Detailed Case Study: John's Mental Health, Treatment, and Nursing Care
VerifiedAdded on 2020/03/04
|12
|2312
|309
Case Study
AI Summary
This case study presents John, a 45-year-old man referred to Monash Medical Centre due to anxiety, depression, and physical symptoms. The case details John's medical history, including headaches, muscle pain, and a history of anxiety and depression. A mental status examination reveals decreased thought processes and anxiety related to his health and financial instability. The case formulation identifies major depressive disorder and anxiety as the main concerns, with predisposing factors including family history and genetic factors. Precipitating factors include financial dependence, physical injuries, and psychosocial stressors. Perpetuating factors involve financial strain and his son's developmental disability. The care plan outlines nursing interventions focusing on establishing a therapeutic relationship, allowing expression of feelings, arranging group sessions, and occupational therapy, with goals to improve emotional expression, work function, and self-motivation. References to relevant literature support the analysis and care plan.

Running head: CASE STUDY OF JOHN
Case Study of John
Name of the Student
Name of the University
Author note
Case Study of John
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CASE STUDY OF JOHN
Past Medical History
John is 45-year-old man who is living with his family. John was referred to the Monash
Medical centre with the history of headache and muscle pain in the legs that he was forced to
leave his job as a carpenter. Upon diagnosis, it was found that John was going through anxiety
and depression that have worsened in the past few months.
Mental Status Examination
General description
John is an English Carpenter who is has come with the problem of major muscular pain
and has problems in sitting and while walking. He is well oriented and well perfuse. There was
no abnormality found while looking at him.
Mood and Affect
He does not have any extreme mood while talking to him. However, he remained
disturbed due to his pain in the muscles.
Speech
John articulated himself very clearly. He answered all the questions very clearly but in a
slower rate. He has soft spoken man and was having some breathing problems while talking for a
very long time.
Perceptual disturbances
John exhibits a normal perception. The symptoms of illusions, delusions, hallucinations,
misinterpretation and passively phenomenon were not seen elicited in John.
Past Medical History
John is 45-year-old man who is living with his family. John was referred to the Monash
Medical centre with the history of headache and muscle pain in the legs that he was forced to
leave his job as a carpenter. Upon diagnosis, it was found that John was going through anxiety
and depression that have worsened in the past few months.
Mental Status Examination
General description
John is an English Carpenter who is has come with the problem of major muscular pain
and has problems in sitting and while walking. He is well oriented and well perfuse. There was
no abnormality found while looking at him.
Mood and Affect
He does not have any extreme mood while talking to him. However, he remained
disturbed due to his pain in the muscles.
Speech
John articulated himself very clearly. He answered all the questions very clearly but in a
slower rate. He has soft spoken man and was having some breathing problems while talking for a
very long time.
Perceptual disturbances
John exhibits a normal perception. The symptoms of illusions, delusions, hallucinations,
misinterpretation and passively phenomenon were not seen elicited in John.
2CASE STUDY OF JOHN
Thought Processes
The thought process of John has decreased. It has also decreased the rate of the speech in
him. He did not exhibit any formal form of thought disorder. He did not use or created his own
word to express his feelings. No negative thought disorder was seen in John.
However, John is very much disturbed and anxious about his health and feels restless
while thinking about his health. He is very much guilty that he is unable to care of himself and
finance his own medication.
Cognition
John is alert and oriented in terms of time and place. He is able to answer all the
questions asked about his past and is able to recall every single incident.
Judgement and Insights treatment
However, when John was questioned about his condition, he accepted that he is ill and he
requires treatment
Case formulation
Summary of presenting problems
80% blood clot in his left leg
Persistent and worsened headache over a last 4 weeks
Experienced non-epileptic tremors
Symptoms of anxiety and irritability
Acute depression
Thought Processes
The thought process of John has decreased. It has also decreased the rate of the speech in
him. He did not exhibit any formal form of thought disorder. He did not use or created his own
word to express his feelings. No negative thought disorder was seen in John.
However, John is very much disturbed and anxious about his health and feels restless
while thinking about his health. He is very much guilty that he is unable to care of himself and
finance his own medication.
Cognition
John is alert and oriented in terms of time and place. He is able to answer all the
questions asked about his past and is able to recall every single incident.
Judgement and Insights treatment
However, when John was questioned about his condition, he accepted that he is ill and he
requires treatment
Case formulation
Summary of presenting problems
80% blood clot in his left leg
Persistent and worsened headache over a last 4 weeks
Experienced non-epileptic tremors
Symptoms of anxiety and irritability
Acute depression
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CASE STUDY OF JOHN
Insomnia
History of melancholy
Fear of brain tumor
Financial crisis and stress
Main concern
Major depressive disorder and anxiety is the main concern of the client.
Predisposing factors
John has a strong family history, which predisposes him to develop a mood disorder.
According to Levinson et al. (2014), a large sample of people diagnosed with non-anxious
control and general anxiety disorder showed the family history of the psychological
problems. As per the behavioral genetics research, metal disorders are highly
attributed to genetic factors. In the govern case study, John’s parental cousin Bipolar
Affective Disorder and maternal cousin has anxiety. His older brother, Jeffrey has also suffered
from panic and depression with admission at the clinic previously. His youngest brother, James
is currently suffering from severe sleep deprivation due to being the new father of twins. John’s
father suffered from Post-Traumatic Stress Disorder. Thus, it is evident that these genetic
factors have cumulative influence on John’s psychological condition.
