Winter 2024 Nursing Project: Infection Control Patchwork Analysis
VerifiedAdded on 2023/04/19
|23
|5679
|483
Project
AI Summary
This project is a "patchwork" assignment focusing on infection control in healthcare settings. The student explores the importance of hand hygiene, proper techniques, and alternatives like alcohol-based sanitizers. The project then moves on to Personal Protective Equipment (PPE), detailing the different types of PPE and their uses to prevent the spread of germs. The assignment also examines the Aseptic Non-Touch Technique (ANTT) and its key concepts. The student emphasizes the importance of these practices for both healthcare workers and patients, providing an in-depth analysis of each component. The project integrates research findings and aims to provide a comprehensive understanding of infection control measures in nursing practice.
Patch Work - Infection Control
1. Introduction
A "patchwork" is an integration of small segments of design that are individually
complete in itself. They are a collection of short writings or notes carefully structured and
made throughout the duration of the course (Winter, 2003). These small write-ups vary in
style and content. They may include, for example, a review article, a set of notes about a
conference and a comment, notes on seminars attended and other analytical notes of
personal experiences, for example, a visit, a field trip, an interview, an activity in the
classroom, etc. I have decided to create a patch file that is important to me in my future
nursing assignment. Patchwork Text's approach has been framed in such a way that
students can move from a descriptive style to an analytical style of approach which will
help him to be more critically reflective in his professional practice.
I have decided to consolidate research findings on infection control and I have planned to
have four patches which will cover a different area of infection control. These
patchworks will contain information from research articles and will cover the following
areas, Patch 1 will contain information on hand hygiene; patch 2 will have Personal
protective equipment; patch 3 will have ANTT aseptic non-touch technique. And patch 4
will contain Isolation of patients to individual rooms from the ward.
Infection prevention and control (IPC) is a practical solution as well as a scientific
approach introduced to prevent both patients as well as health workers against harm
caused by infection. It is based on infectious diseases, social science, epidemiology and
health system. IPC has occupied an important position in the field of patient safety and
quality and coverage of universal health since it is very much relevant to both the health
1. Introduction
A "patchwork" is an integration of small segments of design that are individually
complete in itself. They are a collection of short writings or notes carefully structured and
made throughout the duration of the course (Winter, 2003). These small write-ups vary in
style and content. They may include, for example, a review article, a set of notes about a
conference and a comment, notes on seminars attended and other analytical notes of
personal experiences, for example, a visit, a field trip, an interview, an activity in the
classroom, etc. I have decided to create a patch file that is important to me in my future
nursing assignment. Patchwork Text's approach has been framed in such a way that
students can move from a descriptive style to an analytical style of approach which will
help him to be more critically reflective in his professional practice.
I have decided to consolidate research findings on infection control and I have planned to
have four patches which will cover a different area of infection control. These
patchworks will contain information from research articles and will cover the following
areas, Patch 1 will contain information on hand hygiene; patch 2 will have Personal
protective equipment; patch 3 will have ANTT aseptic non-touch technique. And patch 4
will contain Isolation of patients to individual rooms from the ward.
Infection prevention and control (IPC) is a practical solution as well as a scientific
approach introduced to prevent both patients as well as health workers against harm
caused by infection. It is based on infectious diseases, social science, epidemiology and
health system. IPC has occupied an important position in the field of patient safety and
quality and coverage of universal health since it is very much relevant to both the health
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
professionals and patients at every health-care encounter (Seto, Otaíza & Pessoa-Silva,
2010). The practices on Infection control are of paramount importance for reduction of
infection transmission from one person to another like the patient to nurse or doctor and
vice versa. The IPC measures are targeted to protect vulnerable people from getting
affected by infection while getting treatment due to ailments. Hygiene is the buzz-word
behind the concept of IPC (Bouchoucha & Moore, 2017).
2. PATCH 1: Hand Hygiene
Contaminated hands are responsible for spreading infection. Routine hand washing is
necessary to control or prevent the communication of infectious disease. However, to
make it more effective we have to follow the proper technique.
2.1 Analysis of Hand Hygiene
2.1.1 The Importance of Handwashing
Handwashing is important for elimination or reduction of microorganisms which are
present in the hands that cannot be seen in open eyes. Handwashing will help in reducing
the communication of these microorganisms to other’s body. Washing hands also reduce
the risk of transmitting infectious elements to our own body. This is important
specifically for nurses and doctors. “The contaminated hands of health workers are a
primary source of transmission of infection in health facilities." (Collins, 2019). It helps
to protect them from the most common diseases such as common cold, flu, diarrhoea etc.
Most people who are prone to infectious diseases, failure to wash hands or wash hands
inappropriately may lead to frequent infection-related diseases such as salmonella or E.
coli. This also may lead to intestinal problems causing diarrhoea and vomiting.
