Leadership for Quality Effectiveness: Human Factors in Healthcare
VerifiedAdded on 2020/04/21
|13
|3164
|82
Report
AI Summary
This report provides a comprehensive review of leadership for quality effectiveness within healthcare, focusing on the application of human factors models to enhance patient safety and overall quality of care. It begins by examining the adoption of aviation-based models, such as Crew Resource Management (CRM), and discusses their strengths and limitations in the healthcare context. The report then delves into macro-ergonomic models, which consider the complex interactions within healthcare environments, and explains their role in improving patient safety. The Systems Engineering Initiative for Patient Safety (SEIPS) model is explored in detail, highlighting its structure, application, and the principles of systems-orientation, person-centeredness, and design-driven improvements. Furthermore, the report analyzes the human error model, specifically the accident causation model, and its relevance to understanding medication errors and patient non-adherence. The report provides insights into both the 'sharp end' and 'blunt end' of healthcare processes, differentiating between active failures (slips, lapses, mistakes, and violations) and the underlying system factors that contribute to errors. The report emphasizes the importance of a holistic and methodical approach to assessing and improving healthcare systems, ultimately aiming to enhance the performance of healthcare professionals and ensure better patient outcomes.

Running Head: LEADERSHIP FOR QUALITY EFFECTIVENESS
Leadership for Quality effectiveness
Name of the student
Name of the University
Author Note
Leadership for Quality effectiveness
Name of the student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
LEADERSHIP FOR QUALITY EFFECTIVENESS
Table of Contents
Introduction......................................................................................................................................2
Review of the literature pertaining to human factors related to work performance in health care. 2
Aviation-based Models................................................................................................................2
Macro-ergonomic Models to improve safety and quality of patients..........................................3
SIEPS Model...............................................................................................................................4
Human error model and its application relating to healthcare.........................................................7
The accident causation model......................................................................................................7
Conclusion.......................................................................................................................................9
Reference.......................................................................................................................................10
LEADERSHIP FOR QUALITY EFFECTIVENESS
Table of Contents
Introduction......................................................................................................................................2
Review of the literature pertaining to human factors related to work performance in health care. 2
Aviation-based Models................................................................................................................2
Macro-ergonomic Models to improve safety and quality of patients..........................................3
SIEPS Model...............................................................................................................................4
Human error model and its application relating to healthcare.........................................................7
The accident causation model......................................................................................................7
Conclusion.......................................................................................................................................9
Reference.......................................................................................................................................10
2
LEADERSHIP FOR QUALITY EFFECTIVENESS
Introduction
In this literature review, some of the major human factor models are being described as
well as their applications in respect of patient safety and quality initiatives. Primarily, the
aviation-based models are being discussed whose adoption has been done in respect of practices
related to healthcare. The initial underpinnings regarding the models as well as their
inadequacies are explained as well. Then, the macro-ergonomic models that are accounting for
the intricate interactions within the environment of healthcare are also being explained.
Review of the literature pertaining to human factors related to work performance in health
care
Aviation-based Models
The prevalence of aviation models to do the development of improvements relating to the
safety of the patients is well recognized. Analogies have been drawn by the researchers from
aviation towards healthcare and provided a strong argument to translate to the clinical realm of
insights from many decades of studies relating to Human factors Engineering (HFE). HFE
models in aviation were based upon the use of the methodical approach to do the identification of
the shortages that are contributing to the failures or performances that are considered being sub-
optimal (Wong, 2013).
Application of training in healthcare
There has been the application of training related to Crew Resource Management (CRM)
in an extensive manner in healthcare with changeable degree of success, basically for doing the
improvement of communication as well as teamwork and to do the improvement of the methods.
LEADERSHIP FOR QUALITY EFFECTIVENESS
Introduction
In this literature review, some of the major human factor models are being described as
well as their applications in respect of patient safety and quality initiatives. Primarily, the
aviation-based models are being discussed whose adoption has been done in respect of practices
related to healthcare. The initial underpinnings regarding the models as well as their
inadequacies are explained as well. Then, the macro-ergonomic models that are accounting for
the intricate interactions within the environment of healthcare are also being explained.
