Pathophysiology and Medical Sonography of Hydrocele: A Detailed Report
VerifiedAdded on 2022/11/24
|7
|1192
|85
Report
AI Summary
This report provides a comprehensive overview of hydrocele, detailing its pathophysiology and the medical sonography techniques used for diagnosis. It begins by explaining the condition's underlying causes, including imbalances in fluid production and absorption within the scrotum, and differentiates between communicating and non-communicating hydroceles. The report then explores various medical screening procedures, such as inguinal-scrotal imaging ultrasound and testicular scintigraphy, with a particular focus on Doppler ultrasonography. It explains how Doppler ultrasonography helps in evaluating scrotal swelling, differentiating between conditions like testicular torsion and hernia, and measuring testicular volume. The report includes visual aids like diagrams and ultrasound images to illustrate the findings, and also references several studies that support the information presented.

Running Head: PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
Pathophysiology and Medical Sonography of Testes Hydrocele
Student’s Name
University Name
Author Note
Pathophysiology and Medical Sonography of Testes Hydrocele
Student’s Name
University Name
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
PART A:
Pathophysiology of the disease:
Normally, the testis is bounded by a smooth protective tissue sac. It generates a small amount of
lubricating fluid which allows the testis to move freely. The excess fluid generally drains away
into the veins present in the scrotum. Thus, Hydrocele arises due to the accumulation of excess
fluid inside the scrotum. This results in the enlargement one of the testicles. This is mostly
common in premature new-born babies. This mainly occurs if the processus vaginalis fails to
close completely or the body is incapable of absorbing the excess fluid excreted. But in adults, it
is mainly the result of scrotal inflammation or injury (Patil, Shetty and Das, 2015). Thus, the
pathophysiology of hydroceles involves the imbalance of intrinsic scrotal fluid production by the
mesothelial cells present in the inner surface of the tunica vaginalis and fluid absorption by the
draining the lymphatic vessels present in the parietal layer.
There are mainly two types of hydroceles-
Communicating hydroceles: It is caused from exogenous sources. This type causes
indirect hernia.
Non-communicating hydroceles: It is developed due to the abnormal intrinsic scrotal
fluid shifts.
The hydroceles are positioned anterior and superior to the testis. Thus, hydrocele has a chance of
occurring bilaterally in 7-10 % of the cases. Thus, when it occurs on the right side of the body, it
can be easily linked with hernia. Usually most of the pediatric hydroceles are congenital. When
hydrocele occurs in the cord, it is often associated with failure of processus vaginalis to close
PART A:
Pathophysiology of the disease:
Normally, the testis is bounded by a smooth protective tissue sac. It generates a small amount of
lubricating fluid which allows the testis to move freely. The excess fluid generally drains away
into the veins present in the scrotum. Thus, Hydrocele arises due to the accumulation of excess
fluid inside the scrotum. This results in the enlargement one of the testicles. This is mostly
common in premature new-born babies. This mainly occurs if the processus vaginalis fails to
close completely or the body is incapable of absorbing the excess fluid excreted. But in adults, it
is mainly the result of scrotal inflammation or injury (Patil, Shetty and Das, 2015). Thus, the
pathophysiology of hydroceles involves the imbalance of intrinsic scrotal fluid production by the
mesothelial cells present in the inner surface of the tunica vaginalis and fluid absorption by the
draining the lymphatic vessels present in the parietal layer.
There are mainly two types of hydroceles-
Communicating hydroceles: It is caused from exogenous sources. This type causes
indirect hernia.
Non-communicating hydroceles: It is developed due to the abnormal intrinsic scrotal
fluid shifts.
