Comprehensive Report on Initial Management of Unconscious Patients
VerifiedAdded on 2023/04/17
|21
|4349
|225
Report
AI Summary
This report comprehensively addresses the initial management of unconscious patients in pre-hospital and emergency department settings. It begins by outlining the critical steps in pre-hospital care, emphasizing the ABCDE assessment (Airway, Breathing, Circulation, Disability, Exposure) and the importance of rapid intervention and transportation. The report details non-clinical observations at the scene, such as identifying potential drug use, alcohol consumption, or exposure to toxic substances. Furthermore, it discusses toxidromes, which are specific sets of symptoms indicating particular types of poisoning, and provides a generalized management approach in the emergency department, including resuscitation techniques, decontamination methods, and enhanced elimination strategies. The report underscores the importance of a thorough history, physical examination, and targeted interventions based on the identified toxidrome to improve patient outcomes. Desklib offers a wealth of similar resources for students seeking to enhance their understanding of healthcare and research topics.
Q1: Pre hospital Initial management in an unconscious patient:
It is always challenging, especially if the potential cause is not obvious.The sequence of management
is resuscitation, history and physical examination.
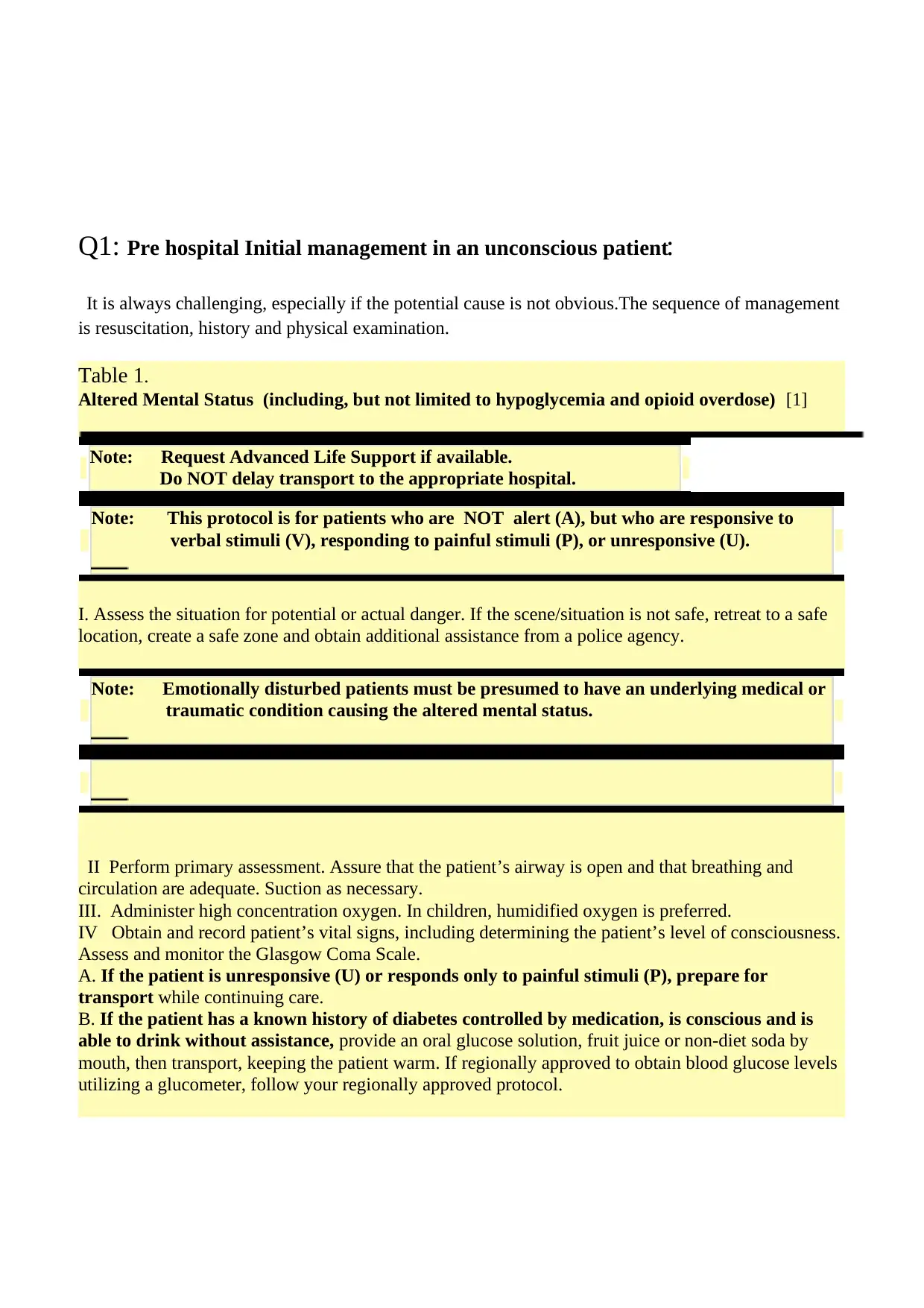
Table 1.
Altered Mental Status (including, but not limited to hypoglycemia and opioid overdose) [1]
Note: Request Advanced Life Support if available.
Do NOT delay transport to the appropriate hospital.
Note: This protocol is for patients who are NOT alert (A), but who are responsive to
verbal stimuli (V), responding to painful stimuli (P), or unresponsive (U).
I. Assess the situation for potential or actual danger. If the scene/situation is not safe, retreat to a safe
location, create a safe zone and obtain additional assistance from a police agency.
Note: Emotionally disturbed patients must be presumed to have an underlying medical or
traumatic condition causing the altered mental status.
II Perform primary assessment. Assure that the patient’s airway is open and that breathing and
circulation are adequate. Suction as necessary.
III. Administer high concentration oxygen. In children, humidified oxygen is preferred.
IV Obtain and record patient’s vital signs, including determining the patient’s level of consciousness.
Assess and monitor the Glasgow Coma Scale.
A. If the patient is unresponsive (U) or responds only to painful stimuli (P), prepare for
transport while continuing care.
B. If the patient has a known history of diabetes controlled by medication, is conscious and is
able to drink without assistance, provide an oral glucose solution, fruit juice or non-diet soda by
mouth, then transport, keeping the patient warm. If regionally approved to obtain blood glucose levels
utilizing a glucometer, follow your regionally approved protocol.
It is always challenging, especially if the potential cause is not obvious.The sequence of management
is resuscitation, history and physical examination.
Table 1.
Altered Mental Status (including, but not limited to hypoglycemia and opioid overdose) [1]
Note: Request Advanced Life Support if available.
Do NOT delay transport to the appropriate hospital.
Note: This protocol is for patients who are NOT alert (A), but who are responsive to
verbal stimuli (V), responding to painful stimuli (P), or unresponsive (U).
I. Assess the situation for potential or actual danger. If the scene/situation is not safe, retreat to a safe
location, create a safe zone and obtain additional assistance from a police agency.
Note: Emotionally disturbed patients must be presumed to have an underlying medical or
traumatic condition causing the altered mental status.
II Perform primary assessment. Assure that the patient’s airway is open and that breathing and
circulation are adequate. Suction as necessary.
III. Administer high concentration oxygen. In children, humidified oxygen is preferred.
IV Obtain and record patient’s vital signs, including determining the patient’s level of consciousness.
Assess and monitor the Glasgow Coma Scale.
A. If the patient is unresponsive (U) or responds only to painful stimuli (P), prepare for
transport while continuing care.
B. If the patient has a known history of diabetes controlled by medication, is conscious and is
able to drink without assistance, provide an oral glucose solution, fruit juice or non-diet soda by
mouth, then transport, keeping the patient warm. If regionally approved to obtain blood glucose levels
utilizing a glucometer, follow your regionally approved protocol.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The initial management starts with the correction of ABCDE assessment [2 ]
Airway:
Immediate effort should be made to clear the airway by “head tilt chin lift maneuver”. Remove any
foreign body, mucous or blood from the mouth and pharynx and place a proper size oropharyngeal
tube.
Breathing:
Breathing should be assessed by counting the Respiratory rate (normal adult rate is 12--20 breaths /
min).Any increase in the R.R. more than 20 /minute and Spo2 less than 92%, indicates, respiratory
distress and O2 should be started to keep the Spo2 more than 92% [2]
Any abnormal odours on breathing (table 2) should be particularly noticed for the causative agents.
