La Trobe University: Leadership in Nursing, Clinical Governance Report
VerifiedAdded on 2021/04/17
|20
|4560
|402
Report
AI Summary
This report delves into the critical aspects of leadership in nursing, emphasizing clinical governance, consumer participation, and professional practice. It examines the importance of clinical governance in maintaining high-quality and safe patient care, highlighting strategies to increase consumer involvement through surveys and staff training. The report discusses the National Safety and Quality Health Service Standards, focusing on governance for safety and quality. It identifies evidence-based leadership skills, such as transformational leadership and inter-professional teamwork, and strategies to achieve them through education and training. The analysis extends to organizational culture, exploring characteristics of a learning culture and strategies to foster it, such as education and feedback. The report concludes with a discussion of professional practice for registered nurses, including self-care strategies, to ensure holistic patient care and continuous improvement in healthcare settings. The report uses the Leadership Skills Inventory to analyze the leadership skills and identify areas for professional development.

Running head: Leadership in Nursing
LEADERSHIP in NURSING
Name of the Student
Name of the University
Author Note
LEADERSHIP in NURSING
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Leadership in Nursing
Contents
Introduction................................................................................................................................2
Clinical Governance...................................................................................................................2
-consumer governance strategies...........................................................................................2
- Strategies to increase consumer participation......................................................................3
Safety and Quality......................................................................................................................4
-One standard from NSQHSS:...............................................................................................4
- Strategy to maintain safety and quality................................................................................4
Leadership and Management.....................................................................................................6
- Two evidence-based leadership skills for RN.....................................................................6
Strategies to achieve the skills-..............................................................................................7
Organizational Culture...............................................................................................................8
-Characteristics of Learning Culture:.....................................................................................8
Two of the evidence-based strategies....................................................................................8
Professional Practice..................................................................................................................9
-Professional Practice for Registered Nurses.........................................................................9
-Self-care strategies..............................................................................................................11
References:...............................................................................................................................13
Appendix:.................................................................................................................................19
Contents
Introduction................................................................................................................................2
Clinical Governance...................................................................................................................2
-consumer governance strategies...........................................................................................2
- Strategies to increase consumer participation......................................................................3
Safety and Quality......................................................................................................................4
-One standard from NSQHSS:...............................................................................................4
- Strategy to maintain safety and quality................................................................................4
Leadership and Management.....................................................................................................6
- Two evidence-based leadership skills for RN.....................................................................6
Strategies to achieve the skills-..............................................................................................7
Organizational Culture...............................................................................................................8
-Characteristics of Learning Culture:.....................................................................................8
Two of the evidence-based strategies....................................................................................8
Professional Practice..................................................................................................................9
-Professional Practice for Registered Nurses.........................................................................9
-Self-care strategies..............................................................................................................11
References:...............................................................................................................................13
Appendix:.................................................................................................................................19
2Leadership in Nursing
Introduction
Leadership and clinical governance are important attributes in any healthcare
organisation, as it helps in the maintenance of high quality and safe care accessible to the
people (rcn.org.uk, 2018). Also, consumer participation in the process of healthcare
transformation can also incorporate accountability and development of patient-centered care
(Mendes & Roseman, 2013). Through clinical governance, an environment of quality and
safety can be maintained as well as foster the development of a learning culture (Phillips et
al., 2017). Skills necessary for such policies can be extensively developed through health
education and leadership. Analysis of my leadership skills was done using the ‘Leadership
Skills Inventory’ from Leadership Theory and Practice (6th Ed) (Northhouse, 2013). The
essay discusses the various factors that contribute to strong leadership and clinical
governance skills, and how such skills can be developed to create an environment of
excellence and competence.
Clinical Governance
Clinical governance can be understood as an ‘umbrella term’ that includes activities
that allows the development and maintenance of high quality care for the patients. Through
clinical governance, the healthcare organizations are able to continuously improve and
maintain high quality care by fostering the development of an environment of excellence
and competence (rcn.org.uk, 2018). Clinical governance revolves around 5 key themes:
focus on patient, focus on information, improvement in quality, focus on staff and
leadership (rcn.org.uk, 2018).