The hydroceles are positioned anterior and superior to the testis. Thus, hydrocele has a chance of
occurring bilaterally in 7-10 % of the cases. Thus, when it occurs on the right side of the body, it
can be easily linked with hernia. Usually most of the pediatric hydroceles are congenital. When
hydrocele occurs in the cord, it is often associated with failure of processus vaginalis to close
2PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
efficiently, which allows pooling of the fluid in the middle of the spermatic cord. Similarly,
communicating hydrocele occurs due to the failed closing of the processus vaginalis at the
internal ring of the testis, which results in the accumulation of the peritoneal fluid. Hydrocele
might result from medical conditions like epididymitis, orchitis, testicular torsion, or from local
injuries, or processes like radiotherapy, and can cause tuberculosis or infections like filariasis, in
adult males. There are almost no significant and visible symptoms other than hernia, or an
infection, only in cases of acute hydrocele. This condition is known to adversely affect fertility
(Beard et al., 2015). Thus, surgery is the best treatment procedure available for individuals
suffering from chronic hydrocele, in order to expose the secretory surface of the tunica vaginalis.
PART B:
Medical Sonography of the disease:
Hydrocele can be detected by several medical screening procedures like Inguinal-Scrotal
Imaging Ultrasound, Testicular Scintigraphy, and the most opted procedure for this condition -
Doppler Ultrasonography.
Imaging ultrasound like the Inguinal Scrotal imaging ultrasound usually is used to confirm the
diagnosis of Hydrocele formation. This test is very suitable for cases involving the testicular pain
or bleeding, to help differentiate between an incarcerated bowel and hydrocele. Another
screening method used is testicular scintigraphy, which is a nuclear scan useful for detecting
testicular torsion, usually in children (Siviero et al., 2019).
The type of sonography method which was observed is Doppler ultrasonography. This is the
most widely accepted color imaging method used to evaluate any medical condition related to
efficiently, which allows pooling of the fluid in the middle of the spermatic cord. Similarly,
communicating hydrocele occurs due to the failed closing of the processus vaginalis at the
internal ring of the testis, which results in the accumulation of the peritoneal fluid. Hydrocele
might result from medical conditions like epididymitis, orchitis, testicular torsion, or from local
injuries, or processes like radiotherapy, and can cause tuberculosis or infections like filariasis, in
adult males. There are almost no significant and visible symptoms other than hernia, or an
infection, only in cases of acute hydrocele. This condition is known to adversely affect fertility
(Beard et al., 2015). Thus, surgery is the best treatment procedure available for individuals
suffering from chronic hydrocele, in order to expose the secretory surface of the tunica vaginalis.
PART B:
Medical Sonography of the disease:
Hydrocele can be detected by several medical screening procedures like Inguinal-Scrotal
Imaging Ultrasound, Testicular Scintigraphy, and the most opted procedure for this condition -
Doppler Ultrasonography.
Imaging ultrasound like the Inguinal Scrotal imaging ultrasound usually is used to confirm the
diagnosis of Hydrocele formation. This test is very suitable for cases involving the testicular pain
or bleeding, to help differentiate between an incarcerated bowel and hydrocele. Another
screening method used is testicular scintigraphy, which is a nuclear scan useful for detecting
testicular torsion, usually in children (Siviero et al., 2019).
The type of sonography method which was observed is Doppler ultrasonography. This is the
most widely accepted color imaging method used to evaluate any medical condition related to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
acute swelling of the scrotum. In cases of Hydrocele formation, the sonography test demonstrates
the conditions of a normal parenchyma as well as its condition in cases of torsion or hernia. This
method is indicates the decrease in the blood flow in the orchitis or in the testicular torsion. This
has a specificity of 90-100%and a sensitivity of 86-88 % (Kühn et al., 2016). The method allows
the measurement of the testicular volume, which will help detect any abnormalities in the gonad
size, if there is any.