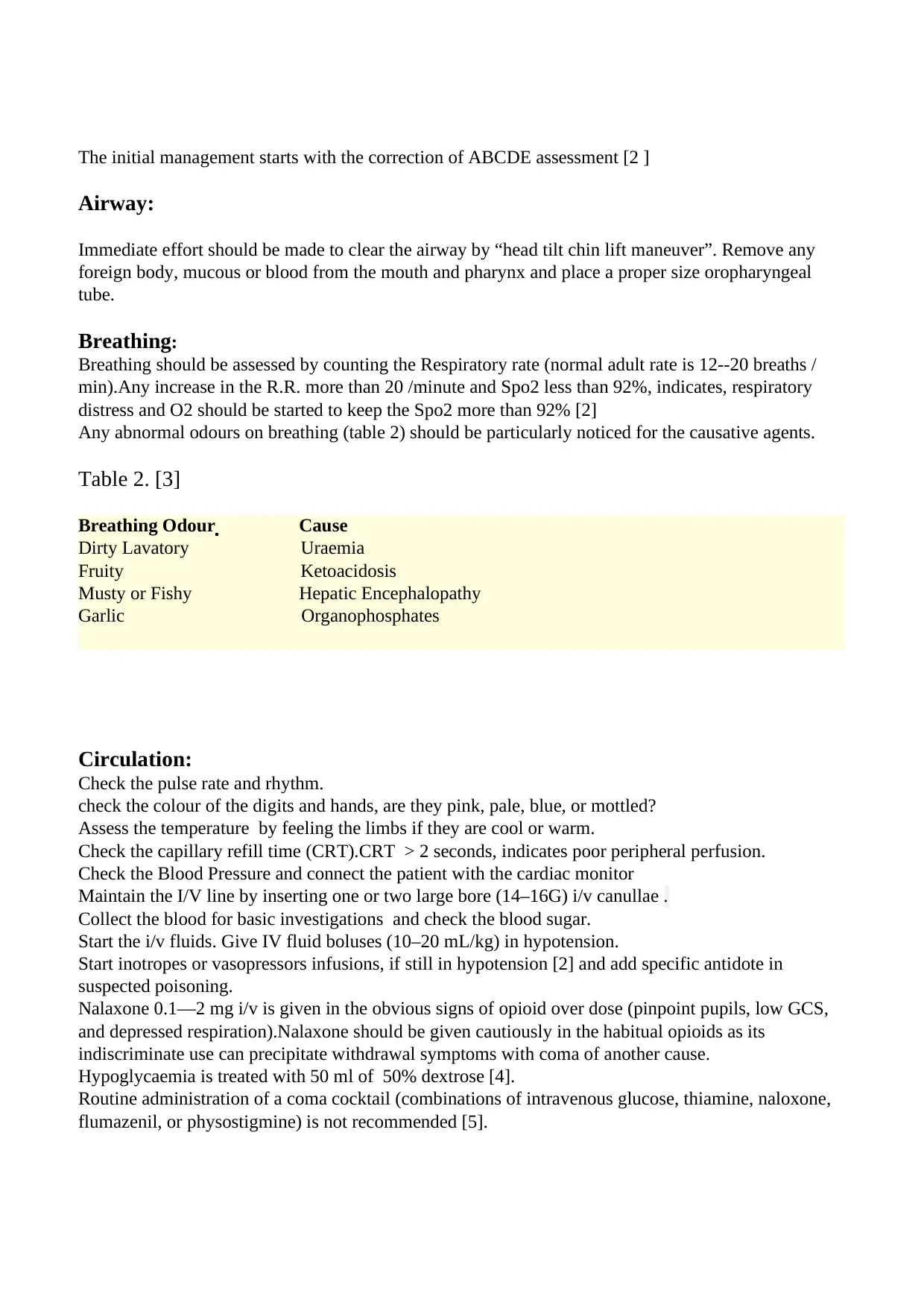
Table 2. [3]
Breathing Odour Cause
Dirty Lavatory Uraemia
Fruity Ketoacidosis
Musty or Fishy Hepatic Encephalopathy
Garlic Organophosphates
Circulation:
Check the pulse rate and rhythm.
check the colour of the digits and hands, are they pink, pale, blue, or mottled?
Assess the temperature by feeling the limbs if they are cool or warm.
Check the capillary refill time (CRT).CRT > 2 seconds, indicates poor peripheral perfusion.
Check the Blood Pressure and connect the patient with the cardiac monitor
Maintain the I/V line by inserting one or two large bore (14–16G) i/v canullae .
Collect the blood for basic investigations and check the blood sugar.
Start the i/v fluids. Give IV fluid boluses (10–20 mL/kg) in hypotension.
Start inotropes or vasopressors infusions, if still in hypotension [2] and add specific antidote in
suspected poisoning.
Nalaxone 0.1—2 mg i/v is given in the obvious signs of opioid over dose (pinpoint pupils, low GCS,
and depressed respiration).Nalaxone should be given cautiously in the habitual opioids as its
indiscriminate use can precipitate withdrawal symptoms with coma of another cause.
Hypoglycaemia is treated with 50 ml of 50% dextrose [4].
Routine administration of a coma cocktail (combinations of intravenous glucose, thiamine, naloxone,
flumazenil, or physostigmine) is not recommended [5].
Airway:
Immediate effort should be made to clear the airway by “head tilt chin lift maneuver”. Remove any
foreign body, mucous or blood from the mouth and pharynx and place a proper size oropharyngeal
tube.
Breathing:
Breathing should be assessed by counting the Respiratory rate (normal adult rate is 12--20 breaths /
min).Any increase in the R.R. more than 20 /minute and Spo2 less than 92%, indicates, respiratory
distress and O2 should be started to keep the Spo2 more than 92% [2]
Any abnormal odours on breathing (table 2) should be particularly noticed for the causative agents.
Table 2. [3]
Breathing Odour Cause
Dirty Lavatory Uraemia
Fruity Ketoacidosis
Musty or Fishy Hepatic Encephalopathy
Garlic Organophosphates
Circulation:
Check the pulse rate and rhythm.
check the colour of the digits and hands, are they pink, pale, blue, or mottled?
Assess the temperature by feeling the limbs if they are cool or warm.
Check the capillary refill time (CRT).CRT > 2 seconds, indicates poor peripheral perfusion.
Check the Blood Pressure and connect the patient with the cardiac monitor
Maintain the I/V line by inserting one or two large bore (14–16G) i/v canullae .
Collect the blood for basic investigations and check the blood sugar.
Start the i/v fluids. Give IV fluid boluses (10–20 mL/kg) in hypotension.
Start inotropes or vasopressors infusions, if still in hypotension [2] and add specific antidote in
suspected poisoning.
Nalaxone 0.1—2 mg i/v is given in the obvious signs of opioid over dose (pinpoint pupils, low GCS,
and depressed respiration).Nalaxone should be given cautiously in the habitual opioids as its
indiscriminate use can precipitate withdrawal symptoms with coma of another cause.
Hypoglycaemia is treated with 50 ml of 50% dextrose [4].
Routine administration of a coma cocktail (combinations of intravenous glucose, thiamine, naloxone,
flumazenil, or physostigmine) is not recommended [5].
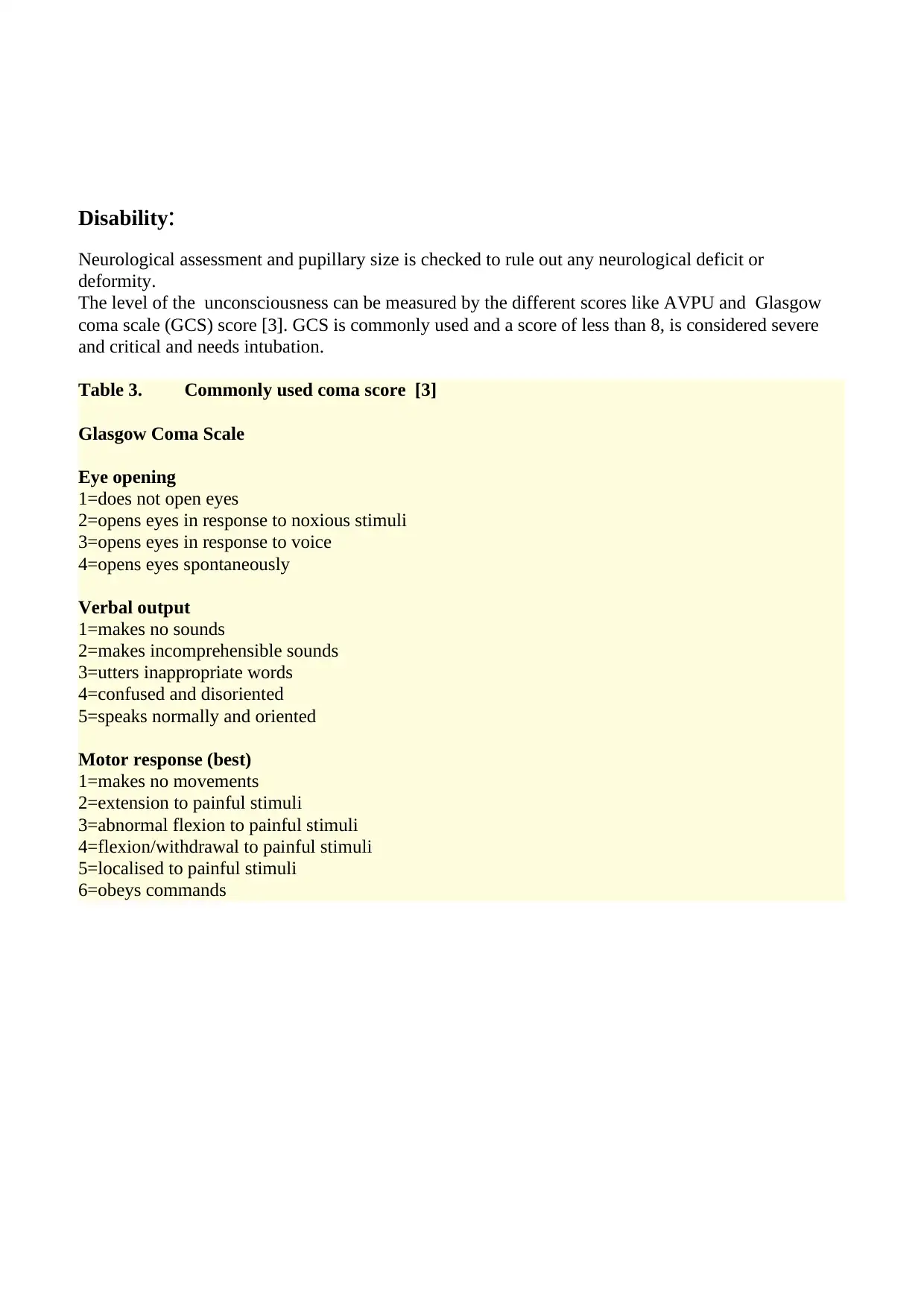
Disability:
Neurological assessment and pupillary size is checked to rule out any neurological deficit or
deformity.
