ICU Case Study: Comprehensive Nursing Analysis of ARDS and Sepsis
VerifiedAdded on 2023/06/04
|9
|4114
|406
Case Study
AI Summary
This nursing case study focuses on Billy, a 32-year-old male admitted to the ICU with suspected tricyclic antidepressant overdose, complicated by obesity, depression, and chronic pain. The case details the pathophysiology of Acute Respiratory Distress Syndrome (ARDS), including arterial blood gas interpretation and ventilation strategies. It discusses the proposed ventilation parameters, such as low tidal volume ventilation, and analyzes their rationale based on current evidence. Furthermore, the case study explores the deterioration of Billy's condition 24 hours post-admission, incorporating the determinants of cardiac output and pathophysiology of severe sepsis, highlighting the inflammatory responses and coagulation activation associated with organ dysfunction. Desklib provides a platform for students to access this and similar solved assignments, offering valuable resources for understanding complex healthcare scenarios.
Nursing Case Study Acute
Respiratory Distress Syndrome
arterial blood cardiac output
sepsisgas
Respiratory Distress Syndrome
arterial blood cardiac output
sepsisgas
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Case study:
Billy, a 32-year-old male, was admitted to the Intensive Care Unit (ICU) with a suspected
overdose of tricyclic antidepressants. He is obese (weight 160kg, height 172cm) and has a
history of depression and chronic back pain for which he takes oxycodone.
On admission to the emergency department, paramedics were maintaining Billy’s airways
with a combination of jaw thrust, head tilt and guedel airway. Billy was obtunded with
evidence of vomitus on his clothing. There was an attempted intubation enroute which was
unsuccessful.
Billy’s initial observations were:
Temperature 35.5 degrees Celsius
Heart rate 140bpm
Blood pressure 100/50mmHg
Respiratory Rate 22 beats/ min, shallow and laboured
Oxygen saturation 92% breathing spontaneously via a bag valve mask with oxygen at
15L/min
Auscultation of lung sounds revealed decreased air entry bilaterally and expiratory
wheezes
Arterial blood gas: pH 7.21, PaCO2 68mmHg, PaO2 90mmHg, HCO3 26mEq/L,
SaO2 94%
GCS 8 (E1, V3, M4)
Question One
PART A)
Describe the pathophysiology of Acute Respiratory Distress Syndrome, including a
systematic interpretation of the arterial blood gas (Consider PaO2/ FiO2 – P/F ratio, assume
PEEP is 5cmH2O). Interpret the ABG, including determining the PaO2/FiO2 ratio. What do
these results indicate for Billy?
Pathophysiology of Acute Respiratory Distress Syndrome: An Acute Respiratory
Distress Syndrome is generally a multifaceted syndrome of acute lung damage specifically
foremost to a non-cardiogenic pulmonary oedema from various reasons which is
heterogeneous within its medical demonstration and are also linked with the 40% death rate.
An Acute Respiratory Distress Syndrome is significantly marked by an inflammation-
medicated disruption within the alveolar-capillary permeability, edema formation, decreased
alveolar clearance as well as collapse/derecruitment, decreased obedience, enhanced
pulmonary vascular resistance as well as a resulting interchange of gases. Within this, an
understanding of ARDS physiology, that can include a key characteristics consisting
exchange of gas abnormalities can frequently need ventilator encouragement as well as
reduced compliance with the specific regional heterogeneity, generally has inferences for the
ventilator encouragement strategies (Ali and Lamont, 2019). A positive pressure ventilation
consisting with the positive as well as an expiratory pressure generally decreases the
breathing work as well as can prevent atelectasis of a nearly collapsed lung units in order to
enhance the interchange of gases. In this, a positive pressure of the airways generally helps to
decrease further ongoing edema synthesis within various oedematous states, consisting the
Billy, a 32-year-old male, was admitted to the Intensive Care Unit (ICU) with a suspected
overdose of tricyclic antidepressants. He is obese (weight 160kg, height 172cm) and has a
history of depression and chronic back pain for which he takes oxycodone.
On admission to the emergency department, paramedics were maintaining Billy’s airways
with a combination of jaw thrust, head tilt and guedel airway. Billy was obtunded with
evidence of vomitus on his clothing. There was an attempted intubation enroute which was
unsuccessful.
Billy’s initial observations were:
Temperature 35.5 degrees Celsius
Heart rate 140bpm
Blood pressure 100/50mmHg
Respiratory Rate 22 beats/ min, shallow and laboured
Oxygen saturation 92% breathing spontaneously via a bag valve mask with oxygen at
15L/min
Auscultation of lung sounds revealed decreased air entry bilaterally and expiratory
wheezes
Arterial blood gas: pH 7.21, PaCO2 68mmHg, PaO2 90mmHg, HCO3 26mEq/L,
SaO2 94%
GCS 8 (E1, V3, M4)
Question One
PART A)
Describe the pathophysiology of Acute Respiratory Distress Syndrome, including a
systematic interpretation of the arterial blood gas (Consider PaO2/ FiO2 – P/F ratio, assume
PEEP is 5cmH2O). Interpret the ABG, including determining the PaO2/FiO2 ratio. What do
these results indicate for Billy?
Pathophysiology of Acute Respiratory Distress Syndrome: An Acute Respiratory
Distress Syndrome is generally a multifaceted syndrome of acute lung damage specifically
foremost to a non-cardiogenic pulmonary oedema from various reasons which is
heterogeneous within its medical demonstration and are also linked with the 40% death rate.