-consumer governance strategies
Introduction
Leadership and clinical governance are important attributes in any healthcare
organisation, as it helps in the maintenance of high quality and safe care accessible to the
people (rcn.org.uk, 2018). Also, consumer participation in the process of healthcare
transformation can also incorporate accountability and development of patient-centered care
(Mendes & Roseman, 2013). Through clinical governance, an environment of quality and
safety can be maintained as well as foster the development of a learning culture (Phillips et
al., 2017). Skills necessary for such policies can be extensively developed through health
education and leadership. Analysis of my leadership skills was done using the ‘Leadership
Skills Inventory’ from Leadership Theory and Practice (6th Ed) (Northhouse, 2013). The
essay discusses the various factors that contribute to strong leadership and clinical
governance skills, and how such skills can be developed to create an environment of
excellence and competence.
Clinical Governance
Clinical governance can be understood as an ‘umbrella term’ that includes activities
that allows the development and maintenance of high quality care for the patients. Through
clinical governance, the healthcare organizations are able to continuously improve and
maintain high quality care by fostering the development of an environment of excellence
and competence (rcn.org.uk, 2018). Clinical governance revolves around 5 key themes:
focus on patient, focus on information, improvement in quality, focus on staff and
leadership (rcn.org.uk, 2018).
-consumer governance strategies
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Leadership in Nursing
Involvement of the consumer is an important strategy to foster improvement in the
quality of healthcare, as well as for improving the effectiveness of service, maintaining
accountability of the organization and empower customers who might be disadvantaged
(Countyhealthrankings.org, 2018; Mendes & Roseman, 2013). Consumer participation can
occur at different levels like Consumer, Program Level, and Organizational level.
Different strategies that can be used to involve customer participation includes the usage of
narratives, surveys, focus groups, rapid improvement events, outreach activities, co-
design, evaluation processes, staff training, staff recruitment, formal committees, and
reporting (healthissuescentre.org.au, 2018). Two strategies that can be selected from these
are the usage of customer/ consumer/ patient surveys and training of the staff to support
the development of a close cooperation between patient and healthcare team, and reinforce
their capacity of self care as well as helping the nurses to understand the patients better
(Sahlsten et al., 2018).
- Strategies to increase consumer participation
Coultier (2016) suggested that patient feedback can be useful in the improvement of
healthcare quality. Feedback from patients can be collected through surveys which allow
patients to share their views through interviews, feedbacks or reports. Boiko et al. (2015) also
supported such a view as their studies showed that feedback from patient experience surveys
creates a therapeutic approach towards getting the concerns of the patients being heard by the
staff, identify areas of improvement and can be used as an evidence for professional
development and appraisal.
Nurses play an important role in the improvement of patient participation by
acknowledging as well as facilitating patient participation in nursing activities. However, the
need to incorporate safety for each participant and proper assessment of risks can complicate
Involvement of the consumer is an important strategy to foster improvement in the
quality of healthcare, as well as for improving the effectiveness of service, maintaining
accountability of the organization and empower customers who might be disadvantaged
(Countyhealthrankings.org, 2018; Mendes & Roseman, 2013). Consumer participation can
occur at different levels like Consumer, Program Level, and Organizational level.
Different strategies that can be used to involve customer participation includes the usage of
narratives, surveys, focus groups, rapid improvement events, outreach activities, co-
design, evaluation processes, staff training, staff recruitment, formal committees, and
reporting (healthissuescentre.org.au, 2018). Two strategies that can be selected from these
are the usage of customer/ consumer/ patient surveys and training of the staff to support
the development of a close cooperation between patient and healthcare team, and reinforce
their capacity of self care as well as helping the nurses to understand the patients better
(Sahlsten et al., 2018).
- Strategies to increase consumer participation
Coultier (2016) suggested that patient feedback can be useful in the improvement of
healthcare quality. Feedback from patients can be collected through surveys which allow
patients to share their views through interviews, feedbacks or reports. Boiko et al. (2015) also
supported such a view as their studies showed that feedback from patient experience surveys
creates a therapeutic approach towards getting the concerns of the patients being heard by the
staff, identify areas of improvement and can be used as an evidence for professional
development and appraisal.
Nurses play an important role in the improvement of patient participation by
acknowledging as well as facilitating patient participation in nursing activities. However, the
need to incorporate safety for each participant and proper assessment of risks can complicate
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Leadership in Nursing
the role of the nurse in the process. Training of the nurses and healthcare staff can improve
their skills and competencies to maintain and improve patient participation (Tobiano et al.,
2015). As a registered nurse, the future practice may include taking patient feedback and
indulging in training activities to further improve consumer participation.
Safety and Quality
-One standard from NSQHSS:
The National Safety and Quality Health Services Standards include several standards
that are incorporated in the second edition of NSHQS standards. One of the important
standards among the seven standards is “Governance for safety and quality in health service
organisation” (Safetyandquality.gov.au, 2018).
