Supporting Individual Journeys in Integrated Health and Social Care
VerifiedAdded on 2020/10/22
|16
|5917
|324
Report
AI Summary
This report delves into the realm of integrated health and social care, focusing on supporting individuals on their healthcare journeys. It begins by examining local provisions and resources that facilitate integrated care working, highlighting the importance of multidisciplinary teams and system leadership. The report then identifies current unmet needs within the community, particularly concerning mental health services, and emphasizes the significance of person-centered care plans in identifying individual needs. The role of healthcare practitioners in promoting person-centered care is discussed, alongside the responsibilities of information sharing between multidisciplinary teams. The report also explores different communication methods and strategies to support diverse service users, including those with mental health issues. Through case studies and analysis, the report underscores the importance of integrated care in improving the quality of life for individuals with complex needs and highlights the essential role of effective communication and teamwork in delivering comprehensive healthcare.

Supporting the Individual
Journey through Integrated
Health and Social Care
Journey through Integrated
Health and Social Care
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INTRODUCTION...........................................................................................................................2
TASK 1............................................................................................................................................2
P1. Local provision and resources which supports integrated care working...............................2
P2. Current local unmet need related to health, care and support service...................................4
M1................................................................................................................................................5
TASK 2 ...........................................................................................................................................5
P3. Support to individual in a health, care service to identify their own care needs with the
help of care plan...........................................................................................................................5
M2................................................................................................................................................7
P4. Role of the health, care or support service practitioner in supporting person centred care...8
TASK 3............................................................................................................................................9
P5. Leadership own role in healthcare service to promote effective inter professional and
multidisciplinary team working...................................................................................................9
M3..............................................................................................................................................10
P6. Responsibilities of information sharing between multidisciplinary teams..........................10
TASK 4..........................................................................................................................................11
P7. Different communication methods used to provide support to different individuals..........11
M4..............................................................................................................................................12
P8. Communication strategies for needs of different service users...........................................12
M5..............................................................................................................................................13
CONCLUSION..............................................................................................................................13
REFERENCES..............................................................................................................................14
1
TASK 1............................................................................................................................................2
P1. Local provision and resources which supports integrated care working...............................2
P2. Current local unmet need related to health, care and support service...................................4
M1................................................................................................................................................5
TASK 2 ...........................................................................................................................................5
P3. Support to individual in a health, care service to identify their own care needs with the
help of care plan...........................................................................................................................5
M2................................................................................................................................................7
P4. Role of the health, care or support service practitioner in supporting person centred care...8
TASK 3............................................................................................................................................9
P5. Leadership own role in healthcare service to promote effective inter professional and
multidisciplinary team working...................................................................................................9
M3..............................................................................................................................................10
P6. Responsibilities of information sharing between multidisciplinary teams..........................10
TASK 4..........................................................................................................................................11
P7. Different communication methods used to provide support to different individuals..........11
M4..............................................................................................................................................12
P8. Communication strategies for needs of different service users...........................................12
M5..............................................................................................................................................13
CONCLUSION..............................................................................................................................13
REFERENCES..............................................................................................................................14
1

INTRODUCTION
Integrated health and social care provide care and improve the quality of the care for the
service users. Healthcare transforms the system to improve responding and efficiency to multiple
needs of the patients both beyond and within field of the mental health. Healthcare organization
must deliver services to better the quality of care with access to care, extending patient choice
and specific focus on problems of partnership working and the integrated care. Integrated care is
essential for the patients who are mentally ill because it will be difficult to provide care and
treatment to patients who are with the mental issues so integrated care is used to deal with these
issues (Glasby and Dickinson, 2014). Coordinated accessible pathway to the care is more
important for the mental health service users compare to other patients. This assignment has two
parts and different cases are given for the first part, second part will include the role of
practitioner in healthcare and responsibilities of information sharing between multidisciplinary
teams. And also need for the person- centred communication in implementing person- centred
plans.
TASK 1
P1. Local provision and resources which supports integrated care working
From the case healthcare practitioner are provided service in local community, as in local
community people do not get sufficient care and treatment so some programmes are organised to
practice in such communities which can provide the proper care to the individuals. In the case
practitioner is chosen by the team manager to investigate and write report of health and social
services that are available in local areas to accomplish needs of people who are with the needs.
There are different healthcare who work to provide support to people in local community as they
do not get effective care (Oakley, 2018). Theses programmes are work to bring together
healthcare service and voluntary organizations in local areas. And with the help of each other
they provided innovative combination of the medical and non medical people support for the ill
and old people who have needs. Integrated care and support working is multidisciplinary care
which involve different healthcare and professionals such as nurses, doctors and care providers.
In case of mental health problems individuals need multidisciplinary care because they will be
with different needs.
2
Integrated health and social care provide care and improve the quality of the care for the
service users. Healthcare transforms the system to improve responding and efficiency to multiple
needs of the patients both beyond and within field of the mental health. Healthcare organization
must deliver services to better the quality of care with access to care, extending patient choice
and specific focus on problems of partnership working and the integrated care. Integrated care is
essential for the patients who are mentally ill because it will be difficult to provide care and
treatment to patients who are with the mental issues so integrated care is used to deal with these
issues (Glasby and Dickinson, 2014). Coordinated accessible pathway to the care is more
important for the mental health service users compare to other patients. This assignment has two
parts and different cases are given for the first part, second part will include the role of
practitioner in healthcare and responsibilities of information sharing between multidisciplinary
teams. And also need for the person- centred communication in implementing person- centred
plans.
