Case Study Analysis: Intellectual Disability and Bipolar Disorder
VerifiedAdded on 2022/09/05
|11
|2967
|21
Case Study
AI Summary
This case study examines Muirne, a 49-year-old woman with severe intellectual disability, bipolar disorder, and autistic spectrum disorder. It details her symptoms, including mood swings, self-injurious behavior, and changes in activity interest. The assessment of her mental health utilizes the PAS-ADD checklist and PIMRA, highlighting the complexities of her conditions. The study explores the challenges of living with these co-occurring conditions, including social isolation and relationship difficulties. Short-term interventions, such as psychotropic medications, and long-term interventions, like cognitive behavioral therapy and patient education, are discussed as potential treatment strategies. The case study emphasizes the need for tailored interventions to improve Muirne's condition and overall well-being, considering both the intellectual disability and the mental health aspects.

Running head: CASE STUDY
CASE STUDY
Name of the Student
Name of the University
Author Note
CASE STUDY
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CASE STUDY
INTRODUCTION
Intellectual Disability can be defined as the inability of using normal mental or
intellectual functions. It affects two main areas, the first of which is intellectual functioning
such as learning various things, solving problems and using normal judgement and the second
is adaptive functioning such as way of communication and way of living independently
(Vissers, Gilissen and Veltman 2016). People with intellectual disability are often observed to
be having Bipolar Disorder. Bipolar Disorder can be defined as the state of mental condition,
which can be characterized by extreme and drastic mood swings including higher emotional
outbursts such as mania or hypomania and lower emotional state like depression (Grunze
2015). In the given case study, Muirne is a 49 year old woman who has severe intellectual
disability and also suffers from bipolar disorder which was first diagnosed in her late 20s. She
also exhibits signs of being in the autistic spectrum. In this study, the case of Muirne will be
studied in details and the symptoms of bipolar disorder she is showing, assessment of her
mental health, complexities of living with a severe intellectual disability, autistic spectrum
and bipolar disorder and the interventions available for Muirne’s short term and long term
care plan.
SYMPTOMS OF BIPOLAR DEPRESSION MUIRNE DISPLAYED
There are quite a few symptoms of bipolar disorder that Muirne has been showing. As
Muirne also has autistic spectrum disorders, therefore many of the symptoms coincide with
that of bipolar disorder. Both the conditions have individually left imprint on the nature of
Murine and it is very evident and distinguishable from her behaviour. The symptoms that are
evidences of Muirne’s bipolar disorder are numerous, one of the main of which is the phases
of two different moods that are elevated mood and depressive mood throughout the year and
sudden interchange between the two magnitudes without any prior noticeable change. During
INTRODUCTION
Intellectual Disability can be defined as the inability of using normal mental or
intellectual functions. It affects two main areas, the first of which is intellectual functioning
such as learning various things, solving problems and using normal judgement and the second
is adaptive functioning such as way of communication and way of living independently
(Vissers, Gilissen and Veltman 2016). People with intellectual disability are often observed to
be having Bipolar Disorder. Bipolar Disorder can be defined as the state of mental condition,
which can be characterized by extreme and drastic mood swings including higher emotional
outbursts such as mania or hypomania and lower emotional state like depression (Grunze
2015). In the given case study, Muirne is a 49 year old woman who has severe intellectual
disability and also suffers from bipolar disorder which was first diagnosed in her late 20s. She
also exhibits signs of being in the autistic spectrum. In this study, the case of Muirne will be
studied in details and the symptoms of bipolar disorder she is showing, assessment of her
mental health, complexities of living with a severe intellectual disability, autistic spectrum
and bipolar disorder and the interventions available for Muirne’s short term and long term
care plan.
