Langara College Philosophy 1105: Jimmy T Case Study Analysis
VerifiedAdded on 2022/10/17
|8
|1886
|353
Case Study
AI Summary
This case study analyzes the ethical challenges presented in the case of Jimmy T, an 11-year-old boy with lymphoma and an incurable neurological disease. The assignment requires an application of philosophical tools and concepts to address the ethical dilemmas. The paper identifies relevant facts using the Four Topics, moral principles, and a central moral problem. The central moral problem in this case is the patient's unwillingness to proceed with chemotherapy. The analysis emphasizes the importance of oncologist-patient communication, informed consent, and the balance between patient autonomy and medical intervention. The paper discusses the moral values in cancer care, including the benefits of treatment, the role of oncologists, and the impact of cost factors. The paper also highlights the importance of clear communication, realistic discussions, and the creation of trust between the doctor and the patient. The assignment draws on the provided case study and encourages the use of course materials to explore the ethical dimensions of the case. It also provides insights into the professional responsibilities of oncologists and the importance of ethical methodology in medical practice, emphasizing the need for shared decision-making and the consideration of patient preferences and values.

Running Head : CLINICAL CARE
Clinical Care
Name of the Student
Name of the University
Author Note
Clinical Care
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CLINICAL CARE
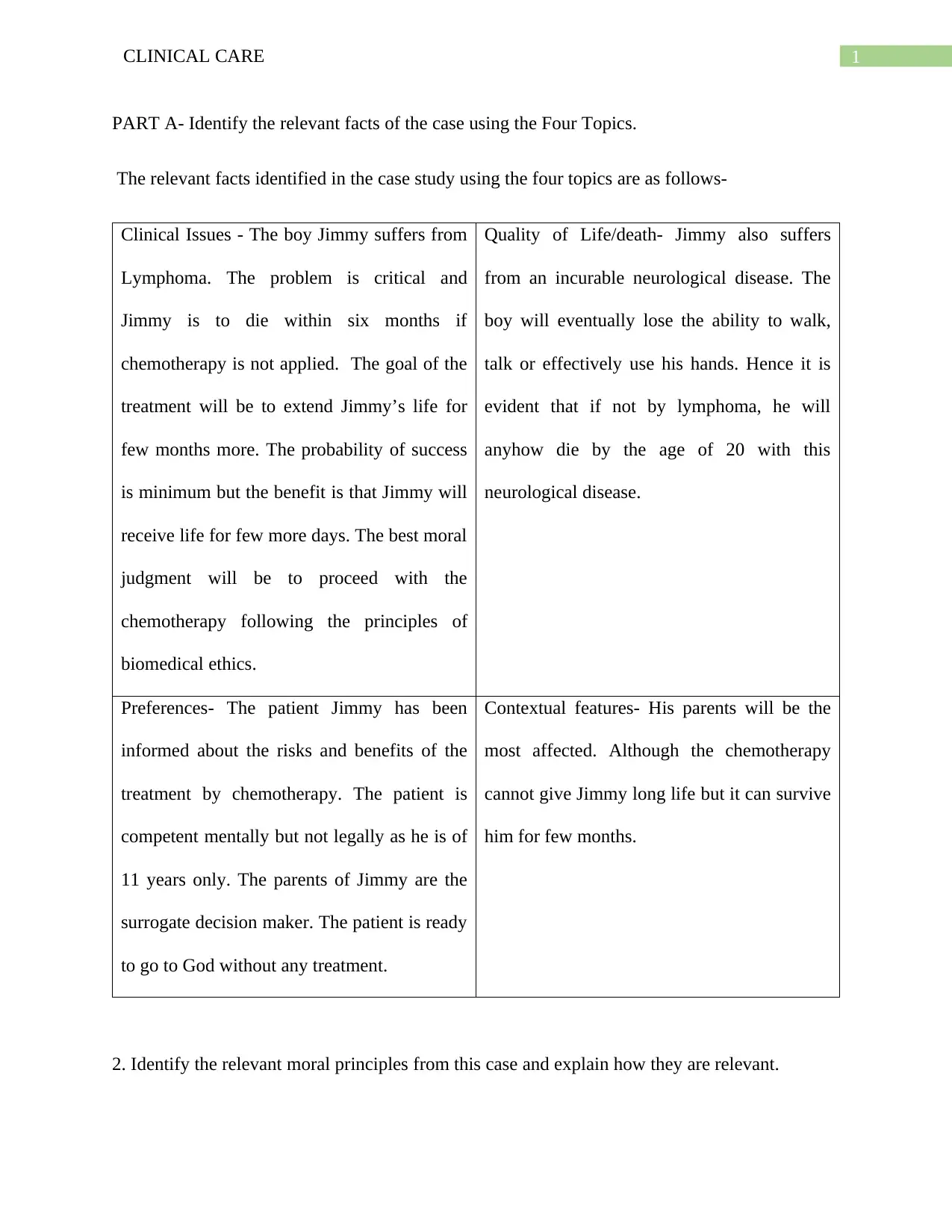
PART A- Identify the relevant facts of the case using the Four Topics.