TASK 1
P1. Local provision and resources which supports integrated care working
From the case healthcare practitioner are provided service in local community, as in local
community people do not get sufficient care and treatment so some programmes are organised to
practice in such communities which can provide the proper care to the individuals. In the case
practitioner is chosen by the team manager to investigate and write report of health and social
services that are available in local areas to accomplish needs of people who are with the needs.
There are different healthcare who work to provide support to people in local community as they
do not get effective care (Oakley, 2018). Theses programmes are work to bring together
healthcare service and voluntary organizations in local areas. And with the help of each other
they provided innovative combination of the medical and non medical people support for the ill
and old people who have needs. Integrated care and support working is multidisciplinary care
which involve different healthcare and professionals such as nurses, doctors and care providers.
In case of mental health problems individuals need multidisciplinary care because they will be
with different needs.
2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Care support team: Good team and support is very essential to provide care and
treatment to the patients who are with mental health issues. And working with better team can
help to provide a good care to the patients who have mental illness. Integrated care and support
gives good results with the better team (Voorberg, Bekkers and Tummers, 2015). With the help
of multidisciplinary care individuals can be implemented and given targets and goals can be
achieved within a short time of period.
System leadership: Main focus of these types of programmes are to complete system
change through leadership and management development. Using these skills practitioner can
provide care and deal with the patients who are with mental health issues.
Barnet is borough which is legally known as the Barnet primary care trust. It has
healthcare services which improve health in that particular population. There are different
healthcare services present in Barnet which provide care to individuals.
Healthcare services: It includes Barnet hospital, National schizophrenia fellowship
(NSF) and royal free hospital which mainly focus on needs of communities and goals related to
health of individuals. These services help people who are with schizophrenia disorder. NSF
provides support to the patients who are suffering with the particular disease and also their
family. This service consists of nurses and doctors who help to mental patients to get over from
the disorder and provide significant care. Local health system is to continue proactive recovery
which focuses on planning to build the healthcare sectors resilience. This planning facilitate
actions like strengthen, stabilize and integrated existing resources, identify de novo preventive as
well as healthcare delivery strategies which are affordable and sustainable that will lead to the
improved public and health outcomes in community.
Social care services: In Barnet there are social services which provide appropriate care
and treatment such as Barnet voice for mental health, Crisis Resolution & Home Treatment and
Enfield & Haringey Mental Health Trust. Barnet assessment service is made up of social
workers, support staff, psychiatrists and mental health nurses who asses health needs of patient
and provide information how individual can recover with the help of self. CRHT provide care to
those who need urgent care. Barnet voice for mental health support sessions for the local people
with mental health issues. This include activities like walking, games, art and reading which
depends on interest of individual. Theses care defined as provision of personal care, social
3
treatment to the patients who are with mental health issues. And working with better team can
help to provide a good care to the patients who have mental illness. Integrated care and support
gives good results with the better team (Voorberg, Bekkers and Tummers, 2015). With the help
of multidisciplinary care individuals can be implemented and given targets and goals can be
achieved within a short time of period.
System leadership: Main focus of these types of programmes are to complete system
change through leadership and management development. Using these skills practitioner can
provide care and deal with the patients who are with mental health issues.
Barnet is borough which is legally known as the Barnet primary care trust. It has
healthcare services which improve health in that particular population. There are different
healthcare services present in Barnet which provide care to individuals.
Healthcare services: It includes Barnet hospital, National schizophrenia fellowship
(NSF) and royal free hospital which mainly focus on needs of communities and goals related to
health of individuals. These services help people who are with schizophrenia disorder. NSF
provides support to the patients who are suffering with the particular disease and also their
family. This service consists of nurses and doctors who help to mental patients to get over from
the disorder and provide significant care. Local health system is to continue proactive recovery
which focuses on planning to build the healthcare sectors resilience. This planning facilitate
actions like strengthen, stabilize and integrated existing resources, identify de novo preventive as
well as healthcare delivery strategies which are affordable and sustainable that will lead to the
improved public and health outcomes in community.
Social care services: In Barnet there are social services which provide appropriate care
and treatment such as Barnet voice for mental health, Crisis Resolution & Home Treatment and
Enfield & Haringey Mental Health Trust. Barnet assessment service is made up of social
workers, support staff, psychiatrists and mental health nurses who asses health needs of patient
and provide information how individual can recover with the help of self. CRHT provide care to
those who need urgent care. Barnet voice for mental health support sessions for the local people
with mental health issues. This include activities like walking, games, art and reading which
depends on interest of individual. Theses care defined as provision of personal care, social
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

support services, social work and protection to both children and adults at risk or in need. This
service provide support to people who are disable and ill in that particular area.
Healthcare and social services which are provided in Barnet can help to patients who are
suffering from Schizophrenia so that they can reduce it with the health of these services. Both the
services provide treatment and care those patients who are dealing with mental issues and can
not help themselves. Under such care system they can visit and get treatment as per their
requirements.
Integrated social and health working assure that gaps in services which has to addressed
and improved, results and experiences for the service users has to be promoted. In case of mental
health problems patients require care with better planning and which should implement health of
patients who are with mental health issues. Different organization which helps to healthcare to
provide a good quality of care to theses patients. Funds and different programs are provided to
practitioner so they can give support and care to mentally ill people in the local community. NHS
also provide opportunity to participate in programmes which are related to the care practice to
people who are with needs.
P2. Current local unmet need related to health, care and support service
Unmet need for the healthcare can be defined as unexpressed demand, it involves those
need with that healthcare is not aware. This can include individuals ineligible for the treatment
and those who get poorer quality of care and treatment, for some people unmet needs can be
combination of these two. In case of patients with mental health issues do not receive relevant
healthcare (Horrocks and Johnson, 2014). There is gaps in terms of treatment, access, funding
and care.
