Intracerebral Hemorrhagic Stroke: Case Study Analysis, Treatment
VerifiedAdded on 2022/08/22
|6
|1674
|55
Case Study
AI Summary
This case study focuses on an intracerebral hemorrhagic stroke (ICH) experienced by a 65-year-old patient, Karl Kennedy, with a history of hypertension. The assignment analyzes the patient's symptoms, including loss of speech, confusion, nausea, and impaired consciousness, linking them to the pathophysiology of ICH. The document explores the risk factors, aetiology, and the step-by-step sequence between aetiology and pathophysiology. It details the diagnostic investigations, such as CT scans and MRIs, and discusses treatment modalities aimed at controlling bleeding, reducing pressure, and rehabilitation. The analysis emphasizes the importance of early diagnosis and intervention in managing this medical emergency. The paper also highlights the role of hypertension and age as key risk factors and the potential for complications such as hydrocephalus and herniation. The student provides a comprehensive overview of the case, supported by evidence-based literature.

Running head: INTRACEREBRAL HAEMORRHAGIC STROKE 1
Intracerebral Haemorrhagic Stroke (ICH)
Student’s Name
(997 words)
Intracerebral Haemorrhagic Stroke (ICH)
Student’s Name
(997 words)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INTRACEREBRAL HAEMORRHAGIC STROKE 2
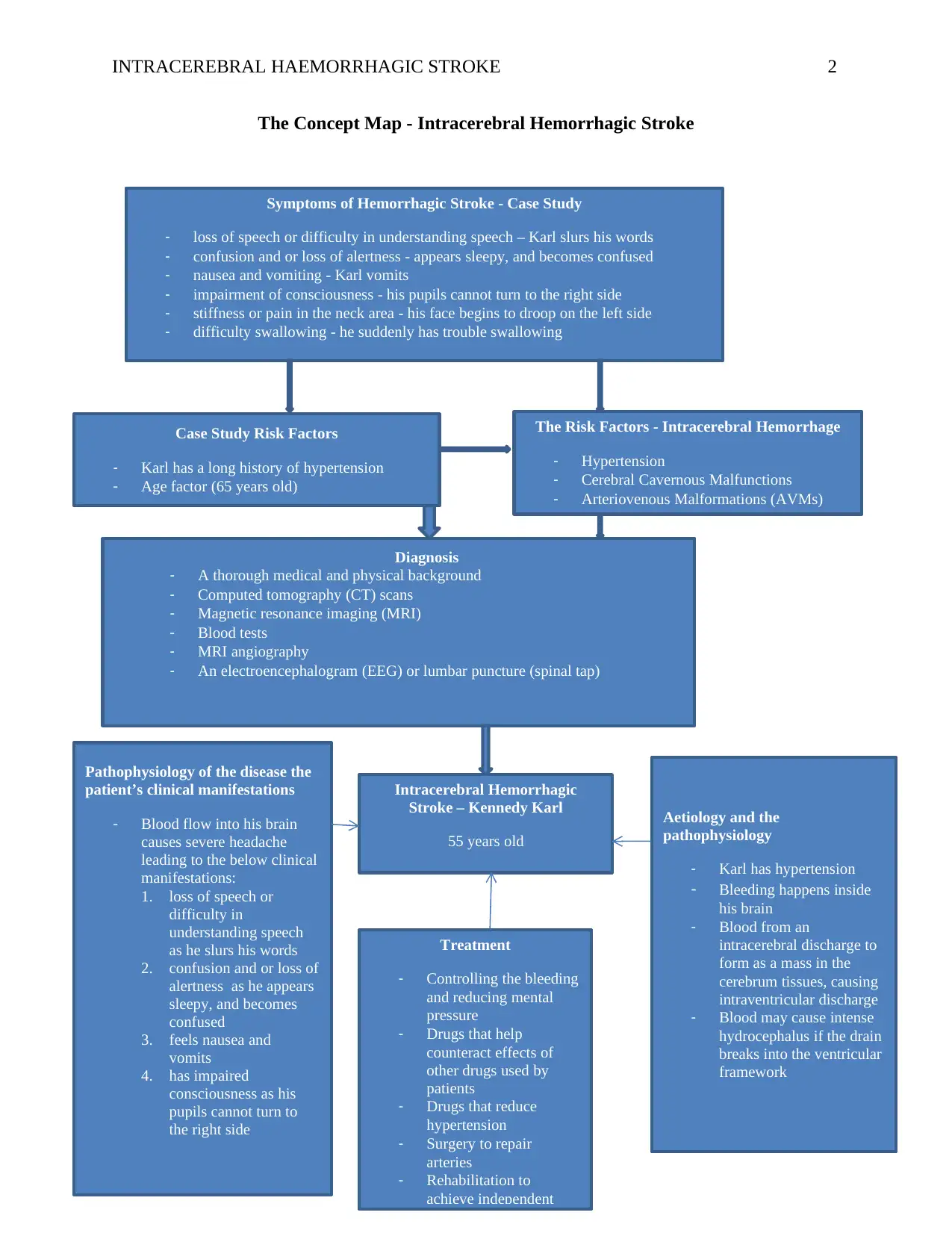
The Concept Map - Intracerebral Hemorrhagic Stroke
Intracerebral Hemorrhagic
Stroke – Kennedy Karl
55 years old
The Risk Factors - Intracerebral Hemorrhage
- Hypertension
- Cerebral Cavernous Malfunctions
- Arteriovenous Malformations (AVMs)
Diagnosis
- A thorough medical and physical background
- Computed tomography (CT) scans
- Magnetic resonance imaging (MRI)
- Blood tests
- MRI angiography
- An electroencephalogram (EEG) or lumbar puncture (spinal tap)
Case Study Risk Factors
- Karl has a long history of hypertension
- Age factor (65 years old)
Symptoms of Hemorrhagic Stroke - Case Study
- loss of speech or difficulty in understanding speech – Karl slurs his words
- confusion and or loss of alertness - appears sleepy, and becomes confused
- nausea and vomiting - Karl vomits
- impairment of consciousness - his pupils cannot turn to the right side
- stiffness or pain in the neck area - his face begins to droop on the left side
- difficulty swallowing - he suddenly has trouble swallowing
Treatment
- Controlling the bleeding
and reducing mental
pressure
- Drugs that help
counteract effects of
other drugs used by
patients
- Drugs that reduce
hypertension
- Surgery to repair
arteries
- Rehabilitation to
achieve independent
Pathophysiology of the disease the
patient’s clinical manifestations
- Blood flow into his brain
causes severe headache
leading to the below clinical
manifestations:
1. loss of speech or
difficulty in
