Microbiology: Investigating Why Eradication of Diseases is a Challenge
VerifiedAdded on 2023/06/10
|21
|5810
|447
Essay
AI Summary
This essay discusses the difficulties in eradicating infectious diseases, focusing on bacterial virulence factors such as adherence mechanisms (fimbriae, Pilli) and toxins. It examines the role of antibiotics in disease prevention and the subsequent development of multi-drug resistance (MDR), along with the impact of biofilm production as a barrier to antibiotics. The essay also addresses the role of microflora in immunocompromised individuals and the roots of infection spread. Furthermore, it explores anti-immune strategies employed by bacteria, including surface modulation, antigenic hypervariability, and interference with TLRs. Finally, the essay touches on potential strategies for combating bacterial infections, such as quorum sensing inhibitors and optimized antibiotic usage, highlighting the complexities in achieving complete eradication. Desklib provides access to similar essays and study tools for students.

Running head: MICROBIOLOGY
Why We Can Never Eradicate Infectious Disease
Name of the Student
Name of the University
Author Note
Why We Can Never Eradicate Infectious Disease
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICROBIOLOGY
Introduction
Infectious disease arising out of bacteria can be transmitted from animals to people
and from one person to another person. These infections can be mild to severe and can
eventually lead to the development of serious illness that if left out may lead to life
threatening diseases (Nelson and Williams 2013). According to the reports published by the
Parliamentary Office of Science and Technology in UK (2017), infectious diseases cause
significant economic and health burden in UK which accounts to about 7% of death and with
an annual cost of £30bn. However, even under the presence of broad spectrum and third or
fourth generation antibiotics and presence of advanced quality molecular detection
technology, the overall eradication of the microbial diseases in UK and both globally is not
very promising. The following essay is mainly based on argument that why there is a
difficulty in eradicating the infections and life threatening diseases from UK or rather says
globally. In doing so, the essay will mainly explore the mechanism of bacterial adherence
and colonization within the host cell via the use of cell adhesion molecule, fimbriae or Pilli.
The essay also aims to throw light on the effects of bacterial toxins in disease propagation
and difficulty in prevention. In order to critically analyse the opinion and come to a
conclusion, the essay will also discuss the importance of antibiotics and is relation to disease
prevention and subsequent generation of multi-drug resistance gene (MDR) along with the
overall concept of biofilm production and its barrier towards antibiotics. The essay will also
discuss the role of microflora and its effect on immune-compromised people and roots behind
spread of infection. At the end essay will try to recommend the possible ways that are
showing promising results in the eradication of the bacterial infections.
Introduction
Infectious disease arising out of bacteria can be transmitted from animals to people
and from one person to another person. These infections can be mild to severe and can
eventually lead to the development of serious illness that if left out may lead to life
threatening diseases (Nelson and Williams 2013). According to the reports published by the
Parliamentary Office of Science and Technology in UK (2017), infectious diseases cause
significant economic and health burden in UK which accounts to about 7% of death and with
an annual cost of £30bn. However, even under the presence of broad spectrum and third or
fourth generation antibiotics and presence of advanced quality molecular detection
technology, the overall eradication of the microbial diseases in UK and both globally is not
very promising. The following essay is mainly based on argument that why there is a
difficulty in eradicating the infections and life threatening diseases from UK or rather says
globally. In doing so, the essay will mainly explore the mechanism of bacterial adherence
and colonization within the host cell via the use of cell adhesion molecule, fimbriae or Pilli.
The essay also aims to throw light on the effects of bacterial toxins in disease propagation
and difficulty in prevention. In order to critically analyse the opinion and come to a
conclusion, the essay will also discuss the importance of antibiotics and is relation to disease
prevention and subsequent generation of multi-drug resistance gene (MDR) along with the
overall concept of biofilm production and its barrier towards antibiotics. The essay will also
discuss the role of microflora and its effect on immune-compromised people and roots behind
spread of infection. At the end essay will try to recommend the possible ways that are
showing promising results in the eradication of the bacterial infections.
MICROBIOLOGY
The virulent factors
The capability of the bacteria to cause disease reflects the relative pathogenicity.
Virulence is the measure of the pathogenicity of the virus. The degree of the virulence is
linked to the ability of the organism for causing diseases in spite of the host resistance
mechanism of the body. The factors that are produced by the microorganism and disease are
called the virulence factors, such as the toxins and the surface coats that inhibit the
phagocytosis and the surface receptors binding to the host cells.
In order to cause infection, the bacteria should adhere to the mucosal surface. For
example, the mucosa of the alimentary tract is repeatedly cleaned by the mucus secreted by
the goblet cells and by the peristaltic movement of the gut content over the epithelium. In
order to establish infection in such a site, the bacteria have to adhere to the mucosal surface.
For accomplishing this, bacteria have evolved certain mechanism such as fimbriae that
recognize and help in attachment of the bacteria (Haiko and Westerlund-Wikström 2013).
The colonization factors of the bacteria play an important role in the pathogenic mechanism
of the bacteria.
