Huddersfield Uni: SMP4002 Applied Therapeutics Case Review
VerifiedAdded on 2022/08/26
|11
|4569
|21
Case Study
AI Summary
This case review focuses on Mrs. AP, a 60-year-old woman admitted with a complex medical history including hypertension, type 2 diabetes, diabetic neuropathy, and GORD, complicated by loss of appetite, abdominal pain, and falls. The assignment details the patient's presentation, including medication-related UTI, poor diabetes control, and adherence issues. It outlines the management plan, encompassing a diabetes team review, antibiotic treatment for pyelonephritis, and cognitive assessments. The case study includes detailed patient information, test results, a problem list addressing medical and pharmaceutical issues, progress notes documenting the patient's response to treatment, and SOAP analyses for both Pylonephritis and management of poor DM control. The document covers drug therapy, adherence issues, and the interventions implemented, such as insulin regimen adjustments and dietary advice. The patient's progress is monitored, and the case highlights the challenges in managing multiple comorbidities and ensuring effective patient care, with recommendations for post-discharge care and medication management. The document also follows the standard clerking proforma of Huddersfield University Hospital NHS Trust.
SMP4002 : Applied Therapeutics
Case Review 2019-20
Student name: Student number: Case Number:
Case summary:
Mrs AP, a 60-years old woman presenting a medical history of hypertension, diabetes type 2, diabetic neuropathy
and GORD diseases, admitted with loss of appetite, abdominal pain and falls at home. Initial investigation showed
falls, medication-related UTI/ Renal infection (pyelonephritis), poor DM control and adherence issues.
The management plan imposed include Diabetes team review for glucose control, repeated blood, IV antibiotics 48
hours followed by a review and finally MMSE +/- Capacity review.
Patient Details and Assessment:
Patient
Initials
A.P Age 60 Date of
admission
22.7 Sex F
Weight 71KG Height 1.62
metres BMI Above
30kg/m2 Ward 05
Drug Allergies NKDA
Impairments (e.g.
visual, hearing,
mobility)
Nil
Presenting Complaint Loss of appetite, abdominal pain Falls at home
History of Presenting
Complaint In general terms, the patient has been unwell for a period of one week. The
patient has also lost appetite and not been eating food due to the occurrence of
stomach cramps. Fall is also a fundamental problem, especially when the patient
went up to make use of a bathroom. On the same note, the patient is cognitively
impaired, whereby she fails to recall banging head or LOC. As per the
information from the patient, no changes have occurred in the bowel habit.
Neither does the patient experience symptoms of vomiting, nausea or presence of
blood in the stool. However, self-care and learning difficulties are one of the
fundamental and primary symptoms illustrates throughout the diagnostic process.
Past Medical History I. Hypertension
II. Diabetes- type 2
III. Diabetic neuropathy
IV. Urinary frequency
1
Case Review 2019-20
Student name: Student number: Case Number:
Case summary:
Mrs AP, a 60-years old woman presenting a medical history of hypertension, diabetes type 2, diabetic neuropathy
and GORD diseases, admitted with loss of appetite, abdominal pain and falls at home. Initial investigation showed
falls, medication-related UTI/ Renal infection (pyelonephritis), poor DM control and adherence issues.
The management plan imposed include Diabetes team review for glucose control, repeated blood, IV antibiotics 48
hours followed by a review and finally MMSE +/- Capacity review.
Patient Details and Assessment:
Patient
Initials
A.P Age 60 Date of
admission
22.7 Sex F
Weight 71KG Height 1.62
metres BMI Above
30kg/m2 Ward 05
Drug Allergies NKDA
Impairments (e.g.
visual, hearing,
mobility)
Nil
Presenting Complaint Loss of appetite, abdominal pain Falls at home
History of Presenting
Complaint In general terms, the patient has been unwell for a period of one week. The
patient has also lost appetite and not been eating food due to the occurrence of
stomach cramps. Fall is also a fundamental problem, especially when the patient
went up to make use of a bathroom. On the same note, the patient is cognitively
impaired, whereby she fails to recall banging head or LOC. As per the
information from the patient, no changes have occurred in the bowel habit.
Neither does the patient experience symptoms of vomiting, nausea or presence of
blood in the stool. However, self-care and learning difficulties are one of the
fundamental and primary symptoms illustrates throughout the diagnostic process.
Past Medical History I. Hypertension
II. Diabetes- type 2
III. Diabetic neuropathy
IV. Urinary frequency
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
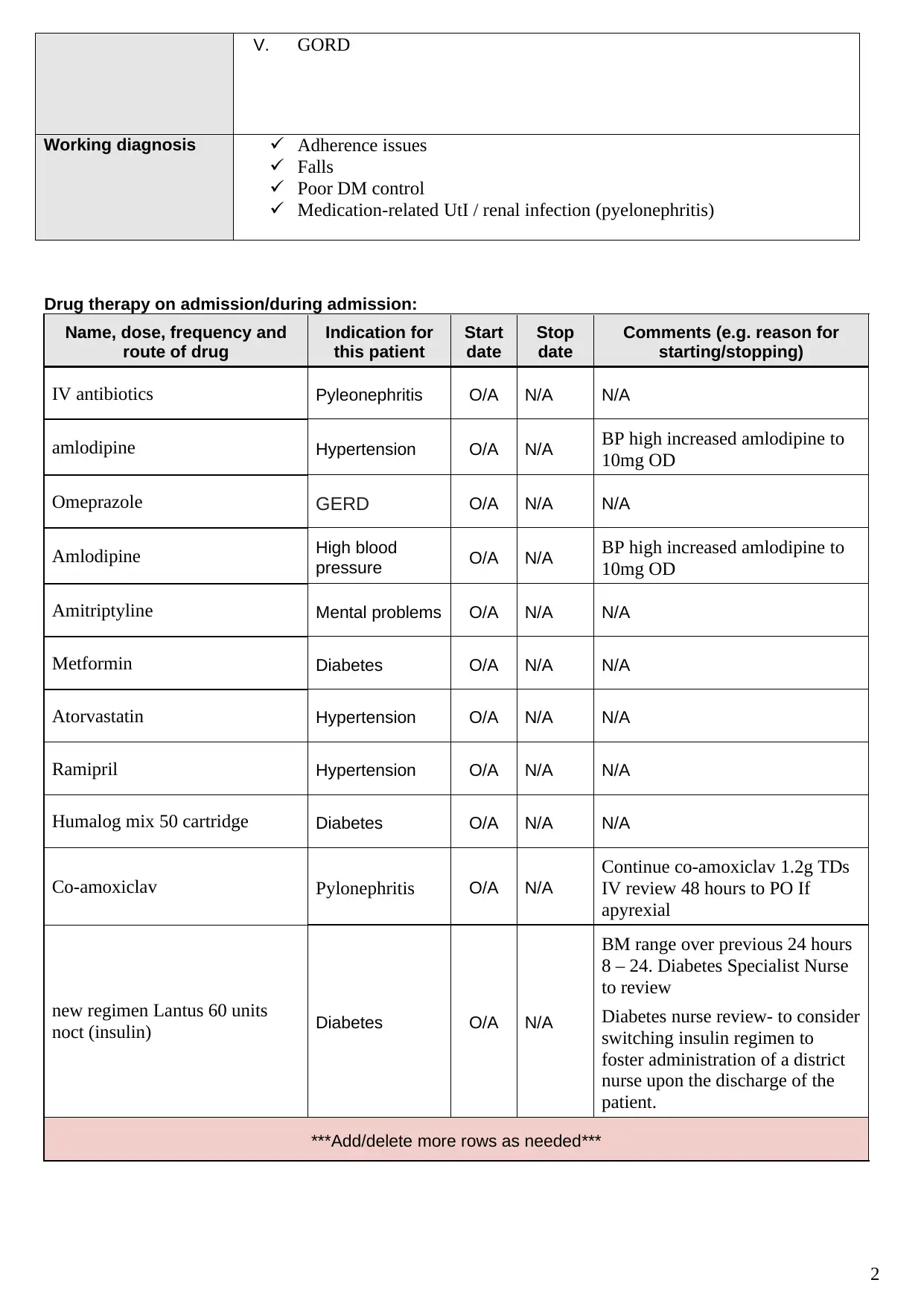
V. GORD
Working diagnosis Adherence issues
Falls
Poor DM control
Medication-related UtI / renal infection (pyelonephritis)
Drug therapy on admission/during admission:
Name, dose, frequency and
route of drug
Indication for
this patient
Start
date
Stop
date
Comments (e.g. reason for
starting/stopping)
IV antibiotics Pyleonephritis O/A N/A N/A
amlodipine Hypertension O/A N/A BP high increased amlodipine to
10mg OD
Omeprazole GERD O/A N/A N/A
Amlodipine High blood
pressure O/A N/A BP high increased amlodipine to
10mg OD
Amitriptyline Mental problems O/A N/A N/A
Metformin Diabetes O/A N/A N/A
Atorvastatin Hypertension O/A N/A N/A
Ramipril Hypertension O/A N/A N/A
Humalog mix 50 cartridge Diabetes O/A N/A N/A
Co-amoxiclav Pylonephritis O/A N/A
Continue co-amoxiclav 1.2g TDs
IV review 48 hours to PO If
apyrexial
new regimen Lantus 60 units
noct (insulin) Diabetes O/A N/A
BM range over previous 24 hours
8 – 24. Diabetes Specialist Nurse
to review
Diabetes nurse review- to consider
switching insulin regimen to
foster administration of a district
nurse upon the discharge of the
patient.