understanding speech
as he slurs his words
2. confusion and or loss of
alertness as he appears
sleepy, and becomes
confused
3. feels nausea and
vomits
4. has impaired
consciousness as his
pupils cannot turn to
the right side
Aetiology and the
pathophysiology
- Karl has hypertension
- Bleeding happens inside
his brain
- Blood from an
intracerebral discharge to
form as a mass in the
cerebrum tissues, causing
intraventricular discharge
- Blood may cause intense
hydrocephalus if the drain
breaks into the ventricular
framework
The Concept Map - Intracerebral Hemorrhagic Stroke
Intracerebral Hemorrhagic
Stroke – Kennedy Karl
55 years old
The Risk Factors - Intracerebral Hemorrhage
- Hypertension
- Cerebral Cavernous Malfunctions
- Arteriovenous Malformations (AVMs)
Diagnosis
- A thorough medical and physical background
- Computed tomography (CT) scans
- Magnetic resonance imaging (MRI)
- Blood tests
- MRI angiography
- An electroencephalogram (EEG) or lumbar puncture (spinal tap)
Case Study Risk Factors
- Karl has a long history of hypertension
- Age factor (65 years old)
Symptoms of Hemorrhagic Stroke - Case Study
- loss of speech or difficulty in understanding speech – Karl slurs his words
- confusion and or loss of alertness - appears sleepy, and becomes confused
- nausea and vomiting - Karl vomits
- impairment of consciousness - his pupils cannot turn to the right side
- stiffness or pain in the neck area - his face begins to droop on the left side
- difficulty swallowing - he suddenly has trouble swallowing
Treatment
- Controlling the bleeding
and reducing mental
pressure
- Drugs that help
counteract effects of
other drugs used by
patients
- Drugs that reduce
hypertension
- Surgery to repair
arteries
- Rehabilitation to
achieve independent
Pathophysiology of the disease the
patient’s clinical manifestations
- Blood flow into his brain
causes severe headache
leading to the below clinical
manifestations:
1. loss of speech or
difficulty in
understanding speech
as he slurs his words
2. confusion and or loss of
alertness as he appears
sleepy, and becomes
confused
3. feels nausea and
vomits
4. has impaired
consciousness as his
pupils cannot turn to
the right side
Aetiology and the
pathophysiology
- Karl has hypertension
- Bleeding happens inside
his brain
- Blood from an
intracerebral discharge to
form as a mass in the
cerebrum tissues, causing
intraventricular discharge
- Blood may cause intense
hydrocephalus if the drain
breaks into the ventricular
framework
INTRACEREBRAL HAEMORRHAGIC STROKE 3
Risk Factors, Aetiology and Pathophysiology of the Disorder
The common cause of intracerebral hemorrhage (ICH) is protracted arterial high-blood
pressure, which is usually large, single as well as catastrophic. Other risk aspects comprise
cigarette smoking, obesity, excessive alcohol usage; use of cocaine, as well as vessel abnormality