Review of the literature pertaining to human factors related to work performance in health
care
Aviation-based Models
The prevalence of aviation models to do the development of improvements relating to the
safety of the patients is well recognized. Analogies have been drawn by the researchers from
aviation towards healthcare and provided a strong argument to translate to the clinical realm of
insights from many decades of studies relating to Human factors Engineering (HFE). HFE
models in aviation were based upon the use of the methodical approach to do the identification of
the shortages that are contributing to the failures or performances that are considered being sub-
optimal (Wong, 2013).
Application of training in healthcare
There has been the application of training related to Crew Resource Management (CRM)
in an extensive manner in healthcare with changeable degree of success, basically for doing the
improvement of communication as well as teamwork and to do the improvement of the methods.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
LEADERSHIP FOR QUALITY EFFECTIVENESS
Despite the fact that, a final decision in regard to the success of the training related to CRM
cannot be made regarding healthcare, since it is still at a growing level of application within the
domain of healthcare, discussion should be made regarding certain interesting factors (West,
2014).
Approaches of CRM regarding healthcare
Primarily, it can be stated that the CRM approaches are focusing upon the behavioral
safety, a methodology that is not addressing the technological, organizational as well as task-
based issues that are considered being complex, and arising within the settings of healthcare.
Therefore, training approaches that are based upon CRM might be considered being ineffective
within the settings of healthcare. Then, in contrast to the methods that are highly engineered and
are technologically reconciled, healthcare is having the requirement for major human input
(West, 2014). For instance, within aviation, the human interactions occurs with an engineering
process, whereas within healthcare, clinicians are interacting with the patients having
significantly diverse conditions as well as sicknesses that changes in a rapid manner overtime.
Such intrinsic differences within the nature of method response, amongst an engineered process
as well as a natural process does the adding of an extra complexity layer making the approaches
of training relating to aviation-style less flourishing (Wong, 2013).
Macro-ergonomic Models to improve safety and quality of patients
The frameworks relating to human factors to do the evaluation of patient safety as well as
quality of care have been predicated through the approaches relating to macro-ergonomics. The
approaches relating to macro-ergonomics take into consideration an overall process (such as, an
intensive care unit). In addition, communications within the different elements regarding that
LEADERSHIP FOR QUALITY EFFECTIVENESS
Despite the fact that, a final decision in regard to the success of the training related to CRM
cannot be made regarding healthcare, since it is still at a growing level of application within the
domain of healthcare, discussion should be made regarding certain interesting factors (West,
2014).
Approaches of CRM regarding healthcare
Primarily, it can be stated that the CRM approaches are focusing upon the behavioral
safety, a methodology that is not addressing the technological, organizational as well as task-
based issues that are considered being complex, and arising within the settings of healthcare.
Therefore, training approaches that are based upon CRM might be considered being ineffective
within the settings of healthcare. Then, in contrast to the methods that are highly engineered and
are technologically reconciled, healthcare is having the requirement for major human input
(West, 2014). For instance, within aviation, the human interactions occurs with an engineering
process, whereas within healthcare, clinicians are interacting with the patients having
significantly diverse conditions as well as sicknesses that changes in a rapid manner overtime.
Such intrinsic differences within the nature of method response, amongst an engineered process
as well as a natural process does the adding of an extra complexity layer making the approaches
of training relating to aviation-style less flourishing (Wong, 2013).
Macro-ergonomic Models to improve safety and quality of patients
The frameworks relating to human factors to do the evaluation of patient safety as well as
quality of care have been predicated through the approaches relating to macro-ergonomics. The
approaches relating to macro-ergonomics take into consideration an overall process (such as, an
intensive care unit). In addition, communications within the different elements regarding that
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
LEADERSHIP FOR QUALITY EFFECTIVENESS
process, as well as its associations with other processes (Wong 2013). The major components
regarding macro-ergonomics in respect of patient safety take into consideration the following
aspects,
Approaches that are system-oriented
Joint optimization relating to human performance as well as welfare
Taking into consideration the organizational as well as socio-technical context
Communications amongst the different components regarding the process.