In Barnet there are certain need of people which are unmet as people do not talk about the
mental health issue so they do not get treatment. Schizophrenia is major mental health issue in
the certain area which is affecting most of individuals. Patients who are with schizophrenia
shows complex mixture of social and clinical needs. Meeting needs are essential because number
of unmet related to reduced health, ongoing health related expenditure and poor quality of the
life. In this area there is lack of professional to treat them and also some mental health needs are
not identified. Mental health service is characterised by the significant variations in accessibility
to user, quality of user and service provision. Main focus of these healthcare is to improve in
availability and also quality of provision in the mental health services. It also include
4
service provide support to people who are disable and ill in that particular area.
Healthcare and social services which are provided in Barnet can help to patients who are
suffering from Schizophrenia so that they can reduce it with the health of these services. Both the
services provide treatment and care those patients who are dealing with mental issues and can
not help themselves. Under such care system they can visit and get treatment as per their
requirements.
Integrated social and health working assure that gaps in services which has to addressed
and improved, results and experiences for the service users has to be promoted. In case of mental
health problems patients require care with better planning and which should implement health of
patients who are with mental health issues. Different organization which helps to healthcare to
provide a good quality of care to theses patients. Funds and different programs are provided to
practitioner so they can give support and care to mentally ill people in the local community. NHS
also provide opportunity to participate in programmes which are related to the care practice to
people who are with needs.
P2. Current local unmet need related to health, care and support service
Unmet need for the healthcare can be defined as unexpressed demand, it involves those
need with that healthcare is not aware. This can include individuals ineligible for the treatment
and those who get poorer quality of care and treatment, for some people unmet needs can be
combination of these two. In case of patients with mental health issues do not receive relevant
healthcare (Horrocks and Johnson, 2014). There is gaps in terms of treatment, access, funding
and care.
In Barnet there are certain need of people which are unmet as people do not talk about the
mental health issue so they do not get treatment. Schizophrenia is major mental health issue in
the certain area which is affecting most of individuals. Patients who are with schizophrenia
shows complex mixture of social and clinical needs. Meeting needs are essential because number
of unmet related to reduced health, ongoing health related expenditure and poor quality of the
life. In this area there is lack of professional to treat them and also some mental health needs are
not identified. Mental health service is characterised by the significant variations in accessibility
to user, quality of user and service provision. Main focus of these healthcare is to improve in
availability and also quality of provision in the mental health services. It also include
4
improvement in safety, physical health, recovery and patient centeredness. Lack of care in case
of metal ill people can negatively effect on the health of individual. Healthcare staff has to
trained so they can provide a better quality of service to community.
M1
There are various needs for health and social care. Healthcare need is like treatment and
control of diseases, providing care with the needs as well as injury or disability. Social care is
related to 'activities of daily living' that means required help with the daily activities like
dressing, washing and feeding. It also involve help with complex relationship, maintaining social
interaction and protection from the vulnerable condition. There are different organizations in
Barnet which help mental health patient to cure the condition such as voluntary sector
organization which provide care to mental health patients. Local and national mental health
services like NHS and other organization like charity which help people to get over their mental
health issues. According to the case study multidisciplinary care is essential in local areas for
the those who are with mental health problems. Practitioner can help people to improve their
condition with the daily care and assessment. And this can be easily done with the help of
integrated health and care to give care as per individual's requirement because multidisciplinary
working help people to approach in multiple ways as case study shows. Care provider has to give
good care do not rush all the time and has to visit regularly, for these requirements NHS can be
provide fund for the better care and treatment.
This practice can have impact on the patients with the mental illness. In multidisciplinary
care, professional with the team can provide a good quality of care to these patients which is
very important in case of mental health problem like schizophrenia and depression cases
(Wenger-Trayner and et. al., 2014). As these patients have their different needs and seek for the
good care and treatment which can be provided with the help of multidisciplinary care working.
TASK 2
P3. Support to individual in a health, care service to identify their own care needs with the help
of care plan
Person centred care refers to assessing health system for treatment and care in hospitals.
These often refer to the individuals who access mental health services as patients. Person centred
care is all about focusing care on needs of individual rather than needs of service.
5
of metal ill people can negatively effect on the health of individual. Healthcare staff has to
trained so they can provide a better quality of service to community.
M1
There are various needs for health and social care. Healthcare need is like treatment and
control of diseases, providing care with the needs as well as injury or disability. Social care is
related to 'activities of daily living' that means required help with the daily activities like
dressing, washing and feeding. It also involve help with complex relationship, maintaining social
interaction and protection from the vulnerable condition. There are different organizations in
Barnet which help mental health patient to cure the condition such as voluntary sector
organization which provide care to mental health patients. Local and national mental health
services like NHS and other organization like charity which help people to get over their mental
health issues. According to the case study multidisciplinary care is essential in local areas for
the those who are with mental health problems. Practitioner can help people to improve their
condition with the daily care and assessment. And this can be easily done with the help of
integrated health and care to give care as per individual's requirement because multidisciplinary
working help people to approach in multiple ways as case study shows. Care provider has to give
good care do not rush all the time and has to visit regularly, for these requirements NHS can be
provide fund for the better care and treatment.
This practice can have impact on the patients with the mental illness. In multidisciplinary
care, professional with the team can provide a good quality of care to these patients which is
very important in case of mental health problem like schizophrenia and depression cases
(Wenger-Trayner and et. al., 2014). As these patients have their different needs and seek for the
good care and treatment which can be provided with the help of multidisciplinary care working.
