Diploma of Nursing HLTENN013: Restraints, Ethics, Dementia Care
VerifiedAdded on 2022/12/27
|11
|3913
|72
Homework Assignment
AI Summary
This document presents a completed homework assignment for the HLTENN013 unit, focusing on the implementation and monitoring of care for older persons. The assignment covers key concepts such as defining and classifying restraints, the nursing code of ethics, and assessment tools. It also explores the use of restraints in patients with dementia, including alternatives and documentation requirements. Furthermore, the assignment addresses stereotypes associated with aging, strategies to minimize stereotyping, and effective communication strategies for patients with sensory impairments. A case study involving an 82-year-old female resident with Alzheimer's disease is included, prompting students to analyze communication, social isolation, and care planning. The assignment provides detailed answers to questions related to the scenario, offering valuable insights into the practical application of nursing principles in aged care settings.
CRS170
Revision 101
July 2017
Page 1 of 11
Assessment Task Three (3): Debate Competition and Case
Based Activity
Student Version: Knowledge
Student information
Student name: Student ID:
Section A – Program/Course details
Qualification code: HLT54115 Qualification title: Diploma of Nursing
Unit code: HLTENN013 Unit title: Implement and monitor care
of the older person
Section B – Assessment task details
Assessment number: 3 Semester/Year: 2/ 2019
Due date: Duration of assessment: Make-up assessment (2 hours)
Assessment task
results:
This assessment task will be marked as:
☒ Ungraded result: Satisfactory or Not Satisfactory
☐ Other (eg points):
Section C – Instructions to students
Task instructions:
This is a make-up assessment and needs to be completed on individual basis
Students can complete this assessment at home
Students must satisfactorily answer all the questions to be deemed satisfactory in this assessment
Students may access internet or other resources to complete this assessment
Students may ask clarifying questions from the teacher.
In the event of failure of an assessment, the student’s progress will be reviewed and eligibility for a resit will be
determined by the Teacher/Program Manager as per departmental policy listed in the student handbook. Where
relevant, remediation may be offered prior to a resit. A student who successfully passes a resit shall be deemed
satisfactory
If you have documented evidence from Student Services that supports reasonable adjustment required for this
assessment, please contact the unit teacher 7 days prior to the assessment date to enable us to prepare
strategies to best assist you
Section D – Conditions for assessment
Conditions:
Student to complete and attach Assessment Submission Cover Sheet to the completed Assessment Task.
Students to complete and attach Assessment Submission Cover Sheet to the completed Assessment Task
This is in individual task
If you have any questions, please ask the teacher
You may access the internet or other resources to complete this assessment
You must meet all elements in the marking guide to be deemed satisfactory for this assessment
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 1 of 11
Assessment Task Three (3): Debate Competition and Case
Based Activity
Student Version: Knowledge
Student information
Student name: Student ID:
Section A – Program/Course details
Qualification code: HLT54115 Qualification title: Diploma of Nursing
Unit code: HLTENN013 Unit title: Implement and monitor care
of the older person
Section B – Assessment task details
Assessment number: 3 Semester/Year: 2/ 2019
Due date: Duration of assessment: Make-up assessment (2 hours)
Assessment task
results:
This assessment task will be marked as:
☒ Ungraded result: Satisfactory or Not Satisfactory
☐ Other (eg points):
Section C – Instructions to students
Task instructions:
This is a make-up assessment and needs to be completed on individual basis
Students can complete this assessment at home
Students must satisfactorily answer all the questions to be deemed satisfactory in this assessment
Students may access internet or other resources to complete this assessment
Students may ask clarifying questions from the teacher.
In the event of failure of an assessment, the student’s progress will be reviewed and eligibility for a resit will be
determined by the Teacher/Program Manager as per departmental policy listed in the student handbook. Where
relevant, remediation may be offered prior to a resit. A student who successfully passes a resit shall be deemed
satisfactory
If you have documented evidence from Student Services that supports reasonable adjustment required for this
assessment, please contact the unit teacher 7 days prior to the assessment date to enable us to prepare
strategies to best assist you
Section D – Conditions for assessment
Conditions:
Student to complete and attach Assessment Submission Cover Sheet to the completed Assessment Task.
Students to complete and attach Assessment Submission Cover Sheet to the completed Assessment Task
This is in individual task
If you have any questions, please ask the teacher
You may access the internet or other resources to complete this assessment
You must meet all elements in the marking guide to be deemed satisfactory for this assessment
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 2 of 11
Section D – Conditions for assessment
In the event of failure of an assessment, the student’s progress will be reviewed and eligibility for a resit will
be determined by the Teacher/Program Manager as per departmental policy listed in the student handbook.
Where relevant, remediation may be offered prior to a resit. A student who successfully passes a resit shall be
deemed satisfactory
Students may appeal the assessment decision according to the Holmesglen procedure
Equipment/resources students must supply: Equipment/resources to be provided by the RTO:
Textbooks, lecture notes, pen and paper Worksheet
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 2 of 11
Section D – Conditions for assessment
In the event of failure of an assessment, the student’s progress will be reviewed and eligibility for a resit will
be determined by the Teacher/Program Manager as per departmental policy listed in the student handbook.
Where relevant, remediation may be offered prior to a resit. A student who successfully passes a resit shall be
deemed satisfactory
Students may appeal the assessment decision according to the Holmesglen procedure
Equipment/resources students must supply: Equipment/resources to be provided by the RTO:
Textbooks, lecture notes, pen and paper Worksheet
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
CRS170
Revision 101
July 2017
Page 3 of 11
Section E – Marking Guide Student Answer Sheet
Assessment number: 3 Assessment title: Debate competition and case based activity
Student ID: Student name:
Unit code: HLTENN013 Unit title: Implement and monitor care of the older person
Date:
Questions: Provide your responses in the boxes below each question.
