Implementing Effective Vaccination Mandates: Best Practices
VerifiedAdded on 2022/09/14
|4
|3814
|11
Report
AI Summary
This report examines the effectiveness and ethical considerations surrounding mandatory vaccination policies. It discusses the rise in measles cases globally and explores how governments are considering compulsory immunizations. The report analyses various approaches to vaccination mandates, including exemptions and penalties, and their impact on vaccination rates. It highlights that while mandates can improve vaccination rates, rigid, punitive policies may not be as effective as more flexible ones. The report emphasizes the importance of addressing the underlying reasons for low vaccination rates, such as poverty, social exclusion, and access difficulties, before implementing mandates. It also outlines five key steps for governments to take when considering mandates, including using multiple interventions, ensuring easy access to vaccines, and avoiding the entrenchment of inequity or fueling of anti-vaccine activism. The report suggests that allowing non-medical exemptions but making them hard to obtain might be the most effective approach, as removing choice entirely could induce parents to seek loopholes and fuel negative attitudes towards vaccination.
PUBLIC HEALTH Citizen science
is helping to map snakebite
risk p.478
ENVIRONMENT A call to safeguard
biodiversity in regions of
armed conflict p.478
POLITICS How Hindu
nationalists have co-opted
the trappings of science p.476
BIAS Why do racial
stereotypes persist
in sport? p.474
Thousands of people worldwide have
been affected by recent measles
outbreaks, even though there is a
safe and effective vaccine.
In the first four months of this year, the
World Health Organization (WHO) reported
about 226,000 measles cases — almost three
times the count recorded in the same period
last year (see go.nature.com/2jkq8d3).
Already, the number of cases in the United
States this year has exceeded the reported
tally in any year since the country halted
sustained transmission of the disease in
2000. Similarly, in Europe, the 2018 figures
were the highest this decade (see ‘Measles
on the rise’).
Partly in response to these outbreaks,
some governments are now considering
making vaccination for measles and other
diseases a legal requirement1. The state of
New York signed legislation to that effect
last month.
Such mandates, which began with small-
pox vaccination in nineteenth-century
Europe, are in place for numerous vaccines
in various countries. And several studies
show that requiring vaccination can
Mandate vaccination with c
Governments that are considering compulsory immunizations must avoid stoking
anti-vaccine sentiment, argue Saad B. Omer, Cornelia Betsch and Julie Lea
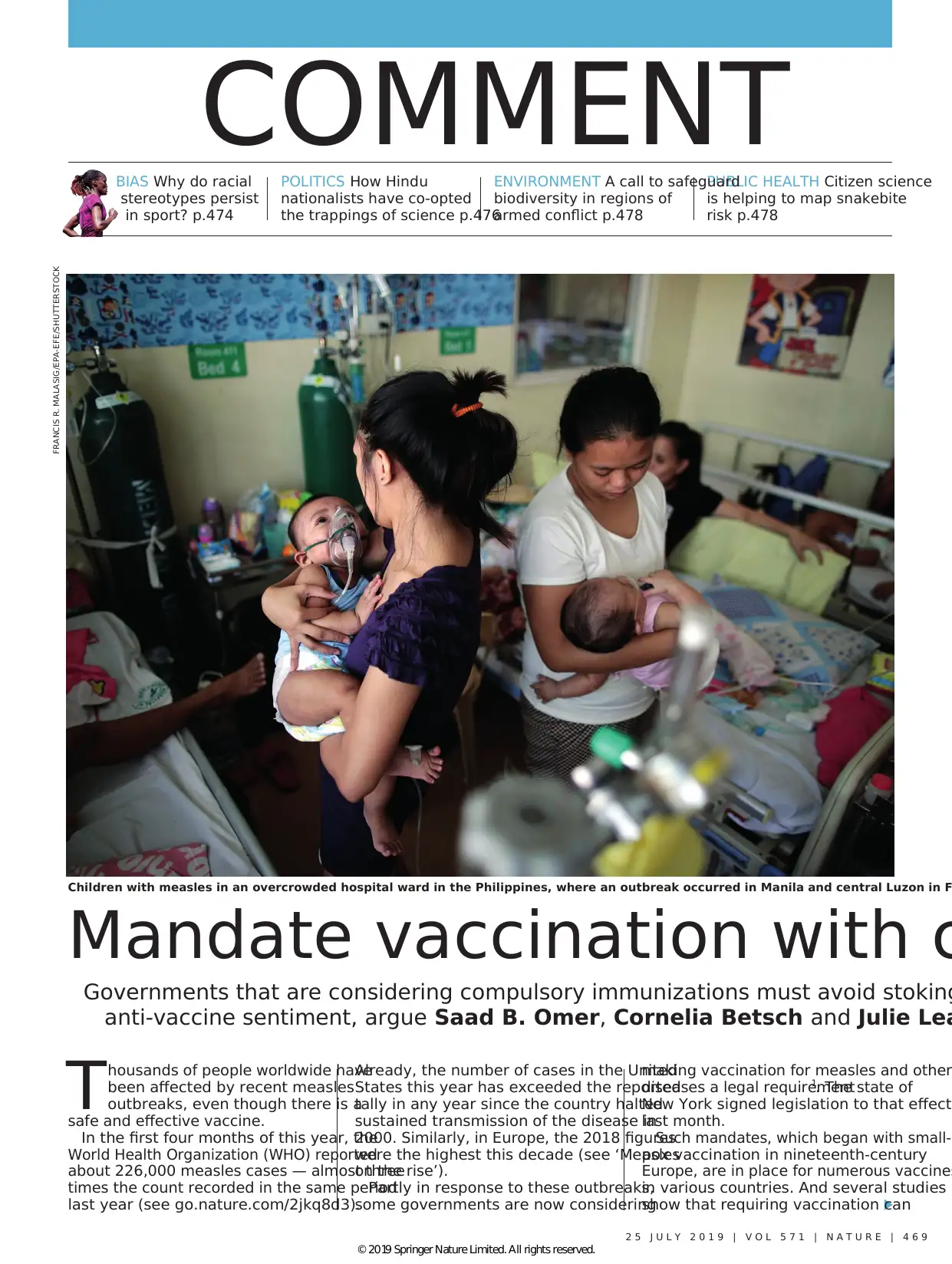
Children with measles in an overcrowded hospital ward in the Philippines, where an outbreak occurred in Manila and central Luzon in F
FRANCIS R. MALASIG/EPA-EFE/SHUTTERSTOCK
2 5 J U L Y 2 0 1 9 | V O L 5 7 1 | N A T U R E | 4 6 9
COMMENT
© 2019 Springer Nature Limited. All rights reserved.
