Pathophysiology of Ischemic Stroke: A Case Study Analysis
VerifiedAdded on 2023/01/16
|4
|1434
|38
Case Study
AI Summary
This case study presents the health illness of a 66-year-old man diagnosed with ischemic stroke due to extra-cranial embolism. The analysis identifies atrial fibrillation, hypertension, and age as key risk factors. The pathophysiology involves decreased cardiac muscle function, leading to reduced oxygen supply to the brain and subsequent embolism. Clinical manifestations include right-sided facial drooping and uncoordinated gait. The diagnosis involves physical examination, CT scans, MRIs, and cerebral angiograms. Treatment strategies encompass tissue plasminogen activator (tPA) administration and decompressed hemicraniectomy. Stroke rehabilitation is crucial, involving a multidisciplinary team including neurologists, physiotherapists, speech pathologists, dietitians, and counselors to support the patient's recovery and well-being. The case study underscores the importance of understanding the complex interplay of factors in ischemic stroke and the need for comprehensive patient care.
activity of the cardiac muscles
decreases
Ischemic stroke
Heart pump blood more
than capacity and failed
oxygen amount decreased in
the blood vessels of the brain
blood clot in brain which is
called extra-cranial embolism
Ischemic stroke
Lack of Coordination of CNS and
body
right-sided facial
drooping
dominant visual
gaze towards the
left
uncoordinated
gait
age
Hypertension
atrial fibrillation cerebral
angiogram
Computerized
tomography
Magnetic resonance
imaging
physical
examination
tissue
plasminogen
activator (TpA)
decompressed
hemicraniectomy
Stroke rehabilation
pathophysiology
Risk factor
Clinical manifestation
Etiology
keys
treatment
diagnosis
decreases
Ischemic stroke
Heart pump blood more
than capacity and failed
oxygen amount decreased in
the blood vessels of the brain
blood clot in brain which is
called extra-cranial embolism
Ischemic stroke
Lack of Coordination of CNS and
body
right-sided facial
drooping
dominant visual
gaze towards the
left
uncoordinated
gait
age
Hypertension
atrial fibrillation cerebral
angiogram
Computerized
tomography
Magnetic resonance
imaging
physical
examination
tissue
plasminogen
activator (TpA)
decompressed
hemicraniectomy
Stroke rehabilation
pathophysiology
Risk factor
Clinical manifestation
Etiology
keys
treatment
