Hypercholesterolemia and Statins: A Comprehensive Report on Treatment
VerifiedAdded on 2022/08/27
|11
|2605
|17
Report
AI Summary
This report provides a comprehensive overview of hypercholesterolemia and its treatment with statins. It begins by defining cholesterol and its functions, differentiating between LDL and HDL cholesterol, and explaining how elevated LDL levels lead to hypercholesterolemia and atherosclerosis. The pathophysiology section details the process of plaque formation in arteries, the role of endothelial cells, and the factors contributing to hypercholesterolemia, including genetic predisposition and lifestyle choices. The pharmacology section focuses on statins, explaining their mechanism of action as HMG-CoA reductase inhibitors, their impact on cholesterol synthesis, and their effects on LDL receptors. The report also discusses the relevance of statins in clinical practice, emphasizing the importance of lifestyle modifications like diet and exercise, and the benefits of statin therapy in reducing cardiovascular risks. The report concludes by highlighting the importance of both medical and non-medical interventions in managing hypercholesterolemia and reducing associated health risks.
Running Head: HYPERCHOLESTEROLEMIA AND STATINS 1
HYPERCHOLESTEROLEMIA AND STATINS
Topic 8
Student Name:
Student Number:
Date:
HYPERCHOLESTEROLEMIA AND STATINS
Topic 8
Student Name:
Student Number:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HYPERCHOLESTEROLEMIA AND STATINS 2
ABSTRACT
Cholesterol is a fatty substance present naturally in the body. Cholesterol is known to
perform several vital functions in the body that is needed for converting certain hormones.
Fats and cholesterols are absorbed in the intestines and then taken to the liver where the fats
get transformed into cholesterol and are released into the bloodstream. There are two types of
cholesterol, that is “low-density lipoprotein (LDL) cholesterol” and “high-density lipoprotein
cholesterol”. High levels of “LDL” cholesterol are referred to as “hypercholesterolemia”,
which is linked to atherosclerosis. The benefits of statin drugs in reducing cardiovascular
events has often led to treating “hypercholesterolemia”. Homeostasis of statin leads to a
favorable impact on lipids with a tremendous reduction in fibrinogen and high-sensitivity
CRP levels. The current scope of discussion relates to the normal physiology,
pathophysiology, and pharmacology of “hypercholesterolemia” and statins.
“Hypercholesterolemia” is known to compound several risk factors for cardiovascular
diseases. Lowering its levels by medication interventions such as statins can have significant
improvement in outcomes. Similarly, other non-medical interventions including lifestyle
changes can help improve levels of “LDL” and reduce risks from “hypercholesterolemia”
with its associated comorbidities and mortalities as well.
ABSTRACT
Cholesterol is a fatty substance present naturally in the body. Cholesterol is known to
perform several vital functions in the body that is needed for converting certain hormones.
Fats and cholesterols are absorbed in the intestines and then taken to the liver where the fats
get transformed into cholesterol and are released into the bloodstream. There are two types of
cholesterol, that is “low-density lipoprotein (LDL) cholesterol” and “high-density lipoprotein
cholesterol”. High levels of “LDL” cholesterol are referred to as “hypercholesterolemia”,
which is linked to atherosclerosis. The benefits of statin drugs in reducing cardiovascular
events has often led to treating “hypercholesterolemia”. Homeostasis of statin leads to a
favorable impact on lipids with a tremendous reduction in fibrinogen and high-sensitivity
CRP levels. The current scope of discussion relates to the normal physiology,
pathophysiology, and pharmacology of “hypercholesterolemia” and statins.
“Hypercholesterolemia” is known to compound several risk factors for cardiovascular
diseases. Lowering its levels by medication interventions such as statins can have significant
improvement in outcomes. Similarly, other non-medical interventions including lifestyle
changes can help improve levels of “LDL” and reduce risks from “hypercholesterolemia”
with its associated comorbidities and mortalities as well.
HYPERCHOLESTEROLEMIA AND STATINS 3
CONTENTS
Abstract......................................................................................................................................2
Introduction................................................................................................................................4
Pathophysiology.........................................................................................................................4
Pharmacology.............................................................................................................................6
Relevance to practice.................................................................................................................7
Conclusion..................................................................................................................................8
References..................................................................................................................................8
CONTENTS
Abstract......................................................................................................................................2
Introduction................................................................................................................................4
Pathophysiology.........................................................................................................................4
Pharmacology.............................................................................................................................6
Relevance to practice.................................................................................................................7
Conclusion..................................................................................................................................8
References..................................................................................................................................8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HYPERCHOLESTEROLEMIA AND STATINS 4
INTRODUCTION
Cholesterol is a fatty substance present naturally in the body. Cholesterol is known to
perform several vital functions in the body that is needed for converting certain hormones.