and a high-risk-diet (An, Kim, & Yoon, 2017). People with high blood pressure and above 55
years old are vulnerable to the disorder. The basic underlying driver for the disease is an
aneurysm, a condition that happens when an area of a vein gets amplified from ceaseless and
hazardously hypertension. According to the case study, Karl Kennedy is 65 years of age and has
a history of hypertension, implying that he is vulnerable.
In the case study, his wife notices that his face begins to droop on the left side, and this
sign is a possible indication that the patient is having stiffness or pain in his neck area, and that
makes it impossible or hard for him to turn his face to the right side. The patient appears sleepy
and this signals a state of unconsciousness. Kennedy vomits and becomes confused and these
signs correspond to the intracerebral hemorrhagic stroke’s symptoms of nausea and vomiting.
The pathophysiology involves the functional developments related to the disease. Blood
from an intracerebral discharge aggregates as a mass that can analyze through and pack nearby
cerebrum tissues, causing neuronal brokenness. Blood may cause intense hydrocephalus if the
drain breaks into the ventricular framework - intraventricular discharge (Dadlani & Agrawal,
2017). The patient also demonstrates the impairment of consciousness when it is reported that his
pupils cannot turn to the right side.
How Disorder’s Pathophysiology Manifests
The mass accumulation of blood from the intracerebral hemorrhage dissects through and
compresses the adjacent brain tissues of Kennedy, prompting a neuronal dysfunction.
Risk Factors, Aetiology and Pathophysiology of the Disorder
The common cause of intracerebral hemorrhage (ICH) is protracted arterial high-blood
pressure, which is usually large, single as well as catastrophic. Other risk aspects comprise
cigarette smoking, obesity, excessive alcohol usage; use of cocaine, as well as vessel abnormality
and a high-risk-diet (An, Kim, & Yoon, 2017). People with high blood pressure and above 55
years old are vulnerable to the disorder. The basic underlying driver for the disease is an
aneurysm, a condition that happens when an area of a vein gets amplified from ceaseless and
hazardously hypertension. According to the case study, Karl Kennedy is 65 years of age and has
a history of hypertension, implying that he is vulnerable.
In the case study, his wife notices that his face begins to droop on the left side, and this
sign is a possible indication that the patient is having stiffness or pain in his neck area, and that
makes it impossible or hard for him to turn his face to the right side. The patient appears sleepy
and this signals a state of unconsciousness. Kennedy vomits and becomes confused and these
signs correspond to the intracerebral hemorrhagic stroke’s symptoms of nausea and vomiting.