The external surface of bacteria acts as the central interface between the pathogen and
the host and recognition of the exposed surface by the immune system provided by the host a
key sign for the microbial clearance (Haiko and Westerlund-Wikström 2013). A study by
Olsen et al. (2013) have shown that the flagellum of a bacteria influences the virulence by
facilitating movement. There are early studies that have shown that the single polar flagellum
of Vibrio cholera is crucial for its virulence. Again V. Cholera that is not motile cannot
induced virulence. Recently, Olsen and colleagues have proved the involvement of the
serovar specific differences of the chemotaxis genes and flagella in the adhesion of the
Salmonella. It also provides the pathogen to mimic the immune modulators of the host, in
order to modify the immune responses of the host or to express receptor ligands or adhesions
The virulent factors
The capability of the bacteria to cause disease reflects the relative pathogenicity.
Virulence is the measure of the pathogenicity of the virus. The degree of the virulence is
linked to the ability of the organism for causing diseases in spite of the host resistance
mechanism of the body. The factors that are produced by the microorganism and disease are
called the virulence factors, such as the toxins and the surface coats that inhibit the
phagocytosis and the surface receptors binding to the host cells.
In order to cause infection, the bacteria should adhere to the mucosal surface. For
example, the mucosa of the alimentary tract is repeatedly cleaned by the mucus secreted by
the goblet cells and by the peristaltic movement of the gut content over the epithelium. In
order to establish infection in such a site, the bacteria have to adhere to the mucosal surface.
For accomplishing this, bacteria have evolved certain mechanism such as fimbriae that
recognize and help in attachment of the bacteria (Haiko and Westerlund-Wikström 2013).
The colonization factors of the bacteria play an important role in the pathogenic mechanism
of the bacteria.
The external surface of bacteria acts as the central interface between the pathogen and
the host and recognition of the exposed surface by the immune system provided by the host a
key sign for the microbial clearance (Haiko and Westerlund-Wikström 2013). A study by
Olsen et al. (2013) have shown that the flagellum of a bacteria influences the virulence by
facilitating movement. There are early studies that have shown that the single polar flagellum
of Vibrio cholera is crucial for its virulence. Again V. Cholera that is not motile cannot
induced virulence. Recently, Olsen and colleagues have proved the involvement of the
serovar specific differences of the chemotaxis genes and flagella in the adhesion of the
Salmonella. It also provides the pathogen to mimic the immune modulators of the host, in
order to modify the immune responses of the host or to express receptor ligands or adhesions
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MICROBIOLOGY
for anchoring to the host surfaces (Haiko and Westerlund-Wikström 2013). Supporting this
findings, Girón and colleagues that some of the wild type strains of E. Coli expressing the H2
or H6 flagella can adhere and form micro-colonies to the HeLa cells.
Other surface molecules like the protective capsules can increase the survival of the
pathogen within the host (Willey et al. 2008). A common mechanism to mask the complex
antigenic surface from spotting by the immune surveillance is the expression of a
carbohydrate capsule. For example Streptococcus pneumonia, uses its capsule to prevent the
deposition of the complement and antibody on its surface, thereby preventing clearance by
phagocytosis or opsonisation (Finlay and McFadden 2006). The lipid A component of the
Lipopolysaccharide (LPS), present in the Gram negative bacteria, plays a crucial role in the
activation of the TLR. However the outer part of the LPS consists of variable forms of
carbohydrates providing each of the strain with their unique serotype (O antigen). Thus
different strains can infect the same host due to different surface antigens (Finlay and
McFadden 2006). There are certain gram negative bacteria that alter the lipid A for altering
the TLR4 response. For Example, There are two component sensors present in Salmonella;
(PhoP/PhoQ) that can sense the host environment regulating many genes. Modification of the
lipid A makes it much less active for TLR4 activation (Prescott and Harley 1994).
The bacterial pathogens have developed special secretion system for exporting the
virulence factors across the bacterial membranes. Virulence factors such as the toxins or the
immune modulators are secreted in to the host cells. Both the type III secretion systems
(T3SS) and type IV secretion systems (T4SS), can introduce, various virulence factors in to the
host cells. These two types of secretion system possess very diverse repertoire of the effector
molecules that can be delivered in to the host cells, paralyzing the phagocytosis and altering
other immune functions (Finlay and McFadden 2006). Although the structures of the gram
positive bacteria are much simpler, they can also generate specialized pores for delivering the
for anchoring to the host surfaces (Haiko and Westerlund-Wikström 2013). Supporting this
findings, Girón and colleagues that some of the wild type strains of E. Coli expressing the H2
or H6 flagella can adhere and form micro-colonies to the HeLa cells.
Other surface molecules like the protective capsules can increase the survival of the
pathogen within the host (Willey et al. 2008). A common mechanism to mask the complex
antigenic surface from spotting by the immune surveillance is the expression of a
carbohydrate capsule. For example Streptococcus pneumonia, uses its capsule to prevent the
deposition of the complement and antibody on its surface, thereby preventing clearance by
phagocytosis or opsonisation (Finlay and McFadden 2006). The lipid A component of the
Lipopolysaccharide (LPS), present in the Gram negative bacteria, plays a crucial role in the
activation of the TLR. However the outer part of the LPS consists of variable forms of
carbohydrates providing each of the strain with their unique serotype (O antigen). Thus
different strains can infect the same host due to different surface antigens (Finlay and
McFadden 2006). There are certain gram negative bacteria that alter the lipid A for altering
the TLR4 response. For Example, There are two component sensors present in Salmonella;
(PhoP/PhoQ) that can sense the host environment regulating many genes. Modification of the
lipid A makes it much less active for TLR4 activation (Prescott and Harley 1994).
