Integrated Care Plan: Diabetes Patient Case Study, University Report
VerifiedAdded on 2021/04/16
|12
|4018
|84
Report
AI Summary
This report presents an integrated care plan for a 65-year-old female patient with a 20-year history of diabetes, admitted with severe glycemic shock, breathing difficulties, and back pain. The patient's case includes cardiac blockage, obesity, hypertension, and clinical depression. The care plan addresses glycemic shock, medication administration, heart blockage, and depression. It emphasizes patient education, including family involvement for home care and fall prevention. The plan outlines objective data from assessments, nursing diagnoses, goals, and implementation strategies, focusing on blood glucose management, medication, lifestyle modifications, and psychosocial support. The report highlights the importance of a holistic approach, considering the patient's physical, psychological, and social needs, and the need for continuous monitoring and adjustments to the care plan.

Running head: INTEGRATED CARE PLAN
Integrated Care Plan
Name of the student
University name
Author’s note
Integrated Care Plan
Name of the student
University name
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
INTEGRATED CARE PLAN
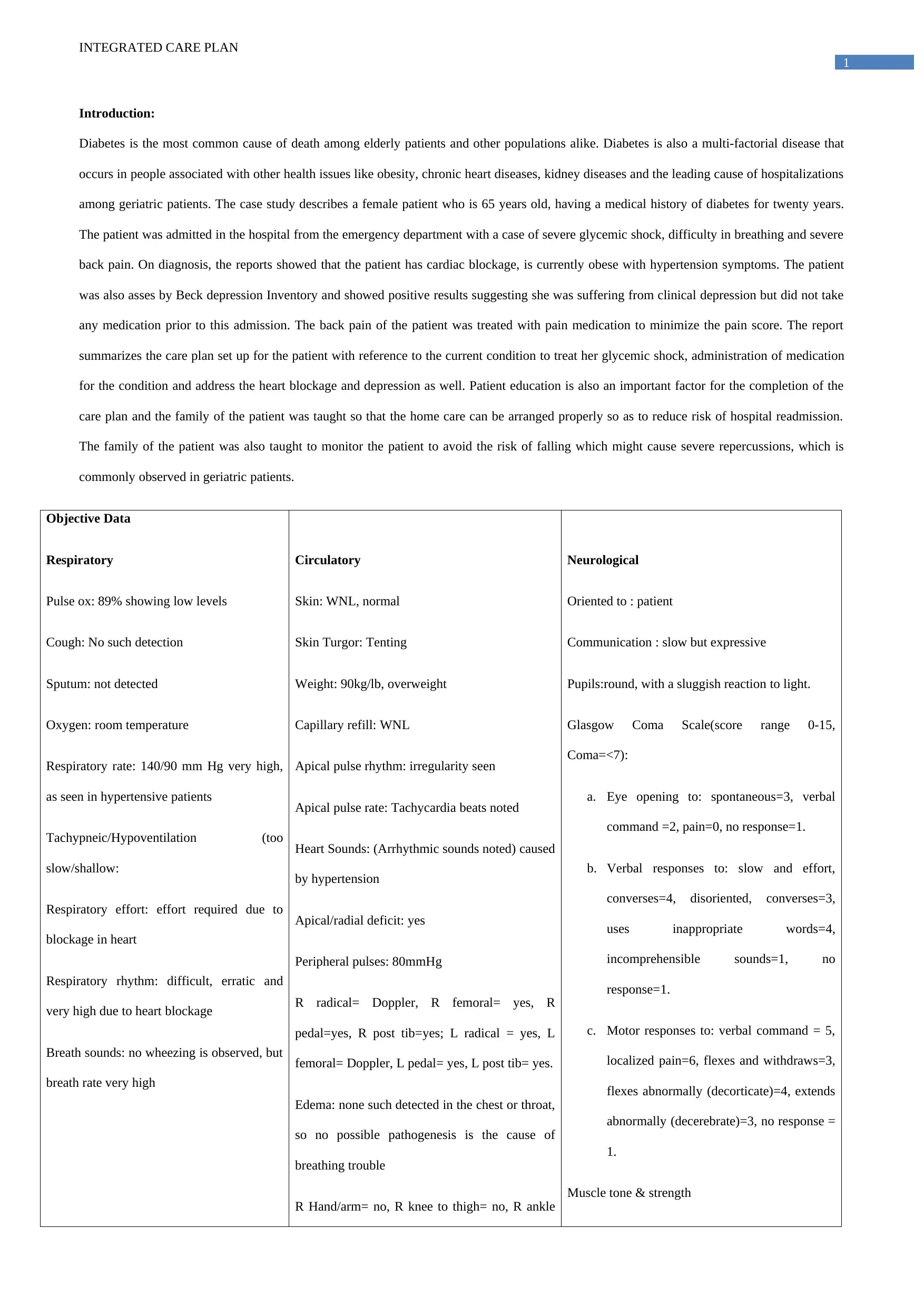
Introduction:
Diabetes is the most common cause of death among elderly patients and other populations alike. Diabetes is also a multi-factorial disease that
occurs in people associated with other health issues like obesity, chronic heart diseases, kidney diseases and the leading cause of hospitalizations
among geriatric patients. The case study describes a female patient who is 65 years old, having a medical history of diabetes for twenty years.
The patient was admitted in the hospital from the emergency department with a case of severe glycemic shock, difficulty in breathing and severe
back pain. On diagnosis, the reports showed that the patient has cardiac blockage, is currently obese with hypertension symptoms. The patient
was also asses by Beck depression Inventory and showed positive results suggesting she was suffering from clinical depression but did not take
any medication prior to this admission. The back pain of the patient was treated with pain medication to minimize the pain score. The report
summarizes the care plan set up for the patient with reference to the current condition to treat her glycemic shock, administration of medication
for the condition and address the heart blockage and depression as well. Patient education is also an important factor for the completion of the
care plan and the family of the patient was taught so that the home care can be arranged properly so as to reduce risk of hospital readmission.
The family of the patient was also taught to monitor the patient to avoid the risk of falling which might cause severe repercussions, which is
commonly observed in geriatric patients.
Objective Data
Respiratory
Pulse ox: 89% showing low levels
Cough: No such detection
Sputum: not detected
Oxygen: room temperature
Respiratory rate: 140/90 mm Hg very high,
as seen in hypertensive patients
Tachypneic/Hypoventilation (too
slow/shallow:
Respiratory effort: effort required due to
blockage in heart
Respiratory rhythm: difficult, erratic and
very high due to heart blockage
Breath sounds: no wheezing is observed, but
breath rate very high
Circulatory
Skin: WNL, normal
Skin Turgor: Tenting
Weight: 90kg/lb, overweight
Capillary refill: WNL
Apical pulse rhythm: irregularity seen
Apical pulse rate: Tachycardia beats noted
Heart Sounds: (Arrhythmic sounds noted) caused
by hypertension
Apical/radial deficit: yes
Peripheral pulses: 80mmHg
R radical= Doppler, R femoral= yes, R
pedal=yes, R post tib=yes; L radical = yes, L
femoral= Doppler, L pedal= yes, L post tib= yes.