SYMPTOMS OF BIPOLAR DEPRESSION MUIRNE DISPLAYED
There are quite a few symptoms of bipolar disorder that Muirne has been showing. As
Muirne also has autistic spectrum disorders, therefore many of the symptoms coincide with
that of bipolar disorder. Both the conditions have individually left imprint on the nature of
Murine and it is very evident and distinguishable from her behaviour. The symptoms that are
evidences of Muirne’s bipolar disorder are numerous, one of the main of which is the phases
of two different moods that are elevated mood and depressive mood throughout the year and
sudden interchange between the two magnitudes without any prior noticeable change. During
2CASE STUDY
the elevated phase of her mood, she has been observed to be in an extreme active state, often
assaults anyone near her, tends to shout, run, jump and bang or knock the furnitures present
near her. During the depressed phase of her mood, she has been observed to be increasingly
irritated and less active (Allardyce et al. 2018). This phase also can be distinguished by
Muirne’s increasing self injurious behaviour causing scars all over arms and thighs from
rigorous scratching over the years. The self injurious behaviour of Muirne is also a noted
symptom of bipolar disorder (Ferron et al. 2016). A pattern has also been found identifying
the time of onset of her sudden mood change, which is mostly observed in the pattern of two
weeks of elevated phase which is followed by a week of depressed phase. Another symptom
of bipolar disorder observed in Muirne is she does not have a liking for surprises and changes
in the daily routine (Martino Samamé and Strejilevich 2016). Apart from these symptoms,
she has also increasingly shown decreasing level of interest in the activities, she once enjoyed
doing. This is also a noted symptom of bipolar disorder (Vancampfort et al. 2017).
ASSESSMENT OF MURINE’S MENTAL HEALTH
Muirne’s mental status can be assessed using two assessment tools that are PAS-ADD
checklist and PIMRA. The PAS-ADD checklist stands for psychiatric assessment schedule
for adults having developmental disabilities checklist which is diagnosing instrument
formulated for helping the caregivers to identify the problems associated with intellectual
disabilities. It either uses a four-point rating scale or six-point rating scale to determine the
severity of the disorder. The scales are made on the basis of symptoms related to psychiatric
disorders. Here Muirne is undergoing three phases of depression- depressive, elevated and
latter phase. The low mood phase lasts for a longer time approximately 2 weeks whereas the
elated phase is for 1 week. The PAS-ADD checklist is filled using an interview of the patient
as well as the carer. The psychiatric assessment is searched for various patterns of symptoms
for depression. These symptoms include- low mood, withdrawal from social activity, loss of
the elevated phase of her mood, she has been observed to be in an extreme active state, often
assaults anyone near her, tends to shout, run, jump and bang or knock the furnitures present
near her. During the depressed phase of her mood, she has been observed to be increasingly
irritated and less active (Allardyce et al. 2018). This phase also can be distinguished by
Muirne’s increasing self injurious behaviour causing scars all over arms and thighs from
rigorous scratching over the years. The self injurious behaviour of Muirne is also a noted
symptom of bipolar disorder (Ferron et al. 2016). A pattern has also been found identifying
the time of onset of her sudden mood change, which is mostly observed in the pattern of two
weeks of elevated phase which is followed by a week of depressed phase. Another symptom
of bipolar disorder observed in Muirne is she does not have a liking for surprises and changes
in the daily routine (Martino Samamé and Strejilevich 2016). Apart from these symptoms,
she has also increasingly shown decreasing level of interest in the activities, she once enjoyed
doing. This is also a noted symptom of bipolar disorder (Vancampfort et al. 2017).
ASSESSMENT OF MURINE’S MENTAL HEALTH
Muirne’s mental status can be assessed using two assessment tools that are PAS-ADD
checklist and PIMRA. The PAS-ADD checklist stands for psychiatric assessment schedule
for adults having developmental disabilities checklist which is diagnosing instrument
formulated for helping the caregivers to identify the problems associated with intellectual
disabilities. It either uses a four-point rating scale or six-point rating scale to determine the
severity of the disorder. The scales are made on the basis of symptoms related to psychiatric
disorders. Here Muirne is undergoing three phases of depression- depressive, elevated and
latter phase. The low mood phase lasts for a longer time approximately 2 weeks whereas the
elated phase is for 1 week. The PAS-ADD checklist is filled using an interview of the patient
as well as the carer. The psychiatric assessment is searched for various patterns of symptoms
for depression. These symptoms include- low mood, withdrawal from social activity, loss of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CASE STUDY
interest, guilt, energy loss, exhaustion, loss of hope, loss of sexual activities. For having a
mild depressive episode, the criteria include sustained depressive mood for atleast two weeks
along with either low energy or reduced interest in activities. In case of Muirne, who shows
depressive mood for two weeks and also has loss of interest in engaging into activities
therefore meets the criteria for mild depression. Any symptoms additional to these symptoms
would result in moderate to severe form of depression as rated by the scale, where the severe
form is the highest scale. For a six factor dependent PAS-ADD checklist, a questionnaire is
prepared with items related to psychotic disorders. The content of items include disturbances
in the basic habits of the patient, anxiety, psychosis which were not present in case of
Muirne, however she showed symptoms of depression such as irritable behaviour and
cognitive symptoms such as loss of interest (Martorell et al. 2017).