The bacterial pathogens have developed special secretion system for exporting the
virulence factors across the bacterial membranes. Virulence factors such as the toxins or the
immune modulators are secreted in to the host cells. Both the type III secretion systems
(T3SS) and type IV secretion systems (T4SS), can introduce, various virulence factors in to the
host cells. These two types of secretion system possess very diverse repertoire of the effector
molecules that can be delivered in to the host cells, paralyzing the phagocytosis and altering
other immune functions (Finlay and McFadden 2006). Although the structures of the gram
positive bacteria are much simpler, they can also generate specialized pores for delivering the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICROBIOLOGY
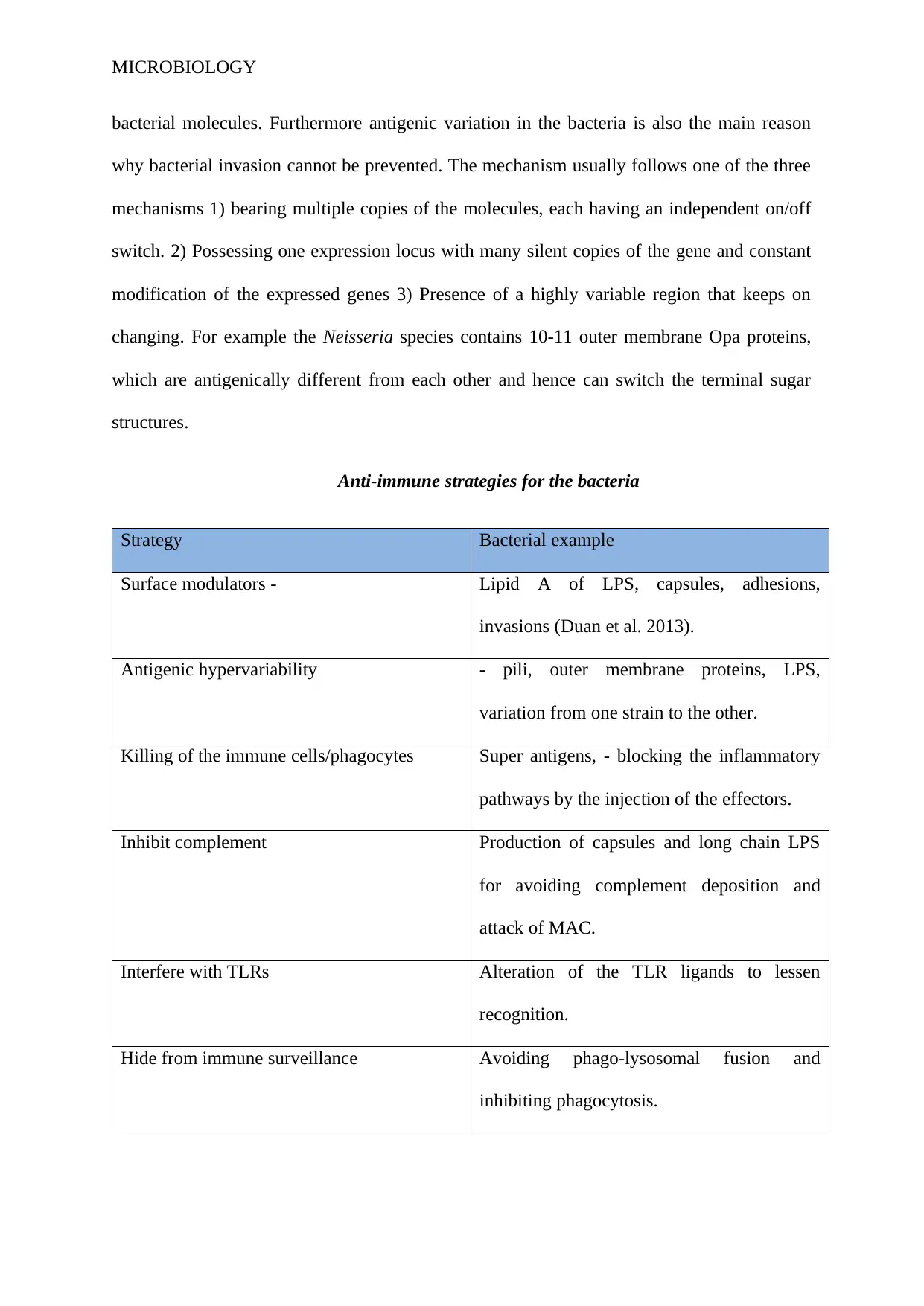
bacterial molecules. Furthermore antigenic variation in the bacteria is also the main reason
why bacterial invasion cannot be prevented. The mechanism usually follows one of the three
mechanisms 1) bearing multiple copies of the molecules, each having an independent on/off
switch. 2) Possessing one expression locus with many silent copies of the gene and constant
modification of the expressed genes 3) Presence of a highly variable region that keeps on
changing. For example the Neisseria species contains 10-11 outer membrane Opa proteins,
which are antigenically different from each other and hence can switch the terminal sugar
structures.