2010). The practices on Infection control are of paramount importance for reduction of
infection transmission from one person to another like the patient to nurse or doctor and
vice versa. The IPC measures are targeted to protect vulnerable people from getting
affected by infection while getting treatment due to ailments. Hygiene is the buzz-word
behind the concept of IPC (Bouchoucha & Moore, 2017).
2. PATCH 1: Hand Hygiene
Contaminated hands are responsible for spreading infection. Routine hand washing is
necessary to control or prevent the communication of infectious disease. However, to
make it more effective we have to follow the proper technique.
2.1 Analysis of Hand Hygiene
2.1.1 The Importance of Handwashing
Handwashing is important for elimination or reduction of microorganisms which are
present in the hands that cannot be seen in open eyes. Handwashing will help in reducing
the communication of these microorganisms to other’s body. Washing hands also reduce
the risk of transmitting infectious elements to our own body. This is important
specifically for nurses and doctors. “The contaminated hands of health workers are a
primary source of transmission of infection in health facilities." (Collins, 2019). It helps
to protect them from the most common diseases such as common cold, flu, diarrhoea etc.
Most people who are prone to infectious diseases, failure to wash hands or wash hands
inappropriately may lead to frequent infection-related diseases such as salmonella or E.
coli. This also may lead to intestinal problems causing diarrhoea and vomiting.
2.1.2 Handwashing Technique
We have to use a few drops of liquid soap or antiseptic liquid and have to rub
vigorously both hands together for around fifteen seconds, then the hands are to be rinsed
completely under running water supply and then we have to dry our hands by using a
clean disposable paper napkin. The technique of hand washing may appear to be simple,
but for effectiveness, it must be done properly. People should be informed about this
handwashing technique, for the maintenance of proper hygiene (Blumstein, 2014).
2.1.3 Short-term alternatives to handwashing
There are some places or occasions when running water may not be easily available,
particularly travelling in a car. In such a situation, we have to use alternate effective
solution. Disinfection includes the use of waterless hand sanitizers containing alcohol.
Alcohol is known to be a very effective disinfectant and it evaporates fast. The hand
sanitizers and antimicrobial gels are available in small bottles and can easily be carried
inside our briefcases ("60% Alcohol-Based Hand Sanitizer Found to Be Most Effective", 2019).
This method of handwashing improves the compliance of handwashing, especially in
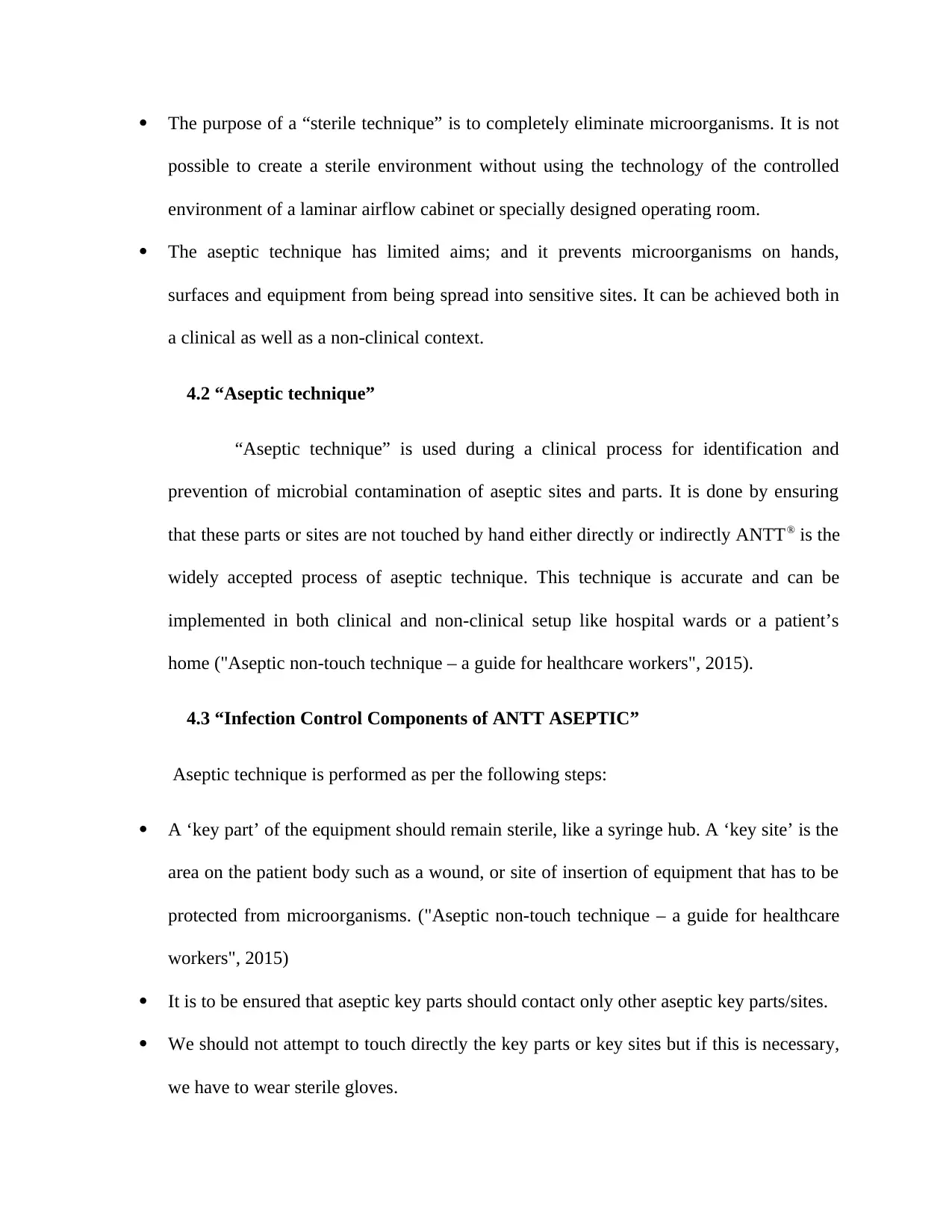
cases where soap and running water are not available readily. Picture 1 shows five
moments of hand hygiene applicable to health care professionals.