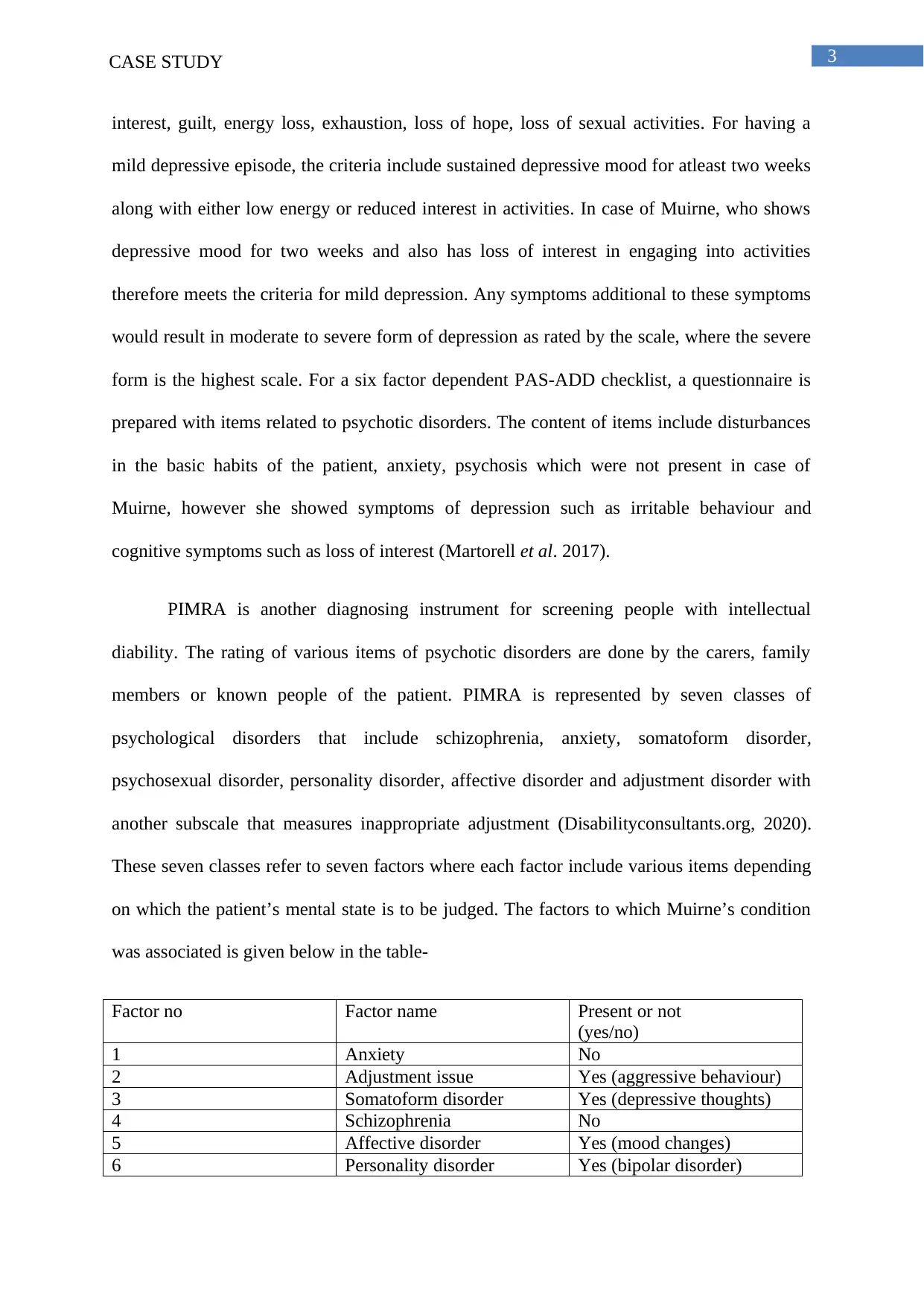
PIMRA is another diagnosing instrument for screening people with intellectual
diability. The rating of various items of psychotic disorders are done by the carers, family
members or known people of the patient. PIMRA is represented by seven classes of
psychological disorders that include schizophrenia, anxiety, somatoform disorder,
psychosexual disorder, personality disorder, affective disorder and adjustment disorder with
another subscale that measures inappropriate adjustment (Disabilityconsultants.org, 2020).