Edema: none such detected in the chest or throat,
so no possible pathogenesis is the cause of
breathing trouble
R Hand/arm= no, R knee to thigh= no, R ankle
Neurological
Oriented to : patient
Communication : slow but expressive
Pupils:round, with a sluggish reaction to light.
Glasgow Coma Scale(score range 0-15,
Coma=<7):
a. Eye opening to: spontaneous=3, verbal
command =2, pain=0, no response=1.
b. Verbal responses to: slow and effort,
converses=4, disoriented, converses=3,
uses inappropriate words=4,
incomprehensible sounds=1, no
response=1.
c. Motor responses to: verbal command = 5,
localized pain=6, flexes and withdraws=3,
flexes abnormally (decorticate)=4, extends
abnormally (decerebrate)=3, no response =
1.
Muscle tone & strength
INTEGRATED CARE PLAN
Introduction:
Diabetes is the most common cause of death among elderly patients and other populations alike. Diabetes is also a multi-factorial disease that
occurs in people associated with other health issues like obesity, chronic heart diseases, kidney diseases and the leading cause of hospitalizations
among geriatric patients. The case study describes a female patient who is 65 years old, having a medical history of diabetes for twenty years.
The patient was admitted in the hospital from the emergency department with a case of severe glycemic shock, difficulty in breathing and severe
back pain. On diagnosis, the reports showed that the patient has cardiac blockage, is currently obese with hypertension symptoms. The patient
was also asses by Beck depression Inventory and showed positive results suggesting she was suffering from clinical depression but did not take
any medication prior to this admission. The back pain of the patient was treated with pain medication to minimize the pain score. The report
summarizes the care plan set up for the patient with reference to the current condition to treat her glycemic shock, administration of medication
for the condition and address the heart blockage and depression as well. Patient education is also an important factor for the completion of the
care plan and the family of the patient was taught so that the home care can be arranged properly so as to reduce risk of hospital readmission.
The family of the patient was also taught to monitor the patient to avoid the risk of falling which might cause severe repercussions, which is
commonly observed in geriatric patients.
Objective Data
Respiratory
Pulse ox: 89% showing low levels
Cough: No such detection
Sputum: not detected
Oxygen: room temperature
Respiratory rate: 140/90 mm Hg very high,
as seen in hypertensive patients
Tachypneic/Hypoventilation (too
slow/shallow:
Respiratory effort: effort required due to
blockage in heart
Respiratory rhythm: difficult, erratic and
very high due to heart blockage
Breath sounds: no wheezing is observed, but
breath rate very high
Circulatory
Skin: WNL, normal
Skin Turgor: Tenting
Weight: 90kg/lb, overweight
Capillary refill: WNL
Apical pulse rhythm: irregularity seen
Apical pulse rate: Tachycardia beats noted
Heart Sounds: (Arrhythmic sounds noted) caused
by hypertension
Apical/radial deficit: yes
Peripheral pulses: 80mmHg
R radical= Doppler, R femoral= yes, R
pedal=yes, R post tib=yes; L radical = yes, L
femoral= Doppler, L pedal= yes, L post tib= yes.
Edema: none such detected in the chest or throat,
so no possible pathogenesis is the cause of
breathing trouble
R Hand/arm= no, R knee to thigh= no, R ankle
Neurological
Oriented to : patient
Communication : slow but expressive
Pupils:round, with a sluggish reaction to light.
Glasgow Coma Scale(score range 0-15,
Coma=<7):
a. Eye opening to: spontaneous=3, verbal
command =2, pain=0, no response=1.
b. Verbal responses to: slow and effort,
converses=4, disoriented, converses=3,
uses inappropriate words=4,
incomprehensible sounds=1, no
response=1.
c. Motor responses to: verbal command = 5,
localized pain=6, flexes and withdraws=3,
flexes abnormally (decorticate)=4, extends
abnormally (decerebrate)=3, no response =
1.
Muscle tone & strength
2
INTEGRATED CARE PLAN
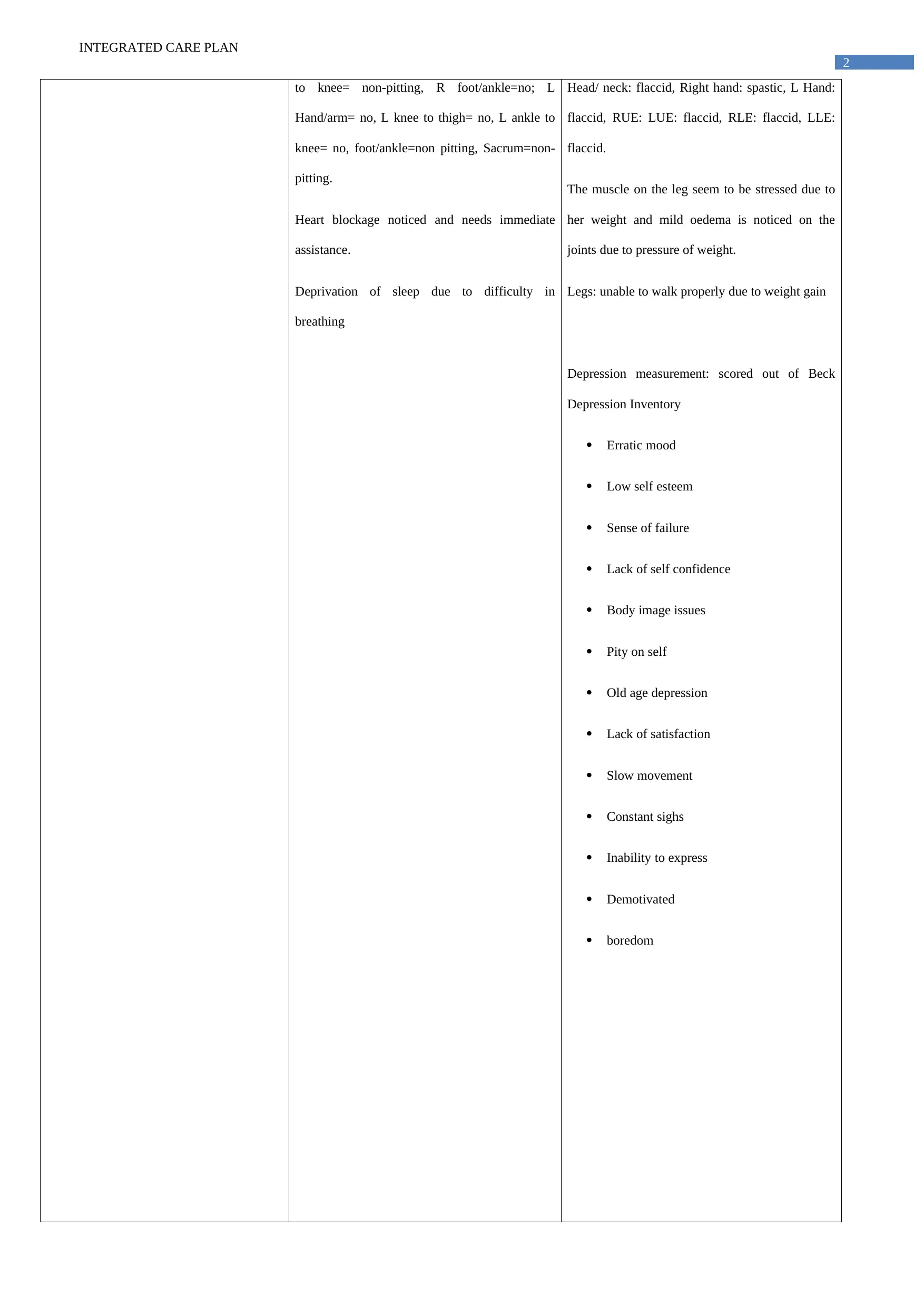
to knee= non-pitting, R foot/ankle=no; L
Hand/arm= no, L knee to thigh= no, L ankle to
knee= no, foot/ankle=non pitting, Sacrum=non-
pitting.