***Add/delete more rows as needed***
2
Working diagnosis Adherence issues
Falls
Poor DM control
Medication-related UtI / renal infection (pyelonephritis)
Drug therapy on admission/during admission:
Name, dose, frequency and
route of drug
Indication for
this patient
Start
date
Stop
date
Comments (e.g. reason for
starting/stopping)
IV antibiotics Pyleonephritis O/A N/A N/A
amlodipine Hypertension O/A N/A BP high increased amlodipine to
10mg OD
Omeprazole GERD O/A N/A N/A
Amlodipine High blood
pressure O/A N/A BP high increased amlodipine to
10mg OD
Amitriptyline Mental problems O/A N/A N/A
Metformin Diabetes O/A N/A N/A
Atorvastatin Hypertension O/A N/A N/A
Ramipril Hypertension O/A N/A N/A
Humalog mix 50 cartridge Diabetes O/A N/A N/A
Co-amoxiclav Pylonephritis O/A N/A
Continue co-amoxiclav 1.2g TDs
IV review 48 hours to PO If
apyrexial
new regimen Lantus 60 units
noct (insulin) Diabetes O/A N/A
BM range over previous 24 hours
8 – 24. Diabetes Specialist Nurse
to review
Diabetes nurse review- to consider
switching insulin regimen to
foster administration of a district
nurse upon the discharge of the
patient.
***Add/delete more rows as needed***
2
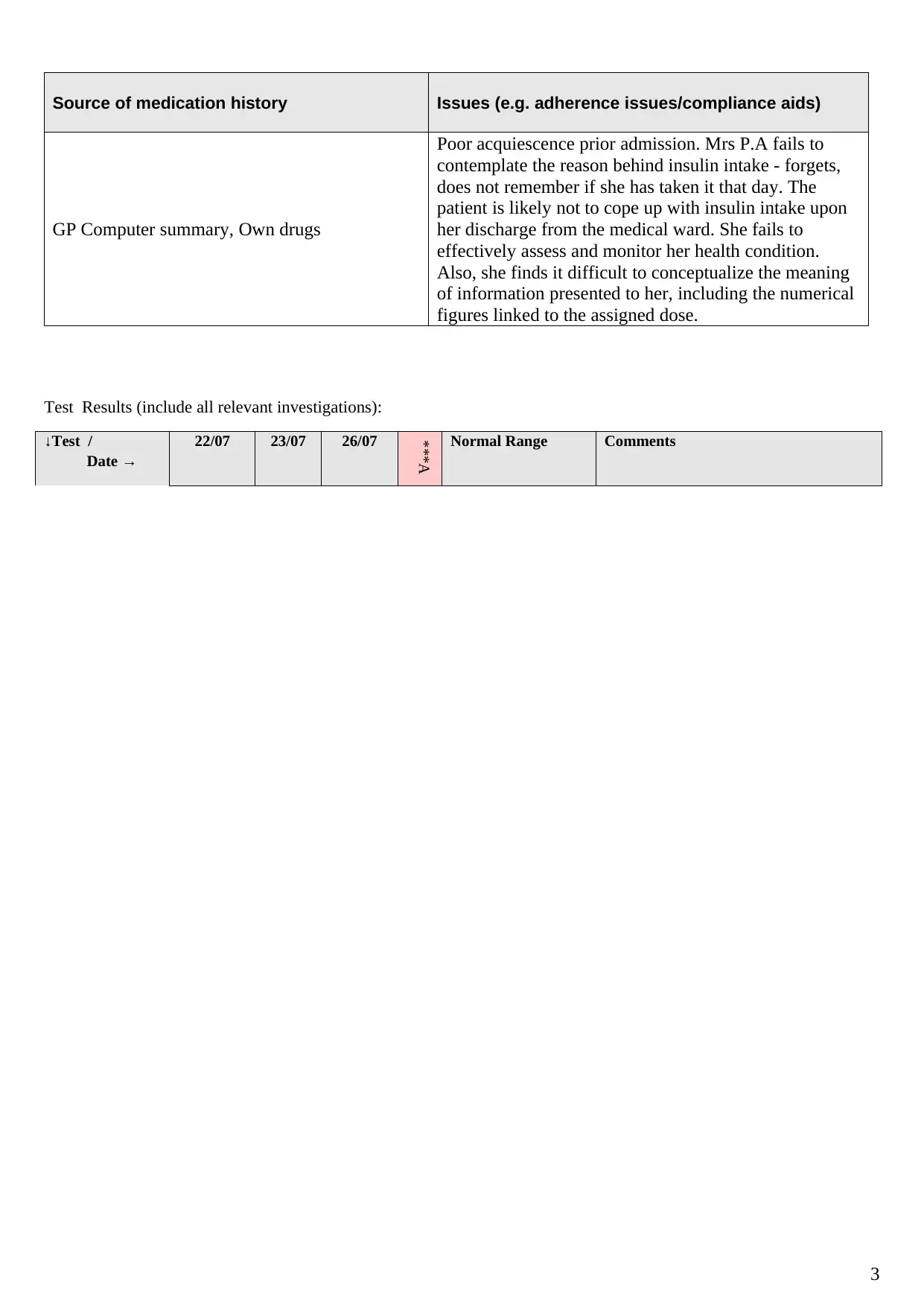
Source of medication history Issues (e.g. adherence issues/compliance aids)
GP Computer summary, Own drugs
Poor acquiescence prior admission. Mrs P.A fails to
contemplate the reason behind insulin intake - forgets,
does not remember if she has taken it that day. The
patient is likely not to cope up with insulin intake upon
her discharge from the medical ward. She fails to
effectively assess and monitor her health condition.
Also, she finds it difficult to conceptualize the meaning
of information presented to her, including the numerical
figures linked to the assigned dose.
Test Results (include all relevant investigations):
↓Test /
Date →
22/07 23/07 26/07
***A
Normal Range Comments
3
GP Computer summary, Own drugs
Poor acquiescence prior admission. Mrs P.A fails to
contemplate the reason behind insulin intake - forgets,
does not remember if she has taken it that day. The
patient is likely not to cope up with insulin intake upon
her discharge from the medical ward. She fails to
effectively assess and monitor her health condition.
Also, she finds it difficult to conceptualize the meaning
of information presented to her, including the numerical
figures linked to the assigned dose.
Test Results (include all relevant investigations):
↓Test /
Date →
22/07 23/07 26/07
***A
Normal Range Comments
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
dd/delete more column as needed***
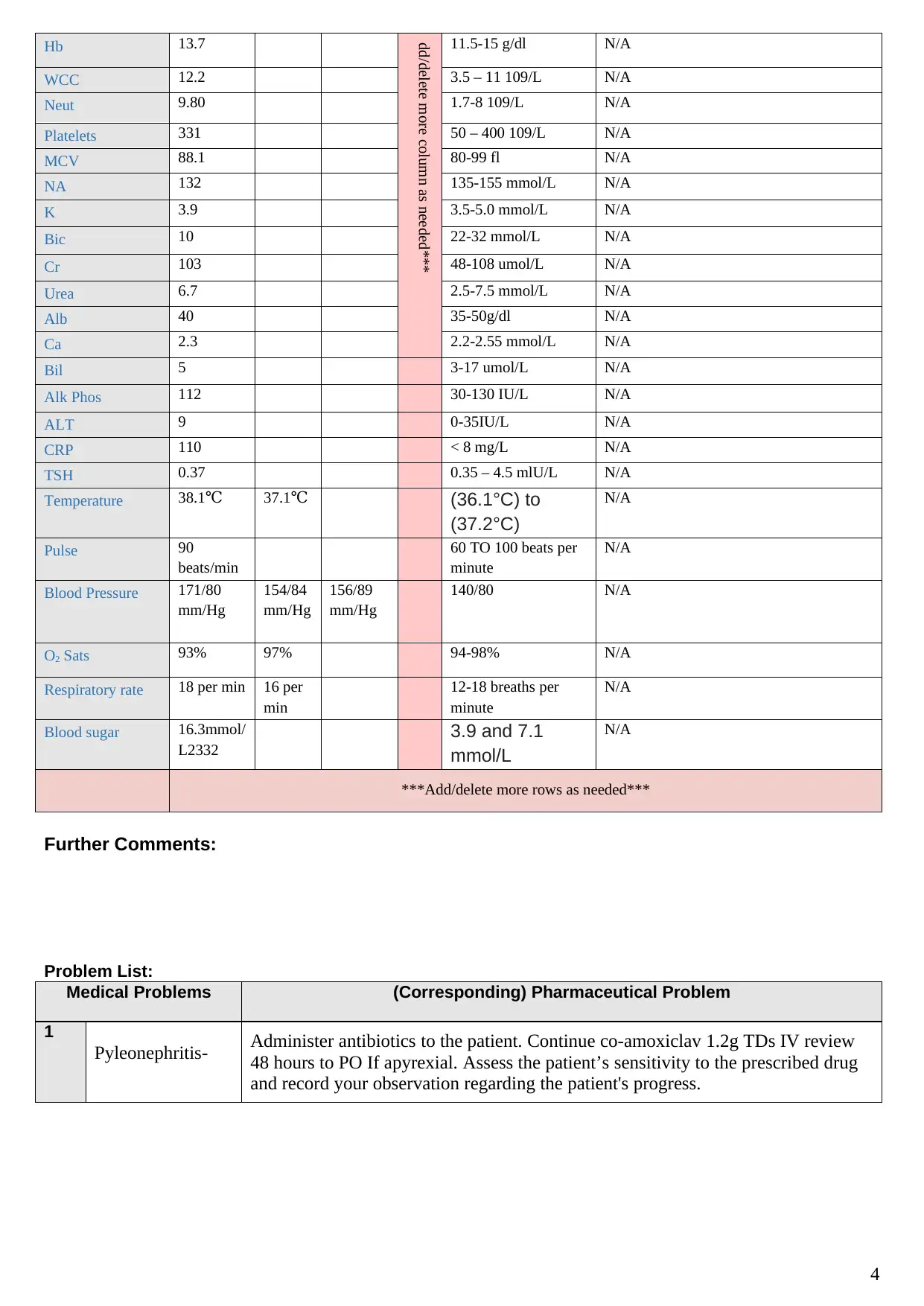
Hb 13.7 11.5-15 g/dl N/A
WCC 12.2 3.5 – 11 109/L N/A
Neut 9.80 1.7-8 109/L N/A
Platelets 331 50 – 400 109/L N/A
MCV 88.1 80-99 fl N/A
NA 132 135-155 mmol/L N/A
K 3.9 3.5-5.0 mmol/L N/A
Bic 10 22-32 mmol/L N/A
Cr 103 48-108 umol/L N/A
Urea 6.7 2.5-7.5 mmol/L N/A
Alb 40 35-50g/dl N/A
Ca 2.3 2.2-2.55 mmol/L N/A
Bil 5 3-17 umol/L N/A
Alk Phos 112 30-130 IU/L N/A
ALT 9 0-35IU/L N/A
CRP 110 < 8 mg/L N/A
TSH 0.37 0.35 – 4.5 mlU/L N/A
Temperature 38.1℃ 37.1℃ (36.1°C) to
(37.2°C)
N/A
Pulse 90
beats/min
60 TO 100 beats per
minute
N/A
Blood Pressure 171/80
mm/Hg
154/84
mm/Hg
156/89
mm/Hg
140/80 N/A
O2 Sats 93% 97% 94-98% N/A
Respiratory rate 18 per min 16 per
min
12-18 breaths per
minute
N/A
Blood sugar 16.3mmol/
L2332
3.9 and 7.1
mmol/L
N/A
***Add/delete more rows as needed***
Further Comments:
Problem List:
Medical Problems (Corresponding) Pharmaceutical Problem
1
Pyleonephritis- Administer antibiotics to the patient. Continue co-amoxiclav 1.2g TDs IV review
48 hours to PO If apyrexial. Assess the patient’s sensitivity to the prescribed drug
and record your observation regarding the patient's progress.