Fats and cholesterols are absorbed in the intestines and then taken to the liver where the fats
get transformed into cholesterol and are released into the bloodstream. There are two types of
cholesterol, that is “low-density lipoprotein (LDL) cholesterol” and “high-density lipoprotein
cholesterol” (Ruel et al, 2018). High levels of “LDL” cholesterol are referred to as
“hypercholesterolemia”, which is linked to atherosclerosis. Normal physiology of
“hypercholesterolemia” is when a patient has elevated levels of “LDL” cholesterol. Patients
with the genetic disposition of high cholesterol are often given cholesterol-lowering
medication such as statins for decreasing risks. The benefits of statin drugs in reducing
cardiovascular events have often led to treating “hypercholesterolemia” (Besseling et al,
2016). Homeostasis of “hypercholesterolemia” is carried by a process of biosynthesis using
“3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGR)” activity. Which uptakes using
“low-density lipoprotein receptors” (“LDLr”), storage of esterification, “lipoprotein” release
in the blood and degrading as well as conversion into bile acids. Homeostasis of statin leads
to a favorable impact on lipids with a tremendous reduction in fibrinogen and high-sensitivity
CRP levels. The current scope of discussion relates to the normal physiology,
pathophysiology, and pharmacology of “hypercholesterolemia” and statins.
PATHOPHYSIOLOGY
Cholesterol comprises a lipophilic molecule important for the normal functioning of cells.
While cholesterol has many important functions in the body most of them are lipophilic and
transported through blood with triglycerides in lipoprotein particles. “Hypercholesterolemia”
is a situation when cholesterol has reached abnormal blood concentration (Huff, & Jialal,
2019). It leads to a risk of premature atherosclerotic cardiovascular diseases (ASCVD)
increases to a substantial level. “Hypercholesterolemia” or high levels of “LDL”-cholesterol
is one of the leading risk factors that lead to forming atherosclerotic plaques (Soslowsky, &
Fryhofer, 2016). Formation of these plaques leads to varied clinical outcomes, such as
coronary artery diseases, aortic aneurysms, PAD, and risks from a stroke. High levels of
“LDL” in the blood lead to the risk of the atherosclerotic lesion. Increases HDL in the blood
INTRODUCTION
Cholesterol is a fatty substance present naturally in the body. Cholesterol is known to
perform several vital functions in the body that is needed for converting certain hormones.
Fats and cholesterols are absorbed in the intestines and then taken to the liver where the fats
get transformed into cholesterol and are released into the bloodstream. There are two types of
cholesterol, that is “low-density lipoprotein (LDL) cholesterol” and “high-density lipoprotein
cholesterol” (Ruel et al, 2018). High levels of “LDL” cholesterol are referred to as
“hypercholesterolemia”, which is linked to atherosclerosis. Normal physiology of
“hypercholesterolemia” is when a patient has elevated levels of “LDL” cholesterol. Patients
with the genetic disposition of high cholesterol are often given cholesterol-lowering
medication such as statins for decreasing risks. The benefits of statin drugs in reducing
cardiovascular events have often led to treating “hypercholesterolemia” (Besseling et al,
2016). Homeostasis of “hypercholesterolemia” is carried by a process of biosynthesis using
“3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGR)” activity. Which uptakes using
“low-density lipoprotein receptors” (“LDLr”), storage of esterification, “lipoprotein” release
in the blood and degrading as well as conversion into bile acids. Homeostasis of statin leads
to a favorable impact on lipids with a tremendous reduction in fibrinogen and high-sensitivity
CRP levels. The current scope of discussion relates to the normal physiology,
pathophysiology, and pharmacology of “hypercholesterolemia” and statins.
PATHOPHYSIOLOGY
Cholesterol comprises a lipophilic molecule important for the normal functioning of cells.
