Human Respiratory System Physiology: Lecture Notes by Dr. Gül Erdemli
VerifiedAdded on 2023/02/03
|33
|9430
|43
Lecture Notes
AI Summary
These lecture notes, authored by Dr. Gül Erdemli, provide a comprehensive overview of human respiratory system physiology. The content covers the mechanics of breathing, including inspiration and expiration, and delves into the coupling of lungs and chest wall, exploring pressure-volume relationships and compliance. Surface tension and the role of surfactant are also discussed. The notes further examine the regulation and control of breathing, detailing the central controller, including medullary respiratory centers, apneustic, and pneumotaxic centers. The document also covers lung volumes, pulmonary function tests, diffusion, perfusion, gas transport, and acid-base regulation, as well as the respiratory system under stress. These notes are ideal for students seeking a thorough understanding of the respiratory system.
1
LECTURE NOTES ON
HUMAN RESPIRATORY SYSTEM PHYSIOLOGY
(Dr. GÜL ERDEMLI)
CONTENTS
1. MECHANICS OF BREATHING:
2. REGULATION AND CONTROL OF BREATHING:
3. VENTILATION
4. LUNG VOLUMES AND PULMONARY FUNCTION TESTS
5. DIFFUSION
6. PERFUSION
7. GAS TRANSPORT TO THE PERIPHERY
8. ACID-BASE REGULATION
9. RESPIRATORY SYSTEM UNDER STRESS
10. RECOMMENDED FURTHER READING:
11. SELF ASSESSMENT
LECTURE NOTES ON
HUMAN RESPIRATORY SYSTEM PHYSIOLOGY
(Dr. GÜL ERDEMLI)
CONTENTS
1. MECHANICS OF BREATHING:
2. REGULATION AND CONTROL OF BREATHING:
3. VENTILATION
4. LUNG VOLUMES AND PULMONARY FUNCTION TESTS
5. DIFFUSION
6. PERFUSION
7. GAS TRANSPORT TO THE PERIPHERY
8. ACID-BASE REGULATION
9. RESPIRATORY SYSTEM UNDER STRESS
10. RECOMMENDED FURTHER READING:
11. SELF ASSESSMENT
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
1. MECHANICS OF BREATHING:
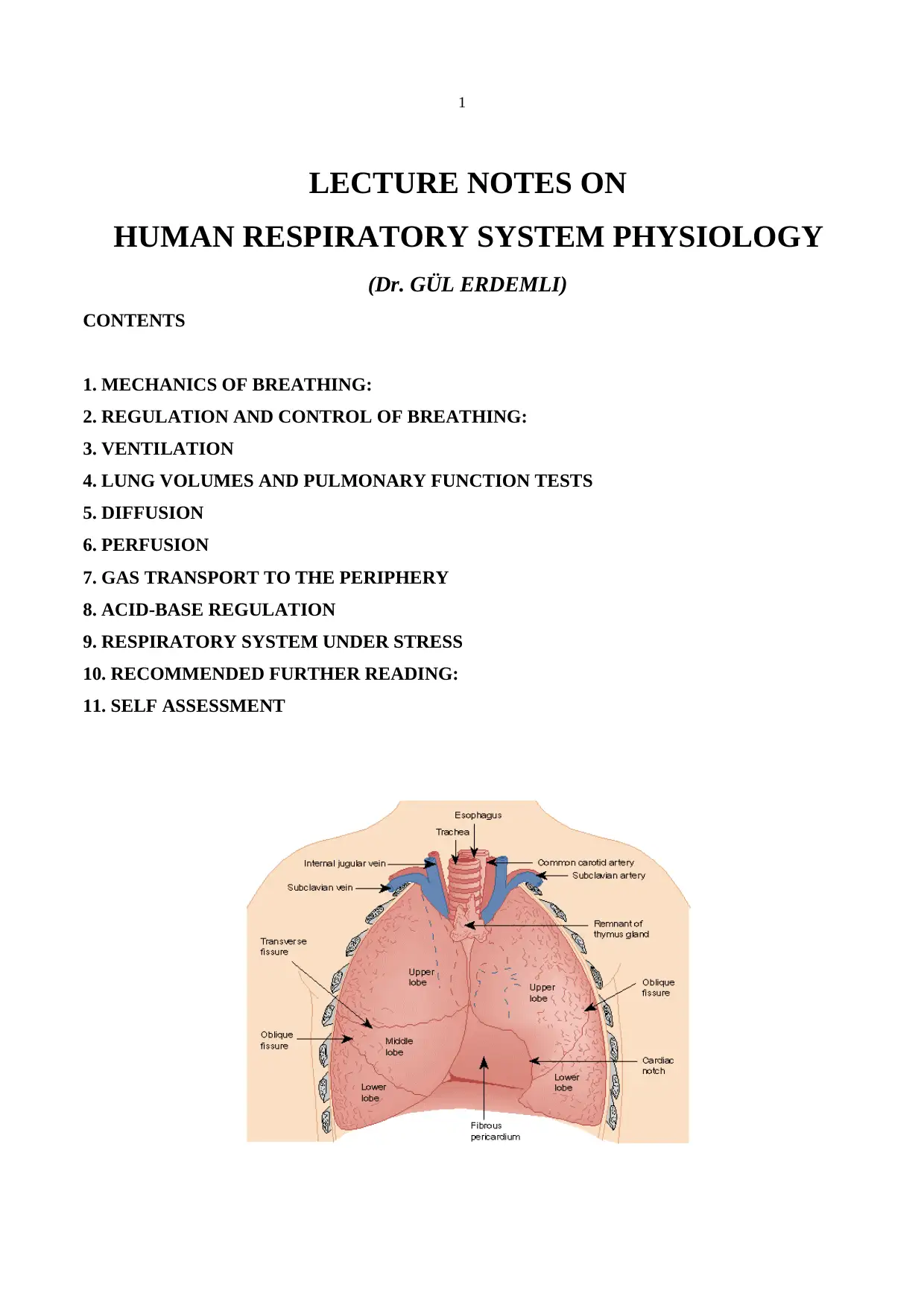
INSPIRATION: Inspiration is the active part of the breathing process, which is initiated by the
respiratory control centre in medulla oblongata (Brain stem). Activation of medulla causes a
contraction of the diaphragm and intercostal muscles leading to an expansion of thoracic cavity and a
decrease in the pleural space pressure. The diaphragm is a dome-shaped structure that separates the
thoracic and abdominal cavities and is the most important muscle of inspiration. When it contracts, it
moves downward and because it is attached to the lower ribs it also rotates the ribs toward the
horizontal plane, and thereby further expands the chest cavity. In normal quite breathing the diaphragm
moves downward about 1 cm but on forced inspiration/expiration total movement could be up to 10
cm. When it is paralysed it moves to the opposite direction (upwards) with inspiration, paradoxical
movement. The external intercostal muscles connect adjacent ribs. When they contract the ribs are
pulled upward and forward causing further increase in the volume of the thoracic cavity. As a result
fresh air flows along the branching airways into the alveoli until the alveolar pressure equals to the
pressure at the airway opening.
EXPIRATION: Expiration is a passive event due to elastic recoil of the lungs. However, when a great
deal of air has to be removed quickly, as in exercise, or when the airways narrow excessively during
expiration, as in asthma, the internal intercostal muscles and the anterior abdominal muscles contract
and accelerate expiration by raising pleural pressure.