An Acute Respiratory Distress Syndrome is significantly marked by an inflammation-
medicated disruption within the alveolar-capillary permeability, edema formation, decreased
alveolar clearance as well as collapse/derecruitment, decreased obedience, enhanced
pulmonary vascular resistance as well as a resulting interchange of gases. Within this, an
understanding of ARDS physiology, that can include a key characteristics consisting
exchange of gas abnormalities can frequently need ventilator encouragement as well as
reduced compliance with the specific regional heterogeneity, generally has inferences for the
ventilator encouragement strategies (Ali and Lamont, 2019). A positive pressure ventilation
consisting with the positive as well as an expiratory pressure generally decreases the
breathing work as well as can prevent atelectasis of a nearly collapsed lung units in order to
enhance the interchange of gases. In this, a positive pressure of the airways generally helps to
decrease further ongoing edema synthesis within various oedematous states, consisting the
enhanced alveolar penetrability of the Acute Respiratory Distress Syndrome. Within acute
respiratory distress syndrome, the damaged lung is generally believed to go via the specific
three phases such as exudative, fibrotic and a proliferative, but the course of every part as
well as entire illness development is quite variable. While talking about exudative phase,
injury towards the alveolar epithelium as well as vascular endothelium creates leakage of
water, inflammatory, protein as well as the red blood cells within the interstitium and an
alveolar lumen. In addition, these such alterations are effectively induced by a complex
interplay of a pro-inflammatory as well as an anti-inflammatory mediator. The specific type 1
alveolar cells are generally irreversibly injured as well as the denuded space is replaced by
the protein deposition, cellular debris, fibrin and can produce a hyaline membrane, while
damage to the type 2 cells produced by surfactant mainly contributes towards an alveolar
collapse. In context with the proliferative phase, type 2 cells generally proliferate with
regeneration of some of the epithelial cells, remodelling and a fibroblastic reaction as well.
Among some of the patients, such things can advance towards a permanent fibrotic phase
consisting the deposition of collagen within alveolar, interstitial beds and vascular with the
advancement of microcyst.
ABG is generally an Arterial Blood Gas that can include various steps. Within this, the
initial step in an interpretation of ABG is to visualise the pH. The standard range of blood pH
is 7.4, minus or plus 0.05, mainly developing the range of 7.35 to 7.45. If the pH falls from
the normal range such as below 7.35 then it can be considered as acidic. Whereas, if the
blood pH increased above 7.45, then it can be considered as alkalotic (Byrne, 2021). The pH
range of Billy’s is about 7.21 is normal but slightly acidic. In addition to this, the another step
is to determine the pCO2 level. A standard pCO2 levels are about 35 to 45 mmHg. An
underneath from the normal range such as >35 is alkalotic and <45 is quite acidic. In context
with provided case scenario, the pCO2 level is 68 mmHg that is quite acidic. The third step
within the interpretation of Arterial Blood Gas is to aspect at the HCO3 level. In this, a
standard range of HCO3 is about 22 to 26 mEq/L. And, if the HCO3 is above the level of 26,
the patient is alkalotic and below of 22 then the patient is acidotic in nature. Within the
provided case scenario, a HCO3 level is given about 26 mEq/L which is normal. Next will
match either the HCO3 or the pCO2 with the pH in order to measure the acid-base disorders.
Such that, if the pH is acidotic, and the CO2 is acidotic, then the acid-base disturbance is
generally being caused by the respiratory system. Therefore, if the pH is alkalotic and the
HCO3 is alkalotic, then the acid-base disturbance is being caused by the metabolic or the
renal system. However, it will be a metabolic alkalosis. In the case of Jelly, while comparing
the normal range of pCO2 or HCO3 with the pH, in his case pH is slightly acidotic and the
CO2 is also acidotic, then the acid-base disturbance that is being caused by the respiratory
system (6 Easy Steps to ABG Interpretation, 2019). The partial arterial pressure of O2 and the
fraction of an inspired oxygen ratio such as PaO2/FiO2 is broadly used within the Intensive
Care Units as an indicator of the oxygenation status. A PaO2/FiO2 ratio is mainly subdivided
using the threshold of about 100-200-300 as per the Berlin criteria of Acute Respiratory
Distress Syndrome. PaO2< 60 and>100 mmHg versus PaO2 60-100. A partial pressure level
of oxygen in Jelly’s case is 90 mmHg.
PART B)
In view of Billy’s current clinical condition, outline the proposed ventilation parameters you
would suggest including rationales.
respiratory distress syndrome, the damaged lung is generally believed to go via the specific
three phases such as exudative, fibrotic and a proliferative, but the course of every part as
well as entire illness development is quite variable. While talking about exudative phase,
injury towards the alveolar epithelium as well as vascular endothelium creates leakage of
water, inflammatory, protein as well as the red blood cells within the interstitium and an
alveolar lumen. In addition, these such alterations are effectively induced by a complex
interplay of a pro-inflammatory as well as an anti-inflammatory mediator. The specific type 1
alveolar cells are generally irreversibly injured as well as the denuded space is replaced by
the protein deposition, cellular debris, fibrin and can produce a hyaline membrane, while
damage to the type 2 cells produced by surfactant mainly contributes towards an alveolar
collapse. In context with the proliferative phase, type 2 cells generally proliferate with
regeneration of some of the epithelial cells, remodelling and a fibroblastic reaction as well.
Among some of the patients, such things can advance towards a permanent fibrotic phase
consisting the deposition of collagen within alveolar, interstitial beds and vascular with the
advancement of microcyst.
ABG is generally an Arterial Blood Gas that can include various steps. Within this, the
initial step in an interpretation of ABG is to visualise the pH. The standard range of blood pH
is 7.4, minus or plus 0.05, mainly developing the range of 7.35 to 7.45. If the pH falls from
the normal range such as below 7.35 then it can be considered as acidic. Whereas, if the
blood pH increased above 7.45, then it can be considered as alkalotic (Byrne, 2021). The pH
range of Billy’s is about 7.21 is normal but slightly acidic. In addition to this, the another step
is to determine the pCO2 level. A standard pCO2 levels are about 35 to 45 mmHg. An
underneath from the normal range such as >35 is alkalotic and <45 is quite acidic. In context
with provided case scenario, the pCO2 level is 68 mmHg that is quite acidic. The third step
within the interpretation of Arterial Blood Gas is to aspect at the HCO3 level. In this, a
standard range of HCO3 is about 22 to 26 mEq/L. And, if the HCO3 is above the level of 26,
the patient is alkalotic and below of 22 then the patient is acidotic in nature. Within the
provided case scenario, a HCO3 level is given about 26 mEq/L which is normal. Next will
match either the HCO3 or the pCO2 with the pH in order to measure the acid-base disorders.
