MOD005910: Report on Integrated Health Centre Development, 2020
VerifiedAdded on 2022/09/18
|7
|1736
|26
Report
AI Summary
This report presents an analysis of an integrated health center initiative involving The Ruskin NHS Foundation Trust and Ruskinshire County Council Social Services, designed to improve healthcare delivery. The report, prepared by a group of health and social care practitioners, details the impact of the integrated health center on service user engagement, the benefits of multidisciplinary teams, and the management of diversity. It explores how the center involves service users and manages diversity, referencing relevant legislation such as the Equality Act 2010 and the Care Act 2014. The report highlights the importance of collaborative teamwork and the positive effects on patient outcomes, concluding with an emphasis on the effective integration of various healthcare professionals. The report also includes a specialist nurse's perspective on the stroke unit, emphasizing patient care and the roles of different professionals. The work is a reflection on the progress made over 18 months.

Case study
The Ruskin NHS Foundation Trust provides acute services to the people of Ruskin.
Ruskinshire County Council Social Services are experiencing severe financial challenges.
The two organisations have agreed to work together using the ‘Better Care Fund’. The initial
step is to establish an inter-professional/ multi-disciplinary health centre that is located in the
heart of the community. The Centre brings together professional from primary care, public
health, local authority and third sector partners to deliver a more integrated health care
service. There is also duplication of effort in some areas of the health care provision. The
intention is to establish an integrated health centre providing ‘wrap around care’ that is
designed to reduce waste and fragmentation in the delivery of health care. The Trust has
established teams across the partnership that will develop sustainable models of health care. It
is hope that the teams will focus on preventative care and wellbeing for the patients. You are
part of a group of five health and social care practitioners who have been leading on this
initiative for the last 18 months. You are now required to write a briefing note reporting back
to the senior managers on the progress you have made in setting up the integrated service.
Setting 2: Stroke ward- patient discharge meeting
Title: specialist nurse for older adults
Student number 1820082/1
Module Title: The Health Care Professional
Module Code: MOD005910
Word Limit: 1000
Submission deadline: 2 pm Friday 22 May 2020
The Ruskin NHS Foundation Trust provides acute services to the people of Ruskin.
Ruskinshire County Council Social Services are experiencing severe financial challenges.
The two organisations have agreed to work together using the ‘Better Care Fund’. The initial
step is to establish an inter-professional/ multi-disciplinary health centre that is located in the
heart of the community. The Centre brings together professional from primary care, public
health, local authority and third sector partners to deliver a more integrated health care
service. There is also duplication of effort in some areas of the health care provision. The
intention is to establish an integrated health centre providing ‘wrap around care’ that is
designed to reduce waste and fragmentation in the delivery of health care. The Trust has
established teams across the partnership that will develop sustainable models of health care. It
is hope that the teams will focus on preventative care and wellbeing for the patients. You are
part of a group of five health and social care practitioners who have been leading on this
initiative for the last 18 months. You are now required to write a briefing note reporting back
to the senior managers on the progress you have made in setting up the integrated service.
Setting 2: Stroke ward- patient discharge meeting
Title: specialist nurse for older adults
Student number 1820082/1
Module Title: The Health Care Professional
Module Code: MOD005910
Word Limit: 1000
Submission deadline: 2 pm Friday 22 May 2020
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Specialist nurse/ stroke unit
In the stroke unit, I am a specialist nurse. I oversee the needs of the patients; monitor
their vital signs, and administering medication. I also refer them to the other professionals if
need be. The other experts in the team are physiotherapy, occupational therapy, a social
worker, and the geriatric consultant. This has helped service user’s progression. During the
last 18 months, the integration has greatly improved the healthcare standard and specialists
have gained learning experience allied to health professions as based on (Smith and Boyd
2012, pp.63-72).
Word count 88
Expound how the new integrated health center will impact on service user engagement
and cope with the different service users
According to Lester, Glasby and Tylee (2004, pp.285-291), integrated care is a range
of different organizations coming together to share experiences and expertise for the benefits
of service and the organization. This analysis summarizes and explains the impact of the
integrated health center on the service user. The built-in health center provides affordable
health services by nursing professionals to meet the needs of their service users.