Precipitating factors
The precipitating factor in case of John is the financial dependence. He is financially not
stable to fund the whole process of medications. Due to lack of financial independence, John
Insomnia
History of melancholy
Fear of brain tumor
Financial crisis and stress
Main concern
Major depressive disorder and anxiety is the main concern of the client.
Predisposing factors
John has a strong family history, which predisposes him to develop a mood disorder.
According to Levinson et al. (2014), a large sample of people diagnosed with non-anxious
control and general anxiety disorder showed the family history of the psychological
problems. As per the behavioral genetics research, metal disorders are highly
attributed to genetic factors. In the govern case study, John’s parental cousin Bipolar
Affective Disorder and maternal cousin has anxiety. His older brother, Jeffrey has also suffered
from panic and depression with admission at the clinic previously. His youngest brother, James
is currently suffering from severe sleep deprivation due to being the new father of twins. John’s
father suffered from Post-Traumatic Stress Disorder. Thus, it is evident that these genetic
factors have cumulative influence on John’s psychological condition.
Precipitating factors
The precipitating factor in case of John is the financial dependence. He is financially not
stable to fund the whole process of medications. Due to lack of financial independence, John
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CASE STUDY OF JOHN
started to have symptoms of anxiety and irritability. Anxiety and acute depression added to
insomnia. (Cruwys et al. 2014). The history of drug and alcohol also precipitated his current
condition. In addition, John has also suffered a lot of physical injuries. He suffered a spider bite
that developed into cellulitis requiring IV antibiotics. He ruptured his anterior cruciate ligament
while on the trampoline and had to undergo surgery. After debilitating pain from osteitis pubis he
also had to undergo psychiatric consolation.
John also carries the feeling of guilt as he was not able to save his co-worker. He had
short term relationships with his two women in the past, which may add to his guilt. Other
precipitating factors are One of his sons has a developmental difficulty that has been categorized
as a sensory processing disorder with attention deficit disorder. John was treated for a depressive
illness that emerged after his son’s developmental difficulties. Increasing alcohol consumption of
John’s wife Marie is the other cause of anxiety in John (Catarino et al. 2014).
The stress due to workplace bullying and fatal accident led to multiple inpatient
admissions. Thus, he is currently in need of social support of community. The lack of
rationalized thoughts, anger, guilt, lack of personal hygiene, and lack of financial stability are the
precipitating factors of John. These factors are manifested as escalating panic attacks and phobic
responses to the workplace, pervasively low mood and neuro-vegetative symptoms. John has the
fear of brain tumor is further adding to anxiety and depression These psychosocial stressors are
responsible for the Major depressive disorder and anxiety in the patient (Song and Lindquist
2015).
Perpetuating factors
started to have symptoms of anxiety and irritability. Anxiety and acute depression added to
insomnia. (Cruwys et al. 2014). The history of drug and alcohol also precipitated his current
condition. In addition, John has also suffered a lot of physical injuries. He suffered a spider bite
that developed into cellulitis requiring IV antibiotics. He ruptured his anterior cruciate ligament
while on the trampoline and had to undergo surgery. After debilitating pain from osteitis pubis he
also had to undergo psychiatric consolation.
John also carries the feeling of guilt as he was not able to save his co-worker. He had
short term relationships with his two women in the past, which may add to his guilt. Other
precipitating factors are One of his sons has a developmental difficulty that has been categorized
as a sensory processing disorder with attention deficit disorder. John was treated for a depressive
illness that emerged after his son’s developmental difficulties. Increasing alcohol consumption of
John’s wife Marie is the other cause of anxiety in John (Catarino et al. 2014).
The stress due to workplace bullying and fatal accident led to multiple inpatient
admissions. Thus, he is currently in need of social support of community. The lack of
rationalized thoughts, anger, guilt, lack of personal hygiene, and lack of financial stability are the
precipitating factors of John. These factors are manifested as escalating panic attacks and phobic
responses to the workplace, pervasively low mood and neuro-vegetative symptoms. John has the
fear of brain tumor is further adding to anxiety and depression These psychosocial stressors are
responsible for the Major depressive disorder and anxiety in the patient (Song and Lindquist
2015).
Perpetuating factors
5CASE STUDY OF JOHN
The major perpetuating factor is the financial strain which is allowing John’s depression
to continue. It is the ongoing problem along with the debilitating pain from osteitis pubis it is
also adding to stress. His son’s developmental disability. Fear of brain tumor and wife;s
increasing alcohol consumption are the perpetuating factors. The use of the antidepressant and
antipsychotic medication and treatment process in condition where he is having financial crisis is
increasing his depressive state (Swank et al. 2014).
Protective factors
The protective factors in case of John are having ECT that improved is condition,
adequate family support to cope with illness, ongoing medications to improve his physical
health. His perceptions, insight and judgments are good. As John is cooperative, he is suppose to
recover soon provided he adheres to medication and interventions (Cuijpers et al. 2014).