While cholesterol has many important functions in the body most of them are lipophilic and
transported through blood with triglycerides in lipoprotein particles. “Hypercholesterolemia”
is a situation when cholesterol has reached abnormal blood concentration (Huff, & Jialal,
2019). It leads to a risk of premature atherosclerotic cardiovascular diseases (ASCVD)
increases to a substantial level. “Hypercholesterolemia” or high levels of “LDL”-cholesterol
is one of the leading risk factors that lead to forming atherosclerotic plaques (Soslowsky, &
Fryhofer, 2016). Formation of these plaques leads to varied clinical outcomes, such as
coronary artery diseases, aortic aneurysms, PAD, and risks from a stroke. High levels of
“LDL” in the blood lead to the risk of the atherosclerotic lesion. Increases HDL in the blood
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HYPERCHOLESTEROLEMIA AND STATINS 5
is related to the risk factor in epidemiological studies with no results in clinical trials.
Atherosclerotic plaques start damaging the endothelial cells which further leads to
dysfunction of such cells (Yoo, 2016). This leads to increased “LDL” particles permeating
through vascular walls. Lipoprotein (such as “LDL”) can accumulate in the vessels within the
cellular matrix in the intima. Then “LDL” is changed and taken up receptors on macrophages
leading to the foal-cell formation. With more lipids accumulating in the vessel walls, smooth
muscle cells start migrating to the lesion. These smooth muscles take up the plaque
formation, by stopping the lipid core to be exposed to the vessel’s lumen (Okuyama et al,
2015). Resulting in decreasing blood flow distally and leading to ischemia. Abundant lipids
along with macrophages rupture forming thrombus that can totality that can block blood flow
as it takes place in unstable angina or acute myocardial infarctions.
“Hypercholesterolemia” condition might also include “very-low-density lipoprotein
(VLDL)” with intermediate-density “lipoprotein (IDL)”, which is “HDL” cholesterol. The
factors which cause “hypercholesterolemia” include genetic factors, stress, diet, medications,
sedentary lifestyle and other disorders such as hypothyroidism and nephrotic syndrome (Cid-
Conde, & López-Castro, 2015). Often genetic defects regulate “LDL” receptors in the liver
leading to increased “LDL” levels in the blood. While “LDL” receptors mediate “LDL”
uptake in the liver, endocytosis of “LDL” is the method by which “LDL” is decreased in the
body. Patients with a genetic disposition for high cholesterol can be placed on statins, which
are cholesterol-lowering drugs for decreasing their levels of risks related to diseases of the
artery.
Statins are microorganism derive drugs which impairs the cellular synthesis of cholesterol
by way of competitive inhibiting of HMG-CoA reductase enzymes. Statins have capabilities
to lower the blood levels of cholesterol by enhancing high-affinity receptors that recognize
plasma “LDL”. Statins decrease “VLDL” synthesis rates in the liver. Mild triglyceride has a
reducing effect of these drugs. Statin has shown efficiency in reducing plasma cholesterol
concentrations as against bile acid-binding polymers (Bergheanu, Bodde, & Jukema, 2017). It
is considered better when compared to nicotinic acids and fibrates, they are also well
tolerated in comparison to other drugs but considerably less effective in lowering plasma
triglycerides or increasing HDL cholesterol concentrations. Patients of
“hypercholesterolemia” can also be treated by providing a variable diet low in saturated fats
and trans fats. As dietary “LDL” has a significant contribution to “LDL” concentrations.
Lifestyle changes including regular aerobic exercises might also help in reducing levels of
is related to the risk factor in epidemiological studies with no results in clinical trials.
Atherosclerotic plaques start damaging the endothelial cells which further leads to
dysfunction of such cells (Yoo, 2016). This leads to increased “LDL” particles permeating
through vascular walls. Lipoprotein (such as “LDL”) can accumulate in the vessels within the
cellular matrix in the intima. Then “LDL” is changed and taken up receptors on macrophages
leading to the foal-cell formation. With more lipids accumulating in the vessel walls, smooth
muscle cells start migrating to the lesion. These smooth muscles take up the plaque
formation, by stopping the lipid core to be exposed to the vessel’s lumen (Okuyama et al,
2015). Resulting in decreasing blood flow distally and leading to ischemia. Abundant lipids
along with macrophages rupture forming thrombus that can totality that can block blood flow
as it takes place in unstable angina or acute myocardial infarctions.