Utilization of macro-ergonomics in patient safety
Moreover, macro-ergonomics does the utilization of a more holistic viewpoint to account for
system performance (such as, healthcare process clinicians), welfare as well as safety regarding
the patients and the results (such as, safety of patients). For instance, the work process within an
ICU will be taking into consideration the clinicians, the technologies that are used by them as
well as their communications. There exist various external concerns such as, communication
with other units, organizational practices, as well as regulatory features. While taking into
consideration the design or incorporating new tools within an ICU, a macro-ergonomic approach
will be taking into consideration each of these aspects (Wong, 2013). A brief description will be
provided regarding the different models of macro-ergonomics that have been used to do the
improvement of patient safety as well as quality within the systems of healthcare.
SIEPS Model
The Systems Engineering Initiative for Patient Safety model does the explaining of
patient safety as well as healthcare quality as a functional aspect relating to work systems as well
as processes. The model is based upon the structure-process-outcome model and comprising of
LEADERSHIP FOR QUALITY EFFECTIVENESS
process, as well as its associations with other processes (Wong 2013). The major components
regarding macro-ergonomics in respect of patient safety take into consideration the following
aspects,
Approaches that are system-oriented
Joint optimization relating to human performance as well as welfare
Taking into consideration the organizational as well as socio-technical context
Communications amongst the different components regarding the process.
Utilization of macro-ergonomics in patient safety
Moreover, macro-ergonomics does the utilization of a more holistic viewpoint to account for
system performance (such as, healthcare process clinicians), welfare as well as safety regarding
the patients and the results (such as, safety of patients). For instance, the work process within an
ICU will be taking into consideration the clinicians, the technologies that are used by them as
well as their communications. There exist various external concerns such as, communication
with other units, organizational practices, as well as regulatory features. While taking into
consideration the design or incorporating new tools within an ICU, a macro-ergonomic approach
will be taking into consideration each of these aspects (Wong, 2013). A brief description will be
provided regarding the different models of macro-ergonomics that have been used to do the
improvement of patient safety as well as quality within the systems of healthcare.
SIEPS Model
The Systems Engineering Initiative for Patient Safety model does the explaining of
patient safety as well as healthcare quality as a functional aspect relating to work systems as well
as processes. The model is based upon the structure-process-outcome model and comprising of
5
LEADERSHIP FOR QUALITY EFFECTIVENESS
three interacting elements, such as the work process, its impacts upon the methods relating to
care as well as the results (West, 2014). The SEIPS model draws on three key human factors
principles such as systems-orientation, person-centeredness as well as developments that are
design-driven. The deriving of system-orientation occurs from the holistic approach in respect of
studying an entire process of healthcare (Weaver, 2016). The deriving of person-centeredness
occurs from taking into consideration individuals to be the core aspect relating to the work of
healthcare with the supposition that there should be the designing as well as development of
tools, technologies as well as systems of support with the consideration of the strengths as well
as limitations of the users. Also, the improvements that are design-driven concentrates upon the
improvement of work related to healthcare via the development of tools as well as activities of
work that will be optimizing the human and team performance (Taylor, 2013).
Work process of SIEPS Model
The work process are consisting of individuals (such as, physicians, nurses as well as
other support staff), tasks, tools as well as technologies, the physical surrounding where the
performance of these tasks will occur, and also the organizational factors that are affecting the
activities related to work. Moreover, the work process is also influenced by the external factors
like institutional policies as well as guidelines that are externally imposed (Sherwood. 2017).