Heart blockage noticed and needs immediate
assistance.
Deprivation of sleep due to difficulty in
breathing
Head/ neck: flaccid, Right hand: spastic, L Hand:
flaccid, RUE: LUE: flaccid, RLE: flaccid, LLE:
flaccid.
The muscle on the leg seem to be stressed due to
her weight and mild oedema is noticed on the
joints due to pressure of weight.
Legs: unable to walk properly due to weight gain
Depression measurement: scored out of Beck
Depression Inventory
Erratic mood
Low self esteem
Sense of failure
Lack of self confidence
Body image issues
Pity on self
Old age depression
Lack of satisfaction
Slow movement
Constant sighs
Inability to express
Demotivated
boredom
INTEGRATED CARE PLAN
to knee= non-pitting, R foot/ankle=no; L
Hand/arm= no, L knee to thigh= no, L ankle to
knee= no, foot/ankle=non pitting, Sacrum=non-
pitting.
Heart blockage noticed and needs immediate
assistance.
Deprivation of sleep due to difficulty in
breathing
Head/ neck: flaccid, Right hand: spastic, L Hand:
flaccid, RUE: LUE: flaccid, RLE: flaccid, LLE:
flaccid.
The muscle on the leg seem to be stressed due to
her weight and mild oedema is noticed on the
joints due to pressure of weight.
Legs: unable to walk properly due to weight gain
Depression measurement: scored out of Beck
Depression Inventory
Erratic mood
Low self esteem
Sense of failure
Lack of self confidence
Body image issues
Pity on self
Old age depression
Lack of satisfaction
Slow movement
Constant sighs
Inability to express
Demotivated
boredom
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
INTEGRATED CARE PLAN
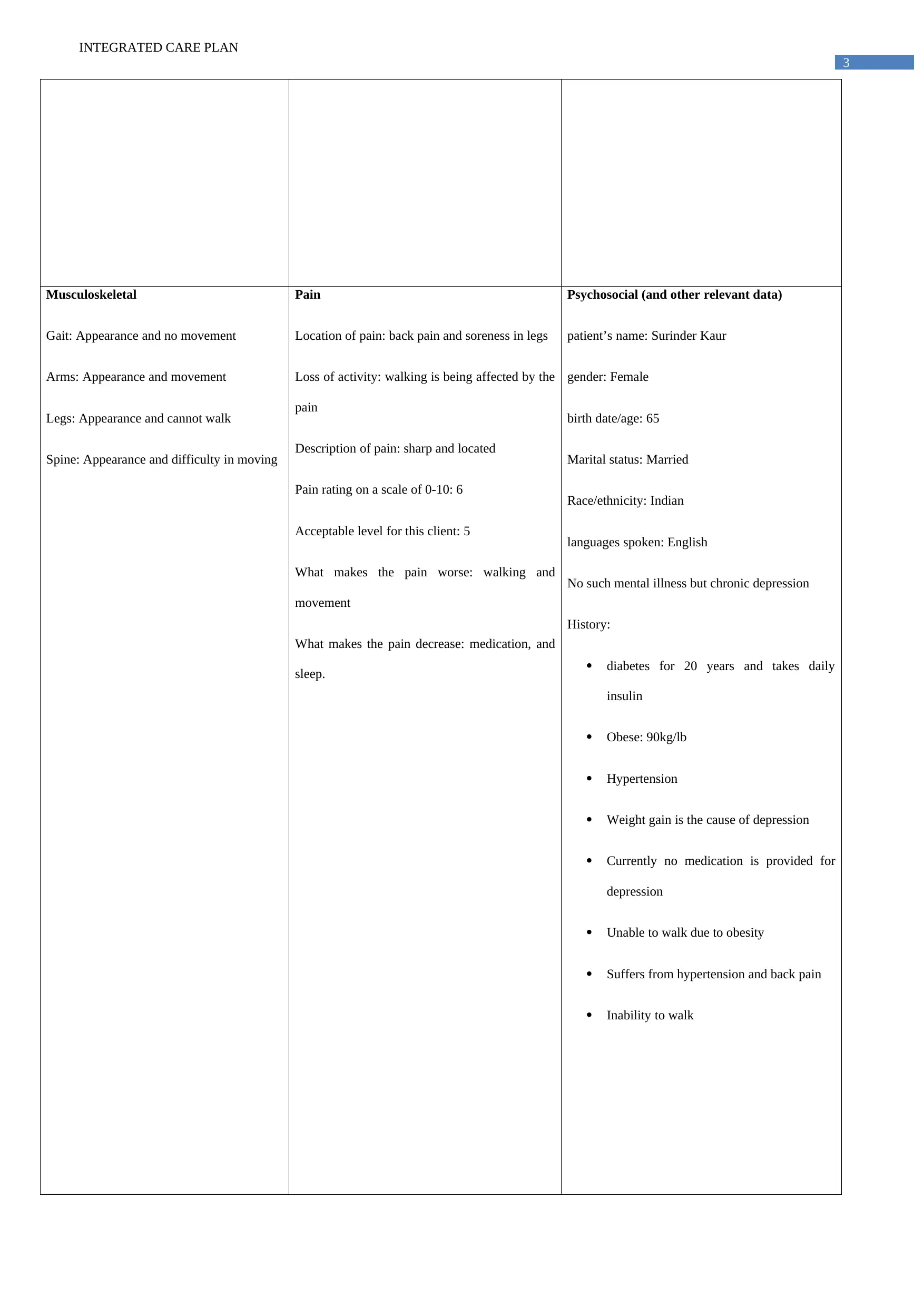
Musculoskeletal
Gait: Appearance and no movement
Arms: Appearance and movement
Legs: Appearance and cannot walk
Spine: Appearance and difficulty in moving
Pain
Location of pain: back pain and soreness in legs
Loss of activity: walking is being affected by the
pain
Description of pain: sharp and located
Pain rating on a scale of 0-10: 6
Acceptable level for this client: 5
What makes the pain worse: walking and
movement
What makes the pain decrease: medication, and
sleep.
