Analysis of Australia's 'No Jab, No Pay' Policy & US Relevance
VerifiedAdded on 2022/09/14
|2
|2153
|27
Report
AI Summary
This report examines Australia's 'No Jab, No Pay' legislation, which links families' eligibility for government welfare and benefits to the immunization status of their children. The policy, implemented to address low vaccination rates, denies benefits to families whose children are not up-to-date on their vaccinations, with limited medical exemptions. The report discusses the potential relevance, legality, and ethical considerations of such a program in the United States, where some state-based welfare programs already have similar links. While the Australian program has shown some success in increasing immunization rates, concerns remain about its disproportionate impact on low-income families and potential adverse consequences for children. The analysis concludes by considering the trade-offs and design details necessary for such a policy to be acceptable and effective in addressing gaps in immunization coverage.
Copyright 2017 American Medical Association. All rights reserved.
Linking Immunization Status and Eligibility
for Welfare and Benefits Payments
The Australian “No Jab, No Pay” Legislation
The recent outbreaks of vaccine-preventable dis-
eases have refocused attention on the threat posed by
unvaccinated and undervaccinated individuals.1Gov-
ernments around the world have responded by strength-
ening laws and policies directed at increasing vaccina-
tion rates. The standard menu of options includes
education and information initiatives, incentives, and
mandates; these may be directed at the general public,
health care organizations, or practitioners.
The term mandate is somewhat misleading, because
there are exceptions1
—always on medical grounds, fre-
quently on religious grounds, and sometimes on philo-
sophical grounds. Moreover, the thrust of mandates is not
to forcibly require vaccination but to predicate eligibility
for a service or benefit on adherence to the recommended
immunizationscheduleofvaccination.IntheUnitedStates,
every state requires proof of immunization for entry into
public schools, and some states also have similar require-
ments for entry into day care facilities and private schools.
These requirements can seem coercive to families who do
not have other feasible schooling or child care options.
However, the logic and acceptability of these requirements
are rooted in the fact that the risks posed by clusters of non-
immunized children are heightened in these very settings.
In Australia, half of its 6 states and 2 territories have
vaccine requirements for school entry, and the 3 most
populous states (New South Wales,Victoria,and
Queensland) recently extended such requirements for
entry to kindergartens and child care facilities. These
rules overlay a more controversial policy: for nearly 20
years, the Australian government has linked families’ eli-
gibility for government welfare and benefits to chil-
dren’s vaccination status. In this Viewpoint, we de-
scribe a recent expansion of the Australian program and
consider the relevance, legality, and ethics of such an ap-
proach in the United States.
No Jab, No Pay
In the mid-1990s, vaccination rates were dangerously
low in Australia: only half of all children had the nation-
ally recommended immunization coverage. To address
the problem, the federal government implemented a
multipronged strategy that is widely regarded as hav-
ing been successful. The welfare incentive program was
one component of the strategy.
In 2015, a controversial new law— titled, “No Jab,
No Pay”—expanded the program and substantially in-
creased the incentives.2Effective January 1, 2016, fami-
lies’ eligibility for federal benefits worth up to US $15 000
per child per year (Table) depends on the immuniza-
tion status of all family members through 19 years of
age.2 The benefits are unavailable to families for each
year in which an otherwise eligible family member in this
age group does not have the recommended vaccines for
1-, 2-, and 5-year-olds or is not participating in an immu-
nization catch-up program.2 The law also ended “con-
scientious objections” as a basis for exemptions,2 fol-
lowing the termination of religious exemptions earlier in
the year. Only medical exemptions remain, which may
be granted after a physician attests to the existence of
a disqualifying condition, such as certain allergies and im-
munocompromising illnesses.