TASK 2
P3. Support to individual in a health, care service to identify their own care needs with the help
of care plan
Person centred care refers to assessing health system for treatment and care in hospitals.
These often refer to the individuals who access mental health services as patients. Person centred
care is all about focusing care on needs of individual rather than needs of service.
5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
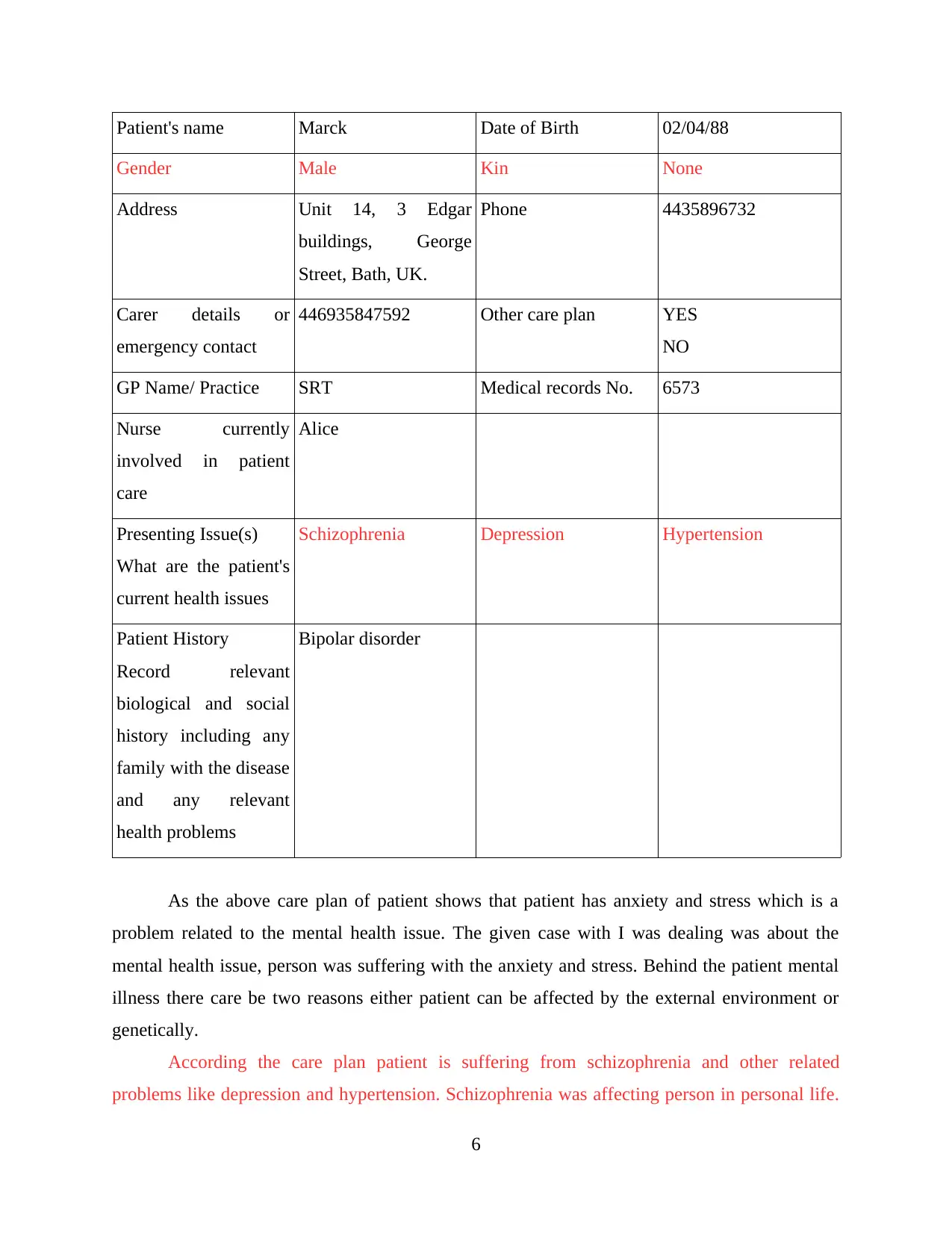
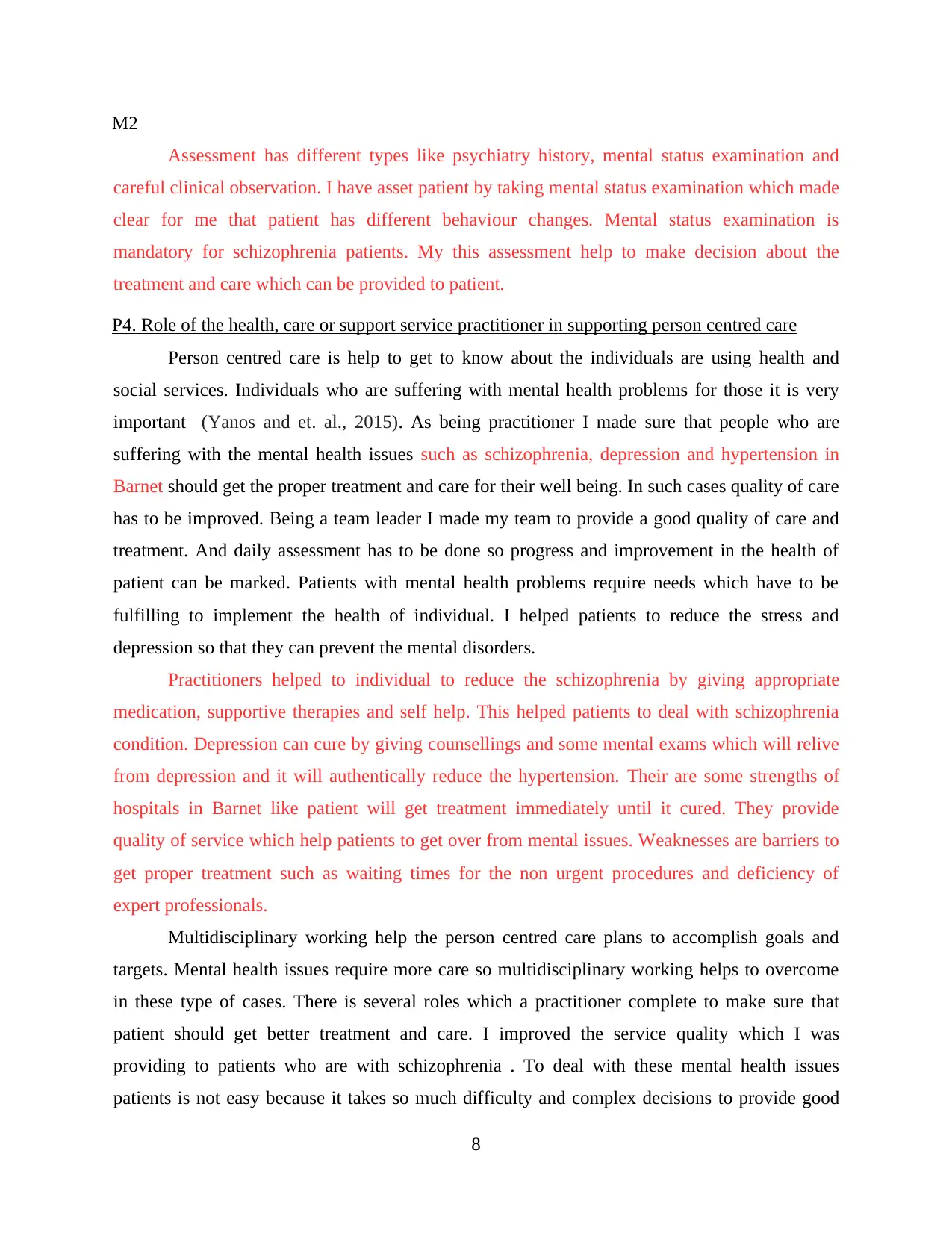
Patient's name Marck Date of Birth 02/04/88
Gender Male Kin None
Address Unit 14, 3 Edgar
buildings, George
Street, Bath, UK.
Phone 4435896732
Carer details or
emergency contact
446935847592 Other care plan YES
NO
GP Name/ Practice SRT Medical records No. 6573
Nurse currently
involved in patient
care
Alice
Presenting Issue(s)
What are the patient's
current health issues
Schizophrenia Depression Hypertension
Patient History
Record relevant
biological and social
history including any
family with the disease
and any relevant
health problems
Bipolar disorder
As the above care plan of patient shows that patient has anxiety and stress which is a
problem related to the mental health issue. The given case with I was dealing was about the
mental health issue, person was suffering with the anxiety and stress. Behind the patient mental
illness there care be two reasons either patient can be affected by the external environment or
genetically.
According the care plan patient is suffering from schizophrenia and other related
problems like depression and hypertension. Schizophrenia was affecting person in personal life.
6
Gender Male Kin None
Address Unit 14, 3 Edgar
buildings, George
Street, Bath, UK.
Phone 4435896732
Carer details or
emergency contact
446935847592 Other care plan YES
NO
GP Name/ Practice SRT Medical records No. 6573
Nurse currently
involved in patient
care
Alice
Presenting Issue(s)
What are the patient's
current health issues
Schizophrenia Depression Hypertension
Patient History
Record relevant
biological and social
history including any
family with the disease
and any relevant
health problems
Bipolar disorder