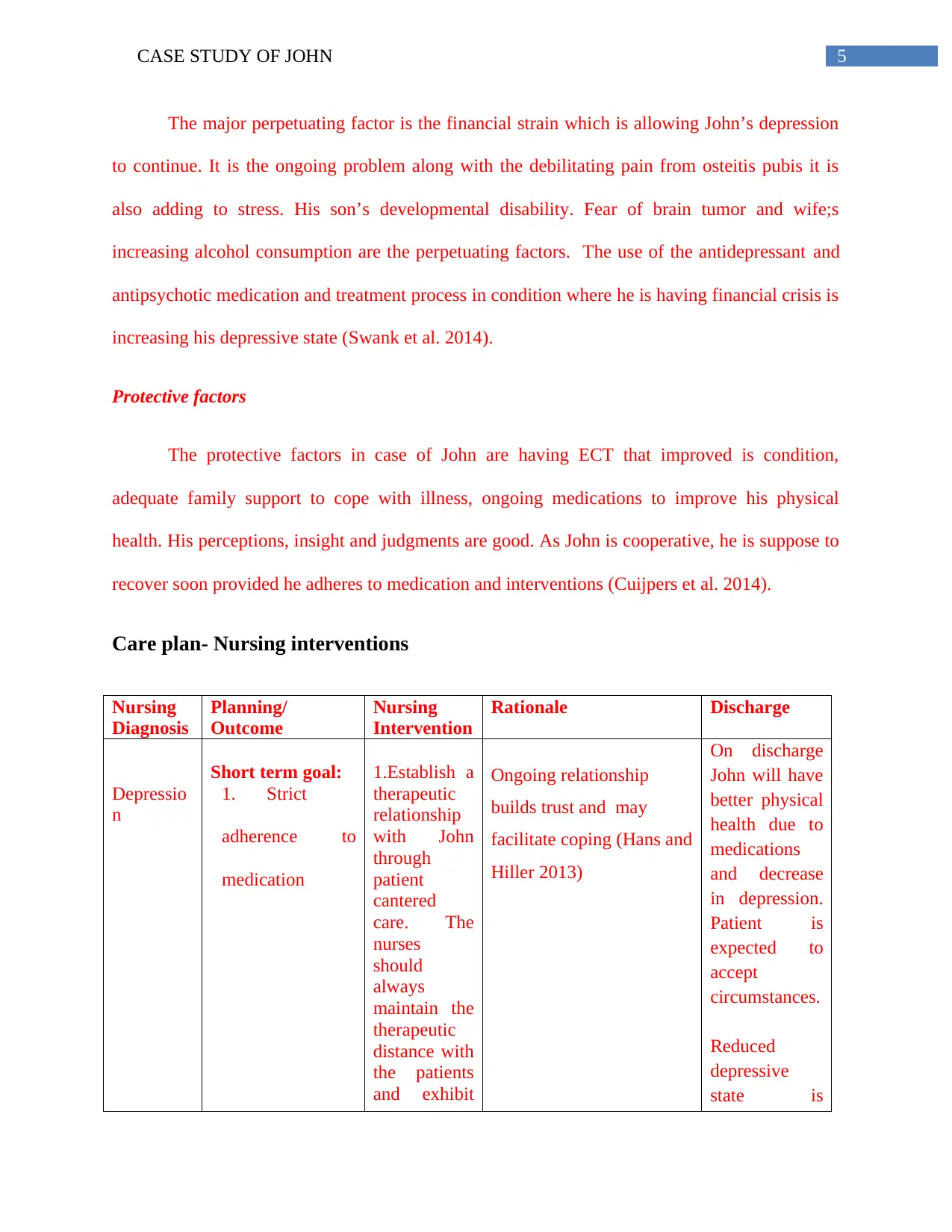
Care plan- Nursing interventions
Nursing
Diagnosis
Planning/
Outcome
Nursing
Intervention
Rationale Discharge
Depressio
n
Short term goal:
1. Strict
adherence to
medication
1.Establish a
therapeutic
relationship
with John
through
patient
cantered
care. The
nurses
should
always
maintain the
therapeutic
distance with
the patients
and exhibit
Ongoing relationship
builds trust and may
facilitate coping (Hans and
Hiller 2013)
On discharge
John will have
better physical
health due to
medications
and decrease
in depression.
Patient is
expected to
accept
circumstances.
Reduced
depressive
state is
The major perpetuating factor is the financial strain which is allowing John’s depression
to continue. It is the ongoing problem along with the debilitating pain from osteitis pubis it is
also adding to stress. His son’s developmental disability. Fear of brain tumor and wife;s
increasing alcohol consumption are the perpetuating factors. The use of the antidepressant and
antipsychotic medication and treatment process in condition where he is having financial crisis is
increasing his depressive state (Swank et al. 2014).
Protective factors
The protective factors in case of John are having ECT that improved is condition,
adequate family support to cope with illness, ongoing medications to improve his physical
health. His perceptions, insight and judgments are good. As John is cooperative, he is suppose to
recover soon provided he adheres to medication and interventions (Cuijpers et al. 2014).
Care plan- Nursing interventions
Nursing
Diagnosis
Planning/
Outcome
Nursing
Intervention
Rationale Discharge
Depressio
n
Short term goal:
1. Strict
adherence to
medication
1.Establish a
therapeutic
relationship
with John
through
patient
cantered
care. The
nurses
should
always
maintain the
therapeutic
distance with
the patients
and exhibit
Ongoing relationship
builds trust and may
facilitate coping (Hans and
Hiller 2013)
On discharge
John will have
better physical
health due to
medications
and decrease
in depression.
Patient is
expected to
accept
circumstances.