We have to use a few drops of liquid soap or antiseptic liquid and have to rub
vigorously both hands together for around fifteen seconds, then the hands are to be rinsed
completely under running water supply and then we have to dry our hands by using a
clean disposable paper napkin. The technique of hand washing may appear to be simple,
but for effectiveness, it must be done properly. People should be informed about this
handwashing technique, for the maintenance of proper hygiene (Blumstein, 2014).
2.1.3 Short-term alternatives to handwashing
There are some places or occasions when running water may not be easily available,
particularly travelling in a car. In such a situation, we have to use alternate effective
solution. Disinfection includes the use of waterless hand sanitizers containing alcohol.
Alcohol is known to be a very effective disinfectant and it evaporates fast. The hand
sanitizers and antimicrobial gels are available in small bottles and can easily be carried
inside our briefcases ("60% Alcohol-Based Hand Sanitizer Found to Be Most Effective", 2019).
This method of handwashing improves the compliance of handwashing, especially in
cases where soap and running water are not available readily. Picture 1 shows five
moments of hand hygiene applicable to health care professionals.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Picture 1 showing 5 moments for hand hygiene for health care workers
2.1.4 Promote hand hygiene
First, we have to analyze the reasons why hand hygiene guidelines are not followed,
particularly regarding hand washing. The reasons generally cited are that people are too
busy with work-load at their place of work and find it inconvenient to wash hands before
any new activity (Barrett & Randle, 2008). This is particularly observed among health
care professionals who should actually follow the guidelines in letter and spirit. Some of
the efforts that may be attempted to improve compliance include appropriate education
on infection control, visual advertisements using different media for promotion of good
hand hygiene, well-located equipment with disinfectants for hand wash and spreading the
message to all via television, radio or social media by the government health
departments. Proper hand hygiene can prevent the transmission of nosocomial infections.
Health care workers should not only wash their hands properly but also guide patients
and their visitors to do the same to continue the infection control process.
2.1.4 Promote hand hygiene
First, we have to analyze the reasons why hand hygiene guidelines are not followed,
particularly regarding hand washing. The reasons generally cited are that people are too
busy with work-load at their place of work and find it inconvenient to wash hands before
any new activity (Barrett & Randle, 2008). This is particularly observed among health
care professionals who should actually follow the guidelines in letter and spirit. Some of
the efforts that may be attempted to improve compliance include appropriate education
on infection control, visual advertisements using different media for promotion of good
hand hygiene, well-located equipment with disinfectants for hand wash and spreading the
message to all via television, radio or social media by the government health
departments. Proper hand hygiene can prevent the transmission of nosocomial infections.
Health care workers should not only wash their hands properly but also guide patients
and their visitors to do the same to continue the infection control process.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Handwashing is not just like a routine activity, it is related to our personal hygiene
and it is one of a most effective way to control the spread of infection from one person to
another. Though it looks simple but is highly effective in controlling the spread of disease
fast. Hands must be washed before and after meals, when they visibly look dirty or
contaminated, after using the toilet, after contact with animals or contact with other
persons by handshaking etc. We should essentially wash or hands after coming back from
a hospital or nursing home.
We have to follow these guidelines if we want to keep ourselves and others
surrounding us fit. We should always remember that if we use gloves it does not
eliminate the need to wash our hands. Hand wash is having different purpose and gloves
are having some other purpose which I am going to discuss in the next patch. Gloves just
protect our hand from direct contact with an object but cannot protect our hands totally
against infection. It is recommended that we should make a habit to wash hands after
finishing any outdoor or indoor activity and before and after our daily meals. Annexure 1
covers SNOB 1.
