Intraoperative Awareness: Incidence, Sequelae, and Prevention
VerifiedAdded on 2022/08/31
|7
|6177
|24
Report
AI Summary
This report is a review article discussing intraoperative awareness, its incidence, sequelae, and prevention. The article explores the controversies and non-controversies surrounding awareness during anesthesia, including the effectiveness of the modified Brice interview in detecting awareness with explicit recall, and the higher incidence of awareness without explicit recall. It also examines the link between intraoperative awareness and post-traumatic stress disorder (PTSD), as well as the role of processed electroencephalographic monitoring in preventing awareness. Furthermore, it addresses the increased incidence of awareness when neuromuscular blocking agents are used. The review synthesizes evidence from multiple studies, highlighting key findings and implications for clinical practice and patient safety.
R E V I E W A R T I C L E
Intraoperative awareness: controversies
and non-controversies
G. A. Mashour1,* and M. S. Avidan2
1University of Michigan Medical School, Ann Arbor, MI, USA, and2Washington University School of Medicine,
St Louis, MO, USA
*Corresponding author. E-mail: gmashour@med.umich.edu
Abstract
Intraoperative awareness, with or without recall, continues to be a topic of clinical significance and neurobiological interest.
In this article, we review evidence pertaining to the incidence, sequelae, and prevention of intraoperative awareness. We also
assess which aspects of the complication are well understood (i.e. non-controversial) and which require further research for
clarification (i.e. controversial).
Key words: anaesthesia, awareness, consciousness, post-traumatic stress disorder
Editor’s key points
• Recent large prospective studies have addressed the
incidence, detection, and prevention of awareness under
general anaesthesia.
• While important controversies remain, a number of con-
cepts regarding intraoperative awareness can be consid-
ered non-controversial.
• Controversies remain in both the aetiological and the
neurobiological bases of awareness.
The unintended experience and memory of surgical or proced-
ural events can be devastating for patients and remains a dynam-
ic area of investigation. Intraoperative awareness, with or
without explicit episodic recall, is relevant to patient safety, stan-
dards for intraoperative monitoring, and the search for the neural
correlates of consciousness. The objective of this narrative
review is to assess the state of the field by addressing key topics
related to intraoperative awareness and to consider whether the
evidence associated with these topics should be deemed contro-
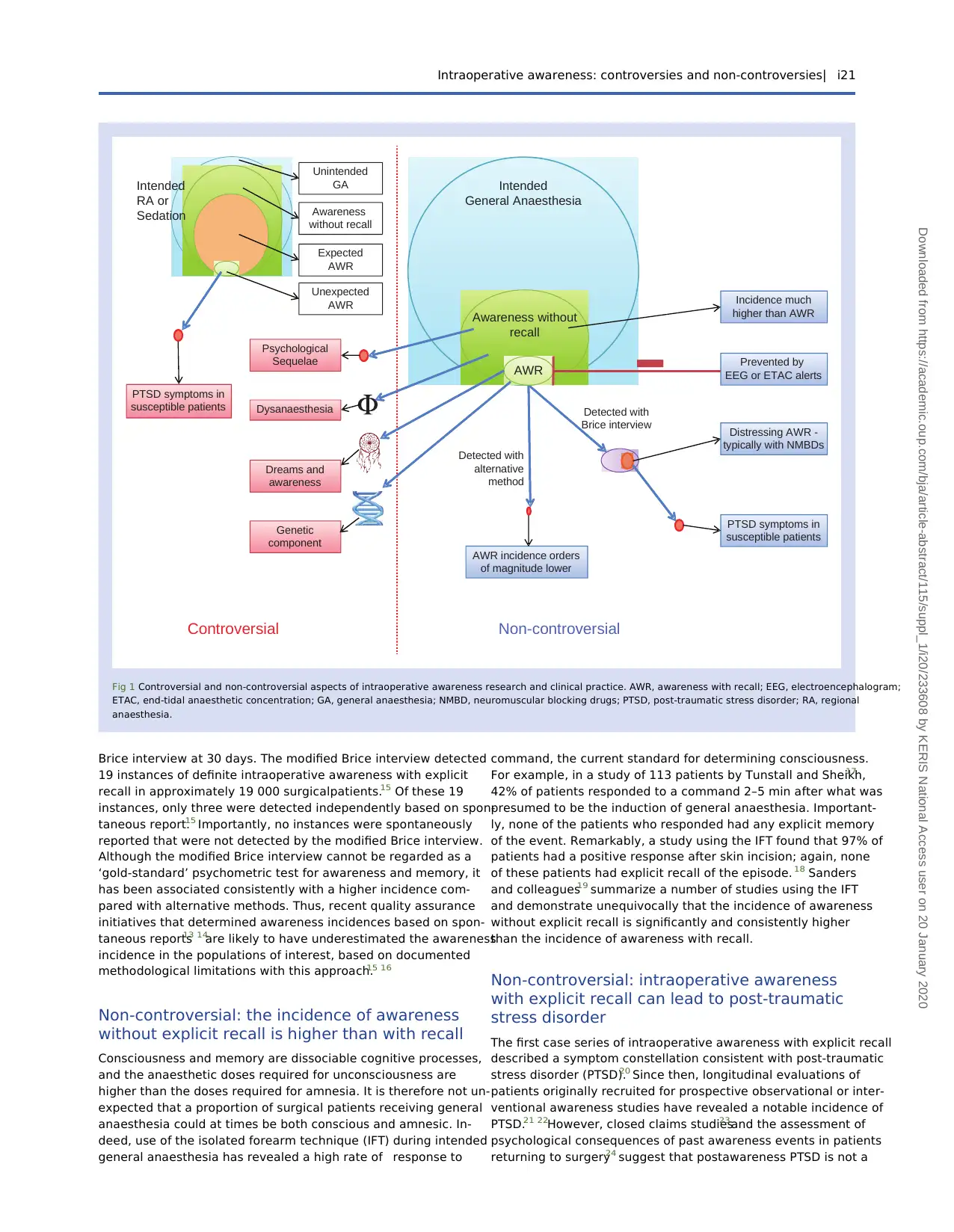
versial or non-controversial (see Figure 1 for summary).
Non-controversial: the modified Brice interview
detects more instances of intraoperative
awareness with explicit recall than alternative
methods
Multiple prospective studies using the modified Brice interview1
as the method of assessing intraoperative awareness with expli-
cit recall have consistently found an incidence of approximately
1–2 per 10002–4 or higher.5–10 In contrast, studies using in-
struments without specific questions pertaining to awareness
(such as Pollard and colleagues),11 quality assurance data (such
as Mashour and colleagues)12 or spontaneous reports [such as
the recent National Audit Project (NAP) 5]13 14 have consistently
found the incidence to be lower by an order of magnitude
(Table 1).11–14 It was unclear from these conflicting reports
whether the differences in incidence resulted from disparities
in patient population, anaesthetic technique, clinical severity,
or method of detection. In an attempt to resolve the controversy
across studies and study populations, Mashour and colleagues15
compared the incidence of intraoperative awareness with expli-
cit recall in a single population of surgical patients who received
both a standard postoperative evaluation (without a structured
interview intended to detect awareness) and a single modified
Accepted: December 4, 2014
© The Author 2015. Published by Oxford University Press on behalf of the British Journal of Anaesthesia. All rights reserved.
For Permissions, please email: journals.permissions@oup.com
British Journal of Anaesthesia 2015, i20–i26
doi: 10.1093/bja/aev034
Advance Access Publication Date: 3 March 2015
Review Article
i20
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
Intraoperative awareness: controversies
and non-controversies
G. A. Mashour1,* and M. S. Avidan2
1University of Michigan Medical School, Ann Arbor, MI, USA, and2Washington University School of Medicine,
St Louis, MO, USA
*Corresponding author. E-mail: gmashour@med.umich.edu
Abstract
Intraoperative awareness, with or without recall, continues to be a topic of clinical significance and neurobiological interest.
In this article, we review evidence pertaining to the incidence, sequelae, and prevention of intraoperative awareness. We also
assess which aspects of the complication are well understood (i.e. non-controversial) and which require further research for
clarification (i.e. controversial).
Key words: anaesthesia, awareness, consciousness, post-traumatic stress disorder
Editor’s key points
• Recent large prospective studies have addressed the
incidence, detection, and prevention of awareness under
general anaesthesia.
• While important controversies remain, a number of con-
cepts regarding intraoperative awareness can be consid-
ered non-controversial.
• Controversies remain in both the aetiological and the
neurobiological bases of awareness.
The unintended experience and memory of surgical or proced-
ural events can be devastating for patients and remains a dynam-
ic area of investigation. Intraoperative awareness, with or
without explicit episodic recall, is relevant to patient safety, stan-
dards for intraoperative monitoring, and the search for the neural
correlates of consciousness. The objective of this narrative
review is to assess the state of the field by addressing key topics
related to intraoperative awareness and to consider whether the
evidence associated with these topics should be deemed contro-
versial or non-controversial (see Figure 1 for summary).