The pathophysiology involves the functional developments related to the disease. Blood
from an intracerebral discharge aggregates as a mass that can analyze through and pack nearby
cerebrum tissues, causing neuronal brokenness. Blood may cause intense hydrocephalus if the
drain breaks into the ventricular framework - intraventricular discharge (Dadlani & Agrawal,
2017). The patient also demonstrates the impairment of consciousness when it is reported that his
pupils cannot turn to the right side.
How Disorder’s Pathophysiology Manifests
The mass accumulation of blood from the intracerebral hemorrhage dissects through and
compresses the adjacent brain tissues of Kennedy, prompting a neuronal dysfunction.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INTRACEREBRAL HAEMORRHAGIC STROKE 4
Consequently, large hematomas continue to pile pressure in his intracranial space (An, Kim, &
Yoon, 2017). Meanwhile, pressure from his supratentorial hematomas as well as the
complementary edema may have caused transtentorial brain herniation, squeezing his brain stem
and always triggering secondary hemorrhages in his midbrain and pons (Toyoda, Anderson, &
Mayer, 2015). For illustration, if the hemorrhage broke into his ventricular system, he may have
suffered from acute hydrocephalus.
In the meantime, there is a possibility that the patient’s cerebellar hematomas could
expand to the extent of blocking the 4th ventricle, eventually leading to acute hydrocephalus,
with an alternative of possibly dissecting into his brain stem (Toyoda, Anderson, & Mayer,
2015). Notably, scientific studies have established that cerebellar hematomas that are more than
three centimeters in diameter may as well lead to a midline shift or herniation. Sadly,
intraventricular hemorrhage can potentially impair consciousness and cause coma and sometimes
death (Toyoda, Anderson, & Mayer, 2015). The patient might have experienced sudden onset of
headache, coupled with focal neurologic deficits, as well as impaired consciousness, particularly
because he has one major risk factor, hypertension and age risk factor.
Justifying Suggested Diagnostic Investigations and Treatment Modalities
Being a condition that requires an emergency response, a thorough physical examination
and medical history of a patient is necessary. From the case study, it possible to classify
Kennedy’s condition as intracerebral hemorrhagic due to matching physical signs and known
signs and symptoms of the disorder (Toyoda, Anderson, & Mayer, 2015). During physical
examination, a doctor can look at the observable indicators that include intellectual attentiveness,
coordination and steadiness abilities, impassiveness and or feebleness in a patient’s face, some
elements of mix-up, and difficulty while talking among others. After examining visible signs and
Consequently, large hematomas continue to pile pressure in his intracranial space (An, Kim, &
Yoon, 2017). Meanwhile, pressure from his supratentorial hematomas as well as the
complementary edema may have caused transtentorial brain herniation, squeezing his brain stem
and always triggering secondary hemorrhages in his midbrain and pons (Toyoda, Anderson, &
Mayer, 2015). For illustration, if the hemorrhage broke into his ventricular system, he may have
suffered from acute hydrocephalus.
In the meantime, there is a possibility that the patient’s cerebellar hematomas could
expand to the extent of blocking the 4th ventricle, eventually leading to acute hydrocephalus,
with an alternative of possibly dissecting into his brain stem (Toyoda, Anderson, & Mayer,
2015). Notably, scientific studies have established that cerebellar hematomas that are more than
three centimeters in diameter may as well lead to a midline shift or herniation. Sadly,
intraventricular hemorrhage can potentially impair consciousness and cause coma and sometimes
death (Toyoda, Anderson, & Mayer, 2015). The patient might have experienced sudden onset of
headache, coupled with focal neurologic deficits, as well as impaired consciousness, particularly
because he has one major risk factor, hypertension and age risk factor.