The importance of clinical governance in the maintenance of safety and quality of
healthcare will be discussed next.
There are certain risks related clinical governance standard for the maintenance of the
health and safety quality in the health service organisations which included breaching of the
clinical standards, malpractices, appalling standards of care regarding infection, control,
medication errors (Safetyandquality.gov.au, 2018).
- Strategy to maintain safety and quality
Phillips et al has proposed the conceptual model for clinical governance., (2017). This
model is shown in the diagram below:
the role of the nurse in the process. Training of the nurses and healthcare staff can improve
their skills and competencies to maintain and improve patient participation (Tobiano et al.,
2015). As a registered nurse, the future practice may include taking patient feedback and
indulging in training activities to further improve consumer participation.
Safety and Quality
-One standard from NSQHSS:
The National Safety and Quality Health Services Standards include several standards
that are incorporated in the second edition of NSHQS standards. One of the important
standards among the seven standards is “Governance for safety and quality in health service
organisation” (Safetyandquality.gov.au, 2018).
The importance of clinical governance in the maintenance of safety and quality of
healthcare will be discussed next.
There are certain risks related clinical governance standard for the maintenance of the
health and safety quality in the health service organisations which included breaching of the
clinical standards, malpractices, appalling standards of care regarding infection, control,
medication errors (Safetyandquality.gov.au, 2018).
- Strategy to maintain safety and quality
Phillips et al has proposed the conceptual model for clinical governance., (2017). This
model is shown in the diagram below:
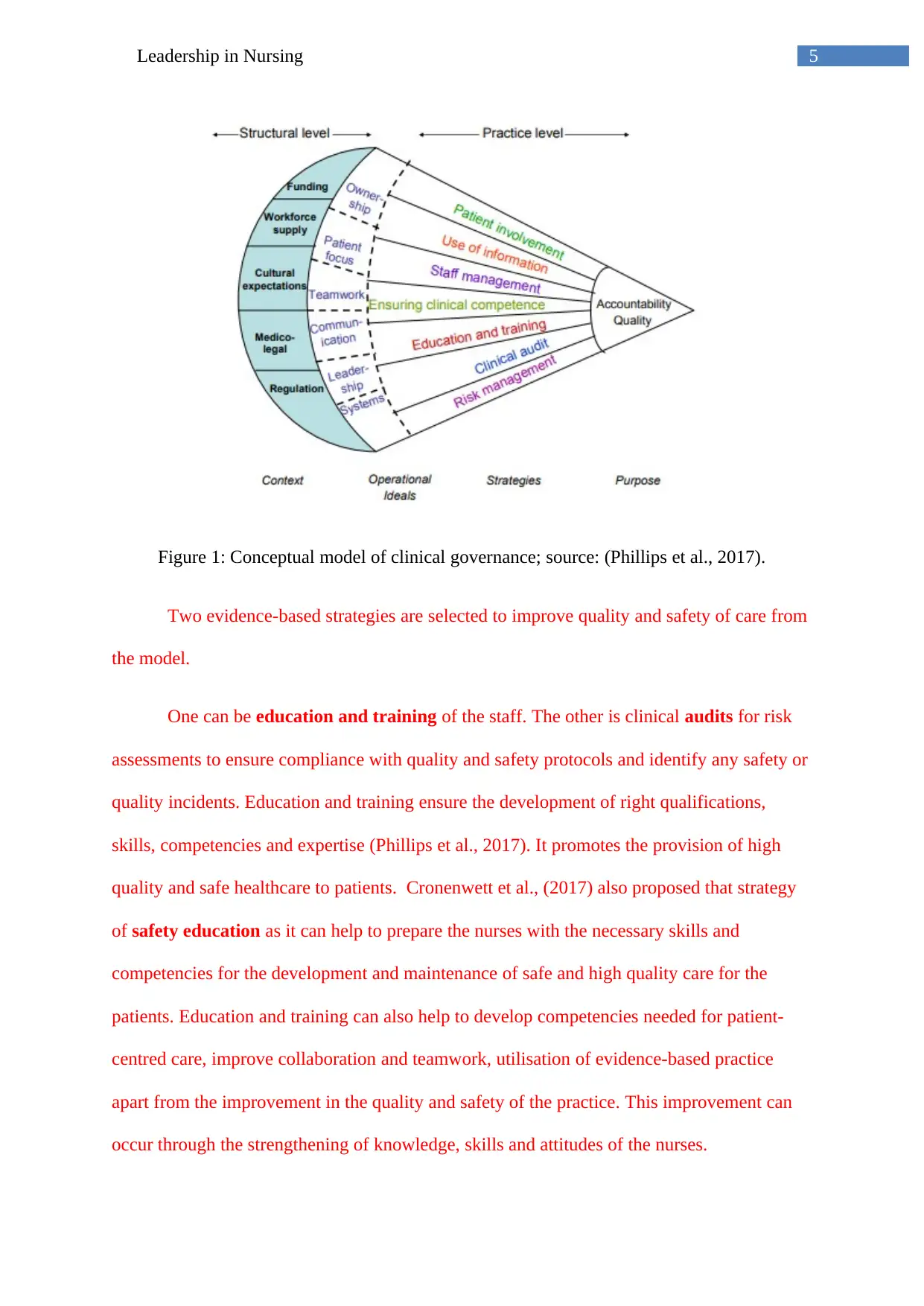
5Leadership in Nursing
Figure 1: Conceptual model of clinical governance; source: (Phillips et al., 2017).