Non-controversial: the modified Brice interview
detects more instances of intraoperative
awareness with explicit recall than alternative
methods
Multiple prospective studies using the modified Brice interview1
as the method of assessing intraoperative awareness with expli-
cit recall have consistently found an incidence of approximately
1–2 per 10002–4 or higher.5–10 In contrast, studies using in-
struments without specific questions pertaining to awareness
(such as Pollard and colleagues),11 quality assurance data (such
as Mashour and colleagues)12 or spontaneous reports [such as
the recent National Audit Project (NAP) 5]13 14 have consistently
found the incidence to be lower by an order of magnitude
(Table 1).11–14 It was unclear from these conflicting reports
whether the differences in incidence resulted from disparities
in patient population, anaesthetic technique, clinical severity,
or method of detection. In an attempt to resolve the controversy
across studies and study populations, Mashour and colleagues15
compared the incidence of intraoperative awareness with expli-
cit recall in a single population of surgical patients who received
both a standard postoperative evaluation (without a structured
interview intended to detect awareness) and a single modified
Accepted: December 4, 2014
© The Author 2015. Published by Oxford University Press on behalf of the British Journal of Anaesthesia. All rights reserved.
For Permissions, please email: journals.permissions@oup.com
British Journal of Anaesthesia 2015, i20–i26
doi: 10.1093/bja/aev034
Advance Access Publication Date: 3 March 2015
Review Article
i20
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Brice interview at 30 days. The modified Brice interview detected
19 instances of definite intraoperative awareness with explicit
recall in approximately 19 000 surgicalpatients.15 Of these 19
instances, only three were detected independently based on spon-
taneous report.15 Importantly, no instances were spontaneously
reported that were not detected by the modified Brice interview.
Although the modified Brice interview cannot be regarded as a
‘gold-standard’ psychometric test for awareness and memory, it
has been associated consistently with a higher incidence com-
pared with alternative methods. Thus, recent quality assurance
initiatives that determined awareness incidences based on spon-
taneous reports13 14
are likely to have underestimated the awareness
incidence in the populations of interest, based on documented
methodological limitations with this approach.15 16
Non-controversial: the incidence of awareness
without explicit recall is higher than with recall
Consciousness and memory are dissociable cognitive processes,
and the anaesthetic doses required for unconsciousness are
higher than the doses required for amnesia. It is therefore not un-
expected that a proportion of surgical patients receiving general
anaesthesia could at times be both conscious and amnesic. In-
deed, use of the isolated forearm technique (IFT) during intended
general anaesthesia has revealed a high rate of response to
command, the current standard for determining consciousness.
For example, in a study of 113 patients by Tunstall and Sheikh,17
42% of patients responded to a command 2–5 min after what was
presumed to be the induction of general anaesthesia. Important-
ly, none of the patients who responded had any explicit memory
of the event. Remarkably, a study using the IFT found that 97% of
patients had a positive response after skin incision; again, none
of these patients had explicit recall of the episode. 18 Sanders
and colleagues19 summarize a number of studies using the IFT
and demonstrate unequivocally that the incidence of awareness
without explicit recall is significantly and consistently higher
than the incidence of awareness with recall.
Non-controversial: intraoperative awareness
with explicit recall can lead to post-traumatic
stress disorder
The first case series of intraoperative awareness with explicit recall
described a symptom constellation consistent with post-traumatic
stress disorder (PTSD).20 Since then, longitudinal evaluations of
patients originally recruited for prospective observational or inter-
ventional awareness studies have revealed a notable incidence of
PTSD.21 22However, closed claims studies23and the assessment of
psychological consequences of past awareness events in patients
returning to surgery24 suggest that postawareness PTSD is not a
AWR
Awareness without
recall
Intended
General Anaesthesia
Detected with
Brice interview
Detected with
alternative
method
Distressing AWR -
typically with NMBDs
PTSD symptoms in
susceptible patients
Prevented by
EEG or ETAC alerts
Non-controversialControversial
Unexpected
AWR
Unintended
GA
Expected
AWR
Awareness
without recall
PTSD symptoms in
susceptible patients
Psychological
Sequelae
Genetic
component
Dysanaesthesia
Dreams and
awareness
AWR incidence orders
of magnitude lower
Incidence much
higher than AWR
Intended
RA or
Sedation
Fig 1 Controversial and non-controversial aspects of intraoperative awareness research and clinical practice. AWR, awareness with recall; EEG, electroencephalogram;
ETAC, end-tidal anaesthetic concentration; GA, general anaesthesia; NMBD, neuromuscular blocking drugs; PTSD, post-traumatic stress disorder; RA, regional
anaesthesia.
Intraoperative awareness: controversies and non-controversies| i21
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
19 instances of definite intraoperative awareness with explicit
recall in approximately 19 000 surgicalpatients.15 Of these 19
instances, only three were detected independently based on spon-
taneous report.15 Importantly, no instances were spontaneously
reported that were not detected by the modified Brice interview.
Although the modified Brice interview cannot be regarded as a
‘gold-standard’ psychometric test for awareness and memory, it
has been associated consistently with a higher incidence com-
pared with alternative methods. Thus, recent quality assurance
initiatives that determined awareness incidences based on spon-
taneous reports13 14
are likely to have underestimated the awareness
incidence in the populations of interest, based on documented
methodological limitations with this approach.15 16
Non-controversial: the incidence of awareness
without explicit recall is higher than with recall
Consciousness and memory are dissociable cognitive processes,
and the anaesthetic doses required for unconsciousness are
higher than the doses required for amnesia. It is therefore not un-
expected that a proportion of surgical patients receiving general
anaesthesia could at times be both conscious and amnesic. In-
deed, use of the isolated forearm technique (IFT) during intended
general anaesthesia has revealed a high rate of response to
command, the current standard for determining consciousness.
For example, in a study of 113 patients by Tunstall and Sheikh,17
42% of patients responded to a command 2–5 min after what was
presumed to be the induction of general anaesthesia. Important-
ly, none of the patients who responded had any explicit memory
of the event. Remarkably, a study using the IFT found that 97% of
patients had a positive response after skin incision; again, none
of these patients had explicit recall of the episode. 18 Sanders
and colleagues19 summarize a number of studies using the IFT
and demonstrate unequivocally that the incidence of awareness
without explicit recall is significantly and consistently higher
than the incidence of awareness with recall.
Non-controversial: intraoperative awareness
with explicit recall can lead to post-traumatic
stress disorder
The first case series of intraoperative awareness with explicit recall
described a symptom constellation consistent with post-traumatic
stress disorder (PTSD).20 Since then, longitudinal evaluations of
patients originally recruited for prospective observational or inter-
ventional awareness studies have revealed a notable incidence of
PTSD.21 22However, closed claims studies23and the assessment of
psychological consequences of past awareness events in patients
returning to surgery24 suggest that postawareness PTSD is not a
AWR
Awareness without
recall
Intended
General Anaesthesia
Detected with
Brice interview
Detected with
alternative
method
Distressing AWR -
typically with NMBDs
PTSD symptoms in
susceptible patients
Prevented by
EEG or ETAC alerts
Non-controversialControversial
Unexpected
AWR
Unintended
GA
Expected
AWR
Awareness
without recall
PTSD symptoms in
susceptible patients
Psychological
Sequelae
Genetic
component
Dysanaesthesia
Dreams and
awareness
AWR incidence orders
of magnitude lower
Incidence much
higher than AWR
Intended
RA or
Sedation
Fig 1 Controversial and non-controversial aspects of intraoperative awareness research and clinical practice. AWR, awareness with recall; EEG, electroencephalogram;
ETAC, end-tidal anaesthetic concentration; GA, general anaesthesia; NMBD, neuromuscular blocking drugs; PTSD, post-traumatic stress disorder; RA, regional
anaesthesia.