Anti-immune strategies for the bacteria
Strategy Bacterial example
Surface modulators - Lipid A of LPS, capsules, adhesions,
invasions (Duan et al. 2013).
Antigenic hypervariability - pili, outer membrane proteins, LPS,
variation from one strain to the other.
Killing of the immune cells/phagocytes Super antigens, - blocking the inflammatory
pathways by the injection of the effectors.
Inhibit complement Production of capsules and long chain LPS
for avoiding complement deposition and
attack of MAC.
Interfere with TLRs Alteration of the TLR ligands to lessen
recognition.
Hide from immune surveillance Avoiding phago-lysosomal fusion and
inhibiting phagocytosis.
bacterial molecules. Furthermore antigenic variation in the bacteria is also the main reason
why bacterial invasion cannot be prevented. The mechanism usually follows one of the three
mechanisms 1) bearing multiple copies of the molecules, each having an independent on/off
switch. 2) Possessing one expression locus with many silent copies of the gene and constant
modification of the expressed genes 3) Presence of a highly variable region that keeps on
changing. For example the Neisseria species contains 10-11 outer membrane Opa proteins,
which are antigenically different from each other and hence can switch the terminal sugar
structures.
Anti-immune strategies for the bacteria
Strategy Bacterial example
Surface modulators - Lipid A of LPS, capsules, adhesions,
invasions (Duan et al. 2013).
Antigenic hypervariability - pili, outer membrane proteins, LPS,
variation from one strain to the other.
Killing of the immune cells/phagocytes Super antigens, - blocking the inflammatory
pathways by the injection of the effectors.
Inhibit complement Production of capsules and long chain LPS
for avoiding complement deposition and
attack of MAC.
Interfere with TLRs Alteration of the TLR ligands to lessen
recognition.
Hide from immune surveillance Avoiding phago-lysosomal fusion and
inhibiting phagocytosis.
MICROBIOLOGY
Bio-films and its relation to spread of infection
Bio-films and the spread of nocosomial infection
Multidrug-resistant (MDR) organisms like Methicillin-resistant Staphylococcus
aureus (MRSA), Acinetobacter baumanni and extended spectrum beta lactum producing
gram-negative bacteria are frequently highlighted as the main causative agent behind the
acute and chronic infectious diseases which lead to the generation of significant mortality and
morbidity along with overall increase in the health care cost (McGrath and Asmar 2011). Till
date various studies have indicated that the human infections are mainly caused by the ability
of the bacteria to develop surface attached polymicrobial communities which are popularly
known as biofilms (Sánchez et al. 2013). According to Flemming et al. (2016), microbial
biofilms are made of a groups of bacterial cells which are adherent to the surface and are
enclosed with in a self-produced extracellular matrix. Adaptation to the surface attached
growth within a biofilm is accompanied via a significant change in the protein and gene
expression along with the overall microbial activity. Numerous pathogenic and nosocomial
bacteria have been observed to exist predominantly as biofilms under both natural
environment and under infected tissues as polymicrobial communities. Notably, the
formation of biofilms is implicated as one of the significant factors behind the increased
number of the chronic bacterial infections (Sánchez et al. 2013).
The randomised control trial (RCT) conducted by Sánchez et al. (2013) from the
clinical isolated of the patients suffering from bacterial infection, highlighted that the
formation of biofilms increases the tendency of recurrent bacterial infection. Their RCT
showed that MDR pathogens are more prone towards the formation of biofilms and the
strains from the patients with persistent bacterial infection generated positive results in
biofilm formation. The systematic review conducted by Bjarnsholt (2013) showed that the
biofilm infections like the pneumonia in cystic fibrosis patients, chronic otitis media, chronic
Bio-films and its relation to spread of infection
Bio-films and the spread of nocosomial infection
Multidrug-resistant (MDR) organisms like Methicillin-resistant Staphylococcus
aureus (MRSA), Acinetobacter baumanni and extended spectrum beta lactum producing
gram-negative bacteria are frequently highlighted as the main causative agent behind the
acute and chronic infectious diseases which lead to the generation of significant mortality and
morbidity along with overall increase in the health care cost (McGrath and Asmar 2011). Till
date various studies have indicated that the human infections are mainly caused by the ability
of the bacteria to develop surface attached polymicrobial communities which are popularly
known as biofilms (Sánchez et al. 2013). According to Flemming et al. (2016), microbial
biofilms are made of a groups of bacterial cells which are adherent to the surface and are
enclosed with in a self-produced extracellular matrix. Adaptation to the surface attached
growth within a biofilm is accompanied via a significant change in the protein and gene
expression along with the overall microbial activity. Numerous pathogenic and nosocomial
bacteria have been observed to exist predominantly as biofilms under both natural
environment and under infected tissues as polymicrobial communities. Notably, the
formation of biofilms is implicated as one of the significant factors behind the increased
number of the chronic bacterial infections (Sánchez et al. 2013).