4
Hb 13.7 11.5-15 g/dl N/A
WCC 12.2 3.5 – 11 109/L N/A
Neut 9.80 1.7-8 109/L N/A
Platelets 331 50 – 400 109/L N/A
MCV 88.1 80-99 fl N/A
NA 132 135-155 mmol/L N/A
K 3.9 3.5-5.0 mmol/L N/A
Bic 10 22-32 mmol/L N/A
Cr 103 48-108 umol/L N/A
Urea 6.7 2.5-7.5 mmol/L N/A
Alb 40 35-50g/dl N/A
Ca 2.3 2.2-2.55 mmol/L N/A
Bil 5 3-17 umol/L N/A
Alk Phos 112 30-130 IU/L N/A
ALT 9 0-35IU/L N/A
CRP 110 < 8 mg/L N/A
TSH 0.37 0.35 – 4.5 mlU/L N/A
Temperature 38.1℃ 37.1℃ (36.1°C) to
(37.2°C)
N/A
Pulse 90
beats/min
60 TO 100 beats per
minute
N/A
Blood Pressure 171/80
mm/Hg
154/84
mm/Hg
156/89
mm/Hg
140/80 N/A
O2 Sats 93% 97% 94-98% N/A
Respiratory rate 18 per min 16 per
min
12-18 breaths per
minute
N/A
Blood sugar 16.3mmol/
L2332
3.9 and 7.1
mmol/L
N/A
***Add/delete more rows as needed***
Further Comments:
Problem List:
Medical Problems (Corresponding) Pharmaceutical Problem
1
Pyleonephritis- Administer antibiotics to the patient. Continue co-amoxiclav 1.2g TDs IV review
48 hours to PO If apyrexial. Assess the patient’s sensitivity to the prescribed drug
and record your observation regarding the patient's progress.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
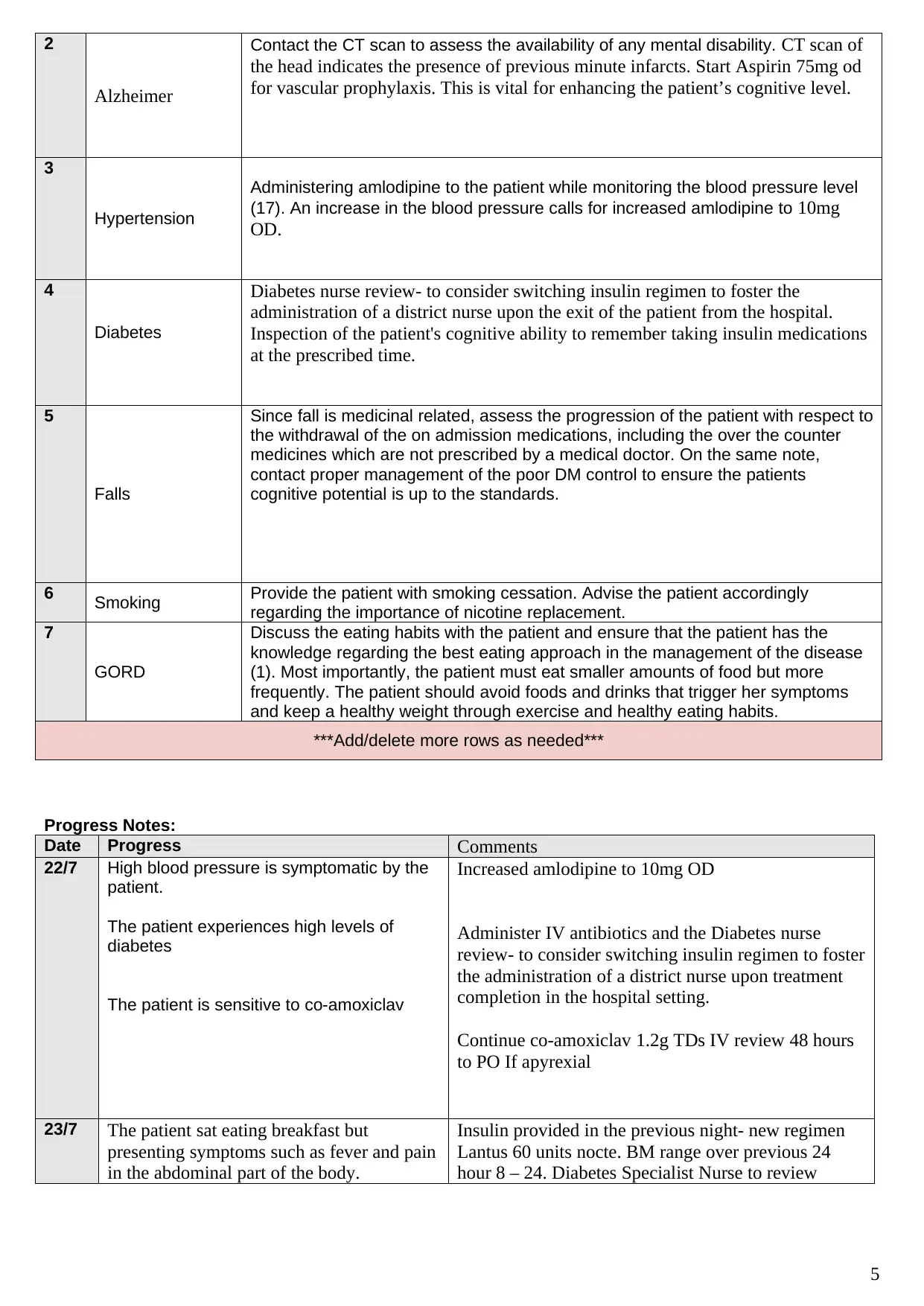
2
Alzheimer
Contact the CT scan to assess the availability of any mental disability. CT scan of
the head indicates the presence of previous minute infarcts. Start Aspirin 75mg od
for vascular prophylaxis. This is vital for enhancing the patient’s cognitive level.
3
Hypertension
Administering amlodipine to the patient while monitoring the blood pressure level
(17). An increase in the blood pressure calls for increased amlodipine to 10mg
OD.
4
Diabetes
Diabetes nurse review- to consider switching insulin regimen to foster the
administration of a district nurse upon the exit of the patient from the hospital.
Inspection of the patient's cognitive ability to remember taking insulin medications
at the prescribed time.
5
Falls
Since fall is medicinal related, assess the progression of the patient with respect to
the withdrawal of the on admission medications, including the over the counter
medicines which are not prescribed by a medical doctor. On the same note,
contact proper management of the poor DM control to ensure the patients
cognitive potential is up to the standards.
6 Smoking Provide the patient with smoking cessation. Advise the patient accordingly
regarding the importance of nicotine replacement.
7
GORD
Discuss the eating habits with the patient and ensure that the patient has the
knowledge regarding the best eating approach in the management of the disease
(1). Most importantly, the patient must eat smaller amounts of food but more
frequently. The patient should avoid foods and drinks that trigger her symptoms
and keep a healthy weight through exercise and healthy eating habits.
***Add/delete more rows as needed***
Progress Notes:
Date Progress Comments
22/7 High blood pressure is symptomatic by the
patient.
The patient experiences high levels of
diabetes
The patient is sensitive to co-amoxiclav
Increased amlodipine to 10mg OD
Administer IV antibiotics and the Diabetes nurse
review- to consider switching insulin regimen to foster
the administration of a district nurse upon treatment
completion in the hospital setting.
Continue co-amoxiclav 1.2g TDs IV review 48 hours
to PO If apyrexial
23/7 The patient sat eating breakfast but
presenting symptoms such as fever and pain
in the abdominal part of the body.
Insulin provided in the previous night- new regimen
Lantus 60 units nocte. BM range over previous 24
hour 8 – 24. Diabetes Specialist Nurse to review
5
Alzheimer
Contact the CT scan to assess the availability of any mental disability. CT scan of
the head indicates the presence of previous minute infarcts. Start Aspirin 75mg od
for vascular prophylaxis. This is vital for enhancing the patient’s cognitive level.
3
Hypertension
Administering amlodipine to the patient while monitoring the blood pressure level
(17). An increase in the blood pressure calls for increased amlodipine to 10mg
OD.
4
Diabetes
Diabetes nurse review- to consider switching insulin regimen to foster the
administration of a district nurse upon the exit of the patient from the hospital.