These seven classes refer to seven factors where each factor include various items depending
on which the patient’s mental state is to be judged. The factors to which Muirne’s condition
was associated is given below in the table-
Factor no Factor name Present or not
(yes/no)
1 Anxiety No
2 Adjustment issue Yes (aggressive behaviour)
3 Somatoform disorder Yes (depressive thoughts)
4 Schizophrenia No
5 Affective disorder Yes (mood changes)
6 Personality disorder Yes (bipolar disorder)
interest, guilt, energy loss, exhaustion, loss of hope, loss of sexual activities. For having a
mild depressive episode, the criteria include sustained depressive mood for atleast two weeks
along with either low energy or reduced interest in activities. In case of Muirne, who shows
depressive mood for two weeks and also has loss of interest in engaging into activities
therefore meets the criteria for mild depression. Any symptoms additional to these symptoms
would result in moderate to severe form of depression as rated by the scale, where the severe
form is the highest scale. For a six factor dependent PAS-ADD checklist, a questionnaire is
prepared with items related to psychotic disorders. The content of items include disturbances
in the basic habits of the patient, anxiety, psychosis which were not present in case of
Muirne, however she showed symptoms of depression such as irritable behaviour and
cognitive symptoms such as loss of interest (Martorell et al. 2017).
PIMRA is another diagnosing instrument for screening people with intellectual
diability. The rating of various items of psychotic disorders are done by the carers, family
members or known people of the patient. PIMRA is represented by seven classes of
psychological disorders that include schizophrenia, anxiety, somatoform disorder,
psychosexual disorder, personality disorder, affective disorder and adjustment disorder with
another subscale that measures inappropriate adjustment (Disabilityconsultants.org, 2020).
These seven classes refer to seven factors where each factor include various items depending
on which the patient’s mental state is to be judged. The factors to which Muirne’s condition
was associated is given below in the table-
Factor no Factor name Present or not
(yes/no)
1 Anxiety No
2 Adjustment issue Yes (aggressive behaviour)
3 Somatoform disorder Yes (depressive thoughts)
4 Schizophrenia No
5 Affective disorder Yes (mood changes)
6 Personality disorder Yes (bipolar disorder)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CASE STUDY
7 Psychosexual disorder No
According to this assessment scale, Muirne is susceptible to most of the factors of
PIMRA tool. The validity of this assessment tool is indicated by the symptoms shown by
Muirne. She suffered from bipolar disorder, depressive mood, and aggressive behaviour not
only towards herself but towards the staff. The four factors that are adjustment, somatoform,
personality and affective disorders showed high correlation with the scales of PIMRA
whereas the rest showed less or no correlation with PIMRA scales because the latter was not
related to the symptoms of Muirne’s mental state. Since most of the factors were present in
Muirne, she suffered from severe intellectual disability (McCarthy and Chaplin, 2016).
COMPLEXITIES OF LIVING WITH AUTISTIC TENDENCY AND
BIPOLAR DISORDER
It has been observed that about 27 percent of individuals having autistic tendencies
have bipolar disorder and vice versa (Selten et al. 2015). There are various complexities that
an individual suffering having severe intellectual disability with bipolar disorder and autistic
tendencies as well as their families face. The individuals having severe intellectual disability
as well as autistic tendency and bipolar disorder are dependent on external assistance for
performing activities of daily living. Activities of daily living can be defined as the routine
daily activities that every individual does including eating, bathing, toileting, getting dressed,
continence and transferring (Träger et al. 2017). People suffering from autistic tendency and
bipolar disorder are often observed to be in the phase where they themselves cannot do these
essential works and needs assistance for it, proving it as one of the main complexities.