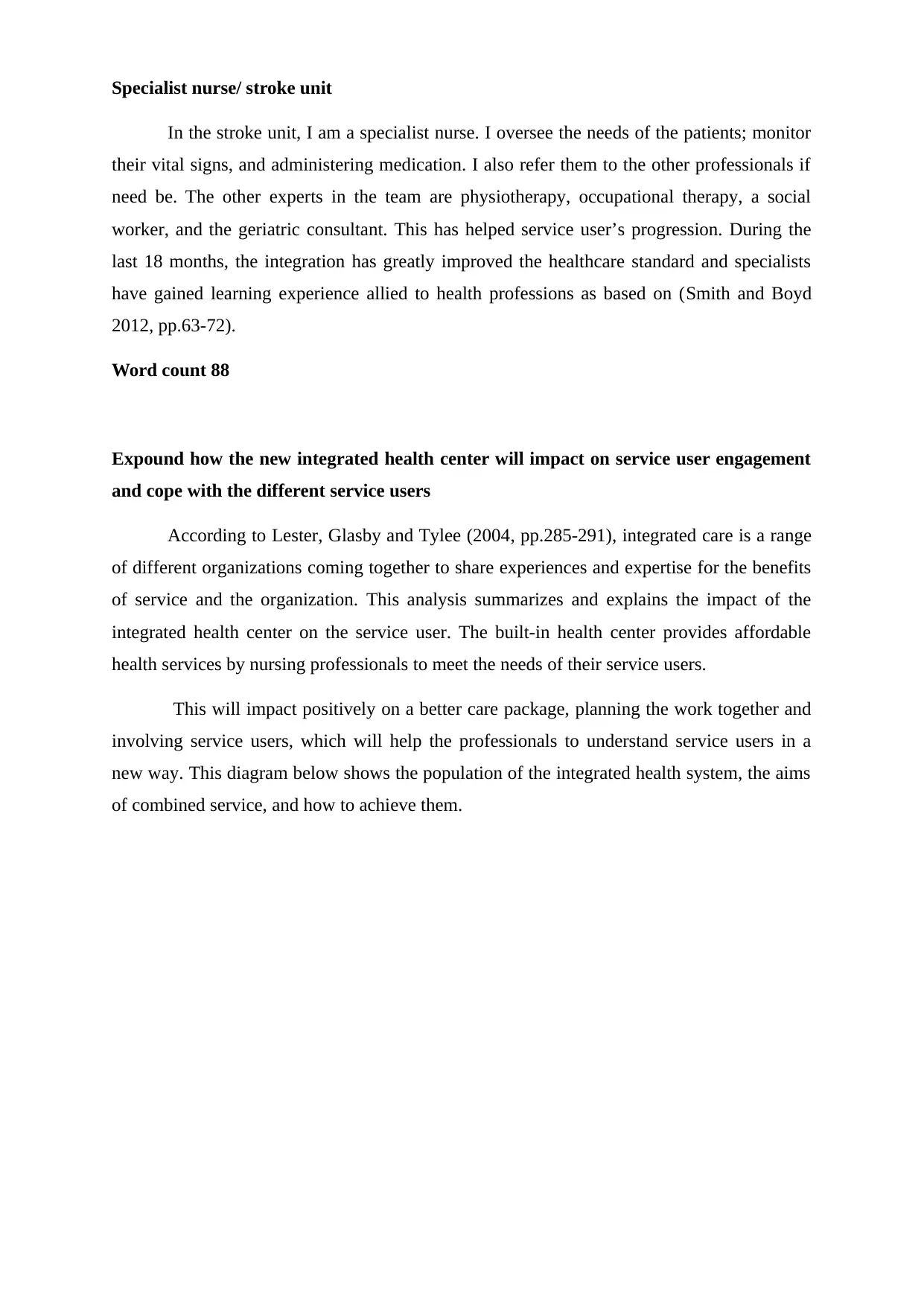
This will impact positively on a better care package, planning the work together and
involving service users, which will help the professionals to understand service users in a
new way. This diagram below shows the population of the integrated health system, the aims
of combined service, and how to achieve them.