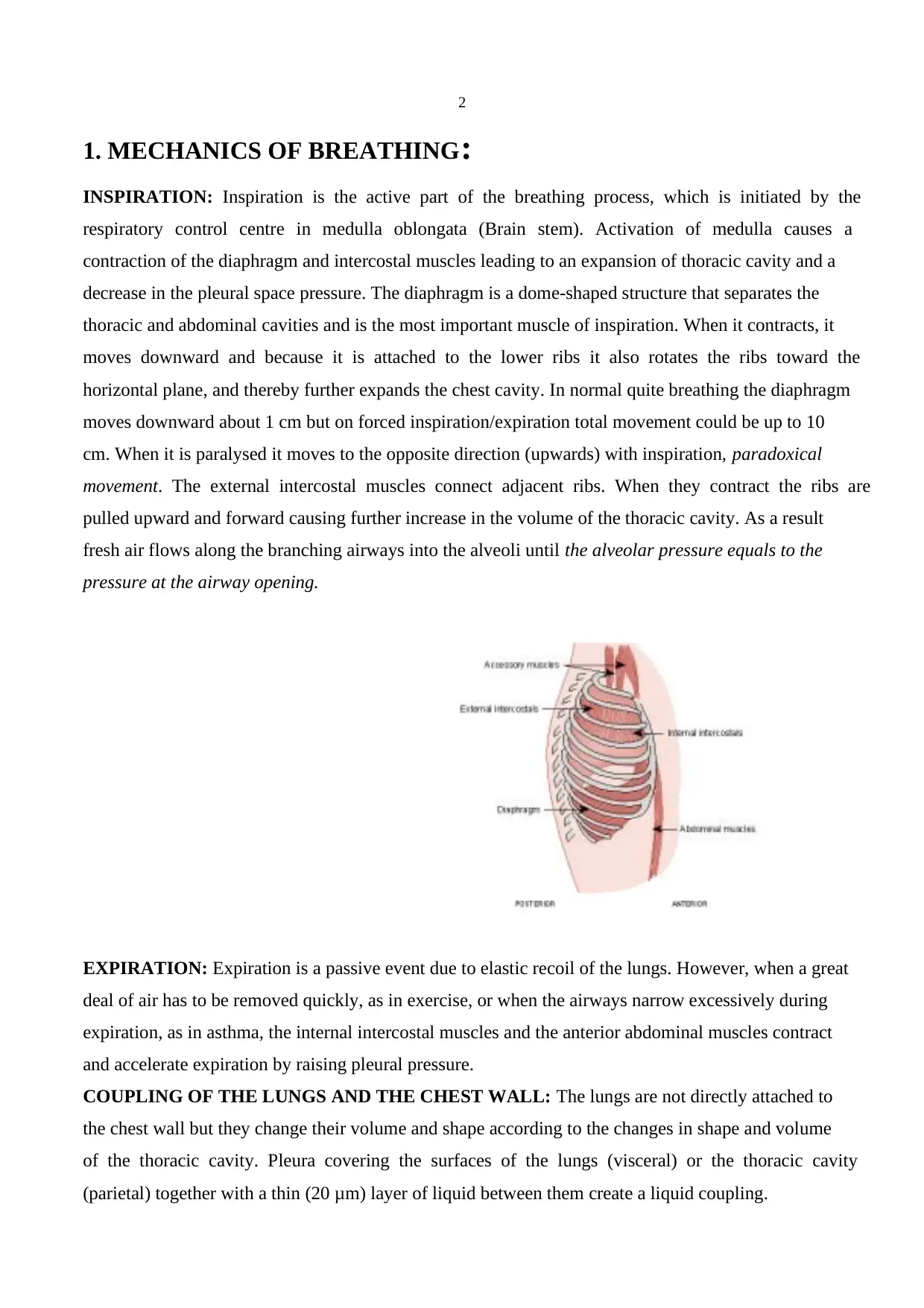
COUPLING OF THE LUNGS AND THE CHEST WALL: The lungs are not directly attached to
the chest wall but they change their volume and shape according to the changes in shape and volume
of the thoracic cavity. Pleura covering the surfaces of the lungs (visceral) or the thoracic cavity
(parietal) together with a thin (20 μm) layer of liquid between them create a liquid coupling.
1. MECHANICS OF BREATHING:
INSPIRATION: Inspiration is the active part of the breathing process, which is initiated by the
respiratory control centre in medulla oblongata (Brain stem). Activation of medulla causes a
contraction of the diaphragm and intercostal muscles leading to an expansion of thoracic cavity and a
decrease in the pleural space pressure. The diaphragm is a dome-shaped structure that separates the
thoracic and abdominal cavities and is the most important muscle of inspiration. When it contracts, it
moves downward and because it is attached to the lower ribs it also rotates the ribs toward the
horizontal plane, and thereby further expands the chest cavity. In normal quite breathing the diaphragm
moves downward about 1 cm but on forced inspiration/expiration total movement could be up to 10
cm. When it is paralysed it moves to the opposite direction (upwards) with inspiration, paradoxical
movement. The external intercostal muscles connect adjacent ribs. When they contract the ribs are
pulled upward and forward causing further increase in the volume of the thoracic cavity. As a result
fresh air flows along the branching airways into the alveoli until the alveolar pressure equals to the
pressure at the airway opening.
EXPIRATION: Expiration is a passive event due to elastic recoil of the lungs. However, when a great
deal of air has to be removed quickly, as in exercise, or when the airways narrow excessively during
expiration, as in asthma, the internal intercostal muscles and the anterior abdominal muscles contract
and accelerate expiration by raising pleural pressure.
COUPLING OF THE LUNGS AND THE CHEST WALL: The lungs are not directly attached to
the chest wall but they change their volume and shape according to the changes in shape and volume
of the thoracic cavity. Pleura covering the surfaces of the lungs (visceral) or the thoracic cavity
(parietal) together with a thin (20 μm) layer of liquid between them create a liquid coupling.
3
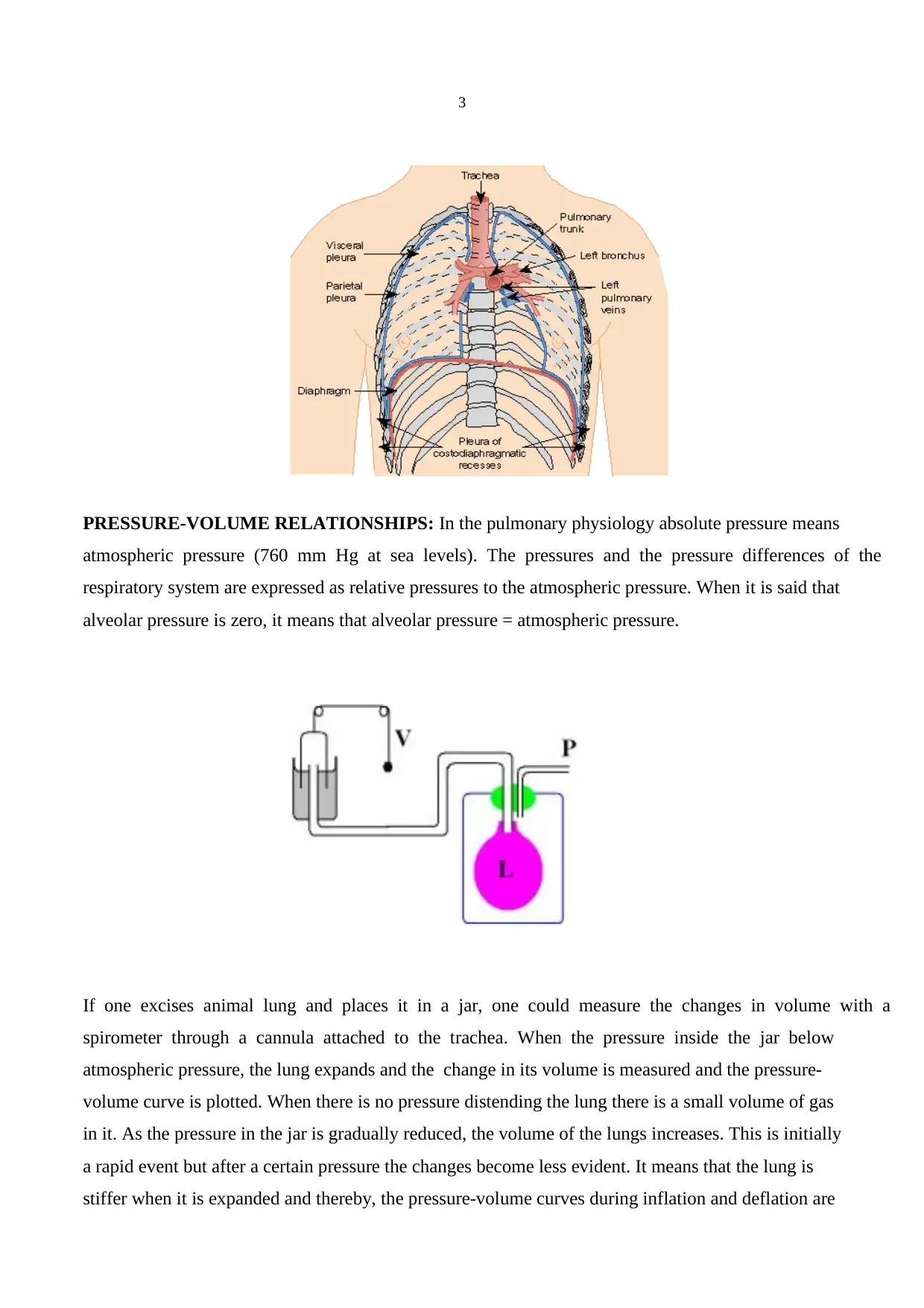
PRESSURE-VOLUME RELATIONSHIPS: In the pulmonary physiology absolute pressure means
atmospheric pressure (760 mm Hg at sea levels). The pressures and the pressure differences of the
respiratory system are expressed as relative pressures to the atmospheric pressure. When it is said that
alveolar pressure is zero, it means that alveolar pressure = atmospheric pressure.
If one excises animal lung and places it in a jar, one could measure the changes in volume with a
spirometer through a cannula attached to the trachea. When the pressure inside the jar below
atmospheric pressure, the lung expands and the change in its volume is measured and the pressure-
volume curve is plotted. When there is no pressure distending the lung there is a small volume of gas
in it. As the pressure in the jar is gradually reduced, the volume of the lungs increases. This is initially
a rapid event but after a certain pressure the changes become less evident. It means that the lung is
stiffer when it is expanded and thereby, the pressure-volume curves during inflation and deflation are
PRESSURE-VOLUME RELATIONSHIPS: In the pulmonary physiology absolute pressure means
atmospheric pressure (760 mm Hg at sea levels). The pressures and the pressure differences of the
respiratory system are expressed as relative pressures to the atmospheric pressure. When it is said that
alveolar pressure is zero, it means that alveolar pressure = atmospheric pressure.