is helping to map snakebite
risk p.478
ENVIRONMENT A call to safeguard
biodiversity in regions of
armed conflict p.478
POLITICS How Hindu
nationalists have co-opted
the trappings of science p.476
BIAS Why do racial
stereotypes persist
in sport? p.474
Thousands of people worldwide have
been affected by recent measles
outbreaks, even though there is a
safe and effective vaccine.
In the first four months of this year, the
World Health Organization (WHO) reported
about 226,000 measles cases — almost three
times the count recorded in the same period
last year (see go.nature.com/2jkq8d3).
Already, the number of cases in the United
States this year has exceeded the reported
tally in any year since the country halted
sustained transmission of the disease in
2000. Similarly, in Europe, the 2018 figures
were the highest this decade (see ‘Measles
on the rise’).
Partly in response to these outbreaks,
some governments are now considering
making vaccination for measles and other
diseases a legal requirement1. The state of
New York signed legislation to that effect
last month.
Such mandates, which began with small-
pox vaccination in nineteenth-century
Europe, are in place for numerous vaccines
in various countries. And several studies
show that requiring vaccination can
Mandate vaccination with c
Governments that are considering compulsory immunizations must avoid stoking
anti-vaccine sentiment, argue Saad B. Omer, Cornelia Betsch and Julie Lea
Children with measles in an overcrowded hospital ward in the Philippines, where an outbreak occurred in Manila and central Luzon in F
FRANCIS R. MALASIG/EPA-EFE/SHUTTERSTOCK
2 5 J U L Y 2 0 1 9 | V O L 5 7 1 | N A T U R E | 4 6 9
COMMENT
© 2019 Springer Nature Limited. All rights reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
improve rates in high-income countries
(see, for example, ref. 2), although there
is limited evidence of the impact of such
requirements in low- or middle-income
nations.
However, mandatory vaccination can
worsen inequities in access to resources,
because penalties for not complying can
disproportionately affect disadvantaged
groups. What’s more, the evidence suggests
that there is no simple linear relationship
between the forcefulness of a policy and its
impact on the rate of vaccination.
It is crucial that policies don’t inadvert-
ently entrench inequity or fuel anti-vaccine
activism. As specialists in vaccination
policy and programmes, we lay out here
what’s known, to help governments con-
sider whether a mandate is the right fit for
their situation. We also discuss what other
changes should be made before introduc-
ing requirements (see ‘Best practice’). And
we distil how mandates should be designed
to ensure effectiveness.
WHICH MANDATES WORK?
There has long been substantial variability
in how governments and jurisdictions
mandate vaccination — specifically, in
what is actually required of people; the
penalties imposed if requirements are not
met; and the age groups and populations
that are covered.
In the United States, for instance, proof
of immunization or exemption documen-
tation is required before children can go to
school. All 50 states and Washington DC
allow exemptions for medical reasons, and
45 states allow philosophical or religious
exemptions. In Australia, certain vaccines
are a requirement for entry into preschool
or childcare in some states, but not in
others. In Uganda, parents who fail to vac-
cinate their children can be jailed for six
months.
Studies conducted largely in the United
States and Europe suggest that making vac-
cination a requirement for enrolment in
childcare and school can help to increase
rates (see, for example, ref. 2). For instance,
a review of studies conducted mostly in the
United States found that the need to pro-
vide documentation to access childcare or to
attend school and college is associated with
a median improvement of 18 percentage
points in the rate of vaccination for diseases
such as measles, hepatitis B and whooping
cough (see go.nature.com/3tzrujo).
When it comes to obtaining an exemption,
having complex administrative procedures
in place (such as those involving counsel-
ling with a physician) reduces the number of
parents who refuse to have their children vac-
cinated. It also lowers the number of people
who are affected by vaccine-preventable
diseases2
. In a 2012 study, non-medical
exemption rates were more than twice as
high in US states that had relatively easy
exemption procedures, compared with states
that had more complex ones3.
Given such evidence, governments have
sometimes removed non-medical exemp-
tions altogether. In the past four years, the
states of Maine,
New York and Cali-
fornia joined West
Virginia and Mis-
sissippi in eliminat-
ing non-medical
exemptions for all
or some vaccines.
And in response
to a media and
public campaign,
Australia implemented legislation in 2016
that prevents parents from obtaining
non-medical exemptions.
Increases in vaccination rates have been
associated with financial penalties. These
take the form of either the withdrawal of
family assistance payments (currently as
much as Aus$26,000 (US$18,200) a year
in Australia, by our calculations) or fines
for parents who refuse to vaccinate their
children. In a study evaluating mandatory
vaccination in Europe, measles vaccine
coverage was 0.8% higher and whooping-
cough vaccine coverage was 1.1% higher
for every €500 (US$560) increase in the
penalty4.