PART A:
Question 1: A) Define restraints (1 point)
B) List and define types of restraints (Physical, chemical,
psychological and environmental) (4 points)
Satisfactory response
Yes ☐ No ☐
Answer:
A) Restraints are referred as the measure that keep a person under control. In
terms of health care restraints can also be regarded as a device to regulate a
person’s movement as well as behaviour.
B) Generally, there are four types of restraints.
Physical restraints: Physical restraints are the most common type of restraints. This
type of restraint hinders the significant and normal access of the patient’s own self.
Physical restraints may include wrist restraint, waist restraint.
Chemical restraints: These are referred as the use of a drug or chemical substances in
order to prevent the patient’s movement as well as behaviour. However, the usage of
drug or chemical substance is not an accepted standard of treatment for that particular
patient’s condition.
Environmental restraints: Seclusion is the other name of environmental restraints.
Environmental restraints are one of the most important restraints among all of the
restraints. Many significant departments such as the oncology departments, psychiatry
departments have a seclusion room as a component of environmental restraint.
Psychological restraints include those therapeutic rules or theories which include the
preventing of participation of a patient in certain activities (Wilson et al., 2017).
Comment:
Question 2: When applying restraints:
A) What health assessments need to be carried out including
health maintenance?
(2 points)
B) What are the nursing code of ethics? (2 points)
C) What type of assessment tools are used? (2 points)
Satisfactory response
Yes ☐ No ☐
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 3 of 11
Section E – Marking Guide Student Answer Sheet
Assessment number: 3 Assessment title: Debate competition and case based activity
Student ID: Student name:
Unit code: HLTENN013 Unit title: Implement and monitor care of the older person
Date:
Questions: Provide your responses in the boxes below each question.
PART A:
Question 1: A) Define restraints (1 point)
B) List and define types of restraints (Physical, chemical,
psychological and environmental) (4 points)
Satisfactory response
Yes ☐ No ☐
Answer:
A) Restraints are referred as the measure that keep a person under control. In
terms of health care restraints can also be regarded as a device to regulate a
person’s movement as well as behaviour.
B) Generally, there are four types of restraints.
Physical restraints: Physical restraints are the most common type of restraints. This
type of restraint hinders the significant and normal access of the patient’s own self.
Physical restraints may include wrist restraint, waist restraint.
Chemical restraints: These are referred as the use of a drug or chemical substances in
order to prevent the patient’s movement as well as behaviour. However, the usage of
drug or chemical substance is not an accepted standard of treatment for that particular
patient’s condition.
Environmental restraints: Seclusion is the other name of environmental restraints.
Environmental restraints are one of the most important restraints among all of the
restraints. Many significant departments such as the oncology departments, psychiatry
departments have a seclusion room as a component of environmental restraint.
Psychological restraints include those therapeutic rules or theories which include the
preventing of participation of a patient in certain activities (Wilson et al., 2017).
Comment:
Question 2: When applying restraints:
A) What health assessments need to be carried out including
health maintenance?
(2 points)
B) What are the nursing code of ethics? (2 points)
C) What type of assessment tools are used? (2 points)
Satisfactory response
Yes ☐ No ☐
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CRS170
Revision 101
July 2017
Page 4 of 11
Answer:
A) Including general health maintenance the geriatric assessment can also be
carried out. This assessment is a multidimensional, hyper-variable assessment
that designed to assess an old aged person’s functionality, cognitive ability, and
physical health. This assessment is initiated when a health expert identifies a
potential problem in that particular old-aged person.
B) The nursing code of ethics are referred as the concise statement of the ethical
values, duties, responsibilities and obligations of nurses. There are five core
values in nursing code of ethics which include empathy, caring, communication
skill, professionalism and critical thinking (Epstein & Turner, 2015).
C) Many different types of health assessment tool are used. Other health
assessment tools include geriatric assessment and ACAT assessment. ACAT
assessment is basically an aged care assessment. This assessment is required
for a person who needs to be accepted for services (Govt. funded) including a
nursing home, transition care, residential aged care (Rozsa, Ford & Flicker,
2016).
Question 3: Describe the following:
A) Use of restraint and safety surrounding its use for people living
with dementia
(2 points)
B) Documentation of restraint used (1 point)
C) Alternatives to restraints (2 points)
Satisfactory response
Yes ☐ No ☐
Answer:
A) People living with dementia are at higher risk for being placed in restraints.
Instead of many limitations of restraints many nurses believe that restraints are
essential to control behavioural symptoms in the patients of dementia. In case
of patients with dementia physical and psychological restraints are commonly
used.
B) Appropriate and precise documentation of the restraint is important for accurate
and effective patient care. The documentation also provides information that
can facilitate the excellence of care. Documentation is necessary so that nurse
or healthcare experts can explain the cause of restraint to the patient and their
family members if needed.
C) There are various alternatives to restraints. The alternatives are validation
therapy, reminiscence therapy, family members or volunteers are encouraged
to visit the patient suffering from dementia at high risk times.
Comment:
Question 4: A) Define stereotype and common stereotypes associated with
ageing (3 points)
B) Impact of one’s own values and impact of stereotyping on
elderly population (2 points)
C) Recommendations on how to minimize stereotyping (2 points)
Satisfactory response
Yes ☐ No ☐
Answer:
A) Stereotype is defined popularly as a detained and fixed concept of a specific
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 4 of 11
Answer:
A) Including general health maintenance the geriatric assessment can also be
carried out. This assessment is a multidimensional, hyper-variable assessment
that designed to assess an old aged person’s functionality, cognitive ability, and
physical health. This assessment is initiated when a health expert identifies a
potential problem in that particular old-aged person.
B) The nursing code of ethics are referred as the concise statement of the ethical
values, duties, responsibilities and obligations of nurses. There are five core
values in nursing code of ethics which include empathy, caring, communication
skill, professionalism and critical thinking (Epstein & Turner, 2015).