2.1.5 Analysis on hand hygiene.
Although the hand hygiene procedure is simple, compliance among health care
workers including nurses is so low that it cannot be easily explained or changed. A
number of studies pointed out that this is due to lack of motivation and increased
workload of health care workers for poor compliance. Since they have to guide the
patients to follow this basic and they should prefer to protect themselves to a greater
extent than the patients (Karaaslan et al., 2014).
and it is one of a most effective way to control the spread of infection from one person to
another. Though it looks simple but is highly effective in controlling the spread of disease
fast. Hands must be washed before and after meals, when they visibly look dirty or
contaminated, after using the toilet, after contact with animals or contact with other
persons by handshaking etc. We should essentially wash or hands after coming back from
a hospital or nursing home.
We have to follow these guidelines if we want to keep ourselves and others
surrounding us fit. We should always remember that if we use gloves it does not
eliminate the need to wash our hands. Hand wash is having different purpose and gloves
are having some other purpose which I am going to discuss in the next patch. Gloves just
protect our hand from direct contact with an object but cannot protect our hands totally
against infection. It is recommended that we should make a habit to wash hands after
finishing any outdoor or indoor activity and before and after our daily meals. Annexure 1
covers SNOB 1.
2.1.5 Analysis on hand hygiene.
Although the hand hygiene procedure is simple, compliance among health care
workers including nurses is so low that it cannot be easily explained or changed. A
number of studies pointed out that this is due to lack of motivation and increased
workload of health care workers for poor compliance. Since they have to guide the
patients to follow this basic and they should prefer to protect themselves to a greater
extent than the patients (Karaaslan et al., 2014).
3. PATCH 2: Personal Protective Equipment (PPE)
PPE is special equipment that health care professionals use for personal protection
against germs. This works as a barrier that reduces the risk of touching and exposure of
other body parts like nose, eye etc. against direct contact with infection (Martin, 2017). It
is important for health setup worldwide. Since the application of personal protective
equipment is important, it protects health professionals as well as patients from all types
of hazards in the hospital. It prevents the spread of germs and protects health officials and
patients from an attack of infection in the hospital. It is recommended that all doctors,
nurses, other health workers, patients and their visitors should use PPE to stop spreading
infection.
It consists of a range of clothing and equipment described below.
3.1 Analysis of Personal Protective Equipment
Our hands are protected from germs if we use clinical gloves. It helps to reduce infection
spread. PPE must be always used in situations where there is possible contact with
patient’s blood or other body fluid. Our skin often has microscopic cuts that can endanger
the transmission of infection when it is coming in contact with blood or other infectious
body fluid. That is why it is important to wear gloves when doctors or nurses come in
contact with any bloodborne pathogen or body fluids such as saliva and sperm. Appendix
2 presents the SNOB analysis of PPE.
3.2 Use of clinical gloves
PPE is special equipment that health care professionals use for personal protection
against germs. This works as a barrier that reduces the risk of touching and exposure of
other body parts like nose, eye etc. against direct contact with infection (Martin, 2017). It
is important for health setup worldwide. Since the application of personal protective
equipment is important, it protects health professionals as well as patients from all types
of hazards in the hospital. It prevents the spread of germs and protects health officials and
patients from an attack of infection in the hospital. It is recommended that all doctors,
nurses, other health workers, patients and their visitors should use PPE to stop spreading
infection.
It consists of a range of clothing and equipment described below.
3.1 Analysis of Personal Protective Equipment
Our hands are protected from germs if we use clinical gloves. It helps to reduce infection
spread. PPE must be always used in situations where there is possible contact with
patient’s blood or other body fluid. Our skin often has microscopic cuts that can endanger
the transmission of infection when it is coming in contact with blood or other infectious
body fluid. That is why it is important to wear gloves when doctors or nurses come in
contact with any bloodborne pathogen or body fluids such as saliva and sperm. Appendix
2 presents the SNOB analysis of PPE.
3.2 Use of clinical gloves
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Gloves are generally effective for protection against splashing but do not protect
against penetrating wounds caused by needles or other sharp objects. Should such an
injury occur, we should immediately report it to our supervisor so that prompt action can
be taken to prevent further infection such as HIV / AIDS.
3.3 Masks cover mouth and nose.
Some masks are available with a transparent plastic cover that protects eyes. A
surgical mask stops germs from spreading through nose and mouth. It helps in safe
breathing. A special type of respiratory mask called respirator has a seal around our
mouth and nose. It protects against infection of minute germs like tuberculosis bacteria
through breathing.
3.4 Eye protection with face shield and a special type of goggles.
This protects the mucous membranes of our eyes from coming into contact with
blood and other body fluids.
3.5 Clothing containing aprons, gowns, headgear and shoe covered.
These clothing are used at the time of surgery to protect us and the patient. These
are also used during surgical operation to protect us when we work with body fluids.
Visitors have to wear protective dresses if they visit a patient in an isolation ward because
the disease can be transmitted easily. We may need special EPP to handle certain
anticancer drugs. This equipment is called cytotoxic EPP. This special PPE should be
used during handling of cytotoxic drugs and related waste in health care facilities (NSW,
1995).
against penetrating wounds caused by needles or other sharp objects. Should such an
injury occur, we should immediately report it to our supervisor so that prompt action can
be taken to prevent further infection such as HIV / AIDS.