Two evidence-based strategies are selected to improve quality and safety of care from
the model.
One can be education and training of the staff. The other is clinical audits for risk
assessments to ensure compliance with quality and safety protocols and identify any safety or
quality incidents. Education and training ensure the development of right qualifications,
skills, competencies and expertise (Phillips et al., 2017). It promotes the provision of high
quality and safe healthcare to patients. Cronenwett et al., (2017) also proposed that strategy
of safety education as it can help to prepare the nurses with the necessary skills and
competencies for the development and maintenance of safe and high quality care for the
patients. Education and training can also help to develop competencies needed for patient-
centred care, improve collaboration and teamwork, utilisation of evidence-based practice
apart from the improvement in the quality and safety of the practice. This improvement can
occur through the strengthening of knowledge, skills and attitudes of the nurses.
Figure 1: Conceptual model of clinical governance; source: (Phillips et al., 2017).
Two evidence-based strategies are selected to improve quality and safety of care from
the model.
One can be education and training of the staff. The other is clinical audits for risk
assessments to ensure compliance with quality and safety protocols and identify any safety or
quality incidents. Education and training ensure the development of right qualifications,
skills, competencies and expertise (Phillips et al., 2017). It promotes the provision of high
quality and safe healthcare to patients. Cronenwett et al., (2017) also proposed that strategy
of safety education as it can help to prepare the nurses with the necessary skills and
competencies for the development and maintenance of safe and high quality care for the
patients. Education and training can also help to develop competencies needed for patient-
centred care, improve collaboration and teamwork, utilisation of evidence-based practice
apart from the improvement in the quality and safety of the practice. This improvement can
occur through the strengthening of knowledge, skills and attitudes of the nurses.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Leadership in Nursing
The second strategy clinical audit ensures measurement and monitoring. It can help
improve the safety of healthcare (Vincent et al., 2014). Clinical audit and risk assessment can
help to analyse, monitor risks/hazards, and even learn from safety and quality information of
past events and help to promote self-reflection at the board and clinical levels. Clinical audit
and monitoring will help identify the system in management that are defective. It can be
followed by the integration of safety and quality systems within management (Vincent et al.,
2014). An audit will help promote an environment of safety and quality care while adopting
best practices (Safetyandquality.gov.au, 2018).
Leadership and Management
- Two evidence-based leadership skills for RN
Healthcare industry is characterised by a dynamic system in constant flux, involving
legislative and economic changes. Healthcare leaders working in the managerial and
administrative levels/positions need a diverse array of skills (operational, relational and
analytical) (McFadden et al. 2015). The competencies and skills of the healthcare leaders can
directly affect both the quality and availability of safe healthcare (utica.edu, 2018;
McFadden et al., 2015). Executive leadership can affect the quality and safety environment of
an organisation, and Transformational Leadership (TFL) have been pointed out to be the most
effective leadership style as per McFadden et al. (2015). Two evidence-based leadership
skills have been identified that are relevant to a registered nurse.
The skills identified as components of transformational leadership that are relevant
for the registered nurse are values, optimism, enthusiasm, importance, morals, compelling
vision, collective mission and confidence. Developing the transformation leadership skills
can be effective in the personal development of registered nurse as a leader in healthcare
(McFadden et al., 2015). According to Savage et al. (2014), another set of leadership skills
The second strategy clinical audit ensures measurement and monitoring. It can help
improve the safety of healthcare (Vincent et al., 2014). Clinical audit and risk assessment can
help to analyse, monitor risks/hazards, and even learn from safety and quality information of
past events and help to promote self-reflection at the board and clinical levels. Clinical audit
and monitoring will help identify the system in management that are defective. It can be
followed by the integration of safety and quality systems within management (Vincent et al.,
2014). An audit will help promote an environment of safety and quality care while adopting
best practices (Safetyandquality.gov.au, 2018).