The government has projected a savings over 5 years
of US $380 million from the new law.3About half the es-
timated savings is expected to come from benefits not
paid, with an estimated 10 000 families expected to lose
eligibility for payments in 2016-2017 alone.3 Although
the effects of the law have yet to be formally evalu-
ated, the government recently announced that 5738 pre-
viously unvaccinated children in families receiving ben-
efits were immunized in the first 6 months of the new
law’s effective date, and 187 695 children who were lag-
ging on the recommended vaccination schedule had
caught up.4,5With a total of approximately 5 million chil-
dren in Australia, these are substantial shifts.
Existing Incentives for Welfare Beneficiaries
in the United States
In the United States, a number of state-based welfare
programs already link welfare payments to vaccination
status. For example, in California’s CalWORKs welfare
program, families who fail to submit up-to-date immu-
nization records or an exemption form for children
younger than 6 years risk losing part of their cash assis-
tance. Florida’s Temporary Cash Assistance program may
withhold benefits from families with children younger
than 5 years whose immunizations are not up to date.
At the federal level, the Special Supplemental Nutrition
Program for Women, Infants, and Children checks the im-
munization status of preschool children and encour-
ages adherence with the recommended schedule.
However, stern approaches such as these are not
widespread in the United States. Questions regarding
whether they are warranted, lawful, and ethically ac-
ceptable warrant attention.
Prospects of No Jab, No Pay in the United States
A program designed to increase adherence with immu-
nizations directed at welfare recipients would seem arbi-
trary, even discriminatory, unless vaccination rates in this
population were especially low. Various state and fed-
eral initiatives over the last 20 years, most notably the
VIEWPOINT
Y. Tony Yang, ScD,
LLM, MPH
Department of Health
Administration and
Policy, George Mason
University, Fairfax,
Virginia.
David M. Studdert,
LLB, ScD, MPH
Stanford University
School of Medicine and
Stanford Law School,
Stanford, California.
Corresponding
Author: Y. Tony Yang,
ScD, LLM, MPH,
Department of Health
Administration and
Policy, George Mason
University, MS: 1J3,
4400 University Dr,
Fairfax, VA 22030
(ytyang@gmu.edu).
Opinion
jama.com (Reprinted)JAMA February 28, 2017Volume 317, Number 8803
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/936072/ by a STANFORD Univ Med Center User on 03/02/2017
Linking Immunization Status and Eligibility
for Welfare and Benefits Payments
The Australian “No Jab, No Pay” Legislation
The recent outbreaks of vaccine-preventable dis-
eases have refocused attention on the threat posed by
unvaccinated and undervaccinated individuals.1Gov-
ernments around the world have responded by strength-
ening laws and policies directed at increasing vaccina-
tion rates. The standard menu of options includes
education and information initiatives, incentives, and
mandates; these may be directed at the general public,
health care organizations, or practitioners.
The term mandate is somewhat misleading, because
there are exceptions1
—always on medical grounds, fre-
quently on religious grounds, and sometimes on philo-
sophical grounds. Moreover, the thrust of mandates is not
to forcibly require vaccination but to predicate eligibility
for a service or benefit on adherence to the recommended
immunizationscheduleofvaccination.IntheUnitedStates,
every state requires proof of immunization for entry into
public schools, and some states also have similar require-
ments for entry into day care facilities and private schools.
These requirements can seem coercive to families who do
not have other feasible schooling or child care options.
However, the logic and acceptability of these requirements
are rooted in the fact that the risks posed by clusters of non-
immunized children are heightened in these very settings.
In Australia, half of its 6 states and 2 territories have
vaccine requirements for school entry, and the 3 most
populous states (New South Wales,Victoria,and
Queensland) recently extended such requirements for
entry to kindergartens and child care facilities. These
rules overlay a more controversial policy: for nearly 20
years, the Australian government has linked families’ eli-
gibility for government welfare and benefits to chil-
dren’s vaccination status. In this Viewpoint, we de-
scribe a recent expansion of the Australian program and
consider the relevance, legality, and ethics of such an ap-
proach in the United States.
No Jab, No Pay
In the mid-1990s, vaccination rates were dangerously
low in Australia: only half of all children had the nation-
ally recommended immunization coverage. To address
the problem, the federal government implemented a
multipronged strategy that is widely regarded as hav-
ing been successful. The welfare incentive program was
one component of the strategy.
