Leadership for Quality & Safety in Health Care - Assessment 1
VerifiedAdded on 2023/06/08
|10
|2325
|461
Homework Assignment
AI Summary
This assignment focuses on quality, effectiveness, and safety in healthcare, addressing key principles of total quality management (TQM) and continuous quality improvement (CQI). It differentiates between healthcare and industry-based quality management approaches, highlighting tools like Six Sigma and the balanced scorecard. The assignment defines patient safety, emphasizing risk management and the importance of identifying and mitigating risk factors. It also explores the concept of safety culture, discussing how organizational culture impacts patient and worker safety, and methods for measuring and improving safety culture within healthcare organizations. Desklib is a platform where students can find similar solved assignments and study resources.

Running head: QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
Name of the Student:
Name of the University:
Author Note:
QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
Answer 1:
Quality in health care can be defined as the process by which research analysts ensure
that the medical health services provided by a health care organization is safe and at the same
time yields positive patient outcomes (Bates et al., 2014). Problems associated with the minimal
use, exploitation or misuse of medical resources are determined on the basis of the evaluation of
the health care services offered by a particular health care organization (Chartier, 2014). It is also
important to note here that by virtue of the iron triangle of health care, researchers can easily
develop an overview to measure and correlate the existing relationship between health care
service quality, cost effectiveness and accessibility of the resources (Clement, 2017). Five
principal concepts are implied in the process of monitoring quality services and related outcomes
in the health care services (Dumont et al., 2013). The first three concepts are synonymous to the
principles of total quality management or TQM and focuses on the customer needs, extensive
research and implementing improvement and participation and collective team work by all
employees. The fourth principle comprises of management commitment to improve service
delivery and to maintain an approach so as to continuously provide better service delivery (Free
et al., 2013). The TQM ensures total quality management in service delivery and is a continuous
process. It majorly aims at incorporating a permanent change in the work culture of the
organization. Total Quality Management heavily relies upon the quality assurance tools and
ensure that the overall quality of the organization in association to the production is continuously
improved (Gittell et al., 2013). It ensures positive employee performance through provision of
adequate funding, staffing and training opportunities. On the other hand the CQI ensures that the
quality of the service delivery is consistently enhanced with the use of latest technological
innovation and infrastructure development. TQM and CQI approach vary for different service
Answer 1:
Quality in health care can be defined as the process by which research analysts ensure
that the medical health services provided by a health care organization is safe and at the same
time yields positive patient outcomes (Bates et al., 2014). Problems associated with the minimal
use, exploitation or misuse of medical resources are determined on the basis of the evaluation of
the health care services offered by a particular health care organization (Chartier, 2014). It is also
important to note here that by virtue of the iron triangle of health care, researchers can easily
develop an overview to measure and correlate the existing relationship between health care
service quality, cost effectiveness and accessibility of the resources (Clement, 2017). Five
principal concepts are implied in the process of monitoring quality services and related outcomes
in the health care services (Dumont et al., 2013). The first three concepts are synonymous to the
principles of total quality management or TQM and focuses on the customer needs, extensive
research and implementing improvement and participation and collective team work by all
employees. The fourth principle comprises of management commitment to improve service
delivery and to maintain an approach so as to continuously provide better service delivery (Free
et al., 2013). The TQM ensures total quality management in service delivery and is a continuous
process. It majorly aims at incorporating a permanent change in the work culture of the
organization. Total Quality Management heavily relies upon the quality assurance tools and
ensure that the overall quality of the organization in association to the production is continuously
improved (Gittell et al., 2013). It ensures positive employee performance through provision of
adequate funding, staffing and training opportunities. On the other hand the CQI ensures that the
quality of the service delivery is consistently enhanced with the use of latest technological
innovation and infrastructure development. TQM and CQI approach vary for different service

2QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
sectors. While the healthcare sector primarily focuses on improving the medical services with the
changing trend in medical technology and innovation, other service sectors focus on the quality
improvement of the related domain. The six sigma tool and the lean thinking or the balance
scorecard are quality improvement tools that make use of a strong methodology to monitor the
efficiency of the services being dispensed by the enterprise (Zornoza et al., 2017). It helps in
making the best use of the empirical as well as the statistical methods to compare the process
management, possible innovation and improvement outcome of every organization (Hunter et al.,
2017). The balance scorecard on the other hand helps in maintaining an equilibrium between the
operational strategies in practice, developing an improvement and aligning the adapted reforms
with the vision of the organization.
