Immunology Assignment: Cytokines, Vaccination, and Immune Responses
VerifiedAdded on 2022/09/02
|11
|2415
|18
Homework Assignment
AI Summary
This immunology assignment explores various aspects of the immune system. It begins by examining the synergistic effects of vaccination and adjuvants, followed by a discussion of clinical immunological techniques such as ELISA and immunoblot. The assignment then delves into the structure and function of antibodies, differentiating between antigens and immunogens. Further topics include the therapeutic potential of cytokines, comparing and contrasting innate and adaptive immunity, and analyzing Type I hypersensitivity reactions. Additionally, the assignment investigates the mechanisms behind cytokine storms and potential therapeutic targets, along with an analysis of the immunological events during the TGN1412 monoclonal antibody drug trial and a review of different types of vaccinations, providing a comprehensive overview of immunological principles and applications.

Running head: IMMUNOLOGY
IMMUNOLOGY
Name of the student:
Name of the university:
Author note
IMMUNOLOGY
Name of the student:
Name of the university:
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Question 1:
Impact of synergism of vaccination and adjuvants:
An adjuvant is used as an additional substance in some vaccines for creating a potential
immune response in patients. In other words, adjuvants assist vaccines to work better. Adjuvants
assist body to produce an immune response stronger immune response to prevent the disease.
Adjuvant exhibits five functional activities such as facilitate translocation of the antigens to
lymph nodes which can be recognized by T cell, upgrade higher production of B and T cells,
amplify the cytokine release for greater production of T and B cells and increase innate immunes
response (Gregg et al. 2016). Hence, adjuvant and vaccination provide a synergistic effect for
killing antigens (Gregg et al. 2016).
Figure: vaccine and adjuvant
Source: (Gregg et al. 2016).
Impact of synergism of vaccination and adjuvants:
An adjuvant is used as an additional substance in some vaccines for creating a potential
immune response in patients. In other words, adjuvants assist vaccines to work better. Adjuvants
assist body to produce an immune response stronger immune response to prevent the disease.
Adjuvant exhibits five functional activities such as facilitate translocation of the antigens to
lymph nodes which can be recognized by T cell, upgrade higher production of B and T cells,
amplify the cytokine release for greater production of T and B cells and increase innate immunes
response (Gregg et al. 2016). Hence, adjuvant and vaccination provide a synergistic effect for
killing antigens (Gregg et al. 2016).
Figure: vaccine and adjuvant
Source: (Gregg et al. 2016).
Question 2:
Two application of clinical immunological techniques:
The two most frequently used immunological techniques in the clinical setting include
ELISA and immuno-blot. ELISA or enzyme-linked immunosorbent assay is a plate-based assay
technique that is used for detecting as well as quantifying peptides, protein, and antibodies
(Aydin 2015). The common application of enzyme-linked immunosorbent assay includes
detection of a potential allergen in food technology, detection of disease outbreak and transition,
detections of drug allergens, pregnancy hormones and detection of antigen in the blood due to
previous exposure (Shih et al. 2016).
On the other hand, immunoblot is a sensitive assay that is used for detecting and
characterizing proteins that work by manipulating the specificity intrinsic in antigen-antibody
recognition (Solimani et al. 2019). Compared to ELISA, it is used in detecting the single protein
and post-translation modification of the protein during disease.
Question 3:
Structure related function of antibodies in the host immunity:
Antibodies are made up of two regions such as Fc and Fab regions where both
participate in host immunity. Considering the Fc region, it is a protein that is found on the cell
surface of immune cells like B lymphocytes, macrophages, natural killer cells and other immune
cells. It is the tail region of the antibody that interacts with some protein of complement system
(Saxen and Wu 2016). This property permits antibodies to activate the immune system and
amplify the response. On the other hand, Fab is considered as antigen-binding region present on
the surface of the antibodies and consists of one constant as well as one variable domain of light
Two application of clinical immunological techniques:
The two most frequently used immunological techniques in the clinical setting include
ELISA and immuno-blot. ELISA or enzyme-linked immunosorbent assay is a plate-based assay
technique that is used for detecting as well as quantifying peptides, protein, and antibodies
(Aydin 2015). The common application of enzyme-linked immunosorbent assay includes
detection of a potential allergen in food technology, detection of disease outbreak and transition,
detections of drug allergens, pregnancy hormones and detection of antigen in the blood due to
previous exposure (Shih et al. 2016).