The level of the unconsciousness can be measured by the different scores like AVPU and Glasgow
coma scale (GCS) score [3]. GCS is commonly used and a score of less than 8, is considered severe
and critical and needs intubation.
Table 3. Commonly used coma score [3]
Glasgow Coma Scale
Eye opening
1=does not open eyes
2=opens eyes in response to noxious stimuli
3=opens eyes in response to voice
4=opens eyes spontaneously
Verbal output
1=makes no sounds
2=makes incomprehensible sounds
3=utters inappropriate words
4=confused and disoriented
5=speaks normally and oriented
Motor response (best)
1=makes no movements
2=extension to painful stimuli
3=abnormal flexion to painful stimuli
4=flexion/withdrawal to painful stimuli
5=localised to painful stimuli
6=obeys commands
Neurological assessment and pupillary size is checked to rule out any neurological deficit or
deformity.
The level of the unconsciousness can be measured by the different scores like AVPU and Glasgow
coma scale (GCS) score [3]. GCS is commonly used and a score of less than 8, is considered severe
and critical and needs intubation.
Table 3. Commonly used coma score [3]
Glasgow Coma Scale
Eye opening
1=does not open eyes
2=opens eyes in response to noxious stimuli
3=opens eyes in response to voice
4=opens eyes spontaneously
Verbal output
1=makes no sounds
2=makes incomprehensible sounds
3=utters inappropriate words
4=confused and disoriented
5=speaks normally and oriented
Motor response (best)
1=makes no movements
2=extension to painful stimuli
3=abnormal flexion to painful stimuli
4=flexion/withdrawal to painful stimuli
5=localised to painful stimuli
6=obeys commands
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
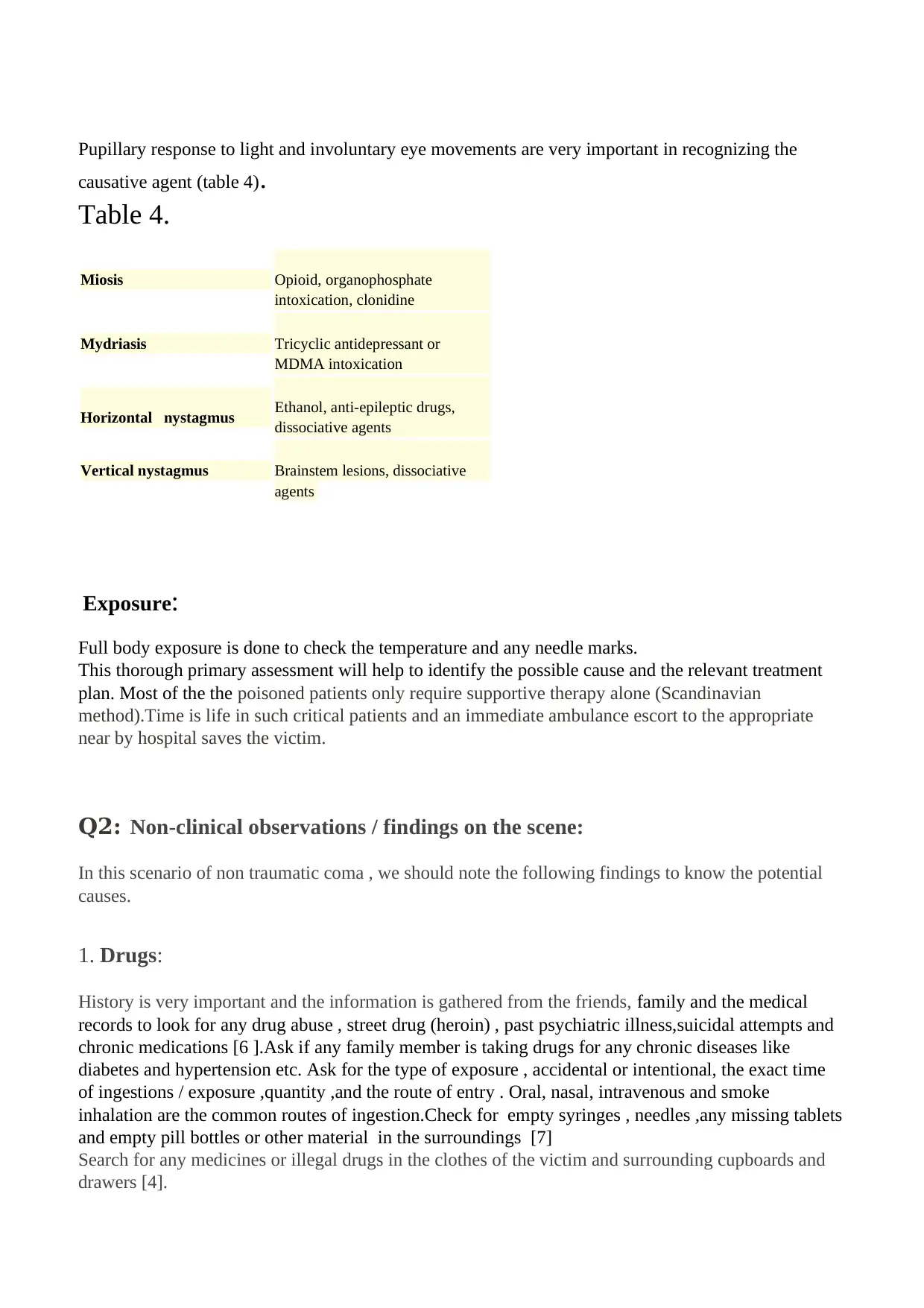
Pupillary response to light and involuntary eye movements are very important in recognizing the
causative agent (table 4).
Table 4.
Miosis Opioid, organophosphate
intoxication, clonidine
Mydriasis Tricyclic antidepressant or
MDMA intoxication
Horizontal nystagmus Ethanol, anti-epileptic drugs,
dissociative agents
Vertical nystagmus Brainstem lesions, dissociative
agents
Exposure:
Full body exposure is done to check the temperature and any needle marks.
This thorough primary assessment will help to identify the possible cause and the relevant treatment
plan. Most of the the poisoned patients only require supportive therapy alone (Scandinavian
method).Time is life in such critical patients and an immediate ambulance escort to the appropriate
near by hospital saves the victim.
Q2: Non-clinical observations / findings on the scene:
In this scenario of non traumatic coma , we should note the following findings to know the potential
causes.
1. Drugs:
History is very important and the information is gathered from the friends, family and the medical
records to look for any drug abuse , street drug (heroin) , past psychiatric illness,suicidal attempts and
chronic medications [6 ].Ask if any family member is taking drugs for any chronic diseases like
diabetes and hypertension etc. Ask for the type of exposure , accidental or intentional, the exact time
of ingestions / exposure ,quantity ,and the route of entry . Oral, nasal, intravenous and smoke
inhalation are the common routes of ingestion.Check for empty syringes , needles ,any missing tablets
and empty pill bottles or other material in the surroundings [7]
Search for any medicines or illegal drugs in the clothes of the victim and surrounding cupboards and
drawers [4].
causative agent (table 4).
Table 4.