diagnosis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
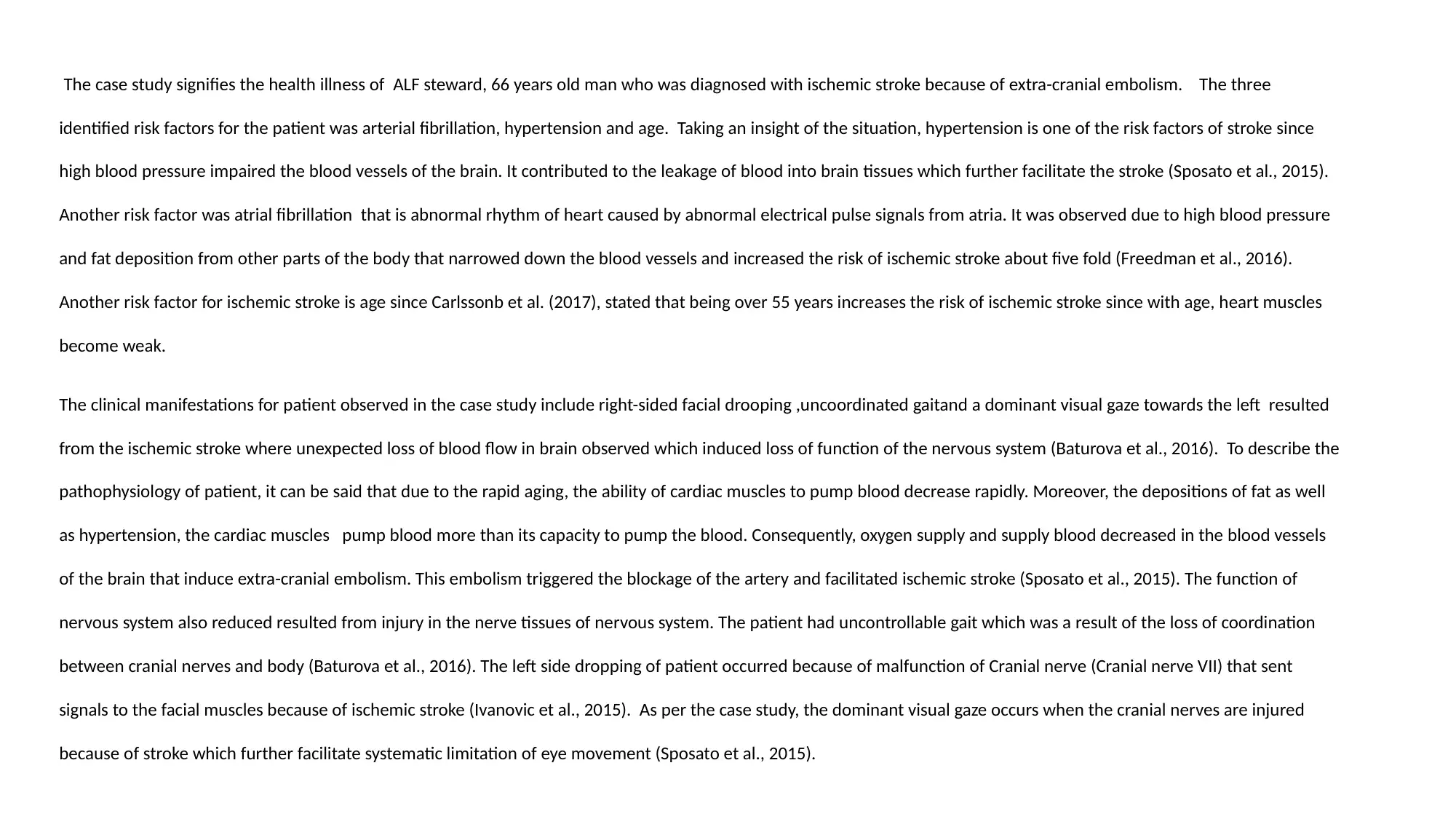
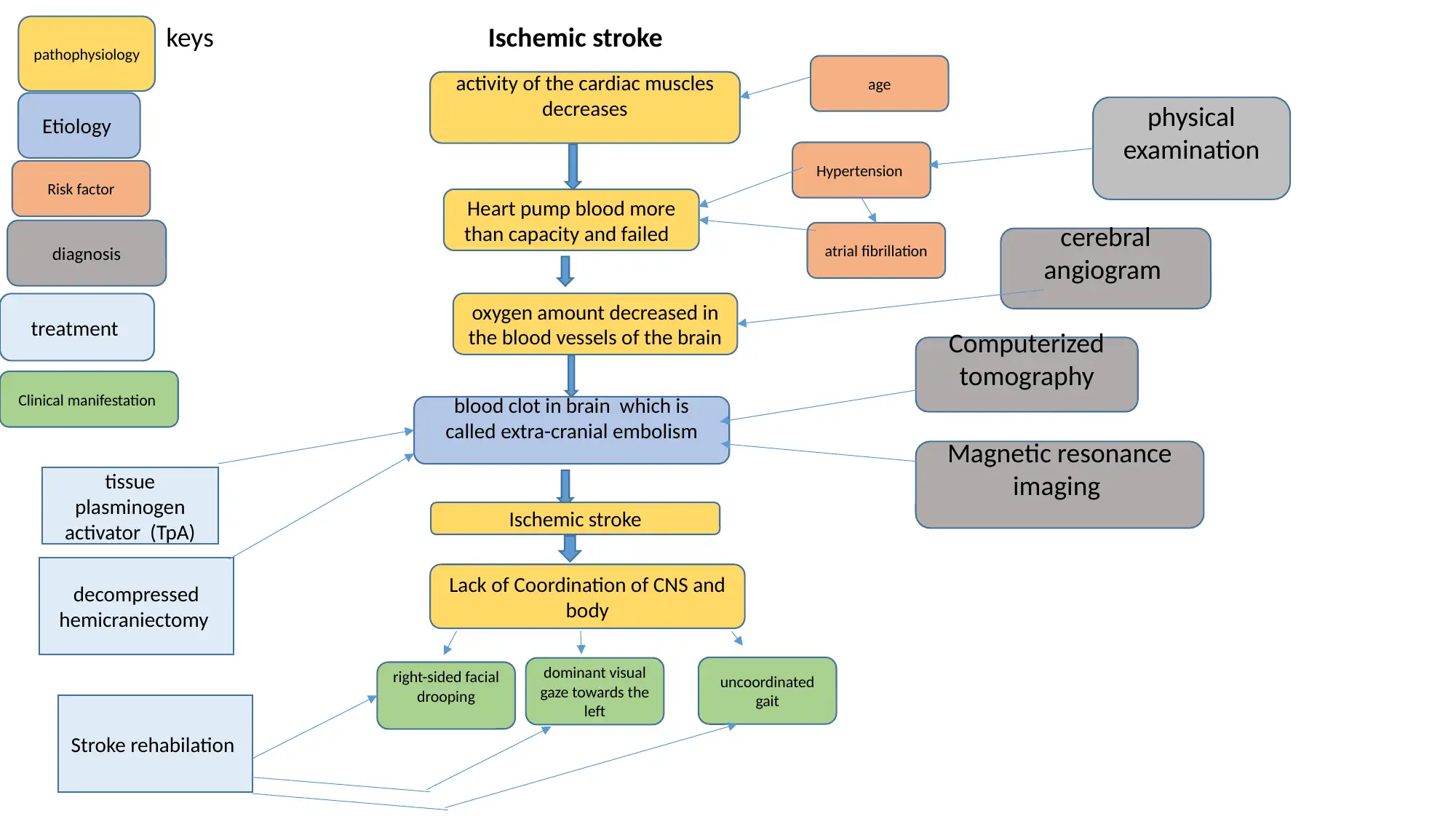
The case study signifies the health illness of ALF steward, 66 years old man who was diagnosed with ischemic stroke because of extra-cranial embolism. The three
identified risk factors for the patient was arterial fibrillation, hypertension and age. Taking an insight of the situation, hypertension is one of the risk factors of stroke since
high blood pressure impaired the blood vessels of the brain. It contributed to the leakage of blood into brain tissues which further facilitate the stroke (Sposato et al., 2015).
Another risk factor was atrial fibrillation that is abnormal rhythm of heart caused by abnormal electrical pulse signals from atria. It was observed due to high blood pressure
and fat deposition from other parts of the body that narrowed down the blood vessels and increased the risk of ischemic stroke about five fold (Freedman et al., 2016).
Another risk factor for ischemic stroke is age since Carlssonb et al. (2017), stated that being over 55 years increases the risk of ischemic stroke since with age, heart muscles
become weak.