In 2015, a controversial new law— titled, “No Jab,
No Pay”—expanded the program and substantially in-
creased the incentives.2Effective January 1, 2016, fami-
lies’ eligibility for federal benefits worth up to US $15 000
per child per year (Table) depends on the immuniza-
tion status of all family members through 19 years of
age.2 The benefits are unavailable to families for each
year in which an otherwise eligible family member in this
age group does not have the recommended vaccines for
1-, 2-, and 5-year-olds or is not participating in an immu-
nization catch-up program.2 The law also ended “con-
scientious objections” as a basis for exemptions,2 fol-
lowing the termination of religious exemptions earlier in
the year. Only medical exemptions remain, which may
be granted after a physician attests to the existence of
a disqualifying condition, such as certain allergies and im-
munocompromising illnesses.
The government has projected a savings over 5 years
of US $380 million from the new law.3About half the es-
timated savings is expected to come from benefits not
paid, with an estimated 10 000 families expected to lose
eligibility for payments in 2016-2017 alone.3 Although
the effects of the law have yet to be formally evalu-
ated, the government recently announced that 5738 pre-
viously unvaccinated children in families receiving ben-
efits were immunized in the first 6 months of the new
law’s effective date, and 187 695 children who were lag-
ging on the recommended vaccination schedule had
caught up.4,5With a total of approximately 5 million chil-
dren in Australia, these are substantial shifts.
Existing Incentives for Welfare Beneficiaries
in the United States
In the United States, a number of state-based welfare
programs already link welfare payments to vaccination
status. For example, in California’s CalWORKs welfare
program, families who fail to submit up-to-date immu-
nization records or an exemption form for children
younger than 6 years risk losing part of their cash assis-
tance. Florida’s Temporary Cash Assistance program may
withhold benefits from families with children younger
than 5 years whose immunizations are not up to date.
At the federal level, the Special Supplemental Nutrition
Program for Women, Infants, and Children checks the im-
munization status of preschool children and encour-
ages adherence with the recommended schedule.
However, stern approaches such as these are not
widespread in the United States. Questions regarding
whether they are warranted, lawful, and ethically ac-
ceptable warrant attention.
Prospects of No Jab, No Pay in the United States
A program designed to increase adherence with immu-
nizations directed at welfare recipients would seem arbi-
trary, even discriminatory, unless vaccination rates in this
population were especially low. Various state and fed-
eral initiatives over the last 20 years, most notably the
VIEWPOINT
Y. Tony Yang, ScD,
LLM, MPH
Department of Health
Administration and
Policy, George Mason
University, Fairfax,
Virginia.
David M. Studdert,
LLB, ScD, MPH
Stanford University
School of Medicine and
Stanford Law School,
Stanford, California.
Corresponding
Author: Y. Tony Yang,
ScD, LLM, MPH,
Department of Health
Administration and
Policy, George Mason
University, MS: 1J3,
4400 University Dr,
Fairfax, VA 22030
(ytyang@gmu.edu).
Opinion
jama.com (Reprinted)JAMA February 28, 2017Volume 317, Number 8803
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/936072/ by a STANFORD Univ Med Center User on 03/02/2017
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Copyright 2017 American Medical Association. All rights reserved.
national Vaccines for Children program,6 have substantially in-
creased the proportion of preschool children in low-income families
who receive recommended vaccinations. Nevertheless, low-income
remains a significant risk factor for incomplete immunization.6,7For
example, the 2015 National Immunization Survey indicated that
in households below the poverty level, the proportion of 19- to
35-month-old children with the recommended coverage across a
range of vaccines was 3 to 10 percentage points lower than among
children of the same age living in households above the poverty line.7
The association between low-income and undervaccination is some-
times obscured by the considerable attention focused on the large
number of nonmedical exemptions claimed by white, high-income
families.8It is debatable how much weight disproportionately low cov-
erage among children in low-income households should carry. Some
will argue that linking welfare eligibility to vaccination status remains
indefensible unless the government can demonstrate that lack of im-
munization is not due to problems of access or cost.