On the other hand, immunoblot is a sensitive assay that is used for detecting and
characterizing proteins that work by manipulating the specificity intrinsic in antigen-antibody
recognition (Solimani et al. 2019). Compared to ELISA, it is used in detecting the single protein
and post-translation modification of the protein during disease.
Question 3:
Structure related function of antibodies in the host immunity:
Antibodies are made up of two regions such as Fc and Fab regions where both
participate in host immunity. Considering the Fc region, it is a protein that is found on the cell
surface of immune cells like B lymphocytes, macrophages, natural killer cells and other immune
cells. It is the tail region of the antibody that interacts with some protein of complement system
(Saxen and Wu 2016). This property permits antibodies to activate the immune system and
amplify the response. On the other hand, Fab is considered as antigen-binding region present on
the surface of the antibodies and consists of one constant as well as one variable domain of light
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
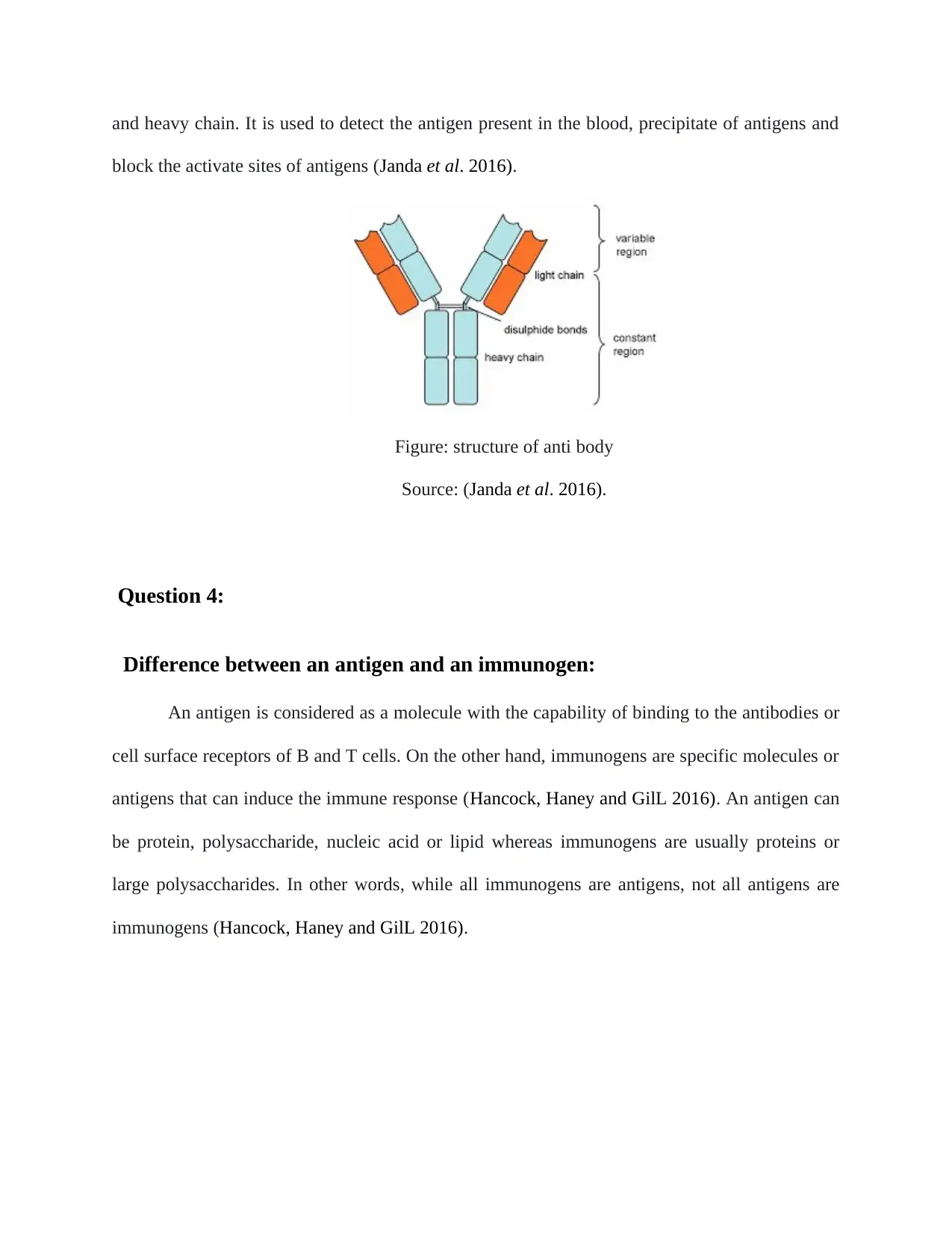
and heavy chain. It is used to detect the antigen present in the blood, precipitate of antigens and
block the activate sites of antigens (Janda et al. 2016).