Vaccination requirements (tied to school
and childcare access, or to monetary pen-
alties) fare well in comparisons with other
large-scale interventions, such as vaccina-
tion drives at schools, or communication
campaigns involving pamphlets, billboards,
television advertisements and so on. A 2017
review of interventions to increase vaccina-
tion found that in high-income countries,
requirements to vaccinate are more likely to
affect rates than are attempts to change ho
people think and feel about vaccination5.
EXEMPTIONS AND PENALTIES
So, in many cases, requirements to vaccina
do seem to improve vaccination rates. But
do rigid, punitive policies work better than
flexible ones? In our view, not necessarily.
In fact, the limited data that are available
suggest that a middle-of-the-road approach
might be more effective. These data come
mainly from California, Washington state
(which eliminated personal-belief exemp-
tions to measles, mumps and rubella (MMR)
vaccination this year) and Australia.
In 2015, California became the third US
state to eliminate all non-medical exemp-
tions, and the first state to do so in more
than three decades. This change in the law
was preceded by a 2014 administrative
initiative to reduce the misuse of a school
admission process involving ‘conditional
entrants’ — children who have started the
required vaccination schedule but haven’t
completed it6
. (Since 1979, children in Cal-
ifornia have been allowed to attend school
as conditional entrants — but before 2014,
only some schools followed up with par-
ents, and some children were never fully
vaccinated6.)
The proportion of children of kinder-
garten age who are not up to date on their
vaccinations has decreased in California,
from 9.8% in 2013 to 4.9% in 2017 (ref. 7).
However, this change seems to be mainly
associated with the administrative crack-
down on conditional entrants. Following
the elimination of non-medical exemp-
tions, many parents with strong objections
to vaccination simply acquired medical
exemptions instead, educated their chil-
dren at home, enrolled them in independ-
ent study programmes that do not require
classroom-based instruction, or found
other loopholes6.
In Australia, following policy changes in
1999, parents had to get their child vacci-
nated to get assistance payments. And they
could obtain non-medical exemptions only
after they had discussed the issue with a
health-care provider. According to surveys,
these policies helped to improve vaccina-
tion coverage from an estimated 80% to
more than 90% in three years8.
Then, in 2016, Australia implemented
a ‘No Jab No Pay’ policy, which removed
non-medical exemptions and applied the
“There is no
simple linear
relationship
between the
forcefulness
of a policy
and its impact
on the rate of
vaccination.”
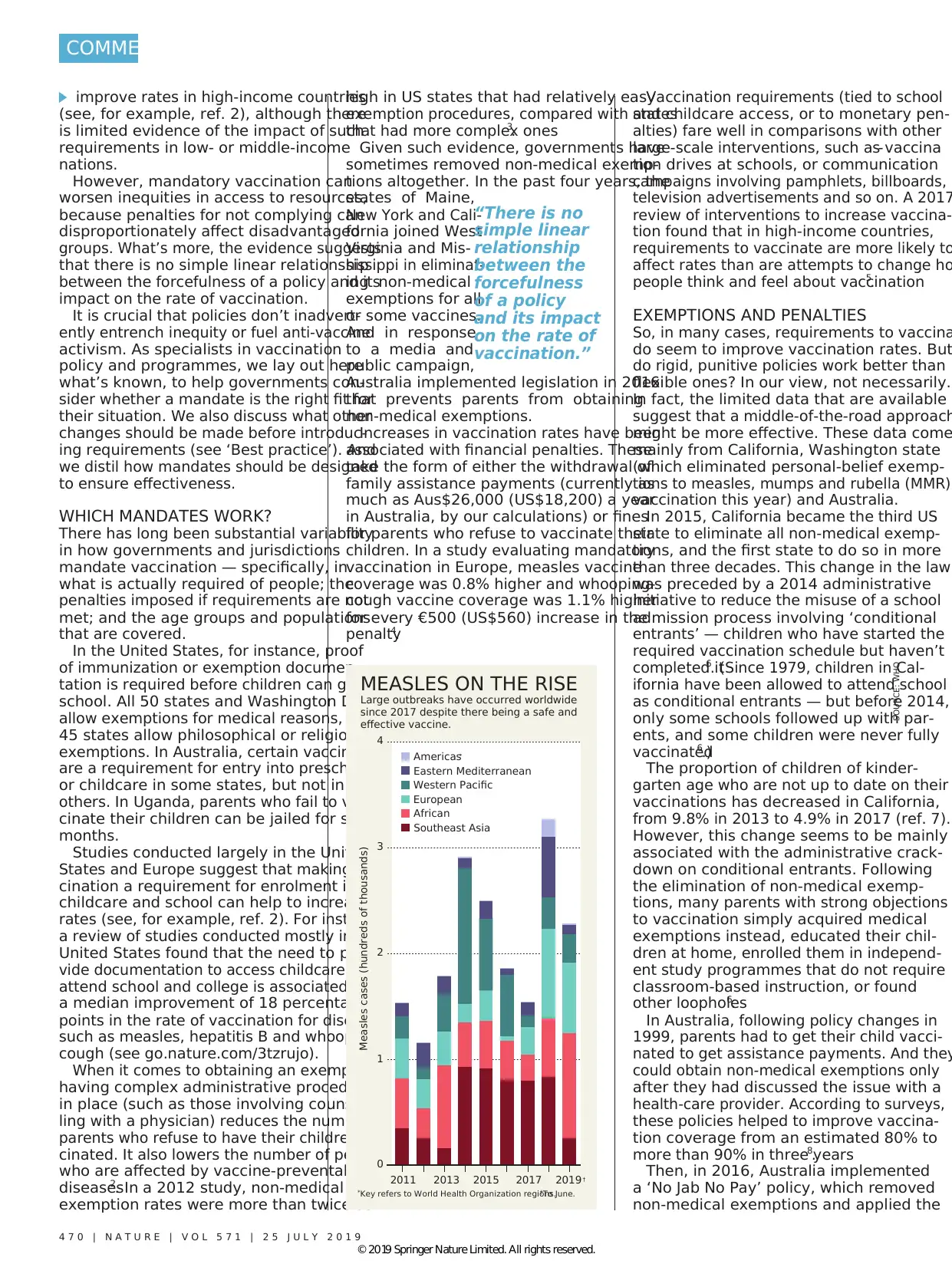
SOURCE: WHO
4 7 0 | N A T U R E | V O L 5 7 1 | 2 5 J U L Y 2 0 1 9
2015 2017 2019 †20132011
Measles cases (hundreds of thousands)
0
1
2
3
4
African
Americas*
Eastern Mediterranean
European
Southeast Asia
Western Pacific
MEASLES ON THE RISE
Large outbreaks have occurred worldwide
since 2017 despite there being a safe and
effective vaccine.