Psychosocial (and other relevant data)
patient’s name: Surinder Kaur
gender: Female
birth date/age: 65
Marital status: Married
Race/ethnicity: Indian
languages spoken: English
No such mental illness but chronic depression
History:
diabetes for 20 years and takes daily
insulin
Obese: 90kg/lb
Hypertension
Weight gain is the cause of depression
Currently no medication is provided for
depression
Unable to walk due to obesity
Suffers from hypertension and back pain
Inability to walk
INTEGRATED CARE PLAN
Musculoskeletal
Gait: Appearance and no movement
Arms: Appearance and movement
Legs: Appearance and cannot walk
Spine: Appearance and difficulty in moving
Pain
Location of pain: back pain and soreness in legs
Loss of activity: walking is being affected by the
pain
Description of pain: sharp and located
Pain rating on a scale of 0-10: 6
Acceptable level for this client: 5
What makes the pain worse: walking and
movement
What makes the pain decrease: medication, and
sleep.
Psychosocial (and other relevant data)
patient’s name: Surinder Kaur
gender: Female
birth date/age: 65
Marital status: Married
Race/ethnicity: Indian
languages spoken: English
No such mental illness but chronic depression
History:
diabetes for 20 years and takes daily
insulin
Obese: 90kg/lb
Hypertension
Weight gain is the cause of depression
Currently no medication is provided for
depression
Unable to walk due to obesity
Suffers from hypertension and back pain
Inability to walk
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4
INTEGRATED CARE PLAN
INTEGRATED CARE PLAN
5
INTEGRATED CARE PLAN
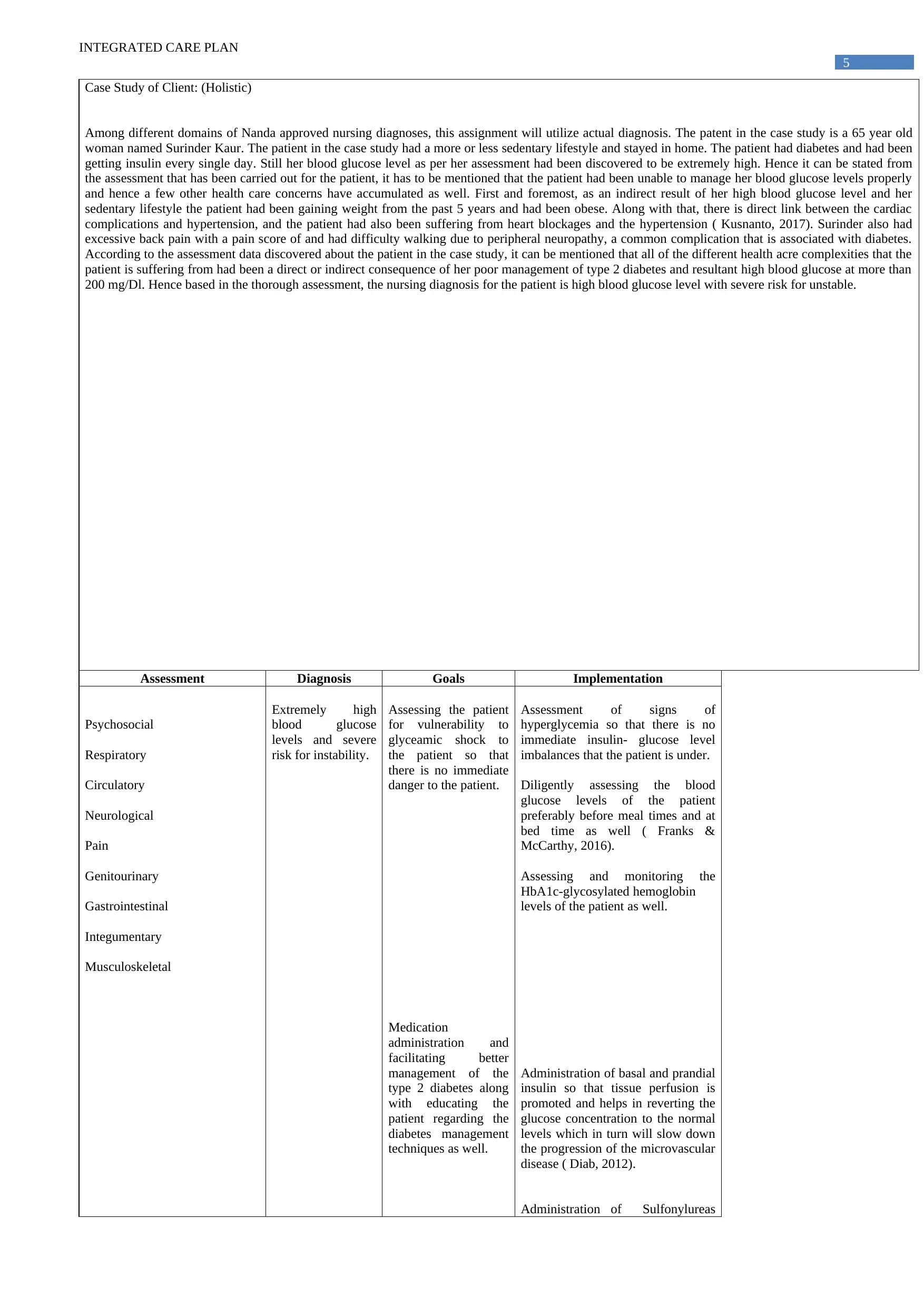
Case Study of Client: (Holistic)
Among different domains of Nanda approved nursing diagnoses, this assignment will utilize actual diagnosis. The patent in the case study is a 65 year old
woman named Surinder Kaur. The patient in the case study had a more or less sedentary lifestyle and stayed in home. The patient had diabetes and had been
getting insulin every single day. Still her blood glucose level as per her assessment had been discovered to be extremely high. Hence it can be stated from
the assessment that has been carried out for the patient, it has to be mentioned that the patient had been unable to manage her blood glucose levels properly
and hence a few other health care concerns have accumulated as well. First and foremost, as an indirect result of her high blood glucose level and her
sedentary lifestyle the patient had been gaining weight from the past 5 years and had been obese. Along with that, there is direct link between the cardiac
complications and hypertension, and the patient had also been suffering from heart blockages and the hypertension ( Kusnanto, 2017). Surinder also had
excessive back pain with a pain score of and had difficulty walking due to peripheral neuropathy, a common complication that is associated with diabetes.
According to the assessment data discovered about the patient in the case study, it can be mentioned that all of the different health acre complexities that the
patient is suffering from had been a direct or indirect consequence of her poor management of type 2 diabetes and resultant high blood glucose at more than
200 mg/Dl. Hence based in the thorough assessment, the nursing diagnosis for the patient is high blood glucose level with severe risk for unstable.