Justifying Suggested Diagnostic Investigations and Treatment Modalities
Being a condition that requires an emergency response, a thorough physical examination
and medical history of a patient is necessary. From the case study, it possible to classify
Kennedy’s condition as intracerebral hemorrhagic due to matching physical signs and known
signs and symptoms of the disorder (Toyoda, Anderson, & Mayer, 2015). During physical
examination, a doctor can look at the observable indicators that include intellectual attentiveness,
coordination and steadiness abilities, impassiveness and or feebleness in a patient’s face, some
elements of mix-up, and difficulty while talking among others. After examining visible signs and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INTRACEREBRAL HAEMORRHAGIC STROKE 5
medical history, it is important to proceed to imaging tests to establish the existence of bleeding
inside a patient’s brain (Dadlani & Agrawal, 2017). However, the use of computed tomography
(CT) scans is preferred for hemorrhagic strokes because they are always the fastest thus serve a
critical role during emergency treatments. Doctors may also conduct alternative tests that entail
MRI, MRI angiography, examinations on blood, and EEG just to ensure that their examination is
adequate and accurate for particular treatment modalities (Toyoda, Anderson, & Mayer, 2015).
As mentioned earlier, the disease is always a medical emergency and immediate
treatment is the difference between life and death (Dadlani & Agrawal, 2017). The medications
are first meant to reduce bleeding into the brain and reducing pressure at the same time. By
lowering blood pressure and pressure in the brain area, the blood vessels stop tightening and
seizures cease (Toyoda, Anderson, & Mayer, 2015). After stopping bleeding, doctors have
treatment options, one being conducting surgery in the brain to repair the blood vessel
abnormalities as well as aneurysm with the help of surgical equipment. Once a patient is safe, he
or she can now undergo rehabilitation whose primary goal is attaining independent living
(Dadlani & Agrawal, 2017).
medical history, it is important to proceed to imaging tests to establish the existence of bleeding
inside a patient’s brain (Dadlani & Agrawal, 2017). However, the use of computed tomography
(CT) scans is preferred for hemorrhagic strokes because they are always the fastest thus serve a
critical role during emergency treatments. Doctors may also conduct alternative tests that entail
MRI, MRI angiography, examinations on blood, and EEG just to ensure that their examination is
adequate and accurate for particular treatment modalities (Toyoda, Anderson, & Mayer, 2015).
As mentioned earlier, the disease is always a medical emergency and immediate
treatment is the difference between life and death (Dadlani & Agrawal, 2017). The medications
are first meant to reduce bleeding into the brain and reducing pressure at the same time. By
lowering blood pressure and pressure in the brain area, the blood vessels stop tightening and
seizures cease (Toyoda, Anderson, & Mayer, 2015). After stopping bleeding, doctors have
treatment options, one being conducting surgery in the brain to repair the blood vessel
abnormalities as well as aneurysm with the help of surgical equipment. Once a patient is safe, he
or she can now undergo rehabilitation whose primary goal is attaining independent living
(Dadlani & Agrawal, 2017).
INTRACEREBRAL HAEMORRHAGIC STROKE 6
References
An, S. J., Kim, T. J., & Yoon, B. W. (2017). Epidemiology, risk factors, and clinical features of
intracerebral hemorrhage: an update. Journal of stroke, 19(1), 3.
Dadlani, R., & Agrawal, A. (October 04, 2017). Intracerebral Hemorrhage: Issues in
Rehabilitation.
Toyoda, K., Anderson, C. S., & Mayer, S. A. (2015). New insights in intracerebral hemorrhage.
Basel; New York, NY: Karger
References
An, S. J., Kim, T. J., & Yoon, B. W. (2017). Epidemiology, risk factors, and clinical features of
intracerebral hemorrhage: an update. Journal of stroke, 19(1), 3.
Dadlani, R., & Agrawal, A. (October 04, 2017). Intracerebral Hemorrhage: Issues in
Rehabilitation.
Toyoda, K., Anderson, C. S., & Mayer, S. A. (2015). New insights in intracerebral hemorrhage.
Basel; New York, NY: Karger
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