The randomised control trial (RCT) conducted by Sánchez et al. (2013) from the
clinical isolated of the patients suffering from bacterial infection, highlighted that the
formation of biofilms increases the tendency of recurrent bacterial infection. Their RCT
showed that MDR pathogens are more prone towards the formation of biofilms and the
strains from the patients with persistent bacterial infection generated positive results in
biofilm formation. The systematic review conducted by Bjarnsholt (2013) showed that the
biofilm infections like the pneumonia in cystic fibrosis patients, chronic otitis media, chronic
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MICROBIOLOGY
wounds and other catheter or implant associated infections affects millions of people both the
developed and developing countries each year and numerous death toll occurs due to this. In
general, it can be said that the bacteria has two types of life forms during their growth and
proliferation stage. In one life form, bacteria exist, as single cell aggregates (planktonic)
whereas in other life forms, bacteria are organized into sessile aggregates. This aggregate
form is commonly referred to as bioflim, which increases the rate of nocosomial infections
(Bjarnsholt 2013). For example, lung infection is the principal cause of mortality and
mortality among the patients of cystic fibrosis and this mostly dominated by Pseudomonas
aeruginosa. The growth of biofilm makes the eradication of infection impossible and thereby
leading to chronic inflammation in the airways that ultimately leads to death (Ciofu et al.
2015). In relation to this Olsen (2015) highlighted that biofilms can be difficult to eradicate
when they lead to the generation of the biofilm-related diseases like the cystic fibrosis,
implant infections, periodontal diseases and urinary tract infections. A number of phenotypic
features associated with the biofilms leads to the generation of the biofilm-specific resistance
and tolerance however, the exact molecular mechanisms involved in the process of
generation of antibiotic tolerance is still not known. However, de la Fuente-Núñez et al.
(2013) is of the opinion that the antibiotic resistance conferred by the biofilms to the bacterial
colony is mainly due to the ability of the biofilm to survive in the hostile environment. de la
Fuente-Núñez et al. (2013) stated that under the clinical settings, bacteria are exposure to
several adverse condition like stress, nutrient limitations, heat shock and anaerobiosis. This
adverse condition lead to the generation of adaptive responses in the bacterial cells, which in
turn leads to the development of highly resistant multicellular structures that are recalcitrant
to the host immune clearance system and at the same time are extremely difficult to eradicate
through the administration of antibiotics.
wounds and other catheter or implant associated infections affects millions of people both the
developed and developing countries each year and numerous death toll occurs due to this. In
general, it can be said that the bacteria has two types of life forms during their growth and
proliferation stage. In one life form, bacteria exist, as single cell aggregates (planktonic)
whereas in other life forms, bacteria are organized into sessile aggregates. This aggregate
form is commonly referred to as bioflim, which increases the rate of nocosomial infections
(Bjarnsholt 2013). For example, lung infection is the principal cause of mortality and
mortality among the patients of cystic fibrosis and this mostly dominated by Pseudomonas
aeruginosa. The growth of biofilm makes the eradication of infection impossible and thereby
leading to chronic inflammation in the airways that ultimately leads to death (Ciofu et al.
2015). In relation to this Olsen (2015) highlighted that biofilms can be difficult to eradicate
when they lead to the generation of the biofilm-related diseases like the cystic fibrosis,
implant infections, periodontal diseases and urinary tract infections. A number of phenotypic
features associated with the biofilms leads to the generation of the biofilm-specific resistance
and tolerance however, the exact molecular mechanisms involved in the process of
generation of antibiotic tolerance is still not known. However, de la Fuente-Núñez et al.
(2013) is of the opinion that the antibiotic resistance conferred by the biofilms to the bacterial
colony is mainly due to the ability of the biofilm to survive in the hostile environment. de la
Fuente-Núñez et al. (2013) stated that under the clinical settings, bacteria are exposure to
several adverse condition like stress, nutrient limitations, heat shock and anaerobiosis. This
adverse condition lead to the generation of adaptive responses in the bacterial cells, which in
turn leads to the development of highly resistant multicellular structures that are recalcitrant
to the host immune clearance system and at the same time are extremely difficult to eradicate
through the administration of antibiotics.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICROBIOLOGY
Ciofu et al. (2015) is of the opinion that the weakening of the bioflims through
quorum sensing inhibitors and antibiotic guided killing through pharmacokinetics and
pharmacodynamics of antibiotics are frequently suggested as remedies to prevent the
colonization of biofilms. In the domain of quorum sensing, O’Loughlin et al. (2013)
highlighted that the quorum-sensing inhibitor blocks Pseudomonas aeruginosa virulence
factor and biofilm formation. The synthetic molecule, meta-bromo-thiolactone not only
prevents virulence expression of Pseudomonas but at the same time prevents biofilm
formation.