Inspection of the patient's cognitive ability to remember taking insulin medications
at the prescribed time.
5
Falls
Since fall is medicinal related, assess the progression of the patient with respect to
the withdrawal of the on admission medications, including the over the counter
medicines which are not prescribed by a medical doctor. On the same note,
contact proper management of the poor DM control to ensure the patients
cognitive potential is up to the standards.
6 Smoking Provide the patient with smoking cessation. Advise the patient accordingly
regarding the importance of nicotine replacement.
7
GORD
Discuss the eating habits with the patient and ensure that the patient has the
knowledge regarding the best eating approach in the management of the disease
(1). Most importantly, the patient must eat smaller amounts of food but more
frequently. The patient should avoid foods and drinks that trigger her symptoms
and keep a healthy weight through exercise and healthy eating habits.
***Add/delete more rows as needed***
Progress Notes:
Date Progress Comments
22/7 High blood pressure is symptomatic by the
patient.
The patient experiences high levels of
diabetes
The patient is sensitive to co-amoxiclav
Increased amlodipine to 10mg OD
Administer IV antibiotics and the Diabetes nurse
review- to consider switching insulin regimen to foster
the administration of a district nurse upon treatment
completion in the hospital setting.
Continue co-amoxiclav 1.2g TDs IV review 48 hours
to PO If apyrexial
23/7 The patient sat eating breakfast but
presenting symptoms such as fever and pain
in the abdominal part of the body.
Insulin provided in the previous night- new regimen
Lantus 60 units nocte. BM range over previous 24
hour 8 – 24. Diabetes Specialist Nurse to review
5
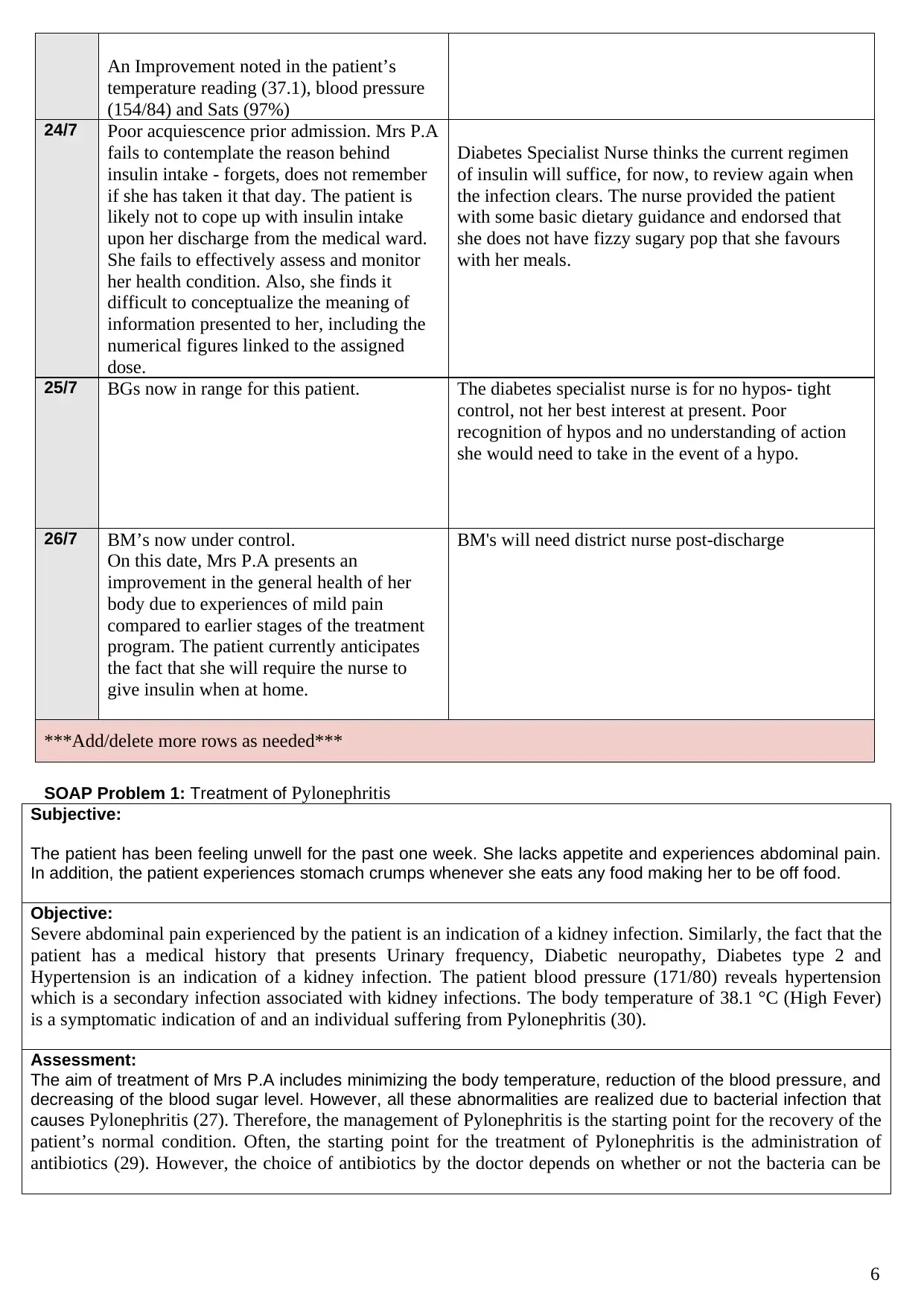
An Improvement noted in the patient’s
temperature reading (37.1), blood pressure
(154/84) and Sats (97%)
24/7 Poor acquiescence prior admission. Mrs P.A
fails to contemplate the reason behind
insulin intake - forgets, does not remember
if she has taken it that day. The patient is
likely not to cope up with insulin intake
upon her discharge from the medical ward.
She fails to effectively assess and monitor
her health condition. Also, she finds it
difficult to conceptualize the meaning of
information presented to her, including the
numerical figures linked to the assigned
dose.
Diabetes Specialist Nurse thinks the current regimen
of insulin will suffice, for now, to review again when
the infection clears. The nurse provided the patient
with some basic dietary guidance and endorsed that
she does not have fizzy sugary pop that she favours
with her meals.
25/7 BGs now in range for this patient. The diabetes specialist nurse is for no hypos- tight
control, not her best interest at present. Poor
recognition of hypos and no understanding of action
she would need to take in the event of a hypo.
26/7 BM’s now under control.
On this date, Mrs P.A presents an
improvement in the general health of her
body due to experiences of mild pain
compared to earlier stages of the treatment
program. The patient currently anticipates
the fact that she will require the nurse to
give insulin when at home.
BM's will need district nurse post-discharge
***Add/delete more rows as needed***
SOAP Problem 1: Treatment of Pylonephritis
Subjective:
The patient has been feeling unwell for the past one week. She lacks appetite and experiences abdominal pain.
In addition, the patient experiences stomach crumps whenever she eats any food making her to be off food.
Objective:
Severe abdominal pain experienced by the patient is an indication of a kidney infection. Similarly, the fact that the
patient has a medical history that presents Urinary frequency, Diabetic neuropathy, Diabetes type 2 and
Hypertension is an indication of a kidney infection. The patient blood pressure (171/80) reveals hypertension
which is a secondary infection associated with kidney infections. The body temperature of 38.1 °C (High Fever)
is a symptomatic indication of and an individual suffering from Pylonephritis (30).
Assessment:
The aim of treatment of Mrs P.A includes minimizing the body temperature, reduction of the blood pressure, and
decreasing of the blood sugar level. However, all these abnormalities are realized due to bacterial infection that
causes Pylonephritis (27). Therefore, the management of Pylonephritis is the starting point for the recovery of the
patient’s normal condition. Often, the starting point for the treatment of Pylonephritis is the administration of
antibiotics (29). However, the choice of antibiotics by the doctor depends on whether or not the bacteria can be
6
temperature reading (37.1), blood pressure
(154/84) and Sats (97%)
24/7 Poor acquiescence prior admission. Mrs P.A
fails to contemplate the reason behind
insulin intake - forgets, does not remember
if she has taken it that day. The patient is
likely not to cope up with insulin intake
upon her discharge from the medical ward.
She fails to effectively assess and monitor
her health condition. Also, she finds it
difficult to conceptualize the meaning of
information presented to her, including the
numerical figures linked to the assigned
dose.
Diabetes Specialist Nurse thinks the current regimen
of insulin will suffice, for now, to review again when
the infection clears. The nurse provided the patient
with some basic dietary guidance and endorsed that
she does not have fizzy sugary pop that she favours
with her meals.
25/7 BGs now in range for this patient. The diabetes specialist nurse is for no hypos- tight
control, not her best interest at present. Poor
recognition of hypos and no understanding of action
she would need to take in the event of a hypo.
26/7 BM’s now under control.
On this date, Mrs P.A presents an
improvement in the general health of her
body due to experiences of mild pain
compared to earlier stages of the treatment
program. The patient currently anticipates
the fact that she will require the nurse to
give insulin when at home.
BM's will need district nurse post-discharge
***Add/delete more rows as needed***
SOAP Problem 1: Treatment of Pylonephritis
Subjective:
The patient has been feeling unwell for the past one week. She lacks appetite and experiences abdominal pain.
In addition, the patient experiences stomach crumps whenever she eats any food making her to be off food.
Objective:
Severe abdominal pain experienced by the patient is an indication of a kidney infection. Similarly, the fact that the
patient has a medical history that presents Urinary frequency, Diabetic neuropathy, Diabetes type 2 and
Hypertension is an indication of a kidney infection. The patient blood pressure (171/80) reveals hypertension
which is a secondary infection associated with kidney infections. The body temperature of 38.1 °C (High Fever)
is a symptomatic indication of and an individual suffering from Pylonephritis (30).