In the stroke unit, I am a specialist nurse. I oversee the needs of the patients; monitor
their vital signs, and administering medication. I also refer them to the other professionals if
need be. The other experts in the team are physiotherapy, occupational therapy, a social
worker, and the geriatric consultant. This has helped service user’s progression. During the
last 18 months, the integration has greatly improved the healthcare standard and specialists
have gained learning experience allied to health professions as based on (Smith and Boyd
2012, pp.63-72).
Word count 88
Expound how the new integrated health center will impact on service user engagement
and cope with the different service users
According to Lester, Glasby and Tylee (2004, pp.285-291), integrated care is a range
of different organizations coming together to share experiences and expertise for the benefits
of service and the organization. This analysis summarizes and explains the impact of the
integrated health center on the service user. The built-in health center provides affordable
health services by nursing professionals to meet the needs of their service users.
This will impact positively on a better care package, planning the work together and
involving service users, which will help the professionals to understand service users in a
new way. This diagram below shows the population of the integrated health system, the aims
of combined service, and how to achieve them.
Word count 117
The benefits of Multidisciplinary team working for service users
A multidisciplinary team is defined as group of health care personnel who have
diverse disciplines providing specific services to the patients. It allows for successful, well-
organized cooperation, and can help us build or maintain a social relationship. Joint
assessment and planning together and involvement of the newly integrated team ensure that
communication and information sharing will become better. This, therefore, improves health
care and lowers overall health care costs on the side of service use.
When everyone is working together, a trusting relationship develops within the team
and they share the vision and goals of improved integrated care (Lee, Haein, Hyejin Park, and
Jinwoo, p.862-877). This relationship also leads to the right mix of professional background
and clear boundaries and responsibilities across the board. Multidisciplinary service also
benefits the users as follows. Lowering depressive symptoms, improves access to services,
and increases the quality of health care.
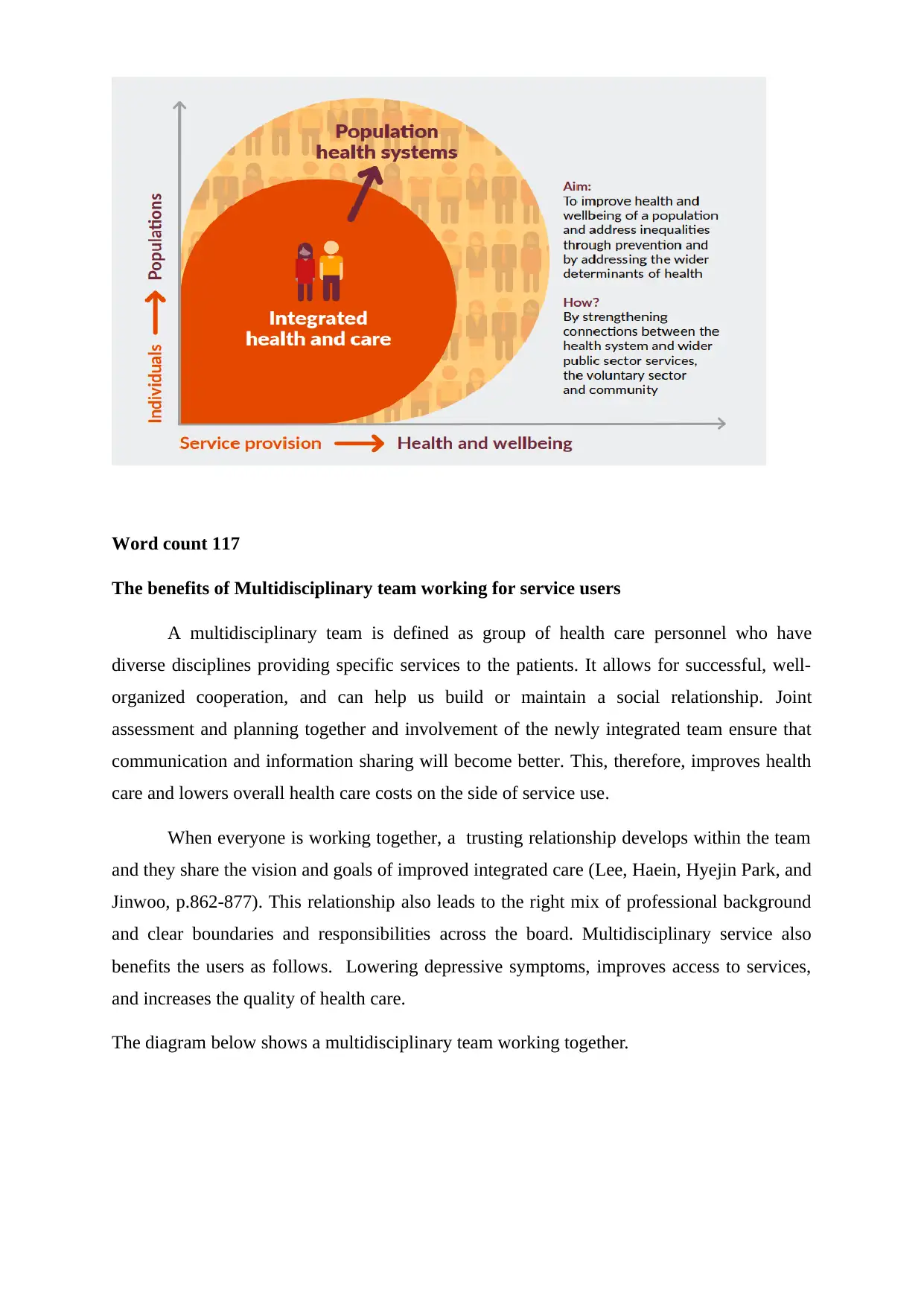
The diagram below shows a multidisciplinary team working together.
The benefits of Multidisciplinary team working for service users
A multidisciplinary team is defined as group of health care personnel who have
diverse disciplines providing specific services to the patients. It allows for successful, well-
organized cooperation, and can help us build or maintain a social relationship. Joint
assessment and planning together and involvement of the newly integrated team ensure that
communication and information sharing will become better. This, therefore, improves health
care and lowers overall health care costs on the side of service use.
When everyone is working together, a trusting relationship develops within the team
and they share the vision and goals of improved integrated care (Lee, Haein, Hyejin Park, and