In spite of having quorum sensing as an important factor behind the inhibition of the
bacterial, the fast colonization and spread of infection of bacteria further increases the
susceptibility of the bacterial infection. The research conducted by Los et al. (2013)
highlighted that the pore-forming toxins (PFTs) are the most common virulence factor in a
wide range of bacterial pathogen including Streptococcus pneumonia, Mycobacterium
tuberculosis, and Escherichia coli. This PFT rapidly disrupt the host cell membrane and
thereby entering into the host cell via the pore. Once inside the host cell, the toxin takes the
control of the host pathways and thereby causing cellular damage and increasing the
chronicity of infection.
Infections caused in the immune-compromised patients by the normal microbiota
The fact that disease can never be irradiated can be supported by the fact that,
although normal micro flora is harmless, but very few can actually cause diseases in immune-
compromised host. Since a diverse community of microorganisms resides in the intestine of
the human (Taur and Pamer 2013). The host intestinal tract possess a local immune system
for controlling the microbial flora. This includes the gut associated dendritic cells, B-cells
and T- cells and Peyer’s patches, in order to prevent the entry of the microorganisms in the
Ciofu et al. (2015) is of the opinion that the weakening of the bioflims through
quorum sensing inhibitors and antibiotic guided killing through pharmacokinetics and
pharmacodynamics of antibiotics are frequently suggested as remedies to prevent the
colonization of biofilms. In the domain of quorum sensing, O’Loughlin et al. (2013)
highlighted that the quorum-sensing inhibitor blocks Pseudomonas aeruginosa virulence
factor and biofilm formation. The synthetic molecule, meta-bromo-thiolactone not only
prevents virulence expression of Pseudomonas but at the same time prevents biofilm
formation.
In spite of having quorum sensing as an important factor behind the inhibition of the
bacterial, the fast colonization and spread of infection of bacteria further increases the
susceptibility of the bacterial infection. The research conducted by Los et al. (2013)
highlighted that the pore-forming toxins (PFTs) are the most common virulence factor in a
wide range of bacterial pathogen including Streptococcus pneumonia, Mycobacterium
tuberculosis, and Escherichia coli. This PFT rapidly disrupt the host cell membrane and
thereby entering into the host cell via the pore. Once inside the host cell, the toxin takes the
control of the host pathways and thereby causing cellular damage and increasing the
chronicity of infection.
Infections caused in the immune-compromised patients by the normal microbiota
The fact that disease can never be irradiated can be supported by the fact that,
although normal micro flora is harmless, but very few can actually cause diseases in immune-
compromised host. Since a diverse community of microorganisms resides in the intestine of
the human (Taur and Pamer 2013). The host intestinal tract possess a local immune system
for controlling the microbial flora. This includes the gut associated dendritic cells, B-cells
and T- cells and Peyer’s patches, in order to prevent the entry of the microorganisms in the
MICROBIOLOGY
tissues. The goblet cells produces the mucus that prevents the penetration of the bacteria
(Steele 2012). According to Taur and Pamer (2013) patients suffer from systemic bacterial
infection after being treated with cytotoxic chemotherapy. The chemotherapic regimens for
the cancer patients that are meant for inhibiting the replication of the tumour can be harmful
for the elements in the bone marrow, including the white blood cells that are immune-
competent. Even the patient’s keep under extraordinary support system have much greater
risk of colonization with multi-resistant microorganisms. As per the evidences, the digestive
tract can become portals of entry for the human pathogens even when there are no mucosal
barriers. Bacterial translocation by a specialized absorptive cells known as the M cells, are
the part of the antigen sampling process leading to the development of the gut associated
lymphoid tissue (Johansson and Rasmussen 2013). Taur and Pamer, (2013) have postulated
that after passing through the intestinal layer, the bacteria id phagocytised by the motile
phagocytes, by which they are transported to the extra-intestinal sites. Facultative anaerobes
like Salmonella spp. and Listeria spp. Can translocate out of the intestinal tract and this is
found mainly in the patient with disrupted T-cell function or those suffering from
Lymphoma, AIDS or organ transplant.
The burden of the Clostridium difficile infection (CDI), has augmented in terms of
morbidity, incidence, cost and mortality and is one of the commonest cause of the infections
(Janoir 2016). Di Bella et al. (2015) have stated that in comparison to specific categories of
immunosuppression, the HIV infected patients are likely to develop CDI in comparison to the
other hospitalized patients. In a nationwide study conducted in USA, the solid organ
transplant has been found to be an independent predictor of the hospital mortality, colectomy
and graft complications.
tissues. The goblet cells produces the mucus that prevents the penetration of the bacteria
(Steele 2012). According to Taur and Pamer (2013) patients suffer from systemic bacterial
infection after being treated with cytotoxic chemotherapy. The chemotherapic regimens for
the cancer patients that are meant for inhibiting the replication of the tumour can be harmful
for the elements in the bone marrow, including the white blood cells that are immune-
competent. Even the patient’s keep under extraordinary support system have much greater
risk of colonization with multi-resistant microorganisms. As per the evidences, the digestive
tract can become portals of entry for the human pathogens even when there are no mucosal
barriers. Bacterial translocation by a specialized absorptive cells known as the M cells, are
the part of the antigen sampling process leading to the development of the gut associated
lymphoid tissue (Johansson and Rasmussen 2013). Taur and Pamer, (2013) have postulated
that after passing through the intestinal layer, the bacteria id phagocytised by the motile
phagocytes, by which they are transported to the extra-intestinal sites. Facultative anaerobes
like Salmonella spp. and Listeria spp. Can translocate out of the intestinal tract and this is
found mainly in the patient with disrupted T-cell function or those suffering from
Lymphoma, AIDS or organ transplant.