Assessment:
The aim of treatment of Mrs P.A includes minimizing the body temperature, reduction of the blood pressure, and
decreasing of the blood sugar level. However, all these abnormalities are realized due to bacterial infection that
causes Pylonephritis (27). Therefore, the management of Pylonephritis is the starting point for the recovery of the
patient’s normal condition. Often, the starting point for the treatment of Pylonephritis is the administration of
antibiotics (29). However, the choice of antibiotics by the doctor depends on whether or not the bacteria can be
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
identified. If it is impossible to identify the bacteria, it is advisable to make use of a broad spectrum of antibiotics.
Antibiotics are expected to sure the condition in a period of two to three days (31). However, it is essential to
proceed and complete the prescribed dose provided by the doctor. Often, the period prescribed is 10 to 14 days
(28). At times when drug therapy fails to work, hospital admission remains the only option like in the case of Mrs
P.A. The length of stay in the hospital depends on the severity of the patient's conditions. At times, the condition
may worsen to an extent that calls for surgery.
Intravenous Antibiotics
Intravenous antibiotics are the ones recommended for patients who fail to respond to oral admission of
antibiotics like in the case of Mrs P.A (26). The antibiotics are used alongside with DVT prophylaxis that aids in
the management of hypertension (22, 24). Aspirin alone is not recommended for DVT prophylaxis (23, 25).
Amlodipine is also used to reduce hypertension. Amlodipine serves a significant role in minimizing blood
pressure hence reducing the potential for kidney problems and heart attacks (18). Amlodipine should not be
employed in the treatment of attacks of chest pains when they occur. However, it is also essential in the
management of certain types of chest pains (19). The dosage of the medicine depends solely on the severity of
the patient’s condition. However, it must be used regularly in order to get the best out of it. The side effects
include dizziness and light-headedness (20). Therefore it is significant for the patient to wake up slowly while
rising from lying or sitting. Failure to do so increases the likelihood of falls like in the case of Mrs P.A.
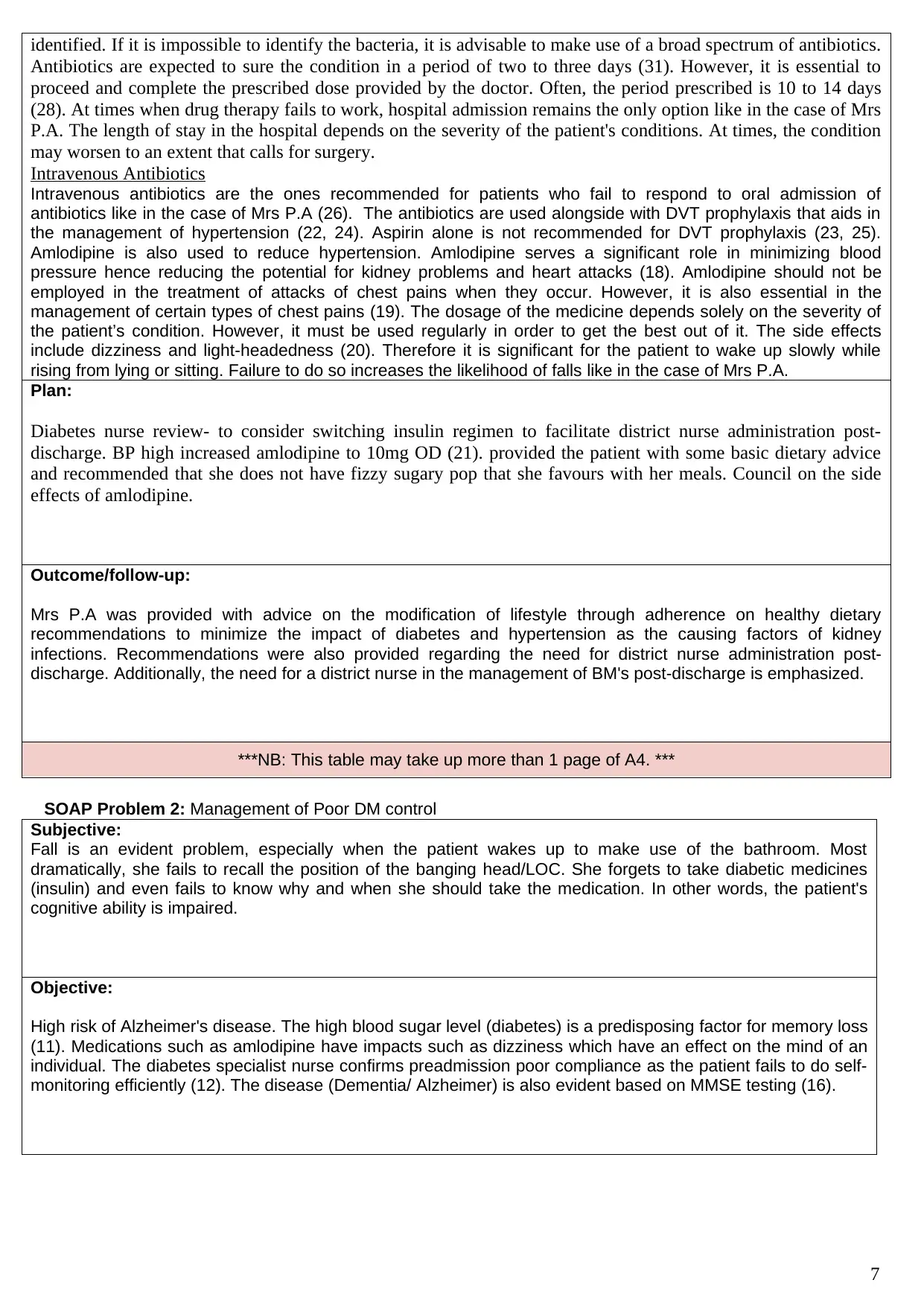
Plan:
Diabetes nurse review- to consider switching insulin regimen to facilitate district nurse administration post-
discharge. BP high increased amlodipine to 10mg OD (21). provided the patient with some basic dietary advice
and recommended that she does not have fizzy sugary pop that she favours with her meals. Council on the side
effects of amlodipine.
Outcome/follow-up:
Mrs P.A was provided with advice on the modification of lifestyle through adherence on healthy dietary
recommendations to minimize the impact of diabetes and hypertension as the causing factors of kidney
infections. Recommendations were also provided regarding the need for district nurse administration post-
discharge. Additionally, the need for a district nurse in the management of BM's post-discharge is emphasized.
***NB: This table may take up more than 1 page of A4. ***
SOAP Problem 2: Management of Poor DM control
Subjective:
Fall is an evident problem, especially when the patient wakes up to make use of the bathroom. Most
dramatically, she fails to recall the position of the banging head/LOC. She forgets to take diabetic medicines
(insulin) and even fails to know why and when she should take the medication. In other words, the patient's
cognitive ability is impaired.
Objective:
High risk of Alzheimer's disease. The high blood sugar level (diabetes) is a predisposing factor for memory loss
(11). Medications such as amlodipine have impacts such as dizziness which have an effect on the mind of an
individual. The diabetes specialist nurse confirms preadmission poor compliance as the patient fails to do self-
monitoring efficiently (12). The disease (Dementia/ Alzheimer) is also evident based on MMSE testing (16).
7
Antibiotics are expected to sure the condition in a period of two to three days (31). However, it is essential to
proceed and complete the prescribed dose provided by the doctor. Often, the period prescribed is 10 to 14 days
(28). At times when drug therapy fails to work, hospital admission remains the only option like in the case of Mrs
P.A. The length of stay in the hospital depends on the severity of the patient's conditions. At times, the condition
may worsen to an extent that calls for surgery.
Intravenous Antibiotics
Intravenous antibiotics are the ones recommended for patients who fail to respond to oral admission of
antibiotics like in the case of Mrs P.A (26). The antibiotics are used alongside with DVT prophylaxis that aids in
the management of hypertension (22, 24). Aspirin alone is not recommended for DVT prophylaxis (23, 25).
Amlodipine is also used to reduce hypertension. Amlodipine serves a significant role in minimizing blood
pressure hence reducing the potential for kidney problems and heart attacks (18). Amlodipine should not be
employed in the treatment of attacks of chest pains when they occur. However, it is also essential in the
management of certain types of chest pains (19). The dosage of the medicine depends solely on the severity of
the patient’s condition. However, it must be used regularly in order to get the best out of it. The side effects
include dizziness and light-headedness (20). Therefore it is significant for the patient to wake up slowly while
rising from lying or sitting. Failure to do so increases the likelihood of falls like in the case of Mrs P.A.
Plan:
Diabetes nurse review- to consider switching insulin regimen to facilitate district nurse administration post-
discharge. BP high increased amlodipine to 10mg OD (21). provided the patient with some basic dietary advice
and recommended that she does not have fizzy sugary pop that she favours with her meals. Council on the side
effects of amlodipine.
Outcome/follow-up:
Mrs P.A was provided with advice on the modification of lifestyle through adherence on healthy dietary
recommendations to minimize the impact of diabetes and hypertension as the causing factors of kidney
infections. Recommendations were also provided regarding the need for district nurse administration post-
discharge. Additionally, the need for a district nurse in the management of BM's post-discharge is emphasized.
***NB: This table may take up more than 1 page of A4. ***
SOAP Problem 2: Management of Poor DM control
Subjective:
Fall is an evident problem, especially when the patient wakes up to make use of the bathroom. Most
dramatically, she fails to recall the position of the banging head/LOC. She forgets to take diabetic medicines
(insulin) and even fails to know why and when she should take the medication. In other words, the patient's
cognitive ability is impaired.
Objective:
High risk of Alzheimer's disease. The high blood sugar level (diabetes) is a predisposing factor for memory loss
(11). Medications such as amlodipine have impacts such as dizziness which have an effect on the mind of an
individual. The diabetes specialist nurse confirms preadmission poor compliance as the patient fails to do self-
monitoring efficiently (12). The disease (Dementia/ Alzheimer) is also evident based on MMSE testing (16).