Intraoperative awareness: controversies and non-controversies| i21
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
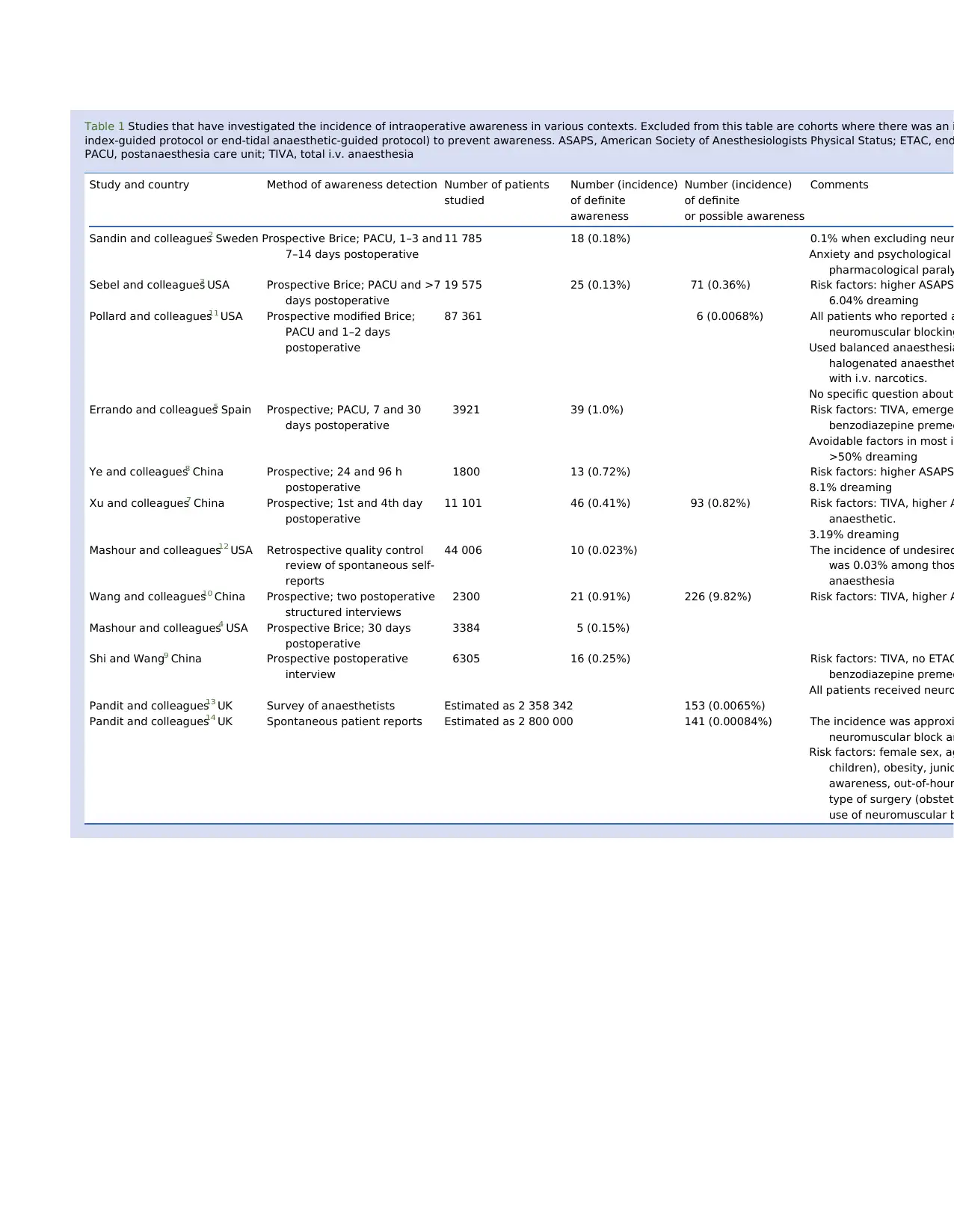
Table 1 Studies that have investigated the incidence of intraoperative awareness in various contexts. Excluded from this table are cohorts where there was an i
index-guided protocol or end-tidal anaesthetic-guided protocol) to prevent awareness. ASAPS, American Society of Anesthesiologists Physical Status; ETAC, end
PACU, postanaesthesia care unit; TIVA, total i.v. anaesthesia
Study and country Method of awareness detection Number of patients
studied
Number (incidence)
of definite
awareness
Number (incidence)
of definite
or possible awareness
Comments
Sandin and colleagues2 Sweden Prospective Brice; PACU, 1–3 and
7–14 days postoperative
11 785 18 (0.18%) 0.1% when excluding neur
Anxiety and psychological
pharmacological paraly
Sebel and colleagues3 USA Prospective Brice; PACU and >7
days postoperative
19 575 25 (0.13%) 71 (0.36%) Risk factors: higher ASAPS
6.04% dreaming
Pollard and colleagues11 USA Prospective modified Brice;
PACU and 1–2 days
postoperative
87 361 6 (0.0068%) All patients who reported a
neuromuscular blocking
Used balanced anaesthesia
halogenated anaesthet
with i.v. narcotics.
No specific question about
Errando and colleagues5 Spain Prospective; PACU, 7 and 30
days postoperative
3921 39 (1.0%) Risk factors: TIVA, emerge
benzodiazepine premed
Avoidable factors in most in
>50% dreaming
Ye and colleagues8 China Prospective; 24 and 96 h
postoperative
1800 13 (0.72%) Risk factors: higher ASAPS
8.1% dreaming
Xu and colleagues7 China Prospective; 1st and 4th day
postoperative
11 101 46 (0.41%) 93 (0.82%) Risk factors: TIVA, higher A
anaesthetic.
3.19% dreaming
Mashour and colleagues12 USA Retrospective quality control
review of spontaneous self-
reports
44 006 10 (0.023%) The incidence of undesired
was 0.03% among thos
anaesthesia
Wang and colleagues10 China Prospective; two postoperative
structured interviews
2300 21 (0.91%) 226 (9.82%) Risk factors: TIVA, higher A
Mashour and colleagues4 USA Prospective Brice; 30 days
postoperative
3384 5 (0.15%)
Shi and Wang9 China Prospective postoperative
interview
6305 16 (0.25%) Risk factors: TIVA, no ETAC
benzodiazepine premed
All patients received neuro
Pandit and colleagues13 UK Survey of anaesthetists Estimated as 2 358 342 153 (0.0065%)
Pandit and colleagues14 UK Spontaneous patient reports Estimated as 2 800 000 141 (0.00084%) The incidence was approxi
neuromuscular block an
Risk factors: female sex, ag
children), obesity, junio
awareness, out-of-hour
type of surgery (obstet
use of neuromuscular b
index-guided protocol or end-tidal anaesthetic-guided protocol) to prevent awareness. ASAPS, American Society of Anesthesiologists Physical Status; ETAC, end
PACU, postanaesthesia care unit; TIVA, total i.v. anaesthesia
Study and country Method of awareness detection Number of patients
studied
Number (incidence)
of definite
awareness
Number (incidence)
of definite
or possible awareness
Comments
Sandin and colleagues2 Sweden Prospective Brice; PACU, 1–3 and
7–14 days postoperative
11 785 18 (0.18%) 0.1% when excluding neur
Anxiety and psychological
pharmacological paraly
Sebel and colleagues3 USA Prospective Brice; PACU and >7
days postoperative
19 575 25 (0.13%) 71 (0.36%) Risk factors: higher ASAPS
6.04% dreaming
Pollard and colleagues11 USA Prospective modified Brice;
PACU and 1–2 days
postoperative
87 361 6 (0.0068%) All patients who reported a
neuromuscular blocking
Used balanced anaesthesia
halogenated anaesthet
with i.v. narcotics.
No specific question about
Errando and colleagues5 Spain Prospective; PACU, 7 and 30
days postoperative
3921 39 (1.0%) Risk factors: TIVA, emerge
benzodiazepine premed
Avoidable factors in most in
>50% dreaming
Ye and colleagues8 China Prospective; 24 and 96 h
postoperative
1800 13 (0.72%) Risk factors: higher ASAPS
8.1% dreaming
Xu and colleagues7 China Prospective; 1st and 4th day
postoperative
11 101 46 (0.41%) 93 (0.82%) Risk factors: TIVA, higher A
anaesthetic.
3.19% dreaming
Mashour and colleagues12 USA Retrospective quality control
review of spontaneous self-
reports
44 006 10 (0.023%) The incidence of undesired
was 0.03% among thos
anaesthesia
Wang and colleagues10 China Prospective; two postoperative
structured interviews
2300 21 (0.91%) 226 (9.82%) Risk factors: TIVA, higher A
Mashour and colleagues4 USA Prospective Brice; 30 days
postoperative
3384 5 (0.15%)
Shi and Wang9 China Prospective postoperative
interview
6305 16 (0.25%) Risk factors: TIVA, no ETAC
benzodiazepine premed
All patients received neuro
Pandit and colleagues13 UK Survey of anaesthetists Estimated as 2 358 342 153 (0.0065%)
Pandit and colleagues14 UK Spontaneous patient reports Estimated as 2 800 000 141 (0.00084%) The incidence was approxi
neuromuscular block an
Risk factors: female sex, ag
children), obesity, junio
awareness, out-of-hour
type of surgery (obstet
use of neuromuscular b
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

significant problem. In one study, even a long-term follow-up of
surgical patients who had been formally determined to have in-
traoperative awareness with explicit recall demonstrated no
long-term consequences.25 However, this might be attributable
to the fact that the initial experiences themselves were not par-
ticularly traumatic. A recent multicentre study demonstrates
that PTSD symptoms are indeed more common after definite or
possible awareness with recall,26 and the NAP5 audit highlights
the importance of neuromuscular paralysis in psychologically
traumatic experiences.27 Thus, although certain screening meth-
ods or patient populations might be associated with apparently
low incidences of PTSD after awareness reports, it is no longer a
matter of controversy as to whether or not intraoperative aware-
ness with explicit recall can lead to PTSD or PTSD symptoms.
Non-controversial: processed
electroencephalographic monitoring
is useful in preventing intraoperative
awareness with explicit recall compared
with clinical signs but not compared with
anaesthetic concentration alarms
The role of processed electroencephalographic devices, such as
the bispectral index (BIS) monitor, in the prevention of intrao-
perative awareness with explicit recall is sometimes regarded
as controversial, but should not be. Clear and consistent findings
have emerged from the five major randomized controlled trials
focused on the BIS.4 28–31The B-Aware trial28 demonstrated that
the BIS monitor was effective in reducing definite awareness
events compared with routine clinical care in patients at high
risk for the complication; this has also been demonstrated
for patients receiving total i.v. anaesthesia.31 In contrast, the
BAG-RECALL and B-Unaware trials demonstrated that alarms
based on the BIS are not superior to alarms based on end-tidal
anaesthetic concentration in preventing awareness with explicit
recall in patients at high risk for the complication.29 30The Mich-
igan Awareness Control Study has confirmed these findings
(i.e. BIS superior to clinical signs but not to anaesthetic concen-
tration alerts) in patients at all risk levels for awareness with ex-
plicit recall.4 An article synthesizing the evidence and an updated
Cochrane systematic review reflect the complementary findings
of all five studies, allowing a non-controversial recommendation
that, when patients receive neuromuscular blocking agents, the
BIS is superior to clinical signs alone, especially in patients
receiving total i.v. anaesthesia.32 33 An electroencephalographic
device may be particularly useful during total i.v. anaesthesia
because of higher interindividual variability of sedative–hypnotic
response and the inability routinely to monitor or set alarms for
i.v. anaesthetic levels. In contrast, BIS monitoring is not superior
at preventing awareness when a potent volatile anaesthetic
agent is administered and an alarm is set for a low anaesthetic
concentration.32 33 It is highly likely that the same findings
would hold true for other devices in the current generation of
processed electroencephalographic monitors.32
Non-controversial: the incidence of
intraoperative awareness and distressing
awareness is higher when neuromuscular
blocking agents are administered
It is self-evident that the avoidance of neuromuscular blocking
agents does not in itself prevent intraoperative awareness if in-
sufficient concentrations of hypnotic agents are administered.