sectors. While the healthcare sector primarily focuses on improving the medical services with the
changing trend in medical technology and innovation, other service sectors focus on the quality
improvement of the related domain. The six sigma tool and the lean thinking or the balance
scorecard are quality improvement tools that make use of a strong methodology to monitor the
efficiency of the services being dispensed by the enterprise (Zornoza et al., 2017). It helps in
making the best use of the empirical as well as the statistical methods to compare the process
management, possible innovation and improvement outcome of every organization (Hunter et al.,
2017). The balance scorecard on the other hand helps in maintaining an equilibrium between the
operational strategies in practice, developing an improvement and aligning the adapted reforms
with the vision of the organization.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
Answer 2: patient safety
As per the Australian patient safety foundation Shekelle et al. (2013), patient safety is
defined as “the reduction and mitigation of unsafe practices within the healthcare system. The
use of best practices have shown to yield optimal patient outcomes. Patient safety can be defined
as all the measures undertaken in order to provide patients with safe and quality health services.
Safety in health care can be defined as the stringent monitoring of the equipment used in order to
promote service delivery in accordance with the NSQHS standards. It encompasses of the
responsibility to cross check and double check the quality of the resources used such as checking
the expiry date of the pharmaceutical drugs and detect any possibility of contamination or
leakage and adopting necessary measures to replace such faulty products in order to maintain
patient safety (Iacob & Constantin, 2014). Hence, it can be said that maintenance of stringent
safety guidelines in the health care sector can effectively contribute to patient safety and
improved quality outcome. Risk management in healthcare can be defined as the complete cycle
of identifying, accessing and prioritizing risk factors associated with poor service delivery and
adapt measures to mitigate the defined risk factors. The prioritization of risk plays an important
role in ensuring patient safety. In this context, it can be said that ‘risk’ is an external factor that
could be manifested due to an unprecedented mismanagement in handling a project, or due to
inappropriate funding or due to disasters rising on account of manhandling and errors at the
professional level (Iuga & McGuire, 2014). On account of each of the mentioned risks there is a
high possibility of a fatal consequence (Wager et al., 2017). Hence, it should be ensured by the
administration that the organization has appropriate mitigation measures to combat an
unforeseen risk factor. While developing strategies to combat the negative effect of the risk
factors it is pivotal to identify the root cause of the happening on a priority basis, following the
Answer 2: patient safety
As per the Australian patient safety foundation Shekelle et al. (2013), patient safety is
defined as “the reduction and mitigation of unsafe practices within the healthcare system. The
use of best practices have shown to yield optimal patient outcomes. Patient safety can be defined
as all the measures undertaken in order to provide patients with safe and quality health services.
Safety in health care can be defined as the stringent monitoring of the equipment used in order to
promote service delivery in accordance with the NSQHS standards. It encompasses of the
responsibility to cross check and double check the quality of the resources used such as checking
the expiry date of the pharmaceutical drugs and detect any possibility of contamination or
leakage and adopting necessary measures to replace such faulty products in order to maintain
patient safety (Iacob & Constantin, 2014). Hence, it can be said that maintenance of stringent
safety guidelines in the health care sector can effectively contribute to patient safety and
improved quality outcome. Risk management in healthcare can be defined as the complete cycle
of identifying, accessing and prioritizing risk factors associated with poor service delivery and
adapt measures to mitigate the defined risk factors. The prioritization of risk plays an important
role in ensuring patient safety. In this context, it can be said that ‘risk’ is an external factor that
could be manifested due to an unprecedented mismanagement in handling a project, or due to
inappropriate funding or due to disasters rising on account of manhandling and errors at the
professional level (Iuga & McGuire, 2014). On account of each of the mentioned risks there is a
high possibility of a fatal consequence (Wager et al., 2017). Hence, it should be ensured by the
administration that the organization has appropriate mitigation measures to combat an
unforeseen risk factor. While developing strategies to combat the negative effect of the risk
factors it is pivotal to identify the root cause of the happening on a priority basis, following the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
procedure of identification, it is important to consider two aspects of policies. The first involving
in strategies that would nullify the negative effect or reduce the adversity of the risk factor and
the second strategy would aim at developing combat strategies in order to avoid such a scenario
in future. In order to perform an effective risk analysis and adapt appropriate mitigation
measures, it is important to correctly evaluate the possibilities of a risk occurrence. This step
could be addressed by using the appropriate risk management analysis tools. The correct use of a
risk management tool is based upon which risk factor is to be evaluated. A wide range of
assessment tools for the evaluation of a diverse range of risk entities is available. Tools could
effectively evaluate the risk factors associated with strategic analysis in order to measure the
efficacy of the business objectives. The threat analysis, effectively analyses the risks associated
with business security. The investment risk analysis accesses the risks pertaining to investment
and returns and develops alternative strategies in order to address such risks effectively. The
program risk management identifies the risks associated with the successful implementation of a
program and also strategically plans an alternative in case of the failure of the project plan. The
cost risk analysis helps in identifying the risk factors associated with the financial fluctuations
and economic risks and accordingly adapt mitigating measures to combat such losses. Hence, it
can be said that the quality of risk management primarily depends upon the identification of the
risk factors followed by prioritization in order to proceed effectively with the mitigation plan.