The task of a physician to enter the orders of patients gets influenced by the characteristics of the
physician, the characteristics of tools utilized in respect of entering the orders as well as the
practices and norms relating to the organization. The model does the assumption that the
components of work process will be interacting as well as affecting the methods of care as well
as workflow, which in turn, influence outcomes regarding healthcare such as safety and, in more
general terms, the quality of healthcare (Phelps, 2014). The model does the incorporation of two
LEADERSHIP FOR QUALITY EFFECTIVENESS
three interacting elements, such as the work process, its impacts upon the methods relating to
care as well as the results (West, 2014). The SEIPS model draws on three key human factors
principles such as systems-orientation, person-centeredness as well as developments that are
design-driven. The deriving of system-orientation occurs from the holistic approach in respect of
studying an entire process of healthcare (Weaver, 2016). The deriving of person-centeredness
occurs from taking into consideration individuals to be the core aspect relating to the work of
healthcare with the supposition that there should be the designing as well as development of
tools, technologies as well as systems of support with the consideration of the strengths as well
as limitations of the users. Also, the improvements that are design-driven concentrates upon the
improvement of work related to healthcare via the development of tools as well as activities of
work that will be optimizing the human and team performance (Taylor, 2013).
Work process of SIEPS Model
The work process are consisting of individuals (such as, physicians, nurses as well as
other support staff), tasks, tools as well as technologies, the physical surrounding where the
performance of these tasks will occur, and also the organizational factors that are affecting the
activities related to work. Moreover, the work process is also influenced by the external factors
like institutional policies as well as guidelines that are externally imposed (Sherwood. 2017).
The task of a physician to enter the orders of patients gets influenced by the characteristics of the
physician, the characteristics of tools utilized in respect of entering the orders as well as the
practices and norms relating to the organization. The model does the assumption that the
components of work process will be interacting as well as affecting the methods of care as well
as workflow, which in turn, influence outcomes regarding healthcare such as safety and, in more
general terms, the quality of healthcare (Phelps, 2014). The model does the incorporation of two
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
LEADERSHIP FOR QUALITY EFFECTIVENESS
loops relating to feedback such as, within the work process as well as care methods, and within
the work process as well as results. The feedback loops does the providing of metrics in respect
of probable redesign.
Application of the SEIPS model
There has been the application of the SEIPS model regarding the study of various
problems relating to safety as well as quality, which included medication safety, emergency
room readmissions as well as management relating to nursing workload. For instance, the SEIPS
structure is being used for categorizing the factors that contribute to the occurrence of duplicate
medication orders through the use of a CPOE process (Parand, 2014). The contributing factors
will be take into consideration the technological, team based as well as organizational
surrounding.
Elements comprised by the SEIPS model
This model comprises of three elements of interaction, such as performance inputs,
transformational methods, performance outputs as well as feedback loops amongst the three
elements. The performance inputs does the representation of the elements relating to the work
system, such as the physician as well as patient, tasks, tools, organizational as well as external
factors. The transformational methods do the representation of the ways by which the inputs are
influencing the physical, cognitive as well as social performance regarding the healthcare
professionals (Millar, 2013). For instance, the proficiency as well as skills regarding the
physicians does the influencing of their capabilities for identifying as well as filtering
inappropriate information regarding the case of patients. The outputs do the representation of
successfully completing the tasks (such as providing the patients necessary medications or doing
LEADERSHIP FOR QUALITY EFFECTIVENESS
loops relating to feedback such as, within the work process as well as care methods, and within
the work process as well as results. The feedback loops does the providing of metrics in respect
of probable redesign.
Application of the SEIPS model
There has been the application of the SEIPS model regarding the study of various
problems relating to safety as well as quality, which included medication safety, emergency
room readmissions as well as management relating to nursing workload. For instance, the SEIPS
structure is being used for categorizing the factors that contribute to the occurrence of duplicate
medication orders through the use of a CPOE process (Parand, 2014). The contributing factors
will be take into consideration the technological, team based as well as organizational
surrounding.