The relevant facts identified in the case study using the four topics are as follows-
Clinical Issues - The boy Jimmy suffers from
Lymphoma. The problem is critical and
Jimmy is to die within six months if
chemotherapy is not applied. The goal of the
treatment will be to extend Jimmy’s life for
few months more. The probability of success
is minimum but the benefit is that Jimmy will
receive life for few more days. The best moral
judgment will be to proceed with the
chemotherapy following the principles of
biomedical ethics.
Quality of Life/death- Jimmy also suffers
from an incurable neurological disease. The
boy will eventually lose the ability to walk,
talk or effectively use his hands. Hence it is
evident that if not by lymphoma, he will
anyhow die by the age of 20 with this
neurological disease.
Preferences- The patient Jimmy has been
informed about the risks and benefits of the
treatment by chemotherapy. The patient is
competent mentally but not legally as he is of
11 years only. The parents of Jimmy are the
surrogate decision maker. The patient is ready
to go to God without any treatment.
Contextual features- His parents will be the
most affected. Although the chemotherapy
cannot give Jimmy long life but it can survive
him for few months.
2. Identify the relevant moral principles from this case and explain how they are relevant.
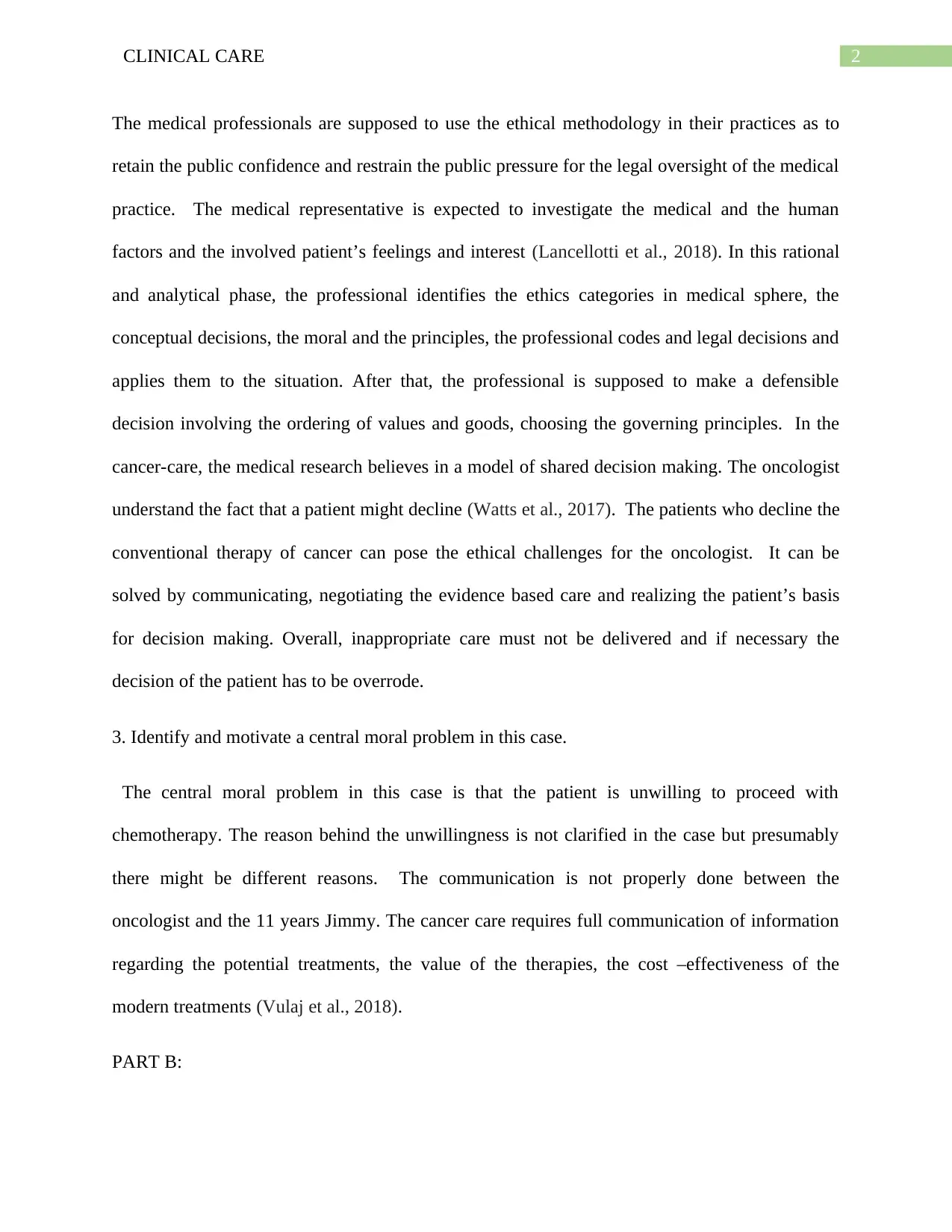
PART A- Identify the relevant facts of the case using the Four Topics.
The relevant facts identified in the case study using the four topics are as follows-
Clinical Issues - The boy Jimmy suffers from
Lymphoma. The problem is critical and
Jimmy is to die within six months if
chemotherapy is not applied. The goal of the
treatment will be to extend Jimmy’s life for
few months more. The probability of success
is minimum but the benefit is that Jimmy will
receive life for few more days. The best moral
judgment will be to proceed with the
chemotherapy following the principles of
biomedical ethics.
Quality of Life/death- Jimmy also suffers
from an incurable neurological disease. The
boy will eventually lose the ability to walk,
talk or effectively use his hands. Hence it is
evident that if not by lymphoma, he will
anyhow die by the age of 20 with this
neurological disease.
Preferences- The patient Jimmy has been
informed about the risks and benefits of the