If one excises animal lung and places it in a jar, one could measure the changes in volume with a
spirometer through a cannula attached to the trachea. When the pressure inside the jar below
atmospheric pressure, the lung expands and the change in its volume is measured and the pressure-
volume curve is plotted. When there is no pressure distending the lung there is a small volume of gas
in it. As the pressure in the jar is gradually reduced, the volume of the lungs increases. This is initially
a rapid event but after a certain pressure the changes become less evident. It means that the lung is
stiffer when it is expanded and thereby, the pressure-volume curves during inflation and deflation are
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
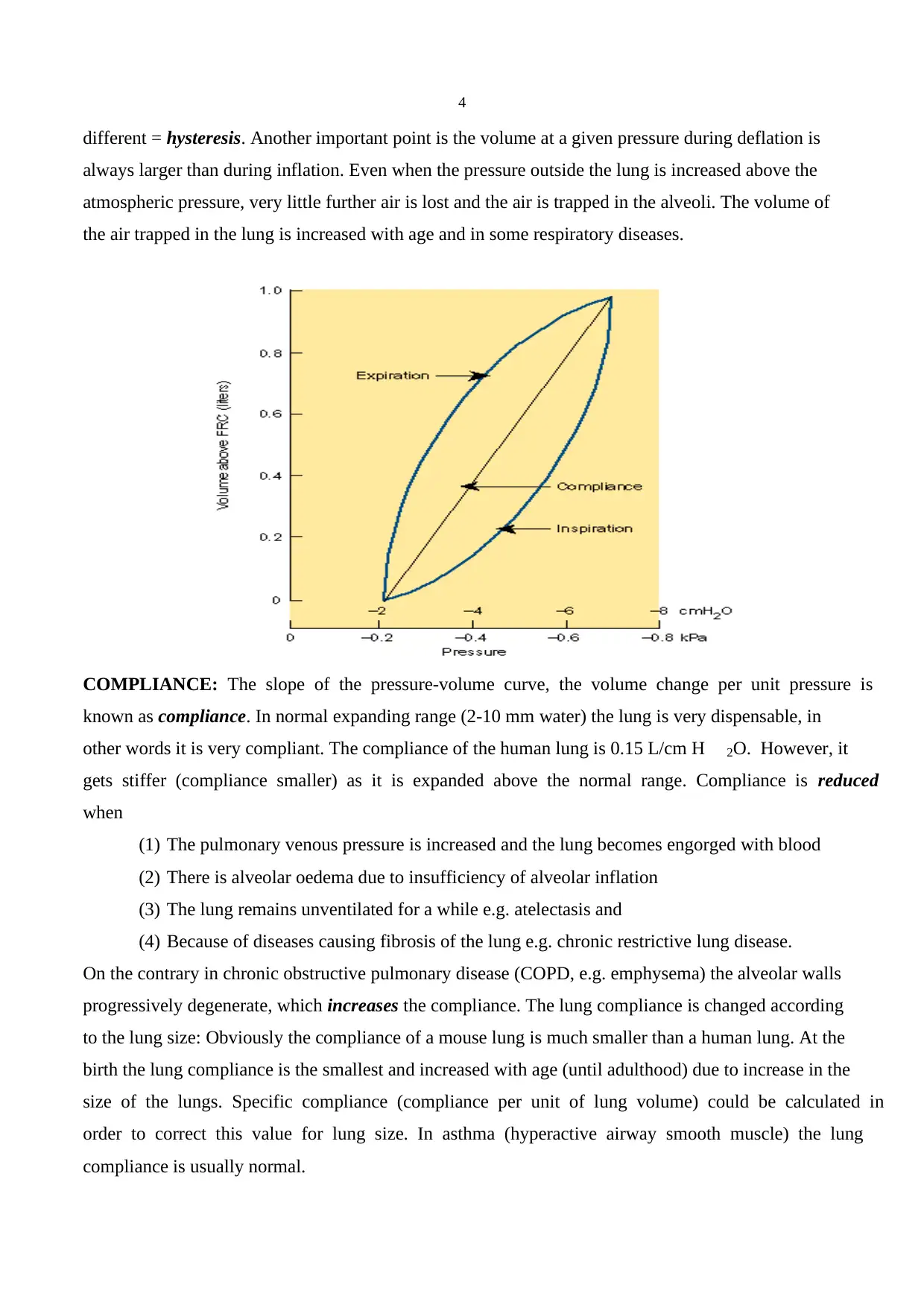
different = hysteresis. Another important point is the volume at a given pressure during deflation is
always larger than during inflation. Even when the pressure outside the lung is increased above the
atmospheric pressure, very little further air is lost and the air is trapped in the alveoli. The volume of
the air trapped in the lung is increased with age and in some respiratory diseases.
COMPLIANCE: The slope of the pressure-volume curve, the volume change per unit pressure is
known as compliance. In normal expanding range (2-10 mm water) the lung is very dispensable, in
other words it is very compliant. The compliance of the human lung is 0.15 L/cm H 2O. However, it
gets stiffer (compliance smaller) as it is expanded above the normal range. Compliance is reduced
when
(1) The pulmonary venous pressure is increased and the lung becomes engorged with blood
(2) There is alveolar oedema due to insufficiency of alveolar inflation
(3) The lung remains unventilated for a while e.g. atelectasis and
(4) Because of diseases causing fibrosis of the lung e.g. chronic restrictive lung disease.
On the contrary in chronic obstructive pulmonary disease (COPD, e.g. emphysema) the alveolar walls
progressively degenerate, which increases the compliance. The lung compliance is changed according
to the lung size: Obviously the compliance of a mouse lung is much smaller than a human lung. At the
birth the lung compliance is the smallest and increased with age (until adulthood) due to increase in the
size of the lungs. Specific compliance (compliance per unit of lung volume) could be calculated in
order to correct this value for lung size. In asthma (hyperactive airway smooth muscle) the lung
compliance is usually normal.
different = hysteresis. Another important point is the volume at a given pressure during deflation is
always larger than during inflation. Even when the pressure outside the lung is increased above the
atmospheric pressure, very little further air is lost and the air is trapped in the alveoli. The volume of
the air trapped in the lung is increased with age and in some respiratory diseases.
COMPLIANCE: The slope of the pressure-volume curve, the volume change per unit pressure is
known as compliance. In normal expanding range (2-10 mm water) the lung is very dispensable, in
other words it is very compliant. The compliance of the human lung is 0.15 L/cm H 2O. However, it
gets stiffer (compliance smaller) as it is expanded above the normal range. Compliance is reduced
when
(1) The pulmonary venous pressure is increased and the lung becomes engorged with blood
(2) There is alveolar oedema due to insufficiency of alveolar inflation
(3) The lung remains unventilated for a while e.g. atelectasis and
(4) Because of diseases causing fibrosis of the lung e.g. chronic restrictive lung disease.
On the contrary in chronic obstructive pulmonary disease (COPD, e.g. emphysema) the alveolar walls
progressively degenerate, which increases the compliance. The lung compliance is changed according
to the lung size: Obviously the compliance of a mouse lung is much smaller than a human lung. At the
birth the lung compliance is the smallest and increased with age (until adulthood) due to increase in the
size of the lungs. Specific compliance (compliance per unit of lung volume) could be calculated in
order to correct this value for lung size. In asthma (hyperactive airway smooth muscle) the lung
compliance is usually normal.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
The standard procedure for measuring compliance in humans is to determine the pressure-volume
relationship during a passive expiration from total lung capacity. If the lung deflates slowly, alveolar
pressure is equal to atmospheric pressure, and pleural pressure is nearly same as the pressure in the
oesophagus, which is usually measured with a thin-walled balloon attached via a plastic tube to a
pressure-sensor.
CHEST WALL COMPLIANCE: Changes in chest wall compliance are less common than changes
in the lung compliance:
(1) pathologic situations preventing the normal movement of the rib cage, such as,
distortion of the spinal column,
(2) pathologic (cancer) or physiologic (pregnancy) reasons increasing the intra
abdominal pressure,
(3) stiff chest, such as broken ribs.