As the above care plan of patient shows that patient has anxiety and stress which is a
problem related to the mental health issue. The given case with I was dealing was about the
mental health issue, person was suffering with the anxiety and stress. Behind the patient mental
illness there care be two reasons either patient can be affected by the external environment or
genetically.
According the care plan patient is suffering from schizophrenia and other related
problems like depression and hypertension. Schizophrenia was affecting person in personal life.
6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
It was gradually affecting on thoughts and patient also tried for suicide. Sometimes individual
used self harm which led to injuries. This condition changed emotion, behaviour and changes in
thinking which was having a negative impact on individual's life. Special request involve
personal needs which has to fulfil. Such patient required good quality of personal hygiene in
schizophrenia condition.
As care plan shows that patient has bipolar disorder in family history so it may transfer to
the patient. In this case patient can provided with the own care plan so it will help to patient to
overcome with the mental issues. As being practitioner I managed the all primary and basic
needs of patients with the team it was easy to manage the care. Patients with mental health issues
required more needs compare to the other patients.
I used to give some mental exercise to help the patients so that they can relieve their mind
and stress can be reduced. With mental and physical activities these patients may feel better and
it also helps to reduce anxiety. With the help of different areas their own needs can be identify
such as:
Information: Enough information should be given to patients and their family how can
they identify their own needs (O’Connor and et. al., 2016). Identifying own needs will help to
get better care and treatment. I provided detailed information about the methods which are used
to identify the own care needs. I have provided the information about the mental diseases and
how these can be reduced. And the alternative methods which are used to reduce stress so it can
prevent the mental health issues.