treatment by chemotherapy. The patient is
competent mentally but not legally as he is of
11 years only. The parents of Jimmy are the
surrogate decision maker. The patient is ready
to go to God without any treatment.
Contextual features- His parents will be the
most affected. Although the chemotherapy
cannot give Jimmy long life but it can survive
him for few months.
2. Identify the relevant moral principles from this case and explain how they are relevant.
2CLINICAL CARE
The medical professionals are supposed to use the ethical methodology in their practices as to
retain the public confidence and restrain the public pressure for the legal oversight of the medical
practice. The medical representative is expected to investigate the medical and the human
factors and the involved patient’s feelings and interest (Lancellotti et al., 2018). In this rational
and analytical phase, the professional identifies the ethics categories in medical sphere, the
conceptual decisions, the moral and the principles, the professional codes and legal decisions and
applies them to the situation. After that, the professional is supposed to make a defensible
decision involving the ordering of values and goods, choosing the governing principles. In the
cancer-care, the medical research believes in a model of shared decision making. The oncologist
understand the fact that a patient might decline (Watts et al., 2017). The patients who decline the
conventional therapy of cancer can pose the ethical challenges for the oncologist. It can be
solved by communicating, negotiating the evidence based care and realizing the patient’s basis
for decision making. Overall, inappropriate care must not be delivered and if necessary the
decision of the patient has to be overrode.
3. Identify and motivate a central moral problem in this case.
The central moral problem in this case is that the patient is unwilling to proceed with
chemotherapy. The reason behind the unwillingness is not clarified in the case but presumably
there might be different reasons. The communication is not properly done between the
oncologist and the 11 years Jimmy. The cancer care requires full communication of information
regarding the potential treatments, the value of the therapies, the cost –effectiveness of the
modern treatments (Vulaj et al., 2018).
