Hand Hygiene and Infection Control in Gastroenterology: A Report
VerifiedAdded on 2020/04/15
|19
|4131
|56
Report
AI Summary
This report examines hand hygiene practices within gastroenterology wards, emphasizing the crucial role in preventing infections. It explores the application of the Plan-Do-Study-Act (PDSA) model to improve hand hygiene protocols, detailing each stage of the model and its strengths and limitations. The report highlights the roles of nurses, physicians, and managers in implementing and overseeing hand hygiene initiatives, including staff education and antimicrobial stewardship programs. It discusses the importance of organizational factors and inter-facility collaboration. The study also analyzes the strengths and limitations of the PDSA model and the challenges faced by healthcare professionals in promoting hand hygiene, such as ethical barriers and resource constraints, offering recommendations for enhancing hand hygiene practices and improving patient outcomes in gastroenterology settings.

Running head: HAND HYGIENE
Hand hygiene
Name of the student
University name
Authors’ note
Hand hygiene
Name of the student
University name
Authors’ note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HAND HYGIENE
Table of Contents
Introduction..................................................................................................................................2
Description of issue......................................................................................................................2
Application of hand hygiene based on PDSA.................................................................................4
Strength of the model.......................................................................................................................5
Limitations of the PDSA model......................................................................................................5
Role of the nurse..........................................................................................................................6
Strength............................................................................................................................................6
Limitations.......................................................................................................................................7
Physician’s role............................................................................................................................7
Critical solution by managers..........................................................................................................7
Application of PDSA model by managers for controlling the rate of infection in gastroenterology
wards................................................................................................................................................8
Strengths and limitations of the managers in healthcare wards.....................................................10
Effectiveness of Registered nurse in establishment of quality improvement initiative.............10
Recommendations for hand hygiene initiative...........................................................................12
Conclusion.................................................................................................................................13
References..................................................................................................................................14
Table of Contents
Introduction..................................................................................................................................2
Description of issue......................................................................................................................2
Application of hand hygiene based on PDSA.................................................................................4
Strength of the model.......................................................................................................................5
Limitations of the PDSA model......................................................................................................5
Role of the nurse..........................................................................................................................6
Strength............................................................................................................................................6
Limitations.......................................................................................................................................7
Physician’s role............................................................................................................................7
Critical solution by managers..........................................................................................................7
Application of PDSA model by managers for controlling the rate of infection in gastroenterology
wards................................................................................................................................................8
Strengths and limitations of the managers in healthcare wards.....................................................10
Effectiveness of Registered nurse in establishment of quality improvement initiative.............10
Recommendations for hand hygiene initiative...........................................................................12
Conclusion.................................................................................................................................13
References..................................................................................................................................14

2HAND HYGIENE
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HAND HYGIENE
Introduction
Quality and safety management is crucial in the context of prevention of infections within
an acute healthcare setup. The quality management here refers to taking care of the overall
aspects of healthcare which are pivotal in maintaining an aseptic condition within the care
setting. For the current study we have taken into consideration hand hygiene which helps in
reducing the chances of infection within a hospital framework. The focus has been narrowed
down to the application of the project initiative within the Gastroenterology Healthcare centre,
Toronto upon the Plan DO Study Act (PDSA) model. The paper discusses the issue in more detail
focussing upon the importance of hand hygiene and relation of the same in ensuring health
improvements within the concerned department. The study further elaborates the role of the
nurses in ensuring the efficiency of the aforementioned processes.
Description of issue
Hand hygiene has been described as the single most effective method of infection prevention
(CDC, 2002; World Health Organization [WHO], 2009). The cleaning of hands before, after and
during surgical processes is crucial in the prevention of infection through the spread of
microorganisms. As commented by Septimus et al. (2014), increased use of hand hygiene
equipments have been seen to reduce the incidents of infection spread within healthcare centres.
Some of the disinfectants which could be used over here are –soap dispensers, alcohol based
foam dispensers, paper towel dispensers. The statistical figures showed a 24 % reduction in the
healthcare associated infections after the implementation of the disinfection process on a regular
basis. This resulted in saving approximately 27 % of the cost of antibiotics (Moraros, Lemstra, &
Nwankwo, 2016).