Reduced
depressive
state is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CASE STUDY OF JOHN
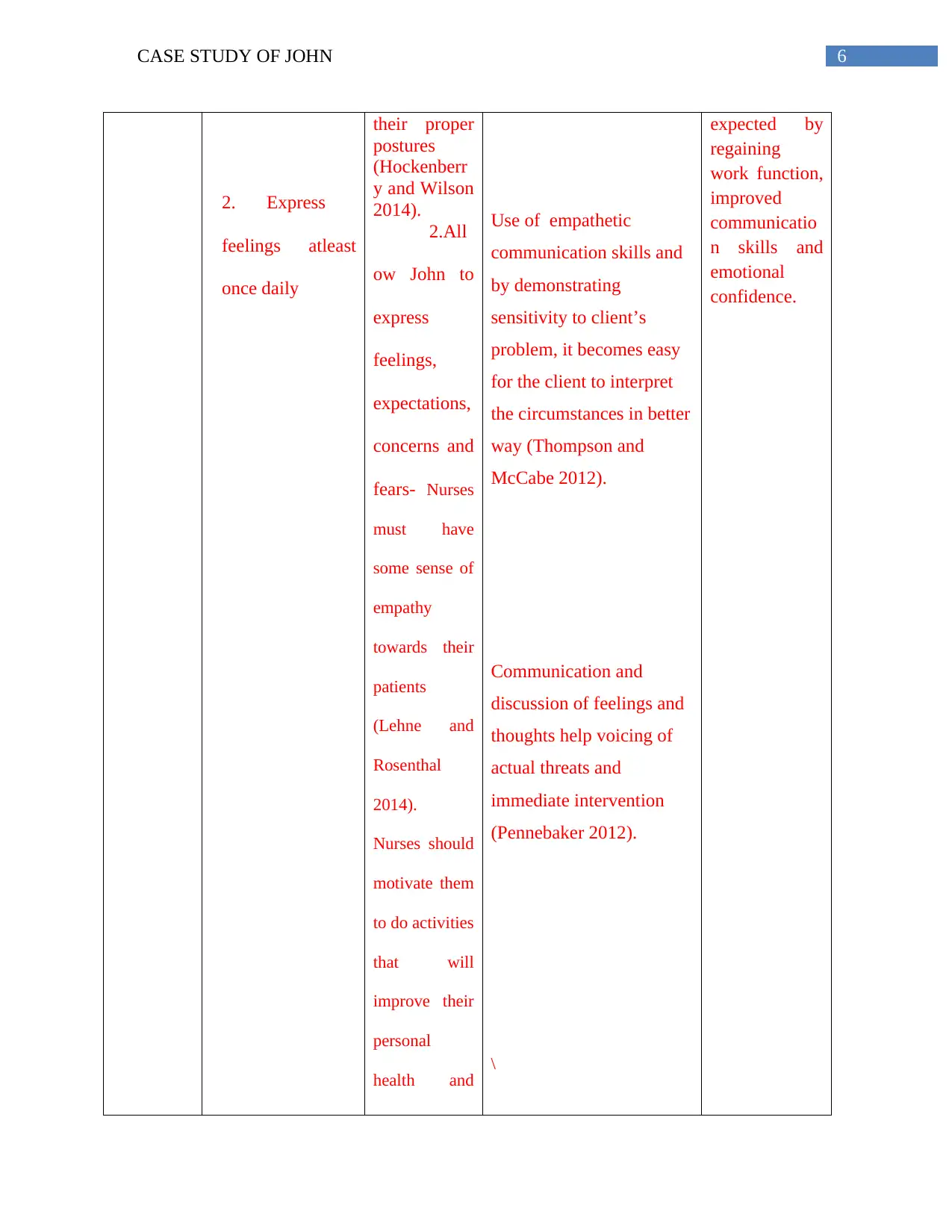
2. Express
feelings atleast
once daily
their proper
postures
(Hockenberr
y and Wilson
2014).
2.All
ow John to
express
feelings,
expectations,
concerns and
fears- Nurses
must have
some sense of
empathy
towards their
patients
(Lehne and
Rosenthal
2014).
Nurses should
motivate them
to do activities
that will
improve their
personal
health and
Use of empathetic
communication skills and
by demonstrating
sensitivity to client’s
problem, it becomes easy
for the client to interpret
the circumstances in better
way (Thompson and
McCabe 2012).
Communication and
discussion of feelings and
thoughts help voicing of
actual threats and
immediate intervention
(Pennebaker 2012).
\
expected by
regaining
work function,
improved
communicatio
n skills and
emotional
confidence.
2. Express
feelings atleast
once daily
their proper
postures
(Hockenberr
y and Wilson
2014).
2.All
ow John to
express
feelings,
expectations,
concerns and
fears- Nurses
must have
some sense of
empathy
towards their
patients
(Lehne and
Rosenthal
2014).
Nurses should
motivate them
to do activities
that will
improve their
personal
health and
Use of empathetic
communication skills and
by demonstrating
sensitivity to client’s
problem, it becomes easy
for the client to interpret
the circumstances in better
way (Thompson and
McCabe 2012).
Communication and
discussion of feelings and
thoughts help voicing of
actual threats and
immediate intervention
(Pennebaker 2012).