PART B:
The medical professionals are supposed to use the ethical methodology in their practices as to
retain the public confidence and restrain the public pressure for the legal oversight of the medical
practice. The medical representative is expected to investigate the medical and the human
factors and the involved patient’s feelings and interest (Lancellotti et al., 2018). In this rational
and analytical phase, the professional identifies the ethics categories in medical sphere, the
conceptual decisions, the moral and the principles, the professional codes and legal decisions and
applies them to the situation. After that, the professional is supposed to make a defensible
decision involving the ordering of values and goods, choosing the governing principles. In the
cancer-care, the medical research believes in a model of shared decision making. The oncologist
understand the fact that a patient might decline (Watts et al., 2017). The patients who decline the
conventional therapy of cancer can pose the ethical challenges for the oncologist. It can be
solved by communicating, negotiating the evidence based care and realizing the patient’s basis
for decision making. Overall, inappropriate care must not be delivered and if necessary the
decision of the patient has to be overrode.
3. Identify and motivate a central moral problem in this case.
The central moral problem in this case is that the patient is unwilling to proceed with
chemotherapy. The reason behind the unwillingness is not clarified in the case but presumably
there might be different reasons. The communication is not properly done between the
oncologist and the 11 years Jimmy. The cancer care requires full communication of information
regarding the potential treatments, the value of the therapies, the cost –effectiveness of the
modern treatments (Vulaj et al., 2018).
PART B:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CLINICAL CARE
The identified moral issue in the previous part is related to the lack of communication from the
part of the oncologist and the patient Jimmy. The moral values in the cancer care should be
perceived as the net benefit of the treatment. The benefits are in terms of the goals of the patient,
considering the expense of the treatment taking into account the negative effects of treatment. It
consists of communicating the value of treatment, the costs of forgoing other treatment along
with the potential alternative uses of the resources in health care. The definition of value in the
cancer care does not only requires complete oncologist-to-patient communication of information
regarding the potential treatments but also gives a responsibility for evaluating the value of
cancer therapies (Purdom, Petersen & Haas, 2017). There are some of the professional
responsibilities of the oncologists. They are at first the healers. The moral basis of the profession
can be found in the moral responsibilities of the physician to the sick person. The principle of
primacy of the patient’ welfare should be focused on by the oncologist. The role of the
oncologist is also to provide fair distribution of the clinical resources and communicate that to
the patient. The patient must know that his clinical care is based on the social justice along with a
cost-effective management (Watts et al., 2017). The oncologist should share his knowledge and
develop bond with the patient to know the understanding and values ad guide the appropriate
cancer care.
The potential treatment options of a patient should not only account for the clinical
situations they have but also consider the goals, personal and family resources, resilience,
perception towards the quality of life , the will to tolerate the after effects and adverse outcomes.
The oncologists usually deal with those patients nearing death like 11 years old Jimmy, but the
breaking of bad news makes the situation more complex. The best practice the oncologist in this
case study should adopt is proper communication with the patient having incurable cancer. Iy
The identified moral issue in the previous part is related to the lack of communication from the
part of the oncologist and the patient Jimmy. The moral values in the cancer care should be
perceived as the net benefit of the treatment. The benefits are in terms of the goals of the patient,
considering the expense of the treatment taking into account the negative effects of treatment. It
consists of communicating the value of treatment, the costs of forgoing other treatment along
with the potential alternative uses of the resources in health care. The definition of value in the
cancer care does not only requires complete oncologist-to-patient communication of information
regarding the potential treatments but also gives a responsibility for evaluating the value of
cancer therapies (Purdom, Petersen & Haas, 2017). There are some of the professional
responsibilities of the oncologists. They are at first the healers. The moral basis of the profession
can be found in the moral responsibilities of the physician to the sick person. The principle of
primacy of the patient’ welfare should be focused on by the oncologist. The role of the
oncologist is also to provide fair distribution of the clinical resources and communicate that to
the patient. The patient must know that his clinical care is based on the social justice along with a
cost-effective management (Watts et al., 2017). The oncologist should share his knowledge and
develop bond with the patient to know the understanding and values ad guide the appropriate
cancer care.
The potential treatment options of a patient should not only account for the clinical
situations they have but also consider the goals, personal and family resources, resilience,
perception towards the quality of life , the will to tolerate the after effects and adverse outcomes.