Leadership and Management
- Two evidence-based leadership skills for RN
Healthcare industry is characterised by a dynamic system in constant flux, involving
legislative and economic changes. Healthcare leaders working in the managerial and
administrative levels/positions need a diverse array of skills (operational, relational and
analytical) (McFadden et al. 2015). The competencies and skills of the healthcare leaders can
directly affect both the quality and availability of safe healthcare (utica.edu, 2018;
McFadden et al., 2015). Executive leadership can affect the quality and safety environment of
an organisation, and Transformational Leadership (TFL) have been pointed out to be the most
effective leadership style as per McFadden et al. (2015). Two evidence-based leadership
skills have been identified that are relevant to a registered nurse.
The skills identified as components of transformational leadership that are relevant
for the registered nurse are values, optimism, enthusiasm, importance, morals, compelling
vision, collective mission and confidence. Developing the transformation leadership skills
can be effective in the personal development of registered nurse as a leader in healthcare
(McFadden et al., 2015). According to Savage et al. (2014), another set of leadership skills
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Leadership in Nursing
healthcare leaders should possess as per literature evidence inter-professional teamwork
skills for collaborative governance that can be beneficial for the organisation. These skills
have also been demonstrated by the transformational leadership.
Key skills that can foster personal leadership abilities in healthcare organization can
include: being able to act as agents of change (requiring a proactive approach, anticipating
challenges beforehand and being aware of the latest trends in the industry), having focus on
the bottom-line (that is the providence of safe and quality healthcare that is both affordable
and accessible) and conflict managing skills (healthcaremba.gwu.edu, 2018).
Strategies to achieve the skills-
1. The skills for being agents of change can be developed through leadership training
and health education programs. Studies by Sheriff et al. (2017) showed that student-led
training of the nurses on leadership can be useful to fill in any gaps in the teaching needs of
the nursing students and be a vital strategy towards equipping the healthcare professionals to
become future leaders of healthcare. In addition, participation in continuous professional
development activities is another strategy to develop leadership and communication for
change development skills ().
2. to learn conflict management skills, simulation, as well as classroom-based
team training, is necessary. It improves communication, collaboration, coordination,
competition, and cooperation (Careau et al. 2014). Up taking such classroom-based training
will foster personal development as a registered nurse and handle conflicting situations.
3. Importance of leadership education programs for registered nurse development of
transformational leadership has been implicated by Careau et al. (2014). Such education can
healthcare leaders should possess as per literature evidence inter-professional teamwork
skills for collaborative governance that can be beneficial for the organisation. These skills
have also been demonstrated by the transformational leadership.
Key skills that can foster personal leadership abilities in healthcare organization can
include: being able to act as agents of change (requiring a proactive approach, anticipating
challenges beforehand and being aware of the latest trends in the industry), having focus on
the bottom-line (that is the providence of safe and quality healthcare that is both affordable
and accessible) and conflict managing skills (healthcaremba.gwu.edu, 2018).
Strategies to achieve the skills-
1. The skills for being agents of change can be developed through leadership training
and health education programs. Studies by Sheriff et al. (2017) showed that student-led
training of the nurses on leadership can be useful to fill in any gaps in the teaching needs of
the nursing students and be a vital strategy towards equipping the healthcare professionals to
become future leaders of healthcare. In addition, participation in continuous professional
development activities is another strategy to develop leadership and communication for
change development skills ().
2. to learn conflict management skills, simulation, as well as classroom-based
team training, is necessary. It improves communication, collaboration, coordination,
competition, and cooperation (Careau et al. 2014). Up taking such classroom-based training
will foster personal development as a registered nurse and handle conflicting situations.
3. Importance of leadership education programs for registered nurse development of
transformational leadership has been implicated by Careau et al. (2014). Such education can
8Leadership in Nursing
help develop registered nurses’ competencies to focus on bottom line. Leadership education
ensures delivering best clinical practices for safety and quality of care.