Introduction
Quality and safety management is crucial in the context of prevention of infections within
an acute healthcare setup. The quality management here refers to taking care of the overall
aspects of healthcare which are pivotal in maintaining an aseptic condition within the care
setting. For the current study we have taken into consideration hand hygiene which helps in
reducing the chances of infection within a hospital framework. The focus has been narrowed
down to the application of the project initiative within the Gastroenterology Healthcare centre,
Toronto upon the Plan DO Study Act (PDSA) model. The paper discusses the issue in more detail
focussing upon the importance of hand hygiene and relation of the same in ensuring health
improvements within the concerned department. The study further elaborates the role of the
nurses in ensuring the efficiency of the aforementioned processes.
Description of issue
Hand hygiene has been described as the single most effective method of infection prevention
(CDC, 2002; World Health Organization [WHO], 2009). The cleaning of hands before, after and
during surgical processes is crucial in the prevention of infection through the spread of
microorganisms. As commented by Septimus et al. (2014), increased use of hand hygiene
equipments have been seen to reduce the incidents of infection spread within healthcare centres.
Some of the disinfectants which could be used over here are –soap dispensers, alcohol based
foam dispensers, paper towel dispensers. The statistical figures showed a 24 % reduction in the
healthcare associated infections after the implementation of the disinfection process on a regular
basis. This resulted in saving approximately 27 % of the cost of antibiotics (Moraros, Lemstra, &
Nwankwo, 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HAND HYGIENE
In the present context, precautionary measures must be taken in dealing with patients
suffering from gastrointestinal issues. The staff may encounter exposure to pathogens such as
Clostridium difficile, vancomycin resistant enterococci (VRE), carbapenam resistant
enterobacteriaceae (CRE). In this respect, rigorous cleaning of the environment with EPA-
registered hospital disinfectant has been seen to eliminate some of the microbial agents such as
C. difficile which have been known to result in acute gastric infection in individuals (Jones et al.,
2016).The aspects of hand hygiene have been further discussed with respect to the PDSA model.
The model has four active components such as ‘Plan, Do, Study and Act’. The application of the
model helps in evaluation of the different steps which could be taken for improvement of quality
within the Gastroenterology health care centre. The different steps of the model have been
represented with the help of flowchart as follows:
What are we trying to accomplish?
How will we know that change is an improvement?
What changes can we make that will result in improvement?
Evaluation of the current scenario through the PDSA model helps in the identification of the
problem situation. The goal is to improve quality of services delivered within the
Gastroenterology healthcare units through implementation of hand hygiene methods. In this
respect, the hand hygiene practices have been promulgated as the cornerstone of preventing
infection by IPAC Canada. The improvements brought about by the implementation of such
methods can be measured using survey analysis. The reduction in the rate of infection after the
application of the cleaning methods could be compared with that of situation before the
In the present context, precautionary measures must be taken in dealing with patients
suffering from gastrointestinal issues. The staff may encounter exposure to pathogens such as
Clostridium difficile, vancomycin resistant enterococci (VRE), carbapenam resistant
enterobacteriaceae (CRE). In this respect, rigorous cleaning of the environment with EPA-
registered hospital disinfectant has been seen to eliminate some of the microbial agents such as
C. difficile which have been known to result in acute gastric infection in individuals (Jones et al.,
2016).The aspects of hand hygiene have been further discussed with respect to the PDSA model.
The model has four active components such as ‘Plan, Do, Study and Act’. The application of the
model helps in evaluation of the different steps which could be taken for improvement of quality
within the Gastroenterology health care centre. The different steps of the model have been
represented with the help of flowchart as follows:
What are we trying to accomplish?
How will we know that change is an improvement?
What changes can we make that will result in improvement?
Evaluation of the current scenario through the PDSA model helps in the identification of the
problem situation. The goal is to improve quality of services delivered within the
Gastroenterology healthcare units through implementation of hand hygiene methods. In this
respect, the hand hygiene practices have been promulgated as the cornerstone of preventing
infection by IPAC Canada. The improvements brought about by the implementation of such
methods can be measured using survey analysis. The reduction in the rate of infection after the
application of the cleaning methods could be compared with that of situation before the
5HAND HYGIENE
application of the control methods. The figures so obtained provide an overview about the
various loopholes and gaps within the delivery of the care services. The gaps could be further
improved with the application of stricter control measures which enhances the quality of the care
services.
Application of hand hygiene based on PDSA
The PDSA model is based upon the objectives of learning through planning, executing
the plan, study the gaps in the processes and act accordingly for the mitigation of the gaps. The
models have been discussed in more details below:
Plan (P):
Will implementing sufficient standards of hand hygiene enhance quality care within the
gastroenterology wards of the hospital?