The oncologists usually deal with those patients nearing death like 11 years old Jimmy, but the
breaking of bad news makes the situation more complex. The best practice the oncologist in this
case study should adopt is proper communication with the patient having incurable cancer. Iy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CLINICAL CARE
includes the addressing of emotional impacts of a long lasting illness, the challenges of
sustaining the hope within and aspiration towards the realistic goals.
The oncologists are trained to measure the condition of the patient who assist the patient
in choosing between the evidence-based and available options for maximizing the quality of life
and health. There are many situations which arise requiring the clinicians to confront the various
choices associated with communication, goals of care, resource utilization and other factors too.
The primary concern of medical ethics is to evaluate the right path in such situations (Neuman et
al., 2016). Having identified the principles which are at stake, providing moral justification after
evaluating the relative obligations it can be possible. The cost factor in the health care become a
major concern in the United States and internationally too. In the international contexts, the
health care consumes a large portion of their budget and develop at an unsustainable rate. In the
cancer care almost 5 % of the total healthcare is consumed which is characterized by expensive
medication (Klemp et al., 2018). In the cost of the cancer care, there are many factors
contributing and among them, that is the failure of the oncologist in communicating with the
patient realistically. Due to this failure, most of the patient decline from the delivery of care.
Although the 11 years old Jimmy is legally incompetent and call of his decisions are to be
taken by his parents who want the chemotherapy to get started, it is the ethical rule to have the
patient’ consent first. The importance of the informed –consent in medication is huge. As per
this consent, the patient is informed properly about the disease, the risks, benefits of treatment,
the cost effectiveness of the treatment and other options of treatment. The oncologist should be
aware that surveys have found that patients expect and appreciate open discussions regarding
goals of care and prognosis (Gori et al., 2016). They further know that during such
conversations, care that is delivered must be changed giving more emphasis on palliative care.
includes the addressing of emotional impacts of a long lasting illness, the challenges of
sustaining the hope within and aspiration towards the realistic goals.
The oncologists are trained to measure the condition of the patient who assist the patient
in choosing between the evidence-based and available options for maximizing the quality of life
and health. There are many situations which arise requiring the clinicians to confront the various
choices associated with communication, goals of care, resource utilization and other factors too.
The primary concern of medical ethics is to evaluate the right path in such situations (Neuman et
al., 2016). Having identified the principles which are at stake, providing moral justification after
evaluating the relative obligations it can be possible. The cost factor in the health care become a
major concern in the United States and internationally too. In the international contexts, the
health care consumes a large portion of their budget and develop at an unsustainable rate. In the
cancer care almost 5 % of the total healthcare is consumed which is characterized by expensive
medication (Klemp et al., 2018). In the cost of the cancer care, there are many factors
contributing and among them, that is the failure of the oncologist in communicating with the
patient realistically. Due to this failure, most of the patient decline from the delivery of care.
Although the 11 years old Jimmy is legally incompetent and call of his decisions are to be
taken by his parents who want the chemotherapy to get started, it is the ethical rule to have the
patient’ consent first. The importance of the informed –consent in medication is huge. As per
this consent, the patient is informed properly about the disease, the risks, benefits of treatment,
the cost effectiveness of the treatment and other options of treatment. The oncologist should be
aware that surveys have found that patients expect and appreciate open discussions regarding
goals of care and prognosis (Gori et al., 2016). They further know that during such
conversations, care that is delivered must be changed giving more emphasis on palliative care.
5CLINICAL CARE
When the realistic discussion becomes difficult, options should be discussed with the patient and
the family members. There has to be a realistic presentation of the best and worst case scenarios,
the harm and benefits of any type of intervention. Additionally, an emphasis on the continued
care will help in avoiding the dichotomy between withdrawing care and aggressive care. It helps
the patients to take strong decisions and increases the optimism and confidence level too
(Yilmaz, 2017). It also creates trust between the doctor and the patient and reduces the risk of the
patient and the doctor. Hence, excellent communication should be developed and makes the
work easy for them.
