LBP Sensory System, NSAIDs: Mechanisms and Treatment of Chronic Pain
VerifiedAdded on 2020/02/24
|5
|978
|59
Report
AI Summary
This report delves into the physiology of Low Back Pain (LBP), examining the LBP sensory system and the role of nociceptors in mediating pain sensation. It explains how nociceptors transmit pain signals to the brain and how chronic stress can lead to peripheral and central sensitization, converting acute pain into chronic pain. The report then focuses on the pharmacological actions of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), commonly used to treat musculoskeletal pain. It details the mechanism of action of NSAIDs, particularly their inhibition of cyclooxygenase (COX) enzymes, especially COX-2, to reduce the production of inflammatory prostaglandins. The report highlights the therapeutic effects of NSAIDs in managing chronic LBP by interrupting the pain pathway. The report is based on the provided references which support the information presented.
LBP
Sensory system
Physiology of LBP
Low back pain (LBP) is one of the most common musculo-skeletal conditions that
affect 84% of adult (Balague, 2012). In chronic LBP, the pain in the low back (lumbar)
lasts for 3 months as Sue (Mostagi, 2015). Nociceptors are the specialized peripheral-
sensorial form of neurons, which mediates pain sensation and provoke Sue to the
potential stimuli (compression in lumbar-segment) in her skin. This occurs by
transduction of the damaging- stimuli into the form of electrical signals, which were then
transmitted (relayed) up to the higher centers of brain (Douglas, 2012).
Nociceptors are the receptors that consist of pseudo-form unipolar-primary
somato-sensory neurons having their neuronal bodies that are located in the DRG
(dorsal-root ganglion) (Allegri, 2016). These are bifurcated axons; peripheral-nerve
branch innervates skin (causes acute tenderness in Sue) while the central-nerve branch
synapses with 2nd-order neurons that are located in the spinal cords dorsal horn which
transmits pain to the mesencephalon & thalamus, then to somato-sensory & anterior-
form cingulated-cortex so as to enable discrimination between sensorial and affective-
cognitive pain features respectively (Dubin, 2010).
As the irritating stimulus of chronic stress persists in Sue, the peripheral as well
as central sensitization occurs that converts acute to chronic pain with central
protrusions. This central sensitization increases the excitability of CNS neurons that
transforms normal inputs into abnormal responses causing acute tenderness in Sue
(Allegri, 2016, Nijs, 2014). Minor alterations in posture, chronic stress with rich
1
Sensory system
Physiology of LBP
Low back pain (LBP) is one of the most common musculo-skeletal conditions that
affect 84% of adult (Balague, 2012). In chronic LBP, the pain in the low back (lumbar)
lasts for 3 months as Sue (Mostagi, 2015). Nociceptors are the specialized peripheral-
sensorial form of neurons, which mediates pain sensation and provoke Sue to the
potential stimuli (compression in lumbar-segment) in her skin. This occurs by
transduction of the damaging- stimuli into the form of electrical signals, which were then
transmitted (relayed) up to the higher centers of brain (Douglas, 2012).
Nociceptors are the receptors that consist of pseudo-form unipolar-primary
somato-sensory neurons having their neuronal bodies that are located in the DRG
(dorsal-root ganglion) (Allegri, 2016). These are bifurcated axons; peripheral-nerve
branch innervates skin (causes acute tenderness in Sue) while the central-nerve branch
synapses with 2nd-order neurons that are located in the spinal cords dorsal horn which
transmits pain to the mesencephalon & thalamus, then to somato-sensory & anterior-
form cingulated-cortex so as to enable discrimination between sensorial and affective-
cognitive pain features respectively (Dubin, 2010).