Will sufficient staff education about the disinfection process help in reducing the rate of
infection?
What are the necessary standards and guidelines which have to be implemented for
achieving success in the above outcome?
Do (D):
The healthcare team need to do planned activities for bringing about the change
Study (S)
Did the planning go right?
Was optimum education regarding the disinfection process given to the staffs?
application of the control methods. The figures so obtained provide an overview about the
various loopholes and gaps within the delivery of the care services. The gaps could be further
improved with the application of stricter control measures which enhances the quality of the care
services.
Application of hand hygiene based on PDSA
The PDSA model is based upon the objectives of learning through planning, executing
the plan, study the gaps in the processes and act accordingly for the mitigation of the gaps. The
models have been discussed in more details below:
Plan (P):
Will implementing sufficient standards of hand hygiene enhance quality care within the
gastroenterology wards of the hospital?
Will sufficient staff education about the disinfection process help in reducing the rate of
infection?
What are the necessary standards and guidelines which have to be implemented for
achieving success in the above outcome?
Do (D):
The healthcare team need to do planned activities for bringing about the change
Study (S)
Did the planning go right?
Was optimum education regarding the disinfection process given to the staffs?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HAND HYGIENE
Were adequate policies and programs followed for the implementation of the objectives
within the gastroenterology healthcare centres?
Act (A):
Based on the results obtained from above interrogation, the gaps or the loopholes are identified
which the team could further work upon.
Strength of the model
There are a number of strengths of the PDSA model such as collective problem and
solution ownership. As commented by Smiddy, O'Connell & Creedon (2015), the collaborative
mode of working helps in building positive relationship between team members. The PDSA
model helps in empowerment of team members through common goal synthesis for achieving
better clinical outcomes. The PDSA provides a structured environment for the realization of the
clinical outcomes (Dai, Milkman, Hofmann & Staats, 2015). The PDSA cycles allow the staff to
better understand the organizational processes. It promotes a gradual shift in accountability for
problems from management to the frontline staff.
Limitations of the PDSA model
There are a number of limitations of the application of the PDSA model such as loss of
momentum due to the removal of a team member. The jumping of the steps of the PDCA cycle
may result in adequate learning which fails to address the root cause of the problem (Smiddy et
al., 2015). The analysis of the problem situation through PDSA requires unit specific and time
sensitive data and is dependent upon human labour for sufficient collection of data. In order to
work through individual steps of the PDSA cycle sufficiently longer time is required.
Were adequate policies and programs followed for the implementation of the objectives
within the gastroenterology healthcare centres?
Act (A):
Based on the results obtained from above interrogation, the gaps or the loopholes are identified
which the team could further work upon.
Strength of the model
There are a number of strengths of the PDSA model such as collective problem and
solution ownership. As commented by Smiddy, O'Connell & Creedon (2015), the collaborative
mode of working helps in building positive relationship between team members. The PDSA
model helps in empowerment of team members through common goal synthesis for achieving
better clinical outcomes. The PDSA provides a structured environment for the realization of the
clinical outcomes (Dai, Milkman, Hofmann & Staats, 2015). The PDSA cycles allow the staff to
better understand the organizational processes. It promotes a gradual shift in accountability for
problems from management to the frontline staff.
Limitations of the PDSA model
There are a number of limitations of the application of the PDSA model such as loss of
momentum due to the removal of a team member. The jumping of the steps of the PDCA cycle
may result in adequate learning which fails to address the root cause of the problem (Smiddy et
al., 2015). The analysis of the problem situation through PDSA requires unit specific and time
sensitive data and is dependent upon human labour for sufficient collection of data. In order to
work through individual steps of the PDSA cycle sufficiently longer time is required.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HAND HYGIENE
Role of the nurse
The nurses play a critical role in reducing the rate of infection within a clinical setup by
the implementation of sufficient policies and procedures. The influences excised by the nurses
within the control of infection can be divided into a number of factors such as – intrapersonal,
interpersonal and organizational factors. The intrapersonal factors here refer to the level of
knowledge, skills along with perceptions or values possessed by the nurses which influence their
set of practices. The interpersonal factors refer to the relation of the nurses with their friends,
peers and patients which further govern the success of the implementation objectives. The
organizational factors refer to the policies norms and culture, which helps in the establishment of
the IPAC standards of clinical hygiene and safety. Additionally, inter facility collaboration can
promote organizational learning regarding techniques and procedures such as alcohol rub for
cleansing hands before, after and during patient handling, which can prevent spread of infection
(Ellingson et al., 2014).The attending nurses need to maintain proper quarantine in dealing with
highly infectious cases. They should wash their hands during each step of attending to the patient
such as making the bed of the patient along with handing and management of the contaminated
soils and articles of the patients.