Communication: Interacting with patients can help to know about their issues and
problems they are suffering (Dickinson and O'Flynn, 2016). With the proper communication
people can understand the things practitioners are trying to tell. It will help them to know more
about their condition and how they can overcome. My communication skills were pretty good so
I was able make people understand about their condition.
Education: Educating community and people for the mental issues will help to control it.
Stress can be avoided by several physical and mental exercise (Wald, 2015). I made individuals
to understand that mental health also important to being fit. I used some effective methods to
educate people so they can know more about the mental health issues. Person centred care plan
are for those individuals who seek for help.
7
used self harm which led to injuries. This condition changed emotion, behaviour and changes in
thinking which was having a negative impact on individual's life. Special request involve
personal needs which has to fulfil. Such patient required good quality of personal hygiene in
schizophrenia condition.
As care plan shows that patient has bipolar disorder in family history so it may transfer to
the patient. In this case patient can provided with the own care plan so it will help to patient to
overcome with the mental issues. As being practitioner I managed the all primary and basic
needs of patients with the team it was easy to manage the care. Patients with mental health issues
required more needs compare to the other patients.
I used to give some mental exercise to help the patients so that they can relieve their mind
and stress can be reduced. With mental and physical activities these patients may feel better and
it also helps to reduce anxiety. With the help of different areas their own needs can be identify
such as:
Information: Enough information should be given to patients and their family how can
they identify their own needs (O’Connor and et. al., 2016). Identifying own needs will help to
get better care and treatment. I provided detailed information about the methods which are used
to identify the own care needs. I have provided the information about the mental diseases and
how these can be reduced. And the alternative methods which are used to reduce stress so it can
prevent the mental health issues.
Communication: Interacting with patients can help to know about their issues and
problems they are suffering (Dickinson and O'Flynn, 2016). With the proper communication
people can understand the things practitioners are trying to tell. It will help them to know more
about their condition and how they can overcome. My communication skills were pretty good so
I was able make people understand about their condition.
Education: Educating community and people for the mental issues will help to control it.
Stress can be avoided by several physical and mental exercise (Wald, 2015). I made individuals
to understand that mental health also important to being fit. I used some effective methods to
educate people so they can know more about the mental health issues. Person centred care plan
are for those individuals who seek for help.
7
M2
Assessment has different types like psychiatry history, mental status examination and
careful clinical observation. I have asset patient by taking mental status examination which made
clear for me that patient has different behaviour changes. Mental status examination is
mandatory for schizophrenia patients. My this assessment help to make decision about the
treatment and care which can be provided to patient.
P4. Role of the health, care or support service practitioner in supporting person centred care
Person centred care is help to get to know about the individuals are using health and
social services. Individuals who are suffering with mental health problems for those it is very
important (Yanos and et. al., 2015). As being practitioner I made sure that people who are
suffering with the mental health issues such as schizophrenia, depression and hypertension in
Barnet should get the proper treatment and care for their well being. In such cases quality of care
has to be improved. Being a team leader I made my team to provide a good quality of care and
treatment. And daily assessment has to be done so progress and improvement in the health of
patient can be marked. Patients with mental health problems require needs which have to be
fulfilling to implement the health of individual. I helped patients to reduce the stress and
depression so that they can prevent the mental disorders.
Practitioners helped to individual to reduce the schizophrenia by giving appropriate
medication, supportive therapies and self help. This helped patients to deal with schizophrenia
condition. Depression can cure by giving counsellings and some mental exams which will relive
from depression and it will authentically reduce the hypertension. Their are some strengths of
hospitals in Barnet like patient will get treatment immediately until it cured. They provide
quality of service which help patients to get over from mental issues. Weaknesses are barriers to
get proper treatment such as waiting times for the non urgent procedures and deficiency of
expert professionals.
Multidisciplinary working help the person centred care plans to accomplish goals and
targets. Mental health issues require more care so multidisciplinary working helps to overcome
in these type of cases. There is several roles which a practitioner complete to make sure that
patient should get better treatment and care. I improved the service quality which I was
providing to patients who are with schizophrenia . To deal with these mental health issues
patients is not easy because it takes so much difficulty and complex decisions to provide good
8
Assessment has different types like psychiatry history, mental status examination and
careful clinical observation. I have asset patient by taking mental status examination which made
clear for me that patient has different behaviour changes. Mental status examination is
mandatory for schizophrenia patients. My this assessment help to make decision about the
treatment and care which can be provided to patient.
P4. Role of the health, care or support service practitioner in supporting person centred care
Person centred care is help to get to know about the individuals are using health and
social services. Individuals who are suffering with mental health problems for those it is very
important (Yanos and et. al., 2015). As being practitioner I made sure that people who are
suffering with the mental health issues such as schizophrenia, depression and hypertension in
Barnet should get the proper treatment and care for their well being. In such cases quality of care
has to be improved. Being a team leader I made my team to provide a good quality of care and
treatment. And daily assessment has to be done so progress and improvement in the health of
patient can be marked. Patients with mental health problems require needs which have to be
fulfilling to implement the health of individual. I helped patients to reduce the stress and
depression so that they can prevent the mental disorders.
Practitioners helped to individual to reduce the schizophrenia by giving appropriate
medication, supportive therapies and self help. This helped patients to deal with schizophrenia
condition. Depression can cure by giving counsellings and some mental exams which will relive
from depression and it will authentically reduce the hypertension. Their are some strengths of
hospitals in Barnet like patient will get treatment immediately until it cured. They provide
quality of service which help patients to get over from mental issues. Weaknesses are barriers to
get proper treatment such as waiting times for the non urgent procedures and deficiency of
expert professionals.