Elements comprised by the SEIPS model
This model comprises of three elements of interaction, such as performance inputs,
transformational methods, performance outputs as well as feedback loops amongst the three
elements. The performance inputs does the representation of the elements relating to the work
system, such as the physician as well as patient, tasks, tools, organizational as well as external
factors. The transformational methods do the representation of the ways by which the inputs are
influencing the physical, cognitive as well as social performance regarding the healthcare
professionals (Millar, 2013). For instance, the proficiency as well as skills regarding the
physicians does the influencing of their capabilities for identifying as well as filtering
inappropriate information regarding the case of patients. The outputs do the representation of
successfully completing the tasks (such as providing the patients necessary medications or doing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
LEADERSHIP FOR QUALITY EFFECTIVENESS
order entry). The three elements relating to the model are having intrinsic feedback loops within
them that are acting as an input regarding other methods. The feedback loop is also serving as a
mechanism of learning, acting as a guide in respect of actions that will be taken in the future
regarding processes or events that are considered being similar (McFadden, 2015). The
healthcare professional performance model is relying upon the key HFE principles to do the
improvement of the technological aspects, practices and methods relating to healthcare via the
design of tools as well as interventions that are supporting the performance of the healthcare
professionals.
Utilization of methodical assessment structure
The utilization of a holistic, methodical assessment structure assists in providing various
advantages relating to patient safety as well as quality schemes. Primarily, these studies does the
utilization of an approach that is regarded as multi-method, offering insights in respect of the
methods regarding work system from different point of views (Hignett, 2015). Then, a holistic
approach in regard to various aspects of a process is taken into consideration. Differently
speaking, in respect of every clinical environment, the individual, team, organizational as well as
other contextual factors relating to the environment are taken into consideration. Hence, there
occurs the capturing of the work system issues from various points of views offering the
capability for discerning in an effective manner potential factors that are hampering the quality
as well as safety regarding patient care (Healy, 2016).
LEADERSHIP FOR QUALITY EFFECTIVENESS
order entry). The three elements relating to the model are having intrinsic feedback loops within
them that are acting as an input regarding other methods. The feedback loop is also serving as a
mechanism of learning, acting as a guide in respect of actions that will be taken in the future
regarding processes or events that are considered being similar (McFadden, 2015). The
healthcare professional performance model is relying upon the key HFE principles to do the
improvement of the technological aspects, practices and methods relating to healthcare via the
design of tools as well as interventions that are supporting the performance of the healthcare
professionals.
Utilization of methodical assessment structure
The utilization of a holistic, methodical assessment structure assists in providing various
advantages relating to patient safety as well as quality schemes. Primarily, these studies does the
utilization of an approach that is regarded as multi-method, offering insights in respect of the
methods regarding work system from different point of views (Hignett, 2015). Then, a holistic
approach in regard to various aspects of a process is taken into consideration. Differently
speaking, in respect of every clinical environment, the individual, team, organizational as well as
other contextual factors relating to the environment are taken into consideration. Hence, there
occurs the capturing of the work system issues from various points of views offering the
capability for discerning in an effective manner potential factors that are hampering the quality
as well as safety regarding patient care (Healy, 2016).
8
LEADERSHIP FOR QUALITY EFFECTIVENESS
Human error model and its application relating to healthcare
The accident causation model
This model of human error has been particularly adapted in respect of healthcare and has
been used for understanding errors related to medication a well as non-adherence of patients. In
accord to the accident causation model, it can be stated that a process is having both a ‘sharp
end’ as well as a ‘blunt end’.