Jinwoo, p.862-877). This relationship also leads to the right mix of professional background
and clear boundaries and responsibilities across the board. Multidisciplinary service also
benefits the users as follows. Lowering depressive symptoms, improves access to services,
and increases the quality of health care.
The diagram below shows a multidisciplinary team working together.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Word count 155
Example of how integrated health care involves and engage with the service users
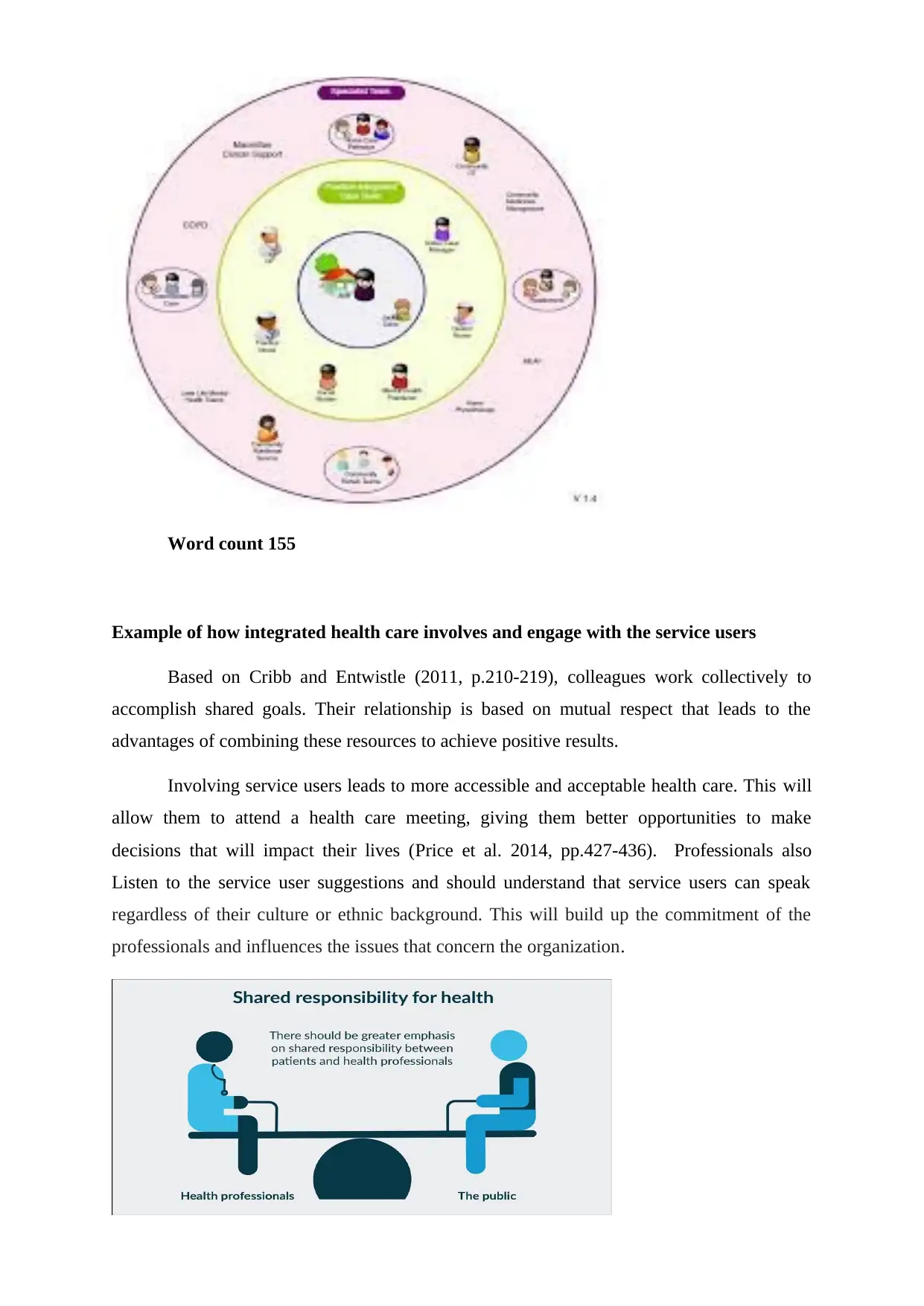
Based on Cribb and Entwistle (2011, p.210-219), colleagues work collectively to
accomplish shared goals. Their relationship is based on mutual respect that leads to the
advantages of combining these resources to achieve positive results.
Involving service users leads to more accessible and acceptable health care. This will
allow them to attend a health care meeting, giving them better opportunities to make
decisions that will impact their lives (Price et al. 2014, pp.427-436). Professionals also
Listen to the service user suggestions and should understand that service users can speak
regardless of their culture or ethnic background. This will build up the commitment of the
professionals and influences the issues that concern the organization.
Example of how integrated health care involves and engage with the service users
Based on Cribb and Entwistle (2011, p.210-219), colleagues work collectively to
accomplish shared goals. Their relationship is based on mutual respect that leads to the
advantages of combining these resources to achieve positive results.