Two lines of jurisprudence in US law converge to support the con-
stitutionality of programs that condition welfare benefits on vaccina-
tion status. First, governments have long enjoyed broad legal author-
ity to require vaccinations in the name of public health.9 This authority
permits conditioning receipt of services (eg, public schooling) on ad-
herence and penalizing nonadherence. Second, because welfare pay-
ments are not a constitutionally protected right, governments have
considerable latitude in how they distribute those payments and are
permitted to make distinctions among recipients. Distinctions made
on the basis of constitutionally protected categories, such as race and
sex, are unlikely to survive judicial review. However, a broad distinc-
tion based on adherence with a clinically recommended vaccination
schedule likely would. To the best of our knowledge, the existing state
programs that link welfare payments to vaccination status have not
encountered serious legal challenge.
Conditioning welfare payments on vaccination status also pro-
vokes a number of ethical concerns. The policy disproportionately
affects the poor. Critics have also charged that it harms the very chil-
dren it is intended to help: in addition to missing the vaccination,
affected children experience adverse consequences from the re-
duction in financial support. Other objections point to undesirable
collateral effects, including victimizing “violators,” perpetuating dis-
advantage, fueling distrust of government and the public health
system, and unhelpfully drawing attention away from barriers to
vaccination such as lack of access, time, and education.
The realities of how choices about childhood vaccinations are
made complicate the ethical calculus. The fact that children may lose
benefits because of a decision their parents made is troubling. On
the other hand, if the law prompts parents who would not other-
wise have vaccinated their children to do so, those children avoid
risks their parents have imposed on them.
These are difficult trade-offs. For many, the question of accept-
ability may come down to details of program design, such as the ac-
cessibility and cost of the required vaccinations, how often pay-
ments are actually withheld, and how important a public health
problem immunization coverage is among the subgroups affected.
Conclusions
The sporadic reemergence of vaccine-preventable illnesses has ex-
posed gaps in the laws and policies that surround one of public
health’s most successful interventions. If outbreaks of vaccine-
preventable disease spread, state and federal governments could
be expected to consider strong measures to plug those gaps. The
Australian experience may be instructive. It may attract special in-
terest in places where immunization coverage among welfare-
dependent families is disproportionately low and themes of per-
sonal responsibility have strong political traction.
ARTICLE INFORMATION
Conflict of Interest Disclosures: All authors have
completed and submitted the ICMJE Form for
Disclosure of Potential Conflicts of Interest and
none were reported.
REFERENCES
1.Phadke VK, Bednarczyk RA, Salmon DA, Omer
SB. Association between vaccine refusal and
vaccine-preventable diseases in the United States:
a review of measles and pertussis. JAMA. 2016;
315(11):1149-1158.
2. Parliament of the Commonwealth of Australia.
Social Services Legislation Amendment
(No Jab, No Pay) Bill 2015. http://www.aph.gov.au
/Parliamentary_Business/Bills_Legislation/Bills
_Search_Results/Result?bId=r5540. Accessed
January 27, 2017.
3. Klapdor M, Grove A. Parliament of the
Commonwealth of Australia website. ‘No Jab No
Pay’ and other immunisation measures. http://www
.aph.gov.au/about_parliament/parliamentary
_departments/parliamentary_library/pubs/rp
/budgetreview201516/vaccination#_ftn7. Published
May 2015. Accessed November 30, 2016.
4. Minister for Social Services. No jab, no pay
lifts immunisation rates. http://christianporter
.dss.gov.au/media-releases/no-jab-no-pay-lifts
-immunisation-rates. Published July 31, 2016.
Accessed November 30, 2016.