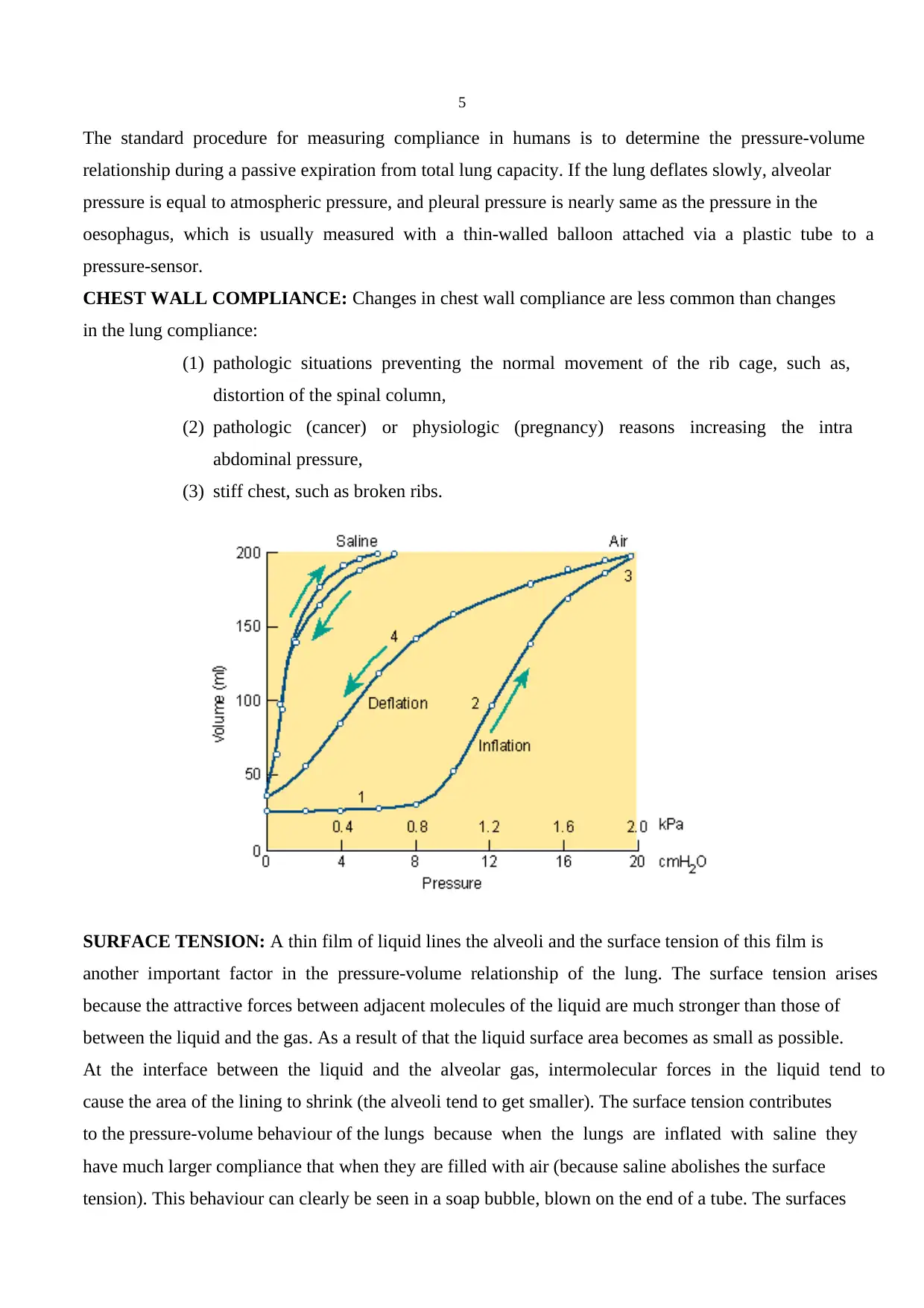
SURFACE TENSION: A thin film of liquid lines the alveoli and the surface tension of this film is
another important factor in the pressure-volume relationship of the lung. The surface tension arises
because the attractive forces between adjacent molecules of the liquid are much stronger than those of
between the liquid and the gas. As a result of that the liquid surface area becomes as small as possible.
At the interface between the liquid and the alveolar gas, intermolecular forces in the liquid tend to
cause the area of the lining to shrink (the alveoli tend to get smaller). The surface tension contributes
to the pressure-volume behaviour of the lungs because when the lungs are inflated with saline they
have much larger compliance that when they are filled with air (because saline abolishes the surface
tension). This behaviour can clearly be seen in a soap bubble, blown on the end of a tube. The surfaces
The standard procedure for measuring compliance in humans is to determine the pressure-volume
relationship during a passive expiration from total lung capacity. If the lung deflates slowly, alveolar
pressure is equal to atmospheric pressure, and pleural pressure is nearly same as the pressure in the
oesophagus, which is usually measured with a thin-walled balloon attached via a plastic tube to a
pressure-sensor.
CHEST WALL COMPLIANCE: Changes in chest wall compliance are less common than changes
in the lung compliance:
(1) pathologic situations preventing the normal movement of the rib cage, such as,
distortion of the spinal column,
(2) pathologic (cancer) or physiologic (pregnancy) reasons increasing the intra
abdominal pressure,
(3) stiff chest, such as broken ribs.
SURFACE TENSION: A thin film of liquid lines the alveoli and the surface tension of this film is
another important factor in the pressure-volume relationship of the lung. The surface tension arises
because the attractive forces between adjacent molecules of the liquid are much stronger than those of
between the liquid and the gas. As a result of that the liquid surface area becomes as small as possible.
At the interface between the liquid and the alveolar gas, intermolecular forces in the liquid tend to
cause the area of the lining to shrink (the alveoli tend to get smaller). The surface tension contributes
to the pressure-volume behaviour of the lungs because when the lungs are inflated with saline they
have much larger compliance that when they are filled with air (because saline abolishes the surface
tension). This behaviour can clearly be seen in a soap bubble, blown on the end of a tube. The surfaces

6
of the bubble contract as much as possible and form the smallest possible surface area, a sphere. This
generates a pressure predicted from Laplace’s law:
Pressure =(4 x surface tension) / radius
The surface tension contributes a large part of the static recoil force of the lung (expiration). The
surface tension changes with the surface area: The larger the area the smaller the surface tension gets.
The most important component of this liquid film is surfactant. It is produced by type 2 alveolar
epithelial cells and its major constituent is dipalmitoyl phosphotidylcholine (DPPC), a phospholipid
with detergent properties. The phospholipid DPPC is synthesised in the lung from fatty acids that are
either extracted from the blood or are themselves synthesised in the lung. Synthesis is fast and there is
a rapid turnover of surfactant. If the blood flow to a region of lung is restricted due to an embolus the
surfactant may be depleted in the effected area. Surfactant synthesis starts relatively late in foetal life
and premature babies without adequate amount of surfactant develop respiratory distress which could
be life threatening.
What are the advantages of having surfactant and the low surface tension?
1. It increases the compliance of the lung
2. It reduces the work of expanding of the lung with each breath
3. It stabilises the alveoli (thus the smaller alveoli do not collapse at the end-expiration)
4. It keeps the alveoli dry (as the surface tension tends to collapse alveoli, it also tends to suck fluid
into the alveolar space from capillaries).
2. REGULATION AND CONTROL OF BREATHING:
In order to maintain normal levels of partial oxygen and carbon dioxide pressure both the depth and
rate of breathing are precisely regulated. Basic elements of the respiratory control system are (1)
strategically placed sensors (2) central controller (3) respiratory muscles.
of the bubble contract as much as possible and form the smallest possible surface area, a sphere. This
generates a pressure predicted from Laplace’s law:
Pressure =(4 x surface tension) / radius
The surface tension contributes a large part of the static recoil force of the lung (expiration). The
surface tension changes with the surface area: The larger the area the smaller the surface tension gets.
The most important component of this liquid film is surfactant. It is produced by type 2 alveolar
epithelial cells and its major constituent is dipalmitoyl phosphotidylcholine (DPPC), a phospholipid
with detergent properties. The phospholipid DPPC is synthesised in the lung from fatty acids that are
either extracted from the blood or are themselves synthesised in the lung. Synthesis is fast and there is
a rapid turnover of surfactant. If the blood flow to a region of lung is restricted due to an embolus the
surfactant may be depleted in the effected area. Surfactant synthesis starts relatively late in foetal life
and premature babies without adequate amount of surfactant develop respiratory distress which could
be life threatening.
What are the advantages of having surfactant and the low surface tension?
1. It increases the compliance of the lung
2. It reduces the work of expanding of the lung with each breath
3. It stabilises the alveoli (thus the smaller alveoli do not collapse at the end-expiration)
4. It keeps the alveoli dry (as the surface tension tends to collapse alveoli, it also tends to suck fluid
into the alveolar space from capillaries).