Miosis Opioid, organophosphate
intoxication, clonidine
Mydriasis Tricyclic antidepressant or
MDMA intoxication
Horizontal nystagmus Ethanol, anti-epileptic drugs,
dissociative agents
Vertical nystagmus Brainstem lesions, dissociative
agents
Exposure:
Full body exposure is done to check the temperature and any needle marks.
This thorough primary assessment will help to identify the possible cause and the relevant treatment
plan. Most of the the poisoned patients only require supportive therapy alone (Scandinavian
method).Time is life in such critical patients and an immediate ambulance escort to the appropriate
near by hospital saves the victim.
Q2: Non-clinical observations / findings on the scene:
In this scenario of non traumatic coma , we should note the following findings to know the potential
causes.
1. Drugs:
History is very important and the information is gathered from the friends, family and the medical
records to look for any drug abuse , street drug (heroin) , past psychiatric illness,suicidal attempts and
chronic medications [6 ].Ask if any family member is taking drugs for any chronic diseases like
diabetes and hypertension etc. Ask for the type of exposure , accidental or intentional, the exact time
of ingestions / exposure ,quantity ,and the route of entry . Oral, nasal, intravenous and smoke
inhalation are the common routes of ingestion.Check for empty syringes , needles ,any missing tablets
and empty pill bottles or other material in the surroundings [7]
Search for any medicines or illegal drugs in the clothes of the victim and surrounding cupboards and
drawers [4].
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2.Alcohal:
Search and count for any empty or half filled bottles to know the quantity of ingestion.
“Binge" drinking, is the excessive consumption of alcohol in a short period of time [8]
3. Tobacco / cigarettes / cigars:
Cocaine , heroin and other drugs are inhaled with tobacco. Count for the empty cigarette boxes for
drug overdose.
4. Pesticides:
Look for any pesticides containers and sense for any recent sprays.
5. Bleaching and cleaning chemicals:
Look for the empty containers of washing powders and liquids used for cleaning floors and wash
rooms.
6. Hand sanitizers:
These contain ethanol. Look and count for the empty bottles.
7. Letter / Document:
Any written note , showing attempted suicide.
Q3:
Toxidromes and Generalized Management Approach in Emergency Department:
Mofenson and Greensher invented the term toxidrome in 1970. Toxidromes are a group of signs or
symptoms produced by a specific class of poisoning drugs or substances. Cholinergic,
Anticholinergic, Sympathomimetic, opioids, and serotonin syndrome are the most common
toxidromes [7, 9 ]
The World Health Organization (WHO) data shows that poisoning is a serious world health issue. In
2008, The number of poisoning deaths exceeded the number of deaths due to motor vehicle crashes
and in 2012, almost 190,000 people died worldwide due to poisoning. Internationally, the numbers of
poisoning patients presenting to the emergency departments have tremendously increased in the last
10 years.
Toxicology has become an important field in the emergency department due to the raised numbers of
accidental and intentional overdoses [10,11].
Search and count for any empty or half filled bottles to know the quantity of ingestion.
“Binge" drinking, is the excessive consumption of alcohol in a short period of time [8]
3. Tobacco / cigarettes / cigars:
Cocaine , heroin and other drugs are inhaled with tobacco. Count for the empty cigarette boxes for
drug overdose.
4. Pesticides:
Look for any pesticides containers and sense for any recent sprays.
5. Bleaching and cleaning chemicals:
Look for the empty containers of washing powders and liquids used for cleaning floors and wash
rooms.
6. Hand sanitizers:
These contain ethanol. Look and count for the empty bottles.
7. Letter / Document:
Any written note , showing attempted suicide.
Q3:
Toxidromes and Generalized Management Approach in Emergency Department:
Mofenson and Greensher invented the term toxidrome in 1970. Toxidromes are a group of signs or
symptoms produced by a specific class of poisoning drugs or substances. Cholinergic,
Anticholinergic, Sympathomimetic, opioids, and serotonin syndrome are the most common
toxidromes [7, 9 ]
The World Health Organization (WHO) data shows that poisoning is a serious world health issue. In
2008, The number of poisoning deaths exceeded the number of deaths due to motor vehicle crashes
and in 2012, almost 190,000 people died worldwide due to poisoning. Internationally, the numbers of
poisoning patients presenting to the emergency departments have tremendously increased in the last
10 years.
Toxicology has become an important field in the emergency department due to the raised numbers of
accidental and intentional overdoses [10,11].
As mentioned above in the prehospital management section, the emergency approach in all the cases
of non traumatic altered sensorium and suspected poisoning , includes: resuscitation, history and
physical examination.After assessing and correcting the ABCDE, the differential diagnosis ,
laboratory investigations and specific antidotes and treatments are considered for the causative agents.
Resuscitation :
Airway (A):
Routine methods are used to secure the airways with airway tubes.Endotracheal intubation and
mechanical ventilation may be needed in case of inadequate ventilation.
Breathing (B):
Normal adult respiratory rate is 12--20 breaths /min.Any increase in the R.R. more than 20 /minute
and Spo2 less than 92%, indicates, respiratory distress and O2 should be started to keep the Spo2 more
than 92%.
Circulation(C):
Blood pressure , pulse rate and rhythm is checked and the patient is connected to the cardiac
monitor.The I/V line is maintained with one or two large bore (14–16G) i/v canullae .Blood is
collected for the basic investigations and the blood sugar is checked.Hypoglycaemia is treated with
50% 50 mL dextrose [3]
If the patient is having hypotension, give repeated iv fluid boluses (10–20ml/kg). Inotropes or
vasopressor infusions are started in case of non responding hypotension.
Disability (D):
Glasgow coma scale (GCS table 3 above) and Full Outline Of Unresponsiveness (FOUR) score [12]
are used and pupillary size is checked to rule out any neurological deficit or deformity.
Pupillary response to light is very important in recognizing the causative agent (table 4 above)
of non traumatic altered sensorium and suspected poisoning , includes: resuscitation, history and
physical examination.After assessing and correcting the ABCDE, the differential diagnosis ,
laboratory investigations and specific antidotes and treatments are considered for the causative agents.
Resuscitation :
Airway (A):
Routine methods are used to secure the airways with airway tubes.Endotracheal intubation and
mechanical ventilation may be needed in case of inadequate ventilation.
Breathing (B):
Normal adult respiratory rate is 12--20 breaths /min.Any increase in the R.R. more than 20 /minute
and Spo2 less than 92%, indicates, respiratory distress and O2 should be started to keep the Spo2 more
than 92%.
Circulation(C):
Blood pressure , pulse rate and rhythm is checked and the patient is connected to the cardiac
monitor.The I/V line is maintained with one or two large bore (14–16G) i/v canullae .Blood is
collected for the basic investigations and the blood sugar is checked.Hypoglycaemia is treated with
50% 50 mL dextrose [3]
If the patient is having hypotension, give repeated iv fluid boluses (10–20ml/kg). Inotropes or
vasopressor infusions are started in case of non responding hypotension.
Disability (D):
Glasgow coma scale (GCS table 3 above) and Full Outline Of Unresponsiveness (FOUR) score [12]
are used and pupillary size is checked to rule out any neurological deficit or deformity.