Such that, if the pH is acidotic, and the CO2 is acidotic, then the acid-base disturbance is
generally being caused by the respiratory system. Therefore, if the pH is alkalotic and the
HCO3 is alkalotic, then the acid-base disturbance is being caused by the metabolic or the
renal system. However, it will be a metabolic alkalosis. In the case of Jelly, while comparing
the normal range of pCO2 or HCO3 with the pH, in his case pH is slightly acidotic and the
CO2 is also acidotic, then the acid-base disturbance that is being caused by the respiratory
system (6 Easy Steps to ABG Interpretation, 2019). The partial arterial pressure of O2 and the
fraction of an inspired oxygen ratio such as PaO2/FiO2 is broadly used within the Intensive
Care Units as an indicator of the oxygenation status. A PaO2/FiO2 ratio is mainly subdivided
using the threshold of about 100-200-300 as per the Berlin criteria of Acute Respiratory
Distress Syndrome. PaO2< 60 and>100 mmHg versus PaO2 60-100. A partial pressure level
of oxygen in Jelly’s case is 90 mmHg.
PART B)
In view of Billy’s current clinical condition, outline the proposed ventilation parameters you
would suggest including rationales.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

An acute respiratory distress syndrome is mainly categorized by the fatal damage of
the pulmonary gas interchange, generally outcomes in hypoxemia, respiratory acidosis,
hypercapnia as well as needing an acute rescue dealing. The distribution of the oxygen
towards tissues are generally essential for all the aerobic life and the tissue hypoxia will
outcomes in several toxic impacts consisting a transformed vascular reactivity, cell apoptosis,
infection as well as organ failure (Haeberle and et. al., 2020). A tissue hypoxia is generally an
outcome of hypoxemia that is a significance of having an inadequate encouragement of the
respiratory system and the oxygen transport system. In order to provide mechanical
ventilation for Jelly’s condition, the specific settings are suggested such as constraint of tidal
volume (6 ml/kg anticipated the body weight), having adequate high PEEP (>12 cm H2O), a
balanced respiratory rate about 20 to 30 beats per minute and a manoeuvre within the special
condition. The use of invasive aeration for the patients with consisting Acute Respiratory
Disorder syndrome, specifically those with a severe or moderate level ARDS<= 200 mmHg
on both the positive end-expiratory pressure. A patient with ARDS such as Jelly’s case will
need an intubation as well as a mechanical ventilation. While having the peri-intubation
period, about 95 to 100 percent of the oxygen must be provided to effectively safeguard a
suitable amount of oxygen saturation. It is because an uptake of oxygen can exceed a
replenishment within the region of consisting a low V/Q ratio. Once it is established, an
absorptive atelectasis is not speedily reversed by the decrease of FiO2 towards a keep levels,
more stressing over the desirability of limiting prolonged periods of elevated FiO2 during and
following the intubation period (Haren, Byrne and Litton, 2019).
PART C)
Using current evidence from the literature, critically analyse one of the mechanical
ventilation strategies/ parameters that you have chosen.
From various chosen articles or websites, it has been determined that the one of the
mechanical ventilation parameter or strategies that is being chosen is Low Tidal Volume
Ventilation. For the patient with involving Acute Respiratory Disorder Syndrome, a Low
Tidal Volume Ventilation is being recommended and is also called as lung protective aeration
having 4 to 8 mL/Kg anticipated body weight. As per the LTVV, a predicted body weight of
Jelly is about 172 cm/ 68.4 Kg and the tidal volume from 4 to 8 mL/Kg should be about
274,342, 410, 479 and 547 ml/Kg. As his body weight is of 160 Kg which fall under obese
category. The LTVV approach is being used and is based on various meta-analysis as well as
a randomized trail which can report a mortality advantages from the LTVV approach among
the patient with ARDS. It is being thought that a LTV generally mitigate an alveolar over
enlargement mainly encouraged by a mechanical ventilation, that can cause a supplementary
lung damage as well as death within the patients with ARDS. A PEEP is being used among
patients with ARDS. The main goal to apply PEEP among patients with ARDS is generally to
enhance as well as maintain an alveolar recruitment, thereby enhancing an oxygenation as
well as limiting oxygen toxicity (Ventilator management strategies for adults with acute
respiratory distress syndrome, 2022).
Question Two
Twenty-four hours after admission to the ICU, Billy’s condition deteriorates. His current
observations are:
the pulmonary gas interchange, generally outcomes in hypoxemia, respiratory acidosis,
hypercapnia as well as needing an acute rescue dealing. The distribution of the oxygen
towards tissues are generally essential for all the aerobic life and the tissue hypoxia will
outcomes in several toxic impacts consisting a transformed vascular reactivity, cell apoptosis,
infection as well as organ failure (Haeberle and et. al., 2020). A tissue hypoxia is generally an
outcome of hypoxemia that is a significance of having an inadequate encouragement of the
respiratory system and the oxygen transport system. In order to provide mechanical
ventilation for Jelly’s condition, the specific settings are suggested such as constraint of tidal
volume (6 ml/kg anticipated the body weight), having adequate high PEEP (>12 cm H2O), a
balanced respiratory rate about 20 to 30 beats per minute and a manoeuvre within the special
condition. The use of invasive aeration for the patients with consisting Acute Respiratory
Disorder syndrome, specifically those with a severe or moderate level ARDS<= 200 mmHg
on both the positive end-expiratory pressure. A patient with ARDS such as Jelly’s case will
need an intubation as well as a mechanical ventilation. While having the peri-intubation
period, about 95 to 100 percent of the oxygen must be provided to effectively safeguard a
suitable amount of oxygen saturation. It is because an uptake of oxygen can exceed a
replenishment within the region of consisting a low V/Q ratio. Once it is established, an
absorptive atelectasis is not speedily reversed by the decrease of FiO2 towards a keep levels,
more stressing over the desirability of limiting prolonged periods of elevated FiO2 during and
following the intubation period (Haren, Byrne and Litton, 2019).