C) Many different types of health assessment tool are used. Other health
assessment tools include geriatric assessment and ACAT assessment. ACAT
assessment is basically an aged care assessment. This assessment is required
for a person who needs to be accepted for services (Govt. funded) including a
nursing home, transition care, residential aged care (Rozsa, Ford & Flicker,
2016).
Question 3: Describe the following:
A) Use of restraint and safety surrounding its use for people living
with dementia
(2 points)
B) Documentation of restraint used (1 point)
C) Alternatives to restraints (2 points)
Satisfactory response
Yes ☐ No ☐
Answer:
A) People living with dementia are at higher risk for being placed in restraints.
Instead of many limitations of restraints many nurses believe that restraints are
essential to control behavioural symptoms in the patients of dementia. In case
of patients with dementia physical and psychological restraints are commonly
used.
B) Appropriate and precise documentation of the restraint is important for accurate
and effective patient care. The documentation also provides information that
can facilitate the excellence of care. Documentation is necessary so that nurse
or healthcare experts can explain the cause of restraint to the patient and their
family members if needed.
C) There are various alternatives to restraints. The alternatives are validation
therapy, reminiscence therapy, family members or volunteers are encouraged
to visit the patient suffering from dementia at high risk times.
Comment:
Question 4: A) Define stereotype and common stereotypes associated with
ageing (3 points)
B) Impact of one’s own values and impact of stereotyping on
elderly population (2 points)
C) Recommendations on how to minimize stereotyping (2 points)
Satisfactory response
Yes ☐ No ☐
Answer:
A) Stereotype is defined popularly as a detained and fixed concept of a specific
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 5 of 11
type of person (in this case patient) who lack the factual information.
Stereotypes of aging are actually the social constructs which are situated
historically and culturally. Stereotypes of aging are also individually interpreted.
Stereotypes of aging include ill health, depression, loneliness, dependency,
and abnormal physical and mental functioning.
B) One’s own values of play an important role in determining the stereotyping of
elderly population. One’s own value can easily prevent the negative symptoms
of stereotyping on elderly population.
C) There are various ways of minimizing stereotyping behaviours in case of
ageing. Minimization includes proper palliative care, increase in the social
interaction. Social interaction helps the old aged persons to become more
interactive which in turn reduces the stereotype behaviour in ageing related
disorders. Proper use of medication often also reduces the stereotype
behaviour. The two most commonly prescribed drugs for ageing related
diseases are cholinesterase inhibitors and memantine.
PART B:
Please read the following case scenario and answer the questions below:
Mrs Alice Wright is an eighty-two (82) years old female resident who has been living in Pines aged care facility for last
three (3) years.
Past history:
Mrs Alice Wright is very well educated and worked at ABC bank for forty-five (45) years as a financial planner. Her job
role was mostly to maintain check and balance of the company finances and provide strategic advice. Mrs Wright’s
husband passed away thirty (30) years back post AMI and heart attack. She has been very independent throughout
her life span and used to live with her only son Mark and her dog Charlie. 5 years back Mark started to observe
changes in Mrs Wright’s behaviour, when she used to become very aggressive and abusive with the family/friends.
Mark took her to a local GP and after the ACAS assessment, cognitive and neuropsychological tests she was referred
for permanent care into residential aged care facility for the diagnosis of Alzheimer’s disease. Mrs Wright felt very
isolated and depressed when she was transferred to Pines aged care facility. Her son Mark was feeling guilty of
letting her mum go into aged care. It took Mrs Wright 3 weeks to settle in the facility. She resided in a dementia
specific unit, to make sure her and others safety. Her dementia was getting worse, she had days when she would not
participate in any activity and times when she would become verbally and physically aggressive. She had aged
related hearing loss and her non-compliance with hearing aid was making the situation more challenging. She was
transferred to hospital twice for physical aggression towards staff and other residents and was diagnosed with UTI
and BPSD (Behavioural and psychological symptoms of dementia).
Medical diagnosis:
Dermatitis (Specifically on B/L arms) for 1 year
Age related hearing loss for 2 years
IHD and angina 10-year back
AF 10 years’ back
Re-current chest infections (3 episodes in last 4 months)
Alzheimer’s disease with BPSD (Diagnosed 5 years back)
Osteoarthritis in B/L knees for 20 years
Re-current UTIs (12 years) on SPC
Hypothyroidism (45 years)
Renal failure post renal cell carcinoma (10 years back)
Current medications:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 5 of 11
type of person (in this case patient) who lack the factual information.
Stereotypes of aging are actually the social constructs which are situated
historically and culturally. Stereotypes of aging are also individually interpreted.
Stereotypes of aging include ill health, depression, loneliness, dependency,
and abnormal physical and mental functioning.
B) One’s own values of play an important role in determining the stereotyping of
elderly population. One’s own value can easily prevent the negative symptoms
of stereotyping on elderly population.
C) There are various ways of minimizing stereotyping behaviours in case of
ageing. Minimization includes proper palliative care, increase in the social
interaction. Social interaction helps the old aged persons to become more
interactive which in turn reduces the stereotype behaviour in ageing related
disorders. Proper use of medication often also reduces the stereotype
behaviour. The two most commonly prescribed drugs for ageing related
diseases are cholinesterase inhibitors and memantine.
PART B:
Please read the following case scenario and answer the questions below:
Mrs Alice Wright is an eighty-two (82) years old female resident who has been living in Pines aged care facility for last
three (3) years.
Past history:
Mrs Alice Wright is very well educated and worked at ABC bank for forty-five (45) years as a financial planner. Her job
role was mostly to maintain check and balance of the company finances and provide strategic advice. Mrs Wright’s
husband passed away thirty (30) years back post AMI and heart attack. She has been very independent throughout
her life span and used to live with her only son Mark and her dog Charlie. 5 years back Mark started to observe
changes in Mrs Wright’s behaviour, when she used to become very aggressive and abusive with the family/friends.