Figure: structure of anti body
Source: (Janda et al. 2016).
Question 4:
Difference between an antigen and an immunogen:
An antigen is considered as a molecule with the capability of binding to the antibodies or
cell surface receptors of B and T cells. On the other hand, immunogens are specific molecules or
antigens that can induce the immune response (Hancock, Haney and GilL 2016). An antigen can
be protein, polysaccharide, nucleic acid or lipid whereas immunogens are usually proteins or
large polysaccharides. In other words, while all immunogens are antigens, not all antigens are
immunogens (Hancock, Haney and GilL 2016).
block the activate sites of antigens (Janda et al. 2016).
Figure: structure of anti body
Source: (Janda et al. 2016).
Question 4:
Difference between an antigen and an immunogen:
An antigen is considered as a molecule with the capability of binding to the antibodies or
cell surface receptors of B and T cells. On the other hand, immunogens are specific molecules or
antigens that can induce the immune response (Hancock, Haney and GilL 2016). An antigen can
be protein, polysaccharide, nucleic acid or lipid whereas immunogens are usually proteins or
large polysaccharides. In other words, while all immunogens are antigens, not all antigens are
immunogens (Hancock, Haney and GilL 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Question 5:
Cytokines as therapeutic targets:
Cytokines are often played a crucial role in the pathogenesis of the inflammatory disease
and autoimmune disease. Cytokines trigger for the breakdown as well as subsequent events
which lead to production T helper cells, IL17 and IL23 that resulted in amplified immune
response amongst patients with autoimmune disease (McInnes, Buckley and Isaacs 2016). In this
context, targeting cytokines in the antibody therapy may reduce amplified actions of interleukins
and antibodies which further minimize inflammatory responses of the patients.
Question 6:
Common features of the innate and adaptive immunity:
The first common feature of innate immunity and adaptive immunity is that both
immune systems are activated by T cells. However, while the innate immune system uses
cytotoxic T cells for activation of immune response, the adaptive immune system use T helper
cells for activation of the immune response (Berry and Call 2017). The second common feature
of innate immunity and adaptive immunity is that both systems use macrophage in their immune
response. However, while the innate immune system uses macrophages for killing and
phagocytosis of the microorganism, adaptive immune systems use macrophages for the
presentation of a phagocytised organism to T lymphocytes (Annunziato, Romagnani and
Romagnani 2015). The third common feature the innate immunity and adaptive immunity is that
both activated by the complement system. While the innate immune system is triggered by the
alternative pathway of the complement system, the adaptive immune system is stimulated by the
classical pathway.
Cytokines as therapeutic targets:
Cytokines are often played a crucial role in the pathogenesis of the inflammatory disease
and autoimmune disease. Cytokines trigger for the breakdown as well as subsequent events
which lead to production T helper cells, IL17 and IL23 that resulted in amplified immune
response amongst patients with autoimmune disease (McInnes, Buckley and Isaacs 2016). In this
context, targeting cytokines in the antibody therapy may reduce amplified actions of interleukins
and antibodies which further minimize inflammatory responses of the patients.