3.3 Masks cover mouth and nose.
Some masks are available with a transparent plastic cover that protects eyes. A
surgical mask stops germs from spreading through nose and mouth. It helps in safe
breathing. A special type of respiratory mask called respirator has a seal around our
mouth and nose. It protects against infection of minute germs like tuberculosis bacteria
through breathing.
3.4 Eye protection with face shield and a special type of goggles.
This protects the mucous membranes of our eyes from coming into contact with
blood and other body fluids.
3.5 Clothing containing aprons, gowns, headgear and shoe covered.
These clothing are used at the time of surgery to protect us and the patient. These
are also used during surgical operation to protect us when we work with body fluids.
Visitors have to wear protective dresses if they visit a patient in an isolation ward because
the disease can be transmitted easily. We may need special EPP to handle certain
anticancer drugs. This equipment is called cytotoxic EPP. This special PPE should be
used during handling of cytotoxic drugs and related waste in health care facilities (NSW,
1995).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
A particular respirator (not a surgical mask) especially used when handling
cytotoxic drugs. A long-sleeved gown made of waterproof material different from the
normal gown is used. Safety glasses with side shields or glasses, long PVC gloves, made
for special surgical purposes. Should be used. We may also need to wear overshoes.
Other recommendations include spill prevention kits that must be placed in such a way as
to be immediately available for immediate use at all sites. Cytotoxic drugs and wastes
should be handled, stored and transported following safety norms. ("Personal Protective
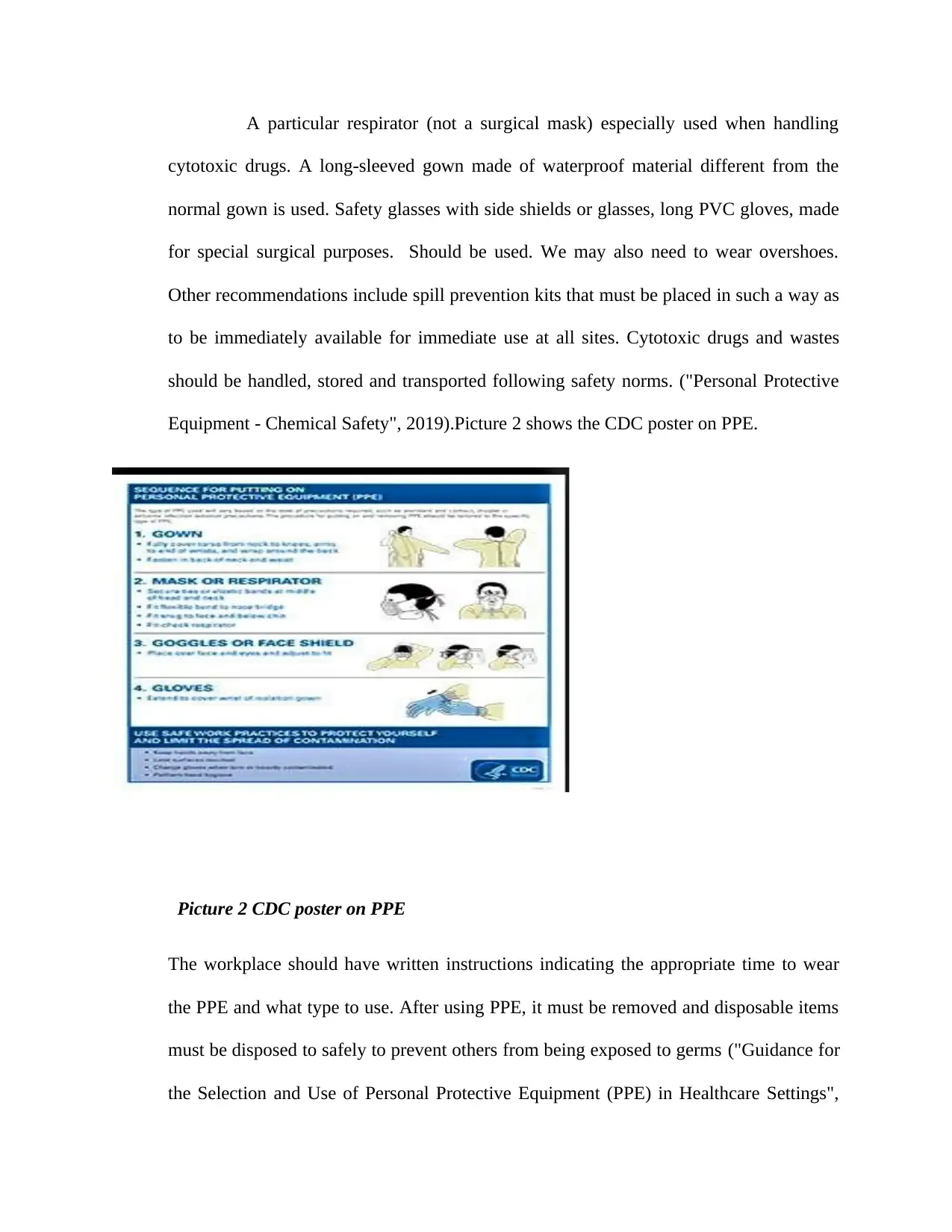
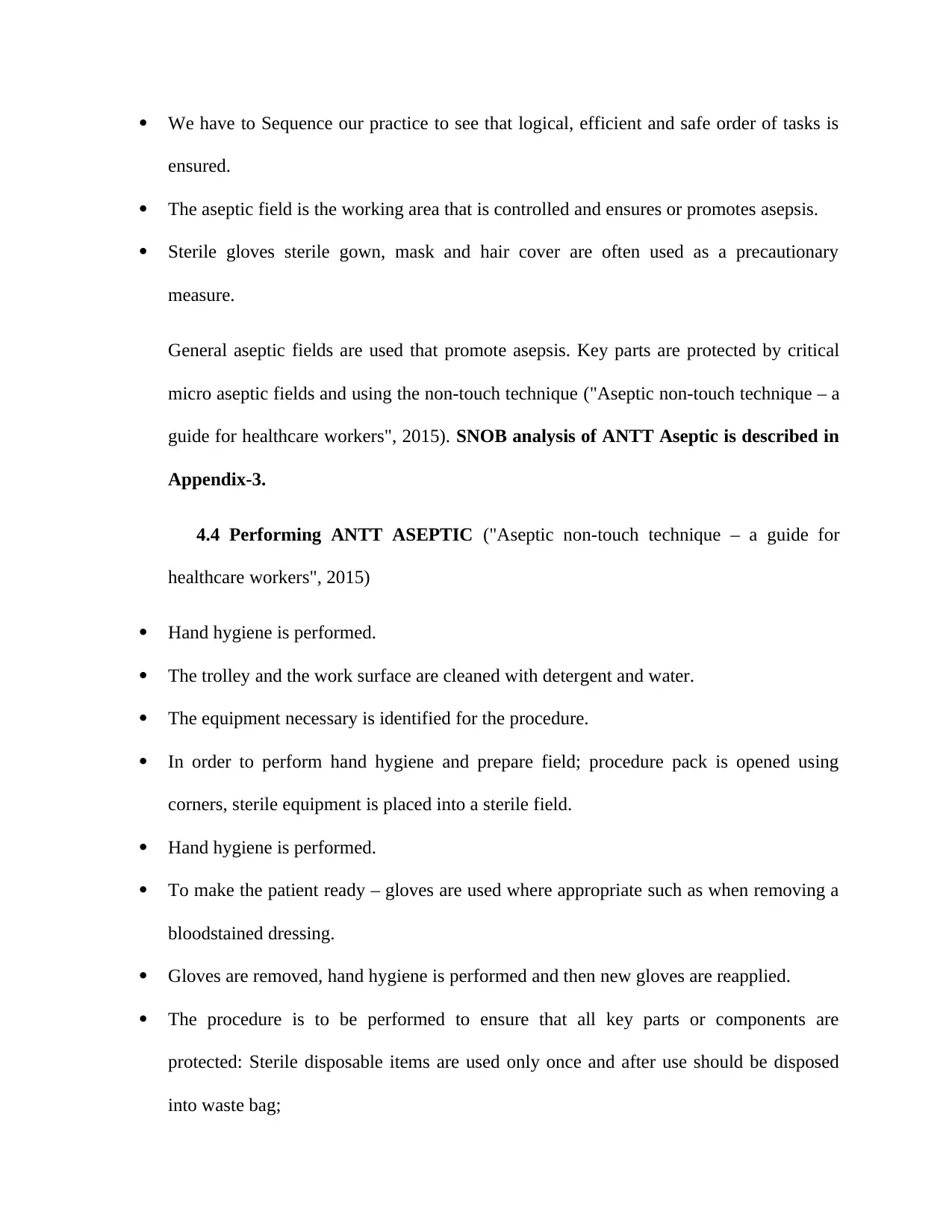
Equipment - Chemical Safety", 2019).Picture 2 shows the CDC poster on PPE.
Picture 2 CDC poster on PPE
The workplace should have written instructions indicating the appropriate time to wear
the PPE and what type to use. After using PPE, it must be removed and disposable items
must be disposed to safely to prevent others from being exposed to germs ("Guidance for
the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings",
cytotoxic drugs. A long-sleeved gown made of waterproof material different from the
normal gown is used. Safety glasses with side shields or glasses, long PVC gloves, made
for special surgical purposes. Should be used. We may also need to wear overshoes.
Other recommendations include spill prevention kits that must be placed in such a way as
to be immediately available for immediate use at all sites. Cytotoxic drugs and wastes
should be handled, stored and transported following safety norms. ("Personal Protective
Equipment - Chemical Safety", 2019).Picture 2 shows the CDC poster on PPE.