Mark took her to a local GP and after the ACAS assessment, cognitive and neuropsychological tests she was referred
for permanent care into residential aged care facility for the diagnosis of Alzheimer’s disease. Mrs Wright felt very
isolated and depressed when she was transferred to Pines aged care facility. Her son Mark was feeling guilty of
letting her mum go into aged care. It took Mrs Wright 3 weeks to settle in the facility. She resided in a dementia
specific unit, to make sure her and others safety. Her dementia was getting worse, she had days when she would not
participate in any activity and times when she would become verbally and physically aggressive. She had aged
related hearing loss and her non-compliance with hearing aid was making the situation more challenging. She was
transferred to hospital twice for physical aggression towards staff and other residents and was diagnosed with UTI
and BPSD (Behavioural and psychological symptoms of dementia).
Medical diagnosis:
Dermatitis (Specifically on B/L arms) for 1 year
Age related hearing loss for 2 years
IHD and angina 10-year back
AF 10 years’ back
Re-current chest infections (3 episodes in last 4 months)
Alzheimer’s disease with BPSD (Diagnosed 5 years back)
Osteoarthritis in B/L knees for 20 years
Re-current UTIs (12 years) on SPC
Hypothyroidism (45 years)
Renal failure post renal cell carcinoma (10 years back)
Current medications:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
CRS170
Revision 101
July 2017
Page 6 of 11
Sorbolene lotion daily PRN
Waxol for ear wax removal every 6 months
GTN 25mg patch daily
PRN Ventolin nebs
PRN N/S nebs
Oxazepam 7.5 mg BD
Memantine 10 mg daily
Panadol 1g BD
Ural sachet once daily
Levo-thyroxine 2 tabs before breakfast
Complex care needs: SPC (suprapubic catheter), Pacemaker, PRN supplementary oxygen 2L and BPSD
Current situation: You are an enrolled nurse working on a morning shift. At around 08:00 hrs you started your
medication round when you pass by Mrs Wright’s room and find her distressed and crying sitting in the corner of her
bathroom. On attending her, she started yelling and throwing towels and soap. You decided to maintain a distance
and gave her sometime to settle, making sure to monitor her from the distance even. You saw that she removed her
SPC, clothes and hearing aids in the room. Her room looked cluttered and all her personal belongings were on the
floor. You saw her incontinent of urine and faeces. You informed your registered nurse on shift and certainly wanted
to help her in the best possible way.
Questions to be answered by student Satisfactory
response
Yes No
Question 1. Communication with people with sensory impairment (Mrs Alice Wright’s case
scenario).
☐ ☐
Answer: To communicate with people with sensory impairment a registered nurse should
always turn his/her face towards the patient so that the patient can see the lip movement of
the nurse clearly. Nurses have to speak clearly and slightly slower with patients (In this case
Mrs. Alice Wright) in order to communicate.
Comment:
Question 2. Dealing with social isolation and social inclusion ☐ ☐
Answer: Considering the fact that Mrs. Alice Wright is suffering from dementia and
Alzheimer’s disease social isolation is one of the common symptoms. In order to treat social
isolation properly social inclusion of that particular patient is highly recommended. In case of
social inclusion all the individuals in a group feel significantly important and included within
the society (Holwerda et al., 2014).
Comment:
Question 3. Identifying and responding to challenging behaviours exhibited by Mrs Alice
Wright. ☐ ☐
Answer:
The challenging behaviours exhibited by Mrs. Alice Wright are verbal and physical
aggression. In order to control this type of behaviour healthcare experts need to be
compassionate about the condition of the patient. Healthcare experts should listen to Mrs.
Alice Wright very carefully and note down the triggers this type of aggressive behaviour.
Mrs. Alice Wright is also suffering from auditory (sensory) impairment and she does not
want to use hearing-aid. To improve this sensory impairment healthcare experts should tell
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 6 of 11
Sorbolene lotion daily PRN
Waxol for ear wax removal every 6 months
GTN 25mg patch daily
PRN Ventolin nebs
PRN N/S nebs
Oxazepam 7.5 mg BD
Memantine 10 mg daily
Panadol 1g BD
Ural sachet once daily
Levo-thyroxine 2 tabs before breakfast
Complex care needs: SPC (suprapubic catheter), Pacemaker, PRN supplementary oxygen 2L and BPSD
Current situation: You are an enrolled nurse working on a morning shift. At around 08:00 hrs you started your
medication round when you pass by Mrs Wright’s room and find her distressed and crying sitting in the corner of her
bathroom. On attending her, she started yelling and throwing towels and soap. You decided to maintain a distance
and gave her sometime to settle, making sure to monitor her from the distance even. You saw that she removed her
SPC, clothes and hearing aids in the room. Her room looked cluttered and all her personal belongings were on the
floor. You saw her incontinent of urine and faeces. You informed your registered nurse on shift and certainly wanted
to help her in the best possible way.
Questions to be answered by student Satisfactory
response
Yes No
Question 1. Communication with people with sensory impairment (Mrs Alice Wright’s case
scenario).
☐ ☐
Answer: To communicate with people with sensory impairment a registered nurse should
always turn his/her face towards the patient so that the patient can see the lip movement of
the nurse clearly. Nurses have to speak clearly and slightly slower with patients (In this case
Mrs. Alice Wright) in order to communicate.
Comment:
Question 2. Dealing with social isolation and social inclusion ☐ ☐
Answer: Considering the fact that Mrs. Alice Wright is suffering from dementia and
Alzheimer’s disease social isolation is one of the common symptoms. In order to treat social
isolation properly social inclusion of that particular patient is highly recommended. In case of
social inclusion all the individuals in a group feel significantly important and included within
the society (Holwerda et al., 2014).