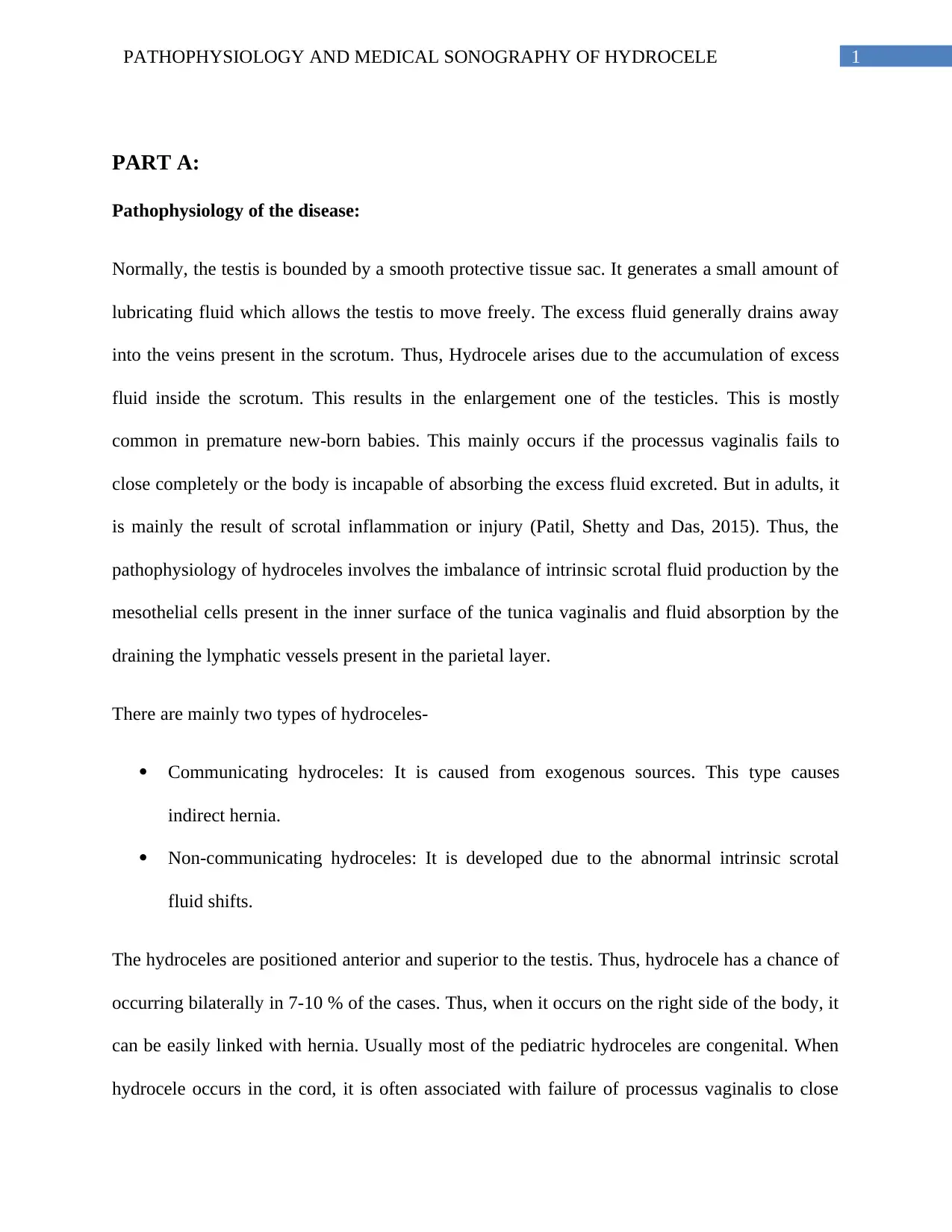
Figure 1: The above image depicts what happens in the case of Inguinal Hernia and
Communicating testicular Hydrocele.
Source: (Parks and Leung, 2013)
The following image is the image of the Doppler Sonography of a normal testis:
Figure 2: This image is the ultrasonography of a normal testis. Here, the peritoneal fluid is
present in a smaller amount, enough for the movement of the testis.
Source: (Mak, Chee Wai, Tzeng, and Wen-Sheng, 2012)
acute swelling of the scrotum. In cases of Hydrocele formation, the sonography test demonstrates
the conditions of a normal parenchyma as well as its condition in cases of torsion or hernia. This
method is indicates the decrease in the blood flow in the orchitis or in the testicular torsion. This
has a specificity of 90-100%and a sensitivity of 86-88 % (Kühn et al., 2016). The method allows
the measurement of the testicular volume, which will help detect any abnormalities in the gonad
size, if there is any.
Figure 1: The above image depicts what happens in the case of Inguinal Hernia and
Communicating testicular Hydrocele.