“Hypercholesterolemia” condition might also include “very-low-density lipoprotein
(VLDL)” with intermediate-density “lipoprotein (IDL)”, which is “HDL” cholesterol. The
factors which cause “hypercholesterolemia” include genetic factors, stress, diet, medications,
sedentary lifestyle and other disorders such as hypothyroidism and nephrotic syndrome (Cid-
Conde, & López-Castro, 2015). Often genetic defects regulate “LDL” receptors in the liver
leading to increased “LDL” levels in the blood. While “LDL” receptors mediate “LDL”
uptake in the liver, endocytosis of “LDL” is the method by which “LDL” is decreased in the
body. Patients with a genetic disposition for high cholesterol can be placed on statins, which
are cholesterol-lowering drugs for decreasing their levels of risks related to diseases of the
artery.
Statins are microorganism derive drugs which impairs the cellular synthesis of cholesterol
by way of competitive inhibiting of HMG-CoA reductase enzymes. Statins have capabilities
to lower the blood levels of cholesterol by enhancing high-affinity receptors that recognize
plasma “LDL”. Statins decrease “VLDL” synthesis rates in the liver. Mild triglyceride has a
reducing effect of these drugs. Statin has shown efficiency in reducing plasma cholesterol
concentrations as against bile acid-binding polymers (Bergheanu, Bodde, & Jukema, 2017). It
is considered better when compared to nicotinic acids and fibrates, they are also well
tolerated in comparison to other drugs but considerably less effective in lowering plasma
triglycerides or increasing HDL cholesterol concentrations. Patients of
“hypercholesterolemia” can also be treated by providing a variable diet low in saturated fats
and trans fats. As dietary “LDL” has a significant contribution to “LDL” concentrations.
Lifestyle changes including regular aerobic exercises might also help in reducing levels of

HYPERCHOLESTEROLEMIA AND STATINS 6
“LDL” in the blood. However, in conjunction with these lifestyle changes, lipid-lowering
drugs such as statins are used for patients with high risk.
Statins are known to support reducing “LDL”-c which in turn reduces atherosclerotic
cardiovascular diseases. It is not only used for lowering “LDL”-c but also in reducing
cardiovascular mortality and morbidity rates using primary and secondary intervention