PART C)
Using current evidence from the literature, critically analyse one of the mechanical
ventilation strategies/ parameters that you have chosen.
From various chosen articles or websites, it has been determined that the one of the
mechanical ventilation parameter or strategies that is being chosen is Low Tidal Volume
Ventilation. For the patient with involving Acute Respiratory Disorder Syndrome, a Low
Tidal Volume Ventilation is being recommended and is also called as lung protective aeration
having 4 to 8 mL/Kg anticipated body weight. As per the LTVV, a predicted body weight of
Jelly is about 172 cm/ 68.4 Kg and the tidal volume from 4 to 8 mL/Kg should be about
274,342, 410, 479 and 547 ml/Kg. As his body weight is of 160 Kg which fall under obese
category. The LTVV approach is being used and is based on various meta-analysis as well as
a randomized trail which can report a mortality advantages from the LTVV approach among
the patient with ARDS. It is being thought that a LTV generally mitigate an alveolar over
enlargement mainly encouraged by a mechanical ventilation, that can cause a supplementary
lung damage as well as death within the patients with ARDS. A PEEP is being used among
patients with ARDS. The main goal to apply PEEP among patients with ARDS is generally to
enhance as well as maintain an alveolar recruitment, thereby enhancing an oxygenation as
well as limiting oxygen toxicity (Ventilator management strategies for adults with acute
respiratory distress syndrome, 2022).
Question Two
Twenty-four hours after admission to the ICU, Billy’s condition deteriorates. His current
observations are:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Temperature 39 degrees Celsius
Sinus Tachycardia with a heart rate 130 beats/min
Arterial Blood pressure 85/55 mmHg
Pulse pressure variation or systolic volume variation (PPV or SVV) 15%
Central venous pressure 5mmHg
Bounding peripheral pulses
Urine output 20mls for the last hour and 80ml total for last 4 hours
PART D)
Discuss Billy’s assessment data, incorporating the determinants of cardiac output and
pathophysiology of severe sepsis.
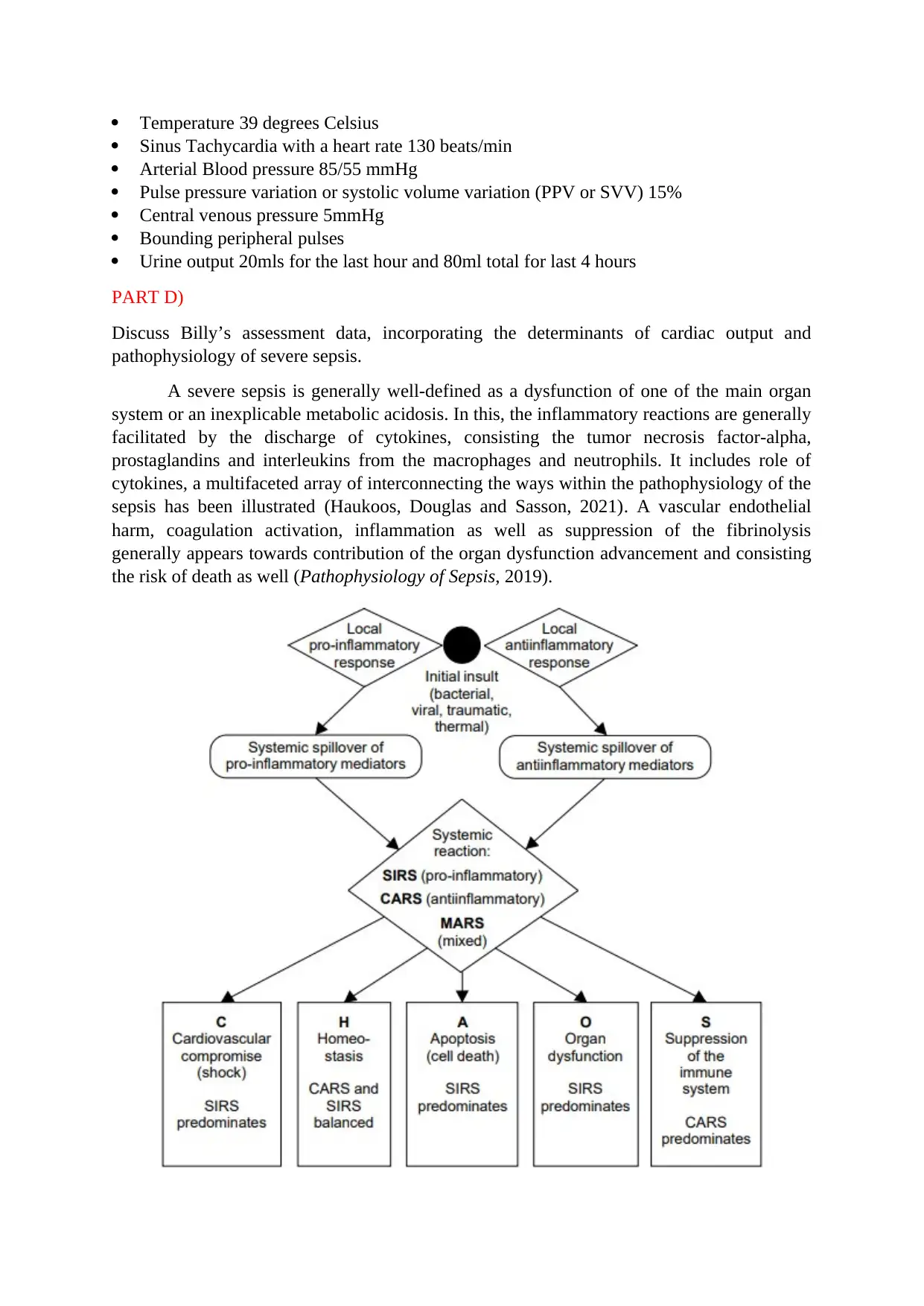
A severe sepsis is generally well-defined as a dysfunction of one of the main organ
system or an inexplicable metabolic acidosis. In this, the inflammatory reactions are generally
facilitated by the discharge of cytokines, consisting the tumor necrosis factor-alpha,
prostaglandins and interleukins from the macrophages and neutrophils. It includes role of
cytokines, a multifaceted array of interconnecting the ways within the pathophysiology of the
sepsis has been illustrated (Haukoos, Douglas and Sasson, 2021). A vascular endothelial
harm, coagulation activation, inflammation as well as suppression of the fibrinolysis
generally appears towards contribution of the organ dysfunction advancement and consisting
the risk of death as well (Pathophysiology of Sepsis, 2019).