Strength
In his respect skill building, peer –to –peer role modelling have been seen to positively
influence the implementation of infection control procedures. As commented by Allegranzi, Sax
& Pittet (2013), the old and experienced nurses can preceptor the newly enrolled nurses about the
disinfection methods and control. The nurses also play a significant role in educating the patients
and the respective family members of the patient about the disinfection process.
Role of the nurse
The nurses play a critical role in reducing the rate of infection within a clinical setup by
the implementation of sufficient policies and procedures. The influences excised by the nurses
within the control of infection can be divided into a number of factors such as – intrapersonal,
interpersonal and organizational factors. The intrapersonal factors here refer to the level of
knowledge, skills along with perceptions or values possessed by the nurses which influence their
set of practices. The interpersonal factors refer to the relation of the nurses with their friends,
peers and patients which further govern the success of the implementation objectives. The
organizational factors refer to the policies norms and culture, which helps in the establishment of
the IPAC standards of clinical hygiene and safety. Additionally, inter facility collaboration can
promote organizational learning regarding techniques and procedures such as alcohol rub for
cleansing hands before, after and during patient handling, which can prevent spread of infection
(Ellingson et al., 2014).The attending nurses need to maintain proper quarantine in dealing with
highly infectious cases. They should wash their hands during each step of attending to the patient
such as making the bed of the patient along with handing and management of the contaminated
soils and articles of the patients.
Strength
In his respect skill building, peer –to –peer role modelling have been seen to positively
influence the implementation of infection control procedures. As commented by Allegranzi, Sax
& Pittet (2013), the old and experienced nurses can preceptor the newly enrolled nurses about the
disinfection methods and control. The nurses also play a significant role in educating the patients
and the respective family members of the patient about the disinfection process.
8HAND HYGIENE
Limitations
In a care set up dealing with patients who have been kept in under quarantine, the nurses
have to monitor that the family members of the patient are allowed restricted entry. There are
similar situations where the nurse has to persuade the family members of the visiting patients to
rub their hand with alcohol before they could meet or touch their loved ones (Al-Tawfiq & Pittet,
2013). The application of such restrictions often results in heated exchange of words between the
nursing professionals and the visitors to the hospitals. Therefore, such ethical barriers limit the
potential contributions of the nursing professionals within a care setup.
Physician’s role
In this respect, the physicians attending to the patient can act as a go-to person by the
family members of the patient being admitted to the hospital with serious infections. Therefore,
they need to practice effective communication skills, where they need to be empathetic in their
approach. As commented by Abdella et al. (2014), values and compassion serves as the core
factors for ensuring less ethical dilemmas are faced by the practising physicians as per the IPAC
hygiene standards. The physicians need to look upon the hygiene standards implied by the
nursing professionals and educate the same. They also need to be careful with the equipments for
treating patients in the gastroenterological wards. The instruments should be dipped in ethanol
after every use.
Critical solution by managers
In this respect, the managers of the healthcare centres can act as volunteers for the
promotion of programs such as antimicrobial stewardship. The antimicrobial stewardship is an
excellent tool for improving the clinical outcomes of patients with severe microbial infections by
Limitations
In a care set up dealing with patients who have been kept in under quarantine, the nurses
have to monitor that the family members of the patient are allowed restricted entry. There are
similar situations where the nurse has to persuade the family members of the visiting patients to
rub their hand with alcohol before they could meet or touch their loved ones (Al-Tawfiq & Pittet,
2013). The application of such restrictions often results in heated exchange of words between the
nursing professionals and the visitors to the hospitals. Therefore, such ethical barriers limit the
potential contributions of the nursing professionals within a care setup.
Physician’s role
In this respect, the physicians attending to the patient can act as a go-to person by the
family members of the patient being admitted to the hospital with serious infections. Therefore,
they need to practice effective communication skills, where they need to be empathetic in their
approach. As commented by Abdella et al. (2014), values and compassion serves as the core
factors for ensuring less ethical dilemmas are faced by the practising physicians as per the IPAC
hygiene standards. The physicians need to look upon the hygiene standards implied by the
nursing professionals and educate the same. They also need to be careful with the equipments for
treating patients in the gastroenterological wards. The instruments should be dipped in ethanol
after every use.
