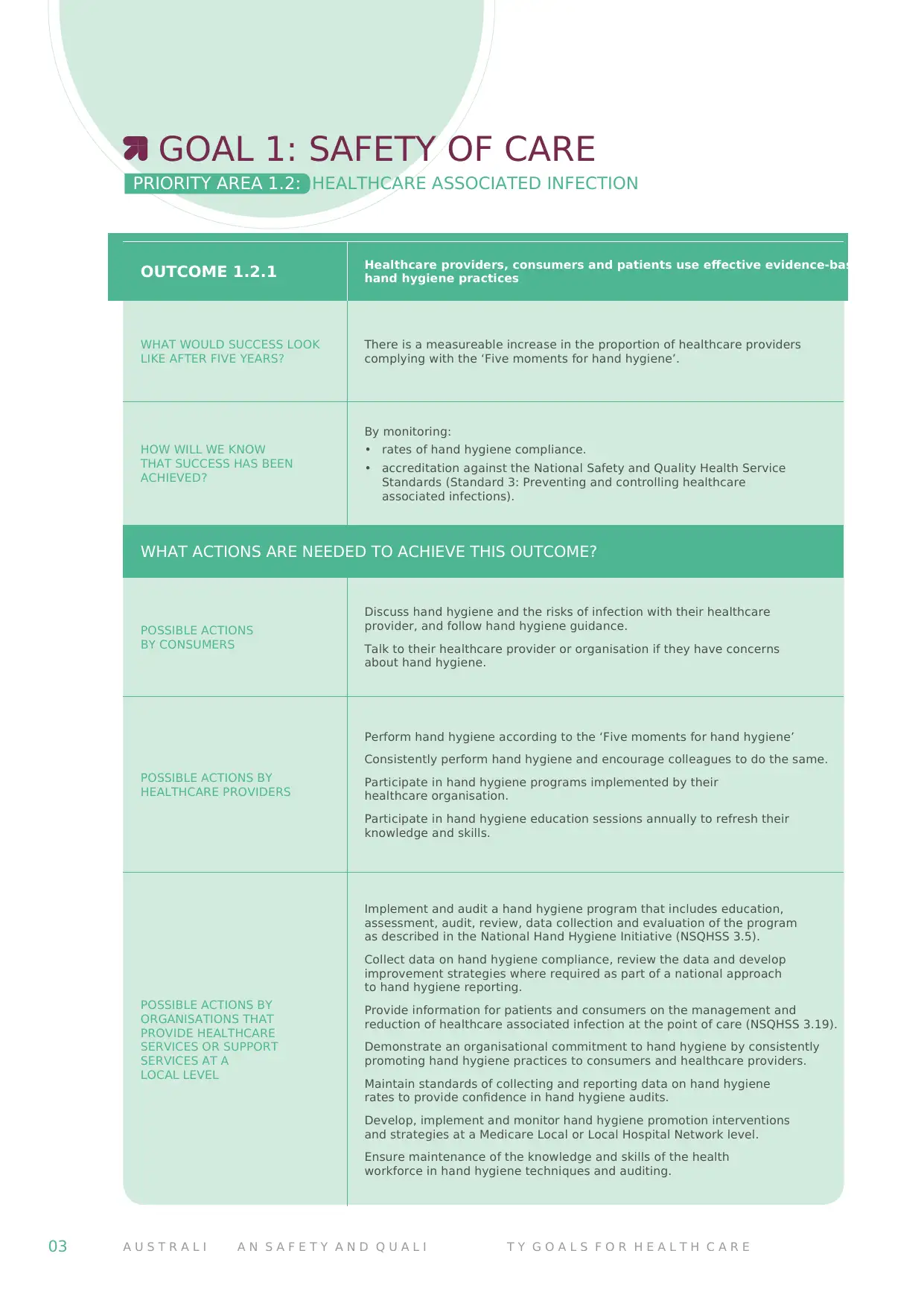
OUTCOME 1.2.1 Healthcare providers, consumers and patients use effective evidence-based
hand hygiene practices
WHAT WOULD SUCCESS LOOK
LIKE AFTER FIVE YEARS?
There is a measureable increase in the proportion of healthcare providers
complying with the ‘Five moments for hand hygiene’.
HOW WILL WE KNOW
THAT SUCCESS HAS BEEN
ACHIEVED?
By monitoring:
• rates of hand hygiene compliance.
• accreditation against the National Safety and Quality Health Service
Standards (Standard 3: Preventing and controlling healthcare
associated infections).
WHAT ACTIONS ARE NEEDED TO ACHIEVE THIS OUTCOME?
POSSIBLE ACTIONS
BY CONSUMERS
Discuss hand hygiene and the risks of infection with their healthcare
provider, and follow hand hygiene guidance.
Talk to their healthcare provider or organisation if they have concerns
about hand hygiene.
POSSIBLE ACTIONS BY
HEALTHCARE PROVIDERS
Perform hand hygiene according to the ‘Five moments for hand hygiene’
Consistently perform hand hygiene and encourage colleagues to do the same.
Participate in hand hygiene programs implemented by their
healthcare organisation.
Participate in hand hygiene education sessions annually to refresh their
knowledge and skills.
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A
LOCAL LEVEL
Implement and audit a hand hygiene program that includes education,
assessment, audit, review, data collection and evaluation of the program
as described in the National Hand Hygiene Initiative (NSQHSS 3.5).
Collect data on hand hygiene compliance, review the data and develop
improvement strategies where required as part of a national approach
to hand hygiene reporting.
Provide information for patients and consumers on the management and
reduction of healthcare associated infection at the point of care (NSQHSS 3.19).
Demonstrate an organisational commitment to hand hygiene by consistently
promoting hand hygiene practices to consumers and healthcare providers.
Maintain standards of collecting and reporting data on hand hygiene
rates to provide confidence in hand hygiene audits.
Develop, implement and monitor hand hygiene promotion interventions
and strategies at a Medicare Local or Local Hospital Network level.
Ensure maintenance of the knowledge and skills of the health
workforce in hand hygiene techniques and auditing.
GOAL 1: SAFETY OF CARE
PRIORITY AREA 1.2: HEALTHCARE ASSOCIATED INFECTION
OUTCOME 1.2.1 Healthcare providers, consumers and patients use effective evidence-based
hand hygiene practices
WHAT WOULD SUCCESS LOOK
LIKE AFTER FIVE YEARS?
There is a measureable increase in the proportion of healthcare providers
complying with the ‘Five moments for hand hygiene’.
HOW WILL WE KNOW
THAT SUCCESS HAS BEEN
ACHIEVED?
By monitoring:
• rates of hand hygiene compliance.
• accreditation against the National Safety and Quality Health Service
Standards (Standard 3: Preventing and controlling healthcare
associated infections).
WHAT ACTIONS ARE NEEDED TO ACHIEVE THIS OUTCOME?
POSSIBLE ACTIONS
BY CONSUMERS
Discuss hand hygiene and the risks of infection with their healthcare
provider, and follow hand hygiene guidance.