Assistance in performing activities of daily living can be provided by the family members or
health carers depending on the severity and financial condition. People with the above
mentioned conditions feels much isolated even in presence of known people. Therefore, it is
7 Psychosexual disorder No
According to this assessment scale, Muirne is susceptible to most of the factors of
PIMRA tool. The validity of this assessment tool is indicated by the symptoms shown by
Muirne. She suffered from bipolar disorder, depressive mood, and aggressive behaviour not
only towards herself but towards the staff. The four factors that are adjustment, somatoform,
personality and affective disorders showed high correlation with the scales of PIMRA
whereas the rest showed less or no correlation with PIMRA scales because the latter was not
related to the symptoms of Muirne’s mental state. Since most of the factors were present in
Muirne, she suffered from severe intellectual disability (McCarthy and Chaplin, 2016).
COMPLEXITIES OF LIVING WITH AUTISTIC TENDENCY AND
BIPOLAR DISORDER
It has been observed that about 27 percent of individuals having autistic tendencies
have bipolar disorder and vice versa (Selten et al. 2015). There are various complexities that
an individual suffering having severe intellectual disability with bipolar disorder and autistic
tendencies as well as their families face. The individuals having severe intellectual disability
as well as autistic tendency and bipolar disorder are dependent on external assistance for
performing activities of daily living. Activities of daily living can be defined as the routine
daily activities that every individual does including eating, bathing, toileting, getting dressed,
continence and transferring (Träger et al. 2017). People suffering from autistic tendency and
bipolar disorder are often observed to be in the phase where they themselves cannot do these
essential works and needs assistance for it, proving it as one of the main complexities.
Assistance in performing activities of daily living can be provided by the family members or
health carers depending on the severity and financial condition. People with the above
mentioned conditions feels much isolated even in presence of known people. Therefore, it is
5CASE STUDY
very crucial to make them feel loved and cared in a continuous basis, so that their condition
does not worsen (Dowling 2015). There is also a notable tendency of shaming and abusing
people with mental illnesses that has been observed widely. The social taboos are extremely
predominant even now and are also causing an increase in the death toll of people suffering
from bipolar disorder and autistic tendencies. The death toll is increasing as the individuals
with these conditions are often seen to exhibit a suicidal and self injuring tendencies, which
escalate very quickly upon hitting their weak points (Esmaeelpour and Sasani 2016). Apart
from this, the social taboo and abuse often leads the patients to avoid treatment as well as stay
isolated from everyone, which also decreases their chances of getting better. Another
important complexity that the people having bipolar disorder and autistic tendencies is their
personal relationships get majorly affected because of the unpredictability of their mood and
the sudden changes in their emotions (Granek et al. 2016)
SHORT TERM & LONG TERM INTERVENTIONS
There are quite a few interventions that can be implemented in the case of Muirne
which can be short term as well as long term. Short term interventions that can be
implemented to treat Muirne include continuous support so that her abilities to perform her
daily activities gets enhanced to a point where she can do her own work. Short term
intervention also include prescribing psychotropic medications, which can be defined as the
medications that has ability to treat bipolar disorder along with depression (Rei et al. 2017).
There has been recorded evidences suggesting that psychotropic medications also cause
various side effects such as drowsiness, abnormal weight gain and sexual dysfunction.
Therefore, it is very important for prescribing the drug in correct dosage and as per the
severity of her condition. Drugs like olanzapine and quentiapine might prove helpful in
treating Muirne’s bipolar disorder. These medicines would help in treating her mood swings
and the frequency of the onset.
very crucial to make them feel loved and cared in a continuous basis, so that their condition
does not worsen (Dowling 2015). There is also a notable tendency of shaming and abusing
people with mental illnesses that has been observed widely. The social taboos are extremely
predominant even now and are also causing an increase in the death toll of people suffering
from bipolar disorder and autistic tendencies. The death toll is increasing as the individuals
with these conditions are often seen to exhibit a suicidal and self injuring tendencies, which
escalate very quickly upon hitting their weak points (Esmaeelpour and Sasani 2016). Apart
from this, the social taboo and abuse often leads the patients to avoid treatment as well as stay
isolated from everyone, which also decreases their chances of getting better. Another
important complexity that the people having bipolar disorder and autistic tendencies is their
personal relationships get majorly affected because of the unpredictability of their mood and
the sudden changes in their emotions (Granek et al. 2016)
SHORT TERM & LONG TERM INTERVENTIONS
There are quite a few interventions that can be implemented in the case of Muirne
which can be short term as well as long term. Short term interventions that can be
implemented to treat Muirne include continuous support so that her abilities to perform her
daily activities gets enhanced to a point where she can do her own work. Short term
intervention also include prescribing psychotropic medications, which can be defined as the
medications that has ability to treat bipolar disorder along with depression (Rei et al. 2017).