Critical solution by managers
In this respect, the managers of the healthcare centres can act as volunteers for the
promotion of programs such as antimicrobial stewardship. The antimicrobial stewardship is an
excellent tool for improving the clinical outcomes of patients with severe microbial infections by
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HAND HYGIENE
analysing each step from infection contraction to recovery, through constant research into the
clinical data and active record keeping (Al-Tawfiq & Pittet, 2013). The programs can be also
used for educating the staffs for coping with future recurrence of such infections. The
implementation of the program can be used for meeting with the loopholes of hand hygiene
techniques implemented within the medical wards. The institution wide programs for guideline
compliance should be followed by the responsible management for reporting of the cases of
infection to the higher authorities, which can help in controlling the rate of infection.
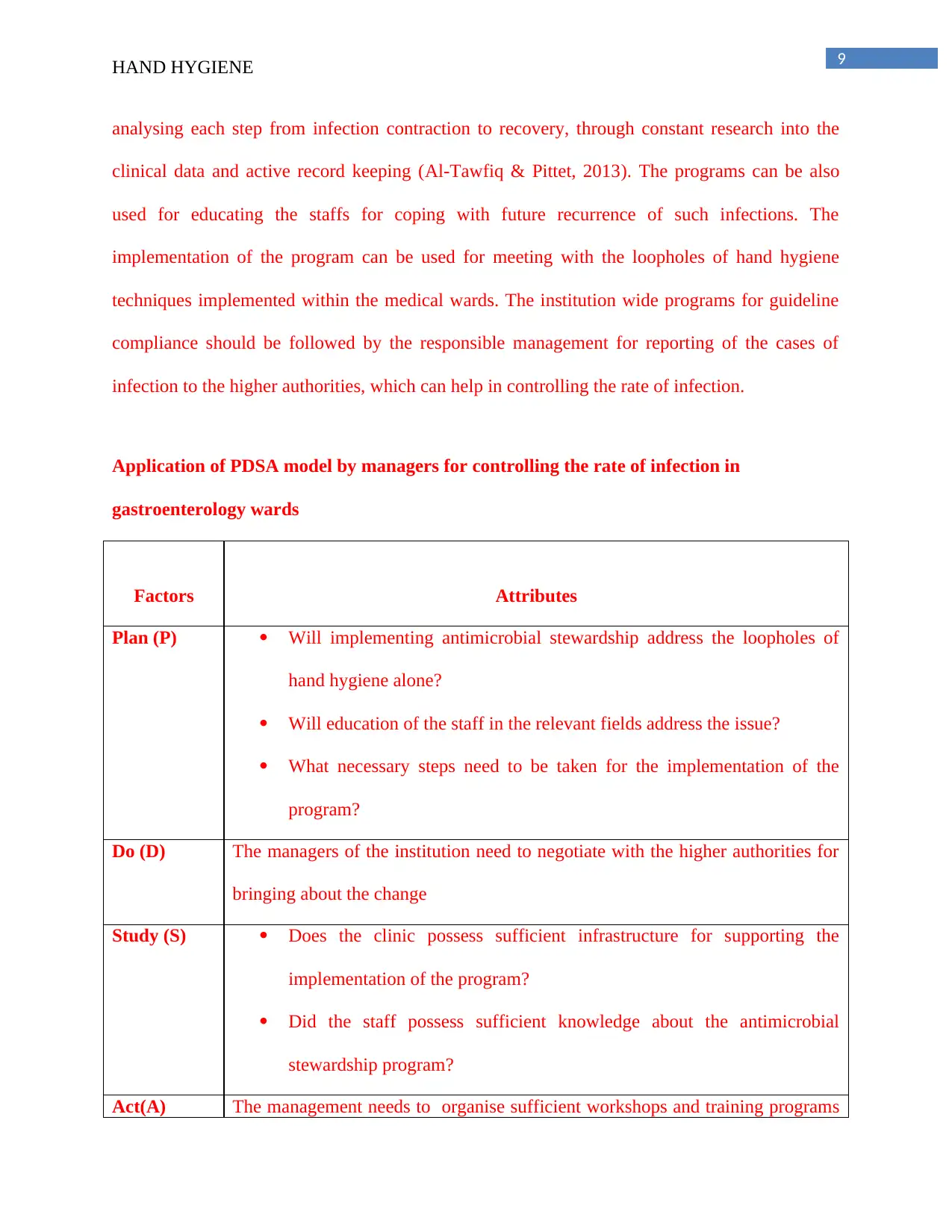
Application of PDSA model by managers for controlling the rate of infection in
gastroenterology wards
Factors Attributes
Plan (P) Will implementing antimicrobial stewardship address the loopholes of
hand hygiene alone?