Sinus Tachycardia with a heart rate 130 beats/min
Arterial Blood pressure 85/55 mmHg
Pulse pressure variation or systolic volume variation (PPV or SVV) 15%
Central venous pressure 5mmHg
Bounding peripheral pulses
Urine output 20mls for the last hour and 80ml total for last 4 hours
PART D)
Discuss Billy’s assessment data, incorporating the determinants of cardiac output and
pathophysiology of severe sepsis.
A severe sepsis is generally well-defined as a dysfunction of one of the main organ
system or an inexplicable metabolic acidosis. In this, the inflammatory reactions are generally
facilitated by the discharge of cytokines, consisting the tumor necrosis factor-alpha,
prostaglandins and interleukins from the macrophages and neutrophils. It includes role of
cytokines, a multifaceted array of interconnecting the ways within the pathophysiology of the
sepsis has been illustrated (Haukoos, Douglas and Sasson, 2021). A vascular endothelial
harm, coagulation activation, inflammation as well as suppression of the fibrinolysis
generally appears towards contribution of the organ dysfunction advancement and consisting
the risk of death as well (Pathophysiology of Sepsis, 2019).
The sepsis progression is generally from the initial insult as well as the local
inflammatory and an anti-inflammatory response via a systemic spill over of the mediators.
Within this, the systemic reactions might consist the characteristics of additional of either an
anti-inflammatory or the inflammatory intermediaries or consisting a mixed pattern as well.
In addition, the medical sequelae of the sepsis generally vary contingent on the balance of
mediators. An excessive inflammatory response (SIRS) might create a shock as well as the
dysfunctioning of organ. CARS specifically inhibits the immune system. Within this, a
composed response of the inflammatory mediators significantly creates homeostasis. Some of
its patients might die with having a reduced inflammation as an outcome of apoptosis
(Kharrat and Jain, 2022). Role of coagulation: In this, an inflammation process as well as
coagulation generally appears to be a closely associated with the components of SIRS and
sepsis. Medically, the patients often demonstrate the low platelets counts, enhance D-dimer
concentrations as well as fibrinogen degradation products as well as other features of the low-
grade disseminated intravascular coagulation or the microvascular coagulopathy (Acute
Respiratory Distress Syndrome, 2022). As per the Billy’s assessment, his body temperature is
quite increased from the normal temperature like it should be about 37 degrees and is
observed at 39 degrees Celsius. He is also noted with Sinus tachycardia with consisting heart
rate about 130 beat per minute which should be about 60 to 100 beats per minute. His central
venous pressure is normal including range of 5 mmHg. In addition to this, He has critical
issue with the urine output of about 20 mL for the last one hour and about 80 mL in total for
last 4 hours which should be about 0.5 to 1.5 mL per hour. He also has low blood pressure
such as having 85/55 mmHg Arterial blood pressure. Patients having ARDS is usually
characterised by the diffusion of alveolar impairment as well as is often complicated by the
pulmonary hypotension. There are generally the various elements which can contribute
towards the development of pulmonary hypotension among patients. In addition to this, he is
an abusive person as he is suspected with over dosage of tricyclic antidepressants
(Pulmonary vascular dysfunction in ARDS, 2014). Due to which he has experienced serotonin
syndrome. It is generally a critical negative drug reaction which can occurs when enough
serotonin arises within the body. The syndrome can cause nausea too among people.
PART E)
Using current evidence critically analyse the best practice therapy in relation to fluid
resuscitation and vasopressor management.
A septic shock is generally a consequence of the systemic contamination which is
being featured by the hypotension unresponsive to the fluid resuscitation. It is specifically a
critical well-being care issue which afflicts a numerous of the people annually across the
nation (Acute respiratory distress syndrome: Supportive care and oxygenation in adults,
2022). An initial management of the patients with consisting a septic shock is generally to
uphold the mean arterial pressure as well as a cardiac outcome while highlighting the
contamination with an antimicrobial therapy and a source control. The patients who generally
fails to retort towards an aggressive fluid resuscitation are generally the participants for the
vasopressor or an inotropic therapy to uphold the hemodynamic parameters.
Practice therapy in relation to Fluid resuscitation: In this, an optimum fluid
management strategy for the acute respiratory distress syndrome is not known. In context
with European Society of Intensive Care Medicine/American Thoracic Society, medical care
inflammatory and an anti-inflammatory response via a systemic spill over of the mediators.
Within this, the systemic reactions might consist the characteristics of additional of either an
anti-inflammatory or the inflammatory intermediaries or consisting a mixed pattern as well.
In addition, the medical sequelae of the sepsis generally vary contingent on the balance of
mediators. An excessive inflammatory response (SIRS) might create a shock as well as the
dysfunctioning of organ. CARS specifically inhibits the immune system. Within this, a
composed response of the inflammatory mediators significantly creates homeostasis. Some of
its patients might die with having a reduced inflammation as an outcome of apoptosis
(Kharrat and Jain, 2022). Role of coagulation: In this, an inflammation process as well as
coagulation generally appears to be a closely associated with the components of SIRS and
sepsis. Medically, the patients often demonstrate the low platelets counts, enhance D-dimer
concentrations as well as fibrinogen degradation products as well as other features of the low-
grade disseminated intravascular coagulation or the microvascular coagulopathy (Acute
Respiratory Distress Syndrome, 2022). As per the Billy’s assessment, his body temperature is
quite increased from the normal temperature like it should be about 37 degrees and is
observed at 39 degrees Celsius. He is also noted with Sinus tachycardia with consisting heart
rate about 130 beat per minute which should be about 60 to 100 beats per minute. His central
venous pressure is normal including range of 5 mmHg. In addition to this, He has critical
issue with the urine output of about 20 mL for the last one hour and about 80 mL in total for
last 4 hours which should be about 0.5 to 1.5 mL per hour. He also has low blood pressure
such as having 85/55 mmHg Arterial blood pressure. Patients having ARDS is usually
characterised by the diffusion of alveolar impairment as well as is often complicated by the
pulmonary hypotension. There are generally the various elements which can contribute
towards the development of pulmonary hypotension among patients. In addition to this, he is
an abusive person as he is suspected with over dosage of tricyclic antidepressants
(Pulmonary vascular dysfunction in ARDS, 2014). Due to which he has experienced serotonin
syndrome. It is generally a critical negative drug reaction which can occurs when enough
serotonin arises within the body. The syndrome can cause nausea too among people.