Question 6:
Common features of the innate and adaptive immunity:
The first common feature of innate immunity and adaptive immunity is that both
immune systems are activated by T cells. However, while the innate immune system uses
cytotoxic T cells for activation of immune response, the adaptive immune system use T helper
cells for activation of the immune response (Berry and Call 2017). The second common feature
of innate immunity and adaptive immunity is that both systems use macrophage in their immune
response. However, while the innate immune system uses macrophages for killing and
phagocytosis of the microorganism, adaptive immune systems use macrophages for the
presentation of a phagocytised organism to T lymphocytes (Annunziato, Romagnani and
Romagnani 2015). The third common feature the innate immunity and adaptive immunity is that
both activated by the complement system. While the innate immune system is triggered by the
alternative pathway of the complement system, the adaptive immune system is stimulated by the
classical pathway.
Question 7:
Type I hypersensitivity reaction:
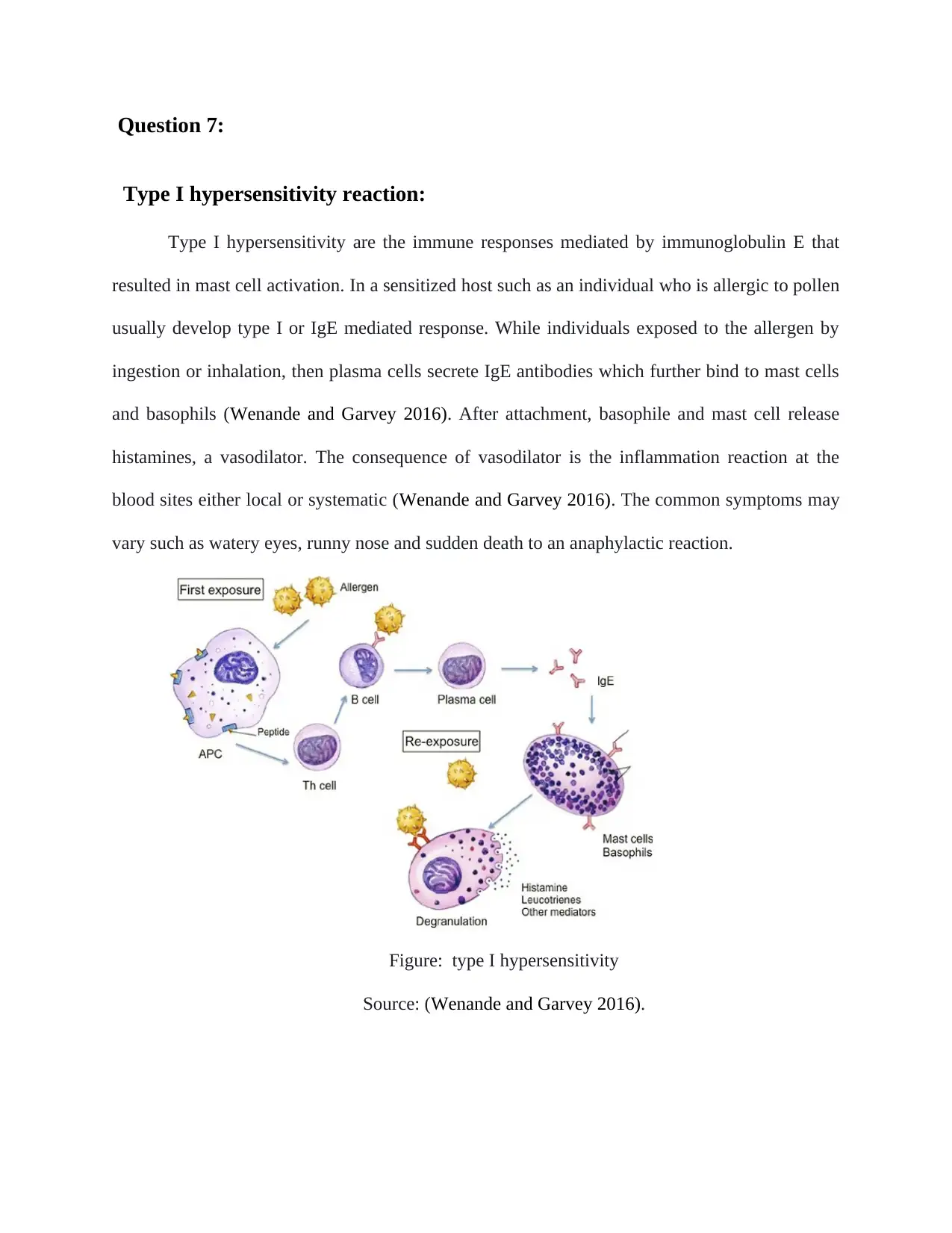
Type I hypersensitivity are the immune responses mediated by immunoglobulin E that
resulted in mast cell activation. In a sensitized host such as an individual who is allergic to pollen
usually develop type I or IgE mediated response. While individuals exposed to the allergen by
ingestion or inhalation, then plasma cells secrete IgE antibodies which further bind to mast cells
and basophils (Wenande and Garvey 2016). After attachment, basophile and mast cell release
histamines, a vasodilator. The consequence of vasodilator is the inflammation reaction at the
blood sites either local or systematic (Wenande and Garvey 2016). The common symptoms may
vary such as watery eyes, runny nose and sudden death to an anaphylactic reaction.