Talk to their healthcare provider or organisation if they have concerns
about hand hygiene.
POSSIBLE ACTIONS BY
HEALTHCARE PROVIDERS
Perform hand hygiene according to the ‘Five moments for hand hygiene’
Consistently perform hand hygiene and encourage colleagues to do the same.
Participate in hand hygiene programs implemented by their
healthcare organisation.
Participate in hand hygiene education sessions annually to refresh their
knowledge and skills.
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A
LOCAL LEVEL
Implement and audit a hand hygiene program that includes education,
assessment, audit, review, data collection and evaluation of the program
as described in the National Hand Hygiene Initiative (NSQHSS 3.5).
Collect data on hand hygiene compliance, review the data and develop
improvement strategies where required as part of a national approach
to hand hygiene reporting.
Provide information for patients and consumers on the management and
reduction of healthcare associated infection at the point of care (NSQHSS 3.19).
Demonstrate an organisational commitment to hand hygiene by consistently
promoting hand hygiene practices to consumers and healthcare providers.
Maintain standards of collecting and reporting data on hand hygiene
rates to provide confidence in hand hygiene audits.
Develop, implement and monitor hand hygiene promotion interventions
and strategies at a Medicare Local or Local Hospital Network level.
Ensure maintenance of the knowledge and skills of the health
workforce in hand hygiene techniques and auditing.
GOAL 1: SAFETY OF CARE
PRIORITY AREA 1.2: HEALTHCARE ASSOCIATED INFECTION
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
A C T I O N G U I D E I H E A L T H C A R E A S S O C I A T E D I N F E C T I O N 04
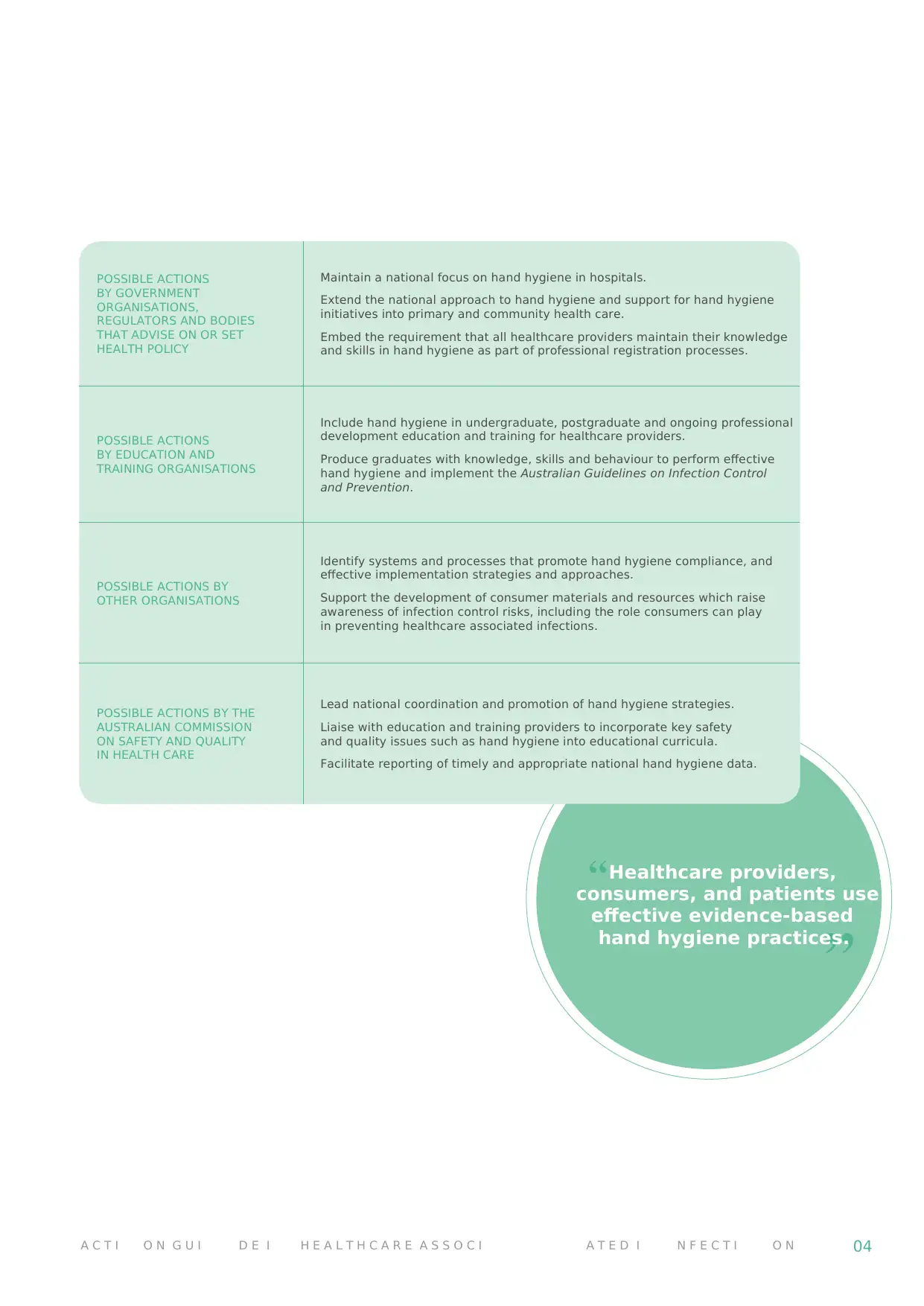
POSSIBLE ACTIONS
BY GOVERNMENT
ORGANISATIONS,
REGULATORS AND BODIES
THAT ADVISE ON OR SET
HEALTH POLICY
Maintain a national focus on hand hygiene in hospitals.
Extend the national approach to hand hygiene and support for hand hygiene
initiatives into primary and community health care.
Embed the requirement that all healthcare providers maintain their knowledge
and skills in hand hygiene as part of professional registration processes.
POSSIBLE ACTIONS
BY EDUCATION AND
TRAINING ORGANISATIONS
Include hand hygiene in undergraduate, postgraduate and ongoing professional
development education and training for healthcare providers.
Produce graduates with knowledge, skills and behaviour to perform effective
hand hygiene and implement the Australian Guidelines on Infection Control
and Prevention.
POSSIBLE ACTIONS BY
OTHER ORGANISATIONS
Identify systems and processes that promote hand hygiene compliance, and
effective implementation strategies and approaches.
Support the development of consumer materials and resources which raise
awareness of infection control risks, including the role consumers can play
in preventing healthcare associated infections.
POSSIBLE ACTIONS BY THE
AUSTRALIAN COMMISSION
ON SAFETY AND QUALITY
IN HEALTH CARE
Lead national coordination and promotion of hand hygiene strategies.
Liaise with education and training providers to incorporate key safety
and quality issues such as hand hygiene into educational curricula.
Facilitate reporting of timely and appropriate national hand hygiene data.