Assessment Diagnosis Goals Implementation
Psychosocial
Respiratory
Circulatory
Neurological
Pain
Genitourinary
Gastrointestinal
Integumentary
Musculoskeletal
Extremely high
blood glucose
levels and severe
risk for instability.
Assessing the patient
for vulnerability to
glyceamic shock to
the patient so that
there is no immediate
danger to the patient.
Medication
administration and
facilitating better
management of the
type 2 diabetes along
with educating the
patient regarding the
diabetes management
techniques as well.
Assessment of signs of
hyperglycemia so that there is no
immediate insulin- glucose level
imbalances that the patient is under.
Diligently assessing the blood
glucose levels of the patient
preferably before meal times and at
bed time as well ( Franks &
McCarthy, 2016).
Assessing and monitoring the
HbA1c-glycosylated hemoglobin
levels of the patient as well.
Administration of basal and prandial
insulin so that tissue perfusion is
promoted and helps in reverting the
glucose concentration to the normal
levels which in turn will slow down
the progression of the microvascular
disease ( Diab, 2012).
Administration of Sulfonylureas
INTEGRATED CARE PLAN
Case Study of Client: (Holistic)
Among different domains of Nanda approved nursing diagnoses, this assignment will utilize actual diagnosis. The patent in the case study is a 65 year old
woman named Surinder Kaur. The patient in the case study had a more or less sedentary lifestyle and stayed in home. The patient had diabetes and had been
getting insulin every single day. Still her blood glucose level as per her assessment had been discovered to be extremely high. Hence it can be stated from
the assessment that has been carried out for the patient, it has to be mentioned that the patient had been unable to manage her blood glucose levels properly
and hence a few other health care concerns have accumulated as well. First and foremost, as an indirect result of her high blood glucose level and her
sedentary lifestyle the patient had been gaining weight from the past 5 years and had been obese. Along with that, there is direct link between the cardiac
complications and hypertension, and the patient had also been suffering from heart blockages and the hypertension ( Kusnanto, 2017). Surinder also had
excessive back pain with a pain score of and had difficulty walking due to peripheral neuropathy, a common complication that is associated with diabetes.
According to the assessment data discovered about the patient in the case study, it can be mentioned that all of the different health acre complexities that the
patient is suffering from had been a direct or indirect consequence of her poor management of type 2 diabetes and resultant high blood glucose at more than
200 mg/Dl. Hence based in the thorough assessment, the nursing diagnosis for the patient is high blood glucose level with severe risk for unstable.
Assessment Diagnosis Goals Implementation
Psychosocial
Respiratory
Circulatory
Neurological
Pain
Genitourinary
Gastrointestinal
Integumentary
Musculoskeletal
Extremely high
blood glucose
levels and severe
risk for instability.
Assessing the patient
for vulnerability to
glyceamic shock to
the patient so that
there is no immediate
danger to the patient.
Medication
administration and
facilitating better
management of the
type 2 diabetes along
with educating the
patient regarding the
diabetes management
techniques as well.
Assessment of signs of
hyperglycemia so that there is no
immediate insulin- glucose level
imbalances that the patient is under.
Diligently assessing the blood
glucose levels of the patient
preferably before meal times and at
bed time as well ( Franks &
McCarthy, 2016).
Assessing and monitoring the
HbA1c-glycosylated hemoglobin
levels of the patient as well.
Administration of basal and prandial
insulin so that tissue perfusion is
promoted and helps in reverting the
glucose concentration to the normal
levels which in turn will slow down
the progression of the microvascular
disease ( Diab, 2012).
Administration of Sulfonylureas
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
INTEGRATED CARE PLAN
Encouraging the
patient to adopt a
healthier life style by
starting to eat healthy
and maintaining a
strict dietary plan with
a strict yet attainable
physical exercise
regimen.
like
Glucotrol and Diabeta, meglitinides
like Prandin, Biguanides like
metformin, Phenylalanine
derivatives lie starlix, alpha glucose
inhibitors like the acarbose and
miglitol, thiazolinidiones like actos
and avandia and lastly Incretin
modifiers like sitagliptin. The
medication will decrease insulin
resistance, increase insulin
production and will delay the
absorption of glucose into the blood
( Paschou & Leslie, 2013).
Monitoring the hypertension of the
patient and administer hypertensive
drugs as prescribed to the patient
which will help in reducing the high
blood pressure of the patent and will
also work to reducing the risk for
strokes. Educating the patient on
how to monitor blood glucose on her
own using the blood glucose meters
(Modic et al., 2012).
Encouraging the patient to develop a
healthier lifestyle that includes both
dietary changes and active and
determined fitness initiative.
Engaging in a therapeutic casual
conversation with the patient with a
cultural liaison assistance to extract
information regarding her sedentary
lifestyle and diet pattern ( Wexler et
al., 2012).
Consultation with a dietician for her
to help her develop a diet plan that
will sit her nutritional requirements
along with facilitating eight loss and
cholesterol concentration drop.
Encouraging the patient to eat less
junk food and maintain a protein
rich and antioxidant rich diet plan
with lesser carbohydrate and fat
content ( Juul et al., 2012).
Educating the patient with
interactive and cognitive therapeutic
intervention towards changing her
health behaviors towards a
promotional health behavior for
diabetes control. Enhancing the
health literacy of the patient
regarding diabetes and the
associated co- occurring disorders so
that she can work towards managing
or preventing it. Lastly, encouraging
and helping the patient to begin with
mild and least tiresome exercise
regimen to help her build her
tolerance towards physical exercise.
As the patient is accustomed to
physical exercise help the patient
build towards more tiresome and
effective exercise patterns that are
targeted at quick weight loss
( Spanakis & Chiarugi, 2011).
INTEGRATED CARE PLAN
Encouraging the
patient to adopt a
healthier life style by
starting to eat healthy
and maintaining a
strict dietary plan with
a strict yet attainable
physical exercise
regimen.
like
Glucotrol and Diabeta, meglitinides
like Prandin, Biguanides like
metformin, Phenylalanine
derivatives lie starlix, alpha glucose
inhibitors like the acarbose and
miglitol, thiazolinidiones like actos
and avandia and lastly Incretin
modifiers like sitagliptin. The
medication will decrease insulin
resistance, increase insulin
production and will delay the
absorption of glucose into the blood
( Paschou & Leslie, 2013).
Monitoring the hypertension of the
patient and administer hypertensive
drugs as prescribed to the patient
which will help in reducing the high
blood pressure of the patent and will
also work to reducing the risk for
strokes. Educating the patient on
how to monitor blood glucose on her
own using the blood glucose meters
(Modic et al., 2012).
Encouraging the patient to develop a
healthier lifestyle that includes both
dietary changes and active and
determined fitness initiative.
Engaging in a therapeutic casual
conversation with the patient with a
cultural liaison assistance to extract
information regarding her sedentary
lifestyle and diet pattern ( Wexler et
al., 2012).