mechanisms. Recent researches depict that usage of statins in adults aged years and above in
patients with elevated atherosclerotic CVD risk has benefits of “LDL”-c reduction with every
1 mmol/L reduction associated with a 22% reduction in coronary and vascular events.
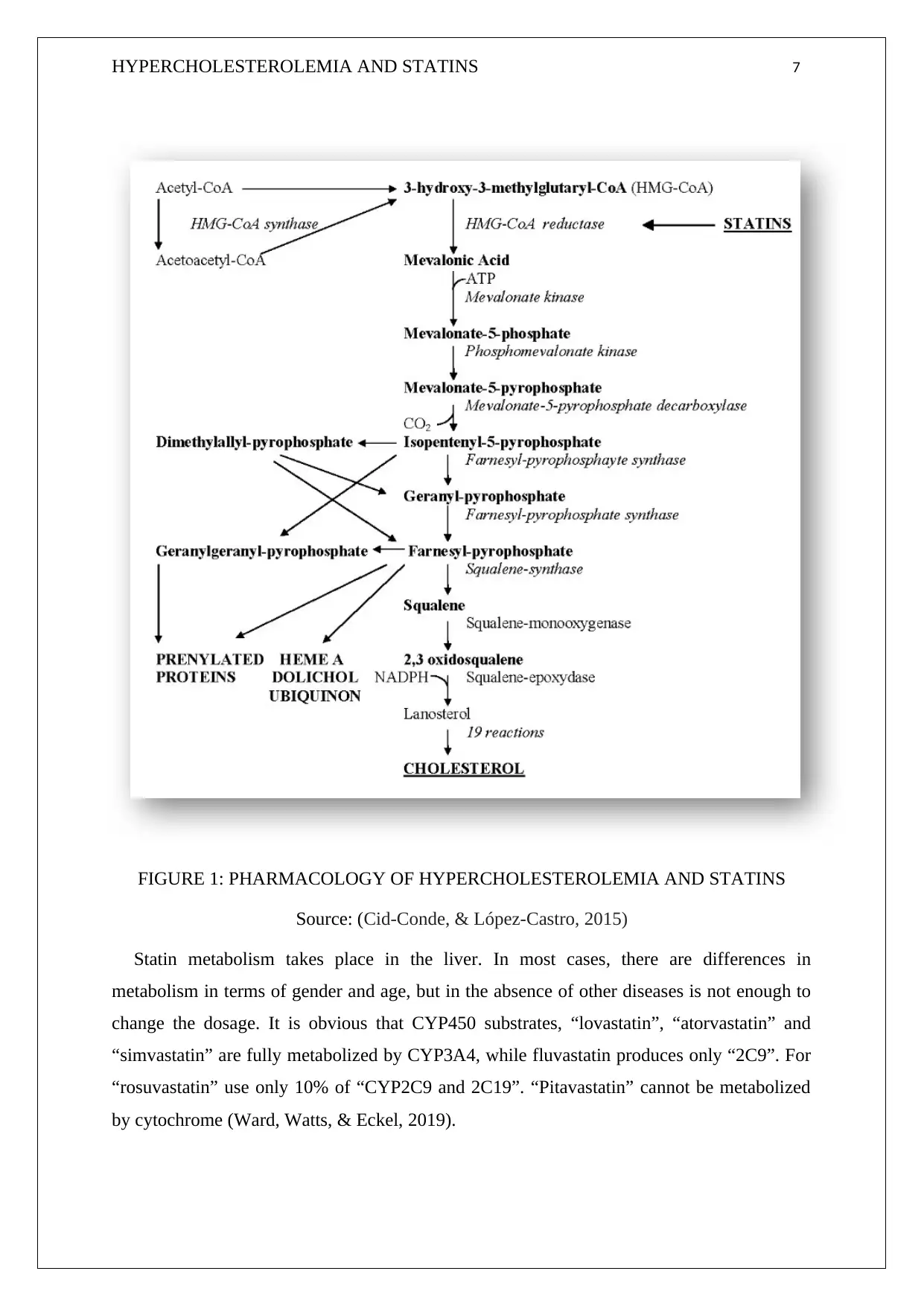
PHARMACOLOGY
Statins are a known group of drugs that are used for treating patients suffering from
“hypercholesterolemia”. It is used to lower levels of cholesterol in patients with increased
risk of cardiovascular diseases. Statins function by competitively blocking the site and key
rate-limiting enzyme in the “mevalonate pathway”.
“LDL” in the blood. However, in conjunction with these lifestyle changes, lipid-lowering
drugs such as statins are used for patients with high risk.
Statins are known to support reducing “LDL”-c which in turn reduces atherosclerotic
cardiovascular diseases. It is not only used for lowering “LDL”-c but also in reducing
cardiovascular mortality and morbidity rates using primary and secondary intervention
mechanisms. Recent researches depict that usage of statins in adults aged years and above in
patients with elevated atherosclerotic CVD risk has benefits of “LDL”-c reduction with every
1 mmol/L reduction associated with a 22% reduction in coronary and vascular events.
PHARMACOLOGY
Statins are a known group of drugs that are used for treating patients suffering from
“hypercholesterolemia”. It is used to lower levels of cholesterol in patients with increased
risk of cardiovascular diseases. Statins function by competitively blocking the site and key
rate-limiting enzyme in the “mevalonate pathway”.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HYPERCHOLESTEROLEMIA AND STATINS 7
FIGURE 1: PHARMACOLOGY OF HYPERCHOLESTEROLEMIA AND STATINS
Source: (Cid-Conde, & López-Castro, 2015)
Statin metabolism takes place in the liver. In most cases, there are differences in
metabolism in terms of gender and age, but in the absence of other diseases is not enough to
change the dosage. It is obvious that CYP450 substrates, “lovastatin”, “atorvastatin” and
“simvastatin” are fully metabolized by CYP3A4, while fluvastatin produces only “2C9”. For
“rosuvastatin” use only 10% of “CYP2C9 and 2C19”. “Pitavastatin” cannot be metabolized
by cytochrome (Ward, Watts, & Eckel, 2019).