The clinical manifestations for patient observed in the case study include right-sided facial drooping ,uncoordinated gaitand a dominant visual gaze towards the left resulted
from the ischemic stroke where unexpected loss of blood flow in brain observed which induced loss of function of the nervous system (Baturova et al., 2016). To describe the
pathophysiology of patient, it can be said that due to the rapid aging, the ability of cardiac muscles to pump blood decrease rapidly. Moreover, the depositions of fat as well
as hypertension, the cardiac muscles pump blood more than its capacity to pump the blood. Consequently, oxygen supply and supply blood decreased in the blood vessels
of the brain that induce extra-cranial embolism. This embolism triggered the blockage of the artery and facilitated ischemic stroke (Sposato et al., 2015). The function of
nervous system also reduced resulted from injury in the nerve tissues of nervous system. The patient had uncontrollable gait which was a result of the loss of coordination
between cranial nerves and body (Baturova et al., 2016). The left side dropping of patient occurred because of malfunction of Cranial nerve (Cranial nerve VII) that sent
signals to the facial muscles because of ischemic stroke (Ivanovic et al., 2015). As per the case study, the dominant visual gaze occurs when the cranial nerves are injured
because of stroke which further facilitate systematic limitation of eye movement (Sposato et al., 2015).
identified risk factors for the patient was arterial fibrillation, hypertension and age. Taking an insight of the situation, hypertension is one of the risk factors of stroke since
high blood pressure impaired the blood vessels of the brain. It contributed to the leakage of blood into brain tissues which further facilitate the stroke (Sposato et al., 2015).
Another risk factor was atrial fibrillation that is abnormal rhythm of heart caused by abnormal electrical pulse signals from atria. It was observed due to high blood pressure
and fat deposition from other parts of the body that narrowed down the blood vessels and increased the risk of ischemic stroke about five fold (Freedman et al., 2016).
Another risk factor for ischemic stroke is age since Carlssonb et al. (2017), stated that being over 55 years increases the risk of ischemic stroke since with age, heart muscles
become weak.
The clinical manifestations for patient observed in the case study include right-sided facial drooping ,uncoordinated gaitand a dominant visual gaze towards the left resulted
from the ischemic stroke where unexpected loss of blood flow in brain observed which induced loss of function of the nervous system (Baturova et al., 2016). To describe the
pathophysiology of patient, it can be said that due to the rapid aging, the ability of cardiac muscles to pump blood decrease rapidly. Moreover, the depositions of fat as well
as hypertension, the cardiac muscles pump blood more than its capacity to pump the blood. Consequently, oxygen supply and supply blood decreased in the blood vessels
of the brain that induce extra-cranial embolism. This embolism triggered the blockage of the artery and facilitated ischemic stroke (Sposato et al., 2015). The function of
nervous system also reduced resulted from injury in the nerve tissues of nervous system. The patient had uncontrollable gait which was a result of the loss of coordination
between cranial nerves and body (Baturova et al., 2016). The left side dropping of patient occurred because of malfunction of Cranial nerve (Cranial nerve VII) that sent
signals to the facial muscles because of ischemic stroke (Ivanovic et al., 2015). As per the case study, the dominant visual gaze occurs when the cranial nerves are injured
because of stroke which further facilitate systematic limitation of eye movement (Sposato et al., 2015).
In the clinical setting, first diagnosis would be physical examination and after that the best possible diagnosis would be CT scan where an array of X rays to generate fine
details of the brain and it displays hemorrhage by injecting dye in brain and neck blood vessel. It is the first line imaging technique which detects its blood clot within 48
hours (Wolf et al., 2018). MRI another suitable standard diagnosis approach since it detects 80% of infracts within 24 hours (Saver et al., 2016). It uses radio waves to
capture finer details of the damaged tissue of the brain. Hence it is more appropriate than the CT scan. Another suitable diagnosis is the cerebral angiogram whereby
using small incision a catheter is inserted to examine blood clotting and blood flow of brain a hence appropriate to gain the understanding of blood clot.