There has been recorded evidences suggesting that psychotropic medications also cause
various side effects such as drowsiness, abnormal weight gain and sexual dysfunction.
Therefore, it is very important for prescribing the drug in correct dosage and as per the
severity of her condition. Drugs like olanzapine and quentiapine might prove helpful in
treating Muirne’s bipolar disorder. These medicines would help in treating her mood swings
and the frequency of the onset.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CASE STUDY
The long term intervention include cognitive behavioural therapy, patient education as
well as making her compliant to take the medications. Cognitive behavioural therapy can be
defined as the therapy that helps in improving the mental condition by challenging and
ultimately changing the thought process, behaviour and emotions. It is widely prescribed for
patients suffering from various mental illnesses like bipolar disorder and depression. As both
of these conditions are spotted in Muirne, this therapy would prove extremely beneficial for
her condition. However, the therapist should proceed with the treatment using non-verbal
communication, as the patient is more comfortable in that as per the given case study (Powel
2017). Patient education is also one of the important aspects of the long term intervention to
improve Muirne’s condition. It can be defined as the process in which the healthcare
professionals enlighten the patients about their condition, treatment strategies and the
consequences that the patient might face thus, educating them about the problems so that they
might work towards enhancing the treatment to achieve better outcomes. In the case of
Muirne, the healthcare professionals might face difficulty in imparting the education to her
because of her condition and behaviour. However, during the active or elevated phase of her
mood the education can be imparted by experts in the form of interactive sessions (Goodwin
2016). This education if correctly imparted on Muirne would help her to become conscious to
a certain extent that she compliantly uptake the prescribed medication and the strategies to
improve her condition (Levin et al. 2016).
CONCLUSION
Thus, to conclude the paper it can be stated that, Muirne is in a complicated situation
and the conditions she is having, which include bipolar disorder and autistic spectrum, might
aid in rapid and drastic deterioration of her health. There are also various complexities of
living with this condition including social seclusion, isolation, which might also lead to self
harming activities. Therefore, to refrain her from committing any such activity as well as
The long term intervention include cognitive behavioural therapy, patient education as
well as making her compliant to take the medications. Cognitive behavioural therapy can be
defined as the therapy that helps in improving the mental condition by challenging and
ultimately changing the thought process, behaviour and emotions. It is widely prescribed for
patients suffering from various mental illnesses like bipolar disorder and depression. As both
of these conditions are spotted in Muirne, this therapy would prove extremely beneficial for
her condition. However, the therapist should proceed with the treatment using non-verbal
communication, as the patient is more comfortable in that as per the given case study (Powel
2017). Patient education is also one of the important aspects of the long term intervention to
improve Muirne’s condition. It can be defined as the process in which the healthcare
professionals enlighten the patients about their condition, treatment strategies and the
consequences that the patient might face thus, educating them about the problems so that they
might work towards enhancing the treatment to achieve better outcomes. In the case of
Muirne, the healthcare professionals might face difficulty in imparting the education to her
because of her condition and behaviour. However, during the active or elevated phase of her
mood the education can be imparted by experts in the form of interactive sessions (Goodwin
2016). This education if correctly imparted on Muirne would help her to become conscious to
a certain extent that she compliantly uptake the prescribed medication and the strategies to
improve her condition (Levin et al. 2016).
CONCLUSION
Thus, to conclude the paper it can be stated that, Muirne is in a complicated situation
and the conditions she is having, which include bipolar disorder and autistic spectrum, might
aid in rapid and drastic deterioration of her health. There are also various complexities of
living with this condition including social seclusion, isolation, which might also lead to self
harming activities. Therefore, to refrain her from committing any such activity as well as
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY
improving her condition, intervention strategies should be designed properly. The
intervention strategies include short term strategies like medication and assistance in activity
of daily living whereas, the long term interventions include cognitive behavioural therapy and
patient education. Following these might improve the condition of Muirne.
improving her condition, intervention strategies should be designed properly. The
intervention strategies include short term strategies like medication and assistance in activity
of daily living whereas, the long term interventions include cognitive behavioural therapy and
patient education. Following these might improve the condition of Muirne.