In 1846, Abbott received ether for a tumour removal and was
aware, although not in pain, during the procedure.34Gray35popu-
larized the use of neuromuscular blocking agents as essential
components of general anaesthesia in Liverpool in the late
1940s. The underlying principle of the new technique was ‘min-
imal narcotization with adequate curarization.’ 35 The motiva-
tions were to minimize the cardiovascular depressant effects of
high concentrations of ether, cyclopropane, kemithal, or thio-
pental and to facilitate more rapid emergence of patients from
the vulnerable state of general anaesthesia after surgery.35 Des-
pite the advent of modern general anaesthetic agents over the
last four decades, with less cardiovascular depression and rapid
elimination, the practice of pharmacological paralysis with lim-
ited hypnotic administration continued to be popular and still
has proponents in modern practice. In the seminal observational
study by Sandin and colleagues,2 the incidence of unintended
awareness among patients who received general anaesthesia
without neuromuscular blocking agents was 0.1%, compared
with 0.18% when patients were pharmacologically paralysed.
A mundane explanation for the reduction in awareness in non-
pharmacologically paralysed patients is that patient movement
can potentially alert anaesthetists to the possibility of inad-
equate general anaesthesia. However, it is also possible that
the need for or use of neuromuscular blocking agents covaries
with other important risk factors for intraoperative awareness.
Interestingly, only patients who had been pharmacologically pa-
ralysed reported anxiety and psychological symptoms in rela-
tionship to their awareness experience. 2 In a comprehensive
literature review, Ghoneim and colleagues36endorsed the finding
that pharmacological paralysis was an important risk factor
for distressing awareness experiences. This important insight
has again been corroborated in the recently published NAP5
study,27 where the overwhelming majority of awareness reports
were from patients who had received neuromuscular blocking
drugs and also where the anaesthetic concentration was reduced
towards the end of surgery before antagonizing neuromuscular
blockade. The avoidance or minimization of pharmacological
paralysis might be the most effective currently available method
to prevent traumatic intraoperative awareness.
Controversial: intraoperative awareness with
explicit recall has a genetic component
It has been argued that awareness with recall is caused by insuf-
ficient anaesthetic dosing.36 37 Although this assertion is true in
what might be considered a tautological sense—that is, insuffi-
cient anaesthesia is caused by insufficient anaesthesia—the
argument is meant to suggest that awareness with explicit recall
is preventable by attention to anaesthetic dosing rather than the
search for occult factors that enable consciousness and memory
despite what reasonable clinicians might consider adequate
anaesthesia. It is well known based on experimental data that
genetic background can influence sensitivity to the sedative–
hypnotic and, independently, the amnesic effects of general
anaesthetics.38–41Furthermore, patients with a history of intrao-
perative awareness with explicit recall had an incidence of
awareness of almost 1 in 50 with subsequent surgery and an es-
timated five-fold adjusted increase in risk for awareness com-
pared with matched patients who also had at least one risk
factor for awareness.42 It is also striking that several studies in
Chinese populations have found surprisingly high incidences of
awareness.6 10 31 It is therefore unclear whether, in some in-
stances, genetically mediated resistance to anaesthetic-induced
Intraoperative awareness: controversies and non-controversies| i23
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
surgical patients who had been formally determined to have in-
traoperative awareness with explicit recall demonstrated no
long-term consequences.25 However, this might be attributable
to the fact that the initial experiences themselves were not par-
ticularly traumatic. A recent multicentre study demonstrates
that PTSD symptoms are indeed more common after definite or
possible awareness with recall,26 and the NAP5 audit highlights
the importance of neuromuscular paralysis in psychologically
traumatic experiences.27 Thus, although certain screening meth-
ods or patient populations might be associated with apparently
low incidences of PTSD after awareness reports, it is no longer a
matter of controversy as to whether or not intraoperative aware-
ness with explicit recall can lead to PTSD or PTSD symptoms.
Non-controversial: processed
electroencephalographic monitoring
is useful in preventing intraoperative
awareness with explicit recall compared
with clinical signs but not compared with
anaesthetic concentration alarms
The role of processed electroencephalographic devices, such as
the bispectral index (BIS) monitor, in the prevention of intrao-
perative awareness with explicit recall is sometimes regarded
as controversial, but should not be. Clear and consistent findings
have emerged from the five major randomized controlled trials
focused on the BIS.4 28–31The B-Aware trial28 demonstrated that
the BIS monitor was effective in reducing definite awareness
events compared with routine clinical care in patients at high
risk for the complication; this has also been demonstrated
for patients receiving total i.v. anaesthesia.31 In contrast, the
BAG-RECALL and B-Unaware trials demonstrated that alarms
based on the BIS are not superior to alarms based on end-tidal
anaesthetic concentration in preventing awareness with explicit
recall in patients at high risk for the complication.29 30The Mich-
igan Awareness Control Study has confirmed these findings
(i.e. BIS superior to clinical signs but not to anaesthetic concen-
tration alerts) in patients at all risk levels for awareness with ex-
plicit recall.4 An article synthesizing the evidence and an updated
Cochrane systematic review reflect the complementary findings
of all five studies, allowing a non-controversial recommendation
that, when patients receive neuromuscular blocking agents, the
BIS is superior to clinical signs alone, especially in patients
receiving total i.v. anaesthesia.32 33 An electroencephalographic
device may be particularly useful during total i.v. anaesthesia
because of higher interindividual variability of sedative–hypnotic
response and the inability routinely to monitor or set alarms for
i.v. anaesthetic levels. In contrast, BIS monitoring is not superior
at preventing awareness when a potent volatile anaesthetic
agent is administered and an alarm is set for a low anaesthetic
concentration.32 33 It is highly likely that the same findings
would hold true for other devices in the current generation of
processed electroencephalographic monitors.32
Non-controversial: the incidence of
intraoperative awareness and distressing
awareness is higher when neuromuscular
blocking agents are administered
It is self-evident that the avoidance of neuromuscular blocking
agents does not in itself prevent intraoperative awareness if in-
sufficient concentrations of hypnotic agents are administered.
In 1846, Abbott received ether for a tumour removal and was
aware, although not in pain, during the procedure.34Gray35popu-
larized the use of neuromuscular blocking agents as essential
components of general anaesthesia in Liverpool in the late
1940s. The underlying principle of the new technique was ‘min-
imal narcotization with adequate curarization.’ 35 The motiva-
tions were to minimize the cardiovascular depressant effects of
high concentrations of ether, cyclopropane, kemithal, or thio-
pental and to facilitate more rapid emergence of patients from
the vulnerable state of general anaesthesia after surgery.35 Des-
pite the advent of modern general anaesthetic agents over the
last four decades, with less cardiovascular depression and rapid
elimination, the practice of pharmacological paralysis with lim-
ited hypnotic administration continued to be popular and still
has proponents in modern practice. In the seminal observational
study by Sandin and colleagues,2 the incidence of unintended
awareness among patients who received general anaesthesia
without neuromuscular blocking agents was 0.1%, compared
with 0.18% when patients were pharmacologically paralysed.
A mundane explanation for the reduction in awareness in non-
pharmacologically paralysed patients is that patient movement
can potentially alert anaesthetists to the possibility of inad-
equate general anaesthesia. However, it is also possible that
the need for or use of neuromuscular blocking agents covaries
with other important risk factors for intraoperative awareness.
Interestingly, only patients who had been pharmacologically pa-
ralysed reported anxiety and psychological symptoms in rela-
tionship to their awareness experience. 2 In a comprehensive
literature review, Ghoneim and colleagues36endorsed the finding
that pharmacological paralysis was an important risk factor
for distressing awareness experiences. This important insight
has again been corroborated in the recently published NAP5
study,27 where the overwhelming majority of awareness reports
were from patients who had received neuromuscular blocking
drugs and also where the anaesthetic concentration was reduced
towards the end of surgery before antagonizing neuromuscular
blockade. The avoidance or minimization of pharmacological
paralysis might be the most effective currently available method
to prevent traumatic intraoperative awareness.
Controversial: intraoperative awareness with
explicit recall has a genetic component
It has been argued that awareness with recall is caused by insuf-
ficient anaesthetic dosing.36 37 Although this assertion is true in
what might be considered a tautological sense—that is, insuffi-
cient anaesthesia is caused by insufficient anaesthesia—the
argument is meant to suggest that awareness with explicit recall
is preventable by attention to anaesthetic dosing rather than the
search for occult factors that enable consciousness and memory
despite what reasonable clinicians might consider adequate
anaesthesia. It is well known based on experimental data that
genetic background can influence sensitivity to the sedative–
hypnotic and, independently, the amnesic effects of general
anaesthetics.38–41Furthermore, patients with a history of intrao-
perative awareness with explicit recall had an incidence of
awareness of almost 1 in 50 with subsequent surgery and an es-
timated five-fold adjusted increase in risk for awareness com-
pared with matched patients who also had at least one risk
factor for awareness.42 It is also striking that several studies in
Chinese populations have found surprisingly high incidences of
awareness.6 10 31 It is therefore unclear whether, in some in-
stances, genetically mediated resistance to anaesthetic-induced
Intraoperative awareness: controversies and non-controversies| i23
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

unconsciousness or amnesia contributes to awareness with re-
call. Furthermore, even assuming a genetic contribution to an-
aesthetic resistance, it is unclear whether reduced potency or
reduced efficacy is the primary cause, which has implications
for how best to alter anaesthetic care in patients at risk.