As the irritating stimulus of chronic stress persists in Sue, the peripheral as well
as central sensitization occurs that converts acute to chronic pain with central
protrusions. This central sensitization increases the excitability of CNS neurons that
transforms normal inputs into abnormal responses causing acute tenderness in Sue
(Allegri, 2016, Nijs, 2014). Minor alterations in posture, chronic stress with rich
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LBP
innervations of A-delta nerve-fibers in the bones, ligaments, vertebral- discs, and
vertebral- bones result in chronification of LBP in Sue (Allegri, 2016).
Pharmacological actions of NSAIDS
NSAIDs are commonly used to treat pain in musculoskeletal problems (Lewis,
2013). Sue’s history suggests that she has long-term LBP along with stiffness, acute-
tenderness and protrusions in lower-back (L3- L4). NSAIDs are used as the front-line
agents for pain relief because of their rapid action with increased drug tolerance which
is needed in Sue’s condition (Yacobi, 2013). NSAIDS exert its therapeutic-actions both
locally at peripheral-inflammatory areas as well as centrally by inhibiting the synthesis
and release of prostaglandins; although there is an effect on leukotriene production.
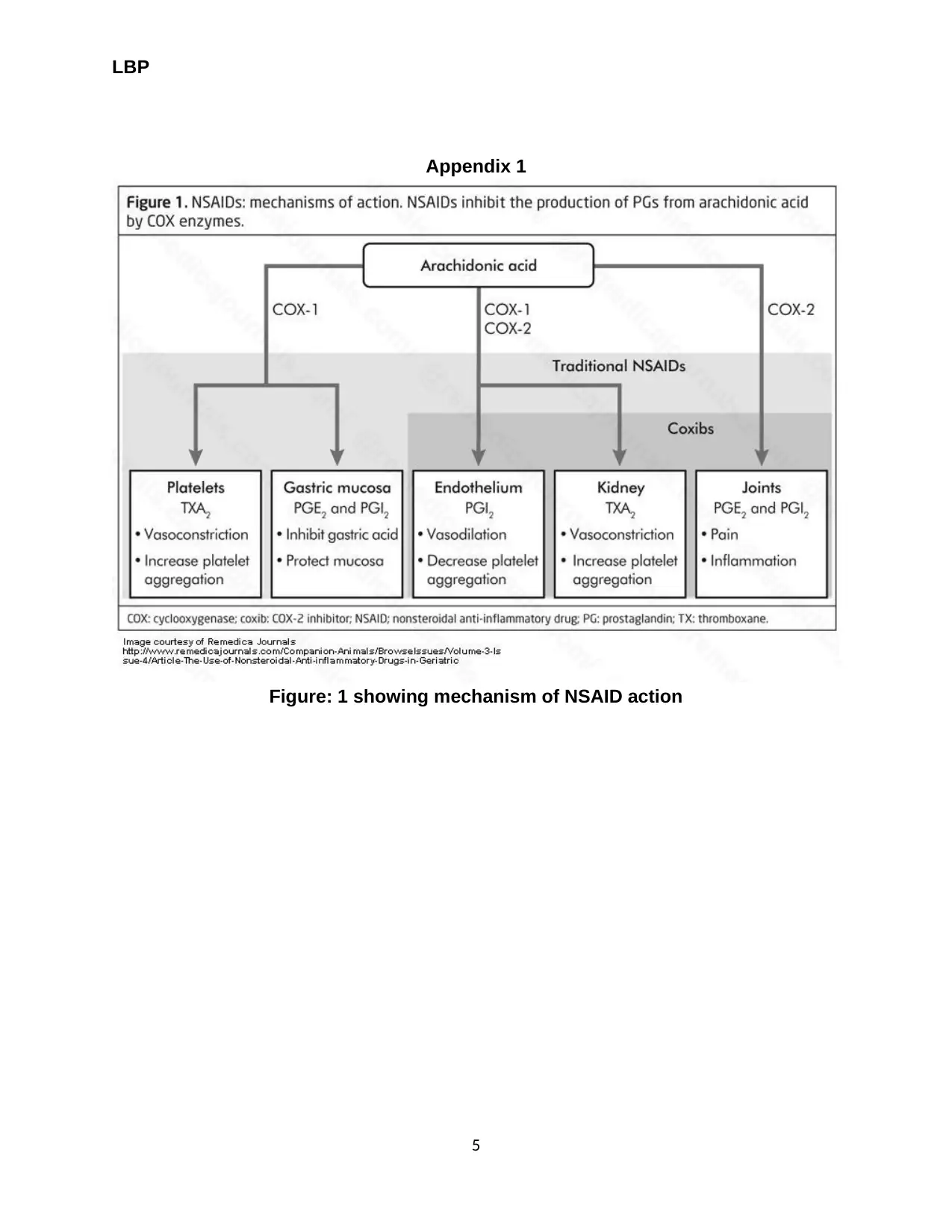
The principal mode of action of NSAIDs is at the molecular level comprising of
the inhibition of cyclooxygenase (COX) which is an enzyme that takes part in the
arachidonic-acid cascade that synthesizes inflammatory- mediators of the
prostaglandins. COX has 2 iso-forms as COX-1 and COX-2 in which COX-2 is better in
its actions than COX-1 (Fig: 1) (Kuritzky, 2012). In Sue, the therapeutic-effects of
NSAIDs occurs because of the therapeutic inhibition of COX-2 (Yacobi, 2013).
COX-2 is the principle pathway along which the conversion of arachidonic- acid
into inflammatory prostaglandins takes place in Sue (that produces pain). Therefore,
interrupting this pathway; an action that is common in all NSAIDs (aspirin) is the basis