FIGURE 1: PHARMACOLOGY OF HYPERCHOLESTEROLEMIA AND STATINS
Source: (Cid-Conde, & López-Castro, 2015)
Statin metabolism takes place in the liver. In most cases, there are differences in
metabolism in terms of gender and age, but in the absence of other diseases is not enough to
change the dosage. It is obvious that CYP450 substrates, “lovastatin”, “atorvastatin” and
“simvastatin” are fully metabolized by CYP3A4, while fluvastatin produces only “2C9”. For
“rosuvastatin” use only 10% of “CYP2C9 and 2C19”. “Pitavastatin” cannot be metabolized
by cytochrome (Ward, Watts, & Eckel, 2019).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HYPERCHOLESTEROLEMIA AND STATINS 8
Statins are “3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase”. The
enzyme catalyzes “HMG-CoA to mevalonate”, an important metabolite for cholesterol
biosynthesis. Blocking arises due to the high structural similarity of these drugs exhibit by
HMG-CoA. Statin affinity is 1,000 to 10,000 times greater than the natural substrate.
Enzyme inhibitors lead to reducing the fraction of cholesterol in the blood impacting
positive intervention on cardiovascular risk factors. All statins are orally used and absorbed in
this manner. However, lovastatin and pravastatin have decreased absorption in the case of
food being present in the stomach (Borghi, Urso, & Cicero, 2017). Blocking cholesterol
synthesis in the liver leads to the activation of the SREBP-regulating protein, which activates
protein transcription, which leads to an increase in the number of higher expressions of
“LDL” receptors and increasing functional receptors on hepatocytes. Also, statins have been
shown to produce the function of lymphocytes inhibiting associated antigen-1.
Along with the reduction in “LDL”-c along with cardiovascular mortality and morbidity
rates, statins have an additional non-lipid related pleiotropic impact (Petyaev, 2015). This
pharmacology is associated with improvements in endothelial functions, stabilizing
atherosclerotic plaques, immunomodulatory, anti-inflammatory and antithrombotic effects
with impacts on bone metabolism and reduced risks of dementia.
RELEVANCE TO PRACTICE
“Hypercholesterolemia” is associated with too much bad cholesterol in the blood and it
can lead to risks of fatty deposits in the arteries and blockages. Changing behaviors, in this
case, might help to improve the cholesterol levels. Eating healthy is a way in which
cholesterol is reduced, by consuming less of trans fats and saturated fats. Limiting the intake
of red meat and dairy products made from whole milk, also limiting the intake of fried foods
and cooking with healthy oils can reduce cholesterol. Having a heart-healthy diet with
vegetables, fruits, whole grains, fish, poultry, and nuts, and curbing sugary foods and
beverages can help in reducing cholesterol. A sedentary lifestyle is known to increase “LDL”
in the arteries. Being physically active can lead to a reduction in cholesterol. Practicing
moderate-intensity aerobic exercise weekly or brisk walking, bicycling, swimming can assist
in maintaining or lowering levels of cholesterol.
By quitting smoking, individuals can significantly lower risks from coronary heart
diseases. Smoking is also known to compound risk factors for diabetes and high blood
Statins are “3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase”. The
enzyme catalyzes “HMG-CoA to mevalonate”, an important metabolite for cholesterol
biosynthesis. Blocking arises due to the high structural similarity of these drugs exhibit by
HMG-CoA. Statin affinity is 1,000 to 10,000 times greater than the natural substrate.
Enzyme inhibitors lead to reducing the fraction of cholesterol in the blood impacting
positive intervention on cardiovascular risk factors. All statins are orally used and absorbed in
this manner. However, lovastatin and pravastatin have decreased absorption in the case of
food being present in the stomach (Borghi, Urso, & Cicero, 2017). Blocking cholesterol
synthesis in the liver leads to the activation of the SREBP-regulating protein, which activates
protein transcription, which leads to an increase in the number of higher expressions of
“LDL” receptors and increasing functional receptors on hepatocytes. Also, statins have been
shown to produce the function of lymphocytes inhibiting associated antigen-1.
Along with the reduction in “LDL”-c along with cardiovascular mortality and morbidity
rates, statins have an additional non-lipid related pleiotropic impact (Petyaev, 2015). This
pharmacology is associated with improvements in endothelial functions, stabilizing
atherosclerotic plaques, immunomodulatory, anti-inflammatory and antithrombotic effects
with impacts on bone metabolism and reduced risks of dementia.