Comment:
Question 3. Identifying and responding to challenging behaviours exhibited by Mrs Alice
Wright. ☐ ☐
Answer:
The challenging behaviours exhibited by Mrs. Alice Wright are verbal and physical
aggression. In order to control this type of behaviour healthcare experts need to be
compassionate about the condition of the patient. Healthcare experts should listen to Mrs.
Alice Wright very carefully and note down the triggers this type of aggressive behaviour.
Mrs. Alice Wright is also suffering from auditory (sensory) impairment and she does not
want to use hearing-aid. To improve this sensory impairment healthcare experts should tell
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CRS170
Revision 101
July 2017
Page 7 of 11
her about the importance of hearing-aid in order to improve the auditory impairment.
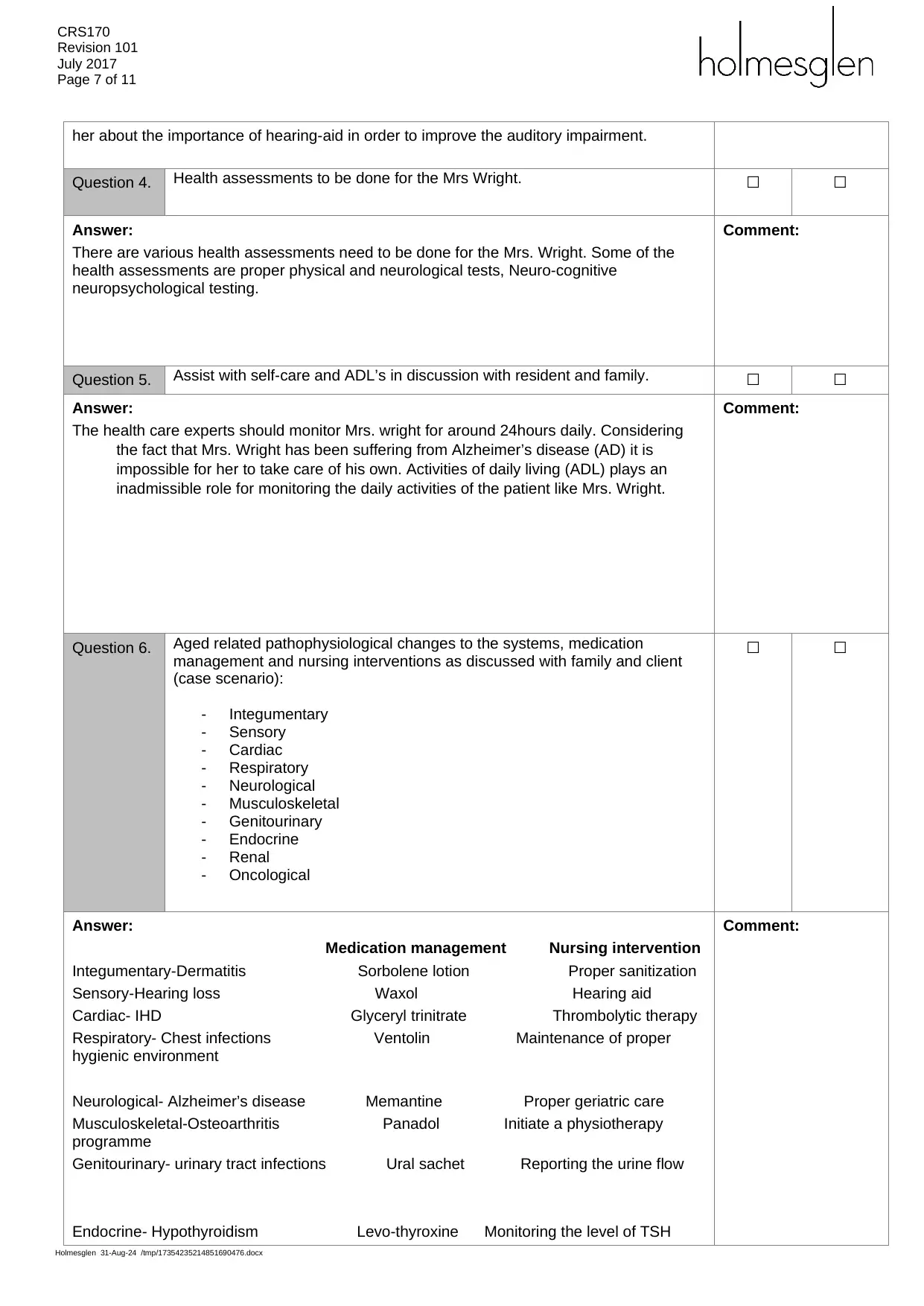
Question 4. Health assessments to be done for the Mrs Wright. ☐ ☐
Answer:
There are various health assessments need to be done for the Mrs. Wright. Some of the
health assessments are proper physical and neurological tests, Neuro-cognitive
neuropsychological testing.
Comment:
Question 5. Assist with self-care and ADL’s in discussion with resident and family. ☐ ☐
Answer:
The health care experts should monitor Mrs. wright for around 24hours daily. Considering
the fact that Mrs. Wright has been suffering from Alzheimer’s disease (AD) it is
impossible for her to take care of his own. Activities of daily living (ADL) plays an
inadmissible role for monitoring the daily activities of the patient like Mrs. Wright.
Comment:
Question 6. Aged related pathophysiological changes to the systems, medication
management and nursing interventions as discussed with family and client
(case scenario):
- Integumentary
- Sensory
- Cardiac
- Respiratory
- Neurological
- Musculoskeletal
- Genitourinary
- Endocrine
- Renal
- Oncological
☐ ☐
Answer:
Medication management Nursing intervention
Integumentary-Dermatitis Sorbolene lotion Proper sanitization
Sensory-Hearing loss Waxol Hearing aid
Cardiac- IHD Glyceryl trinitrate Thrombolytic therapy
Respiratory- Chest infections Ventolin Maintenance of proper
hygienic environment
Neurological- Alzheimer’s disease Memantine Proper geriatric care
Musculoskeletal-Osteoarthritis Panadol Initiate a physiotherapy
programme
Genitourinary- urinary tract infections Ural sachet Reporting the urine flow
Endocrine- Hypothyroidism Levo-thyroxine Monitoring the level of TSH
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 7 of 11
her about the importance of hearing-aid in order to improve the auditory impairment.