Source: (Parks and Leung, 2013)
The following image is the image of the Doppler Sonography of a normal testis:
Figure 2: This image is the ultrasonography of a normal testis. Here, the peritoneal fluid is
present in a smaller amount, enough for the movement of the testis.
Source: (Mak, Chee Wai, Tzeng, and Wen-Sheng, 2012)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
5PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
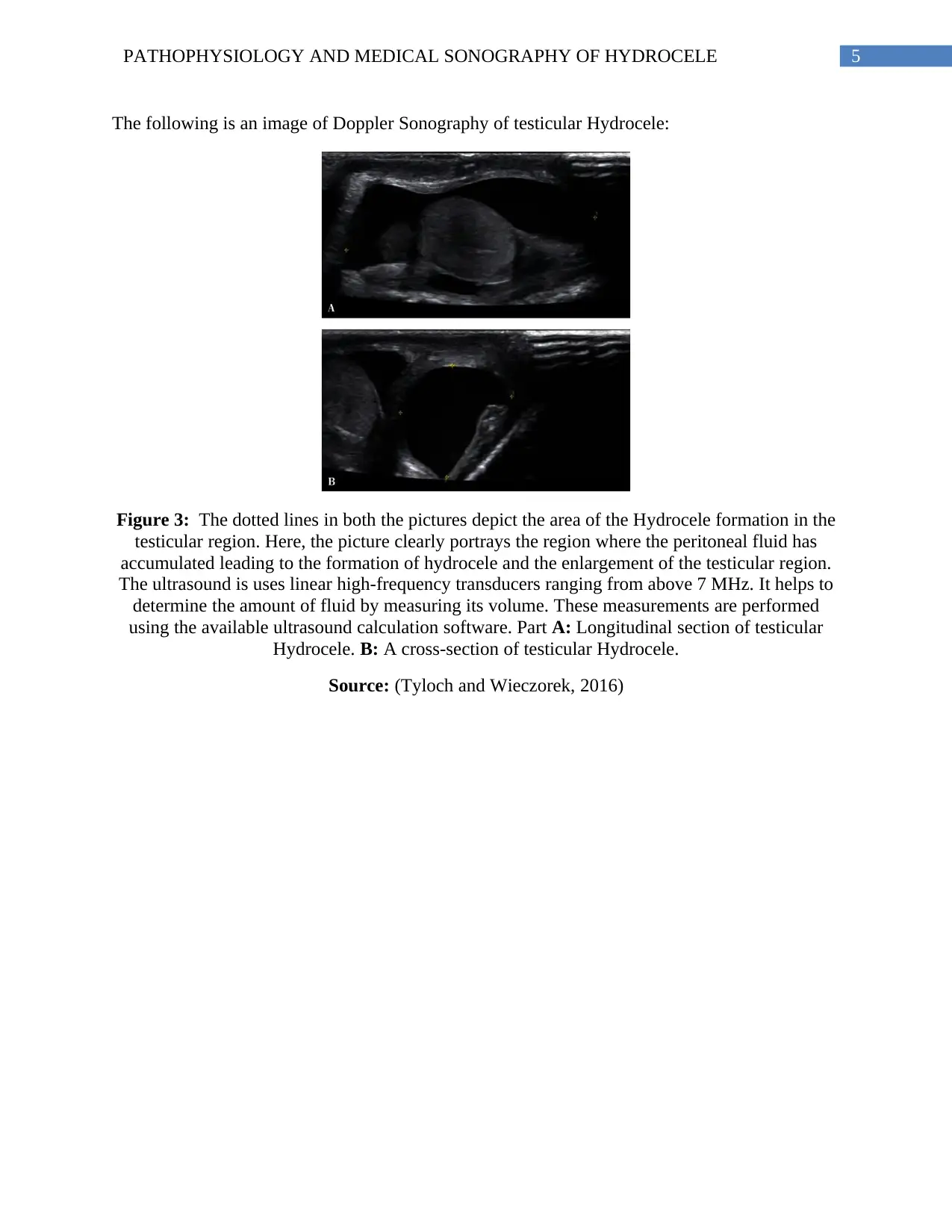
The following is an image of Doppler Sonography of testicular Hydrocele:
Figure 3: The dotted lines in both the pictures depict the area of the Hydrocele formation in the
testicular region. Here, the picture clearly portrays the region where the peritoneal fluid has
accumulated leading to the formation of hydrocele and the enlargement of the testicular region.