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Assessment:
Even though Alzheimer’s disease is not a preventable disorder, several lifestyle changes are recommended to
minimize the associated risk factors of the condition (13). Evidence reveals that the changes in exercise, diet
and habits serve a significant role in minimizing risks of Alzheimer disease (15). Some of the recommended
lifestyle changes include regular exercises, eating of healthy oils and meals that contain low saturated fats,
eating fresh produce diet, adherence to the treatment guidelines that are prescribed in the management of
hypertension, diabetes and cholesterol and quitting of smoking. All these recommendations have a great
correlation with Mrs P.A’s condition (10). Therefore, only medications that aid in quitting smoking can be
provided in the management of the condition.
Nicotine Replacement Therapy
Nicotine replacement therapy has a significant role in minimizing smoking because they contain varying
amounts of nicotine (6). Even though some of this products does not require a prescription from a doctor, it is
important to consult a doctor in order to acknowledge when to take the medication, when to stop and the
associated side effects (7).
Some of the medications include nicotine nasal spray, Bupropion, varenicline, and the nicotine patch. Each of
the medications has its own side effects, advantages and disadvantages (8). Thus, it is fundamental to consult
a doctor in order to create awareness of the best product to use in order to quit smoking.
Plan:
The patient is provided with some basic dietary guidance and endorsed that she does not have fizzy sugary pop
that she favours with her meals (14). patient with some basic dietary advice and recommended that she does not
have fizzy sugary pop that she favours with her meals (9).
Outcome/follow-up:
A district nurse is recommended for post-discharge management of BM.
***NB: This table may take up more than 1 page of A4 ***
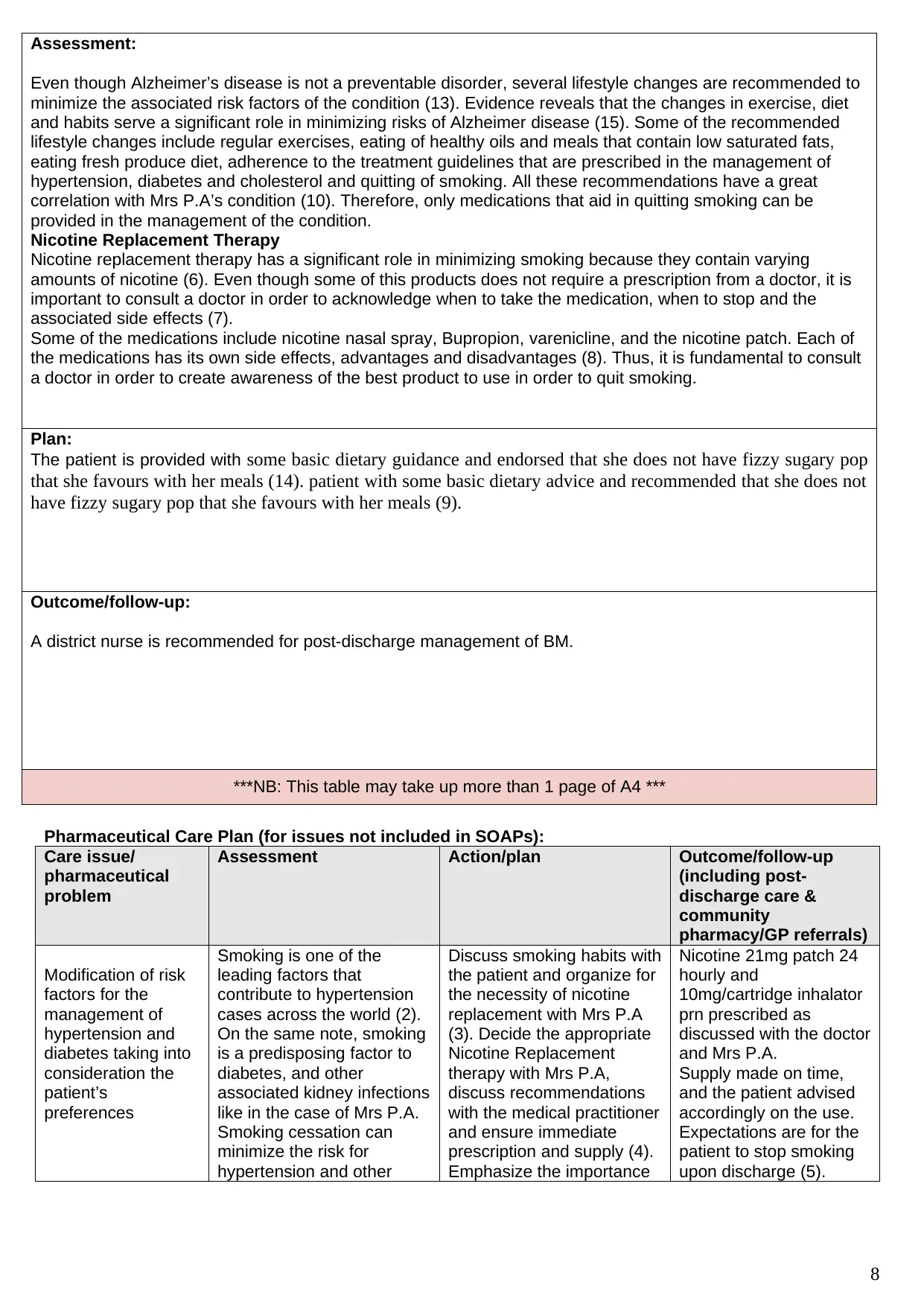
Pharmaceutical Care Plan (for issues not included in SOAPs):
Care issue/
pharmaceutical
problem
Assessment Action/plan Outcome/follow-up
(including post-
discharge care &
community
pharmacy/GP referrals)
Modification of risk
factors for the
management of
hypertension and
diabetes taking into
consideration the
patient’s
preferences
Smoking is one of the
leading factors that
contribute to hypertension
cases across the world (2).
On the same note, smoking
is a predisposing factor to
diabetes, and other
associated kidney infections
like in the case of Mrs P.A.
Smoking cessation can
minimize the risk for
hypertension and other
Discuss smoking habits with
the patient and organize for
the necessity of nicotine
replacement with Mrs P.A
(3). Decide the appropriate
Nicotine Replacement
therapy with Mrs P.A,
discuss recommendations
with the medical practitioner
and ensure immediate
prescription and supply (4).
Emphasize the importance
Nicotine 21mg patch 24
hourly and
10mg/cartridge inhalator
prn prescribed as
discussed with the doctor
and Mrs P.A.
Supply made on time,
and the patient advised
accordingly on the use.
Expectations are for the
patient to stop smoking
upon discharge (5).
8
Even though Alzheimer’s disease is not a preventable disorder, several lifestyle changes are recommended to
minimize the associated risk factors of the condition (13). Evidence reveals that the changes in exercise, diet
and habits serve a significant role in minimizing risks of Alzheimer disease (15). Some of the recommended
lifestyle changes include regular exercises, eating of healthy oils and meals that contain low saturated fats,
eating fresh produce diet, adherence to the treatment guidelines that are prescribed in the management of
hypertension, diabetes and cholesterol and quitting of smoking. All these recommendations have a great
correlation with Mrs P.A’s condition (10). Therefore, only medications that aid in quitting smoking can be
provided in the management of the condition.
Nicotine Replacement Therapy
Nicotine replacement therapy has a significant role in minimizing smoking because they contain varying
amounts of nicotine (6). Even though some of this products does not require a prescription from a doctor, it is
important to consult a doctor in order to acknowledge when to take the medication, when to stop and the
associated side effects (7).
Some of the medications include nicotine nasal spray, Bupropion, varenicline, and the nicotine patch. Each of
the medications has its own side effects, advantages and disadvantages (8). Thus, it is fundamental to consult
a doctor in order to create awareness of the best product to use in order to quit smoking.
Plan:
The patient is provided with some basic dietary guidance and endorsed that she does not have fizzy sugary pop
that she favours with her meals (14). patient with some basic dietary advice and recommended that she does not
have fizzy sugary pop that she favours with her meals (9).
Outcome/follow-up:
A district nurse is recommended for post-discharge management of BM.
***NB: This table may take up more than 1 page of A4 ***
Pharmaceutical Care Plan (for issues not included in SOAPs):
Care issue/
pharmaceutical
problem
Assessment Action/plan Outcome/follow-up
(including post-
discharge care &
community
pharmacy/GP referrals)
Modification of risk
factors for the
management of
hypertension and
diabetes taking into
consideration the
patient’s
preferences
Smoking is one of the
leading factors that
contribute to hypertension
cases across the world (2).
On the same note, smoking
is a predisposing factor to
diabetes, and other
associated kidney infections
like in the case of Mrs P.A.
Smoking cessation can
minimize the risk for
hypertension and other
Discuss smoking habits with
the patient and organize for
the necessity of nicotine
replacement with Mrs P.A
(3). Decide the appropriate
Nicotine Replacement
therapy with Mrs P.A,
discuss recommendations
with the medical practitioner
and ensure immediate
prescription and supply (4).
Emphasize the importance
Nicotine 21mg patch 24
hourly and
10mg/cartridge inhalator
prn prescribed as
discussed with the doctor
and Mrs P.A.
Supply made on time,
and the patient advised
accordingly on the use.
Expectations are for the
patient to stop smoking
upon discharge (5).