A pharmacogenomics approach might help to resolve this con-
troversy, although the rarity of the disorder and the probable
lack of parsimonious genetic culprits (e.g. single nucleotide poly-
morphisms) could render genetic explorations unhelpful.
Controversial: undesired awareness with
explicit recall of procedures performed under
sedation is a clinical problem
Self-reports of undesired intraoperative awareness with explicit
recall occur with the same frequency in patients receiving gen-
eral anaesthesia as in those receiving sedation, regional, or neur-
axial anaesthesia.12 This is likely to be the result of mismatched
expectations regarding levels of consciousness in patients who
are not receiving general anaesthesia during surgery or other in-
vasive procedures.43 Recent studies have suggested that un-
desired awareness and explicit recall in patients receiving
sedation, regional anaesthesia, or neuraxial anaesthesia can be
associated with long-term psychological consequences.27 44
A study based on the American Society of Anesthesiologists An-
esthesia Awareness Registry found comparable rates of long-
term psychological sequelae in those reporting awareness during
general anaesthesia and those reporting awareness during alter-
native anaesthetic techniques. 44 Recent data from the NAP5
study27 support the possibility that undesired awareness and
explicit recall during non-general anaesthetic procedures can
be associated with long-term psychological consequences. Al-
though these data would suggest that undesired awareness in
this population is a true clinical problem, the use of sedation
for minor procedures, such as endoscopy, is extremely common.
If psychological sequelae occurred in a significant proportion of
these instances, the absolute number of patient reports would
probably be a salient signal that would already have captured
the attention of medical professionals. Instead, this phenom-
enon has only recently been observed coincidentally through
systematic study of intraoperative awareness with explicit recall
after an intended general anaesthetic. Although the data remain
incomplete and controversial, it is important for anaesthesia pro-
viders to set appropriate expectations and ensure that patients
understand the planned level of consciousness and the potential
for remembering events during the surgery or procedure. In some
instances, this might mitigate the dissatisfaction with or conse-
quences of undesired awareness and recall.
Controversial: intraoperative awareness
without recall has psychological consequences
It is well known that the incidence of awareness without recall is
significantly higher than with recall. This situation generates an
important question: is it ethically acceptable if a patient is transi-
ently conscious but has no explicit memory of the event? Fur-
thermore, would the complete elimination of consciousness
during surgery require anaesthetic regimens that result in other
and potentially more dangerous adverse effects?45 It is a philo-
sophical question as to whether consciousness without memory
is ethically tenable during surgery, but the clinically relevant
question relates to the potential for postoperative psychological
consequences. Although we have focused on explicit recall in
relationship to conscious experience, there is also the possibility
of implicit (or unconscious) recall. It has been argued that impli-
cit recall of a surgical event—especially involving pain—might
result in PTSD even in the absence of explicit recall.46We support
the opinion that—independently of recall—appropriate anal-
gesia during surgery is of paramount importance given the
known potential for intraoperative awareness. However, it is
less clear whether there is compelling epidemiological evidence
for a negative effect of implicit memory on postoperative psycho-
logical function. Given the high incidence of awareness without
recall (as demonstrated by IFT studies)19—especially at the time
of strong nociceptive stimuli, such as laryngoscopy or surgical
incision—even a small proportion of patients experiencing psy-
chological sequelae as a result of implicit memory would trans-
late to a high absolute number of distressed patients. However,
the number of postoperative patients suffering PTSD without re-
call of surgical events appears to be low. When PTSD is precipi-
tated by perioperative events, the most likely contributing
factors include pain, prolonged intubation, unpleasant experi-
ences in the intensive care unit, physical debility, traumatic ex-
plicit memories, and distressing diagnoses. There is currently
little evidence to suggest that implicit memories are important
contributors. However, the dichotomous determination of PTSD
or not might be less relevant in awareness without recall; subsyn-
dromal PTSD must also be explored in addition to psychological
morbidity (such as mood or anxiety disorders) that cannot neces-
sarily be linked to an index event or experience. As a result of the
ethical implications of this controversy, further data are required.
Controversial: positive responses
to an isolated forearm test reflect
a distinct state of consciousness
A positive and unequivocal response to the command ‘squeeze
my hand’ at the end of a surgical procedure is traditionally
taken to constitute sufficient evidence that consciousness has re-
turned. Likewise, one could argue that a positive and unequivocal
response to the command ‘squeeze my hand’ during a surgical
procedure—for example, a positive IFT response—constitutes
sufficient evidence that consciousness has returned. Until there
is compelling evidence to the contrary, this should be the default
assumption. Sanders and colleagues19have clarified the possibil-
ities of perioperative behaviour and experience with a model of
responsiveness, connected consciousness, and disconnected
consciousness (e.g. a dream state). A recent theoretical perspec-
tive suggests an alternative possibility for IFT responses,
although no data have yet been provided. Pandit 47 48 argues
that the positive IFT response does not signify the full return or
persistence of consciousness but rather a ‘third state’ (referred
to as dysanaesthesia) in which patients can follow a simple com-
mand in the absence of a conscious self (see also Wang and col-
leagues, this issue). It is unclear, of course, whether such a state is
possible and, if so, what the candidate neural correlates would be.
This assertion is provocative but should be tested empirically and/
or potentially situated in broader frameworks of consciousness.49
Controversial: true reports of intraoperative
awareness can be distinguished reliably from
false reports of intraoperative awareness and
from dreaming
Detection of intraoperative awareness is unreliable because it
depends on patient reports rather than objective measures.
i24 | Mashour and Avidan
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
call. Furthermore, even assuming a genetic contribution to an-
aesthetic resistance, it is unclear whether reduced potency or
reduced efficacy is the primary cause, which has implications
for how best to alter anaesthetic care in patients at risk.
A pharmacogenomics approach might help to resolve this con-
troversy, although the rarity of the disorder and the probable
lack of parsimonious genetic culprits (e.g. single nucleotide poly-
morphisms) could render genetic explorations unhelpful.
Controversial: undesired awareness with
explicit recall of procedures performed under
sedation is a clinical problem
Self-reports of undesired intraoperative awareness with explicit
recall occur with the same frequency in patients receiving gen-
eral anaesthesia as in those receiving sedation, regional, or neur-
axial anaesthesia.12 This is likely to be the result of mismatched
expectations regarding levels of consciousness in patients who
are not receiving general anaesthesia during surgery or other in-
vasive procedures.43 Recent studies have suggested that un-
desired awareness and explicit recall in patients receiving
sedation, regional anaesthesia, or neuraxial anaesthesia can be
associated with long-term psychological consequences.27 44
A study based on the American Society of Anesthesiologists An-
esthesia Awareness Registry found comparable rates of long-
term psychological sequelae in those reporting awareness during
general anaesthesia and those reporting awareness during alter-
native anaesthetic techniques. 44 Recent data from the NAP5
study27 support the possibility that undesired awareness and
explicit recall during non-general anaesthetic procedures can
be associated with long-term psychological consequences. Al-
though these data would suggest that undesired awareness in
this population is a true clinical problem, the use of sedation
for minor procedures, such as endoscopy, is extremely common.
If psychological sequelae occurred in a significant proportion of
these instances, the absolute number of patient reports would
probably be a salient signal that would already have captured
the attention of medical professionals. Instead, this phenom-
enon has only recently been observed coincidentally through
systematic study of intraoperative awareness with explicit recall
after an intended general anaesthetic. Although the data remain
incomplete and controversial, it is important for anaesthesia pro-
viders to set appropriate expectations and ensure that patients
understand the planned level of consciousness and the potential
for remembering events during the surgery or procedure. In some
instances, this might mitigate the dissatisfaction with or conse-
quences of undesired awareness and recall.
Controversial: intraoperative awareness
without recall has psychological consequences
It is well known that the incidence of awareness without recall is
significantly higher than with recall. This situation generates an
important question: is it ethically acceptable if a patient is transi-
ently conscious but has no explicit memory of the event? Fur-
thermore, would the complete elimination of consciousness
during surgery require anaesthetic regimens that result in other
and potentially more dangerous adverse effects?45 It is a philo-
sophical question as to whether consciousness without memory
is ethically tenable during surgery, but the clinically relevant
question relates to the potential for postoperative psychological
consequences. Although we have focused on explicit recall in
relationship to conscious experience, there is also the possibility
of implicit (or unconscious) recall. It has been argued that impli-
cit recall of a surgical event—especially involving pain—might
result in PTSD even in the absence of explicit recall.46We support
the opinion that—independently of recall—appropriate anal-
gesia during surgery is of paramount importance given the
known potential for intraoperative awareness. However, it is
less clear whether there is compelling epidemiological evidence
for a negative effect of implicit memory on postoperative psycho-
logical function. Given the high incidence of awareness without
recall (as demonstrated by IFT studies)19—especially at the time
of strong nociceptive stimuli, such as laryngoscopy or surgical
incision—even a small proportion of patients experiencing psy-
chological sequelae as a result of implicit memory would trans-
late to a high absolute number of distressed patients. However,
the number of postoperative patients suffering PTSD without re-
call of surgical events appears to be low. When PTSD is precipi-
tated by perioperative events, the most likely contributing
factors include pain, prolonged intubation, unpleasant experi-
ences in the intensive care unit, physical debility, traumatic ex-
plicit memories, and distressing diagnoses. There is currently
little evidence to suggest that implicit memories are important
contributors. However, the dichotomous determination of PTSD
or not might be less relevant in awareness without recall; subsyn-
dromal PTSD must also be explored in addition to psychological
morbidity (such as mood or anxiety disorders) that cannot neces-
sarily be linked to an index event or experience. As a result of the
ethical implications of this controversy, further data are required.