*Key refers to World Health Organization regions.†To June.
COMMENT
© 2019 Springer Nature Limited. All rights reserved.
(see, for example, ref. 2), although there
is limited evidence of the impact of such
requirements in low- or middle-income
nations.
However, mandatory vaccination can
worsen inequities in access to resources,
because penalties for not complying can
disproportionately affect disadvantaged
groups. What’s more, the evidence suggests
that there is no simple linear relationship
between the forcefulness of a policy and its
impact on the rate of vaccination.
It is crucial that policies don’t inadvert-
ently entrench inequity or fuel anti-vaccine
activism. As specialists in vaccination
policy and programmes, we lay out here
what’s known, to help governments con-
sider whether a mandate is the right fit for
their situation. We also discuss what other
changes should be made before introduc-
ing requirements (see ‘Best practice’). And
we distil how mandates should be designed
to ensure effectiveness.
WHICH MANDATES WORK?
There has long been substantial variability
in how governments and jurisdictions
mandate vaccination — specifically, in
what is actually required of people; the
penalties imposed if requirements are not
met; and the age groups and populations
that are covered.
In the United States, for instance, proof
of immunization or exemption documen-
tation is required before children can go to
school. All 50 states and Washington DC
allow exemptions for medical reasons, and
45 states allow philosophical or religious
exemptions. In Australia, certain vaccines
are a requirement for entry into preschool
or childcare in some states, but not in
others. In Uganda, parents who fail to vac-
cinate their children can be jailed for six
months.
Studies conducted largely in the United
States and Europe suggest that making vac-
cination a requirement for enrolment in
childcare and school can help to increase
rates (see, for example, ref. 2). For instance,
a review of studies conducted mostly in the
United States found that the need to pro-
vide documentation to access childcare or to
attend school and college is associated with
a median improvement of 18 percentage
points in the rate of vaccination for diseases
such as measles, hepatitis B and whooping
cough (see go.nature.com/3tzrujo).
When it comes to obtaining an exemption,
having complex administrative procedures
in place (such as those involving counsel-
ling with a physician) reduces the number of
parents who refuse to have their children vac-
cinated. It also lowers the number of people
who are affected by vaccine-preventable
diseases2
. In a 2012 study, non-medical
exemption rates were more than twice as
high in US states that had relatively easy
exemption procedures, compared with states
that had more complex ones3.
Given such evidence, governments have
sometimes removed non-medical exemp-
tions altogether. In the past four years, the
states of Maine,
New York and Cali-
fornia joined West
Virginia and Mis-
sissippi in eliminat-
ing non-medical
exemptions for all
or some vaccines.
And in response
to a media and
public campaign,
Australia implemented legislation in 2016
that prevents parents from obtaining
non-medical exemptions.
Increases in vaccination rates have been
associated with financial penalties. These
take the form of either the withdrawal of
family assistance payments (currently as
much as Aus$26,000 (US$18,200) a year
in Australia, by our calculations) or fines
for parents who refuse to vaccinate their
children. In a study evaluating mandatory
vaccination in Europe, measles vaccine
coverage was 0.8% higher and whooping-
cough vaccine coverage was 1.1% higher
for every €500 (US$560) increase in the
penalty4.
Vaccination requirements (tied to school
and childcare access, or to monetary pen-
alties) fare well in comparisons with other
large-scale interventions, such as vaccina-
tion drives at schools, or communication
campaigns involving pamphlets, billboards,
television advertisements and so on. A 2017
review of interventions to increase vaccina-
tion found that in high-income countries,
requirements to vaccinate are more likely to
affect rates than are attempts to change ho
people think and feel about vaccination5.
EXEMPTIONS AND PENALTIES
So, in many cases, requirements to vaccina
do seem to improve vaccination rates. But
do rigid, punitive policies work better than
flexible ones? In our view, not necessarily.
In fact, the limited data that are available
suggest that a middle-of-the-road approach
might be more effective. These data come
mainly from California, Washington state
(which eliminated personal-belief exemp-
tions to measles, mumps and rubella (MMR)
vaccination this year) and Australia.
In 2015, California became the third US
state to eliminate all non-medical exemp-
tions, and the first state to do so in more
than three decades. This change in the law
was preceded by a 2014 administrative
initiative to reduce the misuse of a school
admission process involving ‘conditional
entrants’ — children who have started the
required vaccination schedule but haven’t
completed it6
. (Since 1979, children in Cal-
ifornia have been allowed to attend school
as conditional entrants — but before 2014,
only some schools followed up with par-
ents, and some children were never fully
vaccinated6.)