2. REGULATION AND CONTROL OF BREATHING:
In order to maintain normal levels of partial oxygen and carbon dioxide pressure both the depth and
rate of breathing are precisely regulated. Basic elements of the respiratory control system are (1)
strategically placed sensors (2) central controller (3) respiratory muscles.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
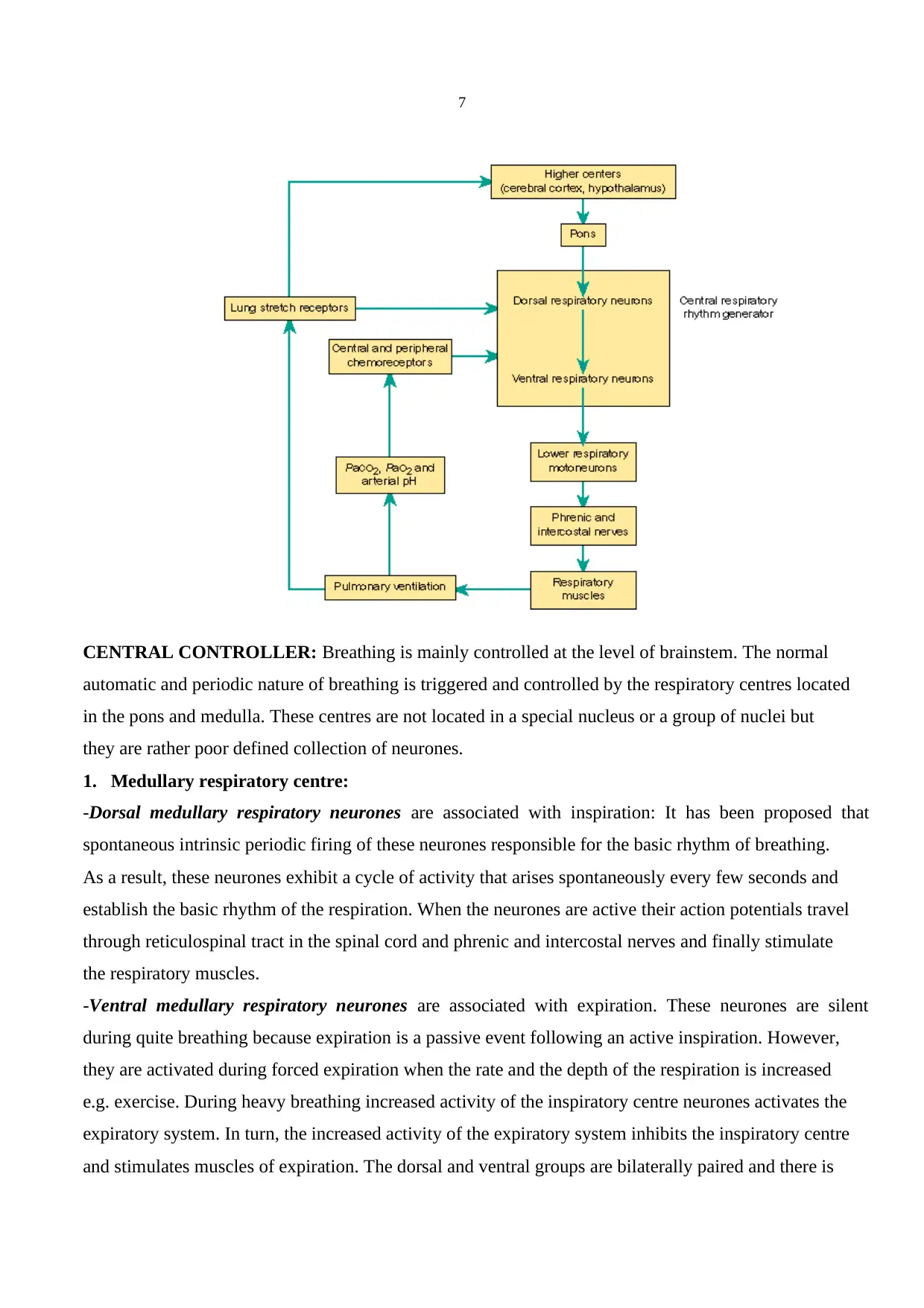
CENTRAL CONTROLLER: Breathing is mainly controlled at the level of brainstem. The normal
automatic and periodic nature of breathing is triggered and controlled by the respiratory centres located
in the pons and medulla. These centres are not located in a special nucleus or a group of nuclei but
they are rather poor defined collection of neurones.
1. Medullary respiratory centre:
-Dorsal medullary respiratory neurones are associated with inspiration: It has been proposed that
spontaneous intrinsic periodic firing of these neurones responsible for the basic rhythm of breathing.
As a result, these neurones exhibit a cycle of activity that arises spontaneously every few seconds and
establish the basic rhythm of the respiration. When the neurones are active their action potentials travel
through reticulospinal tract in the spinal cord and phrenic and intercostal nerves and finally stimulate
the respiratory muscles.
-Ventral medullary respiratory neurones are associated with expiration. These neurones are silent
during quite breathing because expiration is a passive event following an active inspiration. However,
they are activated during forced expiration when the rate and the depth of the respiration is increased
e.g. exercise. During heavy breathing increased activity of the inspiratory centre neurones activates the
expiratory system. In turn, the increased activity of the expiratory system inhibits the inspiratory centre
and stimulates muscles of expiration. The dorsal and ventral groups are bilaterally paired and there is
CENTRAL CONTROLLER: Breathing is mainly controlled at the level of brainstem. The normal
automatic and periodic nature of breathing is triggered and controlled by the respiratory centres located
in the pons and medulla. These centres are not located in a special nucleus or a group of nuclei but
they are rather poor defined collection of neurones.
1. Medullary respiratory centre:
-Dorsal medullary respiratory neurones are associated with inspiration: It has been proposed that
spontaneous intrinsic periodic firing of these neurones responsible for the basic rhythm of breathing.
As a result, these neurones exhibit a cycle of activity that arises spontaneously every few seconds and
establish the basic rhythm of the respiration. When the neurones are active their action potentials travel
through reticulospinal tract in the spinal cord and phrenic and intercostal nerves and finally stimulate
the respiratory muscles.
-Ventral medullary respiratory neurones are associated with expiration. These neurones are silent
during quite breathing because expiration is a passive event following an active inspiration. However,
they are activated during forced expiration when the rate and the depth of the respiration is increased
e.g. exercise. During heavy breathing increased activity of the inspiratory centre neurones activates the
expiratory system. In turn, the increased activity of the expiratory system inhibits the inspiratory centre
and stimulates muscles of expiration. The dorsal and ventral groups are bilaterally paired and there is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
cross communication between them. As a consequence they behave in synchrony and the respiratory
movements are symmetric.
2.Apneustic Centre: It is located in the lower pons. Exact role of this centre in the normal breathing is
not known. Lesions covering this area in the pons cause a pathologic respiratory rhythm with increased
apnoea frequency. What is known is nerve impulses from the apneustic centre stimulate the inspiratory
centre and without constant influence of this centre respiration becomes shallow and irregular.
3.Pneumotaxic centre: It is located in the upper pons. This centre is a group of neurones that have an
inhibitory effect on the both inspiratory and apneustic centres. It is probably responsible for the
termination of inspiration by inhibiting the activity of the dorsal medullar neurones. It primarily
regulates the volume and secondarily the rate of the respiration. Because in the lesions of this area
normal respiration is protected it is generally believed that upper pons is responsible for the fine-tuning
of the respiratory rhythm. Hypoactivation of this centre causes prolonged deep inspirations and brief,
limited expirations by allowing the inspiration centre remain active longer than normal.
Hyperactivation of this centre on the other hand results in shallow inspirations. The apneustic and
pneumotaxic centres function in co-ordination in order to provide a rhythmic respiratory cycle:
Activation of the inspiratory centre stimulates the muscles of inspiration and also the pneumotaxic
centre. Then the pneumotaxic centre inhibits both the apneustic and the inspiratory centres resulting in
initiation of expiration. Spontaneous activity of the neurones in the inspiratory centre starts another
similar cycle again.
Breathing in some extent is also controlled consciously from higher brain centres (e.g. cerebral cortex).
This control is required when we talk, cough and vomit. It is also possible voluntarily change the rate
of the breathing. Hyperventilation can decrease blood partial carbon dioxide pressure (PCO 2) due to
loss of CO 2 resulting in peripheral vasodilatation and decrease in blood pressure. One can also stop
breathing voluntarily. That results in an increase in arterial partial oxygen pressure (PO2), which
produces an urge to breathe. When eventually PCO2 reaches the high enough level it overrides the
conscious influences from the cortex and stimulates the inspiratory system. If one holds his breath long
enough to decrease PO2 to a very low level one may loose his consciousness. In an unconscious person
automatic control of the respiration takes over and the normal breathing resumes.
Other parts of the brain (limbic system, hypothalamus) can also alter the breathing pattern e.g.
affective states, strong emotions such as rage and fear. In addition, stimulation of touch, thermal and
pain receptors can also stimulate the respiratory system.
cross communication between them. As a consequence they behave in synchrony and the respiratory
movements are symmetric.
2.Apneustic Centre: It is located in the lower pons. Exact role of this centre in the normal breathing is
not known. Lesions covering this area in the pons cause a pathologic respiratory rhythm with increased
apnoea frequency. What is known is nerve impulses from the apneustic centre stimulate the inspiratory
centre and without constant influence of this centre respiration becomes shallow and irregular.
3.Pneumotaxic centre: It is located in the upper pons. This centre is a group of neurones that have an
inhibitory effect on the both inspiratory and apneustic centres. It is probably responsible for the
termination of inspiration by inhibiting the activity of the dorsal medullar neurones. It primarily
regulates the volume and secondarily the rate of the respiration. Because in the lesions of this area
normal respiration is protected it is generally believed that upper pons is responsible for the fine-tuning
of the respiratory rhythm. Hypoactivation of this centre causes prolonged deep inspirations and brief,
limited expirations by allowing the inspiration centre remain active longer than normal.
Hyperactivation of this centre on the other hand results in shallow inspirations. The apneustic and
pneumotaxic centres function in co-ordination in order to provide a rhythmic respiratory cycle:
Activation of the inspiratory centre stimulates the muscles of inspiration and also the pneumotaxic
centre. Then the pneumotaxic centre inhibits both the apneustic and the inspiratory centres resulting in
initiation of expiration. Spontaneous activity of the neurones in the inspiratory centre starts another
similar cycle again.