Controversial: positive responses
to an isolated forearm test reflect
a distinct state of consciousness
A positive and unequivocal response to the command ‘squeeze
my hand’ at the end of a surgical procedure is traditionally
taken to constitute sufficient evidence that consciousness has re-
turned. Likewise, one could argue that a positive and unequivocal
response to the command ‘squeeze my hand’ during a surgical
procedure—for example, a positive IFT response—constitutes
sufficient evidence that consciousness has returned. Until there
is compelling evidence to the contrary, this should be the default
assumption. Sanders and colleagues19have clarified the possibil-
ities of perioperative behaviour and experience with a model of
responsiveness, connected consciousness, and disconnected
consciousness (e.g. a dream state). A recent theoretical perspec-
tive suggests an alternative possibility for IFT responses,
although no data have yet been provided. Pandit 47 48 argues
that the positive IFT response does not signify the full return or
persistence of consciousness but rather a ‘third state’ (referred
to as dysanaesthesia) in which patients can follow a simple com-
mand in the absence of a conscious self (see also Wang and col-
leagues, this issue). It is unclear, of course, whether such a state is
possible and, if so, what the candidate neural correlates would be.
This assertion is provocative but should be tested empirically and/
or potentially situated in broader frameworks of consciousness.49
Controversial: true reports of intraoperative
awareness can be distinguished reliably from
false reports of intraoperative awareness and
from dreaming
Detection of intraoperative awareness is unreliable because it
depends on patient reports rather than objective measures.
i24 | Mashour and Avidan
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020

Prospective methods using structured questionnaires detect sub-
stantially more awareness events than approaches based on
spontaneous patient reports. However, a concern regarding the
questions in the Brice questionnaire is that they have not been
psychometrically validated and might have the potential to elicit
false reports or memories.1 15 This latter possibility is consistent
with the finding that a significant proportion of patients only re-
port awareness at later time points after multiple structured inter-
views.2 3 Regardless of the detection method, distinguishing true
from false awareness reports is difficult. Occasionally, a patient re-
port is so detailed and specific in describing intraoperative experi-
ences, events, or discussions that independent arbiters can concur
that awareness definitely occurred.4 28–30
Commonly, however, pa-
tient reports are vague and experts express divergent opinions re-
garding whether or not a patient was truly aware.4 28–30
If many of
the possible awareness reports do represent true awareness, this
would mean that the incidence of intraoperative awareness has
been even higher than studies have suggested. In contrast to pos-
sible awareness experiences, it is important to clarify that most re-
ports of intraoperative dreaming, which were previously viewed as
possible or near awareness experiences, are likely to be unrelated
to intraoperative awareness and do not necessarily indicate that
patients were insufficiently anaesthetized during surgery.50–52
Based on clinical and electroencephalographic evidence, it is pos-
sible that dreaming occurs during emergence from general anaes-
thesia, when patients are sedated or in a physiological sleep
state.50 51 However, Samuelsson and colleagues53 found that,
while the content of dreams was unrelated to awareness, the inci-
dence of intraoperative awareness was 19 times more common
among patients who reported a dream after surgery. Therefore,
the precise relationship between awareness and dreaming re-
mains unresolved.
Conclusion
Substantial progress has been made in understanding the inci-
dence, consequences, and prevention of intraoperative aware-
ness with explicit recall. We are not arguing that further
research is unnecessary in these aspects of the field, but rather
that new studies with disparate results do not necessarily create
‘controversy’ unless the methodology is clearly superior and
results are particularly novel compared with the existing litera-
ture. The truly controversial aspects in this field relate less to
the epidemiology and prevention of awareness and more to the
underlying aetiology (e.g. genetic contribution) and whether
there exist unique states of the brain in association with certain
levels of anaesthesia. These questions may or may not have clear
clinical relevance, but certainly represent some of the most inter-
esting neuroscientific and philosophical dimensions of intrao-
perative awareness.
Authors’ contributions
G.A.M. conceived the project. G.A.M. and M.S.A. wrote the
manuscript.
Declaration of interest
M.S.A. is a member of the Associate Editorial Board of the BJA.
References
1. Brice DD, Hetherington RR, Utting JE. A simple study of aware-
ness and dreaming during anaesthesia. Br J Anaesth 1970; 42:
535–42
2. Sandin RH, Enlund G, Samuelsson P, Lennmarken C. Aware-
ness during anaesthesia: a prospective case study. Lancet
2000; 355: 707–11
3. Sebel PS, Bowdle TA, Ghoneim MM, et al.The incidence of
awareness during anesthesia: a multicenter United States
study. Anesth Analg 2004; 99: 833–9, table of contents
4. Mashour GA, Shanks A, Tremper KK, et al. Prevention of in-
traoperative awareness with explicit recall in an unselected
surgical population: a randomized comparative effectiveness
trial. Anesthesiology 2012; 117: 717–25
5. Errando CL, Sigl JC, Robles M, et al. Awareness with recall dur-
ing general anaesthesia: a prospective observational evalu-
ation of 4001 patients. Br J Anaesth 2008; 101: 178–85
6. Wang Y, Yue Y, Sun YH, et al. Investigation and analysis of
incidence of awareness in patients undergoing cardiac sur-
gery in Beijing, China. Chin Med J (Engl) 2005; 118: 1190–4
7. Xu L, Wu AS, Yue Y. The incidence of intra-operative aware-
ness during general anesthesia in China: a multi-center ob-
servational study. Acta Anaesthesiol Scand 2009; 53: 873–82
8. Ye Z, Guo QL, Zheng H. Investigation and analysis of the inci-
dence of awareness during general anesthesia. Zhong Nan Da
Xue Xue Bao Yi Xue Ban 2008; 33: 533–6
9. Shi X, Wang DX. The incidence of awareness with recall dur-
ing general anesthesia has been lowered: a historical con-
trolled trial. Zhonghua Yi Xue Za Zhi 2013; 93: 3272–5
10. Wang E, Ye Z, Pan Y, et al. Incidence and risk factors of intrao-
perative awareness during general anesthesia. Zhong Nan Da
Xue Xue Bao Yi Xue Ban 2011; 36: 671–5
11. Pollard RJ, Coyle JP, Gilbert RL, Beck JE. Intraoperative aware-
ness in a regional medical system: a review of 3 years’ data.
Anesthesiology 2007; 106: 269–74
12. Mashour GA, Wang LY, Turner CR, et al. A retrospective study
of intraoperative awareness with methodological implica-
tions. Anesth Analg 2009; 108: 521–6
13. Pandit JJ, Cook TM, Jonker WR, O’Sullivan E. A national survey
of anaesthetists (NAP5 Baseline) to estimate an annual inci-
dence of accidental awareness during general anaesthesia
in the UK. Anaesthesia 2013; 68: 343–53
14. Pandit JJ, Andrade J, Bogod DG, et al. 5th National Audit Project
(NAP5) on accidental awareness during general anaesthesia:
summary of main findings and risk factors. Br J Anaesth 2014;
113: 549–59
15. Mashour GA, Kent C, Picton P, et al. Assessment of intraopera-
tive awareness with explicit recall: a comparison of 2 meth-
ods. Anesth Analg 2013; 116: 889–91
16. Pryor KA, Hemmings HC Jr. NAP5: intraoperative awareness
detected, and undetected. Br J Anaesth 2014; 113: 530–3
17. Tunstall ME, Sheikh A. Comparison of 1.5% enflurane with
1.25% isoflurane in oxygen for caesarean section: avoidance
of awareness without nitrous oxide. Br J Anaesth 1989;62:
138–43
18. King H, Ashley S, Brathwaite D, Decayette J, Wooten DJ. Ad-
equacy of general anesthesia for cesarean section. Anesth
Analg 1993; 77: 84–8
19. Sanders RD, Tononi G, Laureys S, Sleigh JW. Unresponsive-
ness ≠ unconsciousness. Anesthesiology 2012; 116: 946–59
20. Meyer BC, Blacher RS. A traumatic neurotic reaction
induced by succinylcholine chloride. N Y State J Med 1961;