\
expected by
regaining
work function,
improved
communicatio
n skills and
emotional
confidence.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY OF JOHN
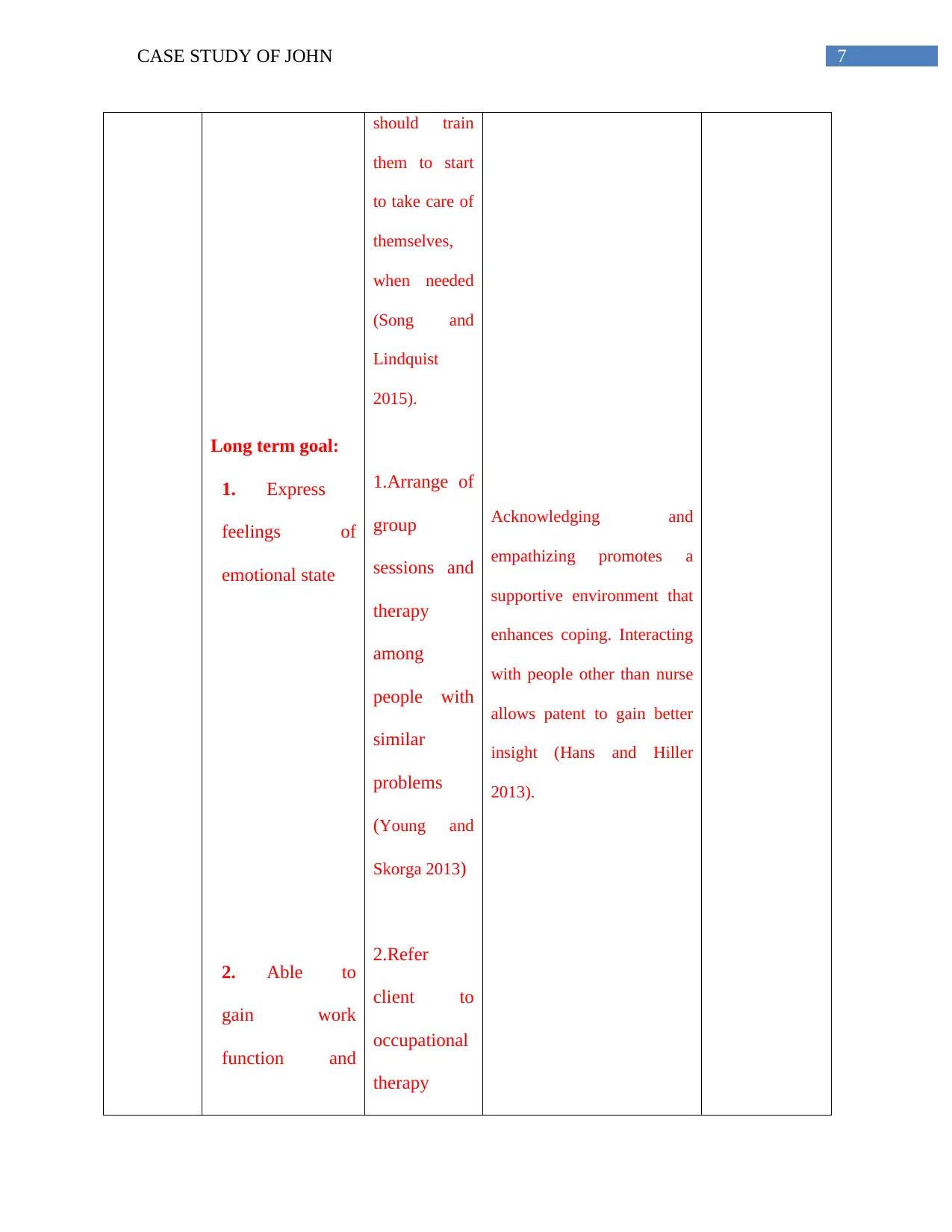
Long term goal:
1. Express
feelings of
emotional state
2. Able to
gain work
function and
should train
them to start
to take care of
themselves,
when needed
(Song and
Lindquist
2015).
1.Arrange of
group
sessions and
therapy
among
people with
similar
problems
(Young and
Skorga 2013)
2.Refer
client to
occupational
therapy
Acknowledging and
empathizing promotes a
supportive environment that
enhances coping. Interacting
with people other than nurse
allows patent to gain better
insight (Hans and Hiller
2013).
Long term goal:
1. Express
feelings of
emotional state
2. Able to
gain work
function and
should train
them to start
to take care of
themselves,
when needed
(Song and
Lindquist
2015).
1.Arrange of
group
sessions and
therapy
among
people with
similar
problems
(Young and
Skorga 2013)
2.Refer
client to
occupational
therapy
Acknowledging and
empathizing promotes a
supportive environment that
enhances coping. Interacting
with people other than nurse
allows patent to gain better
insight (Hans and Hiller
2013).
8CASE STUDY OF JOHN
maintain and job
Occupational therapy will
help client to gain
independent functioning by
learning new skills to cope
with personal and
professional activities in
daily basis (Muskett 2014).