PART E)
Using current evidence critically analyse the best practice therapy in relation to fluid
resuscitation and vasopressor management.
A septic shock is generally a consequence of the systemic contamination which is
being featured by the hypotension unresponsive to the fluid resuscitation. It is specifically a
critical well-being care issue which afflicts a numerous of the people annually across the
nation (Acute respiratory distress syndrome: Supportive care and oxygenation in adults,
2022). An initial management of the patients with consisting a septic shock is generally to
uphold the mean arterial pressure as well as a cardiac outcome while highlighting the
contamination with an antimicrobial therapy and a source control. The patients who generally
fails to retort towards an aggressive fluid resuscitation are generally the participants for the
vasopressor or an inotropic therapy to uphold the hemodynamic parameters.
Practice therapy in relation to Fluid resuscitation: In this, an optimum fluid
management strategy for the acute respiratory distress syndrome is not known. In context
with European Society of Intensive Care Medicine/American Thoracic Society, medical care
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
practice guidelines generally make no significant suggestions for the management of fluid
among the ARDS patients (Fluid management in Acute Respiratory Distress Syndrome: A
narrative review, 2019). While talking about the liberal fluid management, historically the
conventional training, do not limit the administration of the fluid while having the
resuscitation phase or effectively seeking to remove the fluid during the deresuscitative
phase. Within this, the theoretic argument for a liberal management of the fluid strategy is
that it can enhance the stroke volume and thereby can enhance end organ perfusion along
with oxygen delivery (Kornas and et. al., 2021). As compared with the liberal management of
fluid strategy, a conservative strategy can limit the administration of fluid during the
resuscitation phase as well as employs the care treatment to lower the entire body fluid
balance during the deresuscitative phase. Such effective strategy can seek to decrease the
pulmonary perfusion or ventilation mismatch by restricting the pulmonary edema but might
risk as well as end-organ malfunction from reduced cardiac perfusion (Fluid Therapy and
Acute Respiratory Distress Syndrome, 2021). Furthermore, a fluid limitation can decrease the
cardiac output as well as a perfusion of tissue, that can cause or deteriorates the non-
pulmonary dysfunctioning of organs. Among various patients with acute liver injury or
ARDS, the dysfunctioning of the various organs along with systems can happen from a
systemic inflammatory response (Fluid management in ARDS: an evaluation of current
practice and the association between early diuretic use and hospital mortality, 2020).
Practice therapy in relation to vasopressor management: The vasopressor is generally
needed to encourage the systemic Blood pressure or to enhance the cardiac output among
patients with the shock. In addition to this, there is generally no clear reference or
information that any of the vasopressor or grouping of these vasopressor is higher. Within
this, the prudent methods within ARDS patients is generally to re-establish the intravascular
volume towards the euvolemic levels and then to use a vasopressor like the dopamine to
effectively attain a mean arterial pressure of about 55 to 65 mmHg.
Therefore, both the vasopressor and fluid therapy would be effectively directed by the
medical indexes of the organ perfusion. In addition, an output of urine, blood pH as well as a
base discrepancy are effectively supportive to measure the competence of perfusion of
organs. Among some of the patients, a pulmonary arterial catheter can give a beneficial
supplementary information, more specifically when there is a left ventricular dysfunctioning
or the pulmonary hypertension that is quite communal among the patients with ARDS.
Furthermore, there is a new information on the problem of management of fluid as well as the
value consisting a central venous Vs a pulmonary arterial catheter will be approaching from a
wide perspective ARDS network trails which is recently under pathway. While talking about
vasodilators, many of the patients with ARDS have a mild to moderate level of pulmonary
arterial hypertension. Within this, an advanced growth within the pulmonary vascular
resistance generally has been visualised by the patients who specifically die from acute lung
injury. Within this, the main cause of the pulmonary arterial hypertension is generally
multifaceted as well as can consist a hypoxic vasoconstriction, destruction as well as barrier
of the pulmonary vascular bed and an advanced level of PEEP (Vasopressor therapy in
critically ill patients with shock, 2019).
among the ARDS patients (Fluid management in Acute Respiratory Distress Syndrome: A
narrative review, 2019). While talking about the liberal fluid management, historically the
conventional training, do not limit the administration of the fluid while having the
resuscitation phase or effectively seeking to remove the fluid during the deresuscitative
phase. Within this, the theoretic argument for a liberal management of the fluid strategy is
that it can enhance the stroke volume and thereby can enhance end organ perfusion along
with oxygen delivery (Kornas and et. al., 2021). As compared with the liberal management of
fluid strategy, a conservative strategy can limit the administration of fluid during the
resuscitation phase as well as employs the care treatment to lower the entire body fluid
balance during the deresuscitative phase. Such effective strategy can seek to decrease the
pulmonary perfusion or ventilation mismatch by restricting the pulmonary edema but might
risk as well as end-organ malfunction from reduced cardiac perfusion (Fluid Therapy and
Acute Respiratory Distress Syndrome, 2021). Furthermore, a fluid limitation can decrease the
cardiac output as well as a perfusion of tissue, that can cause or deteriorates the non-
pulmonary dysfunctioning of organs. Among various patients with acute liver injury or
ARDS, the dysfunctioning of the various organs along with systems can happen from a
systemic inflammatory response (Fluid management in ARDS: an evaluation of current
practice and the association between early diuretic use and hospital mortality, 2020).