61: 1255–61
21. Lennmarken C, Bildfors K, Enlund G, Samuelsson P, Sandin R.
Victims of awareness.Acta Anaesthesiol Scand 2002; 46: 229–31
22. Leslie K, Chan MT, Myles PS, Forbes A, McCulloch TJ. Post-
traumatic stress disorder in aware patients from the
B-aware trial. Anesth Analg 2010; 110: 823–8
Intraoperative awareness: controversies and non-controversies| i25
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
stantially more awareness events than approaches based on
spontaneous patient reports. However, a concern regarding the
questions in the Brice questionnaire is that they have not been
psychometrically validated and might have the potential to elicit
false reports or memories.1 15 This latter possibility is consistent
with the finding that a significant proportion of patients only re-
port awareness at later time points after multiple structured inter-
views.2 3 Regardless of the detection method, distinguishing true
from false awareness reports is difficult. Occasionally, a patient re-
port is so detailed and specific in describing intraoperative experi-
ences, events, or discussions that independent arbiters can concur
that awareness definitely occurred.4 28–30
Commonly, however, pa-
tient reports are vague and experts express divergent opinions re-
garding whether or not a patient was truly aware.4 28–30
If many of
the possible awareness reports do represent true awareness, this
would mean that the incidence of intraoperative awareness has
been even higher than studies have suggested. In contrast to pos-
sible awareness experiences, it is important to clarify that most re-
ports of intraoperative dreaming, which were previously viewed as
possible or near awareness experiences, are likely to be unrelated
to intraoperative awareness and do not necessarily indicate that
patients were insufficiently anaesthetized during surgery.50–52
Based on clinical and electroencephalographic evidence, it is pos-
sible that dreaming occurs during emergence from general anaes-
thesia, when patients are sedated or in a physiological sleep
state.50 51 However, Samuelsson and colleagues53 found that,
while the content of dreams was unrelated to awareness, the inci-
dence of intraoperative awareness was 19 times more common
among patients who reported a dream after surgery. Therefore,
the precise relationship between awareness and dreaming re-
mains unresolved.
Conclusion
Substantial progress has been made in understanding the inci-
dence, consequences, and prevention of intraoperative aware-
ness with explicit recall. We are not arguing that further
research is unnecessary in these aspects of the field, but rather
that new studies with disparate results do not necessarily create
‘controversy’ unless the methodology is clearly superior and
results are particularly novel compared with the existing litera-
ture. The truly controversial aspects in this field relate less to
the epidemiology and prevention of awareness and more to the
underlying aetiology (e.g. genetic contribution) and whether
there exist unique states of the brain in association with certain
levels of anaesthesia. These questions may or may not have clear
clinical relevance, but certainly represent some of the most inter-
esting neuroscientific and philosophical dimensions of intrao-
perative awareness.
Authors’ contributions
G.A.M. conceived the project. G.A.M. and M.S.A. wrote the
manuscript.
Declaration of interest
M.S.A. is a member of the Associate Editorial Board of the BJA.
References
1. Brice DD, Hetherington RR, Utting JE. A simple study of aware-
ness and dreaming during anaesthesia. Br J Anaesth 1970; 42:
535–42
2. Sandin RH, Enlund G, Samuelsson P, Lennmarken C. Aware-
ness during anaesthesia: a prospective case study. Lancet
2000; 355: 707–11
3. Sebel PS, Bowdle TA, Ghoneim MM, et al.The incidence of
awareness during anesthesia: a multicenter United States
study. Anesth Analg 2004; 99: 833–9, table of contents
4. Mashour GA, Shanks A, Tremper KK, et al. Prevention of in-
traoperative awareness with explicit recall in an unselected
surgical population: a randomized comparative effectiveness
trial. Anesthesiology 2012; 117: 717–25
5. Errando CL, Sigl JC, Robles M, et al. Awareness with recall dur-
ing general anaesthesia: a prospective observational evalu-
ation of 4001 patients. Br J Anaesth 2008; 101: 178–85
6. Wang Y, Yue Y, Sun YH, et al. Investigation and analysis of
incidence of awareness in patients undergoing cardiac sur-
gery in Beijing, China. Chin Med J (Engl) 2005; 118: 1190–4
7. Xu L, Wu AS, Yue Y. The incidence of intra-operative aware-
ness during general anesthesia in China: a multi-center ob-
servational study. Acta Anaesthesiol Scand 2009; 53: 873–82
8. Ye Z, Guo QL, Zheng H. Investigation and analysis of the inci-
dence of awareness during general anesthesia. Zhong Nan Da
Xue Xue Bao Yi Xue Ban 2008; 33: 533–6
9. Shi X, Wang DX. The incidence of awareness with recall dur-
ing general anesthesia has been lowered: a historical con-
trolled trial. Zhonghua Yi Xue Za Zhi 2013; 93: 3272–5
10. Wang E, Ye Z, Pan Y, et al. Incidence and risk factors of intrao-
perative awareness during general anesthesia. Zhong Nan Da
Xue Xue Bao Yi Xue Ban 2011; 36: 671–5
11. Pollard RJ, Coyle JP, Gilbert RL, Beck JE. Intraoperative aware-
ness in a regional medical system: a review of 3 years’ data.
Anesthesiology 2007; 106: 269–74
12. Mashour GA, Wang LY, Turner CR, et al. A retrospective study
of intraoperative awareness with methodological implica-
tions. Anesth Analg 2009; 108: 521–6
13. Pandit JJ, Cook TM, Jonker WR, O’Sullivan E. A national survey
of anaesthetists (NAP5 Baseline) to estimate an annual inci-
dence of accidental awareness during general anaesthesia
in the UK. Anaesthesia 2013; 68: 343–53
14. Pandit JJ, Andrade J, Bogod DG, et al. 5th National Audit Project
(NAP5) on accidental awareness during general anaesthesia:
summary of main findings and risk factors. Br J Anaesth 2014;
113: 549–59
15. Mashour GA, Kent C, Picton P, et al. Assessment of intraopera-
tive awareness with explicit recall: a comparison of 2 meth-
ods. Anesth Analg 2013; 116: 889–91
16. Pryor KA, Hemmings HC Jr. NAP5: intraoperative awareness
detected, and undetected. Br J Anaesth 2014; 113: 530–3
17. Tunstall ME, Sheikh A. Comparison of 1.5% enflurane with
1.25% isoflurane in oxygen for caesarean section: avoidance
of awareness without nitrous oxide. Br J Anaesth 1989;62:
138–43
18. King H, Ashley S, Brathwaite D, Decayette J, Wooten DJ. Ad-
equacy of general anesthesia for cesarean section. Anesth
Analg 1993; 77: 84–8
19. Sanders RD, Tononi G, Laureys S, Sleigh JW. Unresponsive-
ness ≠ unconsciousness. Anesthesiology 2012; 116: 946–59
20. Meyer BC, Blacher RS. A traumatic neurotic reaction
induced by succinylcholine chloride. N Y State J Med 1961;
61: 1255–61
21. Lennmarken C, Bildfors K, Enlund G, Samuelsson P, Sandin R.
Victims of awareness.Acta Anaesthesiol Scand 2002; 46: 229–31
22. Leslie K, Chan MT, Myles PS, Forbes A, McCulloch TJ. Post-
traumatic stress disorder in aware patients from the
B-aware trial. Anesth Analg 2010; 110: 823–8
Intraoperative awareness: controversies and non-controversies| i25
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
23. Domino KB, Posner KL, Caplan RA, Cheney FW. Awareness
during anesthesia: a closed claims analysis. Anesthesiology
1999; 90: 1053–61
24. Samuelsson P, Brudin L, Sandin RH. Late psychological symp-
toms after awareness among consecutively included surgical
patients. Anesthesiology 2007; 106: 26–32
25. Laukkala T, Ranta S, Wennervirta J, et al. Long-term psycho-
social outcomes after intraoperative awareness with recall.
Anesth Analg 2014; 119: 86–92
26. Whitlock E, Rodebaugh T, Hassett A, et al. Psychological se-
quelae of surgery in a prospective cohort of patients from
three intraoperative awareness prevention trials. Anesth
Analg 2015; 120: 87–95
27. Cook TM, Andrade J, Bogod DG, et al. 5th National Audit Pro-
ject (NAP5) on accidental awareness during general anaes-
thesia: patient experiences, human factors, sedation,
consent, and medicolegal issues. Br J Anaesth 2014;113:
560–74
28. Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral
index monitoring to prevent awareness during anaesthesia:
the B-Aware randomised controlled trial. Lancet 2004;363:
1757–63
29. Avidan MS, Jacobsohn E, Glick D, et al. Prevention of intrao-
perative awareness in a high-risk surgical population. N
Engl J Med 2011; 365: 591–600
30. Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness
and the bispectral index. N Engl J Med 2008; 358: 1097–108
31. Zhang C, Xu L, Ma YQ, et al. Bispectral index monitoring
prevent awareness during total intravenous anesthesia: a
prospective, randomized, double-blinded, multi-center con-
trolled trial. Chin Med J (Engl) 2011; 124: 3664–9
32. Avidan MS, Mashour GA. Prevention of intraoperative aware-
ness with explicit recall: making sense of the evidence.
Anesthesiology 2013; 118: 449–56
33. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N.