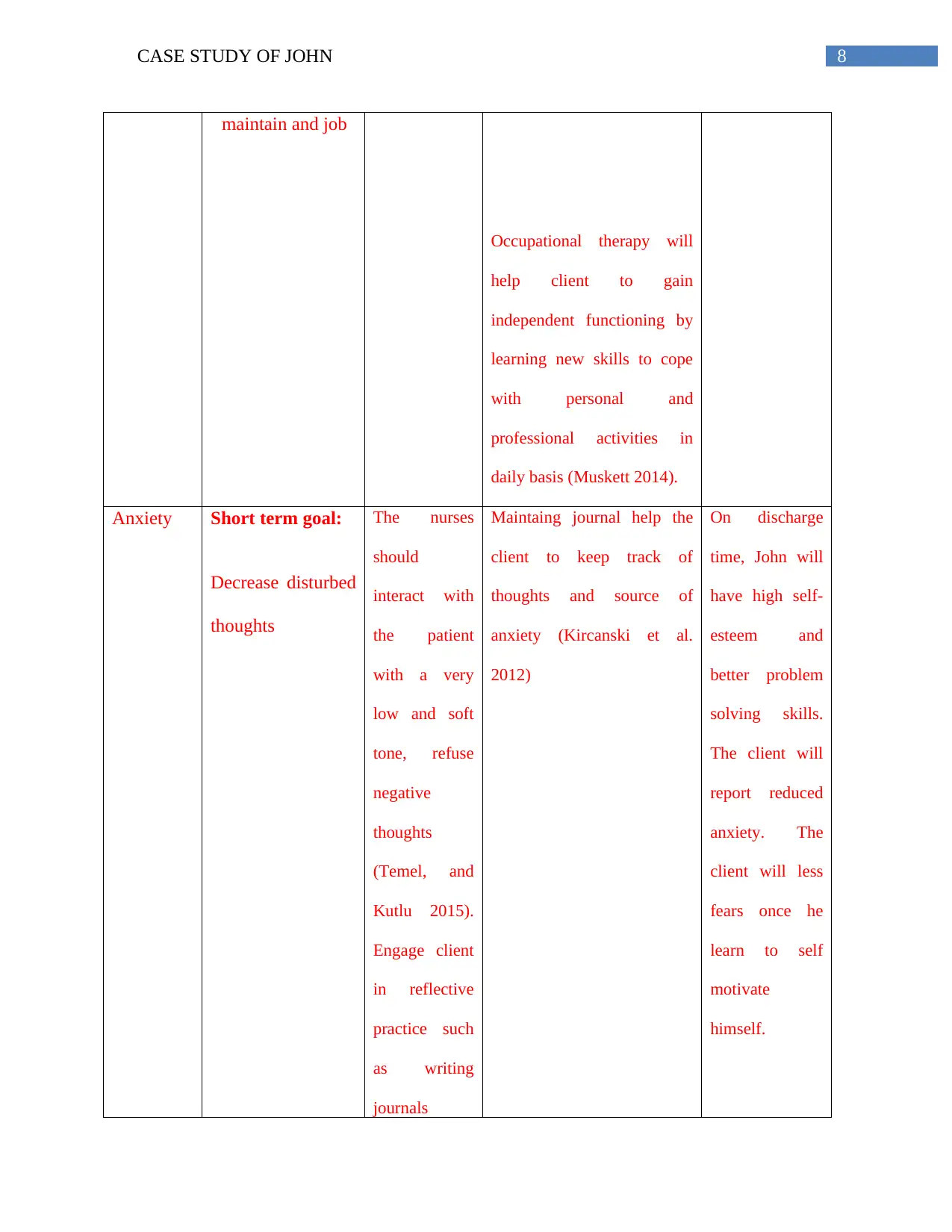
Anxiety Short term goal:
Decrease disturbed
thoughts
The nurses
should
interact with
the patient
with a very
low and soft
tone, refuse
negative
thoughts
(Temel, and
Kutlu 2015).
Engage client
in reflective
practice such
as writing
journals
Maintaing journal help the
client to keep track of
thoughts and source of
anxiety (Kircanski et al.
2012)
On discharge
time, John will
have high self-
esteem and
better problem
solving skills.
The client will
report reduced
anxiety. The
client will less
fears once he
learn to self
motivate
himself.
maintain and job
Occupational therapy will
help client to gain
independent functioning by
learning new skills to cope
with personal and
professional activities in
daily basis (Muskett 2014).
Anxiety Short term goal:
Decrease disturbed
thoughts
The nurses
should
interact with
the patient
with a very
low and soft
tone, refuse
negative
thoughts
(Temel, and
Kutlu 2015).
Engage client
in reflective
practice such
as writing
journals
Maintaing journal help the
client to keep track of
thoughts and source of
anxiety (Kircanski et al.
2012)
On discharge
time, John will
have high self-
esteem and
better problem
solving skills.