RELEVANCE TO PRACTICE
“Hypercholesterolemia” is associated with too much bad cholesterol in the blood and it
can lead to risks of fatty deposits in the arteries and blockages. Changing behaviors, in this
case, might help to improve the cholesterol levels. Eating healthy is a way in which
cholesterol is reduced, by consuming less of trans fats and saturated fats. Limiting the intake
of red meat and dairy products made from whole milk, also limiting the intake of fried foods
and cooking with healthy oils can reduce cholesterol. Having a heart-healthy diet with
vegetables, fruits, whole grains, fish, poultry, and nuts, and curbing sugary foods and
beverages can help in reducing cholesterol. A sedentary lifestyle is known to increase “LDL”
in the arteries. Being physically active can lead to a reduction in cholesterol. Practicing
moderate-intensity aerobic exercise weekly or brisk walking, bicycling, swimming can assist
in maintaining or lowering levels of cholesterol.
By quitting smoking, individuals can significantly lower risks from coronary heart
diseases. Smoking is also known to compound risk factors for diabetes and high blood

HYPERCHOLESTEROLEMIA AND STATINS 9
pressure. Quitting smoking can help lower cholesterol levels and non-smokers need to avoid
passive smoking. Losing weight also significantly affects levels of “LDL” in the blood. Being
obese or overweight increases “LDL”. Losing excess weight can assist in improving levels of
cholesterols.
CONCLUSION
In conclusion, “hypercholesterolemia” is known to compound several risk factors for
cardiovascular diseases. Lowering its levels by medication interventions such as statins can
have significant improvement in outcomes. Similarly, other non-medical interventions
including lifestyle changes can help improve levels of “LDL” and reduce risks from
“hypercholesterolemia” with its associated comorbidities and mortalities as well.
pressure. Quitting smoking can help lower cholesterol levels and non-smokers need to avoid
passive smoking. Losing weight also significantly affects levels of “LDL” in the blood. Being
obese or overweight increases “LDL”. Losing excess weight can assist in improving levels of
cholesterols.
CONCLUSION
In conclusion, “hypercholesterolemia” is known to compound several risk factors for
cardiovascular diseases. Lowering its levels by medication interventions such as statins can
have significant improvement in outcomes. Similarly, other non-medical interventions
including lifestyle changes can help improve levels of “LDL” and reduce risks from
“hypercholesterolemia” with its associated comorbidities and mortalities as well.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HYPERCHOLESTEROLEMIA AND STATINS 10
REFERENCES
Bergheanu, S. C., Bodde, M. C., & Jukema, J. W. (2017). Pathophysiology and treatment of
atherosclerosis. Netherlands Heart Journal, 25(4), 231-242. DOI: 10.1007/s12471-017-
0959-2.
Besseling, J., Hovingh, G. K., Huijgen, R., Kastelein, J. J., & Hutten, B. A. (2016). Statins in
familial hypercholesterolemia: consequences for coronary artery disease and all-cause
mortality. Journal of the American College of Cardiology, 68(3), 252-260.
DOI: 10.1016/j.jacc.2016.04.054.
Borghi, C., Urso, R., & Cicero, A. F. (2017). Renin–angiotensin system at the crossroad of
hypertension and hypercholesterolemia. Nutrition, Metabolism and Cardiovascular
Diseases, 27(2), 115-120. DOI: 10.1016/j.numecd.2016.07.013.
Cid-Conde, L., & López-Castro, J. (2015). Hypercholesterolemia—Statin Therapy—
Indications, Side Effects, Common Mistakes in Handling, Last Evidence and
Recommendations in Current Clinical Practice. Hypercholesterolemia, 159.
Huff, T., & Jialal, I. (2019). Physiology, cholesterol.
Nabulsi, M. (2016). Role of DNA methyltransferase 3a (Dnmt3a) in the adaptation of
atherogenesis key players to proatherogenic environment (Doctoral dissertation,
Université Pierre et Marie Curie-Paris VI).
Okuyama, H., Langsjoen, P. H., Hamazaki, T., Ogushi, Y., Hama, R., Kobayashi, T., &
Uchino, H. (2015). Statins stimulate atherosclerosis and heart failure: pharmacological
mechanisms. Expert review of clinical pharmacology, 8(2), 189-199. DOI:
10.1586/17512433.2015.1011125.
REFERENCES
Bergheanu, S. C., Bodde, M. C., & Jukema, J. W. (2017). Pathophysiology and treatment of
atherosclerosis. Netherlands Heart Journal, 25(4), 231-242. DOI: 10.1007/s12471-017-
0959-2.
Besseling, J., Hovingh, G. K., Huijgen, R., Kastelein, J. J., & Hutten, B. A. (2016). Statins in
familial hypercholesterolemia: consequences for coronary artery disease and all-cause
mortality. Journal of the American College of Cardiology, 68(3), 252-260.