Bispectral index for improving anaesthetic delivery and post-
operative recovery. Cochrane Database Syst Rev 2014;6: CD003843
34. Bigelow H. Insensibility during surgical operations produced
by inhalation. The Boston Medicaland SurgicalJournal 1846;
XXXV: 309–17
35. Gray TC. A system of anaesthesia using d-tubocurarine chlor-
ide for chest surgery. Postgrad Med J 1948; 24: 514–26
36. Ghoneim MM, Block RI, Haffarnan M, Mathews MJ. Awareness
during anesthesia: risk factors, causes and sequelae: a review
of reported cases in the literature. Anesth Analg 2009;108:
527–35
37. Nickalls RW, Mahajan RP. Awareness and anaesthesia: think
dose, think data. Br J Anaesth 2010; 104: 1–2
38. Cheng VY, Martin LJ, Elliott EM, et al. α5GABAA receptors me-
diate the amnestic but not sedative-hypnotic effects of the
general anesthetic etomidate. J Neurosci 2006; 26: 3713–20
39. Kretschmannova K, Hines RM, Revilla-Sanchez R, et al.
Enhanced tonic inhibition influences the hypnotic and am-
nestic actions of the intravenous anesthetics etomidate and
propofol. J Neurosci 2013; 33: 7264–73
40. Jurd R, Arras M, Lambert S, et al. General anesthetic actions
in vivo strongly attenuated by a point mutation in the
GABAA receptor β3 subunit. FASEB J 2003; 17: 250–2
41. Zeller A, Arras M, Jurd R, Rudolph U. Mapping the contribu-
tion of β3-containing GABAA receptors to volatile and intra-
venous general anesthetic actions. BMC Pharmacol 2007; 7: 2
42. Aranake A, Gradwohl S, Ben-Abdallah A, et al. Increased risk
of intraoperative awareness in patients with a history of
awareness. Anesthesiology 2013; 119: 1275–83
43. Esaki RK, Mashour GA. Levels of consciousness during re-
gional anesthesia and monitored anesthesia care: patient
expectations and experiences. Anesth Analg 2009; 108:
1560–3
44. Kent CD, Mashour GA, Metzger NA, Posner KL, Domino KB.
Psychological impact of unexpected explicit recall of events
occurring during surgery performed under sedation, regional
anaesthesia, and general anaesthesia: data from the Anes-
thesia Awareness Registry. Br J Anaesth 2013; 110: 381–7
45. Crosby G. General anesthesia — minding the mind during
surgery. N Engl J Med 2011; 365: 660–1
46. Wang M, Messina AG, Russell IF. The topography of aware-
ness: a classification of intra-operative cognitive states.
Anaesthesia 2012; 67: 1197–201
47. Pandit JJ. Isolated forearm – or isolated brain? Interpreting re-
sponses during anaesthesia – or ‘dysanaesthesia’. Anaesthesia
2013; 68: 995–1000
48. Pandit JJ. Acceptably aware during general anaesthesia:
‘dysanaesthesia’ – the uncoupling of perception from sen-
sory inputs. Conscious Cogn 2014; 27: 194–212
49. Oizumi M, Albantakis L, Tononi G. From the phenomenology
to the mechanisms of consciousness: Integrated Information
Theory 3.0. PLoS Comput Biol 2014; 10: e1003588
50. Leslie K, Skrzypek H, Paech MJ, Kurowski I, Whybrow T.
Dreaming during anesthesia and anesthetic depth in elective
surgery patients: a prospective cohort study. Anesthesiology
2007; 106: 33–42
51. Leslie K, Sleigh J, Paech MJ, et al. Dreaming and electroence-
phalographic changes during anesthesia maintained with
propofol or desflurane. Anesthesiology 2009; 111: 547–55
52. Samuelsson P, Brudin L, Sandin RH. BIS does not predict
dreams reported after anaesthesia.Acta Anaesthesiol Scand
2008; 52: 810–4
53. Samuelsson P, Brudin L, Sandin RH. Intraoperative dreams
reported after general anaesthesia are not early interpre-
tations of delayed awareness. Acta Anaesthesiol Scand
2008; 52: 805–9
Handling editor: H. C. Hemmings
i26 | Mashour and Avidan
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
during anesthesia: a closed claims analysis. Anesthesiology
1999; 90: 1053–61
24. Samuelsson P, Brudin L, Sandin RH. Late psychological symp-
toms after awareness among consecutively included surgical
patients. Anesthesiology 2007; 106: 26–32
25. Laukkala T, Ranta S, Wennervirta J, et al. Long-term psycho-
social outcomes after intraoperative awareness with recall.
Anesth Analg 2014; 119: 86–92
26. Whitlock E, Rodebaugh T, Hassett A, et al. Psychological se-
quelae of surgery in a prospective cohort of patients from
three intraoperative awareness prevention trials. Anesth
Analg 2015; 120: 87–95
27. Cook TM, Andrade J, Bogod DG, et al. 5th National Audit Pro-
ject (NAP5) on accidental awareness during general anaes-
thesia: patient experiences, human factors, sedation,
consent, and medicolegal issues. Br J Anaesth 2014;113:
560–74
28. Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral
index monitoring to prevent awareness during anaesthesia:
the B-Aware randomised controlled trial. Lancet 2004;363:
1757–63
29. Avidan MS, Jacobsohn E, Glick D, et al. Prevention of intrao-
perative awareness in a high-risk surgical population. N
Engl J Med 2011; 365: 591–600
30. Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness
and the bispectral index. N Engl J Med 2008; 358: 1097–108
31. Zhang C, Xu L, Ma YQ, et al. Bispectral index monitoring
prevent awareness during total intravenous anesthesia: a
prospective, randomized, double-blinded, multi-center con-
trolled trial. Chin Med J (Engl) 2011; 124: 3664–9
32. Avidan MS, Mashour GA. Prevention of intraoperative aware-
ness with explicit recall: making sense of the evidence.
Anesthesiology 2013; 118: 449–56
33. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N.
Bispectral index for improving anaesthetic delivery and post-
operative recovery. Cochrane Database Syst Rev 2014;6: CD003843
34. Bigelow H. Insensibility during surgical operations produced
by inhalation. The Boston Medicaland SurgicalJournal 1846;
XXXV: 309–17
35. Gray TC. A system of anaesthesia using d-tubocurarine chlor-
ide for chest surgery. Postgrad Med J 1948; 24: 514–26
36. Ghoneim MM, Block RI, Haffarnan M, Mathews MJ. Awareness
during anesthesia: risk factors, causes and sequelae: a review
of reported cases in the literature. Anesth Analg 2009;108:
527–35
37. Nickalls RW, Mahajan RP. Awareness and anaesthesia: think
dose, think data. Br J Anaesth 2010; 104: 1–2
38. Cheng VY, Martin LJ, Elliott EM, et al. α5GABAA receptors me-
diate the amnestic but not sedative-hypnotic effects of the
general anesthetic etomidate. J Neurosci 2006; 26: 3713–20
39. Kretschmannova K, Hines RM, Revilla-Sanchez R, et al.
Enhanced tonic inhibition influences the hypnotic and am-
nestic actions of the intravenous anesthetics etomidate and
propofol. J Neurosci 2013; 33: 7264–73
40. Jurd R, Arras M, Lambert S, et al. General anesthetic actions
in vivo strongly attenuated by a point mutation in the
GABAA receptor β3 subunit. FASEB J 2003; 17: 250–2
41. Zeller A, Arras M, Jurd R, Rudolph U. Mapping the contribu-
tion of β3-containing GABAA receptors to volatile and intra-
venous general anesthetic actions. BMC Pharmacol 2007; 7: 2
42. Aranake A, Gradwohl S, Ben-Abdallah A, et al. Increased risk
of intraoperative awareness in patients with a history of
awareness. Anesthesiology 2013; 119: 1275–83
43. Esaki RK, Mashour GA. Levels of consciousness during re-
gional anesthesia and monitored anesthesia care: patient
expectations and experiences. Anesth Analg 2009; 108:
1560–3
44. Kent CD, Mashour GA, Metzger NA, Posner KL, Domino KB.
Psychological impact of unexpected explicit recall of events
occurring during surgery performed under sedation, regional
anaesthesia, and general anaesthesia: data from the Anes-
thesia Awareness Registry. Br J Anaesth 2013; 110: 381–7
45. Crosby G. General anesthesia — minding the mind during
surgery. N Engl J Med 2011; 365: 660–1
46. Wang M, Messina AG, Russell IF. The topography of aware-
ness: a classification of intra-operative cognitive states.
Anaesthesia 2012; 67: 1197–201
47. Pandit JJ. Isolated forearm – or isolated brain? Interpreting re-
sponses during anaesthesia – or ‘dysanaesthesia’. Anaesthesia
2013; 68: 995–1000
48. Pandit JJ. Acceptably aware during general anaesthesia:
‘dysanaesthesia’ – the uncoupling of perception from sen-
sory inputs. Conscious Cogn 2014; 27: 194–212
49. Oizumi M, Albantakis L, Tononi G. From the phenomenology
to the mechanisms of consciousness: Integrated Information
Theory 3.0. PLoS Comput Biol 2014; 10: e1003588
50. Leslie K, Skrzypek H, Paech MJ, Kurowski I, Whybrow T.
Dreaming during anesthesia and anesthetic depth in elective
surgery patients: a prospective cohort study. Anesthesiology
2007; 106: 33–42
51. Leslie K, Sleigh J, Paech MJ, et al. Dreaming and electroence-
phalographic changes during anesthesia maintained with
propofol or desflurane. Anesthesiology 2009; 111: 547–55
52. Samuelsson P, Brudin L, Sandin RH. BIS does not predict
dreams reported after anaesthesia.Acta Anaesthesiol Scand
2008; 52: 810–4
53. Samuelsson P, Brudin L, Sandin RH. Intraoperative dreams
reported after general anaesthesia are not early interpre-
tations of delayed awareness. Acta Anaesthesiol Scand
2008; 52: 805–9
Handling editor: H. C. Hemmings
i26 | Mashour and Avidan
Downloaded from https://academic.oup.com/bja/article-abstract/115/suppl_1/i20/233608 by KERIS National Access user on 20 January 2020
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