for relief of pain in Sue (Kuritzky, 2012). COX-2 is commonly accepted as an ‘inducible
enzyme’, i.e., COX-2 is inactive when the stimuli (as inflammation) are absent. Hence,
NSAIDS are used at a low dose and at short- time for pain relief in Sue with chronic
LBP.
2
innervations of A-delta nerve-fibers in the bones, ligaments, vertebral- discs, and
vertebral- bones result in chronification of LBP in Sue (Allegri, 2016).
Pharmacological actions of NSAIDS
NSAIDs are commonly used to treat pain in musculoskeletal problems (Lewis,
2013). Sue’s history suggests that she has long-term LBP along with stiffness, acute-
tenderness and protrusions in lower-back (L3- L4). NSAIDs are used as the front-line
agents for pain relief because of their rapid action with increased drug tolerance which
is needed in Sue’s condition (Yacobi, 2013). NSAIDS exert its therapeutic-actions both
locally at peripheral-inflammatory areas as well as centrally by inhibiting the synthesis
and release of prostaglandins; although there is an effect on leukotriene production.
The principal mode of action of NSAIDs is at the molecular level comprising of
the inhibition of cyclooxygenase (COX) which is an enzyme that takes part in the
arachidonic-acid cascade that synthesizes inflammatory- mediators of the
prostaglandins. COX has 2 iso-forms as COX-1 and COX-2 in which COX-2 is better in
its actions than COX-1 (Fig: 1) (Kuritzky, 2012). In Sue, the therapeutic-effects of
NSAIDs occurs because of the therapeutic inhibition of COX-2 (Yacobi, 2013).
COX-2 is the principle pathway along which the conversion of arachidonic- acid
into inflammatory prostaglandins takes place in Sue (that produces pain). Therefore,
interrupting this pathway; an action that is common in all NSAIDs (aspirin) is the basis
for relief of pain in Sue (Kuritzky, 2012). COX-2 is commonly accepted as an ‘inducible
enzyme’, i.e., COX-2 is inactive when the stimuli (as inflammation) are absent. Hence,
NSAIDS are used at a low dose and at short- time for pain relief in Sue with chronic
LBP.