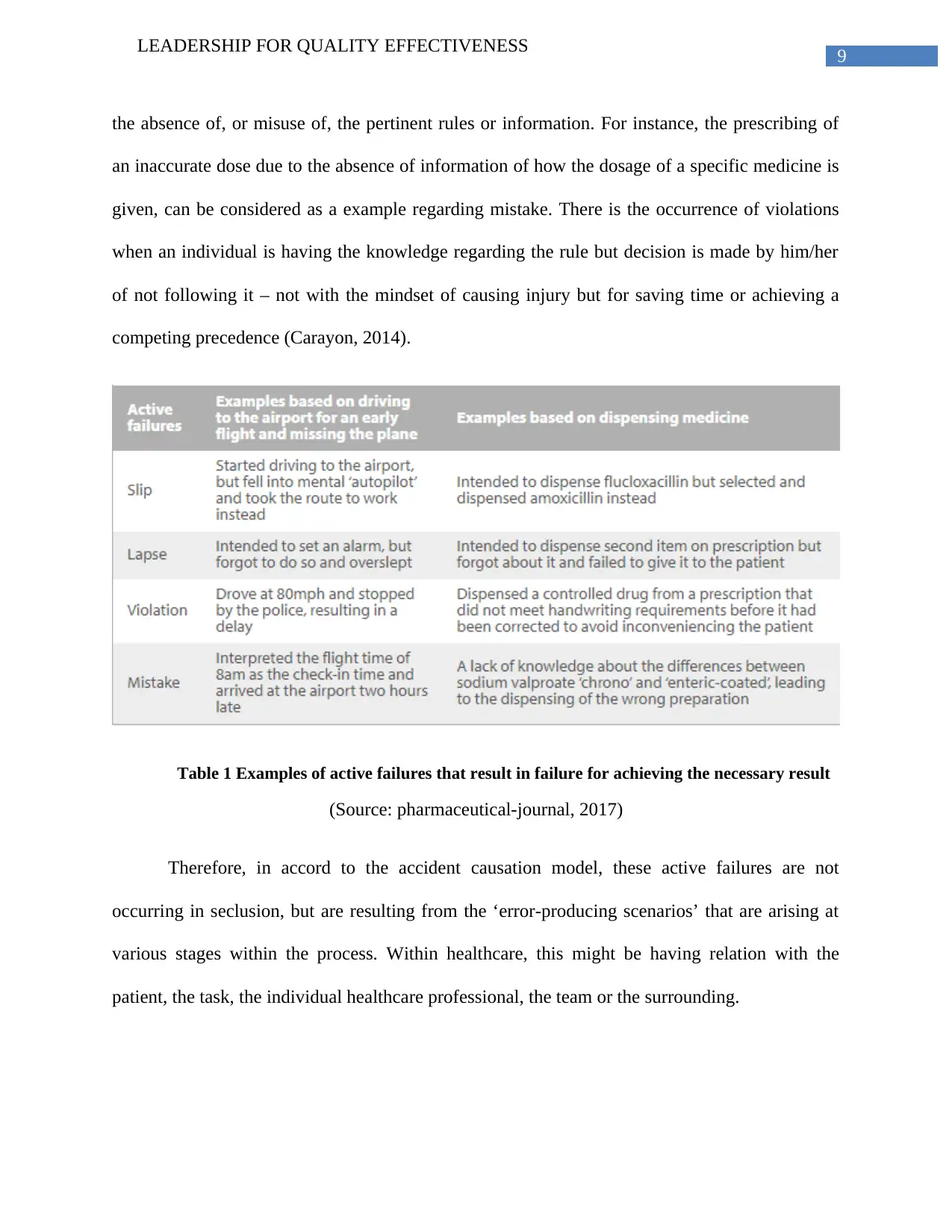
Active failures in health care
At the sharp end, there will be the occurrence of ‘active failures’ regarding the front-line workers
(Grol, 2013). These active failures are considered being acts that are considered unsafe and its
classification can be done regarding slips, lapses, violations as well as mistakes. There is the
occurrence of slips as well as lapses when the preparation of the correct plan is done but its
execution is done in an incorrect manner (Finkelman, 2015).