Involving service users leads to more accessible and acceptable health care. This will
allow them to attend a health care meeting, giving them better opportunities to make
decisions that will impact their lives (Price et al. 2014, pp.427-436). Professionals also
Listen to the service user suggestions and should understand that service users can speak
regardless of their culture or ethnic background. This will build up the commitment of the
professionals and influences the issues that concern the organization.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Word count 112
Example of how multidisciplinary and inter-professional manage the diversity
Multidisciplinary teams are endorsed as a way to enable practitioners and other
professionals in health and social care to collaborate successfully. The team involved should
have a mutual understanding regarding the service user's care; for example, their approach
will be different depending on their diverse culture. Therefore, an improved planning and
policy development will be clinically useful and help will help enhance problem solving as
well as share knowledge
Based on (Kraut, Egido, and Galegher 2014, pp.163-186), specialists from many areas
must work as one and regularly communicate to share ideas and resources. A fruitful
multidisciplinary health group tries to make the most inclusive review of a patient's situation
and to follow it up with a full-range treatment plan. Heiman and Artiga ( 2015, pp.1-10) also
stated that the teams to always work together to produce and promote health plans for diverse
communities and to provide valuable information that will impact care for the patients
therefore multi-disciplinary co-operation is a cornerstone for good results. These
multidisciplinary teams ensure better health outcomes for service users.
Word count 174
Relevant legislation models or policies that relate to diversity and service users
Policies and practices are a vital part of any association. These policies and
procedures provide a pathway for daily tasks. They confirm agreement with laws and
regulations, give guidance for decision-making, and update internal processes. Below is a
table showing some of these policies and legislations
The Equality & diversity legislation in
health care 2010
states that individuals maintain dignity and
equality
Equality Act of 2010 Set out to protect the right of persons and
develops the equality of opportunity for all.
Example of how multidisciplinary and inter-professional manage the diversity
Multidisciplinary teams are endorsed as a way to enable practitioners and other
professionals in health and social care to collaborate successfully. The team involved should
have a mutual understanding regarding the service user's care; for example, their approach
will be different depending on their diverse culture. Therefore, an improved planning and
policy development will be clinically useful and help will help enhance problem solving as
well as share knowledge
Based on (Kraut, Egido, and Galegher 2014, pp.163-186), specialists from many areas
must work as one and regularly communicate to share ideas and resources. A fruitful
multidisciplinary health group tries to make the most inclusive review of a patient's situation
and to follow it up with a full-range treatment plan. Heiman and Artiga ( 2015, pp.1-10) also
stated that the teams to always work together to produce and promote health plans for diverse
communities and to provide valuable information that will impact care for the patients
therefore multi-disciplinary co-operation is a cornerstone for good results. These
multidisciplinary teams ensure better health outcomes for service users.
Word count 174
Relevant legislation models or policies that relate to diversity and service users
Policies and practices are a vital part of any association. These policies and
procedures provide a pathway for daily tasks. They confirm agreement with laws and
regulations, give guidance for decision-making, and update internal processes. Below is a
table showing some of these policies and legislations
The Equality & diversity legislation in
health care 2010
states that individuals maintain dignity and
equality
Equality Act of 2010 Set out to protect the right of persons and
develops the equality of opportunity for all.