procedure of identification, it is important to consider two aspects of policies. The first involving
in strategies that would nullify the negative effect or reduce the adversity of the risk factor and
the second strategy would aim at developing combat strategies in order to avoid such a scenario
in future. In order to perform an effective risk analysis and adapt appropriate mitigation
measures, it is important to correctly evaluate the possibilities of a risk occurrence. This step
could be addressed by using the appropriate risk management analysis tools. The correct use of a
risk management tool is based upon which risk factor is to be evaluated. A wide range of
assessment tools for the evaluation of a diverse range of risk entities is available. Tools could
effectively evaluate the risk factors associated with strategic analysis in order to measure the
efficacy of the business objectives. The threat analysis, effectively analyses the risks associated
with business security. The investment risk analysis accesses the risks pertaining to investment
and returns and develops alternative strategies in order to address such risks effectively. The
program risk management identifies the risks associated with the successful implementation of a
program and also strategically plans an alternative in case of the failure of the project plan. The
cost risk analysis helps in identifying the risk factors associated with the financial fluctuations
and economic risks and accordingly adapt mitigating measures to combat such losses. Hence, it
can be said that the quality of risk management primarily depends upon the identification of the
risk factors followed by prioritization in order to proceed effectively with the mitigation plan.
5QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
Answer 3: safety culture
The concept of safety culture for healthcare is determined as a positive thinking and
perception of the workers about their physical and psychological safety, teamwork and
leadership related safety. Further, they are comfortable to discuss the flaws of the system and
possess a collective and cumulative thinking about the loopholes and the frontline workers take
responsibility of change so that safety can be ensured again. High reliability organizations
possess positive safety culture however, when the suggestions of workers are not included for
safety betterment, a lack of self-satisfaction and a constant concern about safety is built into the
organization that affects the fabric of it. It has been noted through healthcare practices that
culture influences safety in healthcare, however little research has been conducted to determine
this concept. Hence, it cannot be said with the help of research evidence that culture of any
organization will help increasing positive outcomes for patients, but healthcare professionals and
their culturally compliance care process helps and contributes in safety for patients and
professionals safety in healthcare organizations.
Shekelle et al. (2013) suggests that culture can never be described or measured, but it can
be manifested. As a healthcare organization is cumulative result of many thoughts and beliefs, all
these different elements it is quite difficult to measure the beliefs which contributes in effective
safety culture and others that imparts poor and negative or unsafe culture. Therefore,
measurements are made by sharing the staff and patient’s stories about their safety culture related
feedback for the organization and fostering the right environment to create a positive and
developed safety culture. This will help to create an environment where sharing of information is
done based on their job satisfaction and reporting rates and an improved methodology is found.
Further () mentions another way to create an environment of measurement of safety culture for
Answer 3: safety culture
The concept of safety culture for healthcare is determined as a positive thinking and
perception of the workers about their physical and psychological safety, teamwork and
leadership related safety. Further, they are comfortable to discuss the flaws of the system and
possess a collective and cumulative thinking about the loopholes and the frontline workers take
responsibility of change so that safety can be ensured again. High reliability organizations
possess positive safety culture however, when the suggestions of workers are not included for
safety betterment, a lack of self-satisfaction and a constant concern about safety is built into the
organization that affects the fabric of it. It has been noted through healthcare practices that
culture influences safety in healthcare, however little research has been conducted to determine
this concept. Hence, it cannot be said with the help of research evidence that culture of any
organization will help increasing positive outcomes for patients, but healthcare professionals and
their culturally compliance care process helps and contributes in safety for patients and
professionals safety in healthcare organizations.
Shekelle et al. (2013) suggests that culture can never be described or measured, but it can
be manifested. As a healthcare organization is cumulative result of many thoughts and beliefs, all
these different elements it is quite difficult to measure the beliefs which contributes in effective
safety culture and others that imparts poor and negative or unsafe culture. Therefore,
measurements are made by sharing the staff and patient’s stories about their safety culture related
feedback for the organization and fostering the right environment to create a positive and
developed safety culture. This will help to create an environment where sharing of information is
done based on their job satisfaction and reporting rates and an improved methodology is found.
Further () mentions another way to create an environment of measurement of safety culture for
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
patients and staff and this is demonstrated by allotting a day in month, when all the staff and
patients of the health care facility will come together and will share their fundamental, emotional
and social challenges they had to face while working and receiving care respectively.