8
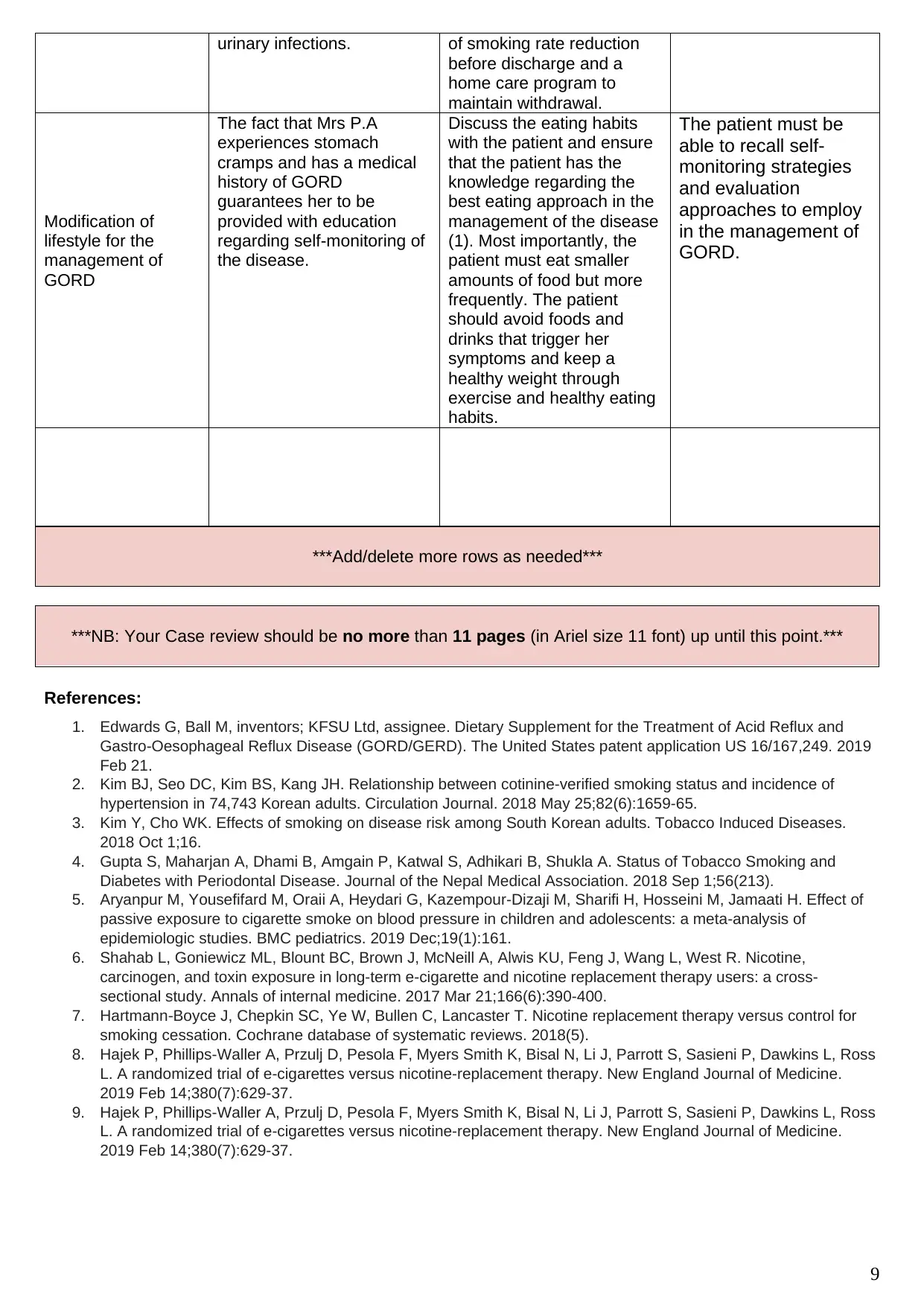
urinary infections. of smoking rate reduction
before discharge and a
home care program to
maintain withdrawal.
Modification of
lifestyle for the
management of
GORD
The fact that Mrs P.A
experiences stomach
cramps and has a medical
history of GORD
guarantees her to be
provided with education
regarding self-monitoring of
the disease.
Discuss the eating habits
with the patient and ensure
that the patient has the
knowledge regarding the
best eating approach in the
management of the disease
(1). Most importantly, the
patient must eat smaller
amounts of food but more
frequently. The patient
should avoid foods and
drinks that trigger her
symptoms and keep a
healthy weight through
exercise and healthy eating
habits.
The patient must be
able to recall self-
monitoring strategies
and evaluation
approaches to employ
in the management of
GORD.
***Add/delete more rows as needed***
References:
1. Edwards G, Ball M, inventors; KFSU Ltd, assignee. Dietary Supplement for the Treatment of Acid Reflux and
Gastro-Oesophageal Reflux Disease (GORD/GERD). The United States patent application US 16/167,249. 2019
Feb 21.
2. Kim BJ, Seo DC, Kim BS, Kang JH. Relationship between cotinine-verified smoking status and incidence of
hypertension in 74,743 Korean adults. Circulation Journal. 2018 May 25;82(6):1659-65.
3. Kim Y, Cho WK. Effects of smoking on disease risk among South Korean adults. Tobacco Induced Diseases.
2018 Oct 1;16.
4. Gupta S, Maharjan A, Dhami B, Amgain P, Katwal S, Adhikari B, Shukla A. Status of Tobacco Smoking and
Diabetes with Periodontal Disease. Journal of the Nepal Medical Association. 2018 Sep 1;56(213).
5. Aryanpur M, Yousefifard M, Oraii A, Heydari G, Kazempour-Dizaji M, Sharifi H, Hosseini M, Jamaati H. Effect of
passive exposure to cigarette smoke on blood pressure in children and adolescents: a meta-analysis of
epidemiologic studies. BMC pediatrics. 2019 Dec;19(1):161.
6. Shahab L, Goniewicz ML, Blount BC, Brown J, McNeill A, Alwis KU, Feng J, Wang L, West R. Nicotine,
carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: a cross-
sectional study. Annals of internal medicine. 2017 Mar 21;166(6):390-400.
7. Hartmann‐Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for
smoking cessation. Cochrane database of systematic reviews. 2018(5).
8. Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross
L. A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine.
2019 Feb 14;380(7):629-37.
9. Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross
L. A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine.
2019 Feb 14;380(7):629-37.
9
***NB: Your Case review should be no more than 11 pages (in Ariel size 11 font) up until this point.***
before discharge and a
home care program to
maintain withdrawal.
Modification of
lifestyle for the
management of
GORD
The fact that Mrs P.A
experiences stomach
cramps and has a medical
history of GORD
guarantees her to be
provided with education
regarding self-monitoring of
the disease.
Discuss the eating habits
with the patient and ensure
that the patient has the
knowledge regarding the
best eating approach in the
management of the disease
(1). Most importantly, the
patient must eat smaller
amounts of food but more
frequently. The patient
should avoid foods and
drinks that trigger her
symptoms and keep a
healthy weight through
exercise and healthy eating
habits.
The patient must be
able to recall self-
monitoring strategies
and evaluation
approaches to employ
in the management of
GORD.
***Add/delete more rows as needed***
References:
1. Edwards G, Ball M, inventors; KFSU Ltd, assignee. Dietary Supplement for the Treatment of Acid Reflux and
Gastro-Oesophageal Reflux Disease (GORD/GERD). The United States patent application US 16/167,249. 2019
Feb 21.
2. Kim BJ, Seo DC, Kim BS, Kang JH. Relationship between cotinine-verified smoking status and incidence of
hypertension in 74,743 Korean adults. Circulation Journal. 2018 May 25;82(6):1659-65.
3. Kim Y, Cho WK. Effects of smoking on disease risk among South Korean adults. Tobacco Induced Diseases.
2018 Oct 1;16.
4. Gupta S, Maharjan A, Dhami B, Amgain P, Katwal S, Adhikari B, Shukla A. Status of Tobacco Smoking and
Diabetes with Periodontal Disease. Journal of the Nepal Medical Association. 2018 Sep 1;56(213).
5. Aryanpur M, Yousefifard M, Oraii A, Heydari G, Kazempour-Dizaji M, Sharifi H, Hosseini M, Jamaati H. Effect of
passive exposure to cigarette smoke on blood pressure in children and adolescents: a meta-analysis of
epidemiologic studies. BMC pediatrics. 2019 Dec;19(1):161.
6. Shahab L, Goniewicz ML, Blount BC, Brown J, McNeill A, Alwis KU, Feng J, Wang L, West R. Nicotine,
carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: a cross-
sectional study. Annals of internal medicine. 2017 Mar 21;166(6):390-400.
7. Hartmann‐Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for
smoking cessation. Cochrane database of systematic reviews. 2018(5).
8. Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross
L. A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine.
2019 Feb 14;380(7):629-37.
9. Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross
L. A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine.
2019 Feb 14;380(7):629-37.
9
***NB: Your Case review should be no more than 11 pages (in Ariel size 11 font) up until this point.***
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10. Lindson N, Chepkin SC, Ye W, Fanshawe TR, Bullen C, Hartmann‐Boyce J. Different doses, durations and
modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic
Reviews. 2019(4).
11. Dumanski JP, Lambert JC, Rasi C, Giedraitis V, Davies H, Grenier-Boley B, Lindgren CM, Campion D, Dufouil C,
Initiative TE, Pasquier F. Mosaic loss of chromosome Y in blood is associated with Alzheimer disease. The
American Journal of Human Genetics. 2016 Jun 2;98(6):1208-19.
12. Prince M, Bryce R, Ferri C. World Alzheimer Report 2011: The benefits of early diagnosis and intervention.
13. Bird TD. Alzheimer disease overview. InGeneReviews®[Internet] 2018 Dec 20. University of Washington, Seattle.
14. Bateman R, Benzinger TL, Berry S, Clifford D, Fagan AM, Duggan C, Fanning K, Goate AM, Hassenstab J,
McDade E, Mills S. THE DOMINANTLY INHERITED ALZHEIMER NETWORK TRIALS UNIT. Alzheimer's &
Dementia: The Journal of the Alzheimer's Association. 2016 Jul 1;12(7):P326.
15. Götz J, Bodea LG, Goedert M. Rodent models for Alzheimer disease. Nature Reviews Neuroscience. 2018 Sep
7:1.
16. Hong S, Beja-Glasser VF, Nfonoyim BM, Frouin A, Li S, Ramakrishnan S, Merry KM, Shi Q, Rosenthal A, Barres
BA, Lemere CA. Complement and microglia mediate early synapse loss in Alzheimer mouse models. Science.