Picture 2 CDC poster on PPE
The workplace should have written instructions indicating the appropriate time to wear
the PPE and what type to use. After using PPE, it must be removed and disposable items
must be disposed to safely to prevent others from being exposed to germs ("Guidance for
the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings",
2019). Before leaving our work area, all other personal protective equipment should be
placed in the right place. This may include special laundry bins that can be reused after
cleaning, special waste bins that are different from other waste bins.
4. PATCH 3: “ANTT aseptic non-touch technique”
Analysis of “ANTT Aseptic Non-Touch Technique”
4.1 Key concepts
Aseptic technique is applied in clinical processes for identification and prevention
of microbial contamination of aseptic parts and sites by ensuring that these parts or sites
are not directly or indirectly affected. One of the most common processes of aseptic
technique is known as a non-touch technique (ANTT®).
Asepsis means there is no infectious material or infection. Surgical asepsis means
that there are no microorganisms present in any type of clinical procedure. Sterile
technique is a combination of specific practices and procedures which are performed to
make the equipment and work areas free from any microorganisms and how to maintain
this sterility. Aseptic Non-Touch Technique (ANTT®) is used for the prevention of
infections in most of the healthcare setup. Each organization should develop their own
methodologies for implementation of ANTT® in their setup ("Aseptic Non-Contact
Technique - A Guide for Health Personnel", 2015). Health professionals are using the
terms "sterile technique" and "aseptic technique" interchangeably. However, they are
different techniques.
placed in the right place. This may include special laundry bins that can be reused after
cleaning, special waste bins that are different from other waste bins.
4. PATCH 3: “ANTT aseptic non-touch technique”
Analysis of “ANTT Aseptic Non-Touch Technique”
4.1 Key concepts
Aseptic technique is applied in clinical processes for identification and prevention
of microbial contamination of aseptic parts and sites by ensuring that these parts or sites
are not directly or indirectly affected. One of the most common processes of aseptic
technique is known as a non-touch technique (ANTT®).
Asepsis means there is no infectious material or infection. Surgical asepsis means
that there are no microorganisms present in any type of clinical procedure. Sterile
technique is a combination of specific practices and procedures which are performed to
make the equipment and work areas free from any microorganisms and how to maintain
this sterility. Aseptic Non-Touch Technique (ANTT®) is used for the prevention of
infections in most of the healthcare setup. Each organization should develop their own
methodologies for implementation of ANTT® in their setup ("Aseptic Non-Contact
Technique - A Guide for Health Personnel", 2015). Health professionals are using the
terms "sterile technique" and "aseptic technique" interchangeably. However, they are
different techniques.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The purpose of a “sterile technique” is to completely eliminate microorganisms. It is not
possible to create a sterile environment without using the technology of the controlled
environment of a laminar airflow cabinet or specially designed operating room.
The aseptic technique has limited aims; and it prevents microorganisms on hands,
surfaces and equipment from being spread into sensitive sites. It can be achieved both in
a clinical as well as a non-clinical context.
4.2 “Aseptic technique”
“Aseptic technique” is used during a clinical process for identification and
prevention of microbial contamination of aseptic sites and parts. It is done by ensuring
that these parts or sites are not touched by hand either directly or indirectly ANTT® is the
widely accepted process of aseptic technique. This technique is accurate and can be
implemented in both clinical and non-clinical setup like hospital wards or a patient’s
home ("Aseptic non-touch technique – a guide for healthcare workers", 2015).
4.3 “Infection Control Components of ANTT ASEPTIC”
Aseptic technique is performed as per the following steps:
A ‘key part’ of the equipment should remain sterile, like a syringe hub. A ‘key site’ is the
area on the patient body such as a wound, or site of insertion of equipment that has to be
protected from microorganisms. ("Aseptic non-touch technique – a guide for healthcare
workers", 2015)
It is to be ensured that aseptic key parts should contact only other aseptic key parts/sites.
We should not attempt to touch directly the key parts or key sites but if this is necessary,
we have to wear sterile gloves.
possible to create a sterile environment without using the technology of the controlled
environment of a laminar airflow cabinet or specially designed operating room.
The aseptic technique has limited aims; and it prevents microorganisms on hands,
surfaces and equipment from being spread into sensitive sites. It can be achieved both in
a clinical as well as a non-clinical context.
4.2 “Aseptic technique”
“Aseptic technique” is used during a clinical process for identification and
prevention of microbial contamination of aseptic sites and parts. It is done by ensuring
that these parts or sites are not touched by hand either directly or indirectly ANTT® is the
widely accepted process of aseptic technique. This technique is accurate and can be
implemented in both clinical and non-clinical setup like hospital wards or a patient’s
home ("Aseptic non-touch technique – a guide for healthcare workers", 2015).