Consultation with a dietician for her
to help her develop a diet plan that
will sit her nutritional requirements
along with facilitating eight loss and
cholesterol concentration drop.
Encouraging the patient to eat less
junk food and maintain a protein
rich and antioxidant rich diet plan
with lesser carbohydrate and fat
content ( Juul et al., 2012).
Educating the patient with
interactive and cognitive therapeutic
intervention towards changing her
health behaviors towards a
promotional health behavior for
diabetes control. Enhancing the
health literacy of the patient
regarding diabetes and the
associated co- occurring disorders so
that she can work towards managing
or preventing it. Lastly, encouraging
and helping the patient to begin with
mild and least tiresome exercise
regimen to help her build her
tolerance towards physical exercise.
As the patient is accustomed to
physical exercise help the patient
build towards more tiresome and
effective exercise patterns that are
targeted at quick weight loss
( Spanakis & Chiarugi, 2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
INTEGRATED CARE PLAN
3. The current case study here focuses upon the Surinder Kaur who is a 65 years old woman and suffering from a number of co-morbid health
conditions. She is suffering from hypertension along with back pain; hear blockage and diabetes; depression and weight gain. She had been
talking insulin for the past 20 years. In this respect, a care plan could be made for the patient based upon the North American nursing diagnosis
association (NANDA). The NANDA diagnosis could be divided into following four types such as actual diagnosis, risks diagnosis, health
promotion diagnosis and syndrome diagnosis. In this respect, the actual diagnosis has been taken into consideration where the present health
responses shown by the patient are taken into consideration. For the current study, a range of complications depicted by the patient have been
taken into consideration. Out of this, blood glucose monitoring have been taken onto consideration for the current study. The patient her had
been suffering from type 2 diabetes and had been taking insulin for the past five years. As mentioned by Rosenberg et al. (2014), excessive dose
of insulin can often lead to the deposition of body fat. Some of these have been seen to contribute to the worsening of already existent clinical
condition in the patient. As the patient has heart blockage the presence of obesity could further worsen the condition. As mentioned by Jindal et
al. (2017), obesity has been linked with high blood cholesterol levels. Some of these conditions restricted the life processes of the patient. This
further developed depressive thoughts or feelings within the patient. However, one of the most important clinical conditions which were
expressed within the patient and needed immediate clinical intervention are monitoring of high levels of blood glucose level. Therefore, the
high levels of blood glucose level could lead to fatal consequences where the patient could develop glycaemia shocks. The hyperglycaemia
could be associated with a range of symptomatic expressions, which could dishevel the normal life of the patients. Some of these are –excessive
urination, excessive thirst, weight gain, diabetic neuropathy and diabetic retinopathy. As mentioned by Ng, Finnigan, Connellan, Kiernan &
Coward (2014), high levels of blood glucose can lead to a condition of nerve damage known as diabetic neuropathy. The diabetic neuropathy
can have much serious consequences such as development of leg amputations in the patient. The leg amputations can disrupt the normal day to
day movement making the patient dependent upon medication and aid. In this stage, additional level of support and care is required for the
patient. Hence, the patient looses autonomy over their activities of daily living (ADL) which could further aggaravate the presence and
expression of depression in the patient. The high blood glucose level has been associated with the development of retinopathy conditions which
INTEGRATED CARE PLAN
3. The current case study here focuses upon the Surinder Kaur who is a 65 years old woman and suffering from a number of co-morbid health
conditions. She is suffering from hypertension along with back pain; hear blockage and diabetes; depression and weight gain. She had been
talking insulin for the past 20 years. In this respect, a care plan could be made for the patient based upon the North American nursing diagnosis
association (NANDA). The NANDA diagnosis could be divided into following four types such as actual diagnosis, risks diagnosis, health
promotion diagnosis and syndrome diagnosis. In this respect, the actual diagnosis has been taken into consideration where the present health
responses shown by the patient are taken into consideration. For the current study, a range of complications depicted by the patient have been
taken into consideration. Out of this, blood glucose monitoring have been taken onto consideration for the current study. The patient her had
been suffering from type 2 diabetes and had been taking insulin for the past five years. As mentioned by Rosenberg et al. (2014), excessive dose
of insulin can often lead to the deposition of body fat. Some of these have been seen to contribute to the worsening of already existent clinical
condition in the patient. As the patient has heart blockage the presence of obesity could further worsen the condition. As mentioned by Jindal et
al. (2017), obesity has been linked with high blood cholesterol levels. Some of these conditions restricted the life processes of the patient. This
further developed depressive thoughts or feelings within the patient. However, one of the most important clinical conditions which were
expressed within the patient and needed immediate clinical intervention are monitoring of high levels of blood glucose level. Therefore, the
high levels of blood glucose level could lead to fatal consequences where the patient could develop glycaemia shocks. The hyperglycaemia
could be associated with a range of symptomatic expressions, which could dishevel the normal life of the patients. Some of these are –excessive
urination, excessive thirst, weight gain, diabetic neuropathy and diabetic retinopathy. As mentioned by Ng, Finnigan, Connellan, Kiernan &
Coward (2014), high levels of blood glucose can lead to a condition of nerve damage known as diabetic neuropathy. The diabetic neuropathy
can have much serious consequences such as development of leg amputations in the patient. The leg amputations can disrupt the normal day to
day movement making the patient dependent upon medication and aid. In this stage, additional level of support and care is required for the
patient. Hence, the patient looses autonomy over their activities of daily living (ADL) which could further aggaravate the presence and
expression of depression in the patient. The high blood glucose level has been associated with the development of retinopathy conditions which

8
INTEGRATED CARE PLAN
can affect the vision in the patient considerably. Therefore, the daily care activities of the patient need to be effectively monitored for the
reduction in the clinical manifestations of the patient.
Further complications
The patient also had hypertension and was suggested regular medications for the control and management of depression. However, the
patient hardly followed the medications pattern and doses. This increased the severity of clinical symptoms such as sleep deprivation in the
patient. Moreover, the patient could not sleep owing to pain which was also aggravated due to psychological reasons ion the patient. Therefore,
in order to control the pain and sleeo deprivation in the patient, the patient was suggested metformin and oxazepam, which could effectively
control the rate of depression within the patient. In the lack of effective medication intake by the patient, she could be struck with lethal
consequences such as myocardial infarction (MI). Therefore, in order to relieve the overall condition of the patient a holistic care regimen could
be developed for the patient (Rossom et al., 2014).
Discussion of interventions
One of the most important nursing interventions and strategies which could be developed for the patient is implementation of physical
exercises. Some of the physical exercises could include light walking, jogging along with light stretching. This could restore the movement and
agility patterns in the patient. Additionally, provision of effective medication to the patient could also help in controlling and monitoring the
blood glucose level. As mentioned by Zhou et al. (2017), provision of fresh food and supplements to the patient can also be effective in
controlling the blood glucose level.