Pupillary response to light is very important in recognizing the causative agent (table 4 above)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
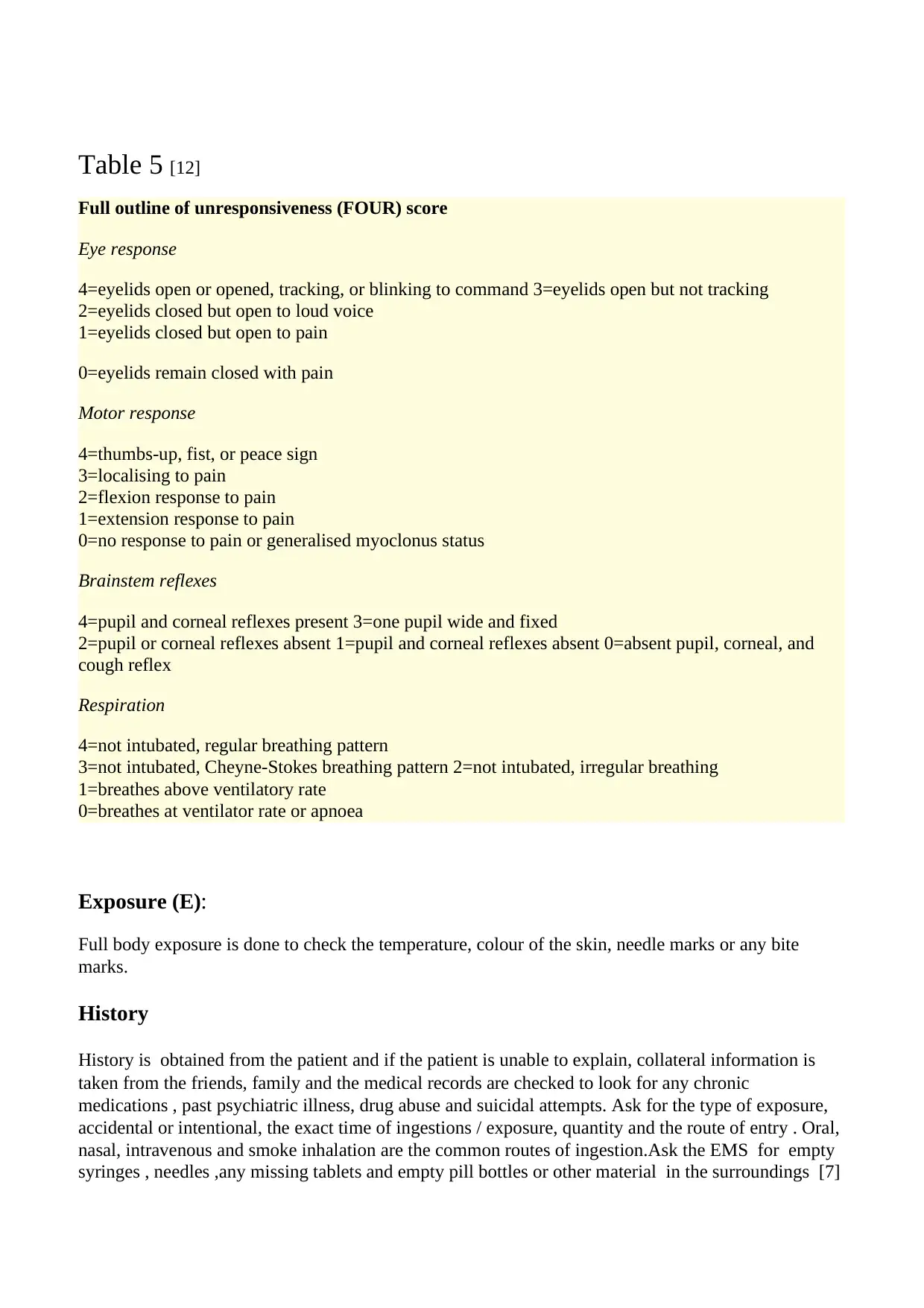
Table 5 [12]
Full outline of unresponsiveness (FOUR) score
Eye response
4=eyelids open or opened, tracking, or blinking to command 3=eyelids open but not tracking
2=eyelids closed but open to loud voice
1=eyelids closed but open to pain
0=eyelids remain closed with pain
Motor response
4=thumbs-up, fist, or peace sign
3=localising to pain
2=flexion response to pain
1=extension response to pain
0=no response to pain or generalised myoclonus status
Brainstem reflexes
4=pupil and corneal reflexes present 3=one pupil wide and fixed
2=pupil or corneal reflexes absent 1=pupil and corneal reflexes absent 0=absent pupil, corneal, and
cough reflex
Respiration
4=not intubated, regular breathing pattern
3=not intubated, Cheyne-Stokes breathing pattern 2=not intubated, irregular breathing
1=breathes above ventilatory rate
0=breathes at ventilator rate or apnoea
Exposure (E):
Full body exposure is done to check the temperature, colour of the skin, needle marks or any bite
marks.
History
History is obtained from the patient and if the patient is unable to explain, collateral information is
taken from the friends, family and the medical records are checked to look for any chronic
medications , past psychiatric illness, drug abuse and suicidal attempts. Ask for the type of exposure,
accidental or intentional, the exact time of ingestions / exposure, quantity and the route of entry . Oral,
nasal, intravenous and smoke inhalation are the common routes of ingestion.Ask the EMS for empty
syringes , needles ,any missing tablets and empty pill bottles or other material in the surroundings [7]
Full outline of unresponsiveness (FOUR) score
Eye response
4=eyelids open or opened, tracking, or blinking to command 3=eyelids open but not tracking
2=eyelids closed but open to loud voice
1=eyelids closed but open to pain
0=eyelids remain closed with pain
Motor response
4=thumbs-up, fist, or peace sign
3=localising to pain
2=flexion response to pain
1=extension response to pain
0=no response to pain or generalised myoclonus status
Brainstem reflexes
4=pupil and corneal reflexes present 3=one pupil wide and fixed
2=pupil or corneal reflexes absent 1=pupil and corneal reflexes absent 0=absent pupil, corneal, and
cough reflex
Respiration
4=not intubated, regular breathing pattern
3=not intubated, Cheyne-Stokes breathing pattern 2=not intubated, irregular breathing
1=breathes above ventilatory rate
0=breathes at ventilator rate or apnoea
Exposure (E):
Full body exposure is done to check the temperature, colour of the skin, needle marks or any bite
marks.
History
History is obtained from the patient and if the patient is unable to explain, collateral information is
taken from the friends, family and the medical records are checked to look for any chronic
medications , past psychiatric illness, drug abuse and suicidal attempts. Ask for the type of exposure,
accidental or intentional, the exact time of ingestions / exposure, quantity and the route of entry . Oral,
nasal, intravenous and smoke inhalation are the common routes of ingestion.Ask the EMS for empty
syringes , needles ,any missing tablets and empty pill bottles or other material in the surroundings [7]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Physical examination:
Some clues and information about the toxidromes can be obtained from the Physical examination
including general appearance, mental status ,skin colour physical signs of intravenous drugs abuse
(track marks), pupilary size and nystagmus, odour (table 2 above), hyper salivation, abnormal breath
sounds, heart rate and rhythm and the patient’s clothing ( any medications) [4].
Decontaminations
Gross decontamination:
It is used in chemical and biological poisoning and should be done in a specified and isolated area.
Toxins are removed from the patient’s body by gross external washing with copious amount of water.
Gastrointestinal decontamination
1. Gastric Lavage.
It can be done in conscious, alert patients with ingestion of less than 1 hour or more, depending on the
quantity of the toxic drugs. It is contraindicated in corrosive/hydrocarbons, unprotected airway and
unstable patients with seizures and hypotension.[13]
2.Activated charcoal
It is most effective within first hour of ingestion and is not effective in alcohols, metal, corrosive, and
lithium. It is contraindicated in caustic ingestion , gut perforation and unprotected airway and can be
given through nasogastric tube.[14 ]
3. Whole-bowel irrigation
It is the mechanical cleaning of the whole gastrointestinal tract which can be done by Polyethylene
glycol solution. It can be done in potential toxins not absorbed by activated charcoal such as metals
and lithium. Absent bowel sound and perforation are the contraindications.[15 ]
Enhanced elimination
It is used to accelerate the rate of toxic removal from the body to reduce the duration of clinical
intoxication. Different methods are used for this extraordinary enhanced elimination in a poor
outcome despite all the taken measures[7]
1.Multiple dose activated charcoal (MDAC).
2.Urinary alkalinisation.
3.Extracorporeal elimination e.g. haemodialysis, haemoperfusion, and exchange transfusion.
Some clues and information about the toxidromes can be obtained from the Physical examination
including general appearance, mental status ,skin colour physical signs of intravenous drugs abuse
(track marks), pupilary size and nystagmus, odour (table 2 above), hyper salivation, abnormal breath
sounds, heart rate and rhythm and the patient’s clothing ( any medications) [4].
Decontaminations
Gross decontamination:
It is used in chemical and biological poisoning and should be done in a specified and isolated area.
Toxins are removed from the patient’s body by gross external washing with copious amount of water.
Gastrointestinal decontamination
1. Gastric Lavage.
It can be done in conscious, alert patients with ingestion of less than 1 hour or more, depending on the
quantity of the toxic drugs. It is contraindicated in corrosive/hydrocarbons, unprotected airway and
unstable patients with seizures and hypotension.[13]
2.Activated charcoal
It is most effective within first hour of ingestion and is not effective in alcohols, metal, corrosive, and
lithium. It is contraindicated in caustic ingestion , gut perforation and unprotected airway and can be
given through nasogastric tube.[14 ]
3. Whole-bowel irrigation
It is the mechanical cleaning of the whole gastrointestinal tract which can be done by Polyethylene
glycol solution. It can be done in potential toxins not absorbed by activated charcoal such as metals
and lithium. Absent bowel sound and perforation are the contraindications.[15 ]
Enhanced elimination
It is used to accelerate the rate of toxic removal from the body to reduce the duration of clinical
intoxication. Different methods are used for this extraordinary enhanced elimination in a poor
outcome despite all the taken measures[7]
1.Multiple dose activated charcoal (MDAC).
2.Urinary alkalinisation.
3.Extracorporeal elimination e.g. haemodialysis, haemoperfusion, and exchange transfusion.