Healthcare providers,
consumers, and patients use
effective evidence-based
hand hygiene practices.
POSSIBLE ACTIONS
BY GOVERNMENT
ORGANISATIONS,
REGULATORS AND BODIES
THAT ADVISE ON OR SET
HEALTH POLICY
Maintain a national focus on hand hygiene in hospitals.
Extend the national approach to hand hygiene and support for hand hygiene
initiatives into primary and community health care.
Embed the requirement that all healthcare providers maintain their knowledge
and skills in hand hygiene as part of professional registration processes.
POSSIBLE ACTIONS
BY EDUCATION AND
TRAINING ORGANISATIONS
Include hand hygiene in undergraduate, postgraduate and ongoing professional
development education and training for healthcare providers.
Produce graduates with knowledge, skills and behaviour to perform effective
hand hygiene and implement the Australian Guidelines on Infection Control
and Prevention.
POSSIBLE ACTIONS BY
OTHER ORGANISATIONS
Identify systems and processes that promote hand hygiene compliance, and
effective implementation strategies and approaches.
Support the development of consumer materials and resources which raise
awareness of infection control risks, including the role consumers can play
in preventing healthcare associated infections.
POSSIBLE ACTIONS BY THE
AUSTRALIAN COMMISSION
ON SAFETY AND QUALITY
IN HEALTH CARE
Lead national coordination and promotion of hand hygiene strategies.
Liaise with education and training providers to incorporate key safety
and quality issues such as hand hygiene into educational curricula.
Facilitate reporting of timely and appropriate national hand hygiene data.
Healthcare providers,
consumers, and patients use
effective evidence-based
hand hygiene practices.
05 A U S T R A L I A N S A F E T Y A N D Q U A L I T Y G O A L S F O R H E A L T H C A R E
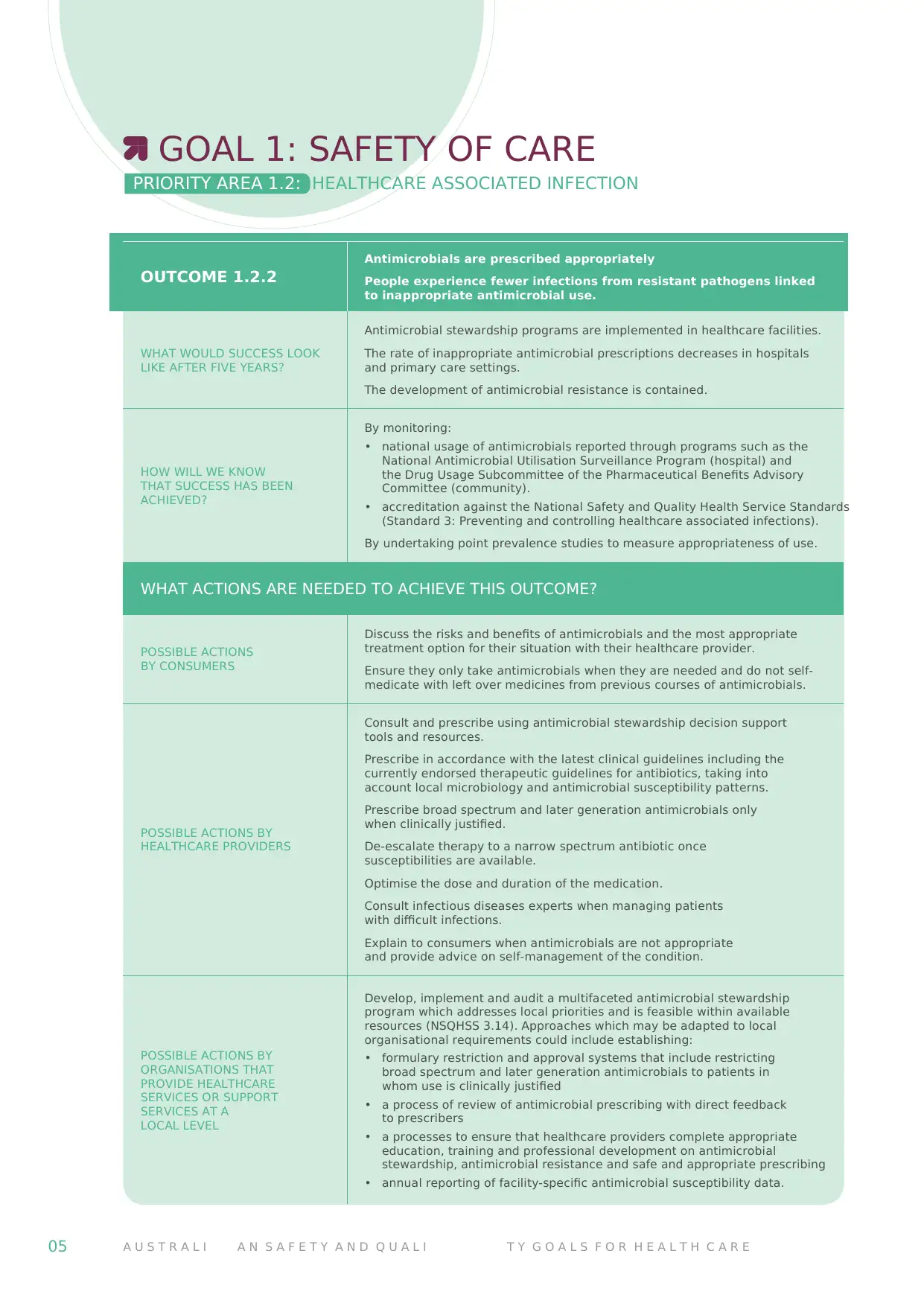
OUTCOME 1.2.2
Antimicrobials are prescribed appropriately
People experience fewer infections from resistant pathogens linked
to inappropriate antimicrobial use.
WHAT WOULD SUCCESS LOOK
LIKE AFTER FIVE YEARS?
Antimicrobial stewardship programs are implemented in healthcare facilities.
The rate of inappropriate antimicrobial prescriptions decreases in hospitals
and primary care settings.
The development of antimicrobial resistance is contained.
HOW WILL WE KNOW
THAT SUCCESS HAS BEEN
ACHIEVED?
By monitoring:
• national usage of antimicrobials reported through programs such as the
National Antimicrobial Utilisation Surveillance Program (hospital) and
the Drug Usage Subcommittee of the Pharmaceutical Benefits Advisory
Committee (community).
• accreditation against the National Safety and Quality Health Service Standards
(Standard 3: Preventing and controlling healthcare associated infections).
By undertaking point prevalence studies to measure appropriateness of use.
WHAT ACTIONS ARE NEEDED TO ACHIEVE THIS OUTCOME?
POSSIBLE ACTIONS
BY CONSUMERS
Discuss the risks and benefits of antimicrobials and the most appropriate
treatment option for their situation with their healthcare provider.
Ensure they only take antimicrobials when they are needed and do not self-
medicate with left over medicines from previous courses of antimicrobials.