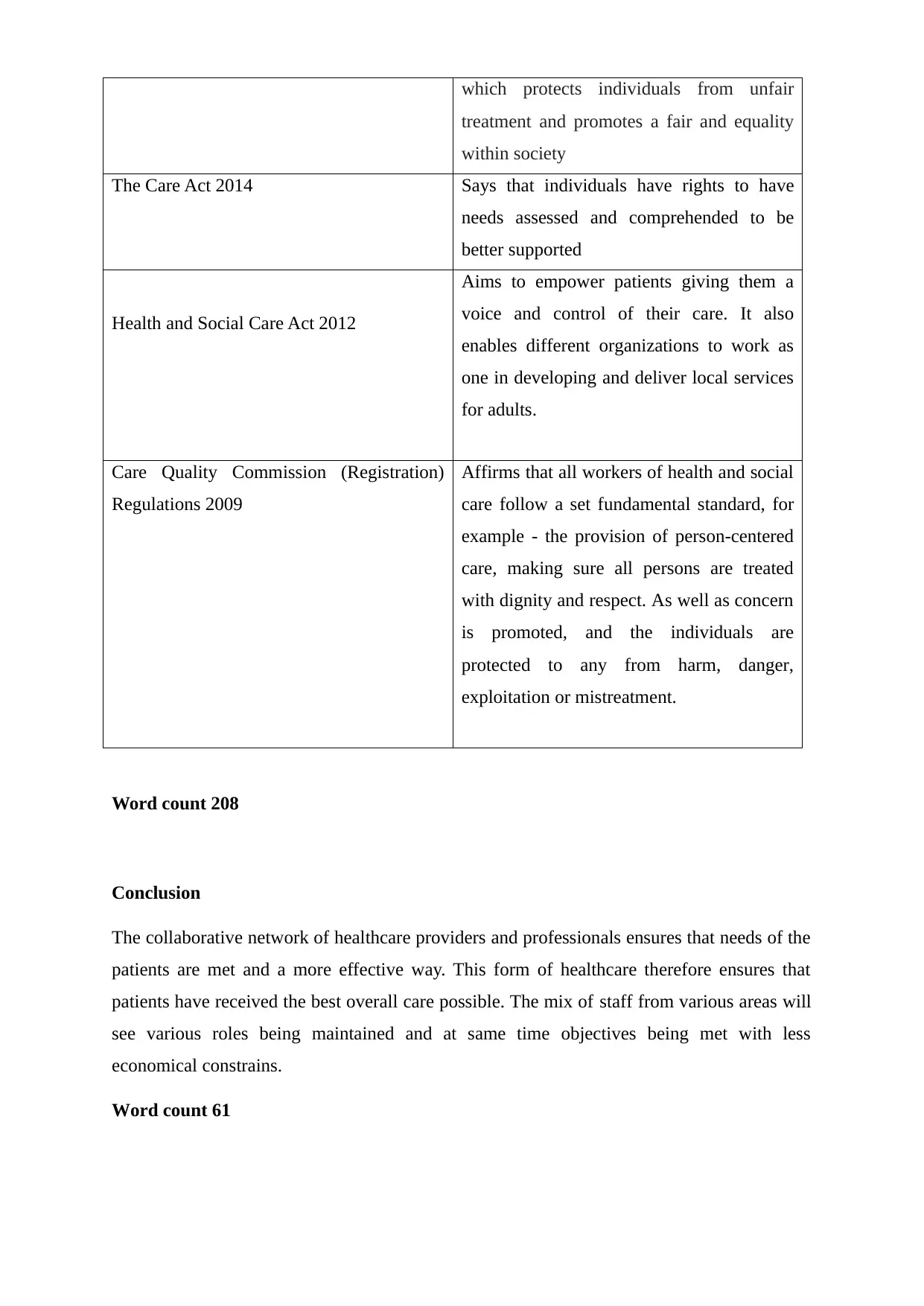
which protects individuals from unfair
treatment and promotes a fair and equality
within society
The Care Act 2014 Says that individuals have rights to have
needs assessed and comprehended to be
better supported
Health and Social Care Act 2012
Aims to empower patients giving them a
voice and control of their care. It also
enables different organizations to work as
one in developing and deliver local services
for adults.
Care Quality Commission (Registration)
Regulations 2009
Affirms that all workers of health and social
care follow a set fundamental standard, for
example - the provision of person-centered
care, making sure all persons are treated
with dignity and respect. As well as concern
is promoted, and the individuals are
protected to any from harm, danger,
exploitation or mistreatment.
Word count 208
Conclusion
The collaborative network of healthcare providers and professionals ensures that needs of the
patients are met and a more effective way. This form of healthcare therefore ensures that
patients have received the best overall care possible. The mix of staff from various areas will
see various roles being maintained and at same time objectives being met with less
economical constrains.
Word count 61
treatment and promotes a fair and equality
within society
The Care Act 2014 Says that individuals have rights to have
needs assessed and comprehended to be
better supported
Health and Social Care Act 2012
Aims to empower patients giving them a
voice and control of their care. It also
enables different organizations to work as
one in developing and deliver local services
for adults.