The client will
report reduced
anxiety. The
client will less
fears once he
learn to self
motivate
himself.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CASE STUDY OF JOHN
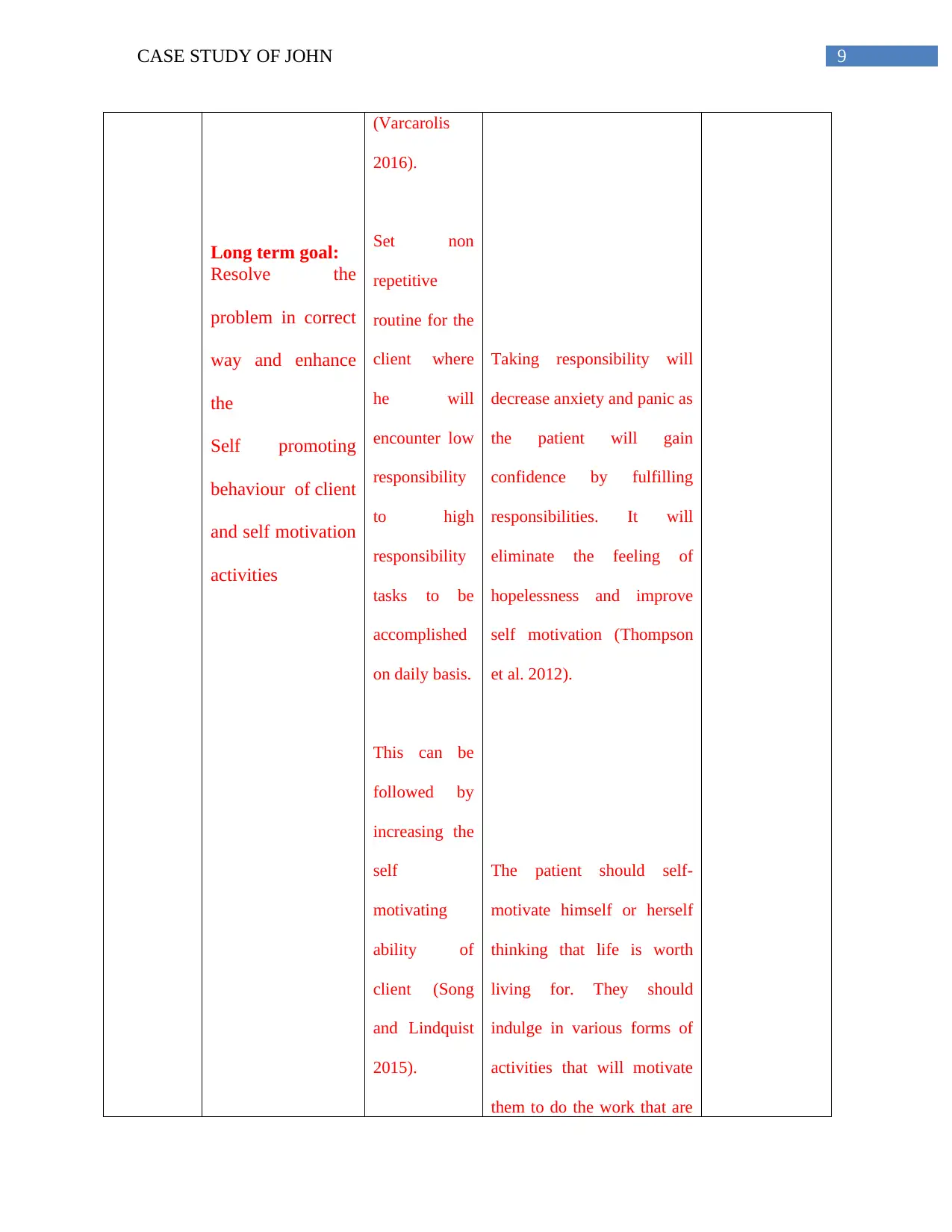
Long term goal:
Resolve the
problem in correct
way and enhance
the
Self promoting
behaviour of client
and self motivation
activities
(Varcarolis
2016).
Set non
repetitive
routine for the
client where
he will
encounter low
responsibility
to high
responsibility
tasks to be
accomplished
on daily basis.
This can be
followed by
increasing the
self
motivating
ability of
client (Song
and Lindquist
2015).
Taking responsibility will
decrease anxiety and panic as
the patient will gain
confidence by fulfilling
responsibilities. It will
eliminate the feeling of
hopelessness and improve
self motivation (Thompson
et al. 2012).
The patient should self-
motivate himself or herself
thinking that life is worth
living for. They should
indulge in various forms of
activities that will motivate
them to do the work that are
Long term goal:
Resolve the
problem in correct
way and enhance
the
Self promoting
behaviour of client
and self motivation
activities
(Varcarolis
2016).
Set non
repetitive
routine for the
client where
he will
encounter low
responsibility
to high
responsibility
tasks to be
accomplished
on daily basis.
This can be
followed by
increasing the
self
motivating
ability of
client (Song
and Lindquist
2015).
Taking responsibility will
decrease anxiety and panic as
the patient will gain
confidence by fulfilling
responsibilities. It will
eliminate the feeling of
hopelessness and improve
self motivation (Thompson
et al. 2012).
The patient should self-
motivate himself or herself
thinking that life is worth
living for. They should
indulge in various forms of
activities that will motivate
them to do the work that are
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10CASE STUDY OF JOHN
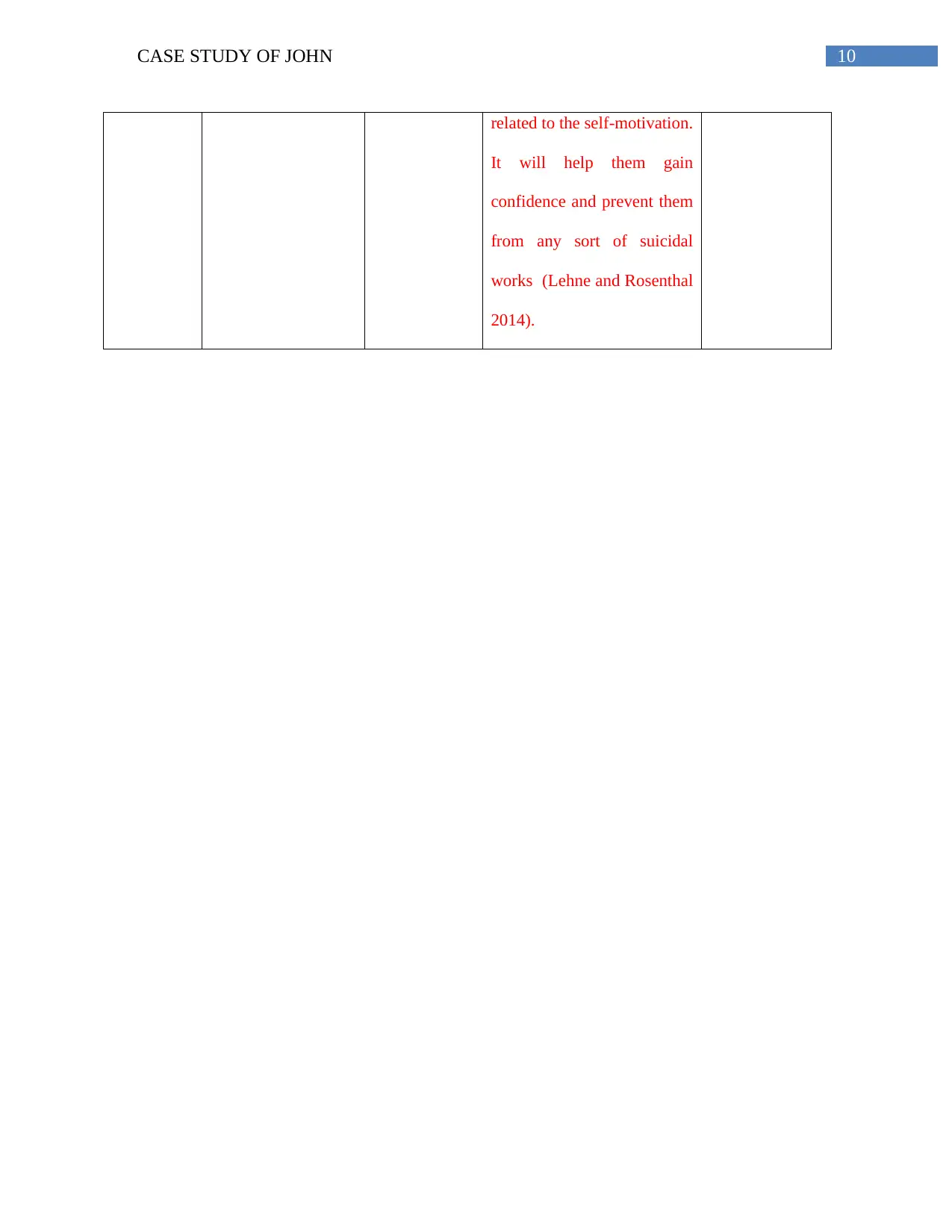
related to the self-motivation.
It will help them gain
confidence and prevent them
from any sort of suicidal
works (Lehne and Rosenthal
2014).
related to the self-motivation.
It will help them gain
confidence and prevent them
from any sort of suicidal
works (Lehne and Rosenthal
2014).
11CASE STUDY OF JOHN
References
Catarino, F., Gilbert, P., McEwan, K. and Baião, R., 2014. Compassion motivations:
Distinguishing submissive compassion from genuine compassion and its association with shame,