POSSIBLE ACTIONS BY
HEALTHCARE PROVIDERS
Consult and prescribe using antimicrobial stewardship decision support
tools and resources.
Prescribe in accordance with the latest clinical guidelines including the
currently endorsed therapeutic guidelines for antibiotics, taking into
account local microbiology and antimicrobial susceptibility patterns.
Prescribe broad spectrum and later generation antimicrobials only
when clinically justified.
De-escalate therapy to a narrow spectrum antibiotic once
susceptibilities are available.
Optimise the dose and duration of the medication.
Consult infectious diseases experts when managing patients
with difficult infections.
Explain to consumers when antimicrobials are not appropriate
and provide advice on self-management of the condition.
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A
LOCAL LEVEL
Develop, implement and audit a multifaceted antimicrobial stewardship
program which addresses local priorities and is feasible within available
resources (NSQHSS 3.14). Approaches which may be adapted to local
organisational requirements could include establishing:
• formulary restriction and approval systems that include restricting
broad spectrum and later generation antimicrobials to patients in
whom use is clinically justified
• a process of review of antimicrobial prescribing with direct feedback
to prescribers
• a processes to ensure that healthcare providers complete appropriate
education, training and professional development on antimicrobial
stewardship, antimicrobial resistance and safe and appropriate prescribing
• annual reporting of facility-specific antimicrobial susceptibility data.
GOAL 1: SAFETY OF CARE
PRIORITY AREA 1.2: HEALTHCARE ASSOCIATED INFECTION
OUTCOME 1.2.2
Antimicrobials are prescribed appropriately
People experience fewer infections from resistant pathogens linked
to inappropriate antimicrobial use.
WHAT WOULD SUCCESS LOOK
LIKE AFTER FIVE YEARS?
Antimicrobial stewardship programs are implemented in healthcare facilities.
The rate of inappropriate antimicrobial prescriptions decreases in hospitals
and primary care settings.
The development of antimicrobial resistance is contained.
HOW WILL WE KNOW
THAT SUCCESS HAS BEEN
ACHIEVED?
By monitoring:
• national usage of antimicrobials reported through programs such as the
National Antimicrobial Utilisation Surveillance Program (hospital) and
the Drug Usage Subcommittee of the Pharmaceutical Benefits Advisory
Committee (community).
• accreditation against the National Safety and Quality Health Service Standards
(Standard 3: Preventing and controlling healthcare associated infections).
By undertaking point prevalence studies to measure appropriateness of use.
WHAT ACTIONS ARE NEEDED TO ACHIEVE THIS OUTCOME?
POSSIBLE ACTIONS
BY CONSUMERS
Discuss the risks and benefits of antimicrobials and the most appropriate
treatment option for their situation with their healthcare provider.
Ensure they only take antimicrobials when they are needed and do not self-
medicate with left over medicines from previous courses of antimicrobials.
POSSIBLE ACTIONS BY
HEALTHCARE PROVIDERS
Consult and prescribe using antimicrobial stewardship decision support
tools and resources.
Prescribe in accordance with the latest clinical guidelines including the
currently endorsed therapeutic guidelines for antibiotics, taking into
account local microbiology and antimicrobial susceptibility patterns.
Prescribe broad spectrum and later generation antimicrobials only
when clinically justified.
De-escalate therapy to a narrow spectrum antibiotic once
susceptibilities are available.
Optimise the dose and duration of the medication.
Consult infectious diseases experts when managing patients
with difficult infections.
Explain to consumers when antimicrobials are not appropriate
and provide advice on self-management of the condition.
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A
LOCAL LEVEL
Develop, implement and audit a multifaceted antimicrobial stewardship
program which addresses local priorities and is feasible within available
resources (NSQHSS 3.14). Approaches which may be adapted to local
organisational requirements could include establishing:
• formulary restriction and approval systems that include restricting
broad spectrum and later generation antimicrobials to patients in
whom use is clinically justified
• a process of review of antimicrobial prescribing with direct feedback
to prescribers
• a processes to ensure that healthcare providers complete appropriate
education, training and professional development on antimicrobial
stewardship, antimicrobial resistance and safe and appropriate prescribing
• annual reporting of facility-specific antimicrobial susceptibility data.
GOAL 1: SAFETY OF CARE
PRIORITY AREA 1.2: HEALTHCARE ASSOCIATED INFECTION
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
A C T I O N G U I D E I H E A L T H C A R E A S S O C I A T E D I N F E C T I O N 06
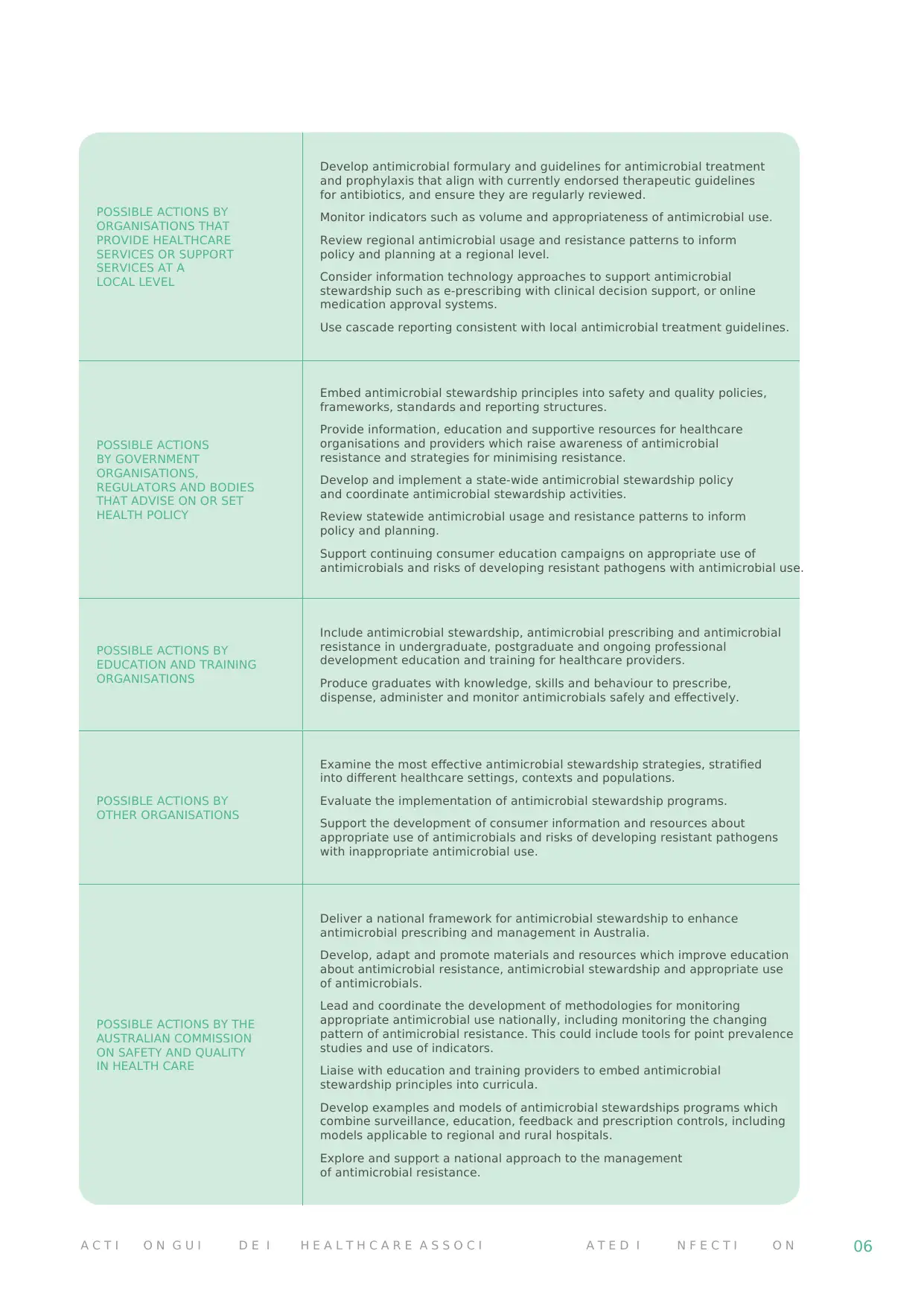
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A
LOCAL LEVEL
Develop antimicrobial formulary and guidelines for antimicrobial treatment
and prophylaxis that align with currently endorsed therapeutic guidelines
for antibiotics, and ensure they are regularly reviewed.