DOI: 10.1016/j.jacc.2016.04.054.
Borghi, C., Urso, R., & Cicero, A. F. (2017). Renin–angiotensin system at the crossroad of
hypertension and hypercholesterolemia. Nutrition, Metabolism and Cardiovascular
Diseases, 27(2), 115-120. DOI: 10.1016/j.numecd.2016.07.013.
Cid-Conde, L., & López-Castro, J. (2015). Hypercholesterolemia—Statin Therapy—
Indications, Side Effects, Common Mistakes in Handling, Last Evidence and
Recommendations in Current Clinical Practice. Hypercholesterolemia, 159.
Huff, T., & Jialal, I. (2019). Physiology, cholesterol.
Nabulsi, M. (2016). Role of DNA methyltransferase 3a (Dnmt3a) in the adaptation of
atherogenesis key players to proatherogenic environment (Doctoral dissertation,
Université Pierre et Marie Curie-Paris VI).
Okuyama, H., Langsjoen, P. H., Hamazaki, T., Ogushi, Y., Hama, R., Kobayashi, T., &
Uchino, H. (2015). Statins stimulate atherosclerosis and heart failure: pharmacological
mechanisms. Expert review of clinical pharmacology, 8(2), 189-199. DOI:
10.1586/17512433.2015.1011125.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HYPERCHOLESTEROLEMIA AND STATINS 11
Petyaev, I. M. (2015). Improvement of hepatic bioavailability as a new step for the future of
statin. Archives of medical science: AMS, 11(2), 406. doi: 10.5114/aoms.2015.50972.
Ruel, I., Aljenedil, S., Sadri, I., de Varennes, É., Hegele, R.A., Couture, P., Bergeron, J.,
Wanneh, E., Baass, A., Dufour, R. and Gaudet, D. (2018). Imputation of baseline LDL
cholesterol concentration in patients with familial hypercholesterolemia on statins or
ezetimibe. Clinical chemistry, 64(2), 355-362. DOI: 10.1373/clinchem.2017.279422
Soslowsky, L. J., & Fryhofer, G. W. (2016). Tendon homeostasis in hypercholesterolemia.
In Metabolic Influences on Risk for Tendon Disorders (pp. 151-165). Springer, Cham.
DOI: 10.1007/978-3-319-33943-6_14.
Ward, N. C., Watts, G. F., & Eckel, R. H. (2019). Statin toxicity: mechanistic insights and
clinical implications. Circulation Research, 124(2), 328-350. DOI:
10.1161/CIRCRESAHA.118.312782.
Yoo, E. G. (2016). Sitosterolemia: a review and update of pathophysiology, clinical
spectrum, diagnosis, and management. Annals of pediatric endocrinology &
metabolism, 21(1), 7. doi: 10.6065/apem.2016.21.1.7.
Petyaev, I. M. (2015). Improvement of hepatic bioavailability as a new step for the future of
statin. Archives of medical science: AMS, 11(2), 406. doi: 10.5114/aoms.2015.50972.
Ruel, I., Aljenedil, S., Sadri, I., de Varennes, É., Hegele, R.A., Couture, P., Bergeron, J.,
Wanneh, E., Baass, A., Dufour, R. and Gaudet, D. (2018). Imputation of baseline LDL
cholesterol concentration in patients with familial hypercholesterolemia on statins or
ezetimibe. Clinical chemistry, 64(2), 355-362. DOI: 10.1373/clinchem.2017.279422
Soslowsky, L. J., & Fryhofer, G. W. (2016). Tendon homeostasis in hypercholesterolemia.
In Metabolic Influences on Risk for Tendon Disorders (pp. 151-165). Springer, Cham.
DOI: 10.1007/978-3-319-33943-6_14.
Ward, N. C., Watts, G. F., & Eckel, R. H. (2019). Statin toxicity: mechanistic insights and
clinical implications. Circulation Research, 124(2), 328-350. DOI:
10.1161/CIRCRESAHA.118.312782.
Yoo, E. G. (2016). Sitosterolemia: a review and update of pathophysiology, clinical
spectrum, diagnosis, and management. Annals of pediatric endocrinology &
metabolism, 21(1), 7. doi: 10.6065/apem.2016.21.1.7.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