4.3 “Infection Control Components of ANTT ASEPTIC”
Aseptic technique is performed as per the following steps:
A ‘key part’ of the equipment should remain sterile, like a syringe hub. A ‘key site’ is the
area on the patient body such as a wound, or site of insertion of equipment that has to be
protected from microorganisms. ("Aseptic non-touch technique – a guide for healthcare
workers", 2015)
It is to be ensured that aseptic key parts should contact only other aseptic key parts/sites.
We should not attempt to touch directly the key parts or key sites but if this is necessary,
we have to wear sterile gloves.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
We have to Sequence our practice to see that logical, efficient and safe order of tasks is
ensured.
The aseptic field is the working area that is controlled and ensures or promotes asepsis.
Sterile gloves sterile gown, mask and hair cover are often used as a precautionary
measure.
General aseptic fields are used that promote asepsis. Key parts are protected by critical
micro aseptic fields and using the non-touch technique ("Aseptic non-touch technique – a
guide for healthcare workers", 2015). SNOB analysis of ANTT Aseptic is described in
Appendix-3.
4.4 Performing ANTT ASEPTIC ("Aseptic non-touch technique – a guide for
healthcare workers", 2015)
Hand hygiene is performed.
The trolley and the work surface are cleaned with detergent and water.
The equipment necessary is identified for the procedure.
In order to perform hand hygiene and prepare field; procedure pack is opened using
corners, sterile equipment is placed into a sterile field.
Hand hygiene is performed.
To make the patient ready – gloves are used where appropriate such as when removing a
bloodstained dressing.
Gloves are removed, hand hygiene is performed and then new gloves are reapplied.
The procedure is to be performed to ensure that all key parts or components are
protected: Sterile disposable items are used only once and after use should be disposed
into waste bag;
ensured.
The aseptic field is the working area that is controlled and ensures or promotes asepsis.
Sterile gloves sterile gown, mask and hair cover are often used as a precautionary
measure.
General aseptic fields are used that promote asepsis. Key parts are protected by critical
micro aseptic fields and using the non-touch technique ("Aseptic non-touch technique – a
guide for healthcare workers", 2015). SNOB analysis of ANTT Aseptic is described in
Appendix-3.
4.4 Performing ANTT ASEPTIC ("Aseptic non-touch technique – a guide for
healthcare workers", 2015)
Hand hygiene is performed.
The trolley and the work surface are cleaned with detergent and water.
The equipment necessary is identified for the procedure.
In order to perform hand hygiene and prepare field; procedure pack is opened using
corners, sterile equipment is placed into a sterile field.
Hand hygiene is performed.
To make the patient ready – gloves are used where appropriate such as when removing a
bloodstained dressing.
Gloves are removed, hand hygiene is performed and then new gloves are reapplied.
The procedure is to be performed to ensure that all key parts or components are
protected: Sterile disposable items are used only once and after use should be disposed
into waste bag;
The gloves are to be taken off and hand hygiene routine is performed.
The trolley, as well as floor, tables and other furniture near him, are to be cleaned after
use and hand hygiene is to be performed.
5. PATCH 4: Isolation of patients to individual rooms from ward
5.1 Analysis of patient isolation
Isolation is a precautionary measure in a hospital set-up to prevent the spread of
infectious disease. Infection easily spreads at hospitals and it is a risk element for staffs,
patients and visitors. Special precautions should be taken to prevent the transmission of
infections (e.g. infectious diarrhoea, MRSA, tuberculosis and chicken pox) ("Patient
Information Factsheet", 2016). So, if a person is infected, it may be necessary to treat him
separately from other patients. Isolation will continue until there is no risk that the
infection will be transmitted to others ("Patient Information Factsheet", 2016). SNOB
analysis of Isolation of patients is explained in Appendix-4.
5.2 Patients who are isolated
The person is believed to have an infection that can communicate with other patients or
staff.
He needs protection against infection because he has weak immunity or is taking certain
medications. This is called "protective isolation" ("Patient Information Factsheet", 2016).
The trolley, as well as floor, tables and other furniture near him, are to be cleaned after
use and hand hygiene is to be performed.
5. PATCH 4: Isolation of patients to individual rooms from ward
5.1 Analysis of patient isolation
Isolation is a precautionary measure in a hospital set-up to prevent the spread of
infectious disease. Infection easily spreads at hospitals and it is a risk element for staffs,
patients and visitors. Special precautions should be taken to prevent the transmission of
infections (e.g. infectious diarrhoea, MRSA, tuberculosis and chicken pox) ("Patient
Information Factsheet", 2016). So, if a person is infected, it may be necessary to treat him
separately from other patients. Isolation will continue until there is no risk that the
infection will be transmitted to others ("Patient Information Factsheet", 2016). SNOB
analysis of Isolation of patients is explained in Appendix-4.
5.2 Patients who are isolated
The person is believed to have an infection that can communicate with other patients or
staff.
He needs protection against infection because he has weak immunity or is taking certain
medications. This is called "protective isolation" ("Patient Information Factsheet", 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