Organizational Culture
-Characteristics of Learning Culture:
Learning culture can be understood as a set of values, practices and processes that
fosters all the employees of an organisation to develop their competence, knowledge and
performance in the organisation (Oracle.com, 2018). Hahn et al. (2015) suggested that
learning culture can help to improve employee creativity by leading the employees to
acquire knowledge and develop innovative ideas. The learning culture is a product of a
culture with organisational learning. Hahn et al. (2015) proposed that organisational learning
culture can positively influence exploitation, exploration and creativity. Because of such
aspects, a learning culture usually have the following characteristics: a culture based on
values, a culture that has support from top management, seeking feedback and information
from all levels in the organization, effective communication, availability of resources,
empowerment of the employees, orientation towards performance, knowledge and the
willingness to learn from mistakes or failures (Jeong et al., 2017; Hjahn et al., 2015; Newton
et al., 2015).
Two of the evidence-based strategies
Two of the evidence-based strategies to contribute to learning culture as a registered nurse-
Education and training - Utilising training and development programs that has
been formalised. A formal developmental plan is more likely to be taken
seriously and therefore implemented (Manuti et al., 2015).
help develop registered nurses’ competencies to focus on bottom line. Leadership education
ensures delivering best clinical practices for safety and quality of care.
Organizational Culture
-Characteristics of Learning Culture:
Learning culture can be understood as a set of values, practices and processes that
fosters all the employees of an organisation to develop their competence, knowledge and
performance in the organisation (Oracle.com, 2018). Hahn et al. (2015) suggested that
learning culture can help to improve employee creativity by leading the employees to
acquire knowledge and develop innovative ideas. The learning culture is a product of a
culture with organisational learning. Hahn et al. (2015) proposed that organisational learning
culture can positively influence exploitation, exploration and creativity. Because of such
aspects, a learning culture usually have the following characteristics: a culture based on
values, a culture that has support from top management, seeking feedback and information
from all levels in the organization, effective communication, availability of resources,
empowerment of the employees, orientation towards performance, knowledge and the
willingness to learn from mistakes or failures (Jeong et al., 2017; Hjahn et al., 2015; Newton
et al., 2015).
Two of the evidence-based strategies
Two of the evidence-based strategies to contribute to learning culture as a registered nurse-
Education and training - Utilising training and development programs that has
been formalised. A formal developmental plan is more likely to be taken
seriously and therefore implemented (Manuti et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9Leadership in Nursing
Feedback sessions and pools can be conducted to evaluate the efficacy of the
training program and identify scope for further development (Watling et al.,
2014).
The importance of education and training in the development of learning culture has
been emphasised by several authors. Maldi et al. (2016) proposed that through education
clinical reasoning skills of healthcare professionals can be improved. Sheriff et al. (2017) also
emphasised the importance of student-led training programs in the development of skills
and competencies of the professionals, which can foster the development of a culture of
excellence and continuous learning.
Taking feedbacks as a registered nurse will help in acquiring and sharing
knowledge in the organisation (Manuti et al., 2015). Learning occurs when nurses
demonstrate good practice, share their knowledge through communication and discussion and
also provide feedback to the learners. Such type of interactions can only occur when positive
leadership practice fosters trust and rapport between the staffs or the administrative team
provides sessions to the learners or the staffs regarding the handling of the patient. After
taking feedback, a formal structure can be developed to overcome drawbacks in system.
Thus, it is processed for acquiring and sharing knowledge in the organisation (Manuti et al.,
2015).
Professional Practice
-Professional Practice for Registered Nurses
Professional practices define the behaviour and practice of midwives and nurses are:
code of conduct, standards for practice and code of ethics. The professional practice can
Feedback sessions and pools can be conducted to evaluate the efficacy of the
training program and identify scope for further development (Watling et al.,
2014).
The importance of education and training in the development of learning culture has
been emphasised by several authors. Maldi et al. (2016) proposed that through education
clinical reasoning skills of healthcare professionals can be improved. Sheriff et al. (2017) also
emphasised the importance of student-led training programs in the development of skills
and competencies of the professionals, which can foster the development of a culture of
excellence and continuous learning.
Taking feedbacks as a registered nurse will help in acquiring and sharing
knowledge in the organisation (Manuti et al., 2015). Learning occurs when nurses
demonstrate good practice, share their knowledge through communication and discussion and
also provide feedback to the learners. Such type of interactions can only occur when positive
leadership practice fosters trust and rapport between the staffs or the administrative team
provides sessions to the learners or the staffs regarding the handling of the patient. After
taking feedback, a formal structure can be developed to overcome drawbacks in system.
Thus, it is processed for acquiring and sharing knowledge in the organisation (Manuti et al.,
2015).