Figure: type I hypersensitivity
Source: (Wenande and Garvey 2016).
Type I hypersensitivity reaction:
Type I hypersensitivity are the immune responses mediated by immunoglobulin E that
resulted in mast cell activation. In a sensitized host such as an individual who is allergic to pollen
usually develop type I or IgE mediated response. While individuals exposed to the allergen by
ingestion or inhalation, then plasma cells secrete IgE antibodies which further bind to mast cells
and basophils (Wenande and Garvey 2016). After attachment, basophile and mast cell release
histamines, a vasodilator. The consequence of vasodilator is the inflammation reaction at the
blood sites either local or systematic (Wenande and Garvey 2016). The common symptoms may
vary such as watery eyes, runny nose and sudden death to an anaphylactic reaction.
Figure: type I hypersensitivity
Source: (Wenande and Garvey 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Long question:
Question 1:
The mechanism that induces cytokine storms and a potential target:
In the recent era, the cytokine storm has caught the attention of public health. Liu, Zhou
and Yang (2016), define the concept of a cytokine storm as of cytokine overproduction due to
amplified activation of the immune cells. It is often common in cases of flu infection when
immune cells are activated in the lungs. Many researchers highlighted that when the immune
cells are killing pathogens, cytokines act as a signal for immune cells such as macrophages and T
cells to mobile to infection sites. In addition, cytokine also unregulated those cells which induce
the production of more cytokines. While this feedback loop is effectively regulated, sometimes
the reaction becomes unrestrained, and a huge number of immune cells are triggered in a single
place (Chousterman, Swirski and Weber 2017). The uncontrollable reaction is caused by an
amplified response while immune cells encounter potential pathogenic invasion. Consequently,
both pro-inflammatory cytokines such as interleukin 1 and interleukin 6 and anti-cytokines such
as interleukin 10 and 1 are released (Chousterman, Swirski and Weber 2017). Additionally, it
releases more than 150 inflammatory mediators such as oxygen free radical, coagulation factors
and cytokines.
In this context, it is considered during designing therapeutic antibodies since it induces
the endothelial damage which resulted in pulmonary infiltrates, lung injury and renal failure.
Hence, the therapeutic antibodies are designed in such a way that they can regulate the cytokine
release and associated damage ((Chousterman, Swirski and Weber 2017).
Question 1:
The mechanism that induces cytokine storms and a potential target:
In the recent era, the cytokine storm has caught the attention of public health. Liu, Zhou
and Yang (2016), define the concept of a cytokine storm as of cytokine overproduction due to
amplified activation of the immune cells. It is often common in cases of flu infection when
immune cells are activated in the lungs. Many researchers highlighted that when the immune
cells are killing pathogens, cytokines act as a signal for immune cells such as macrophages and T
cells to mobile to infection sites. In addition, cytokine also unregulated those cells which induce
the production of more cytokines. While this feedback loop is effectively regulated, sometimes
the reaction becomes unrestrained, and a huge number of immune cells are triggered in a single
place (Chousterman, Swirski and Weber 2017). The uncontrollable reaction is caused by an
amplified response while immune cells encounter potential pathogenic invasion. Consequently,
both pro-inflammatory cytokines such as interleukin 1 and interleukin 6 and anti-cytokines such
as interleukin 10 and 1 are released (Chousterman, Swirski and Weber 2017). Additionally, it
releases more than 150 inflammatory mediators such as oxygen free radical, coagulation factors
and cytokines.