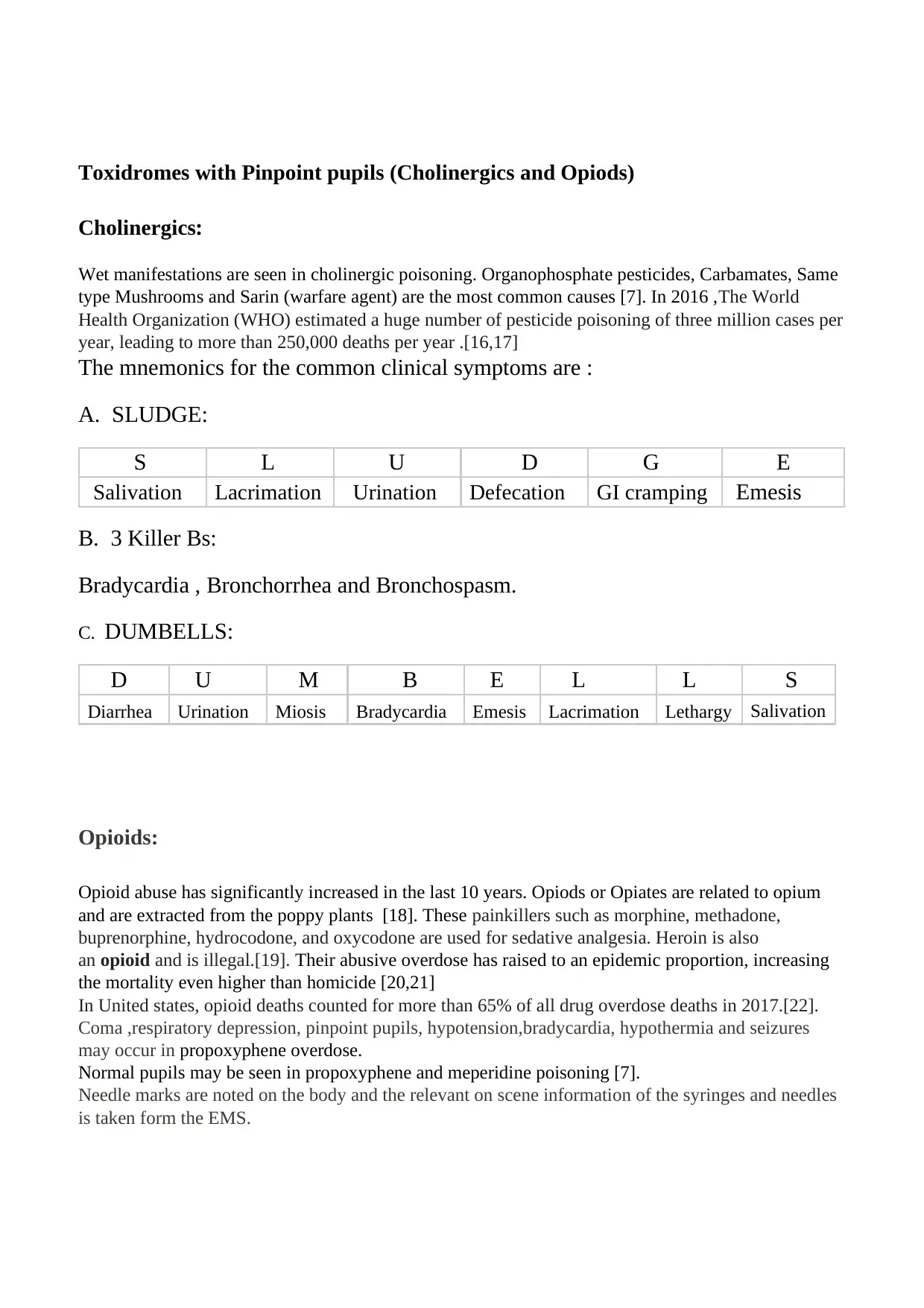
Toxidromes with Pinpoint pupils (Cholinergics and Opiods)
Cholinergics:
Wet manifestations are seen in cholinergic poisoning. Organophosphate pesticides, Carbamates, Same
type Mushrooms and Sarin (warfare agent) are the most common causes [7]. In 2016 ,The World
Health Organization (WHO) estimated a huge number of pesticide poisoning of three million cases per
year, leading to more than 250,000 deaths per year .[16,17]
The mnemonics for the common clinical symptoms are :
A. SLUDGE:
S L U D G E
Salivation Lacrimation Urination Defecation GI cramping Emesis
B. 3 Killer Bs:
Bradycardia , Bronchorrhea and Bronchospasm.
C. DUMBELLS:
D U M B E L L S
Diarrhea Urination Miosis Bradycardia Emesis Lacrimation Lethargy Salivation
Opioids:
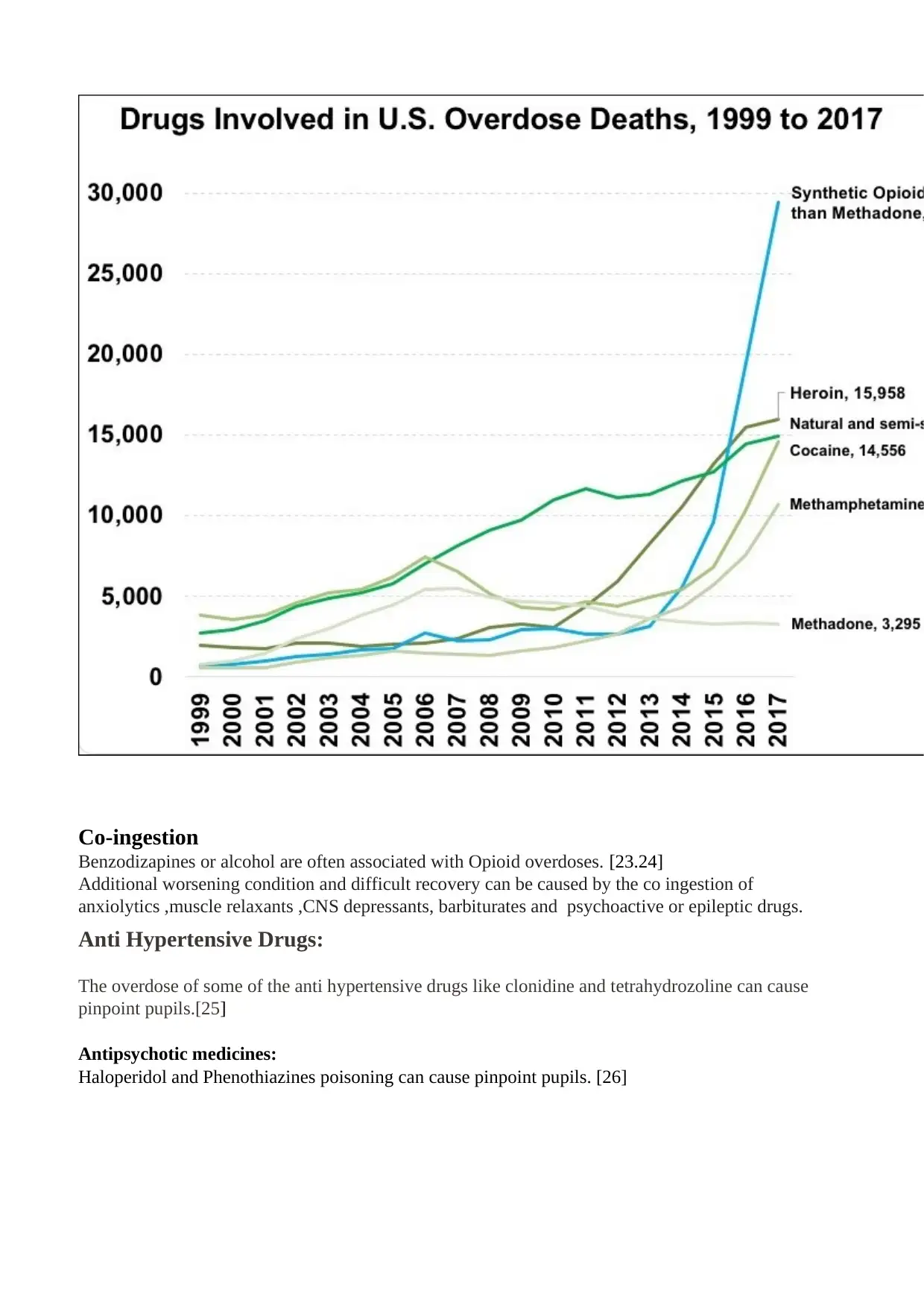
Opioid abuse has significantly increased in the last 10 years. Opiods or Opiates are related to opium
and are extracted from the poppy plants [18]. These painkillers such as morphine, methadone,
buprenorphine, hydrocodone, and oxycodone are used for sedative analgesia. Heroin is also
an opioid and is illegal.[19]. Their abusive overdose has raised to an epidemic proportion, increasing
the mortality even higher than homicide [20,21]
In United states, opioid deaths counted for more than 65% of all drug overdose deaths in 2017.[22].
Coma ,respiratory depression, pinpoint pupils, hypotension,bradycardia, hypothermia and seizures
may occur in propoxyphene overdose.