Professional Practice
-Professional Practice for Registered Nurses
Professional practices define the behaviour and practice of midwives and nurses are:
code of conduct, standards for practice and code of ethics. The professional practice can
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
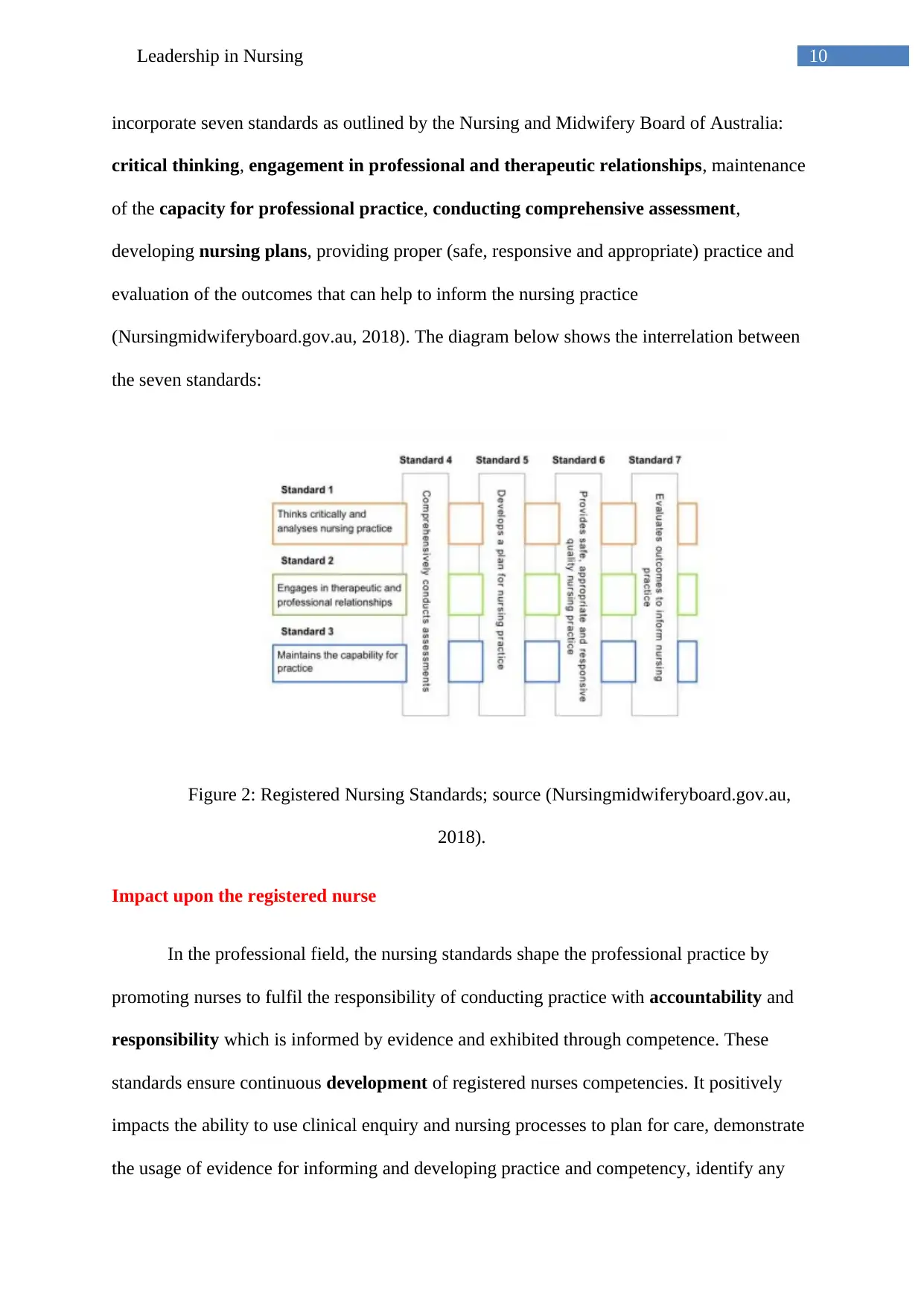
10Leadership in Nursing
incorporate seven standards as outlined by the Nursing and Midwifery Board of Australia:
critical thinking, engagement in professional and therapeutic relationships, maintenance
of the capacity for professional practice, conducting comprehensive assessment,
developing nursing plans, providing proper (safe, responsive and appropriate) practice and
evaluation of the outcomes that can help to inform the nursing practice
(Nursingmidwiferyboard.gov.au, 2018). The diagram below shows the interrelation between
the seven standards:
Figure 2: Registered Nursing Standards; source (Nursingmidwiferyboard.gov.au,
2018).