In this context, it is considered during designing therapeutic antibodies since it induces
the endothelial damage which resulted in pulmonary infiltrates, lung injury and renal failure.
Hence, the therapeutic antibodies are designed in such a way that they can regulate the cytokine
release and associated damage ((Chousterman, Swirski and Weber 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Question 2:
Immunological events during potentially fatal TGN1412 monoclonal antibody
drug trial:
CD28 superagonist antibodies induce activation as well as the propagation of regulatory
T cells irrespective of indication received by T-cell receptor. Regulatory CD4+CD25+ T cells
play a significant role in the inhibition of autoimmune diseases (Attarwala 2010). This activation
along with co-stimulation CD28 receptor by CD86 ligand on dendritic cells is activate T-cell.
Usually in In vitro experiments it is possible to induce activation of T cells by combination of
antibodies against T-cell receptor as well as CD28 receptor. TGN1412 (Monoclonal anti-CD28
antibody) can activate T cells by attaching to CD28 receptors irrespective of activation of the T-
cell receptor. Hence it was characterised as a CD28 superagonist (Attarwala 2010).
Consequently, due to cytokine storms, the immune responses such as TN alpha, IFN gamma, IL-
1B, IL-2 and IL4 which resulted in endothelial damage. Consequently, multiple organ failure
includes pulmonary infiltrate, cardiovascular shock, renal failure, and lung injury.
Question 3:
Application of diverse types of vaccinations:
There are several different types of vaccines that are designed to kill the diverse type of
pathogens. There are four types of vaccinations such as live attenuated vaccines, subunit or
recombinant and conjugate vaccines, inactivated vaccines and toxoid vaccines.
Live-attenuated vaccines:
Immunological events during potentially fatal TGN1412 monoclonal antibody
drug trial:
CD28 superagonist antibodies induce activation as well as the propagation of regulatory
T cells irrespective of indication received by T-cell receptor. Regulatory CD4+CD25+ T cells
play a significant role in the inhibition of autoimmune diseases (Attarwala 2010). This activation
along with co-stimulation CD28 receptor by CD86 ligand on dendritic cells is activate T-cell.
Usually in In vitro experiments it is possible to induce activation of T cells by combination of
antibodies against T-cell receptor as well as CD28 receptor. TGN1412 (Monoclonal anti-CD28
antibody) can activate T cells by attaching to CD28 receptors irrespective of activation of the T-
cell receptor. Hence it was characterised as a CD28 superagonist (Attarwala 2010).
Consequently, due to cytokine storms, the immune responses such as TN alpha, IFN gamma, IL-
1B, IL-2 and IL4 which resulted in endothelial damage. Consequently, multiple organ failure
includes pulmonary infiltrate, cardiovascular shock, renal failure, and lung injury.
Question 3:
Application of diverse types of vaccinations:
There are several different types of vaccines that are designed to kill the diverse type of
pathogens. There are four types of vaccinations such as live attenuated vaccines, subunit or
recombinant and conjugate vaccines, inactivated vaccines and toxoid vaccines.
Live-attenuated vaccines:
The live attenuated vaccines use an attenuated form of the microbes to induce immune
responses and 1 or 2 doses of live vaccines are effective in inducing an immune response (Minor
2015). The common live attenuated vaccines are used measles, mumps, rotavirus, chickenpox
and yellow fever.
Subunit, conjugate vaccines:
These vaccination use specific pieces of microbes such as protein, sugar, and capsid
since they give strong immune responses for mitigating the infection (Vartak and Sucheck 2016).
The common application of hepatitis B, HPV, meningococcal disease and shingles.
Inactivated vaccines:
Inactivated vaccines used the inhibited form of the germ which induces infection.
Inactivated vaccines do not provide immunity in one dose and require several doses as a booster
dose for ongoing immunity against disease (Sridhar, Brokstad and Cox 2015). The common
applications such as hepatitis A, Flu, polio, and rabies.