The proportion of children of kinder-
garten age who are not up to date on their
vaccinations has decreased in California,
from 9.8% in 2013 to 4.9% in 2017 (ref. 7).
However, this change seems to be mainly
associated with the administrative crack-
down on conditional entrants. Following
the elimination of non-medical exemp-
tions, many parents with strong objections
to vaccination simply acquired medical
exemptions instead, educated their chil-
dren at home, enrolled them in independ-
ent study programmes that do not require
classroom-based instruction, or found
other loopholes6.
In Australia, following policy changes in
1999, parents had to get their child vacci-
nated to get assistance payments. And they
could obtain non-medical exemptions only
after they had discussed the issue with a
health-care provider. According to surveys,
these policies helped to improve vaccina-
tion coverage from an estimated 80% to
more than 90% in three years8.
Then, in 2016, Australia implemented
a ‘No Jab No Pay’ policy, which removed
non-medical exemptions and applied the
“There is no
simple linear
relationship
between the
forcefulness
of a policy
and its impact
on the rate of
vaccination.”
SOURCE: WHO
4 7 0 | N A T U R E | V O L 5 7 1 | 2 5 J U L Y 2 0 1 9
2015 2017 2019 †20132011
Measles cases (hundreds of thousands)
0
1
2
3
4
African
Americas*
Eastern Mediterranean
European
Southeast Asia
Western Pacific
MEASLES ON THE RISE
Large outbreaks have occurred worldwide
since 2017 despite there being a safe and
effective vaccine.
*Key refers to World Health Organization regions.†To June.
COMMENT
© 2019 Springer Nature Limited. All rights reserved.

loss of payments more frequently. Overall
immunization rates for five-year-olds
have since increased nationally, from
92.6% in 2015 to 94.8% by March 2019
(see go.nature.com/2xmgtun). But this
smaller improvement comes after the
roll-out of several concurrent strategies
designed to improve coverage — from
schemes to remind parents to get their
child vaccinated, to campaigns to improve
public awareness. So the impact of the ‘No
Jab No Pay’ policy alone is unclear.
In 2017, one of us (J.L.) was involved
in a study that interviewed 31 parents in
Australia who were refusing vaccination
for their child9. Of this group, 17 indicated
that they planned to get more involved in
protest action if additional such measures
were implemented, because they felt that
the government was coercing them. Inter-
estingly, in an experimental study10
, more
people with a negative attitude towards
vaccination chose to accept a hypothetical
second vaccine when they had previously
been told that they could choose to be vac-
cinated with a first vaccine. When these
individuals were told that they had to be
vaccinated with the first vaccine, 39% less
people elected to receive the optional one10
.
In short, various findings suggest that the
most effective approach when it comes to
mandating vaccination could be to allow
non-medical exemptions, but to make
them hard to obtain. Removing the choice
of opting out entirely might simply induce
parents to seek loopholes, and, worse, fuel
negative attitudes towards vaccination.
SMART AND ETHICAL
If vaccination rates are low in a particular
region or community, a government’s
first step must be to find out why. Guid-
ance from the WHO Regional Office for
Europe, for example, lays out steps for tar-
geting specific communities, such as by
working with community leaders, health-
care workers and service users to establish
whether people are struggling to get to
their local clinics or avoiding health-care
providers for some other reason11
. (J. L.
was a reviewer of this guide, and all three
of us have received funds from the WHO,
which, as a UN agency, has no financial
competing interest regarding this article.)
Mandates are often inspired by the per-
ception among politicians and the public
that vaccine refusal by parents is the big-
gest problem. But poverty, social exclusion
and difficulties over access also depress
rates, and, in many settings, more so than
refusal. In Germany, for example, barriers
to access probably explain why children of
migrant parents have a 10% lower immu-
nization rate for booster doses (such as fo
tetanus or human papillomavirus) than do
children who were born there12
.
A requirement to vaccinate when the
vaccine or primary-care service is difficult
or impossible for many people to reach is
not justifiable or fair13
. Thus, before even
considering mandates, governments must
ensure that people from all sectors of
society can get vaccines easily and safely
This means making primary-care services
flexible, welcoming and easy to reach, and
ensuring a stable supply of vaccines.
If governments then decide that
mandates are appropriate, they should tak
the following five steps.
Use multiple interventions. Ideally,
requirements to vaccinate should be part
of a suite of interventions. These could
include: robust methods for recording
immunization, such as in a registry; text-
message or e-mail reminders to parents
before a child’s vaccines are due; and a
process to monitor and give feedback on
how primary-care providers perform on
vaccination rates5 (see also go.nature.
Parents on a march protesting against mandatory vaccinations in Washington state earlier this year.
2 5 J U L Y 2 0 1 9 | V O L 5 7 1 | N A T U R E | 4 7 1
COMMENT
LINDSEY WASSON/REUTERS
© 2019 Springer Nature Limited. All rights reserved.
immunization rates for five-year-olds
have since increased nationally, from
92.6% in 2015 to 94.8% by March 2019
(see go.nature.com/2xmgtun). But this
smaller improvement comes after the
roll-out of several concurrent strategies
designed to improve coverage — from
schemes to remind parents to get their
child vaccinated, to campaigns to improve
public awareness. So the impact of the ‘No
Jab No Pay’ policy alone is unclear.
In 2017, one of us (J.L.) was involved
in a study that interviewed 31 parents in
Australia who were refusing vaccination
for their child9. Of this group, 17 indicated
that they planned to get more involved in
protest action if additional such measures
were implemented, because they felt that
the government was coercing them. Inter-
estingly, in an experimental study10
, more
people with a negative attitude towards
vaccination chose to accept a hypothetical
second vaccine when they had previously
been told that they could choose to be vac-
cinated with a first vaccine. When these
individuals were told that they had to be
vaccinated with the first vaccine, 39% less
people elected to receive the optional one10
.