Causes for active failure in health care
In particular, there is the occurrence of a ‘slip’ when a step regarding the plan will be
carried out in an incorrect manner, while a ‘lapse’ will be occurring when a stage regarding the
plan will get omitted. For instance, within clinical practice, the slips that are recognized are
considered to be the selection of the wrong drug from a drop-down menu or having the intention
to do the dispensing of one quantity of tablet while dispensing the other (Doyle, 2013). Lapses
take into consideration a prescriber forgetting to strike off a drug from the drug chart or a patient
not remembering when to take a dose regarding the medicine they are having. On the other hand,
there is the occurrence of ‘mistakes’ as well as ‘violations’ when there occurs the formulation of
an incorrect plan and then pursued (Chassin, 2013). There is the occurrence of mistakes due to
LEADERSHIP FOR QUALITY EFFECTIVENESS
Human error model and its application relating to healthcare
The accident causation model
This model of human error has been particularly adapted in respect of healthcare and has
been used for understanding errors related to medication a well as non-adherence of patients. In
accord to the accident causation model, it can be stated that a process is having both a ‘sharp
end’ as well as a ‘blunt end’.
Active failures in health care
At the sharp end, there will be the occurrence of ‘active failures’ regarding the front-line workers
(Grol, 2013). These active failures are considered being acts that are considered unsafe and its
classification can be done regarding slips, lapses, violations as well as mistakes. There is the
occurrence of slips as well as lapses when the preparation of the correct plan is done but its
execution is done in an incorrect manner (Finkelman, 2015).
Causes for active failure in health care
In particular, there is the occurrence of a ‘slip’ when a step regarding the plan will be
carried out in an incorrect manner, while a ‘lapse’ will be occurring when a stage regarding the
plan will get omitted. For instance, within clinical practice, the slips that are recognized are
considered to be the selection of the wrong drug from a drop-down menu or having the intention
to do the dispensing of one quantity of tablet while dispensing the other (Doyle, 2013). Lapses
take into consideration a prescriber forgetting to strike off a drug from the drug chart or a patient
not remembering when to take a dose regarding the medicine they are having. On the other hand,
there is the occurrence of ‘mistakes’ as well as ‘violations’ when there occurs the formulation of
an incorrect plan and then pursued (Chassin, 2013). There is the occurrence of mistakes due to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
LEADERSHIP FOR QUALITY EFFECTIVENESS
the absence of, or misuse of, the pertinent rules or information. For instance, the prescribing of
an inaccurate dose due to the absence of information of how the dosage of a specific medicine is
given, can be considered as a example regarding mistake. There is the occurrence of violations
when an individual is having the knowledge regarding the rule but decision is made by him/her
of not following it – not with the mindset of causing injury but for saving time or achieving a
competing precedence (Carayon, 2014).
Table 1 Examples of active failures that result in failure for achieving the necessary result
(Source: pharmaceutical-journal, 2017)
Therefore, in accord to the accident causation model, these active failures are not
occurring in seclusion, but are resulting from the ‘error-producing scenarios’ that are arising at
various stages within the process. Within healthcare, this might be having relation with the
patient, the task, the individual healthcare professional, the team or the surrounding.
LEADERSHIP FOR QUALITY EFFECTIVENESS
the absence of, or misuse of, the pertinent rules or information. For instance, the prescribing of
an inaccurate dose due to the absence of information of how the dosage of a specific medicine is
given, can be considered as a example regarding mistake. There is the occurrence of violations
when an individual is having the knowledge regarding the rule but decision is made by him/her
of not following it – not with the mindset of causing injury but for saving time or achieving a
competing precedence (Carayon, 2014).
Table 1 Examples of active failures that result in failure for achieving the necessary result
(Source: pharmaceutical-journal, 2017)
Therefore, in accord to the accident causation model, these active failures are not
occurring in seclusion, but are resulting from the ‘error-producing scenarios’ that are arising at
various stages within the process. Within healthcare, this might be having relation with the
patient, the task, the individual healthcare professional, the team or the surrounding.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
LEADERSHIP FOR QUALITY EFFECTIVENESS
Conclusion
From the above discussion, it can be concluded that there has been the demonstration of
the concepts relating to patient safety as well as quality within healthcare. The impact of human
factors regarding the context of healthcare as well as their impact on staff performance in respect
of patient safety has been explained. There has also been the explanation regarding the human
error theory as well as application regarding healthcare. There has also been an analysis of the
association of the human factors with the quality as well as safety regarding healthcare.