Considering the treatment, literature documented best suitable treatment is an emergency endovascular procedure such as injection of tissue plasminogen activator (tPA)
that disperse the blood clots of vessels and facilitate normal blood flow (Saver et al., 2016). The removal of blood clot using decompressed hemicraniectomy can be a
good treatment which include operating the skulls which help the brain to swell without being squashed. In the current context, after stroke, non-pharmacological
interventions would be assistance multidisciplinary team in a stroke rehabilitation which focuses on recovery for returning to independent life (Wolf et al., 2018). He
would require a rehabilitation doctor where patient would be assessed for her physical condition of the patient and with the collaboration of his wife as well as other
members of rehabilitation design interventions (Sposato et al., 2015). A neurologist would assess the activity of his nervous system. In order to assist in uncontrollable
gait, a physiotherapist would be required who will support in walking (Saver et al., 2016). Speech pathologist would assist in recovery and dietitian would design diet
devoid of high fat as well as Carbohydrate. A counselor would be required to support the mental wellbeing (Saver et al., 2016). A safe and comfortable environment would
be required to create in order to empower patient and boost self-esteem (Baturova et al., 2016).
details of the brain and it displays hemorrhage by injecting dye in brain and neck blood vessel. It is the first line imaging technique which detects its blood clot within 48
hours (Wolf et al., 2018). MRI another suitable standard diagnosis approach since it detects 80% of infracts within 24 hours (Saver et al., 2016). It uses radio waves to
capture finer details of the damaged tissue of the brain. Hence it is more appropriate than the CT scan. Another suitable diagnosis is the cerebral angiogram whereby
using small incision a catheter is inserted to examine blood clotting and blood flow of brain a hence appropriate to gain the understanding of blood clot.
Considering the treatment, literature documented best suitable treatment is an emergency endovascular procedure such as injection of tissue plasminogen activator (tPA)
that disperse the blood clots of vessels and facilitate normal blood flow (Saver et al., 2016). The removal of blood clot using decompressed hemicraniectomy can be a
good treatment which include operating the skulls which help the brain to swell without being squashed. In the current context, after stroke, non-pharmacological
interventions would be assistance multidisciplinary team in a stroke rehabilitation which focuses on recovery for returning to independent life (Wolf et al., 2018). He
would require a rehabilitation doctor where patient would be assessed for her physical condition of the patient and with the collaboration of his wife as well as other
members of rehabilitation design interventions (Sposato et al., 2015). A neurologist would assess the activity of his nervous system. In order to assist in uncontrollable
gait, a physiotherapist would be required who will support in walking (Saver et al., 2016). Speech pathologist would assist in recovery and dietitian would design diet
devoid of high fat as well as Carbohydrate. A counselor would be required to support the mental wellbeing (Saver et al., 2016). A safe and comfortable environment would
be required to create in order to empower patient and boost self-esteem (Baturova et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Aspberg, S., Smedback, K., Gigante, B., Yu, L., Chang, Y., & Singer, D. E. (2018). P6344 Pulmonary embolism is a possible risk factor for
ischemic stroke before 65 years of age in patients with atrial fibrillation. European Heart Journal, 39(suppl_1), ehy566-P6344.
https://doi.org/10.1093/eurheartj/ehy566.P6344
Baturova, M. A., Sheldon, S. H., Carlson, J., Brady, P. A., Lin, G., Rabinstein, A. A., ... & Platonov, P. G. (2016). Electrocardiographic and
Echocardiographic predictors of paroxysmal atrial fibrillation detected after ischemic stroke. BMC cardiovascular disorders, 16(1), 209.
https://doi.org/10.1186/s12872-016-0384-2
Freedman, B., Potpara, T. S., & Lip, G. Y. (2016). Stroke prevention in atrial fibrillation. The Lancet, 388(10046), 806-817. DOI:10.1136/jnnp-
2015-311947
Ivanovic, E., Zafirovic, S., ... & R Isenovic, E. (2017). Apoptosis and acute brain ischemia in ischemic stroke. Current vascular
pharmacology, 15(2), 115-122. doi.org/10.1111/cns.12326
Saver, J. L., Goyal, M., Van der Lugt, A. A. D., Menon, B. K., Majoie, C. B., Dippel, D. W., ... & Cardona, P. (2016). Time to treatment with
endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. Jama, 316(12), 1279-1289. DOI: 10.1056/NEJMoa1414905
Smits, P. C., Abdel-Wahab, M., Neumann, F. J., Boxma-de Klerk, B. M., Lunde, K., Schotborgh, C. E., ... & Hambrecht, R. (2017). Fractional flow
reserve–guidóed multivessel angioplasty in myocardial infarction. New England Journal of Medicine, 376(13), 1234-1244. DOI:
10.1056/NEJMoa1701067
Sposato, L. A., Cipriano, L. E., Saposnik, G., Vargas, E. R., Riccio, P. M., & Hachinski, V. (2015). Diagnosis of atrial fibrillation after stroke and
transient ischaemic attack: a systematic review and meta-analysis. The Lancet Neurology, 14(4), 377-387.