Breathing in some extent is also controlled consciously from higher brain centres (e.g. cerebral cortex).
This control is required when we talk, cough and vomit. It is also possible voluntarily change the rate
of the breathing. Hyperventilation can decrease blood partial carbon dioxide pressure (PCO 2) due to
loss of CO 2 resulting in peripheral vasodilatation and decrease in blood pressure. One can also stop
breathing voluntarily. That results in an increase in arterial partial oxygen pressure (PO2), which
produces an urge to breathe. When eventually PCO2 reaches the high enough level it overrides the
conscious influences from the cortex and stimulates the inspiratory system. If one holds his breath long
enough to decrease PO2 to a very low level one may loose his consciousness. In an unconscious person
automatic control of the respiration takes over and the normal breathing resumes.
Other parts of the brain (limbic system, hypothalamus) can also alter the breathing pattern e.g.
affective states, strong emotions such as rage and fear. In addition, stimulation of touch, thermal and
pain receptors can also stimulate the respiratory system.
9
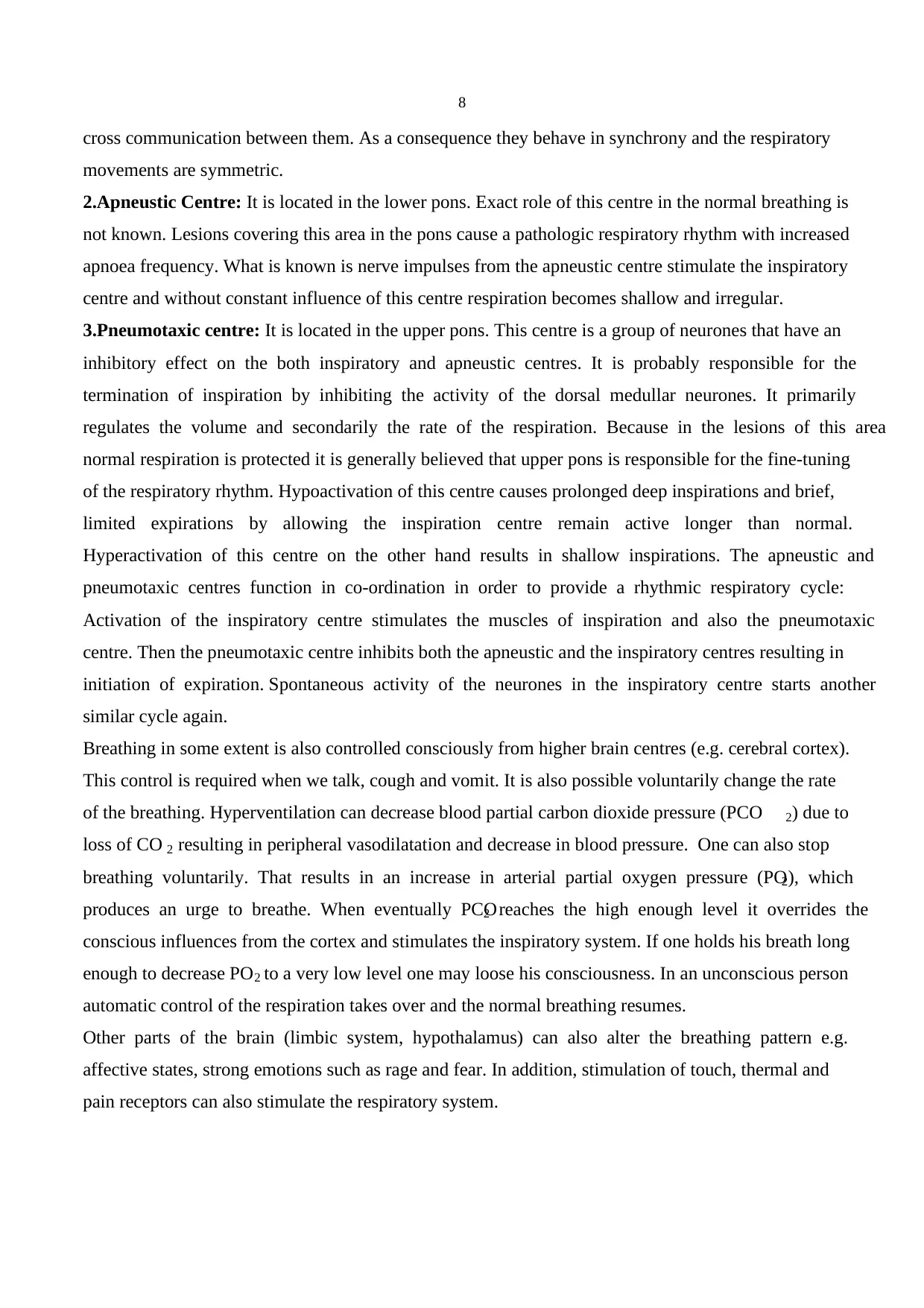
RESPIRATORY MUSCLES: Diaphragm, intercostal muscles and the other accessory respiratory
muscles work in co-ordination for normal breathing under central controller. There is evidence
suggesting that in premature new-born babies this co-ordination is not mature enough and this could be
responsible for the sudden infant death syndrome.
RESPIRATORY MUSCLES: Diaphragm, intercostal muscles and the other accessory respiratory
muscles work in co-ordination for normal breathing under central controller. There is evidence
suggesting that in premature new-born babies this co-ordination is not mature enough and this could be
responsible for the sudden infant death syndrome.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
SENSORS:
1.MECHANORECEPTORS: These receptors are placed in the walls of bronchi and bronchioles of
the lung and the main function of these receptors is to prevent the overinflation of the lungs. Inflation
of the lungs activates these receptors and activation of the stretch receptors in turn inhibits the
neurones in inspiratory centre via vagus nerve. When the expiration starts activation of the stretch
receptors gradually ceases allowing neurones in the inspiratory neurones become active again. This
phenomenon is called Hering-Breuer Reflex. It is particularly important for infants. In adults it is
functional only during exercise when the tidal volume is larger than normal.
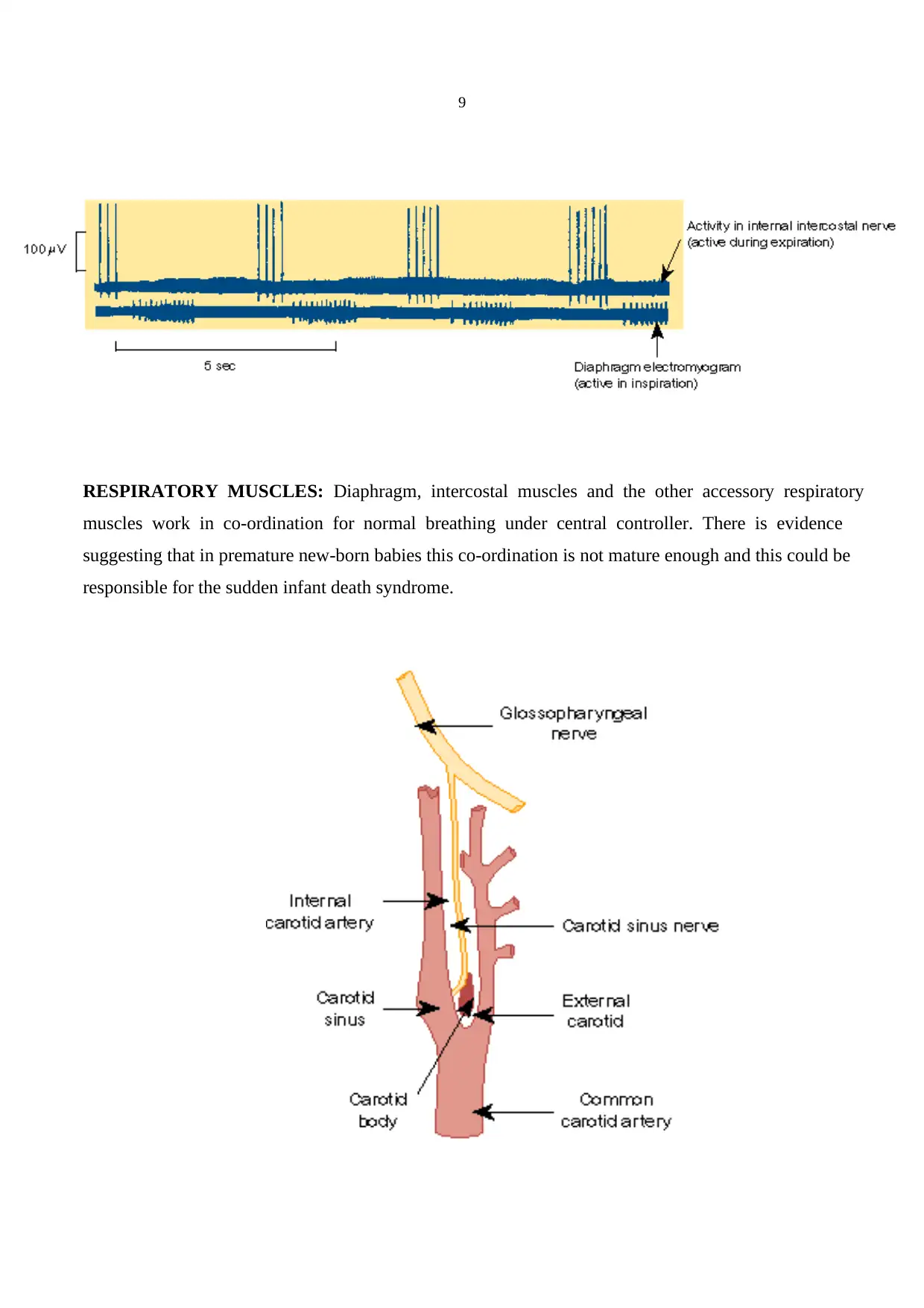
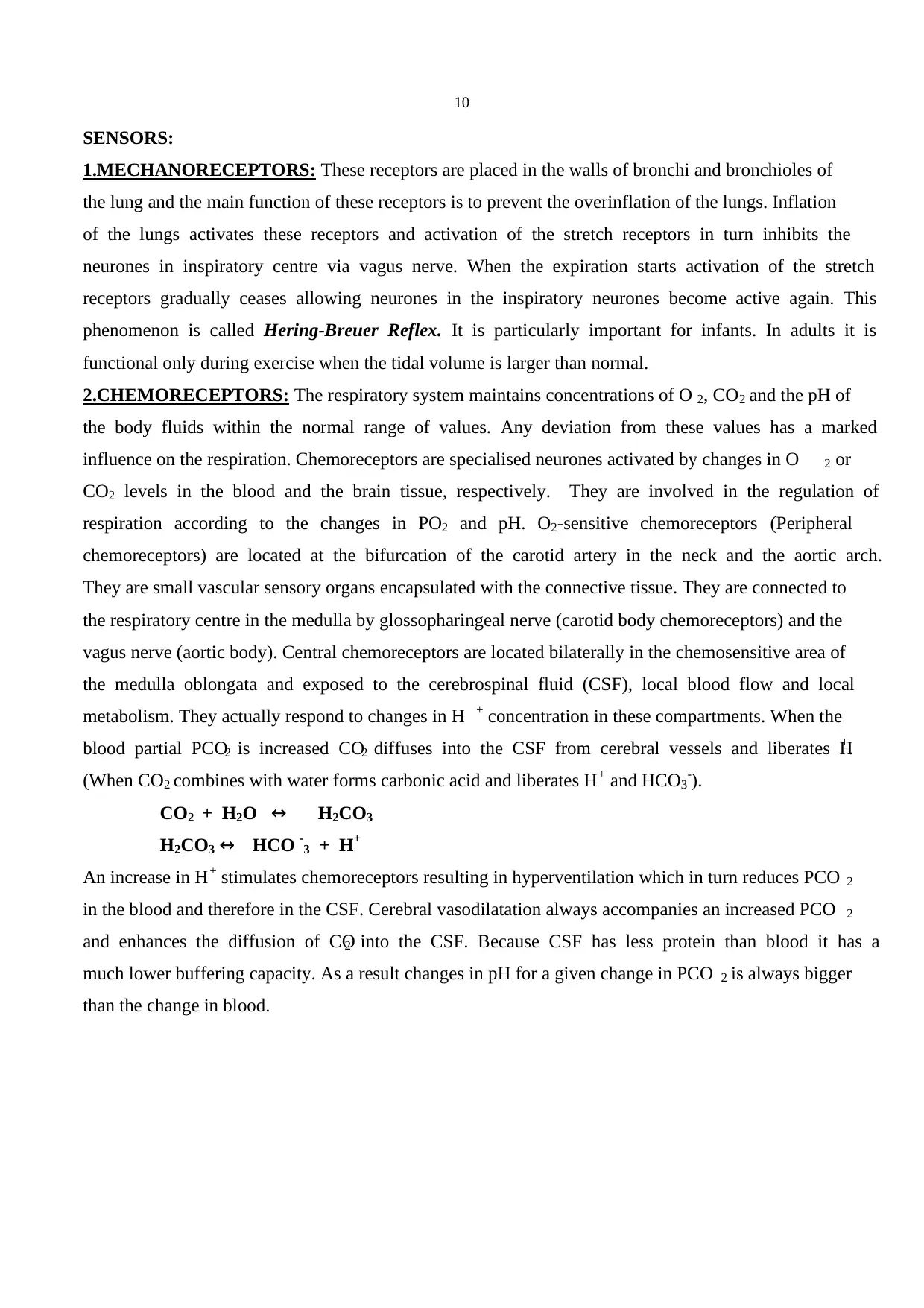
2.CHEMORECEPTORS: The respiratory system maintains concentrations of O 2, CO2 and the pH of
the body fluids within the normal range of values. Any deviation from these values has a marked
influence on the respiration. Chemoreceptors are specialised neurones activated by changes in O 2 or
CO2 levels in the blood and the brain tissue, respectively. They are involved in the regulation of
respiration according to the changes in PO2 and pH. O2-sensitive chemoreceptors (Peripheral
chemoreceptors) are located at the bifurcation of the carotid artery in the neck and the aortic arch.
They are small vascular sensory organs encapsulated with the connective tissue. They are connected to
the respiratory centre in the medulla by glossopharingeal nerve (carotid body chemoreceptors) and the
vagus nerve (aortic body). Central chemoreceptors are located bilaterally in the chemosensitive area of
the medulla oblongata and exposed to the cerebrospinal fluid (CSF), local blood flow and local
metabolism. They actually respond to changes in H + concentration in these compartments. When the
blood partial PCO2 is increased CO2 diffuses into the CSF from cerebral vessels and liberates H+.