5. Minister for Social Services. Tasmania leads
childhood immunisation rate improvement
as indigenous immunisation rates soar.
http://christianporter.dss.gov.au/media-releases
/20161106-immunisation. Published November 6,
2016. Accessed November 30, 2016.
6. Lieu TA, Ray GT, Klein NP, Chung C, Kulldorff M.
Geographic clusters in underimmunization and
vaccine refusal. Pediatrics. 2015;135(2):280-289.
7. Hill HA, Elam-Evans LD, Yankey D, Singleton JA,
Dietz V. Vaccination coverage among children aged
19-35 months—United States, 2015. MMWR Morb
Mortal Wkly Rep. 2016;65(39):1065-1071.
8. Yang YT, Delamater PL, Leslie TF, Mello MM.
Sociodemographic predictors of vaccination
exemptions on the basis of personal belief in
California. Am J Public Health. 2016;106(1):172-177.
9. Jacobson v Commonwealth of Massachusetts,
197 US 11 (1905).
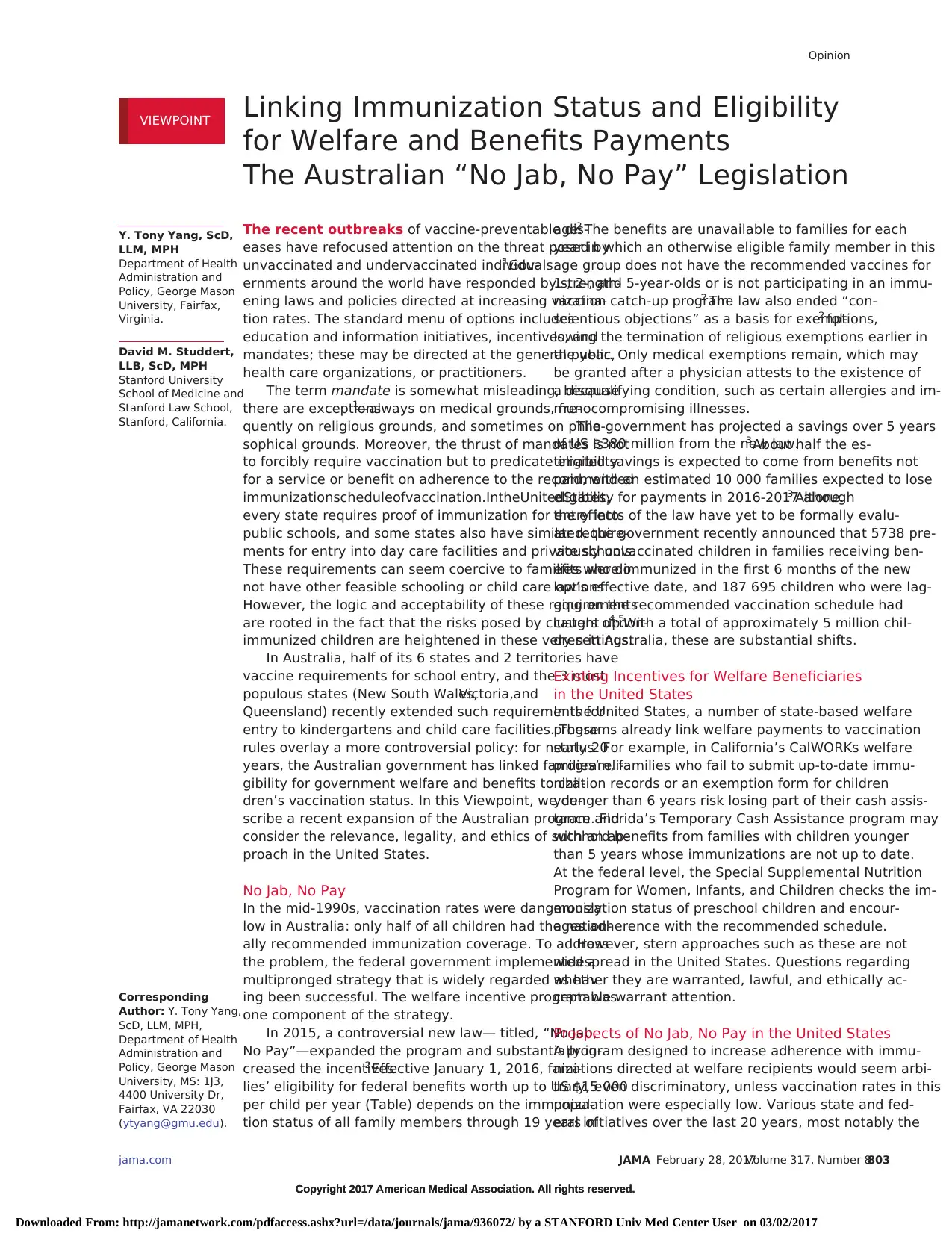
Table. Federal Benefits Conditioned on Children’s Immunization Status in Australia
Program Description Income Tested?