Will education of the staff in the relevant fields address the issue?
What necessary steps need to be taken for the implementation of the
program?
Do (D) The managers of the institution need to negotiate with the higher authorities for
bringing about the change
Study (S) Does the clinic possess sufficient infrastructure for supporting the
implementation of the program?
Did the staff possess sufficient knowledge about the antimicrobial
stewardship program?
Act(A) The management needs to organise sufficient workshops and training programs
analysing each step from infection contraction to recovery, through constant research into the
clinical data and active record keeping (Al-Tawfiq & Pittet, 2013). The programs can be also
used for educating the staffs for coping with future recurrence of such infections. The
implementation of the program can be used for meeting with the loopholes of hand hygiene
techniques implemented within the medical wards. The institution wide programs for guideline
compliance should be followed by the responsible management for reporting of the cases of
infection to the higher authorities, which can help in controlling the rate of infection.
Application of PDSA model by managers for controlling the rate of infection in
gastroenterology wards
Factors Attributes
Plan (P) Will implementing antimicrobial stewardship address the loopholes of
hand hygiene alone?
Will education of the staff in the relevant fields address the issue?
What necessary steps need to be taken for the implementation of the
program?
Do (D) The managers of the institution need to negotiate with the higher authorities for
bringing about the change
Study (S) Does the clinic possess sufficient infrastructure for supporting the
implementation of the program?
Did the staff possess sufficient knowledge about the antimicrobial
stewardship program?
Act(A) The management needs to organise sufficient workshops and training programs
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10HAND HYGIENE
for educating the staff in the alternate methods of hygiene implementation
Table 1: PDSA model applied by the managers for controlling infection rate in hospitals
and clinics
(Source: Author)
Figure1: Antimicrobial stewardship program
for educating the staff in the alternate methods of hygiene implementation
Table 1: PDSA model applied by the managers for controlling infection rate in hospitals
and clinics
(Source: Author)
Figure1: Antimicrobial stewardship program
11HAND HYGIENE
(Source: Davey et al., 2015)
Strengths and limitations of the managers in healthcare wards
The managers can influence positive organizational processes along with guaranteeing
swift flow of funds through active engagement with stakeholders, for implementation of the
some of the hygiene maintenance protocols and devices. As commented by Smolowitz et al.
(2015), the negotiations skills of the mangers are particularly important in generating
organizational change by focussing more upon the outcomes. The managers can act as
preceptors by training the newly recruited staff about ways to improve organizational
performance by employing active engagement policies.
However, the lack of trained staff and additional funds often delimit the role of the
managers. Additionally, organizational disputes often hinder the application of the said
objectives and programs.
Effectiveness of Registered nurse in establishment of quality improvement
initiative
The registered nurse can play an effective role in controlling the spread of infection
within a clinical set up. Some of the methods which could be applied by the registered nurse are
maintaining active documentation entailing the patient record and history (Unroe et al., 2015).
The time of recurrence of chronic infections can be noted down by the nurse. As commented by
Grol et al. ( 2013), the relapse of chronic infection can often be related to breach of hygiene
(Source: Davey et al., 2015)
Strengths and limitations of the managers in healthcare wards
The managers can influence positive organizational processes along with guaranteeing
swift flow of funds through active engagement with stakeholders, for implementation of the
some of the hygiene maintenance protocols and devices. As commented by Smolowitz et al.
(2015), the negotiations skills of the mangers are particularly important in generating
organizational change by focussing more upon the outcomes. The managers can act as
preceptors by training the newly recruited staff about ways to improve organizational
performance by employing active engagement policies.
However, the lack of trained staff and additional funds often delimit the role of the
managers. Additionally, organizational disputes often hinder the application of the said
objectives and programs.
Effectiveness of Registered nurse in establishment of quality improvement
initiative
The registered nurse can play an effective role in controlling the spread of infection
within a clinical set up. Some of the methods which could be applied by the registered nurse are
maintaining active documentation entailing the patient record and history (Unroe et al., 2015).
The time of recurrence of chronic infections can be noted down by the nurse. As commented by
Grol et al. ( 2013), the relapse of chronic infection can often be related to breach of hygiene
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