Monitor indicators such as volume and appropriateness of antimicrobial use.
Review regional antimicrobial usage and resistance patterns to inform
policy and planning at a regional level.
Consider information technology approaches to support antimicrobial
stewardship such as e-prescribing with clinical decision support, or online
medication approval systems.
Use cascade reporting consistent with local antimicrobial treatment guidelines.
POSSIBLE ACTIONS
BY GOVERNMENT
ORGANISATIONS,
REGULATORS AND BODIES
THAT ADVISE ON OR SET
HEALTH POLICY
Embed antimicrobial stewardship principles into safety and quality policies,
frameworks, standards and reporting structures.
Provide information, education and supportive resources for healthcare
organisations and providers which raise awareness of antimicrobial
resistance and strategies for minimising resistance.
Develop and implement a state-wide antimicrobial stewardship policy
and coordinate antimicrobial stewardship activities.
Review statewide antimicrobial usage and resistance patterns to inform
policy and planning.
Support continuing consumer education campaigns on appropriate use of
antimicrobials and risks of developing resistant pathogens with antimicrobial use.
POSSIBLE ACTIONS BY
EDUCATION AND TRAINING
ORGANISATIONS
Include antimicrobial stewardship, antimicrobial prescribing and antimicrobial
resistance in undergraduate, postgraduate and ongoing professional
development education and training for healthcare providers.
Produce graduates with knowledge, skills and behaviour to prescribe,
dispense, administer and monitor antimicrobials safely and effectively.
POSSIBLE ACTIONS BY
OTHER ORGANISATIONS
Examine the most effective antimicrobial stewardship strategies, stratified
into different healthcare settings, contexts and populations.
Evaluate the implementation of antimicrobial stewardship programs.
Support the development of consumer information and resources about
appropriate use of antimicrobials and risks of developing resistant pathogens
with inappropriate antimicrobial use.
POSSIBLE ACTIONS BY THE
AUSTRALIAN COMMISSION
ON SAFETY AND QUALITY
IN HEALTH CARE
Deliver a national framework for antimicrobial stewardship to enhance
antimicrobial prescribing and management in Australia.
Develop, adapt and promote materials and resources which improve education
about antimicrobial resistance, antimicrobial stewardship and appropriate use
of antimicrobials.
Lead and coordinate the development of methodologies for monitoring
appropriate antimicrobial use nationally, including monitoring the changing
pattern of antimicrobial resistance. This could include tools for point prevalence
studies and use of indicators.
Liaise with education and training providers to embed antimicrobial
stewardship principles into curricula.
Develop examples and models of antimicrobial stewardships programs which
combine surveillance, education, feedback and prescription controls, including
models applicable to regional and rural hospitals.
Explore and support a national approach to the management
of antimicrobial resistance.
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A
LOCAL LEVEL
Develop antimicrobial formulary and guidelines for antimicrobial treatment
and prophylaxis that align with currently endorsed therapeutic guidelines
for antibiotics, and ensure they are regularly reviewed.
Monitor indicators such as volume and appropriateness of antimicrobial use.
Review regional antimicrobial usage and resistance patterns to inform
policy and planning at a regional level.
Consider information technology approaches to support antimicrobial
stewardship such as e-prescribing with clinical decision support, or online
medication approval systems.
Use cascade reporting consistent with local antimicrobial treatment guidelines.
POSSIBLE ACTIONS
BY GOVERNMENT
ORGANISATIONS,
REGULATORS AND BODIES
THAT ADVISE ON OR SET
HEALTH POLICY
Embed antimicrobial stewardship principles into safety and quality policies,
frameworks, standards and reporting structures.
Provide information, education and supportive resources for healthcare
organisations and providers which raise awareness of antimicrobial
resistance and strategies for minimising resistance.
Develop and implement a state-wide antimicrobial stewardship policy
and coordinate antimicrobial stewardship activities.
Review statewide antimicrobial usage and resistance patterns to inform
policy and planning.
Support continuing consumer education campaigns on appropriate use of
antimicrobials and risks of developing resistant pathogens with antimicrobial use.
POSSIBLE ACTIONS BY
EDUCATION AND TRAINING
ORGANISATIONS
Include antimicrobial stewardship, antimicrobial prescribing and antimicrobial
resistance in undergraduate, postgraduate and ongoing professional
development education and training for healthcare providers.
Produce graduates with knowledge, skills and behaviour to prescribe,
dispense, administer and monitor antimicrobials safely and effectively.
POSSIBLE ACTIONS BY
OTHER ORGANISATIONS
Examine the most effective antimicrobial stewardship strategies, stratified
into different healthcare settings, contexts and populations.
Evaluate the implementation of antimicrobial stewardship programs.
Support the development of consumer information and resources about
appropriate use of antimicrobials and risks of developing resistant pathogens
with inappropriate antimicrobial use.
POSSIBLE ACTIONS BY THE
AUSTRALIAN COMMISSION
ON SAFETY AND QUALITY
IN HEALTH CARE
Deliver a national framework for antimicrobial stewardship to enhance
antimicrobial prescribing and management in Australia.
Develop, adapt and promote materials and resources which improve education
about antimicrobial resistance, antimicrobial stewardship and appropriate use
of antimicrobials.
Lead and coordinate the development of methodologies for monitoring
appropriate antimicrobial use nationally, including monitoring the changing
pattern of antimicrobial resistance. This could include tools for point prevalence
studies and use of indicators.