In short, various findings suggest that the
most effective approach when it comes to
mandating vaccination could be to allow
non-medical exemptions, but to make
them hard to obtain. Removing the choice
of opting out entirely might simply induce
parents to seek loopholes, and, worse, fuel
negative attitudes towards vaccination.
SMART AND ETHICAL
If vaccination rates are low in a particular
region or community, a government’s
first step must be to find out why. Guid-
ance from the WHO Regional Office for
Europe, for example, lays out steps for tar-
geting specific communities, such as by
working with community leaders, health-
care workers and service users to establish
whether people are struggling to get to
their local clinics or avoiding health-care
providers for some other reason11
. (J. L.
was a reviewer of this guide, and all three
of us have received funds from the WHO,
which, as a UN agency, has no financial
competing interest regarding this article.)
Mandates are often inspired by the per-
ception among politicians and the public
that vaccine refusal by parents is the big-
gest problem. But poverty, social exclusion
and difficulties over access also depress
rates, and, in many settings, more so than
refusal. In Germany, for example, barriers
to access probably explain why children of
migrant parents have a 10% lower immu-
nization rate for booster doses (such as fo
tetanus or human papillomavirus) than do
children who were born there12
.
A requirement to vaccinate when the
vaccine or primary-care service is difficult
or impossible for many people to reach is
not justifiable or fair13
. Thus, before even
considering mandates, governments must
ensure that people from all sectors of
society can get vaccines easily and safely
This means making primary-care services
flexible, welcoming and easy to reach, and
ensuring a stable supply of vaccines.
If governments then decide that
mandates are appropriate, they should tak
the following five steps.
Use multiple interventions. Ideally,
requirements to vaccinate should be part
of a suite of interventions. These could
include: robust methods for recording
immunization, such as in a registry; text-
message or e-mail reminders to parents
before a child’s vaccines are due; and a
process to monitor and give feedback on
how primary-care providers perform on
vaccination rates5 (see also go.nature.
Parents on a march protesting against mandatory vaccinations in Washington state earlier this year.
2 5 J U L Y 2 0 1 9 | V O L 5 7 1 | N A T U R E | 4 7 1
COMMENT
LINDSEY WASSON/REUTERS
© 2019 Springer Nature Limited. All rights reserved.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

com/3puzrga). All of these interventions
should be in place whether or not mandates
are implemented (see ‘Best practice’).
Ensure just procedures. Limited restric-
tions on personal autonomy are more likely
to be workable in democracies. In these,
societies are more able to express their
collective will than in dictatorships, where
such restrictions can be abused. Indeed,
it is crucial that the process of develop-
ing mandates is itself democratic. Delib-
erative methods can ask what an informed
citizenry would find an acceptable policy
response and why. A good model is the
community juries used for more than
two decades, mostly in the United States,
Australia and Canada, to address policy
issues in other areas of health care, such
as for cancer screening. In these, panels
of citizens hear evidence, then debate the
issue and give their verdicts14
.
Make penalties proportionate. In our
view, incarceration is never justified
for enforcing vaccination. Temporary
quarantine or the use of child protection
laws might be an appropriate action when
the risk of a vaccine-preventable disease
is very high (such as in a newborn whose
mother tests positive for hepatitis B)15
. Even
with penalties such as fines, withheld bene-
fits or blocked entry to childcare or schools,
care must be taken to ensure that they do
not exacerbate social or health inequities.
Monitor safety and compensate for side
effects. In the exceedingly rare instances in
which required vaccines cause harm, those
affected should be adequately compen-
sated. (For instance, around 2.6 cases of the
rare bleeding disorder thrombocytopenic
purpura arise for every 100,000 doses of
MMR vaccine that are given16
.)
Proactive surveillance systems that
monitor side effects should be paired with
a timely programme for compensation
that minimizes administrative and legal
burdens for those injured17
. In the United
States, people seeking compensation
following vaccination have to demonstrate
only that they (or their child) had an
adverse event known to be associated
with the vaccine. By contrast, people in
Australia have to pursue compensation
through the courts — a time-consuming
and expensive process.
Such programmes can be financially
sustainable. In the United States, vaccine
manufacturers are taxed on vaccines sold
in the country to finance this (currently,
75 cents per antigen). Other financial mod-
els have been proposed, including for low
and middle-income countries18
.
Avoid selective mandates. Governments
should avoid making specific vaccines
mand ator y.In
Fr a n c ei n t h e
1960s, there was a
policy shift. Older
vaccines such as
those for smallpox,
diphtheria, tetanus,
tuberculosis and
polio remained
mandatory; newer
ones for diseases such as measles were only
‘recommended’19
. For many years, there
has been a difference in uptake of up to
20% between the two classes. Vaccines that
were ‘only’ recommended were perceived
as non-essential by French parents. (In
2018, the recommended vaccines became
mandatory20
.) And experimental evidence
shows that making one vaccine mandatory
might reduce people’s uptake of others10
.
In our view, Germany, which is currently
considering a mandate for just measles,
should rethink.
In summary, making vaccination a
legal requirement can be a powerful and
effective tool if implemented with care and
with regard to the context. Crucially, evi-
dence for the effectiveness of mandates is
largely limited to high-income countries.