Multidisciplinary working help the person centred care plans to accomplish goals and
targets. Mental health issues require more care so multidisciplinary working helps to overcome
in these type of cases. There is several roles which a practitioner complete to make sure that
patient should get better treatment and care. I improved the service quality which I was
providing to patients who are with schizophrenia . To deal with these mental health issues
patients is not easy because it takes so much difficulty and complex decisions to provide good
8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
quality of care to these patients. I was working with team which helped me to bring skills,
achieve continuity and sharing information to perform roles to provide good quality of care.
Important roles such as planning for the treatment and care as well as collecting the data which
helps to provide treatment to the patient in Barnet.
There are major roles in healthcare which a practitioner plays to provide a good care to
those patients who are with various needs who are with schizophrenia and other mental health
problems. I made daily observation with the assessment which helped to know more about the
patient's condition like observation and writing the behaviour changes which are taking place in
daily life. Woking with the team always help to the person centred care to achieve the targets and
goals with the multidisciplinary care. Being a leader I divided tasks in team so they can complete
within given time and it helped individuals who were with mental health issues such as
schizophrenia and depression. Providing good treatment and care for schizophrenia, depression
and hypertension to the patient that will make them satisfied and also their family in Barnet.
TASK 3
P5. Leadership own role in healthcare service to promote effective inter professional and
multidisciplinary team working
In healthcare leadership plays major role to perform function with inter professional and
multidisciplinary team. To work with multidisciplinary and inter professional team requires
mutual understanding and a leader has to provide effective care to patients. It also requires a
greater inter professional collaboration. Inter professional collaboration will result to provide a
good quality of care and treatment. Working with multidisciplinary and inter professional team
can impact on organization as well as individuals. Task and goals can be complete with the help
of inter professional and multidisciplinary working (Oliver, Foot and Humphries, 2014).
Multidisciplinary and inter professional working improve the knowledge and skills of the
leadership. Being a leader management and planning things is very important to get better results
of treatment and care.
Decision making in case of inter professional and multidisciplinary can be improved with
mutual understanding and cooperation of team members. These are complex process because it
requires more skills, knowledge, expertise and professionals. These type of practice also explore
more knowledge and understanding about specific situation that is faced in healthcare. Such
9
achieve continuity and sharing information to perform roles to provide good quality of care.
Important roles such as planning for the treatment and care as well as collecting the data which
helps to provide treatment to the patient in Barnet.
There are major roles in healthcare which a practitioner plays to provide a good care to
those patients who are with various needs who are with schizophrenia and other mental health
problems. I made daily observation with the assessment which helped to know more about the
patient's condition like observation and writing the behaviour changes which are taking place in
daily life. Woking with the team always help to the person centred care to achieve the targets and
goals with the multidisciplinary care. Being a leader I divided tasks in team so they can complete
within given time and it helped individuals who were with mental health issues such as
schizophrenia and depression. Providing good treatment and care for schizophrenia, depression
and hypertension to the patient that will make them satisfied and also their family in Barnet.
TASK 3
P5. Leadership own role in healthcare service to promote effective inter professional and
multidisciplinary team working
In healthcare leadership plays major role to perform function with inter professional and
multidisciplinary team. To work with multidisciplinary and inter professional team requires
mutual understanding and a leader has to provide effective care to patients. It also requires a
greater inter professional collaboration. Inter professional collaboration will result to provide a
good quality of care and treatment. Working with multidisciplinary and inter professional team
can impact on organization as well as individuals. Task and goals can be complete with the help
of inter professional and multidisciplinary working (Oliver, Foot and Humphries, 2014).
Multidisciplinary and inter professional working improve the knowledge and skills of the
leadership. Being a leader management and planning things is very important to get better results
of treatment and care.
Decision making in case of inter professional and multidisciplinary can be improved with
mutual understanding and cooperation of team members. These are complex process because it
requires more skills, knowledge, expertise and professionals. These type of practice also explore
more knowledge and understanding about specific situation that is faced in healthcare. Such
9
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
practice helps to know more about education, organizational behaviour and human resource
management (Martinson and Berridge, 2014). Multidisciplinary helps learn how to work in a
team and coordinate which help to provide good quality of care to patients who are suffering
with mental health issues as they need more care and support to fulfil their needs. Such type of
care gives satisfaction to the service users and their family. Teams have shared vision which can
help them have a clear interaction and solve the any issue with mutual understanding. Working
with inter professional and multi disciplinary care can help to get more fund from the other
organization so they can provide good quality of care to the patients who are with mental health
issues.
M3
Leader in multidisciplinary team provide instruction and important information related to
the care and treatment of mental health patients. To run any team their should be a leader which
has independent functions and immediate measures to save patient's life. It helps in different
discussion related to treatment and patient mental condition. This also improves information
management and decision making.
Leadership always helps to lead a team and also require to manage all the strategies and
plans in healthcare to provide good treatment and support to the patients who need it. Team
leader should be able to understand and solve the every problem which they face while providing
care to patients who are suffering from mental health problems (Light and Mcnaughton, 2015).
These patients can not fulfil their own needs so they need special support and care which can be
provided by the practitioners. Such types of care need the multi disciplinary and inter
professional working.
P6. Responsibilities of information sharing between multidisciplinary teams
There are different responsibilities of sharing information between multidisciplinary teams
which are essential. In healthcare every little information is very important and required to
provide treatment to the patients. As in case of patients who are with mental health issues have
very complex condition and providing care in this case can be hard for the care providers.