Care Quality Commission (Registration)
Regulations 2009
Affirms that all workers of health and social
care follow a set fundamental standard, for
example - the provision of person-centered
care, making sure all persons are treated
with dignity and respect. As well as concern
is promoted, and the individuals are
protected to any from harm, danger,
exploitation or mistreatment.
Word count 208
Conclusion
The collaborative network of healthcare providers and professionals ensures that needs of the
patients are met and a more effective way. This form of healthcare therefore ensures that
patients have received the best overall care possible. The mix of staff from various areas will
see various roles being maintained and at same time objectives being met with less
economical constrains.
Word count 61
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Cribb, A., and Entwistle, V.A., 2011. Shared decision making: trade‐offs between narrower
and broader conceptions. Health Expectations, 14(2), pp.210-219.
Heiman, H.J. and Artiga, S., 2015. Beyond health care: the role of social determinants in
promoting health and health equity. Health, 20(10), pp.1-10.
Kraut, R.E., Egido, C., and Galegher, J., 2014. Patterns of contact and communication in
scientific research collaborations. In Intellectual teamwork (pp. 163-186).
Lee, H., Park, H. and Kim, J., 2013. Why do people share their context information on Social
Network Services? A qualitative study and an experimental study on users' behavior of
balancing perceived benefit and risk. International Journal of Human-Computer Studies,
71(9), pp.862-877.
Lester, H., Glasby, J. and Tylee, A., 2004. Integrated primary mental health care: threat or
opportunity in the new NHS?. Br J Gen Pract, 54(501), pp.285-291.
Price, M., Yuen, E.K., Goetter, E.M., Herbert, J.D., Forman, E.M., Acierno, R. and Ruggiero,
K.J., 2014. mHealth: a mechanism to deliver more accessible, more effective mental health
care. Clinical psychology & psychotherapy, 21(5), pp.427-436.
Smith, C. and Boyd, P., 2012. Becoming an academic: The reconstruction of identity by
recently appointed lecturers in nursing, midwifery and the allied health professions.
Innovations in Education and Teaching International, 49(1), pp.63-72.
Wilberforce, M., Tucker, S., Abendstern, M., Brand, C., Giebel, C.M. and Challis, D., 2013.
Membership and management: structures of inter-professional working in community mental
health teams for older people in England. International psychogeriatrics, 25(9), pp.1485-
1492.
Cribb, A., and Entwistle, V.A., 2011. Shared decision making: trade‐offs between narrower
and broader conceptions. Health Expectations, 14(2), pp.210-219.
Heiman, H.J. and Artiga, S., 2015. Beyond health care: the role of social determinants in
promoting health and health equity. Health, 20(10), pp.1-10.
Kraut, R.E., Egido, C., and Galegher, J., 2014. Patterns of contact and communication in
scientific research collaborations. In Intellectual teamwork (pp. 163-186).
Lee, H., Park, H. and Kim, J., 2013. Why do people share their context information on Social
Network Services? A qualitative study and an experimental study on users' behavior of
balancing perceived benefit and risk. International Journal of Human-Computer Studies,
71(9), pp.862-877.
Lester, H., Glasby, J. and Tylee, A., 2004. Integrated primary mental health care: threat or
opportunity in the new NHS?. Br J Gen Pract, 54(501), pp.285-291.
Price, M., Yuen, E.K., Goetter, E.M., Herbert, J.D., Forman, E.M., Acierno, R. and Ruggiero,
K.J., 2014. mHealth: a mechanism to deliver more accessible, more effective mental health
care. Clinical psychology & psychotherapy, 21(5), pp.427-436.
Smith, C. and Boyd, P., 2012. Becoming an academic: The reconstruction of identity by
recently appointed lecturers in nursing, midwifery and the allied health professions.
Innovations in Education and Teaching International, 49(1), pp.63-72.
Wilberforce, M., Tucker, S., Abendstern, M., Brand, C., Giebel, C.M. and Challis, D., 2013.
Membership and management: structures of inter-professional working in community mental
health teams for older people in England. International psychogeriatrics, 25(9), pp.1485-
1492.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