2
LBP
Reference
Allegri, M., Montella, S., Salici, F., Valente, A., Marchesini, M., Compagnone, C.,…
Fanelli, G. (2016). Mechanisms of low back pain: a guide for diagnosis and
therapy. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC4926733/#ref-1
Balague, F., Mannion, A.F., & Pellise, F. (2012). Non-specific low back pain. Lancet,
(9814), 482–91. doi. 10.1016/S0140-6736(11)60610-7
Douglas, C. (2012). Potter and Perry’s Fundamentals of Nursing- Australian version. (4th
edition). Elsevier: St. Louis, Missouri
Dubin, A.E. (2010). Patapoutian A: Nociceptors: the sensors of the pain pathway. J Clin
Invest, 120(11), 3760–72. doi. 10.1172/JCI42843
Kuritzky, L., & Samraj, G. P. (2012). Nonsteroidal anti-inflammatory drugs in the
treatment of low back pain. J Pain Res, 5. 579–590. doi: 10.2147/JPR.S6775
Lewis, S.M., Heitkemper, M. M., & Dirksen, S.R. (2013). Medical Surgical Nursing:
Assessment and Management of Clinical Problems. (9th ed.). Missouri: Mosby.
Mostagi, F.Q., Dias, J.M., & Pereira, L.M. (2015). Pilates versus general exercise
effectiveness on pain and functionality in non-specific chronic low back pain
subjects. J Bodyw Mov Ther, 19(4), 636–45. doi. 10.1016/j.jbmt.2014.11.009
3
Reference
Allegri, M., Montella, S., Salici, F., Valente, A., Marchesini, M., Compagnone, C.,…
Fanelli, G. (2016). Mechanisms of low back pain: a guide for diagnosis and
therapy. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC4926733/#ref-1
Balague, F., Mannion, A.F., & Pellise, F. (2012). Non-specific low back pain. Lancet,
(9814), 482–91. doi. 10.1016/S0140-6736(11)60610-7
Douglas, C. (2012). Potter and Perry’s Fundamentals of Nursing- Australian version. (4th
edition). Elsevier: St. Louis, Missouri
Dubin, A.E. (2010). Patapoutian A: Nociceptors: the sensors of the pain pathway. J Clin
Invest, 120(11), 3760–72. doi. 10.1172/JCI42843
Kuritzky, L., & Samraj, G. P. (2012). Nonsteroidal anti-inflammatory drugs in the
treatment of low back pain. J Pain Res, 5. 579–590. doi: 10.2147/JPR.S6775
Lewis, S.M., Heitkemper, M. M., & Dirksen, S.R. (2013). Medical Surgical Nursing:
Assessment and Management of Clinical Problems. (9th ed.). Missouri: Mosby.
Mostagi, F.Q., Dias, J.M., & Pereira, L.M. (2015). Pilates versus general exercise
effectiveness on pain and functionality in non-specific chronic low back pain
subjects. J Bodyw Mov Ther, 19(4), 636–45. doi. 10.1016/j.jbmt.2014.11.009
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LBP
Nijs, J., Malfliet, A., & Ickmans, K. (2014). Treatment of central sensitization in patients
with 'unexplained' chronic pain: an update. Expert Opin Pharmacother, 15(12),
1671–83. doi. 10.1517/14656566.2014.925446
Yacobi, A. (2013). Integration of Pharmacokinetics, Pharmacodynamics, and ..effects of
NSAIDS, 193, Retrieved from https://books.google.co.in/books?isbn
=147571520X
4
Nijs, J., Malfliet, A., & Ickmans, K. (2014). Treatment of central sensitization in patients
with 'unexplained' chronic pain: an update. Expert Opin Pharmacother, 15(12),
1671–83. doi. 10.1517/14656566.2014.925446
Yacobi, A. (2013). Integration of Pharmacokinetics, Pharmacodynamics, and ..effects of
NSAIDS, 193, Retrieved from https://books.google.co.in/books?isbn
=147571520X
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LBP
Appendix 1
Figure: 1 showing mechanism of NSAID action
5
Appendix 1
Figure: 1 showing mechanism of NSAID action
5
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