Value per Child
per Year in 2016, A$a
Child care benefit Helps meet costs of approved and registered care (eg, long-term, family,
or occasional day care; vacation care; preschool and kindergarten)
Yes ≤11 024
Child care rebate Covers 50% of out-of-pocket child care expenses for approved child care,
up to an annual limit per child
No ≤7500
Family tax benefit part A end-of-year
supplement (“family assistance payments”)
Payment to assist families with costs of raising children Yes ≤726
a Dollar amounts are current as of September 2016. Between December 1, 2015, and November 30, 2016, the Australian dollar averaged US $0.75.
Opinion Viewpoint
804 JAMA February 28, 2017Volume 317, Number 8(Reprinted) jama.com
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/936072/ by a STANFORD Univ Med Center User on 03/02/2017
national Vaccines for Children program,6 have substantially in-
creased the proportion of preschool children in low-income families
who receive recommended vaccinations. Nevertheless, low-income
remains a significant risk factor for incomplete immunization.6,7For
example, the 2015 National Immunization Survey indicated that
in households below the poverty level, the proportion of 19- to
35-month-old children with the recommended coverage across a
range of vaccines was 3 to 10 percentage points lower than among
children of the same age living in households above the poverty line.7
The association between low-income and undervaccination is some-
times obscured by the considerable attention focused on the large
number of nonmedical exemptions claimed by white, high-income
families.8It is debatable how much weight disproportionately low cov-
erage among children in low-income households should carry. Some
will argue that linking welfare eligibility to vaccination status remains
indefensible unless the government can demonstrate that lack of im-
munization is not due to problems of access or cost.
Two lines of jurisprudence in US law converge to support the con-
stitutionality of programs that condition welfare benefits on vaccina-
tion status. First, governments have long enjoyed broad legal author-
ity to require vaccinations in the name of public health.9 This authority
permits conditioning receipt of services (eg, public schooling) on ad-
herence and penalizing nonadherence. Second, because welfare pay-
ments are not a constitutionally protected right, governments have
considerable latitude in how they distribute those payments and are
permitted to make distinctions among recipients. Distinctions made
on the basis of constitutionally protected categories, such as race and
sex, are unlikely to survive judicial review. However, a broad distinc-
tion based on adherence with a clinically recommended vaccination
schedule likely would. To the best of our knowledge, the existing state
programs that link welfare payments to vaccination status have not
encountered serious legal challenge.
Conditioning welfare payments on vaccination status also pro-
vokes a number of ethical concerns. The policy disproportionately
affects the poor. Critics have also charged that it harms the very chil-
dren it is intended to help: in addition to missing the vaccination,
affected children experience adverse consequences from the re-
duction in financial support. Other objections point to undesirable
collateral effects, including victimizing “violators,” perpetuating dis-
advantage, fueling distrust of government and the public health
system, and unhelpfully drawing attention away from barriers to
vaccination such as lack of access, time, and education.
The realities of how choices about childhood vaccinations are
made complicate the ethical calculus. The fact that children may lose
benefits because of a decision their parents made is troubling. On
the other hand, if the law prompts parents who would not other-
wise have vaccinated their children to do so, those children avoid
risks their parents have imposed on them.