8CASE STUDY
REFERENCES
Allardyce, J., Leonenko, G., Hamshere, M., Pardiñas, A.F., Forty, L., Knott, S., Gordon-
Smith, K., Porteous, D.J., Haywood, C., Di Florio, A. and Jones, L., 2018. Association
between schizophrenia-related polygenic liability and the occurrence and level of mood-
incongruent psychotic symptoms in bipolar disorder. JAMA psychiatry, 75(1), pp.28-35.
Disabilityconsultants.org, 2020. Psychopathology - PIMRA. [online]
Disabilityconsultants.org. Available at: <http://www.disabilityconsultants.org/PIMRA.php>
[Accessed 16 April 2020].
Dowling, J., 2015. When someone you love has bipolar disorder: Experiences of family
members (Doctoral dissertation, City University of Seattle).
Esmaeelpour, E. and Sasani, F., 2016. The effect of bipolar mood disorder on Sadegh
Hedayat’s letters. Journal of psycholinguistic research, 45(2), pp.367-377.
Ferro, M.A., 2016. Major depressive disorder, suicidal behaviour, bipolar disorder, and
generalised anxiety disorder among emerging adults with and without chronic health
conditions. Epidemiology and psychiatric sciences, 25(5), pp.462-474.
Goodwin, G.M., 2016. Bipolar disorder. Medicine, 44(11), pp.661-663.
Granek, L., Danan, D., Bersudsky, Y. and Osher, Y., 2016. Living with bipolar disorder: the
impact on patients, spouses, and their marital relationship. Bipolar disorders, 18(2), pp.192-
199.
Grunze, H., 2015. Bipolar disorder. In Neurobiology of brain disorders (pp. 655-673).
Academic Press.
REFERENCES
Allardyce, J., Leonenko, G., Hamshere, M., Pardiñas, A.F., Forty, L., Knott, S., Gordon-
Smith, K., Porteous, D.J., Haywood, C., Di Florio, A. and Jones, L., 2018. Association
between schizophrenia-related polygenic liability and the occurrence and level of mood-
incongruent psychotic symptoms in bipolar disorder. JAMA psychiatry, 75(1), pp.28-35.
Disabilityconsultants.org, 2020. Psychopathology - PIMRA. [online]
Disabilityconsultants.org. Available at: <http://www.disabilityconsultants.org/PIMRA.php>
[Accessed 16 April 2020].
Dowling, J., 2015. When someone you love has bipolar disorder: Experiences of family
members (Doctoral dissertation, City University of Seattle).
Esmaeelpour, E. and Sasani, F., 2016. The effect of bipolar mood disorder on Sadegh
Hedayat’s letters. Journal of psycholinguistic research, 45(2), pp.367-377.
Ferro, M.A., 2016. Major depressive disorder, suicidal behaviour, bipolar disorder, and
generalised anxiety disorder among emerging adults with and without chronic health
conditions. Epidemiology and psychiatric sciences, 25(5), pp.462-474.
Goodwin, G.M., 2016. Bipolar disorder. Medicine, 44(11), pp.661-663.
Granek, L., Danan, D., Bersudsky, Y. and Osher, Y., 2016. Living with bipolar disorder: the
impact on patients, spouses, and their marital relationship. Bipolar disorders, 18(2), pp.192-
199.
Grunze, H., 2015. Bipolar disorder. In Neurobiology of brain disorders (pp. 655-673).
Academic Press.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CASE STUDY
Levin, J.B., Aebi, M.E., Tatsuoka, C., Cassidy, K.A. and Sajatovic, M., 2016. Adherence to
psychotropic and nonpsychotropic medication among patients with bipolar disorder and
general medical conditions. Psychiatric Services, 67(3), pp.342-345.
Martino, D.J., Samamé, C. and Strejilevich, S.A., 2016. Stability of facial emotion
recognition performance in bipolar disorder. Psychiatry research, 243, pp.182-184.
Martorell, A., González, M.C., Gutiérrez, P., Rincón, F. and Núñez‐Polo, M.H., 2017.
Spanish validation of the PAS‐ADD Checklist Questionnaire for people with intellectual
disabilities for Spanish population. Journal of Intellectual Disability Research, 61(10),
pp.909-915.