(When CO2 combines with water forms carbonic acid and liberates H+ and HCO3-).
CO2 + H2O ↔ H2CO3
H2CO3 ↔ HCO -3 + H+
An increase in H+ stimulates chemoreceptors resulting in hyperventilation which in turn reduces PCO 2
in the blood and therefore in the CSF. Cerebral vasodilatation always accompanies an increased PCO 2
and enhances the diffusion of CO2 into the CSF. Because CSF has less protein than blood it has a
much lower buffering capacity. As a result changes in pH for a given change in PCO 2 is always bigger
than the change in blood.
SENSORS:
1.MECHANORECEPTORS: These receptors are placed in the walls of bronchi and bronchioles of
the lung and the main function of these receptors is to prevent the overinflation of the lungs. Inflation
of the lungs activates these receptors and activation of the stretch receptors in turn inhibits the
neurones in inspiratory centre via vagus nerve. When the expiration starts activation of the stretch
receptors gradually ceases allowing neurones in the inspiratory neurones become active again. This
phenomenon is called Hering-Breuer Reflex. It is particularly important for infants. In adults it is
functional only during exercise when the tidal volume is larger than normal.
2.CHEMORECEPTORS: The respiratory system maintains concentrations of O 2, CO2 and the pH of
the body fluids within the normal range of values. Any deviation from these values has a marked
influence on the respiration. Chemoreceptors are specialised neurones activated by changes in O 2 or
CO2 levels in the blood and the brain tissue, respectively. They are involved in the regulation of
respiration according to the changes in PO2 and pH. O2-sensitive chemoreceptors (Peripheral
chemoreceptors) are located at the bifurcation of the carotid artery in the neck and the aortic arch.
They are small vascular sensory organs encapsulated with the connective tissue. They are connected to
the respiratory centre in the medulla by glossopharingeal nerve (carotid body chemoreceptors) and the
vagus nerve (aortic body). Central chemoreceptors are located bilaterally in the chemosensitive area of
the medulla oblongata and exposed to the cerebrospinal fluid (CSF), local blood flow and local
metabolism. They actually respond to changes in H + concentration in these compartments. When the
blood partial PCO2 is increased CO2 diffuses into the CSF from cerebral vessels and liberates H+.
(When CO2 combines with water forms carbonic acid and liberates H+ and HCO3-).
CO2 + H2O ↔ H2CO3
H2CO3 ↔ HCO -3 + H+
An increase in H+ stimulates chemoreceptors resulting in hyperventilation which in turn reduces PCO 2
in the blood and therefore in the CSF. Cerebral vasodilatation always accompanies an increased PCO 2
and enhances the diffusion of CO2 into the CSF. Because CSF has less protein than blood it has a
much lower buffering capacity. As a result changes in pH for a given change in PCO 2 is always bigger
than the change in blood.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
CO2 level is a major regulator of respiration. It is much more important than oxygen to maintain
normal respiration. Even very small changes in carbon dioxide levels (5 mm Hg increase in PCO2,
hypercapnia) in the blood cause large increases in the rate and depth of respiration (100 % increase in
ventilation). Hypocapnia, lower than normal PCO2 level in the blood causes in periods in which
respiratory movements do not occur. Effects of PO 2 (if the changes occur within the normal range) on
respiration is very minor. A decrease in PO 2 is called hypoxia and only after 50 % decrease in PO 2 can
produce significant changes in respiration. This is due to the nature of O2-Hb saturation that at any PO2
level above 80 mm Hg Hb is saturated with O2. Consequently only big changes in PO2 produce
symptoms otherwise it is compensated by O2, which is bound with Hb.