LEADERSHIP FOR QUALITY EFFECTIVENESS
Conclusion
From the above discussion, it can be concluded that there has been the demonstration of
the concepts relating to patient safety as well as quality within healthcare. The impact of human
factors regarding the context of healthcare as well as their impact on staff performance in respect
of patient safety has been explained. There has also been the explanation regarding the human
error theory as well as application regarding healthcare. There has also been an analysis of the
association of the human factors with the quality as well as safety regarding healthcare.
11
LEADERSHIP FOR QUALITY EFFECTIVENESS
Reference
Carayon, P., Wetterneck, T. B., Rivera-Rodriguez, A. J., Hundt, A. S., Hoonakker, P., Holden,
R., & Gurses, A. P. (2014). Human factors systems approach to healthcare quality and
patient safety. Applied ergonomics, 45(1), 14-25.
Chassin, M. R. (2013). Improving the quality of health care: what’s taking so long?. Health
Affairs, 32(10), 1761-1765.
Doyle, C., Lennox, L., & Bell, D. (2013). A systematic review of evidence on the links between
patient experience and clinical safety and effectiveness. BMJ open, 3(1), e001570.
Finkelman, A. (2015). Leadership and Management in Nursing: Core Competencies for Quality
Care. Pearson.
Grol, R., Wensing, M., Eccles, M., & Davis, D. (Eds.). (2013). Improving patient care: the
implementation of change in health care. John Wiley & Sons.
Healy, J. (2016). Improving health care safety and quality: reluctant regulators. Routledge.
Hignett, S., Jones, E. L., Miller, D., Wolf, L., Modi, C., Shahzad, M. W., ... & Catchpole, K.
(2015). Human factors and ergonomics and quality improvement science: integrating
approaches for safety in healthcare. BMJ Qual Saf, 24(4), 250-254.
McFadden, K. L., Stock, G. N., & Gowen III, C. R. (2015). Leadership, safety climate, and
continuous quality improvement: impact on process quality and patient safety. Health
care management review, 40(1), 24-34.
LEADERSHIP FOR QUALITY EFFECTIVENESS
Reference
Carayon, P., Wetterneck, T. B., Rivera-Rodriguez, A. J., Hundt, A. S., Hoonakker, P., Holden,
R., & Gurses, A. P. (2014). Human factors systems approach to healthcare quality and
patient safety. Applied ergonomics, 45(1), 14-25.
Chassin, M. R. (2013). Improving the quality of health care: what’s taking so long?. Health
Affairs, 32(10), 1761-1765.
Doyle, C., Lennox, L., & Bell, D. (2013). A systematic review of evidence on the links between
patient experience and clinical safety and effectiveness. BMJ open, 3(1), e001570.
Finkelman, A. (2015). Leadership and Management in Nursing: Core Competencies for Quality
Care. Pearson.
Grol, R., Wensing, M., Eccles, M., & Davis, D. (Eds.). (2013). Improving patient care: the
implementation of change in health care. John Wiley & Sons.
Healy, J. (2016). Improving health care safety and quality: reluctant regulators. Routledge.
Hignett, S., Jones, E. L., Miller, D., Wolf, L., Modi, C., Shahzad, M. W., ... & Catchpole, K.
(2015). Human factors and ergonomics and quality improvement science: integrating
approaches for safety in healthcare. BMJ Qual Saf, 24(4), 250-254.
McFadden, K. L., Stock, G. N., & Gowen III, C. R. (2015). Leadership, safety climate, and
continuous quality improvement: impact on process quality and patient safety. Health
care management review, 40(1), 24-34.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