submissive behavior, depression, anxiety and stress. Journal of Social and Clinical
Psychology, 33(5), pp.399-412.
Cruwys, T., Haslam, S.A., Dingle, G.A., Haslam, C. and Jetten, J., 2014. Depression and social
identity: An integrative review. Personality and Social Psychology Review, 18(3), pp.215-238.
Cuijpers, P., Sijbrandij, M., Koole, S.L., Andersson, G., Beekman, A.T. and Reynolds, C.F.,
2014. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a
meta‐analysis. World Psychiatry, 13(1), pp.56-67.
Hans, E. and Hiller, W., 2013. A meta-analysis of nonrandomized effectiveness studies on
outpatient cognitive behavioral therapy for adult anxiety disorders. Clinical Psychology
Review, 33(8), pp.954-964.
Hockenberry, M.J. and Wilson, D., 2014. Wong's Nursing Care of Infants and Children-E-Book.
Elsevier Health Sciences.
Kircanski, K., Lieberman, M.D. and Craske, M.G., 2012. Feelings into words: contributions of
language to exposure therapy. Psychological science, 23(10), pp.1086-1091.
Lehne, R.A. and Rosenthal, L., 2014. Pharmacology for Nursing Care-E-Book. Elsevier Health
Sciences.
References
Catarino, F., Gilbert, P., McEwan, K. and Baião, R., 2014. Compassion motivations:
Distinguishing submissive compassion from genuine compassion and its association with shame,
submissive behavior, depression, anxiety and stress. Journal of Social and Clinical
Psychology, 33(5), pp.399-412.
Cruwys, T., Haslam, S.A., Dingle, G.A., Haslam, C. and Jetten, J., 2014. Depression and social
identity: An integrative review. Personality and Social Psychology Review, 18(3), pp.215-238.
Cuijpers, P., Sijbrandij, M., Koole, S.L., Andersson, G., Beekman, A.T. and Reynolds, C.F.,
2014. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a
meta‐analysis. World Psychiatry, 13(1), pp.56-67.
Hans, E. and Hiller, W., 2013. A meta-analysis of nonrandomized effectiveness studies on
outpatient cognitive behavioral therapy for adult anxiety disorders. Clinical Psychology
Review, 33(8), pp.954-964.
Hockenberry, M.J. and Wilson, D., 2014. Wong's Nursing Care of Infants and Children-E-Book.
Elsevier Health Sciences.
Kircanski, K., Lieberman, M.D. and Craske, M.G., 2012. Feelings into words: contributions of
language to exposure therapy. Psychological science, 23(10), pp.1086-1091.
Lehne, R.A. and Rosenthal, L., 2014. Pharmacology for Nursing Care-E-Book. Elsevier Health
Sciences.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