Liaise with education and training providers to embed antimicrobial
stewardship principles into curricula.
Develop examples and models of antimicrobial stewardships programs which
combine surveillance, education, feedback and prescription controls, including
models applicable to regional and rural hospitals.
Explore and support a national approach to the management
of antimicrobial resistance.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
07 A U S T R A L I A N S A F E T Y A N D Q U A L I T Y G O A L S F O R H E A L T H C A R E
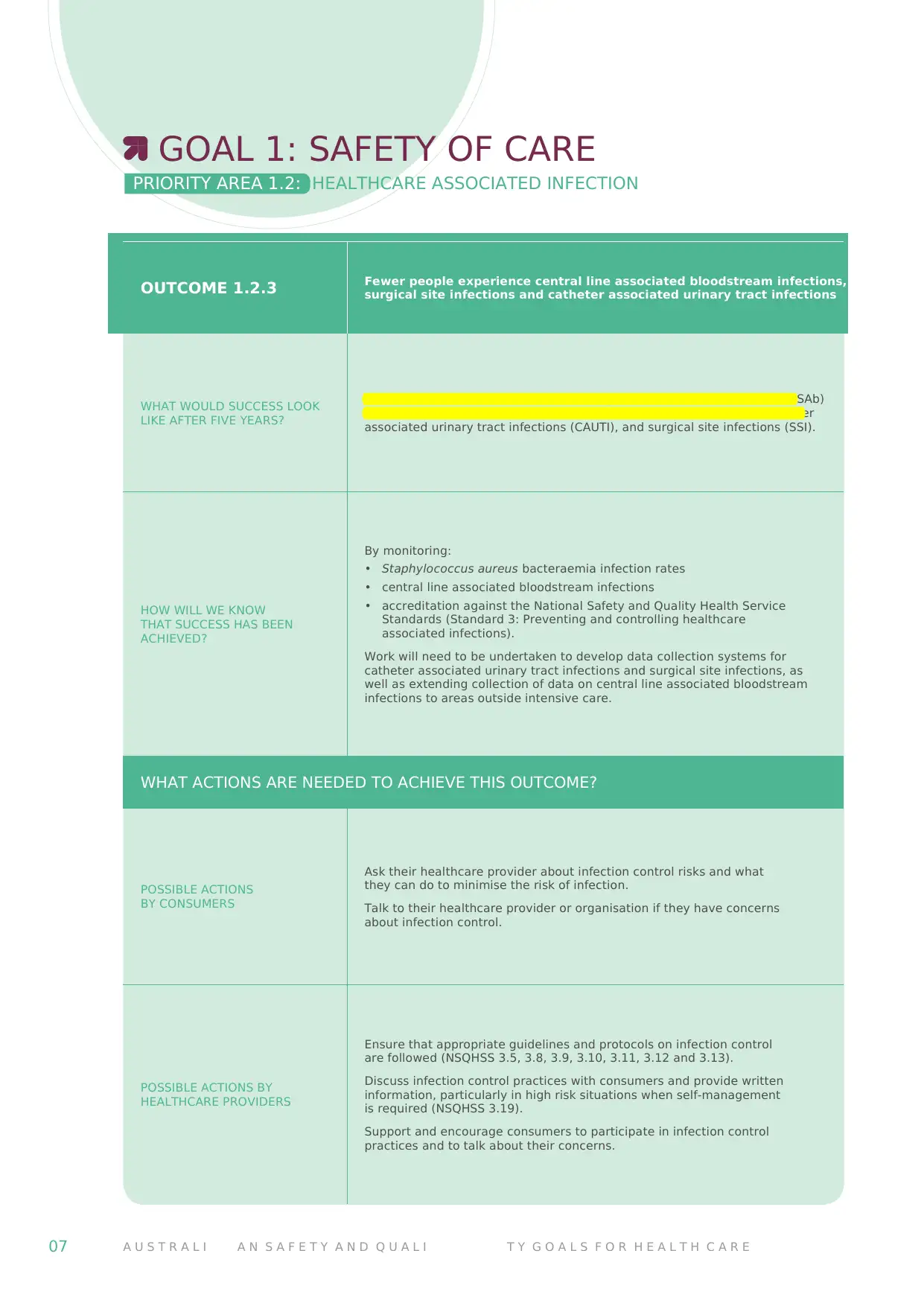
OUTCOME 1.2.3 Fewer people experience central line associated bloodstream infections,
surgical site infections and catheter associated urinary tract infections
WHAT WOULD SUCCESS LOOK
LIKE AFTER FIVE YEARS?
There is a measurable reduction in Staphylococcus aureus bacteraemia (SAb)
infections, central line associated bloodstream infections (CLABSI), catheter
associated urinary tract infections (CAUTI), and surgical site infections (SSI).
HOW WILL WE KNOW
THAT SUCCESS HAS BEEN
ACHIEVED?
By monitoring:
• Staphylococcus aureus bacteraemia infection rates
• central line associated bloodstream infections
• accreditation against the National Safety and Quality Health Service
Standards (Standard 3: Preventing and controlling healthcare
associated infections).
Work will need to be undertaken to develop data collection systems for
catheter associated urinary tract infections and surgical site infections, as
well as extending collection of data on central line associated bloodstream
infections to areas outside intensive care.
WHAT ACTIONS ARE NEEDED TO ACHIEVE THIS OUTCOME?
POSSIBLE ACTIONS
BY CONSUMERS
Ask their healthcare provider about infection control risks and what
they can do to minimise the risk of infection.
Talk to their healthcare provider or organisation if they have concerns
about infection control.
POSSIBLE ACTIONS BY
HEALTHCARE PROVIDERS
Ensure that appropriate guidelines and protocols on infection control
are followed (NSQHSS 3.5, 3.8, 3.9, 3.10, 3.11, 3.12 and 3.13).
Discuss infection control practices with consumers and provide written
information, particularly in high risk situations when self-management
is required (NSQHSS 3.19).
Support and encourage consumers to participate in infection control
practices and to talk about their concerns.
GOAL 1: SAFETY OF CARE
PRIORITY AREA 1.2: HEALTHCARE ASSOCIATED INFECTION
OUTCOME 1.2.3 Fewer people experience central line associated bloodstream infections,
surgical site infections and catheter associated urinary tract infections
WHAT WOULD SUCCESS LOOK
LIKE AFTER FIVE YEARS?
There is a measurable reduction in Staphylococcus aureus bacteraemia (SAb)
infections, central line associated bloodstream infections (CLABSI), catheter
associated urinary tract infections (CAUTI), and surgical site infections (SSI).
HOW WILL WE KNOW
THAT SUCCESS HAS BEEN
ACHIEVED?
By monitoring:
• Staphylococcus aureus bacteraemia infection rates
• central line associated bloodstream infections
• accreditation against the National Safety and Quality Health Service
Standards (Standard 3: Preventing and controlling healthcare
associated infections).