These are difficult trade-offs. For many, the question of accept-
ability may come down to details of program design, such as the ac-
cessibility and cost of the required vaccinations, how often pay-
ments are actually withheld, and how important a public health
problem immunization coverage is among the subgroups affected.
Conclusions
The sporadic reemergence of vaccine-preventable illnesses has ex-
posed gaps in the laws and policies that surround one of public
health’s most successful interventions. If outbreaks of vaccine-
preventable disease spread, state and federal governments could
be expected to consider strong measures to plug those gaps. The
Australian experience may be instructive. It may attract special in-
terest in places where immunization coverage among welfare-
dependent families is disproportionately low and themes of per-
sonal responsibility have strong political traction.
ARTICLE INFORMATION
Conflict of Interest Disclosures: All authors have
completed and submitted the ICMJE Form for
Disclosure of Potential Conflicts of Interest and
none were reported.
REFERENCES
1.Phadke VK, Bednarczyk RA, Salmon DA, Omer
SB. Association between vaccine refusal and
vaccine-preventable diseases in the United States:
a review of measles and pertussis. JAMA. 2016;
315(11):1149-1158.
2. Parliament of the Commonwealth of Australia.
Social Services Legislation Amendment
(No Jab, No Pay) Bill 2015. http://www.aph.gov.au
/Parliamentary_Business/Bills_Legislation/Bills
_Search_Results/Result?bId=r5540. Accessed
January 27, 2017.
3. Klapdor M, Grove A. Parliament of the
Commonwealth of Australia website. ‘No Jab No
Pay’ and other immunisation measures. http://www
.aph.gov.au/about_parliament/parliamentary
_departments/parliamentary_library/pubs/rp
/budgetreview201516/vaccination#_ftn7. Published
May 2015. Accessed November 30, 2016.
4. Minister for Social Services. No jab, no pay
lifts immunisation rates. http://christianporter
.dss.gov.au/media-releases/no-jab-no-pay-lifts
-immunisation-rates. Published July 31, 2016.
Accessed November 30, 2016.
5. Minister for Social Services. Tasmania leads
childhood immunisation rate improvement
as indigenous immunisation rates soar.
http://christianporter.dss.gov.au/media-releases
/20161106-immunisation. Published November 6,
2016. Accessed November 30, 2016.
6. Lieu TA, Ray GT, Klein NP, Chung C, Kulldorff M.
Geographic clusters in underimmunization and
vaccine refusal. Pediatrics. 2015;135(2):280-289.
7. Hill HA, Elam-Evans LD, Yankey D, Singleton JA,
Dietz V. Vaccination coverage among children aged
19-35 months—United States, 2015. MMWR Morb
Mortal Wkly Rep. 2016;65(39):1065-1071.
8. Yang YT, Delamater PL, Leslie TF, Mello MM.
Sociodemographic predictors of vaccination
exemptions on the basis of personal belief in
California. Am J Public Health. 2016;106(1):172-177.
9. Jacobson v Commonwealth of Massachusetts,
197 US 11 (1905).
Table. Federal Benefits Conditioned on Children’s Immunization Status in Australia
Program Description Income Tested?
Value per Child
per Year in 2016, A$a
Child care benefit Helps meet costs of approved and registered care (eg, long-term, family,
or occasional day care; vacation care; preschool and kindergarten)
Yes ≤11 024
Child care rebate Covers 50% of out-of-pocket child care expenses for approved child care,
up to an annual limit per child
No ≤7500
Family tax benefit part A end-of-year
supplement (“family assistance payments”)
Payment to assist families with costs of raising children Yes ≤726
a Dollar amounts are current as of September 2016. Between December 1, 2015, and November 30, 2016, the Australian dollar averaged US $0.75.
Opinion Viewpoint
804 JAMA February 28, 2017Volume 317, Number 8(Reprinted) jama.com
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/936072/ by a STANFORD Univ Med Center User on 03/02/2017
1 out of 2
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.