Collaborative work is a domain of the healthcare that extremely dynamic in nature, different
forms and the multiple modes, each one of them are supported by different kind of mechanisms
and practices (Fox, McMullen and Newburn, 2015). This type of variety and flexibility make
healthcare work more challenging and also ideal object to study for collaborative work and the
10
management (Martinson and Berridge, 2014). Multidisciplinary helps learn how to work in a
team and coordinate which help to provide good quality of care to patients who are suffering
with mental health issues as they need more care and support to fulfil their needs. Such type of
care gives satisfaction to the service users and their family. Teams have shared vision which can
help them have a clear interaction and solve the any issue with mutual understanding. Working
with inter professional and multi disciplinary care can help to get more fund from the other
organization so they can provide good quality of care to the patients who are with mental health
issues.
M3
Leader in multidisciplinary team provide instruction and important information related to
the care and treatment of mental health patients. To run any team their should be a leader which
has independent functions and immediate measures to save patient's life. It helps in different
discussion related to treatment and patient mental condition. This also improves information
management and decision making.
Leadership always helps to lead a team and also require to manage all the strategies and
plans in healthcare to provide good treatment and support to the patients who need it. Team
leader should be able to understand and solve the every problem which they face while providing
care to patients who are suffering from mental health problems (Light and Mcnaughton, 2015).
These patients can not fulfil their own needs so they need special support and care which can be
provided by the practitioners. Such types of care need the multi disciplinary and inter
professional working.
P6. Responsibilities of information sharing between multidisciplinary teams
There are different responsibilities of sharing information between multidisciplinary teams
which are essential. In healthcare every little information is very important and required to
provide treatment to the patients. As in case of patients who are with mental health issues have
very complex condition and providing care in this case can be hard for the care providers.
Collaborative work is a domain of the healthcare that extremely dynamic in nature, different
forms and the multiple modes, each one of them are supported by different kind of mechanisms
and practices (Fox, McMullen and Newburn, 2015). This type of variety and flexibility make
healthcare work more challenging and also ideal object to study for collaborative work and the
10
decision making. Working together is not easy it is quite difficult to coordinate with each other,
there will be different opinions on the same topic so it is challenging for the practitioners.
Working together raises responsibility of every work such as reporting and recording has to
share with the professionals. Data recording and sharing is very essential in healthcare in case of
multidisciplinary. There are various roles and responsibilities involved in care which are
provided at home have to be defined more carefully. In such work different types of home care
manager, social workers, workers, health practitioner and carer. This type of work leads to
coordinate working. It also makes sure that every care provider should involved in delivering
care and support, also know what type of care and treatment they are providing. Care diary of
every patient should be updated daily and remark should be written because this type of
information helps to know more about patient’s condition and implement in patients who are
with mental health problems. And also ensure that everybody has to involve in delivering care
and support as well as communicating on regular basis.
Individual who accepts care role coordinator has to do willingly and everyone involved in
support and care should know, also care coordinator responsibilities should be respected.
Working together can reduce the cost and it can save the cost which can be utilized for the other
purpose of healthcare. There are different challenges which are faced to accomplish these
responsibilities a leader has to face. Working with multidisciplinary can be critical, which is
depends on the leader and co workers. Practitioner has to play a major role to provide support
and care to individuals who are with mental health issues as they need it more and in different
way to fulfil their needs (Drake and Whitley, 2014). Sharing information in multidisciplinary
care requires more responsibility and knowledge. Good leader with the effective information
sharing skills will able to do this type of work. Multidisciplinary team work impact on
organization as well as patients care.
TASK 4
P7. Different communication methods used to provide support to different individuals
For a practitioner communication plays a major role to provide a good quality of care. Care
worker use different methods of the communication during the treatment and providing care. In
healthcare communication has to be more effective to interact with the patient. There are
different kinds of patients which can be seen in healthcare during treatment. In case of patients
11
there will be different opinions on the same topic so it is challenging for the practitioners.
Working together raises responsibility of every work such as reporting and recording has to
share with the professionals. Data recording and sharing is very essential in healthcare in case of
multidisciplinary. There are various roles and responsibilities involved in care which are
provided at home have to be defined more carefully. In such work different types of home care
manager, social workers, workers, health practitioner and carer. This type of work leads to
coordinate working. It also makes sure that every care provider should involved in delivering
care and support, also know what type of care and treatment they are providing. Care diary of
every patient should be updated daily and remark should be written because this type of
information helps to know more about patient’s condition and implement in patients who are
with mental health problems. And also ensure that everybody has to involve in delivering care
and support as well as communicating on regular basis.
Individual who accepts care role coordinator has to do willingly and everyone involved in
support and care should know, also care coordinator responsibilities should be respected.
Working together can reduce the cost and it can save the cost which can be utilized for the other
purpose of healthcare. There are different challenges which are faced to accomplish these
responsibilities a leader has to face. Working with multidisciplinary can be critical, which is
depends on the leader and co workers. Practitioner has to play a major role to provide support
and care to individuals who are with mental health issues as they need it more and in different
way to fulfil their needs (Drake and Whitley, 2014). Sharing information in multidisciplinary
care requires more responsibility and knowledge. Good leader with the effective information
sharing skills will able to do this type of work. Multidisciplinary team work impact on
organization as well as patients care.
TASK 4
P7. Different communication methods used to provide support to different individuals
For a practitioner communication plays a major role to provide a good quality of care. Care
worker use different methods of the communication during the treatment and providing care. In
healthcare communication has to be more effective to interact with the patient. There are
different kinds of patients which can be seen in healthcare during treatment. In case of patients
11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