Question 4. Health assessments to be done for the Mrs Wright. ☐ ☐
Answer:
There are various health assessments need to be done for the Mrs. Wright. Some of the
health assessments are proper physical and neurological tests, Neuro-cognitive
neuropsychological testing.
Comment:
Question 5. Assist with self-care and ADL’s in discussion with resident and family. ☐ ☐
Answer:
The health care experts should monitor Mrs. wright for around 24hours daily. Considering
the fact that Mrs. Wright has been suffering from Alzheimer’s disease (AD) it is
impossible for her to take care of his own. Activities of daily living (ADL) plays an
inadmissible role for monitoring the daily activities of the patient like Mrs. Wright.
Comment:
Question 6. Aged related pathophysiological changes to the systems, medication
management and nursing interventions as discussed with family and client
(case scenario):
- Integumentary
- Sensory
- Cardiac
- Respiratory
- Neurological
- Musculoskeletal
- Genitourinary
- Endocrine
- Renal
- Oncological
☐ ☐
Answer:
Medication management Nursing intervention
Integumentary-Dermatitis Sorbolene lotion Proper sanitization
Sensory-Hearing loss Waxol Hearing aid
Cardiac- IHD Glyceryl trinitrate Thrombolytic therapy
Respiratory- Chest infections Ventolin Maintenance of proper
hygienic environment
Neurological- Alzheimer’s disease Memantine Proper geriatric care
Musculoskeletal-Osteoarthritis Panadol Initiate a physiotherapy
programme
Genitourinary- urinary tract infections Ural sachet Reporting the urine flow
Endocrine- Hypothyroidism Levo-thyroxine Monitoring the level of TSH
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 8 of 11
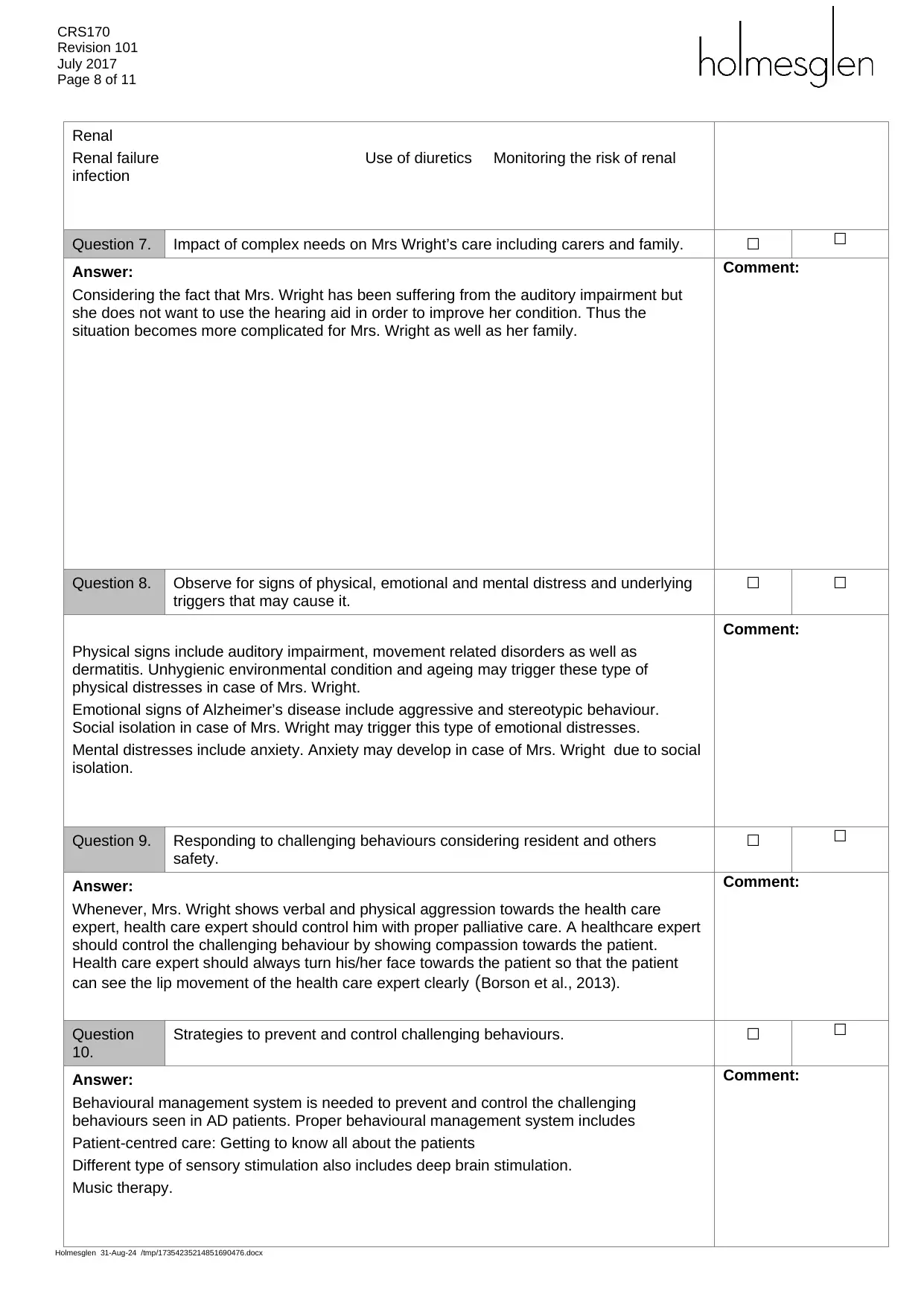
Renal
Renal failure Use of diuretics Monitoring the risk of renal
infection
Question 7. Impact of complex needs on Mrs Wright’s care including carers and family. ☐ ☐
Answer:
Considering the fact that Mrs. Wright has been suffering from the auditory impairment but
she does not want to use the hearing aid in order to improve her condition. Thus the
situation becomes more complicated for Mrs. Wright as well as her family.