Overly strict mandates can result in
parents finding ways to avoid the vaccine
requirements, and selective mandates
might damage the broader vaccination
programme. Most importantly, vaccine
policy — like other types of effective public
policy — must be based on evidence, and
not driven by political and ideological
considerations.■
Saad B. Omer is the director of the Yale
Institute for Global Health; professor of
medicine (infectious diseases) at Yale Schoo
of Medicine; and professor of epidemiology
of microbial diseases at Yale School of
Public Health, New Haven, Connecticut,
USA. Cornelia Betsch is professor of
health communication at the University of
Erfurt, Psychology and Infectious Diseases
Lab, Erfurt, Germany. Julie Leask is
professor in the Susan Wakil School of
Nursing and Midwifery at the University
of Sydney, Faculty of Medicine and Health,
Camperdown, New South Wales, Australia.
e-mail: julie.leask@sydney.edu.au
1. MacDonald, N. E. et al. Vaccine 36, 5811–5818
(2018).
2. Omer, S. B. et al. J. Am. Med. Assoc. 296,
1757–1763 (2006).
3. Omer, S. B., Richards, J. L., Ward, M. &
Bednarczyk, R. A. N. Engl. J. Med. 367,
1170–1171 (2012).
4. Vaz, O. M. et al. Pediatrics (in the press).
5. Brewer, N. T., Chapman, G. B., Rothman, A. J.,
Leask, J. & Kempe, A. Psychol. Sci. Public Interest
18, 149–207 (2017).
6. Delamater P. L. et al. Pediatrics 143, e20183301
(2019).
7. Pingali, S. C. et al. J. Am. Med. Assoc. 322, 49–56
(2019).
8. Bond, L., Davie, G., Carlin, J. B., Lester, R. & Nolan,
T. Aust. N. Z. J. Public Health 26, 58–64 (2002).
9. Helps, C., Leask, J. & Barclay, L. J. Pub. Health
Policy 39, 156–169 (2018).
10. Betsch, C. & Böhm, R. Eur. J. Public Health 26,
378–381 (2016).
11. World Health Organization Regional Office for
Europe. The Guide to Tailoring Immunization
Programmes (TIP) (WHO, 2013).
12. Poethko-Müller, C., Kuhnert, R., Gillesberg
Lassen, S. & Siedler, A. [in German]
Bundesgesundheitsblatt Gesundheitsforschung
Gesundheitsschutz 62, 410–421 (2019).
13. Boyce, T. et al. Eurosurveillance 24, 1800204
(2019).
14. Degeling, C., Rychetnik, L., Street, J., Thomas, R.
& Carter, S. M. Soc. Sci. Med. 179, 166–171
(2017).
15. Isaacs, D., Kilham, H., Leask, J. & Tobin, B. Vaccine
27, 615–618 (2009).
16. Mantadakis, E., Farmaki, E. & Buchanan, G. R.
J. Pediatr. 156, 623–628 (2010).
17. Attwell, K., Drislane, S. & Leask, J. Vaccine 37,
2843–2848 (2019).
18. Halabi, S. & Omer, S. B. J. Am. Med. Assoc. 317,
471–472 (2017).
19. Attwell, K. et al. Vaccine 36, 7377–7384 (2018).
20. Lévy-Bruhl D. et al. Eurosurveillance 24, 1900301
(2019).
“Experimental
evidence shows
that making
one vaccine
mandatory
might reduce
people’s uptake
of others.”
4 7 2 | N A T U R E | V O L 5 7 1 | 2 5 J U L Y 2 0 1 9
COMMENT
Ensure everyone can
access vaccines
Use immunization
registry and reminders
Diagnose reasons for
under-vaccination
Monitor performance of
providers and give feedback
Provide vaccinations in
communities
Make clinics welcoming,
safe and easy to get to
Ensure stable supply
of vaccines
Use multiple interventions
to improve uptake
Create smart and
ethical mandates
Ensure procedures
are fair
Make penalties
appropriate
Compensate for
side effects
Avoid implementing
selective mandates
Essential
If mandates are politically
considered appropriate
STEP 1 STEP 2 STEP 3
Monitor safety
BEST PRACTICE
Before even considering mandatory vaccination, governments must first ensure easy access to vaccines.
(Examples in white boxes are not exhaustive.)
© 2019 Springer Nature Limited. All rights reserved.
should be in place whether or not mandates
are implemented (see ‘Best practice’).
Ensure just procedures. Limited restric-
tions on personal autonomy are more likely
to be workable in democracies. In these,
societies are more able to express their
collective will than in dictatorships, where
such restrictions can be abused. Indeed,
it is crucial that the process of develop-
ing mandates is itself democratic. Delib-
erative methods can ask what an informed
citizenry would find an acceptable policy
response and why. A good model is the
community juries used for more than
two decades, mostly in the United States,
Australia and Canada, to address policy
issues in other areas of health care, such
as for cancer screening. In these, panels
of citizens hear evidence, then debate the
issue and give their verdicts14
.
Make penalties proportionate. In our
view, incarceration is never justified
for enforcing vaccination. Temporary
quarantine or the use of child protection
laws might be an appropriate action when
the risk of a vaccine-preventable disease
is very high (such as in a newborn whose
mother tests positive for hepatitis B)15
. Even
with penalties such as fines, withheld bene-
fits or blocked entry to childcare or schools,
care must be taken to ensure that they do
not exacerbate social or health inequities.
Monitor safety and compensate for side
effects. In the exceedingly rare instances in
which required vaccines cause harm, those
affected should be adequately compen-
sated. (For instance, around 2.6 cases of the
rare bleeding disorder thrombocytopenic
purpura arise for every 100,000 doses of
MMR vaccine that are given16
.)
Proactive surveillance systems that
monitor side effects should be paired with
a timely programme for compensation
that minimizes administrative and legal
burdens for those injured17
. In the United
States, people seeking compensation
following vaccination have to demonstrate
only that they (or their child) had an
adverse event known to be associated
with the vaccine. By contrast, people in
Australia have to pursue compensation
through the courts — a time-consuming
and expensive process.