McCarthy, J. and Chaplin, E., 2016. Mental disorders. Psychiatric and Behavioural Disorders
in Intellectual and Developmental Disabilities, p.89.
Powell, T., 2017. The Mental Health Handbook: A Cognitive Behavioural Approach.
Routledge.
Rej, S., Herrmann, N., Shulman, K., Fischer, H.D., Fung, K. and Gruneir, A., 2017. Current
psychotropic medication prescribing patterns in late‐life bipolar disorder. International
journal of geriatric psychiatry, 32(12), pp.1459-1465.
Selten, J.P., Lundberg, M., Rai, D. and Magnusson, C., 2015. Risks for nonaffective
psychotic disorder and bipolar disorder in young people with autism spectrum disorder: a
population-based study. JAMA psychiatry, 72(5), pp.483-489.
Träger, C., Decker, L., Wæhrens, E.E., Knorr, U., Miskowiak, K. and Vinberg, M., 2017.
Influences of patient informed cognitive complaints on activities of daily living in patients
with bipolar disorder. An exploratory cross-sectional study. Psychiatry research, 249,
pp.268-274.
Levin, J.B., Aebi, M.E., Tatsuoka, C., Cassidy, K.A. and Sajatovic, M., 2016. Adherence to
psychotropic and nonpsychotropic medication among patients with bipolar disorder and
general medical conditions. Psychiatric Services, 67(3), pp.342-345.
Martino, D.J., Samamé, C. and Strejilevich, S.A., 2016. Stability of facial emotion
recognition performance in bipolar disorder. Psychiatry research, 243, pp.182-184.
Martorell, A., González, M.C., Gutiérrez, P., Rincón, F. and Núñez‐Polo, M.H., 2017.
Spanish validation of the PAS‐ADD Checklist Questionnaire for people with intellectual
disabilities for Spanish population. Journal of Intellectual Disability Research, 61(10),
pp.909-915.
McCarthy, J. and Chaplin, E., 2016. Mental disorders. Psychiatric and Behavioural Disorders
in Intellectual and Developmental Disabilities, p.89.
Powell, T., 2017. The Mental Health Handbook: A Cognitive Behavioural Approach.
Routledge.
Rej, S., Herrmann, N., Shulman, K., Fischer, H.D., Fung, K. and Gruneir, A., 2017. Current
psychotropic medication prescribing patterns in late‐life bipolar disorder. International
journal of geriatric psychiatry, 32(12), pp.1459-1465.
Selten, J.P., Lundberg, M., Rai, D. and Magnusson, C., 2015. Risks for nonaffective
psychotic disorder and bipolar disorder in young people with autism spectrum disorder: a
population-based study. JAMA psychiatry, 72(5), pp.483-489.
Träger, C., Decker, L., Wæhrens, E.E., Knorr, U., Miskowiak, K. and Vinberg, M., 2017.
Influences of patient informed cognitive complaints on activities of daily living in patients
with bipolar disorder. An exploratory cross-sectional study. Psychiatry research, 249,
pp.268-274.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10CASE STUDY
Vancampfort, D., Firth, J., Schuch, F.B., Rosenbaum, S., Mugisha, J., Hallgren, M., Probst,
M., Ward, P.B., Gaughran, F., De Hert, M. and Carvalho, A.F., 2017. Sedentary behavior and
physical activity levels in people with schizophrenia, bipolar disorder and major depressive
disorder: a global systematic review and meta‐analysis. World Psychiatry, 16(3), pp.308-315.
Vissers, L.E., Gilissen, C. and Veltman, J.A., 2016. Genetic studies in intellectual disability
and related disorders. Nature Reviews Genetics, 17(1), pp.9-18.
Vancampfort, D., Firth, J., Schuch, F.B., Rosenbaum, S., Mugisha, J., Hallgren, M., Probst,
M., Ward, P.B., Gaughran, F., De Hert, M. and Carvalho, A.F., 2017. Sedentary behavior and
physical activity levels in people with schizophrenia, bipolar disorder and major depressive
disorder: a global systematic review and meta‐analysis. World Psychiatry, 16(3), pp.308-315.
Vissers, L.E., Gilissen, C. and Veltman, J.A., 2016. Genetic studies in intellectual disability
and related disorders. Nature Reviews Genetics, 17(1), pp.9-18.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