Comment:
Question 8. Observe for signs of physical, emotional and mental distress and underlying
triggers that may cause it.
☐ ☐
Physical signs include auditory impairment, movement related disorders as well as
dermatitis. Unhygienic environmental condition and ageing may trigger these type of
physical distresses in case of Mrs. Wright.
Emotional signs of Alzheimer’s disease include aggressive and stereotypic behaviour.
Social isolation in case of Mrs. Wright may trigger this type of emotional distresses.
Mental distresses include anxiety. Anxiety may develop in case of Mrs. Wright due to social
isolation.
Comment:
Question 9. Responding to challenging behaviours considering resident and others
safety.
☐ ☐
Answer:
Whenever, Mrs. Wright shows verbal and physical aggression towards the health care
expert, health care expert should control him with proper palliative care. A healthcare expert
should control the challenging behaviour by showing compassion towards the patient.
Health care expert should always turn his/her face towards the patient so that the patient
can see the lip movement of the health care expert clearly (Borson et al., 2013).
Comment:
Question
10.
Strategies to prevent and control challenging behaviours. ☐ ☐
Answer:
Behavioural management system is needed to prevent and control the challenging
behaviours seen in AD patients. Proper behavioural management system includes
Patient-centred care: Getting to know all about the patients
Different type of sensory stimulation also includes deep brain stimulation.
Music therapy.
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 8 of 11
Renal
Renal failure Use of diuretics Monitoring the risk of renal
infection
Question 7. Impact of complex needs on Mrs Wright’s care including carers and family. ☐ ☐
Answer:
Considering the fact that Mrs. Wright has been suffering from the auditory impairment but
she does not want to use the hearing aid in order to improve her condition. Thus the
situation becomes more complicated for Mrs. Wright as well as her family.
Comment:
Question 8. Observe for signs of physical, emotional and mental distress and underlying
triggers that may cause it.
☐ ☐
Physical signs include auditory impairment, movement related disorders as well as
dermatitis. Unhygienic environmental condition and ageing may trigger these type of
physical distresses in case of Mrs. Wright.
Emotional signs of Alzheimer’s disease include aggressive and stereotypic behaviour.
Social isolation in case of Mrs. Wright may trigger this type of emotional distresses.
Mental distresses include anxiety. Anxiety may develop in case of Mrs. Wright due to social
isolation.
Comment:
Question 9. Responding to challenging behaviours considering resident and others
safety.
☐ ☐
Answer:
Whenever, Mrs. Wright shows verbal and physical aggression towards the health care
expert, health care expert should control him with proper palliative care. A healthcare expert
should control the challenging behaviour by showing compassion towards the patient.
Health care expert should always turn his/her face towards the patient so that the patient
can see the lip movement of the health care expert clearly (Borson et al., 2013).
Comment:
Question
10.
Strategies to prevent and control challenging behaviours. ☐ ☐
Answer:
Behavioural management system is needed to prevent and control the challenging
behaviours seen in AD patients. Proper behavioural management system includes
Patient-centred care: Getting to know all about the patients
Different type of sensory stimulation also includes deep brain stimulation.
Music therapy.
Comment:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
CRS170
Revision 101
July 2017
Page 9 of 11
Question
11.
Nursing intervention for Alice that are applicable to a nursing care plan for
Alice.
☐ ☐
Answer:
Alice is suffering from Alzheimer’s disease (AD) and proper nursing care plan for Alice is
immediately needed.
Nurses have to assess patient’s ability for proper thought processing every shift. Nurses
have to observe patient for cognitive calibration, memory changes, variation in neuro-
cognitive patterns.
Nurses also have to assess level of confusion and disorientation of the AD affected patient.
For a proper nursing care plan nurses also have to establish an operative communication
system with the patient and his family. This communication system helps the patient’s family
to adjust to the patient’s altered cognitive abilities. Proper emotional support is another vital
nursing care plan for AD affected patient (Wilson et al., 2017).
Comment:
Question
12.
Theory of ageing that best suits Mrs Wright. ☐ ☐
Answer:
Theory of ageing that best suits Mrs Wright is the programmes theory of ageing. The
programmed theory of ageing includes three components. Three components consist of
programmed Longevity, endocrine theory and immunological theory.
The programmed longevity which considers ageing as a result of a sequential up regulation
and down regulation of certain genes.
In endocrine theory biological clocks act through the secretion of hormones to control the
speed of ageing. Melatonin secreted from the pineal gland plays an inadmissible role in the
development of ageing. Supra-chiasmatic-hypothalamo pathway also acts as a key player in
ageing development.
Immunological theory concludes that the immune system is automated to decay over time.
This causes an increase in the vulnerability to infectious disease and thus causes ageing
leading to death (Steptoe, Deaton & Stone 2015)
Comment:
Section F – Feedback to Student
Has the student successfully completed this assessment task? Yes No
☐ ☐
Additional Assessor comments (as appropriate):
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 9 of 11
Question
11.
Nursing intervention for Alice that are applicable to a nursing care plan for
Alice.
☐ ☐
Answer:
Alice is suffering from Alzheimer’s disease (AD) and proper nursing care plan for Alice is
immediately needed.
Nurses have to assess patient’s ability for proper thought processing every shift. Nurses
have to observe patient for cognitive calibration, memory changes, variation in neuro-
cognitive patterns.