Toxoid vaccines:
These vaccines use a toxin produced by the microbes that cause disease. They create
immunity and require a booster dose to get ongoing protection (Sridhar, Brokstad and Cox
2015). The common application of vaccines such as diphtheria and tetanus.
References:
Annunziato, F., Romagnani, C. and Romagnani, S., 2015. The 3 major types of innate and
adaptive cell-mediated effector immunity. Journal of Allergy and Clinical Immunology, 135(3),
pp.626-635.
responses and 1 or 2 doses of live vaccines are effective in inducing an immune response (Minor
2015). The common live attenuated vaccines are used measles, mumps, rotavirus, chickenpox
and yellow fever.
Subunit, conjugate vaccines:
These vaccination use specific pieces of microbes such as protein, sugar, and capsid
since they give strong immune responses for mitigating the infection (Vartak and Sucheck 2016).
The common application of hepatitis B, HPV, meningococcal disease and shingles.
Inactivated vaccines:
Inactivated vaccines used the inhibited form of the germ which induces infection.
Inactivated vaccines do not provide immunity in one dose and require several doses as a booster
dose for ongoing immunity against disease (Sridhar, Brokstad and Cox 2015). The common
applications such as hepatitis A, Flu, polio, and rabies.
Toxoid vaccines:
These vaccines use a toxin produced by the microbes that cause disease. They create
immunity and require a booster dose to get ongoing protection (Sridhar, Brokstad and Cox
2015). The common application of vaccines such as diphtheria and tetanus.
References:
Annunziato, F., Romagnani, C. and Romagnani, S., 2015. The 3 major types of innate and
adaptive cell-mediated effector immunity. Journal of Allergy and Clinical Immunology, 135(3),
pp.626-635.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Attarwala H. 2010. TGN1412: From Discovery to Disaster. Journal of young pharmacists :
JYP, 2(3), 332–336. doi:10.4103/0975-1483.66810
Aydin, S., 2015. A short history, principles, and types of ELISA, and our laboratory experience
with peptide/protein analyses using ELISA. Peptides, 72, pp.4-15.
Berry, R. and Call, M.E., 2017. Modular activating receptors in innate and adaptive
immunity. Biochemistry, 56(10), pp.1383-1402.
c. The cytokine storm of severe influenza and development of immunomodulatory
therapy. Cellular & molecular immunology, 13(1), p.3.
Chousterman, B.G., Swirski, F.K. and Weber, G.F., 2017, July. Cytokine storm and sepsis
disease pathogenesis. In Seminars in immunopathology (Vol. 39, No. 5, pp. 517-528). Springer
Berlin Heidelberg.
Gregg, K.A., Harberts, E., Gardner, F.M., Pelletier, M.R., Cayatte, C., Yu, L., McCarthy, M.P.,
Marshall, J.D. and Ernst, R.K., 2017. Rationally designed TLR4 ligands for vaccine adjuvant
discovery. MBio, 8(3), pp.e00492-17.
Hancock, R.E., Haney, E.F. and Gill, E.E., 2016. The immunology of host defence peptides:
beyond antimicrobial activity. Nature Reviews Immunology, 16(5), p.321
Janda, A., Bowen, A., Greenspan, N.S. and Casadevall, A., 2016. Ig constant region effects on
variable region structure and function. Frontiers in microbiology, 7, p.22.
McInnes, I.B., Buckley, C.D. and Isaacs, J.D., 2016. Cytokines in rheumatoid arthritis—shaping
the immunological landscape. Nature Reviews Rheumatology, 12(1), p.63.
JYP, 2(3), 332–336. doi:10.4103/0975-1483.66810
Aydin, S., 2015. A short history, principles, and types of ELISA, and our laboratory experience
with peptide/protein analyses using ELISA. Peptides, 72, pp.4-15.
Berry, R. and Call, M.E., 2017. Modular activating receptors in innate and adaptive
immunity. Biochemistry, 56(10), pp.1383-1402.
c. The cytokine storm of severe influenza and development of immunomodulatory
therapy. Cellular & molecular immunology, 13(1), p.3.