Such programmes can be financially
sustainable. In the United States, vaccine
manufacturers are taxed on vaccines sold
in the country to finance this (currently,
75 cents per antigen). Other financial mod-
els have been proposed, including for low
and middle-income countries18
.
Avoid selective mandates. Governments
should avoid making specific vaccines
mand ator y.In
Fr a n c ei n t h e
1960s, there was a
policy shift. Older
vaccines such as
those for smallpox,
diphtheria, tetanus,
tuberculosis and
polio remained
mandatory; newer
ones for diseases such as measles were only
‘recommended’19
. For many years, there
has been a difference in uptake of up to
20% between the two classes. Vaccines that
were ‘only’ recommended were perceived
as non-essential by French parents. (In
2018, the recommended vaccines became
mandatory20
.) And experimental evidence
shows that making one vaccine mandatory
might reduce people’s uptake of others10
.
In our view, Germany, which is currently
considering a mandate for just measles,
should rethink.
In summary, making vaccination a
legal requirement can be a powerful and
effective tool if implemented with care and
with regard to the context. Crucially, evi-
dence for the effectiveness of mandates is
largely limited to high-income countries.
Overly strict mandates can result in
parents finding ways to avoid the vaccine
requirements, and selective mandates
might damage the broader vaccination
programme. Most importantly, vaccine
policy — like other types of effective public
policy — must be based on evidence, and
not driven by political and ideological
considerations.■
Saad B. Omer is the director of the Yale
Institute for Global Health; professor of
medicine (infectious diseases) at Yale Schoo
of Medicine; and professor of epidemiology
of microbial diseases at Yale School of
Public Health, New Haven, Connecticut,
USA. Cornelia Betsch is professor of
health communication at the University of
Erfurt, Psychology and Infectious Diseases
Lab, Erfurt, Germany. Julie Leask is
professor in the Susan Wakil School of
Nursing and Midwifery at the University
of Sydney, Faculty of Medicine and Health,
Camperdown, New South Wales, Australia.
e-mail: julie.leask@sydney.edu.au
1. MacDonald, N. E. et al. Vaccine 36, 5811–5818
(2018).
2. Omer, S. B. et al. J. Am. Med. Assoc. 296,
1757–1763 (2006).
3. Omer, S. B., Richards, J. L., Ward, M. &
Bednarczyk, R. A. N. Engl. J. Med. 367,
1170–1171 (2012).
4. Vaz, O. M. et al. Pediatrics (in the press).
5. Brewer, N. T., Chapman, G. B., Rothman, A. J.,
Leask, J. & Kempe, A. Psychol. Sci. Public Interest
18, 149–207 (2017).
6. Delamater P. L. et al. Pediatrics 143, e20183301
(2019).
7. Pingali, S. C. et al. J. Am. Med. Assoc. 322, 49–56
(2019).
8. Bond, L., Davie, G., Carlin, J. B., Lester, R. & Nolan,
T. Aust. N. Z. J. Public Health 26, 58–64 (2002).
9. Helps, C., Leask, J. & Barclay, L. J. Pub. Health
Policy 39, 156–169 (2018).
10. Betsch, C. & Böhm, R. Eur. J. Public Health 26,
378–381 (2016).
11. World Health Organization Regional Office for
Europe. The Guide to Tailoring Immunization
Programmes (TIP) (WHO, 2013).
12. Poethko-Müller, C., Kuhnert, R., Gillesberg
Lassen, S. & Siedler, A. [in German]
Bundesgesundheitsblatt Gesundheitsforschung
Gesundheitsschutz 62, 410–421 (2019).
13. Boyce, T. et al. Eurosurveillance 24, 1800204
(2019).
14. Degeling, C., Rychetnik, L., Street, J., Thomas, R.
& Carter, S. M. Soc. Sci. Med. 179, 166–171
(2017).
15. Isaacs, D., Kilham, H., Leask, J. & Tobin, B. Vaccine
27, 615–618 (2009).
16. Mantadakis, E., Farmaki, E. & Buchanan, G. R.
J. Pediatr. 156, 623–628 (2010).
17. Attwell, K., Drislane, S. & Leask, J. Vaccine 37,
2843–2848 (2019).
18. Halabi, S. & Omer, S. B. J. Am. Med. Assoc. 317,
471–472 (2017).
19. Attwell, K. et al. Vaccine 36, 7377–7384 (2018).
20. Lévy-Bruhl D. et al. Eurosurveillance 24, 1900301
(2019).
“Experimental
evidence shows
that making
one vaccine
mandatory
might reduce
people’s uptake
of others.”
4 7 2 | N A T U R E | V O L 5 7 1 | 2 5 J U L Y 2 0 1 9
COMMENT
Ensure everyone can
access vaccines
Use immunization
registry and reminders
Diagnose reasons for
under-vaccination
Monitor performance of
providers and give feedback
Provide vaccinations in
communities
Make clinics welcoming,
safe and easy to get to
Ensure stable supply
of vaccines
Use multiple interventions
to improve uptake
Create smart and
ethical mandates
Ensure procedures
are fair
Make penalties
appropriate
Compensate for
side effects
Avoid implementing
selective mandates
Essential
If mandates are politically
considered appropriate
STEP 1 STEP 2 STEP 3
Monitor safety
BEST PRACTICE
Before even considering mandatory vaccination, governments must first ensure easy access to vaccines.
(Examples in white boxes are not exhaustive.)
© 2019 Springer Nature Limited. All rights reserved.
1 out of 4
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