Normal pupils may be seen in propoxyphene and meperidine poisoning [7].
Needle marks are noted on the body and the relevant on scene information of the syringes and needles
is taken form the EMS.
Cholinergics:
Wet manifestations are seen in cholinergic poisoning. Organophosphate pesticides, Carbamates, Same
type Mushrooms and Sarin (warfare agent) are the most common causes [7]. In 2016 ,The World
Health Organization (WHO) estimated a huge number of pesticide poisoning of three million cases per
year, leading to more than 250,000 deaths per year .[16,17]
The mnemonics for the common clinical symptoms are :
A. SLUDGE:
S L U D G E
Salivation Lacrimation Urination Defecation GI cramping Emesis
B. 3 Killer Bs:
Bradycardia , Bronchorrhea and Bronchospasm.
C. DUMBELLS:
D U M B E L L S
Diarrhea Urination Miosis Bradycardia Emesis Lacrimation Lethargy Salivation
Opioids:
Opioid abuse has significantly increased in the last 10 years. Opiods or Opiates are related to opium
and are extracted from the poppy plants [18]. These painkillers such as morphine, methadone,
buprenorphine, hydrocodone, and oxycodone are used for sedative analgesia. Heroin is also
an opioid and is illegal.[19]. Their abusive overdose has raised to an epidemic proportion, increasing
the mortality even higher than homicide [20,21]
In United states, opioid deaths counted for more than 65% of all drug overdose deaths in 2017.[22].
Coma ,respiratory depression, pinpoint pupils, hypotension,bradycardia, hypothermia and seizures
may occur in propoxyphene overdose.
Normal pupils may be seen in propoxyphene and meperidine poisoning [7].
Needle marks are noted on the body and the relevant on scene information of the syringes and needles
is taken form the EMS.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Co-ingestion
Benzodizapines or alcohol are often associated with Opioid overdoses. [23.24]
Additional worsening condition and difficult recovery can be caused by the co ingestion of
anxiolytics ,muscle relaxants ,CNS depressants, barbiturates and psychoactive or epileptic drugs.
Anti Hypertensive Drugs:
The overdose of some of the anti hypertensive drugs like clonidine and tetrahydrozoline can cause
pinpoint pupils.[25]
Antipsychotic medicines:
Haloperidol and Phenothiazines poisoning can cause pinpoint pupils. [26]
Benzodizapines or alcohol are often associated with Opioid overdoses. [23.24]
Additional worsening condition and difficult recovery can be caused by the co ingestion of
anxiolytics ,muscle relaxants ,CNS depressants, barbiturates and psychoactive or epileptic drugs.
Anti Hypertensive Drugs:
The overdose of some of the anti hypertensive drugs like clonidine and tetrahydrozoline can cause
pinpoint pupils.[25]
Antipsychotic medicines:
Haloperidol and Phenothiazines poisoning can cause pinpoint pupils. [26]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
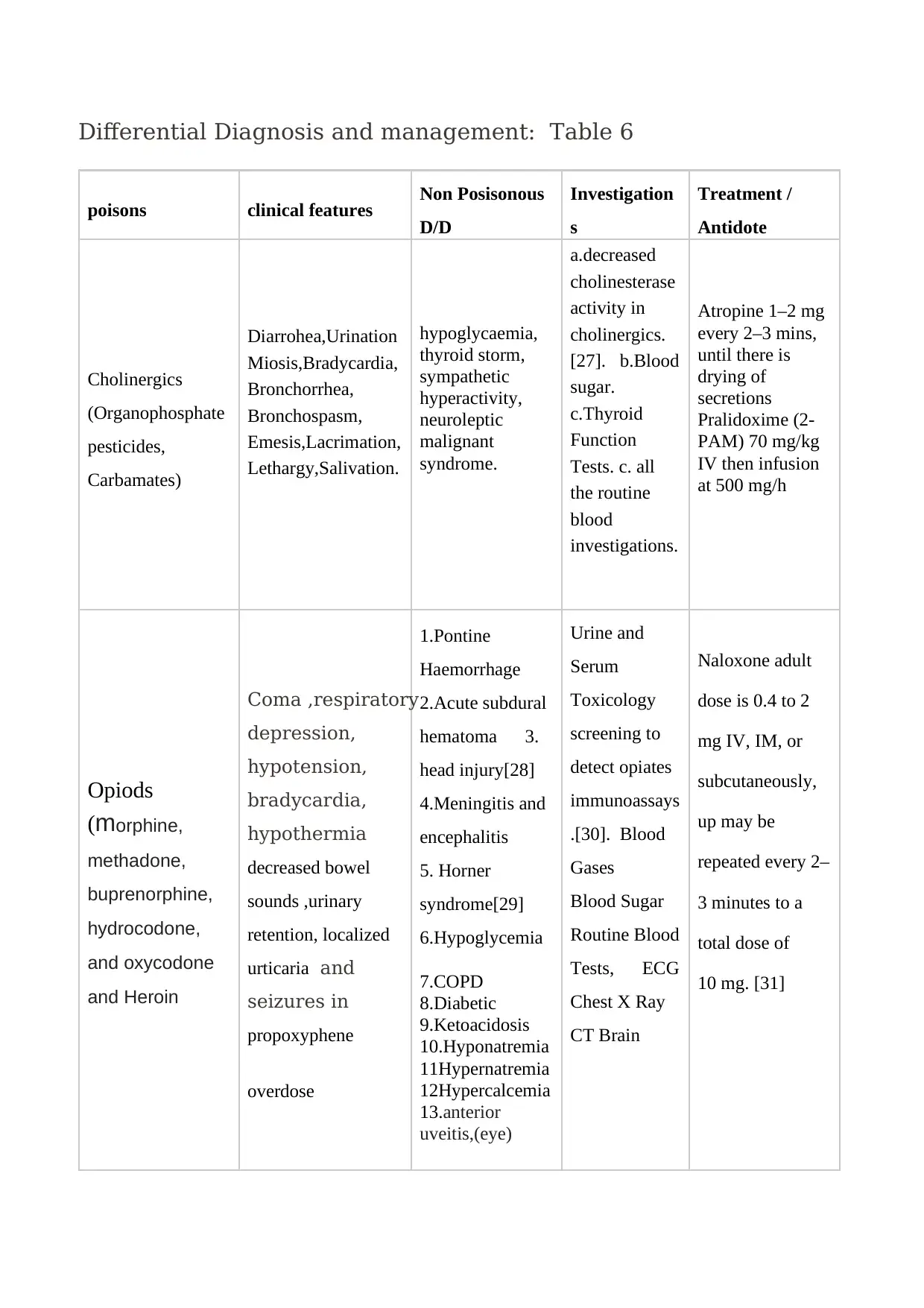
Differential Diagnosis and management: Table 6
poisons clinical features Non Posisonous
D/D
Investigation
s
Treatment /
Antidote
Cholinergics
(Organophosphate
pesticides,
Carbamates)
Diarrohea,Urination
Miosis,Bradycardia,
Bronchorrhea,
Bronchospasm,
Emesis,Lacrimation,
Lethargy,Salivation.
hypoglycaemia,
thyroid storm,
sympathetic
hyperactivity,
neuroleptic
malignant
syndrome.
a.decreased
cholinesterase
activity in
cholinergics.
[27]. b.Blood
sugar.
c.Thyroid
Function
Tests. c. all
the routine
blood
investigations.
Atropine 1–2 mg
every 2–3 mins,
until there is
drying of
secretions
Pralidoxime (2-
PAM) 70 mg/kg
IV then infusion
at 500 mg/h
Opiods
(morphine,
methadone,
buprenorphine,
hydrocodone,
and oxycodone
and Heroin
Coma ,respiratory
depression,
hypotension,
bradycardia,
hypothermia
decreased bowel
sounds ,urinary
retention, localized
urticaria and
seizures in
propoxyphene
overdose
1.Pontine
Haemorrhage
2.Acute subdural
hematoma 3.
head injury[28]
4.Meningitis and
encephalitis
5. Horner
syndrome[29]
6.Hypoglycemia
7.COPD
8.Diabetic
9.Ketoacidosis
10.Hyponatremia
11Hypernatremia
12Hypercalcemia
13.anterior
uveitis,(eye)
Urine and
Serum
Toxicology
screening to
detect opiates
immunoassays
.[30]. Blood
Gases
Blood Sugar
Routine Blood
Tests, ECG
Chest X Ray
CT Brain
Naloxone adult
dose is 0.4 to 2
mg IV, IM, or
subcutaneously,
up may be
repeated every 2–
3 minutes to a
total dose of
10 mg. [31]
poisons clinical features Non Posisonous
D/D
Investigation
s
Treatment /
Antidote
Cholinergics
(Organophosphate
pesticides,
Carbamates)
Diarrohea,Urination
Miosis,Bradycardia,
Bronchorrhea,
Bronchospasm,
Emesis,Lacrimation,
Lethargy,Salivation.
hypoglycaemia,
thyroid storm,
sympathetic
hyperactivity,
neuroleptic
malignant
syndrome.
a.decreased
cholinesterase
activity in
cholinergics.