Work will need to be undertaken to develop data collection systems for
catheter associated urinary tract infections and surgical site infections, as
well as extending collection of data on central line associated bloodstream
infections to areas outside intensive care.
WHAT ACTIONS ARE NEEDED TO ACHIEVE THIS OUTCOME?
POSSIBLE ACTIONS
BY CONSUMERS
Ask their healthcare provider about infection control risks and what
they can do to minimise the risk of infection.
Talk to their healthcare provider or organisation if they have concerns
about infection control.
POSSIBLE ACTIONS BY
HEALTHCARE PROVIDERS
Ensure that appropriate guidelines and protocols on infection control
are followed (NSQHSS 3.5, 3.8, 3.9, 3.10, 3.11, 3.12 and 3.13).
Discuss infection control practices with consumers and provide written
information, particularly in high risk situations when self-management
is required (NSQHSS 3.19).
Support and encourage consumers to participate in infection control
practices and to talk about their concerns.
GOAL 1: SAFETY OF CARE
PRIORITY AREA 1.2: HEALTHCARE ASSOCIATED INFECTION
A C T I O N G U I D E I H E A L T H C A R E A S S O C I A T E D I N F E C T I O N 08
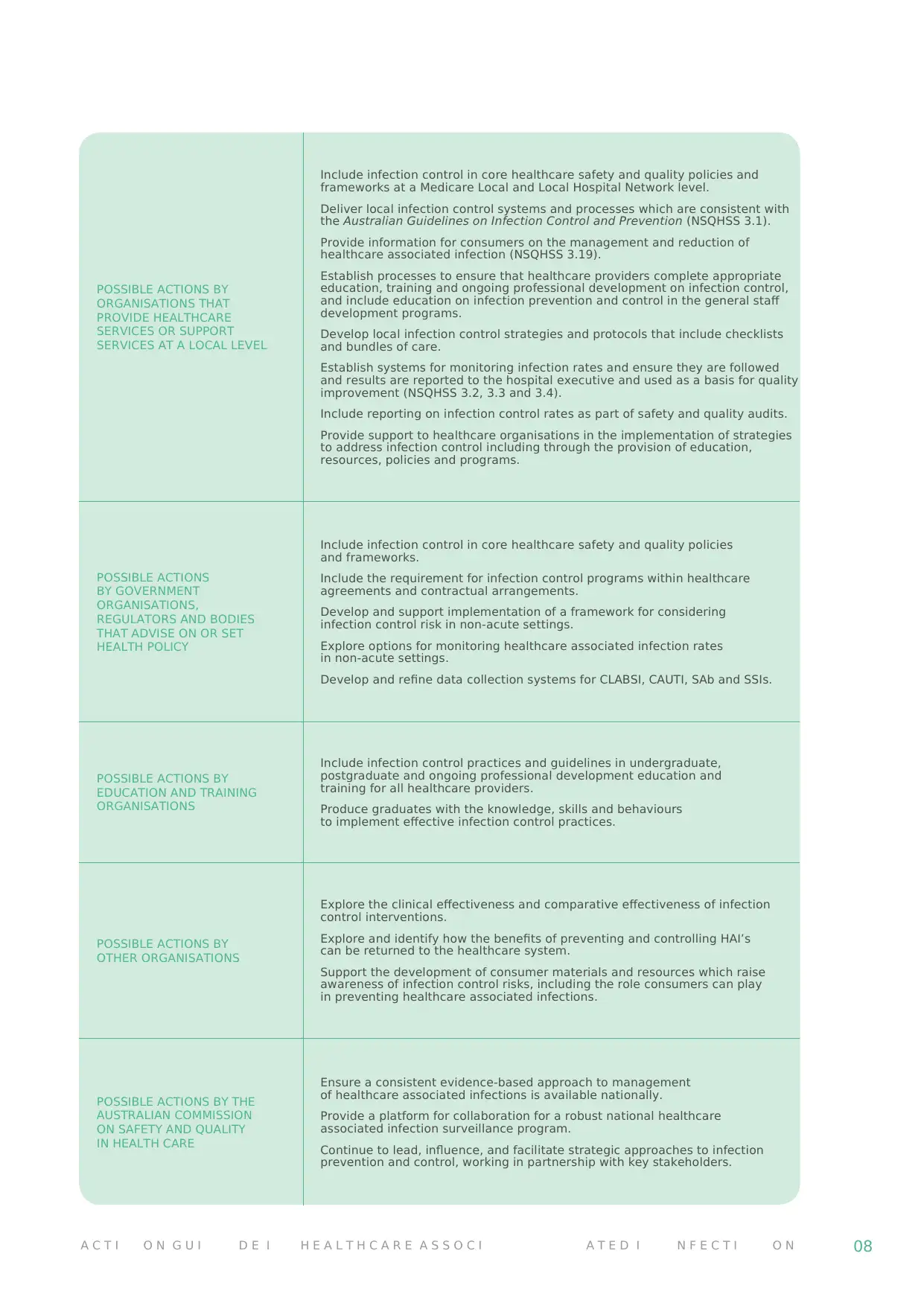
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A LOCAL LEVEL
Include infection control in core healthcare safety and quality policies and
frameworks at a Medicare Local and Local Hospital Network level.
Deliver local infection control systems and processes which are consistent with
the Australian Guidelines on Infection Control and Prevention (NSQHSS 3.1).
Provide information for consumers on the management and reduction of
healthcare associated infection (NSQHSS 3.19).
Establish processes to ensure that healthcare providers complete appropriate
education, training and ongoing professional development on infection control,
and include education on infection prevention and control in the general staff
development programs.
Develop local infection control strategies and protocols that include checklists
and bundles of care.
Establish systems for monitoring infection rates and ensure they are followed
and results are reported to the hospital executive and used as a basis for quality
improvement (NSQHSS 3.2, 3.3 and 3.4).
Include reporting on infection control rates as part of safety and quality audits.
Provide support to healthcare organisations in the implementation of strategies
to address infection control including through the provision of education,
resources, policies and programs.
POSSIBLE ACTIONS
BY GOVERNMENT
ORGANISATIONS,
REGULATORS AND BODIES
THAT ADVISE ON OR SET
HEALTH POLICY
Include infection control in core healthcare safety and quality policies
and frameworks.
Include the requirement for infection control programs within healthcare
agreements and contractual arrangements.
Develop and support implementation of a framework for considering
infection control risk in non-acute settings.
Explore options for monitoring healthcare associated infection rates
in non-acute settings.
Develop and refine data collection systems for CLABSI, CAUTI, SAb and SSIs.
POSSIBLE ACTIONS BY
EDUCATION AND TRAINING
ORGANISATIONS
Include infection control practices and guidelines in undergraduate,
postgraduate and ongoing professional development education and
training for all healthcare providers.
Produce graduates with the knowledge, skills and behaviours
to implement effective infection control practices.