When the realistic discussion becomes difficult, options should be discussed with the patient and
the family members. There has to be a realistic presentation of the best and worst case scenarios,
the harm and benefits of any type of intervention. Additionally, an emphasis on the continued
care will help in avoiding the dichotomy between withdrawing care and aggressive care. It helps
the patients to take strong decisions and increases the optimism and confidence level too
(Yilmaz, 2017). It also creates trust between the doctor and the patient and reduces the risk of the
patient and the doctor. Hence, excellent communication should be developed and makes the
work easy for them.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CLINICAL CARE
Bibliography
Gori, S., Pinto, C., Caminiti, C., Aprile, G., Marchetti, P., Perrone, F., ... & Di Costanzo, F.
(2016). Ethics in oncology: principles and responsibilities declared in the Italian Ragusa
statement.
Klemp, J. R., Lowry, B. N., Johnston, J. A., Alsman, K., Peereboom, D., Long, T., ... & Greiner,
A. (2018). Delivery of survivorship care from rural primary care and oncology practices.
Lancellotti, P., Suter, T. M., López-Fernández, T., Galderisi, M., Lyon, A. R., Van der Meer,
P., ... & Aboyans, V. (2018). Cardio-Oncology Services: rationale, organization, and
implementation: A report from the ESC Cardio-Oncology council. European heart
journal, 40(22), 1756-1763.
Neuman, H. B., Steffens, N. M., Jacobson, N., Tevaarwerk, A., Anderson, B., Wilke, L. G., &
Greenberg, C. C. (2016). Oncologists’ perspectives of their roles and responsibilities
during multi-disciplinary breast cancer follow-up. Annals of surgical oncology, 23(3),
708-714.
Purdom, M. A., Petersen, S., & Haas, B. K. (2017, September). Results of an Oncology Clinical
Trial Nurse Role Delineation Study. In Oncology nursing forum (Vol. 44, No. 5).
Vulaj, V., Hough, S., Bedard, L., Farris, K., & Mackler, E. (2018). Oncology pharmacist
opportunities: Closing the gap in quality care. Journal of oncology practice, 14(6), e403-
e411.
Watts, K. J., Meiser, B., Zilliacus, E., Kaur, R., Taouk, M., Girgis, A., ... & Aranda, S. K. (2017).
Communicating with patients from minority backgrounds: Individual challenges
Bibliography
Gori, S., Pinto, C., Caminiti, C., Aprile, G., Marchetti, P., Perrone, F., ... & Di Costanzo, F.
(2016). Ethics in oncology: principles and responsibilities declared in the Italian Ragusa
statement.
Klemp, J. R., Lowry, B. N., Johnston, J. A., Alsman, K., Peereboom, D., Long, T., ... & Greiner,
A. (2018). Delivery of survivorship care from rural primary care and oncology practices.
Lancellotti, P., Suter, T. M., López-Fernández, T., Galderisi, M., Lyon, A. R., Van der Meer,
P., ... & Aboyans, V. (2018). Cardio-Oncology Services: rationale, organization, and
implementation: A report from the ESC Cardio-Oncology council. European heart
journal, 40(22), 1756-1763.
Neuman, H. B., Steffens, N. M., Jacobson, N., Tevaarwerk, A., Anderson, B., Wilke, L. G., &
Greenberg, C. C. (2016). Oncologists’ perspectives of their roles and responsibilities
during multi-disciplinary breast cancer follow-up. Annals of surgical oncology, 23(3),
708-714.
Purdom, M. A., Petersen, S., & Haas, B. K. (2017, September). Results of an Oncology Clinical
Trial Nurse Role Delineation Study. In Oncology nursing forum (Vol. 44, No. 5).
Vulaj, V., Hough, S., Bedard, L., Farris, K., & Mackler, E. (2018). Oncology pharmacist
opportunities: Closing the gap in quality care. Journal of oncology practice, 14(6), e403-
e411.
Watts, K. J., Meiser, B., Zilliacus, E., Kaur, R., Taouk, M., Girgis, A., ... & Aranda, S. K. (2017).
Communicating with patients from minority backgrounds: Individual challenges
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CLINICAL CARE
experienced by oncology health professionals. European Journal of Oncology
Nursing, 26, 83-90.
Yilmaz, M. (2017). Pediatric Oncology Nursing in Childhood Cancer.
experienced by oncology health professionals. European Journal of Oncology
Nursing, 26, 83-90.
Yilmaz, M. (2017). Pediatric Oncology Nursing in Childhood Cancer.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