The burden of the Clostridium difficile infection (CDI), has augmented in terms of
morbidity, incidence, cost and mortality and is one of the commonest cause of the infections
(Janoir 2016). Di Bella et al. (2015) have stated that in comparison to specific categories of
immunosuppression, the HIV infected patients are likely to develop CDI in comparison to the
other hospitalized patients. In a nationwide study conducted in USA, the solid organ
transplant has been found to be an independent predictor of the hospital mortality, colectomy
and graft complications.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MICROBIOLOGY
Antibiotic resistance and spread of infection
Development of multidrug resistant micro-organism is another reason behind the
recurrent bacterial infection. Antibiotic resistance of the bacteria is recognized as one of the
principal threats to human health throughout the world. For example, MRSA kills more
people worldwide in comparison to the HIV/AIDS, homicide and Parkinson’s disease.
Globally, there are 3.7% of new cases of tuberculosis reported and these new strains of
tuberculosis are resistant to isoniazid and rifampicin. Apart from tuberculosis, evidence also
indicated the existence of carbapenem-resistant enterobacteriaceae spp. and extended beta-
lactamase producing Enterobacteriacea. The main reason highlighted by the increase in the
antibiotic resistance among the microbial pathogen includes high rate of consumption of
antibiotics (Llor and Bjerrum 2014). According to Llor and Bjerrum (2014), there is a direct
correlation between the use of antibiotics and generation of antibiotic resistance. Countries
with the higher consumption of antibiotics like in European countries have higher rate of
antibiotic resistance. Ventola (2015) highlighted a completely different perspective behind
the increase in the antibiotic resistance. According to Ventola (2015), inappropriate
prescribing of antibiotic also leads to the generation of multidrug resistance bacteria. Studies
have indicated that choice of agents or duration of the antibiotic therapy leads to the
development of antibiotic resistance.
Zilberberg et al. (2014) is of the opinion that the improper dosage of antibiotic leads
to the change in the antibiotic induced gene expression and thereby increasing virulence.
Improper use of antibiotic also leads to microbial mutagenesis and leading to the
development of antibiotic resistance and subsequently rapid spread of the disease. In order to
study the improper dosage of antibiotics on the generation of multidrug resistance bacteria,
Antibiotic resistance and spread of infection
Development of multidrug resistant micro-organism is another reason behind the
recurrent bacterial infection. Antibiotic resistance of the bacteria is recognized as one of the
principal threats to human health throughout the world. For example, MRSA kills more
people worldwide in comparison to the HIV/AIDS, homicide and Parkinson’s disease.
Globally, there are 3.7% of new cases of tuberculosis reported and these new strains of
tuberculosis are resistant to isoniazid and rifampicin. Apart from tuberculosis, evidence also
indicated the existence of carbapenem-resistant enterobacteriaceae spp. and extended beta-
lactamase producing Enterobacteriacea. The main reason highlighted by the increase in the
antibiotic resistance among the microbial pathogen includes high rate of consumption of
antibiotics (Llor and Bjerrum 2014). According to Llor and Bjerrum (2014), there is a direct
correlation between the use of antibiotics and generation of antibiotic resistance. Countries
with the higher consumption of antibiotics like in European countries have higher rate of
antibiotic resistance. Ventola (2015) highlighted a completely different perspective behind
the increase in the antibiotic resistance. According to Ventola (2015), inappropriate
prescribing of antibiotic also leads to the generation of multidrug resistance bacteria. Studies
have indicated that choice of agents or duration of the antibiotic therapy leads to the
development of antibiotic resistance.
Zilberberg et al. (2014) is of the opinion that the improper dosage of antibiotic leads
to the change in the antibiotic induced gene expression and thereby increasing virulence.
Improper use of antibiotic also leads to microbial mutagenesis and leading to the
development of antibiotic resistance and subsequently rapid spread of the disease. In order to
study the improper dosage of antibiotics on the generation of multidrug resistance bacteria,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICROBIOLOGY
Zilberberg et al. (2014) conducted single-centre retrospective cohort study over the adult
patients in the intensive care units who are suffering from bacteremia or severe sepsis due to
gram negative bacterial infection. There results highlighted that the inappropriate use of the
antibiotics or in appropriate dosage of antibiotics lead to the development of multidrug
resistant (MDR) bacteria and thereby increasing the chances of hospital mortaility and re-
infection by the same bacteria.
Extensive use of agriculture is another reason behind the increase in the generation of
multidrug resistance bacteria. In the United Kingdom, antibiotics are widely used as growth
supplements in animal husbandry (Gelband et al. 2015). It is also used to prevent infection.