2016 May 6;352(6286):712-6.
17. Donato A, Brown K. In black Africans with hypertension, amlodipine-based therapy vs perindopril–
hydrochlorothiazide improved BP control. Annals of internal medicine. 2019 Jul 16;171(2):JC5-.
18. Poulter NR, Dolan E, Gupta AK, O’Brien E, Whitehouse A, Sever PS. Efficacy and Safety of Incremental Dosing
of a New Single-Pill Formulation of Perindopril and Amlodipine in the Management of Hypertension. American
Journal of Cardiovascular Drugs. 2019 Jun 1;19(3):313-23.
19. Uddina AH, Alaamaa M, Zaidul IS, Abbasb SA. Current Analytical Methods For Amlodipine And its Formulations:
A Review.
20. Yi Z, Pei Z, Xiaoyan M. Evaluation of Amlodipine Inhibition and Antimicrobial Effects. International Journal of
Pharmacy and Chemistry. 2019 Apr 15;5(1):12.
21. Morgan JL, Kogutt BK, Meek C, Stehel EK, McIntire DD, Sheffield JS, Roberts SW. Pharmacokinetics of
Amlodipine Besylate at Delivery and During Lactation. Obstetric Anesthesia Digest. 2019 Sep 1;39(3):158-9.
22. Dizon MA, De Leon JM. Effectiveness of initiating deep vein thrombosis prophylaxis in patients with stroke: an
integrative review. Journal of Neuroscience Nursing. 2018 Oct 1;50(5):308-12.
23. DiGiorgio AM, Tsolinas R, Alazzeh M, Haefeli J, Talbott JF, Ferguson AR, Bresnahan JC, Beattie MS, Manley
GT, Whetstone WD, Mummaneni PV. Safety and effectiveness of early chemical deep venous thrombosis
prophylaxis after spinal cord injury: pilot prospective data. Neurosurgical focus. 2017 Nov 1;43(5):E21.
24. Keller RA, Moutzouros V, Dines JS, Bush-Joseph CA, Limpisvasti O. Deep venous thrombosis prophylaxis in
anterior cruciate ligament reconstructive surgery: what is the current state of practice?. Sports health. 2018
Mar;10(2):156-9.
25. Baldwin KD, Namdari S, Zhao J, Mehta S. DVT Prophylaxis in Orthopedic Trauma. InOrthopedic Traumatology
2018 (pp. 385-394). Springer, Cham.
26. Jacobs JJ. DVT PROPHYLAXIS: RISK STRATIFICATION SOLUTIONS. InOrthopaedic Proceedings 2018 Jun
(Vol. 100, No. SUPP_10, pp. 39-39). The British Editorial Society of Bone & Joint Surgery.
27. Demchuk OV, Slobodian DA, Piddubna АA VV, Vintonyak MA. TREATMENT OF PATIENTS WITH CHRONIC
DISEASE KIDNEYS OF THE PRESENCE OF LESIONS GASTRODUODENAL AREAS AND CHRONIC
PYLONEPHRITIS IN COMBINATION WITH METABOLIC SYNDROME. Молодий вчений. 2018 Dec;64(12):48.
28. Vakulenko LI. Dysmetabolic nephropathy as a risk factor of pylonephritis in children. CHILDS HEALTH.
2018;13(1):35-9.
29. Qadir HA, Abdulla AB, Abduljabbar HN. Molecular Study of Virulence Factors of Escherichia coli Isolated from
Patient with urinary tract infection in Wasit Province.
30. Almahjuob AA. Diagnosis of Renal Infection using Ultrasonography (Doctoral dissertation, Sudan University of
Science and Technology).
31. Liao CY, Tsai CC, Kuo WH, Ben RJ, Lin HC, Lee CC, Su KJ, Wang HE, Wang CC, Chen IH, Chien ST.
Emphysematous cholecystitis presenting as gas-forming liver abscess and pneumoperitoneum in a dialysis
patient: a case report and review of the literature. BMC nephrology. 2016 Dec;17(1):23.
10
modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic
Reviews. 2019(4).
11. Dumanski JP, Lambert JC, Rasi C, Giedraitis V, Davies H, Grenier-Boley B, Lindgren CM, Campion D, Dufouil C,
Initiative TE, Pasquier F. Mosaic loss of chromosome Y in blood is associated with Alzheimer disease. The
American Journal of Human Genetics. 2016 Jun 2;98(6):1208-19.
12. Prince M, Bryce R, Ferri C. World Alzheimer Report 2011: The benefits of early diagnosis and intervention.
13. Bird TD. Alzheimer disease overview. InGeneReviews®[Internet] 2018 Dec 20. University of Washington, Seattle.
14. Bateman R, Benzinger TL, Berry S, Clifford D, Fagan AM, Duggan C, Fanning K, Goate AM, Hassenstab J,
McDade E, Mills S. THE DOMINANTLY INHERITED ALZHEIMER NETWORK TRIALS UNIT. Alzheimer's &
Dementia: The Journal of the Alzheimer's Association. 2016 Jul 1;12(7):P326.
15. Götz J, Bodea LG, Goedert M. Rodent models for Alzheimer disease. Nature Reviews Neuroscience. 2018 Sep
7:1.
16. Hong S, Beja-Glasser VF, Nfonoyim BM, Frouin A, Li S, Ramakrishnan S, Merry KM, Shi Q, Rosenthal A, Barres
BA, Lemere CA. Complement and microglia mediate early synapse loss in Alzheimer mouse models. Science.
2016 May 6;352(6286):712-6.
17. Donato A, Brown K. In black Africans with hypertension, amlodipine-based therapy vs perindopril–
hydrochlorothiazide improved BP control. Annals of internal medicine. 2019 Jul 16;171(2):JC5-.
18. Poulter NR, Dolan E, Gupta AK, O’Brien E, Whitehouse A, Sever PS. Efficacy and Safety of Incremental Dosing
of a New Single-Pill Formulation of Perindopril and Amlodipine in the Management of Hypertension. American
Journal of Cardiovascular Drugs. 2019 Jun 1;19(3):313-23.
19. Uddina AH, Alaamaa M, Zaidul IS, Abbasb SA. Current Analytical Methods For Amlodipine And its Formulations:
A Review.
20. Yi Z, Pei Z, Xiaoyan M. Evaluation of Amlodipine Inhibition and Antimicrobial Effects. International Journal of
Pharmacy and Chemistry. 2019 Apr 15;5(1):12.
21. Morgan JL, Kogutt BK, Meek C, Stehel EK, McIntire DD, Sheffield JS, Roberts SW. Pharmacokinetics of
Amlodipine Besylate at Delivery and During Lactation. Obstetric Anesthesia Digest. 2019 Sep 1;39(3):158-9.
22. Dizon MA, De Leon JM. Effectiveness of initiating deep vein thrombosis prophylaxis in patients with stroke: an
integrative review. Journal of Neuroscience Nursing. 2018 Oct 1;50(5):308-12.
23. DiGiorgio AM, Tsolinas R, Alazzeh M, Haefeli J, Talbott JF, Ferguson AR, Bresnahan JC, Beattie MS, Manley
GT, Whetstone WD, Mummaneni PV. Safety and effectiveness of early chemical deep venous thrombosis
prophylaxis after spinal cord injury: pilot prospective data. Neurosurgical focus. 2017 Nov 1;43(5):E21.
24. Keller RA, Moutzouros V, Dines JS, Bush-Joseph CA, Limpisvasti O. Deep venous thrombosis prophylaxis in
anterior cruciate ligament reconstructive surgery: what is the current state of practice?. Sports health. 2018
Mar;10(2):156-9.
25. Baldwin KD, Namdari S, Zhao J, Mehta S. DVT Prophylaxis in Orthopedic Trauma. InOrthopedic Traumatology
2018 (pp. 385-394). Springer, Cham.
26. Jacobs JJ. DVT PROPHYLAXIS: RISK STRATIFICATION SOLUTIONS. InOrthopaedic Proceedings 2018 Jun
(Vol. 100, No. SUPP_10, pp. 39-39). The British Editorial Society of Bone & Joint Surgery.
27. Demchuk OV, Slobodian DA, Piddubna АA VV, Vintonyak MA. TREATMENT OF PATIENTS WITH CHRONIC
DISEASE KIDNEYS OF THE PRESENCE OF LESIONS GASTRODUODENAL AREAS AND CHRONIC
PYLONEPHRITIS IN COMBINATION WITH METABOLIC SYNDROME. Молодий вчений. 2018 Dec;64(12):48.
28. Vakulenko LI. Dysmetabolic nephropathy as a risk factor of pylonephritis in children. CHILDS HEALTH.
2018;13(1):35-9.
29. Qadir HA, Abdulla AB, Abduljabbar HN. Molecular Study of Virulence Factors of Escherichia coli Isolated from
Patient with urinary tract infection in Wasit Province.
30. Almahjuob AA. Diagnosis of Renal Infection using Ultrasonography (Doctoral dissertation, Sudan University of
Science and Technology).
31. Liao CY, Tsai CC, Kuo WH, Ben RJ, Lin HC, Lee CC, Su KJ, Wang HE, Wang CC, Chen IH, Chien ST.
Emphysematous cholecystitis presenting as gas-forming liver abscess and pneumoperitoneum in a dialysis
patient: a case report and review of the literature. BMC nephrology. 2016 Dec;17(1):23.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Reflective account – to be completed by the student
Knowledge from the course that I applied to this patient:
New knowledge learnt from undertaking this coursework:
Further learning I would like to undertake:
I found the following things about this coursework particularly challenging:
I would like specific feedback on the following points:
What I would do differently if I did this coursework again:
11
Knowledge from the course that I applied to this patient:
New knowledge learnt from undertaking this coursework:
Further learning I would like to undertake:
I found the following things about this coursework particularly challenging:
I would like specific feedback on the following points:
What I would do differently if I did this coursework again:
11
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.