In stroke patients or physiologically at high altitude blood PO2 level may drop considerably and
activate peripheral chemoreceptors and activate stimulation. At high altitude because the ability of the
lung to eliminate CO2 is not affected, in response to increased respiration, blood PCO 2 is decreased. If
PO2 drops under certain level respiratory system does not respond and death will occur.
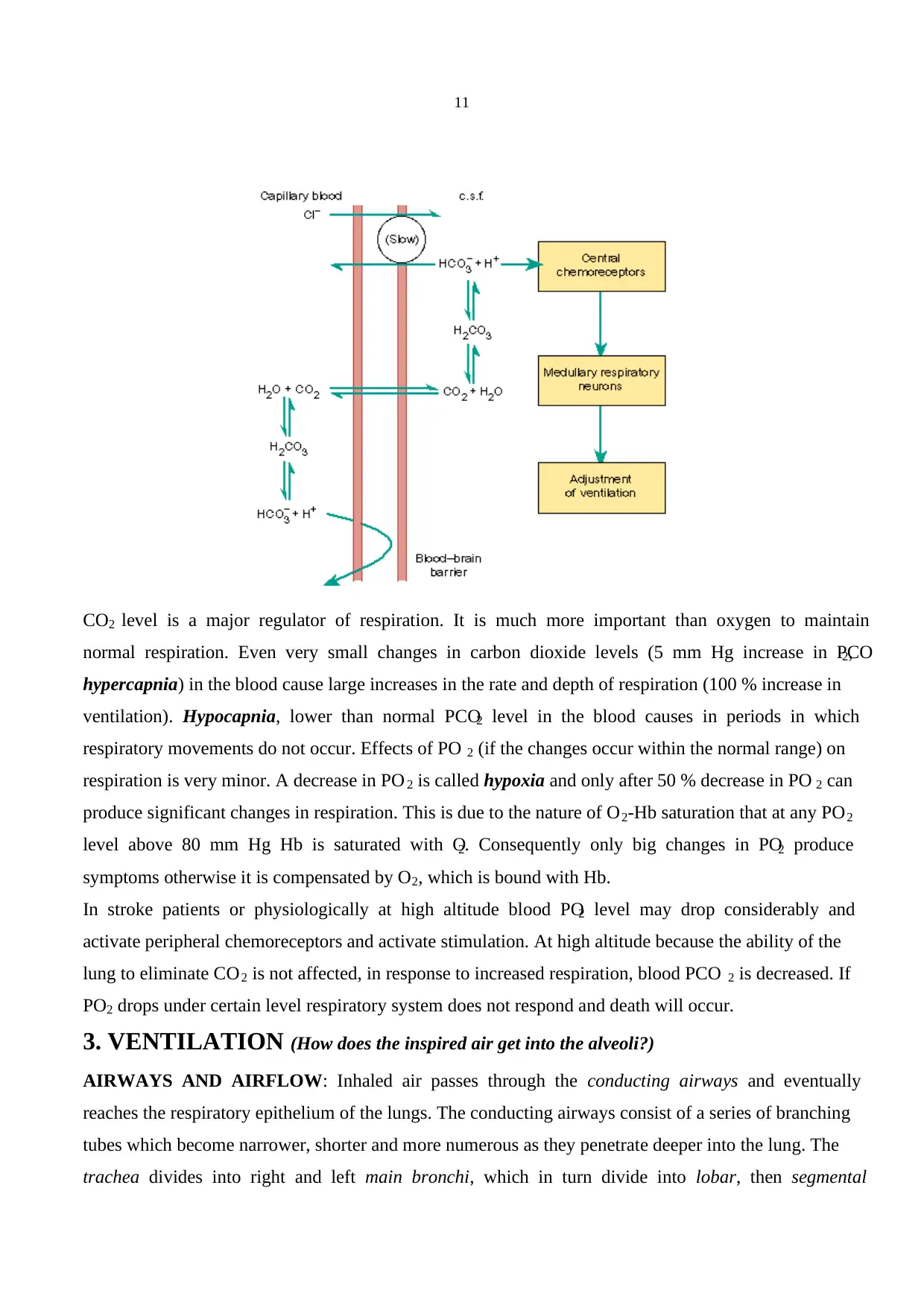
3. VENTILATION (How does the inspired air get into the alveoli?)
AIRWAYS AND AIRFLOW: Inhaled air passes through the conducting airways and eventually
reaches the respiratory epithelium of the lungs. The conducting airways consist of a series of branching
tubes which become narrower, shorter and more numerous as they penetrate deeper into the lung. The
trachea divides into right and left main bronchi, which in turn divide into lobar, then segmental
CO2 level is a major regulator of respiration. It is much more important than oxygen to maintain
normal respiration. Even very small changes in carbon dioxide levels (5 mm Hg increase in PCO2,
hypercapnia) in the blood cause large increases in the rate and depth of respiration (100 % increase in
ventilation). Hypocapnia, lower than normal PCO2 level in the blood causes in periods in which
respiratory movements do not occur. Effects of PO 2 (if the changes occur within the normal range) on
respiration is very minor. A decrease in PO 2 is called hypoxia and only after 50 % decrease in PO 2 can
produce significant changes in respiration. This is due to the nature of O2-Hb saturation that at any PO2
level above 80 mm Hg Hb is saturated with O2. Consequently only big changes in PO2 produce
symptoms otherwise it is compensated by O2, which is bound with Hb.
In stroke patients or physiologically at high altitude blood PO2 level may drop considerably and
activate peripheral chemoreceptors and activate stimulation. At high altitude because the ability of the
lung to eliminate CO2 is not affected, in response to increased respiration, blood PCO 2 is decreased. If
PO2 drops under certain level respiratory system does not respond and death will occur.
3. VENTILATION (How does the inspired air get into the alveoli?)
AIRWAYS AND AIRFLOW: Inhaled air passes through the conducting airways and eventually
reaches the respiratory epithelium of the lungs. The conducting airways consist of a series of branching
tubes which become narrower, shorter and more numerous as they penetrate deeper into the lung. The
trachea divides into right and left main bronchi, which in turn divide into lobar, then segmental
12
bronchi. This process continues down to the terminal bronchioles, which are the smallest airways
without alveoli. Since the conducting airways have no alveoli they do not take part in gas exchange but
constitute the anatomical dead space. Its volume is about 150 ml but it varies because airways are not
rigid; during inspiration, respiratory tubes are lengthened and dilated, especially in deep breathing.
Since the airways serve as a barrier as well, harmful foreign material including most micro-organisms
can not easily enter the lower respiratory passages. The very first barrier starts at the vestibules of the
nose, which contain hairs, and healthy, sticky mucus intercepting air-borne particles. Caught particles
are then ejected by ciliated epithelium, which covers the entire upper respiratory tract. Various factors
can interfere with ciliary activity: for example nicotine and tar in tobacco smoking. Coughing occurs in
response to chemical or mechanical irritation of nerve endings in the upper respiratory tract. The
larynx and the bifurcation of the trachea are the most sensitive regions and any particles of foreign
matter lodged in these regions are removed when a cough sends a rapid blast of air sweeping out the
respiratory tree.
The alveolated region of the lung includes respiratory bronchioles (divided from terminal bronchioles
and have only occasional alveoli on their walls) and alveolar ducts (completely lined with alveoli).
This zone is called respiratory zone and the gas exchange occurs here. The distance from the terminal
bronchiole to the distal alveous is only a few mm, but the respiratory zone makes up most of the lung,
its volume being about 2.5 to 3 L.
bronchi. This process continues down to the terminal bronchioles, which are the smallest airways
without alveoli. Since the conducting airways have no alveoli they do not take part in gas exchange but
constitute the anatomical dead space. Its volume is about 150 ml but it varies because airways are not
rigid; during inspiration, respiratory tubes are lengthened and dilated, especially in deep breathing.
Since the airways serve as a barrier as well, harmful foreign material including most micro-organisms
can not easily enter the lower respiratory passages. The very first barrier starts at the vestibules of the
nose, which contain hairs, and healthy, sticky mucus intercepting air-borne particles. Caught particles
are then ejected by ciliated epithelium, which covers the entire upper respiratory tract. Various factors
can interfere with ciliary activity: for example nicotine and tar in tobacco smoking. Coughing occurs in
response to chemical or mechanical irritation of nerve endings in the upper respiratory tract. The
larynx and the bifurcation of the trachea are the most sensitive regions and any particles of foreign
matter lodged in these regions are removed when a cough sends a rapid blast of air sweeping out the
respiratory tree.
The alveolated region of the lung includes respiratory bronchioles (divided from terminal bronchioles
and have only occasional alveoli on their walls) and alveolar ducts (completely lined with alveoli).
This zone is called respiratory zone and the gas exchange occurs here. The distance from the terminal
bronchiole to the distal alveous is only a few mm, but the respiratory zone makes up most of the lung,
its volume being about 2.5 to 3 L.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 33
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