Nurses also have to assess level of confusion and disorientation of the AD affected patient.
For a proper nursing care plan nurses also have to establish an operative communication
system with the patient and his family. This communication system helps the patient’s family
to adjust to the patient’s altered cognitive abilities. Proper emotional support is another vital
nursing care plan for AD affected patient (Wilson et al., 2017).
Comment:
Question
12.
Theory of ageing that best suits Mrs Wright. ☐ ☐
Answer:
Theory of ageing that best suits Mrs Wright is the programmes theory of ageing. The
programmed theory of ageing includes three components. Three components consist of
programmed Longevity, endocrine theory and immunological theory.
The programmed longevity which considers ageing as a result of a sequential up regulation
and down regulation of certain genes.
In endocrine theory biological clocks act through the secretion of hormones to control the
speed of ageing. Melatonin secreted from the pineal gland plays an inadmissible role in the
development of ageing. Supra-chiasmatic-hypothalamo pathway also acts as a key player in
ageing development.
Immunological theory concludes that the immune system is automated to decay over time.
This causes an increase in the vulnerability to infectious disease and thus causes ageing
leading to death (Steptoe, Deaton & Stone 2015)
Comment:
Section F – Feedback to Student
Has the student successfully completed this assessment task? Yes No
☐ ☐
Additional Assessor comments (as appropriate):
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CRS170
Revision 101
July 2017
Page 10 of 11
Resubmission allowed: Yes ☐ No ☐ Resubmission due date:
Assessor name: Kiran Kiran
Assessor signature:
Date:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 10 of 11
Resubmission allowed: Yes ☐ No ☐ Resubmission due date:
Assessor name: Kiran Kiran
Assessor signature:
Date:
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CRS170
Revision 101
July 2017
Page 11 of 11
REFERENCES
Borson, S., Frank, L., Bayley, P. J., Boustani, M., Dean, M., Lin, P. J., .. & Stefanacci, R. G.
(2013). Improving dementia care: the role of screening and detection of cognitive
impairment. Alzheimer's & Dementia, 9(2), 151-159.
Epstein, B., & Turner, M. (2015). The nursing code of ethics: Its value, its history. OJIN: The
Online Journal of Issues in Nursing, 20(2), 1-10.
Holwerda, T. J., Deeg, D. J., Beekman, A. T., van Tilburg, T. G., Stek, M. L., Jonker, C., &
Schoevers, R. A. (2014). Feelings of loneliness, but not social isolation, predict dementia
onset: results from the Amsterdam Study of the Elderly (AMSTEL). J Neurol Neurosurg
Psychiatry, 85(2), 135-142.
Perales, J., Cosco, T. D., Stephan, B. C., Haro, J. M., & Brayne, C. (2013). Health-related quality-
of-life instruments for Alzheimer's disease and mixed dementia. International
Psychogeriatrics, 25(5), 691-706.
Rozsa, M., Ford, A., & Flicker, L. (2016). Assessing people with dementia: the role of the aged
care assessment team and memory clinics. Internal medicine journal, 46(9), 1081-1088.
Steptoe, A., Deaton, A., & Stone, A. A. (2015). Subjective wellbeing, health, and ageing. The
Lancet, 385(9968), 640-648.
Wilson, C., Rouse, L., Rae, S., & Kar Ray, M. (2017). Is restraint a ‘necessary evil’in mental health
care? Mental health inpatients’ and staff members’ experience of physical
restraint. International journal of mental health nursing, 26(5), 500-512.
Yaffe, K., Yaffe, K., Aisen, P., Albert, M., & Anstey, K. (2014). Dementia (including Alzheimer’s
disease) can be prevented: statement supported by international experts. Journal of
Alzheimer’s disease, 38, 699-703.
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
Revision 101
July 2017
Page 11 of 11
REFERENCES
Borson, S., Frank, L., Bayley, P. J., Boustani, M., Dean, M., Lin, P. J., .. & Stefanacci, R. G.
(2013). Improving dementia care: the role of screening and detection of cognitive
impairment. Alzheimer's & Dementia, 9(2), 151-159.
Epstein, B., & Turner, M. (2015). The nursing code of ethics: Its value, its history. OJIN: The
Online Journal of Issues in Nursing, 20(2), 1-10.
Holwerda, T. J., Deeg, D. J., Beekman, A. T., van Tilburg, T. G., Stek, M. L., Jonker, C., &
Schoevers, R. A. (2014). Feelings of loneliness, but not social isolation, predict dementia
onset: results from the Amsterdam Study of the Elderly (AMSTEL). J Neurol Neurosurg
Psychiatry, 85(2), 135-142.
Perales, J., Cosco, T. D., Stephan, B. C., Haro, J. M., & Brayne, C. (2013). Health-related quality-
of-life instruments for Alzheimer's disease and mixed dementia. International
Psychogeriatrics, 25(5), 691-706.
Rozsa, M., Ford, A., & Flicker, L. (2016). Assessing people with dementia: the role of the aged
care assessment team and memory clinics. Internal medicine journal, 46(9), 1081-1088.
Steptoe, A., Deaton, A., & Stone, A. A. (2015). Subjective wellbeing, health, and ageing. The
Lancet, 385(9968), 640-648.
Wilson, C., Rouse, L., Rae, S., & Kar Ray, M. (2017). Is restraint a ‘necessary evil’in mental health
care? Mental health inpatients’ and staff members’ experience of physical
restraint. International journal of mental health nursing, 26(5), 500-512.
Yaffe, K., Yaffe, K., Aisen, P., Albert, M., & Anstey, K. (2014). Dementia (including Alzheimer’s
disease) can be prevented: statement supported by international experts. Journal of
Alzheimer’s disease, 38, 699-703.
Holmesglen 31-Aug-24 /tmp/17354235214851690476.docx
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