4. The areas which had been highlighted as requiring care management in the above discussion are –blood glucose monitoring and reduction in
the symptomatic expression of several health co-morbidities. This area of care management was highlighted as the patient had expressed a
number of physical abnormalities which impaired the daily life of the patient along with dependence upon insulin. Research and evidences have
proved that too much of dependence upon insulin can impair the functioning of the heart and the patient was already suffering from heart
blockage (Feigenbaum, 2012). Therefore, the patient had to be provided with a balanced care treatment plan which will help in reducing the
daily life grievances of the patient. The focus has to be more upon a holistic care regimen. Additionally, diabetes could also stem unto a number
of major health complications such as movement disability, retinopathy and cardiac shock. Therefore, in order to prevent such conditions from
the disrupting the life of the patient an effective and balanced car plan is required. Additionally, the patient was also suffering from depressions
which affected the rate of recovery of the patient. Hence, providing the patient with a holistic care regimen can help in infusing positive spirit in
the life of the patient which could speed the recovery rate (Plat, 2017). Additionally, provision of effective counselling measures along with
community based development program can also help in reducing the stress in the life of the patient. The community development program can
also motivate Surinder Kaur to lose weight as she was suffering from obesity.
INTEGRATED CARE PLAN
can affect the vision in the patient considerably. Therefore, the daily care activities of the patient need to be effectively monitored for the
reduction in the clinical manifestations of the patient.
Further complications
The patient also had hypertension and was suggested regular medications for the control and management of depression. However, the
patient hardly followed the medications pattern and doses. This increased the severity of clinical symptoms such as sleep deprivation in the
patient. Moreover, the patient could not sleep owing to pain which was also aggravated due to psychological reasons ion the patient. Therefore,
in order to control the pain and sleeo deprivation in the patient, the patient was suggested metformin and oxazepam, which could effectively
control the rate of depression within the patient. In the lack of effective medication intake by the patient, she could be struck with lethal
consequences such as myocardial infarction (MI). Therefore, in order to relieve the overall condition of the patient a holistic care regimen could
be developed for the patient (Rossom et al., 2014).
Discussion of interventions
One of the most important nursing interventions and strategies which could be developed for the patient is implementation of physical
exercises. Some of the physical exercises could include light walking, jogging along with light stretching. This could restore the movement and
agility patterns in the patient. Additionally, provision of effective medication to the patient could also help in controlling and monitoring the
blood glucose level. As mentioned by Zhou et al. (2017), provision of fresh food and supplements to the patient can also be effective in
controlling the blood glucose level.
4. The areas which had been highlighted as requiring care management in the above discussion are –blood glucose monitoring and reduction in
the symptomatic expression of several health co-morbidities. This area of care management was highlighted as the patient had expressed a
number of physical abnormalities which impaired the daily life of the patient along with dependence upon insulin. Research and evidences have
proved that too much of dependence upon insulin can impair the functioning of the heart and the patient was already suffering from heart
blockage (Feigenbaum, 2012). Therefore, the patient had to be provided with a balanced care treatment plan which will help in reducing the
daily life grievances of the patient. The focus has to be more upon a holistic care regimen. Additionally, diabetes could also stem unto a number
of major health complications such as movement disability, retinopathy and cardiac shock. Therefore, in order to prevent such conditions from
the disrupting the life of the patient an effective and balanced car plan is required. Additionally, the patient was also suffering from depressions
which affected the rate of recovery of the patient. Hence, providing the patient with a holistic care regimen can help in infusing positive spirit in
the life of the patient which could speed the recovery rate (Plat, 2017). Additionally, provision of effective counselling measures along with
community based development program can also help in reducing the stress in the life of the patient. The community development program can
also motivate Surinder Kaur to lose weight as she was suffering from obesity.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

9
INTEGRATED CARE PLAN
Conclusion
The above discussion makes it clear that the geriatric patients like Surinder Kaur, need to be closely monitored to avoid rick of glycemic shock.
The care plan organized for the patient needs to holistic providing the medication with the respective rationale. Obesity is an indirect effect of
diabetes, which needs to be controlled from early signs as weight gain had severe repercussions like cardiac blockage, which is very risky. The
patient had also developed depression due to her prolonged illness, which needed to be addressed to help her recover. The glycemic shock was
assessed and nutritive as well as pharmaceutical help was provided to her to minimize further risk leading to fatality. The main criteria of the
care plan was to control the blood glucose level and control weigh gain to reduce her weight to help her improve her blocked heart condition and
improve her ability to walk which she was then facing due to obesity. Obesity and diabetes are correlated with each other and create co-morbid
conditions in geriatric patients. Cases like this require patient education planning after care plan management, which would help minimize the
risk of hospital readmission and falling in these cases. The hypertensive condition clubbed with depression in the patient makes the situation
serious and she needs to be well monitored in even home care facilities to minimize the risk of falling.
INTEGRATED CARE PLAN
Conclusion
The above discussion makes it clear that the geriatric patients like Surinder Kaur, need to be closely monitored to avoid rick of glycemic shock.
The care plan organized for the patient needs to holistic providing the medication with the respective rationale. Obesity is an indirect effect of
diabetes, which needs to be controlled from early signs as weight gain had severe repercussions like cardiac blockage, which is very risky. The
patient had also developed depression due to her prolonged illness, which needed to be addressed to help her recover. The glycemic shock was
assessed and nutritive as well as pharmaceutical help was provided to her to minimize further risk leading to fatality. The main criteria of the
care plan was to control the blood glucose level and control weigh gain to reduce her weight to help her improve her blocked heart condition and
improve her ability to walk which she was then facing due to obesity. Obesity and diabetes are correlated with each other and create co-morbid
conditions in geriatric patients. Cases like this require patient education planning after care plan management, which would help minimize the
risk of hospital readmission and falling in these cases. The hypertensive condition clubbed with depression in the patient makes the situation
serious and she needs to be well monitored in even home care facilities to minimize the risk of falling.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
INTEGRATED CARE PLAN
References
American Diabetes Association. (2015). Standards of medical care in diabetes—2015 abridged for primary care providers. Clinical diabetes: a
publication of the American Diabetes Association, 33(2), 97.
Bray, G. A., & Popkin, B. M. (2014). Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes?: health
be damned! Pour on the sugar. Diabetes care, 37(4), 950-956.
Diab, P. (2012). Communication in diabetes management: overcoming the challenges. Journal of Endocrinology, Metabolism and Diabetes of
South Africa, 17(1), 52-54.
Feigenbaum, K., Brooks, P. G., Chamberlain, C. E., Cochran, E., Adams-McLean, A., Malek, R., & Harlan, D. M. (2012). The Clinical Center’s
Blood Glucose Management Service: A Story in Quality Integrated Care. The Diabetes Educator, 38(2), 194-206.
Franks, P. W., & McCarthy, M. I. (2016). Exposing the exposures responsible for type 2 diabetes and obesity. Science, 354(6308), 69-73.