Practice therapy in relation to vasopressor management: The vasopressor is generally
needed to encourage the systemic Blood pressure or to enhance the cardiac output among
patients with the shock. In addition to this, there is generally no clear reference or
information that any of the vasopressor or grouping of these vasopressor is higher. Within
this, the prudent methods within ARDS patients is generally to re-establish the intravascular
volume towards the euvolemic levels and then to use a vasopressor like the dopamine to
effectively attain a mean arterial pressure of about 55 to 65 mmHg.
Therefore, both the vasopressor and fluid therapy would be effectively directed by the
medical indexes of the organ perfusion. In addition, an output of urine, blood pH as well as a
base discrepancy are effectively supportive to measure the competence of perfusion of
organs. Among some of the patients, a pulmonary arterial catheter can give a beneficial
supplementary information, more specifically when there is a left ventricular dysfunctioning
or the pulmonary hypertension that is quite communal among the patients with ARDS.
Furthermore, there is a new information on the problem of management of fluid as well as the
value consisting a central venous Vs a pulmonary arterial catheter will be approaching from a
wide perspective ARDS network trails which is recently under pathway. While talking about
vasodilators, many of the patients with ARDS have a mild to moderate level of pulmonary
arterial hypertension. Within this, an advanced growth within the pulmonary vascular
resistance generally has been visualised by the patients who specifically die from acute lung
injury. Within this, the main cause of the pulmonary arterial hypertension is generally
multifaceted as well as can consist a hypoxic vasoconstriction, destruction as well as barrier
of the pulmonary vascular bed and an advanced level of PEEP (Vasopressor therapy in
critically ill patients with shock, 2019).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Books and Journals:
Ali, A. and Lamont, R.F., 2019. Recent advances in the diagnosis and management of sepsis
in pregnancy. F1000Research, 8.
Byrne, L., 2021. Fluid resuscitation in ovine sepsis: re-examining the role of a common
resuscitation therapy.
Haeberle, H., Prohaska, S., Martus, P., Straub, A., Zarbock, A., Marx, G., Zago, M., Giera,
M., Koeppen, M. and Rosenberger, P., 2020. Therapeutic iloprost for the treatment of
acute respiratory distress syndrome (ARDS)(the ThIlo trial): a prospective,
randomized, multicenter phase II study. Trials, 21(1), pp.1-11.
Haren, F.V., Byrne, L. and Litton, E., 2019. Potential harm related to fluid resuscitation in
sepsis. In Annual Update in Intensive Care and Emergency Medicine 2019 (pp. 547-
557). Springer, Cham.
Haukoos, J., Douglas, I.S. and Sasson, C., 2021. Vasopressin and steroids as adjunctive
treatment for in-hospital cardiac arrest. JAMA, 326(16), pp.1583-1585.
Kharrat, A. and Jain, A., 2022. Hemodynamic dysfunction in neonatal sepsis. Pediatric
Research, 91(2), pp.413-424.
Kornas, R.L., Owyang, C.G., Sakles, J.C., Foley, L.J. and Mosier, J.M., 2021. Evaluation and
management of the physiologically difficult airway: Consensus recommendations
from society for airway management. Anesthesia & Analgesia, 132(2), pp.395-405.
MALINVERNI, S., OCHOGAVIA, Q., LECRENIER, S., SCORPINNITI, M., Est, U.T.S.,
PREISER, J.C., COTTON, F., Pierre, M.O.L.S. and BARTIAUX, M., Vitamin D
severe deficiency in patients admitted to the Emergency Department with severe
sepsis is associated with an increased hospital mortality.
Martimbianco, A.L.C., Pacheco, R.L., Bagattini, Â.M., Padovez, R.D.F.C.M., Azevedo,
L.C.P. and Riera, R., 2022. Vitamin C-based regimens for sepsis and septic shock:
Systematic review and meta-analysis of randomized clinical trials. Journal of Critical
Care, 71, p.154099.
Shadvar, K., Nader-Djalal, N., Vahed, N., Sanaie, S., Iranpour, A., Mahmoodpoor, A.,
Vahedian-Azimi, A., Samim, A. and Rahimi-Bashar, F., 2022. Comparison of
lactate/albumin ratio to lactate and lactate clearance for predicting outcomes in
patients with septic shock admitted to intensive care unit: an observational
study. Scientific reports, 12(1), pp.1-12.
Suzuki, J., Sasabuchi, Y., Hatakeyama, S., Matsui, H., Sasahara, T., Morisawa, Y., Yamada,
T., Fushimi, K. and Yasunaga, H., 2022. Additional effect of azithromycin over β-
lactam alone for severe community-acquired pneumonia-associated acute respiratory
distress syndrome: a retrospective cohort study. Pneumonia, 14(1), pp.1-8.
Valk, Christel MA, Anissa M. Tsonas, Michela Botta, Lieuwe DJ Bos, Janesh Pillay, Ary
Serpa Neto, Marcus J. Schultz, and Frederique Paulus. "Association of early positive
end-expiratory pressure settings with ventilator-free days in patients with coronavirus
disease 2019 acute respiratory distress syndrome: a secondary analysis of the Practice
Books and Journals:
Ali, A. and Lamont, R.F., 2019. Recent advances in the diagnosis and management of sepsis
in pregnancy. F1000Research, 8.
Byrne, L., 2021. Fluid resuscitation in ovine sepsis: re-examining the role of a common
resuscitation therapy.
Haeberle, H., Prohaska, S., Martus, P., Straub, A., Zarbock, A., Marx, G., Zago, M., Giera,
M., Koeppen, M. and Rosenberger, P., 2020. Therapeutic iloprost for the treatment of
acute respiratory distress syndrome (ARDS)(the ThIlo trial): a prospective,
randomized, multicenter phase II study. Trials, 21(1), pp.1-11.
Haren, F.V., Byrne, L. and Litton, E., 2019. Potential harm related to fluid resuscitation in
sepsis. In Annual Update in Intensive Care and Emergency Medicine 2019 (pp. 547-
557). Springer, Cham.