[27]. b.Blood
sugar.
c.Thyroid
Function
Tests. c. all
the routine
blood
investigations.
Atropine 1–2 mg
every 2–3 mins,
until there is
drying of
secretions
Pralidoxime (2-
PAM) 70 mg/kg
IV then infusion
at 500 mg/h
Opiods
(morphine,
methadone,
buprenorphine,
hydrocodone,
and oxycodone
and Heroin
Coma ,respiratory
depression,
hypotension,
bradycardia,
hypothermia
decreased bowel
sounds ,urinary
retention, localized
urticaria and
seizures in
propoxyphene
overdose
1.Pontine
Haemorrhage
2.Acute subdural
hematoma 3.
head injury[28]
4.Meningitis and
encephalitis
5. Horner
syndrome[29]
6.Hypoglycemia
7.COPD
8.Diabetic
9.Ketoacidosis
10.Hyponatremia
11Hypernatremia
12Hypercalcemia
13.anterior
uveitis,(eye)
Urine and
Serum
Toxicology
screening to
detect opiates
immunoassays
.[30]. Blood
Gases
Blood Sugar
Routine Blood
Tests, ECG
Chest X Ray
CT Brain
Naloxone adult
dose is 0.4 to 2
mg IV, IM, or
subcutaneously,
up may be
repeated every 2–
3 minutes to a
total dose of
10 mg. [31]
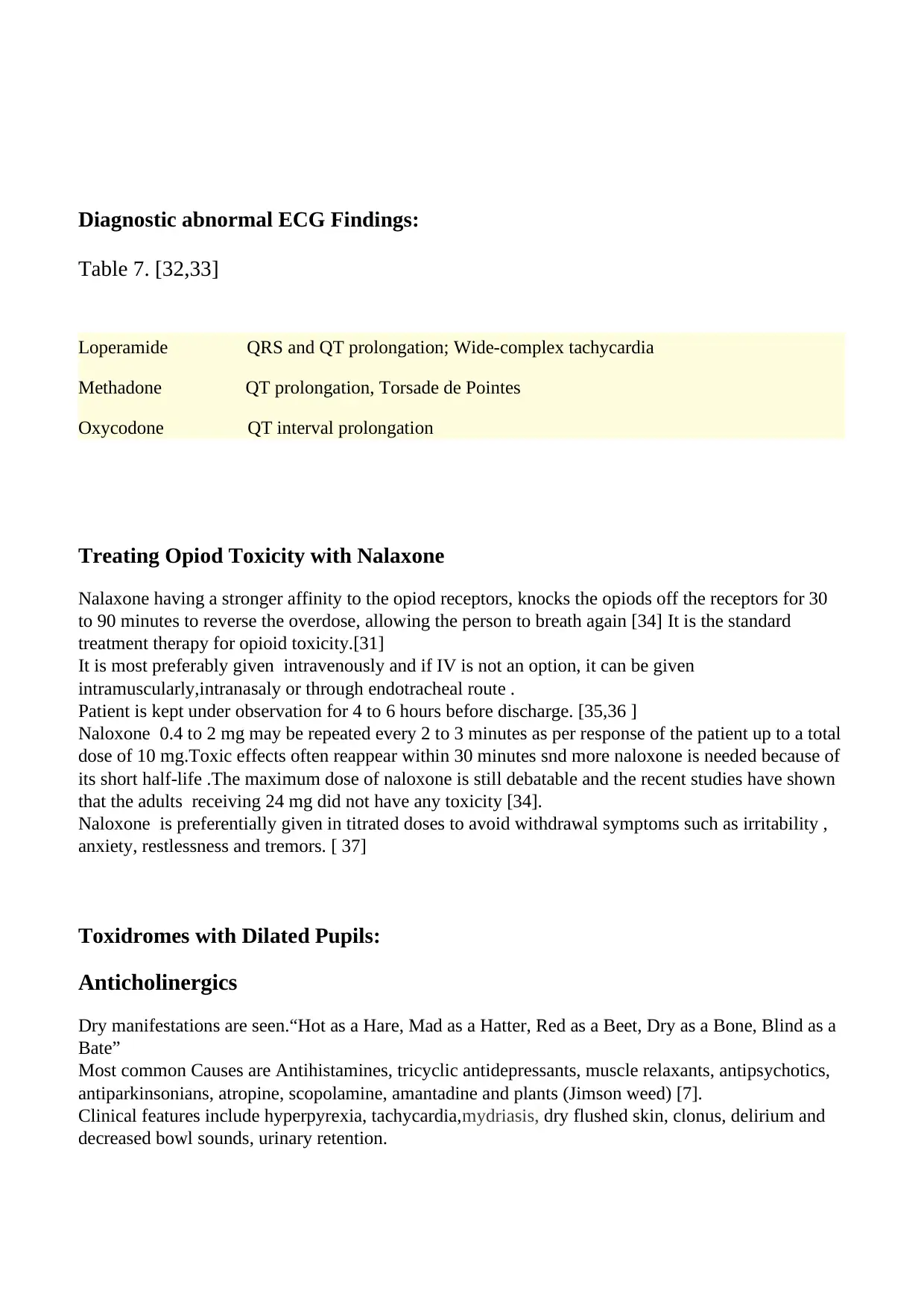
Diagnostic abnormal ECG Findings:
Table 7. [32,33]
Loperamide QRS and QT prolongation; Wide-complex tachycardia
Methadone QT prolongation, Torsade de Pointes
Oxycodone QT interval prolongation
Treating Opiod Toxicity with Nalaxone
Nalaxone having a stronger affinity to the opiod receptors, knocks the opiods off the receptors for 30
to 90 minutes to reverse the overdose, allowing the person to breath again [34] It is the standard
treatment therapy for opioid toxicity.[31]
It is most preferably given intravenously and if IV is not an option, it can be given
intramuscularly,intranasaly or through endotracheal route .
Patient is kept under observation for 4 to 6 hours before discharge. [35,36 ]
Naloxone 0.4 to 2 mg may be repeated every 2 to 3 minutes as per response of the patient up to a total
dose of 10 mg.Toxic effects often reappear within 30 minutes snd more naloxone is needed because of
its short half-life .The maximum dose of naloxone is still debatable and the recent studies have shown
that the adults receiving 24 mg did not have any toxicity [34].
Naloxone is preferentially given in titrated doses to avoid withdrawal symptoms such as irritability ,
anxiety, restlessness and tremors. [ 37]
Toxidromes with Dilated Pupils:
Anticholinergics
Dry manifestations are seen.“Hot as a Hare, Mad as a Hatter, Red as a Beet, Dry as a Bone, Blind as a
Bate”
Most common Causes are Antihistamines, tricyclic antidepressants, muscle relaxants, antipsychotics,
antiparkinsonians, atropine, scopolamine, amantadine and plants (Jimson weed) [7].
Clinical features include hyperpyrexia, tachycardia,mydriasis, dry flushed skin, clonus, delirium and
decreased bowl sounds, urinary retention.
Table 7. [32,33]
Loperamide QRS and QT prolongation; Wide-complex tachycardia
Methadone QT prolongation, Torsade de Pointes
Oxycodone QT interval prolongation
Treating Opiod Toxicity with Nalaxone
Nalaxone having a stronger affinity to the opiod receptors, knocks the opiods off the receptors for 30
to 90 minutes to reverse the overdose, allowing the person to breath again [34] It is the standard
treatment therapy for opioid toxicity.[31]
It is most preferably given intravenously and if IV is not an option, it can be given
intramuscularly,intranasaly or through endotracheal route .
Patient is kept under observation for 4 to 6 hours before discharge. [35,36 ]
Naloxone 0.4 to 2 mg may be repeated every 2 to 3 minutes as per response of the patient up to a total
dose of 10 mg.Toxic effects often reappear within 30 minutes snd more naloxone is needed because of
its short half-life .The maximum dose of naloxone is still debatable and the recent studies have shown
that the adults receiving 24 mg did not have any toxicity [34].
Naloxone is preferentially given in titrated doses to avoid withdrawal symptoms such as irritability ,
anxiety, restlessness and tremors. [ 37]
Toxidromes with Dilated Pupils:
Anticholinergics
Dry manifestations are seen.“Hot as a Hare, Mad as a Hatter, Red as a Beet, Dry as a Bone, Blind as a
Bate”
Most common Causes are Antihistamines, tricyclic antidepressants, muscle relaxants, antipsychotics,
antiparkinsonians, atropine, scopolamine, amantadine and plants (Jimson weed) [7].
Clinical features include hyperpyrexia, tachycardia,mydriasis, dry flushed skin, clonus, delirium and
decreased bowl sounds, urinary retention.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