Jindal, D., Gupta, P., Jha, D., Ajay, V. S., Jacob, P., Mehrotra, K., ... & Prabhakaran, D. (2017). The Development of mWellcare, an mHealth
System for the Integrated Management of Hypertension and Diabetes in Primary Care. Studies in health technology and informatics, 245,
1230.
Juul, L., Maindal, H. T., Frydenberg, M., Kristensen, J. K., & Sandbaek, A. (2012). Quality of type 2 diabetes management in general practice is
associated with involvement of general practice nurses. Primary care diabetes, 6(3), 221-228.
Kusnanto, K. (2017). Self Care Management-holistic Psychospiritual Care on Independence, Glucose Level, and Hba1c of Type 2 Diabetes
Mellitus Patient. Jurnal Ners, 7(2), 99-106.
Modic, M. B., Canfield, C., Kaser, N., Sauvey, R., & Kukla, A. (2012). A diabetes management mentor program: outcomes of a clinical nurse
specialist initiative to empower staff nurses. Clinical Nurse Specialist, 26(5), 263-271.
Ng, S. M., Finnigan, L., Connellan, L., Kiernan, C., & Coward, S. (2014). Improving paediatric diabetes care with the use of an integrated
paediatric electronic diabetes information management system and routine uploading of blood glucose meters and insulin pumps in
outpatient clinics. Archives of disease in childhood, 99(11), 1059-1059.
Paschou, S. A., & Leslie, R. D. (2013). Personalizing guidelines for diabetes management: twilight or dawn of the expert?. BMC
medicine, 11(1), 161.
Plat, L. (2017). Diabetes care pathways and the diabetic convention in 2017. Revue medicale de Bruxelles, 38(4), 347-352.
Rosenberg, D., Lin, E., Peterson, D., Ludman, E., Von Korff, M., & Katon, W. (2014). Integrated medical care management and behavioral risk
factor reduction for multicondition patients: behavioral outcomes of the TEAMcare trial. General hospital psychiatry, 36(2), 129-134.
Rossom, R. C., Solberg, L. I., Magnan, S., Crain, A. L., Beck, A., Coleman, K. J., ... & Whitebird, R. (2017). Impact of a national collaborative
care initiative for patients with depression and diabetes or cardiovascular disease. Focus, 15(3), 324-332.
Spanakis, E. G., & Chiarugi, F. (2011, October). Diabetes management: Devices, ICT technologies and future perspectives. In International
Conference on Wireless Mobile Communication and Healthcare (pp. 197-202). Springer, Berlin, Heidelberg.
INTEGRATED CARE PLAN
References
American Diabetes Association. (2015). Standards of medical care in diabetes—2015 abridged for primary care providers. Clinical diabetes: a
publication of the American Diabetes Association, 33(2), 97.
Bray, G. A., & Popkin, B. M. (2014). Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes?: health
be damned! Pour on the sugar. Diabetes care, 37(4), 950-956.
Diab, P. (2012). Communication in diabetes management: overcoming the challenges. Journal of Endocrinology, Metabolism and Diabetes of
South Africa, 17(1), 52-54.
Feigenbaum, K., Brooks, P. G., Chamberlain, C. E., Cochran, E., Adams-McLean, A., Malek, R., & Harlan, D. M. (2012). The Clinical Center’s
Blood Glucose Management Service: A Story in Quality Integrated Care. The Diabetes Educator, 38(2), 194-206.
Franks, P. W., & McCarthy, M. I. (2016). Exposing the exposures responsible for type 2 diabetes and obesity. Science, 354(6308), 69-73.
Jindal, D., Gupta, P., Jha, D., Ajay, V. S., Jacob, P., Mehrotra, K., ... & Prabhakaran, D. (2017). The Development of mWellcare, an mHealth
System for the Integrated Management of Hypertension and Diabetes in Primary Care. Studies in health technology and informatics, 245,
1230.
Juul, L., Maindal, H. T., Frydenberg, M., Kristensen, J. K., & Sandbaek, A. (2012). Quality of type 2 diabetes management in general practice is
associated with involvement of general practice nurses. Primary care diabetes, 6(3), 221-228.
Kusnanto, K. (2017). Self Care Management-holistic Psychospiritual Care on Independence, Glucose Level, and Hba1c of Type 2 Diabetes
Mellitus Patient. Jurnal Ners, 7(2), 99-106.
Modic, M. B., Canfield, C., Kaser, N., Sauvey, R., & Kukla, A. (2012). A diabetes management mentor program: outcomes of a clinical nurse
specialist initiative to empower staff nurses. Clinical Nurse Specialist, 26(5), 263-271.
Ng, S. M., Finnigan, L., Connellan, L., Kiernan, C., & Coward, S. (2014). Improving paediatric diabetes care with the use of an integrated
paediatric electronic diabetes information management system and routine uploading of blood glucose meters and insulin pumps in
outpatient clinics. Archives of disease in childhood, 99(11), 1059-1059.
Paschou, S. A., & Leslie, R. D. (2013). Personalizing guidelines for diabetes management: twilight or dawn of the expert?. BMC
medicine, 11(1), 161.
Plat, L. (2017). Diabetes care pathways and the diabetic convention in 2017. Revue medicale de Bruxelles, 38(4), 347-352.
Rosenberg, D., Lin, E., Peterson, D., Ludman, E., Von Korff, M., & Katon, W. (2014). Integrated medical care management and behavioral risk
factor reduction for multicondition patients: behavioral outcomes of the TEAMcare trial. General hospital psychiatry, 36(2), 129-134.
Rossom, R. C., Solberg, L. I., Magnan, S., Crain, A. L., Beck, A., Coleman, K. J., ... & Whitebird, R. (2017). Impact of a national collaborative
care initiative for patients with depression and diabetes or cardiovascular disease. Focus, 15(3), 324-332.
Spanakis, E. G., & Chiarugi, F. (2011, October). Diabetes management: Devices, ICT technologies and future perspectives. In International
Conference on Wireless Mobile Communication and Healthcare (pp. 197-202). Springer, Berlin, Heidelberg.
11
INTEGRATED CARE PLAN
Wexler, D. J., Beauharnais, C. C., Regan, S., Nathan, D. M., Cagliero, E., & Larkin, M. E. (2012). Impact of inpatient diabetes management,
education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes research and clinical
practice, 98(2), 249-256.
Zhou, H., Zhu, J., Liu, L., Li, F., Fish, A. F., Chen, T., & Lou, Q. (2017). Diabetes-related distress and its associated factors among patients with
type 2 diabetes mellitus in China. Psychiatry research, 252, 45-50.
INTEGRATED CARE PLAN
Wexler, D. J., Beauharnais, C. C., Regan, S., Nathan, D. M., Cagliero, E., & Larkin, M. E. (2012). Impact of inpatient diabetes management,
education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes research and clinical
practice, 98(2), 249-256.
Zhou, H., Zhu, J., Liu, L., Li, F., Fish, A. F., Chen, T., & Lou, Q. (2017). Diabetes-related distress and its associated factors among patients with
type 2 diabetes mellitus in China. Psychiatry research, 252, 45-50.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