According to Rinsky et al. (2013), treating livestock with antibiotics is said to improve the
overall health of the animal and thereby helping to gee rate larger yields and higher-quality of
product. Anomaly (2015) is of the opinion that human ingests the antibiotics, which are used
for livestock rising, when they feed them. This leads to the transfer of resistant bacteria to
human body leading to the development of antibiotic resistance. The research conducted by
Rinsky et al. (2013), is of the opinion that the molecular detection method demonstrated the
existence of the resistant bacteria in the farm animals and this reach to the consumers when
they consume the meat of that animal. This occurs through a series of steps. At first the
antibiotic used in the process of food producing animals kills or suppresses susceptible
bacteria and thereby enabling the antibiotic-resistant bacteria to thrive. These antibiotic
resistant bacteria are transmitted through the food supply and causing infections in human
that may lead to adverse health consequences (Van Boeckel et al. 2015).
In relation to the use of antibiotics in the livestock raising and its effects on human
health, Seiffert et al. (2013) conducted a study. According to Seiffert et al. (2013),
Salmonella spp., Escherichia coli and Acinetobacter spp. are important human pathogens
causing serious infections to mankind. These infections are mainly treated via the application
Zilberberg et al. (2014) conducted single-centre retrospective cohort study over the adult
patients in the intensive care units who are suffering from bacteremia or severe sepsis due to
gram negative bacterial infection. There results highlighted that the inappropriate use of the
antibiotics or in appropriate dosage of antibiotics lead to the development of multidrug
resistant (MDR) bacteria and thereby increasing the chances of hospital mortaility and re-
infection by the same bacteria.
Extensive use of agriculture is another reason behind the increase in the generation of
multidrug resistance bacteria. In the United Kingdom, antibiotics are widely used as growth
supplements in animal husbandry (Gelband et al. 2015). It is also used to prevent infection.
According to Rinsky et al. (2013), treating livestock with antibiotics is said to improve the
overall health of the animal and thereby helping to gee rate larger yields and higher-quality of
product. Anomaly (2015) is of the opinion that human ingests the antibiotics, which are used
for livestock rising, when they feed them. This leads to the transfer of resistant bacteria to
human body leading to the development of antibiotic resistance. The research conducted by
Rinsky et al. (2013), is of the opinion that the molecular detection method demonstrated the
existence of the resistant bacteria in the farm animals and this reach to the consumers when
they consume the meat of that animal. This occurs through a series of steps. At first the
antibiotic used in the process of food producing animals kills or suppresses susceptible
bacteria and thereby enabling the antibiotic-resistant bacteria to thrive. These antibiotic
resistant bacteria are transmitted through the food supply and causing infections in human
that may lead to adverse health consequences (Van Boeckel et al. 2015).
In relation to the use of antibiotics in the livestock raising and its effects on human
health, Seiffert et al. (2013) conducted a study. According to Seiffert et al. (2013),
Salmonella spp., Escherichia coli and Acinetobacter spp. are important human pathogens
causing serious infections to mankind. These infections are mainly treated via the application
MICROBIOLOGY
of extended spectrum cephalosporins (ESCs). However, during the past few decades, it has
been highlighted that there is a rapid increase in the infections along with colonization of
ESC-resistant isolates. The reason highlighted by Seiffert et al. (2013) is overuse of
antibiotics or lack of completion of the antibiotic dosage generates resistance in the bacterial
strain. This generation of resistance within the bacterial strain is mainly mediated by the
formation of plasmid-mediated AmpCs or carbapenemase enzyme or via the production of
extended spectrum beta lactamase gene within the bacteria. This production of the antibiotic
specific lyses enzyme within the bacteria cleaves or inactivates antibiotics resulting in the
spread of the infection or recurrent infection. Animals are considered as the principal
reservoirs of MDR gram negative organisms due to the overuse of antibiotics in the
veterinary medicines. This overuse of antibiotics in veterinary medicine has lead to the
specific selection of ESC R E. coli, ESC-R Salmonella spp and to a lesser extent of MDR
Acinetobacter spp. This complex scenario is responsible for the expansion of MDR
organisms which have life-threatening significance over human race (Seiffert et al. 2013).
of extended spectrum cephalosporins (ESCs). However, during the past few decades, it has
been highlighted that there is a rapid increase in the infections along with colonization of
ESC-resistant isolates. The reason highlighted by Seiffert et al. (2013) is overuse of
antibiotics or lack of completion of the antibiotic dosage generates resistance in the bacterial
strain. This generation of resistance within the bacterial strain is mainly mediated by the
formation of plasmid-mediated AmpCs or carbapenemase enzyme or via the production of
extended spectrum beta lactamase gene within the bacteria. This production of the antibiotic
specific lyses enzyme within the bacteria cleaves or inactivates antibiotics resulting in the
spread of the infection or recurrent infection. Animals are considered as the principal
reservoirs of MDR gram negative organisms due to the overuse of antibiotics in the
veterinary medicines. This overuse of antibiotics in veterinary medicine has lead to the
specific selection of ESC R E. coli, ESC-R Salmonella spp and to a lesser extent of MDR
Acinetobacter spp. This complex scenario is responsible for the expansion of MDR
organisms which have life-threatening significance over human race (Seiffert et al. 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