Haukoos, J., Douglas, I.S. and Sasson, C., 2021. Vasopressin and steroids as adjunctive
treatment for in-hospital cardiac arrest. JAMA, 326(16), pp.1583-1585.
Kharrat, A. and Jain, A., 2022. Hemodynamic dysfunction in neonatal sepsis. Pediatric
Research, 91(2), pp.413-424.
Kornas, R.L., Owyang, C.G., Sakles, J.C., Foley, L.J. and Mosier, J.M., 2021. Evaluation and
management of the physiologically difficult airway: Consensus recommendations
from society for airway management. Anesthesia & Analgesia, 132(2), pp.395-405.
MALINVERNI, S., OCHOGAVIA, Q., LECRENIER, S., SCORPINNITI, M., Est, U.T.S.,
PREISER, J.C., COTTON, F., Pierre, M.O.L.S. and BARTIAUX, M., Vitamin D
severe deficiency in patients admitted to the Emergency Department with severe
sepsis is associated with an increased hospital mortality.
Martimbianco, A.L.C., Pacheco, R.L., Bagattini, Â.M., Padovez, R.D.F.C.M., Azevedo,
L.C.P. and Riera, R., 2022. Vitamin C-based regimens for sepsis and septic shock:
Systematic review and meta-analysis of randomized clinical trials. Journal of Critical
Care, 71, p.154099.
Shadvar, K., Nader-Djalal, N., Vahed, N., Sanaie, S., Iranpour, A., Mahmoodpoor, A.,
Vahedian-Azimi, A., Samim, A. and Rahimi-Bashar, F., 2022. Comparison of
lactate/albumin ratio to lactate and lactate clearance for predicting outcomes in
patients with septic shock admitted to intensive care unit: an observational
study. Scientific reports, 12(1), pp.1-12.
Suzuki, J., Sasabuchi, Y., Hatakeyama, S., Matsui, H., Sasahara, T., Morisawa, Y., Yamada,
T., Fushimi, K. and Yasunaga, H., 2022. Additional effect of azithromycin over β-
lactam alone for severe community-acquired pneumonia-associated acute respiratory
distress syndrome: a retrospective cohort study. Pneumonia, 14(1), pp.1-8.
Valk, Christel MA, Anissa M. Tsonas, Michela Botta, Lieuwe DJ Bos, Janesh Pillay, Ary
Serpa Neto, Marcus J. Schultz, and Frederique Paulus. "Association of early positive
end-expiratory pressure settings with ventilator-free days in patients with coronavirus
disease 2019 acute respiratory distress syndrome: a secondary analysis of the Practice
of VENTilation in COVID-19 study." European journal of anaesthesiology 38, no. 12
(2021): 1274.
Online:
6 Easy Steps to ABG Interpretation, 2019 [Online] Available through:
https://thenursingprof.com/blog/certification-tips/6-easy-steps-to-abg-interpretation/
Acute Respiratory Distress Syndrome, 2022 [Online] Available through:
https://www.ncbi.nlm.nih.gov/books/NBK436002/
Acute respiratory distress syndrome: Supportive care and oxygenation in adults, 2022
[Online] Available through: https://www.uptodate.com/contents/acute-respiratory-
distress-syndrome-supportive-care-and-oxygenation-in-adults
Fluid management in Acute Respiratory Distress Syndrome: A narrative review, 2019
[Online] Available through:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6591787/
Fluid management in ARDS: an evaluation of current practice and the association between
early diuretic use and hospital mortality, 2020 [Online] Available through:
https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-020-00496-7
Fluid Therapy and Acute Respiratory Distress Syndrome, 2021 [Online] Available through:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8449136/
Pathophysiology of Sepsis, 2019 [Online] available through:
https://sci-hub.se/10.1093/ajhp/59.suppl_1.S3
Pulmonary vascular dysfunction in ARDS, 2014 [Online] Available through:
https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-014-0028-6
Vasopressor therapy in critically ill patients with shock, 2019 [Online] Available through:
https://link.springer.com/article/10.1007/s00134-019-05801-z
Ventilator management strategies for adults with acute respiratory distress syndrome, 2022
[Online] Available through: https://www.uptodate.com/contents/ventilator-
management-strategies-for-adults-with-acute-respiratory-distress-
syndrome#:~:text=Most%20patients%20with%20ARDS%20require,ensure%20an
%20adequate%20oxygen%20saturation.
(2021): 1274.
Online:
6 Easy Steps to ABG Interpretation, 2019 [Online] Available through:
https://thenursingprof.com/blog/certification-tips/6-easy-steps-to-abg-interpretation/
Acute Respiratory Distress Syndrome, 2022 [Online] Available through:
https://www.ncbi.nlm.nih.gov/books/NBK436002/
Acute respiratory distress syndrome: Supportive care and oxygenation in adults, 2022
[Online] Available through: https://www.uptodate.com/contents/acute-respiratory-
distress-syndrome-supportive-care-and-oxygenation-in-adults
Fluid management in Acute Respiratory Distress Syndrome: A narrative review, 2019
[Online] Available through:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6591787/
Fluid management in ARDS: an evaluation of current practice and the association between
early diuretic use and hospital mortality, 2020 [Online] Available through:
https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-020-00496-7
Fluid Therapy and Acute Respiratory Distress Syndrome, 2021 [Online] Available through:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8449136/
Pathophysiology of Sepsis, 2019 [Online] available through:
https://sci-hub.se/10.1093/ajhp/59.suppl_1.S3
Pulmonary vascular dysfunction in ARDS, 2014 [Online] Available through:
https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-014-0028-6
Vasopressor therapy in critically ill patients with shock, 2019 [Online] Available through:
https://link.springer.com/article/10.1007/s00134-019-05801-z
Ventilator management strategies for adults with acute respiratory distress syndrome, 2022
[Online] Available through: https://www.uptodate.com/contents/ventilator-
management-strategies-for-adults-with-acute-respiratory-distress-
syndrome#:~:text=Most%20patients%20with%20ARDS%20require,ensure%20an
%20adequate%20oxygen%20saturation.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