POSSIBLE ACTIONS BY
OTHER ORGANISATIONS
Explore the clinical effectiveness and comparative effectiveness of infection
control interventions.
Explore and identify how the benefits of preventing and controlling HAI’s
can be returned to the healthcare system.
Support the development of consumer materials and resources which raise
awareness of infection control risks, including the role consumers can play
in preventing healthcare associated infections.
POSSIBLE ACTIONS BY THE
AUSTRALIAN COMMISSION
ON SAFETY AND QUALITY
IN HEALTH CARE
Ensure a consistent evidence-based approach to management
of healthcare associated infections is available nationally.
Provide a platform for collaboration for a robust national healthcare
associated infection surveillance program.
Continue to lead, influence, and facilitate strategic approaches to infection
prevention and control, working in partnership with key stakeholders.
POSSIBLE ACTIONS BY
ORGANISATIONS THAT
PROVIDE HEALTHCARE
SERVICES OR SUPPORT
SERVICES AT A LOCAL LEVEL
Include infection control in core healthcare safety and quality policies and
frameworks at a Medicare Local and Local Hospital Network level.
Deliver local infection control systems and processes which are consistent with
the Australian Guidelines on Infection Control and Prevention (NSQHSS 3.1).
Provide information for consumers on the management and reduction of
healthcare associated infection (NSQHSS 3.19).
Establish processes to ensure that healthcare providers complete appropriate
education, training and ongoing professional development on infection control,
and include education on infection prevention and control in the general staff
development programs.
Develop local infection control strategies and protocols that include checklists
and bundles of care.
Establish systems for monitoring infection rates and ensure they are followed
and results are reported to the hospital executive and used as a basis for quality
improvement (NSQHSS 3.2, 3.3 and 3.4).
Include reporting on infection control rates as part of safety and quality audits.
Provide support to healthcare organisations in the implementation of strategies
to address infection control including through the provision of education,
resources, policies and programs.
POSSIBLE ACTIONS
BY GOVERNMENT
ORGANISATIONS,
REGULATORS AND BODIES
THAT ADVISE ON OR SET
HEALTH POLICY
Include infection control in core healthcare safety and quality policies
and frameworks.
Include the requirement for infection control programs within healthcare
agreements and contractual arrangements.
Develop and support implementation of a framework for considering
infection control risk in non-acute settings.
Explore options for monitoring healthcare associated infection rates
in non-acute settings.
Develop and refine data collection systems for CLABSI, CAUTI, SAb and SSIs.
POSSIBLE ACTIONS BY
EDUCATION AND TRAINING
ORGANISATIONS
Include infection control practices and guidelines in undergraduate,
postgraduate and ongoing professional development education and
training for all healthcare providers.
Produce graduates with the knowledge, skills and behaviours
to implement effective infection control practices.
POSSIBLE ACTIONS BY
OTHER ORGANISATIONS
Explore the clinical effectiveness and comparative effectiveness of infection
control interventions.
Explore and identify how the benefits of preventing and controlling HAI’s
can be returned to the healthcare system.
Support the development of consumer materials and resources which raise
awareness of infection control risks, including the role consumers can play
in preventing healthcare associated infections.
POSSIBLE ACTIONS BY THE
AUSTRALIAN COMMISSION
ON SAFETY AND QUALITY
IN HEALTH CARE
Ensure a consistent evidence-based approach to management
of healthcare associated infections is available nationally.
Provide a platform for collaboration for a robust national healthcare
associated infection surveillance program.
Continue to lead, influence, and facilitate strategic approaches to infection
prevention and control, working in partnership with key stakeholders.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

09 A U S T R A L I A N S A F E T Y A N D Q U A L I T Y G O A L S F O R H E A L T H C A R E
APPENDIX: DEFINITIONS
Antibiotic:
A substance that kills or inhibits the growth of bacteria.
Antimicrobial:
A chemical substance that inhibits or destroys bacteria,
viruses and fungi, including yeasts or moulds.
Antimicrobial stewardship:
A program implemented in a health care organisation
to reduce the risks associated with increasing microbial
resistance and to extend the effectiveness of antimicrobial
treatments. Antimicrobial stewardship may incorporate
a broad range of strategies including the monitoring and
reviews of antimicrobial use.
Consumers:
When referring to consumers the Commission is referring
to patients, consumers, families, carers and other
support people.
Five moments for hand hygiene:
A hand hygiene initiative from the World Health
Organisation that defines the key moments for
hand hygiene.
Hand hygiene:
A general term referring to any action of hand cleansing.
Healthcare associated infections:
Infections that are acquired in healthcare facilities
(nosocomial infections) or that occur as a result of
healthcare interventions (iatrogenic infections). Healthcare
associated infections may manifest after people leave the
healthcare facility.
Infection control:
Actions to prevent the spread of pathogens between
people in a healthcare setting. Examples of infection
control measures include targeted healthcare associated
infection surveillance, infectious disease monitoring, hand
hygiene and personal protective equipment.
APPENDIX: DEFINITIONS
Antibiotic:
A substance that kills or inhibits the growth of bacteria.
Antimicrobial:
A chemical substance that inhibits or destroys bacteria,
viruses and fungi, including yeasts or moulds.
Antimicrobial stewardship:
A program implemented in a health care organisation
to reduce the risks associated with increasing microbial
resistance and to extend the effectiveness of antimicrobial
treatments. Antimicrobial stewardship may incorporate
a broad range of strategies including the monitoring and
reviews of antimicrobial use.
Consumers:
When referring to consumers the Commission is referring
to patients, consumers, families, carers and other
support people.
Five moments for hand hygiene:
A hand hygiene initiative from the World Health
Organisation that defines the key moments for
hand hygiene.
Hand hygiene:
A general term referring to any action of hand cleansing.
Healthcare associated infections:
Infections that are acquired in healthcare facilities
(nosocomial infections) or that occur as a result of
healthcare interventions (iatrogenic infections). Healthcare
associated infections may manifest after people leave the
healthcare facility.
Infection control:
Actions to prevent the spread of pathogens between
people in a healthcare setting. Examples of infection
control measures include targeted healthcare associated
infection surveillance, infectious disease monitoring, hand
hygiene and personal protective equipment.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
A C T I O N G U I D E I H E A L T H C A R E A S S O C I A T E D I N F E C T I O N 10
Healthcare associated
infections are one of the most
common, significant and
preventable patient safety
issues today.
Healthcare associated
infections are one of the most
common, significant and
preventable patient safety
issues today.

AUSTRALIAN COMMISSION ON SAFETY
AND QUALITY IN HEALTH CARE
Level 7, 1 Oxford St. Darlinghurst NSW 2010
Telephone: 02 9126 3600
Email: mail@safetyandquality.gov.au
www.safetyandquality.gov.au
AND QUALITY IN HEALTH CARE
Level 7, 1 Oxford St. Darlinghurst NSW 2010
Telephone: 02 9126 3600
Email: mail@safetyandquality.gov.au
www.safetyandquality.gov.au
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