Impact upon the registered nurse
In the professional field, the nursing standards shape the professional practice by
promoting nurses to fulfil the responsibility of conducting practice with accountability and
responsibility which is informed by evidence and exhibited through competence. These
standards ensure continuous development of registered nurses competencies. It positively
impacts the ability to use clinical enquiry and nursing processes to plan for care, demonstrate
the usage of evidence for informing and developing practice and competency, identify any
incorporate seven standards as outlined by the Nursing and Midwifery Board of Australia:
critical thinking, engagement in professional and therapeutic relationships, maintenance
of the capacity for professional practice, conducting comprehensive assessment,
developing nursing plans, providing proper (safe, responsive and appropriate) practice and
evaluation of the outcomes that can help to inform the nursing practice
(Nursingmidwiferyboard.gov.au, 2018). The diagram below shows the interrelation between
the seven standards:
Figure 2: Registered Nursing Standards; source (Nursingmidwiferyboard.gov.au,
2018).
Impact upon the registered nurse
In the professional field, the nursing standards shape the professional practice by
promoting nurses to fulfil the responsibility of conducting practice with accountability and
responsibility which is informed by evidence and exhibited through competence. These
standards ensure continuous development of registered nurses competencies. It positively
impacts the ability to use clinical enquiry and nursing processes to plan for care, demonstrate
the usage of evidence for informing and developing practice and competency, identify any
11Leadership in Nursing
limitations in knowledge and skills and work within the limitations, taking personal
responsibility for professional conduct, reposting unsafe practices/incompetency/professional
misconduct, demonstrate the ability to act as a mentor, and demonstrate an ability to
safeguard the work environment (Crnm.mb.ca, 2018).
The negative impact on registered nurse is the role ambiguity and role conflict due to
lack of knowledge of the professional practice and responsibilities. It has joint effect on the
performance. Having unclear roles about registered nurses practice, leads to conflicting set of
expectations, incompatibilities or disagreements based on difference, consequently
disturbing the working relationships. It decreases the work productivity (Fong, 2016).
-Self-care strategies
1. Use of Dorothea Orem’s self care theory- that provides an efficient model for the
development of patient’s ability for caring for own health, and revolves around the theories of
self care, self care deficit and nursing system. Here self-care is explained as the activities
individuals initiate and perform for their own selves to maintain the health and well being of
themselves. The important self-care needs are termed as universal self-care requisites which
include the maintaining sufficient intake of air, water food; care for elimination and excretory
processes, balancing activity and rest, balancing solitude and social interaction and avoidance
of hazards. A registered nurse is able to fill this deficit by guiding and supporting patients,
promoting an environment that facilitates personal development and teaching or educating
them about illness and adherence interventions. The Orem’s model comprises of three steps:
Assessment, Nursing diagnosis and Plans and Evaluation & Implementation. As a registered
nurse implementing this theory, will minimise care deficits in patient holistically. Self-care
limitations in knowledge and skills and work within the limitations, taking personal
responsibility for professional conduct, reposting unsafe practices/incompetency/professional
misconduct, demonstrate the ability to act as a mentor, and demonstrate an ability to
safeguard the work environment (Crnm.mb.ca, 2018).
The negative impact on registered nurse is the role ambiguity and role conflict due to
lack of knowledge of the professional practice and responsibilities. It has joint effect on the
performance. Having unclear roles about registered nurses practice, leads to conflicting set of
expectations, incompatibilities or disagreements based on difference, consequently
disturbing the working relationships. It decreases the work productivity (Fong, 2016).
-Self-care strategies
1. Use of Dorothea Orem’s self care theory- that provides an efficient model for the
development of patient’s ability for caring for own health, and revolves around the theories of
self care, self care deficit and nursing system. Here self-care is explained as the activities
individuals initiate and perform for their own selves to maintain the health and well being of
themselves. The important self-care needs are termed as universal self-care requisites which
include the maintaining sufficient intake of air, water food; care for elimination and excretory
processes, balancing activity and rest, balancing solitude and social interaction and avoidance
of hazards. A registered nurse is able to fill this deficit by guiding and supporting patients,
promoting an environment that facilitates personal development and teaching or educating
them about illness and adherence interventions. The Orem’s model comprises of three steps:
Assessment, Nursing diagnosis and Plans and Evaluation & Implementation. As a registered
nurse implementing this theory, will minimise care deficits in patient holistically. Self-care
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