The ultrasound is uses linear high-frequency transducers ranging from above 7 MHz. It helps to
determine the amount of fluid by measuring its volume. These measurements are performed
using the available ultrasound calculation software. Part A: Longitudinal section of testicular
Hydrocele. B: A cross-section of testicular Hydrocele.
Source: (Tyloch and Wieczorek, 2016)
The following is an image of Doppler Sonography of testicular Hydrocele:
Figure 3: The dotted lines in both the pictures depict the area of the Hydrocele formation in the
testicular region. Here, the picture clearly portrays the region where the peritoneal fluid has
accumulated leading to the formation of hydrocele and the enlargement of the testicular region.
The ultrasound is uses linear high-frequency transducers ranging from above 7 MHz. It helps to
determine the amount of fluid by measuring its volume. These measurements are performed
using the available ultrasound calculation software. Part A: Longitudinal section of testicular
Hydrocele. B: A cross-section of testicular Hydrocele.
Source: (Tyloch and Wieczorek, 2016)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PATHOPHYSIOLOGY AND MEDICAL SONOGRAPHY OF HYDROCELE
References
Beard, J., Ohene-Yeboah, M., devries, C. and Schecter, W. (2015). Hernia and Hydrocele.
[online] Ncbi.nlm.nih.gov. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK333501/ [Accessed 12 Jul. 2019].
Kühn, A., Scortegagna, E., Nowitzki, K. and Kim, Y. (2016). Ultrasonography of the scrotum in
adults. Ultrasonography, 35(3), pp.180-197.
Mak, Chee Wai and Tzeng, Wen-Sheng. (2012). Sonography of the Scrotum. 10.5772/27586.
Parks, K. and Leung, L. (2013). Recurrent hydrocoele. Journal of Family Medicine and Primary
Care, 2(1), p.109.
Patil, V., Shetty, S. and Das, S. (2015). Common and Uncommon Presentation of Fluid within
the Scrotal Spaces. Ultrasound International Open, 01(02), pp.E34-E40.
Siviero, I., Méio, I., Ferrante, S., Forny, D. and Cunha, A. (2019). Torsion of a
Communicating Hydrocele Presented as Acute Scrotum: A Case Report and Literature
Review. [online] Dx.doi.org. Available at: http://dx.doi.org/10.1155/2016/7236104
[Accessed 12 Jul. 2019].
Tyloch, J. and Wieczorek, A. (2016). Standardy badania ultrasonograficznego moszny. Journal
of Ultrasonography, 16(67), pp.391-403.
References
Beard, J., Ohene-Yeboah, M., devries, C. and Schecter, W. (2015). Hernia and Hydrocele.
[online] Ncbi.nlm.nih.gov. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK333501/ [Accessed 12 Jul. 2019].
Kühn, A., Scortegagna, E., Nowitzki, K. and Kim, Y. (2016). Ultrasonography of the scrotum in
adults. Ultrasonography, 35(3), pp.180-197.
Mak, Chee Wai and Tzeng, Wen-Sheng. (2012). Sonography of the Scrotum. 10.5772/27586.
Parks, K. and Leung, L. (2013). Recurrent hydrocoele. Journal of Family Medicine and Primary
Care, 2(1), p.109.
Patil, V., Shetty, S. and Das, S. (2015). Common and Uncommon Presentation of Fluid within
the Scrotal Spaces. Ultrasound International Open, 01(02), pp.E34-E40.
Siviero, I., Méio, I., Ferrante, S., Forny, D. and Cunha, A. (2019). Torsion of a
Communicating Hydrocele Presented as Acute Scrotum: A Case Report and Literature
Review. [online] Dx.doi.org. Available at: http://dx.doi.org/10.1155/2016/7236104
[Accessed 12 Jul. 2019].
Tyloch, J. and Wieczorek, A. (2016). Standardy badania ultrasonograficznego moszny. Journal
of Ultrasonography, 16(67), pp.391-403.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.