Chousterman, B.G., Swirski, F.K. and Weber, G.F., 2017, July. Cytokine storm and sepsis
disease pathogenesis. In Seminars in immunopathology (Vol. 39, No. 5, pp. 517-528). Springer
Berlin Heidelberg.
Gregg, K.A., Harberts, E., Gardner, F.M., Pelletier, M.R., Cayatte, C., Yu, L., McCarthy, M.P.,
Marshall, J.D. and Ernst, R.K., 2017. Rationally designed TLR4 ligands for vaccine adjuvant
discovery. MBio, 8(3), pp.e00492-17.
Hancock, R.E., Haney, E.F. and Gill, E.E., 2016. The immunology of host defence peptides:
beyond antimicrobial activity. Nature Reviews Immunology, 16(5), p.321
Janda, A., Bowen, A., Greenspan, N.S. and Casadevall, A., 2016. Ig constant region effects on
variable region structure and function. Frontiers in microbiology, 7, p.22.
McInnes, I.B., Buckley, C.D. and Isaacs, J.D., 2016. Cytokines in rheumatoid arthritis—shaping
the immunological landscape. Nature Reviews Rheumatology, 12(1), p.63.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Minor, P.D., 2015. Live attenuated vaccines: historical successes and current
challenges. Virology, 479, pp.379-392.
Saxena, A. and Wu, D., 2016. Advances in therapeutic Fc engineering–modulation of IgG-
associated effector functions and serum half-life. Frontiers in immunology, 7, p.580.
Shih, C.M., Chang, C.L., Hsu, M.Y., Lin, J.Y., Kuan, C.M., Wang, H.K., Huang, C.T., Chung,
M.C., Huang, K.C., Hsu, C.E. and Wang, C.Y., 2015. based ELISA to rapidly detect Escherichia
coli. Talanta, 145, pp.2-5.
Solimani, F., Pollmann, R., Ishii, N., Eming, R., Hashimoto, T., Schmidt, T. and Hertl, M., 2019.
Diagnosis of anti‐laminin γ‐1 pemphigoid by immunoblot analysis. Journal of the European
Academy of Dermatology and Venereology, 33(4), pp.735-741.
Sridhar, S., Brokstad, K.A. and Cox, R.J., 2015. Influenza vaccination strategies: comparing
inactivated and live attenuated influenza vaccines. Vaccines, 3(2), pp.373-389.
Vartak, A. and Sucheck, S.J., 2016. Recent advances in subunit vaccine carriers. Vaccines, 4(2),
p.12.
Wenande, E. and Garvey, L.H., 2016. Immediate‐type hypersensitivity to polyethylene glycols: a
review. Clinical & Experimental Allergy, 46(7), pp.907-922.
challenges. Virology, 479, pp.379-392.
Saxena, A. and Wu, D., 2016. Advances in therapeutic Fc engineering–modulation of IgG-
associated effector functions and serum half-life. Frontiers in immunology, 7, p.580.
Shih, C.M., Chang, C.L., Hsu, M.Y., Lin, J.Y., Kuan, C.M., Wang, H.K., Huang, C.T., Chung,
M.C., Huang, K.C., Hsu, C.E. and Wang, C.Y., 2015. based ELISA to rapidly detect Escherichia
coli. Talanta, 145, pp.2-5.
Solimani, F., Pollmann, R., Ishii, N., Eming, R., Hashimoto, T., Schmidt, T. and Hertl, M., 2019.
Diagnosis of anti‐laminin γ‐1 pemphigoid by immunoblot analysis. Journal of the European
Academy of Dermatology and Venereology, 33(4), pp.735-741.
Sridhar, S., Brokstad, K.A. and Cox, R.J., 2015. Influenza vaccination strategies: comparing
inactivated and live attenuated influenza vaccines. Vaccines, 3(2), pp.373-389.
Vartak, A. and Sucheck, S.J., 2016. Recent advances in subunit vaccine carriers. Vaccines, 4(2),
p.12.
Wenande, E. and Garvey, L.H., 2016. Immediate‐type hypersensitivity to polyethylene glycols: a
review. Clinical & Experimental Allergy, 46(7), pp.907-922.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