http://dx.doi.org/10.1016/S1474-4422(15)70027-X
Wolf, M. E., Ebert, AToth, M., Little, P., Arnberg, F., Häggkvist, J., Mulder, J., Halldin, C., ... & Holmin, S. (2016). Acute neuroinflammation in a
clinically relevant focal cortical ischemic stroke model in rat: longitudinal positron emission tomography and immunofluorescent tracking. Brain
Structure and Function, 221(3), 1279-1290. doi: 10.1586/14737175.4.2.255
Aspberg, S., Smedback, K., Gigante, B., Yu, L., Chang, Y., & Singer, D. E. (2018). P6344 Pulmonary embolism is a possible risk factor for
ischemic stroke before 65 years of age in patients with atrial fibrillation. European Heart Journal, 39(suppl_1), ehy566-P6344.
https://doi.org/10.1093/eurheartj/ehy566.P6344
Baturova, M. A., Sheldon, S. H., Carlson, J., Brady, P. A., Lin, G., Rabinstein, A. A., ... & Platonov, P. G. (2016). Electrocardiographic and
Echocardiographic predictors of paroxysmal atrial fibrillation detected after ischemic stroke. BMC cardiovascular disorders, 16(1), 209.
https://doi.org/10.1186/s12872-016-0384-2
Freedman, B., Potpara, T. S., & Lip, G. Y. (2016). Stroke prevention in atrial fibrillation. The Lancet, 388(10046), 806-817. DOI:10.1136/jnnp-
2015-311947
Ivanovic, E., Zafirovic, S., ... & R Isenovic, E. (2017). Apoptosis and acute brain ischemia in ischemic stroke. Current vascular
pharmacology, 15(2), 115-122. doi.org/10.1111/cns.12326
Saver, J. L., Goyal, M., Van der Lugt, A. A. D., Menon, B. K., Majoie, C. B., Dippel, D. W., ... & Cardona, P. (2016). Time to treatment with
endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. Jama, 316(12), 1279-1289. DOI: 10.1056/NEJMoa1414905
Smits, P. C., Abdel-Wahab, M., Neumann, F. J., Boxma-de Klerk, B. M., Lunde, K., Schotborgh, C. E., ... & Hambrecht, R. (2017). Fractional flow
reserve–guidóed multivessel angioplasty in myocardial infarction. New England Journal of Medicine, 376(13), 1234-1244. DOI:
10.1056/NEJMoa1701067
Sposato, L. A., Cipriano, L. E., Saposnik, G., Vargas, E. R., Riccio, P. M., & Hachinski, V. (2015). Diagnosis of atrial fibrillation after stroke and
transient ischaemic attack: a systematic review and meta-analysis. The Lancet Neurology, 14(4), 377-387.
http://dx.doi.org/10.1016/S1474-4422(15)70027-X
Wolf, M. E., Ebert, AToth, M., Little, P., Arnberg, F., Häggkvist, J., Mulder, J., Halldin, C., ... & Holmin, S. (2016). Acute neuroinflammation in a
clinically relevant focal cortical ischemic stroke model in rat: longitudinal positron emission tomography and immunofluorescent tracking. Brain
Structure and Function, 221(3), 1279-1290. doi: 10.1586/14737175.4.2.255
1 out of 4
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