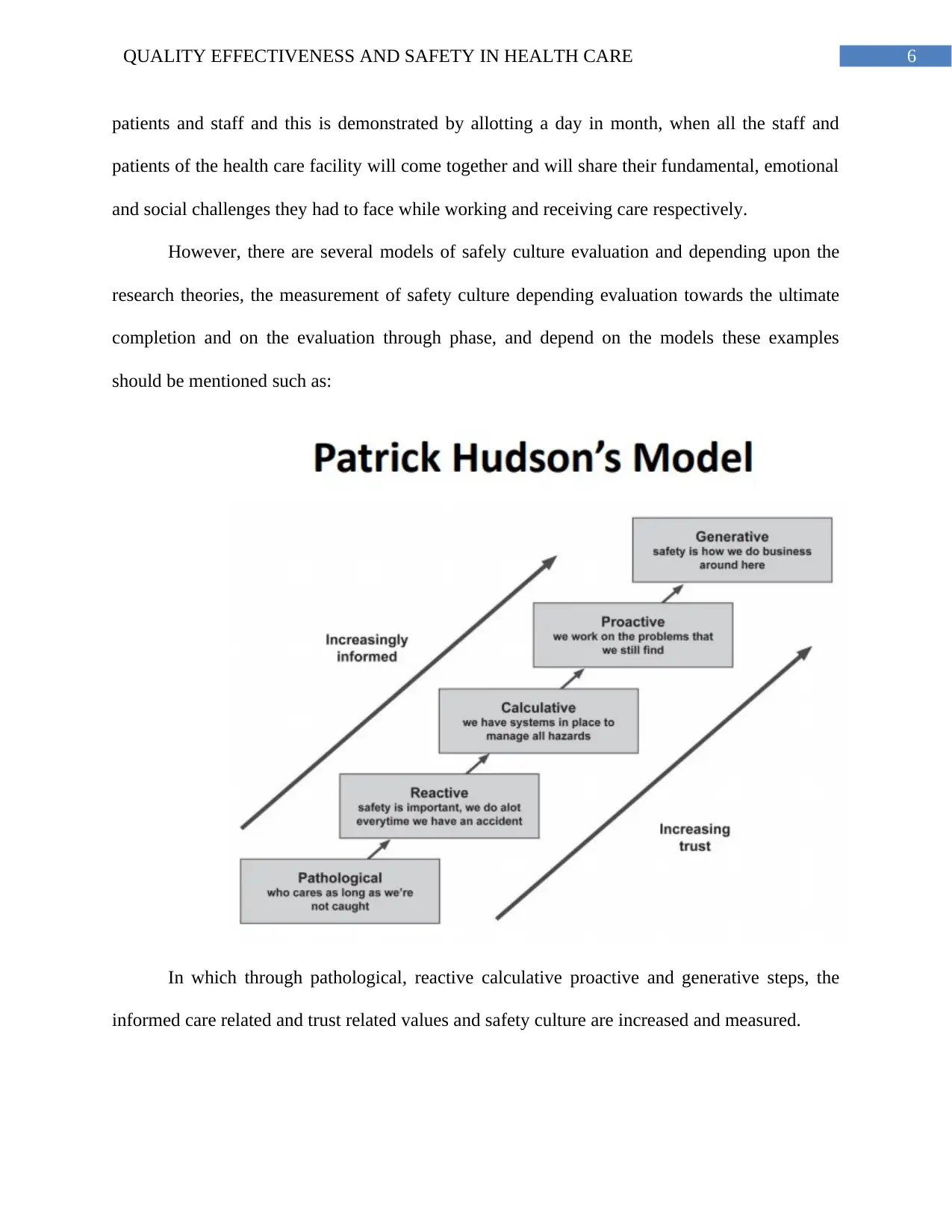
However, there are several models of safely culture evaluation and depending upon the
research theories, the measurement of safety culture depending evaluation towards the ultimate
completion and on the evaluation through phase, and depend on the models these examples
should be mentioned such as:
In which through pathological, reactive calculative proactive and generative steps, the
informed care related and trust related values and safety culture are increased and measured.
patients and staff and this is demonstrated by allotting a day in month, when all the staff and
patients of the health care facility will come together and will share their fundamental, emotional
and social challenges they had to face while working and receiving care respectively.
However, there are several models of safely culture evaluation and depending upon the
research theories, the measurement of safety culture depending evaluation towards the ultimate
completion and on the evaluation through phase, and depend on the models these examples
should be mentioned such as:
In which through pathological, reactive calculative proactive and generative steps, the
informed care related and trust related values and safety culture are increased and measured.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
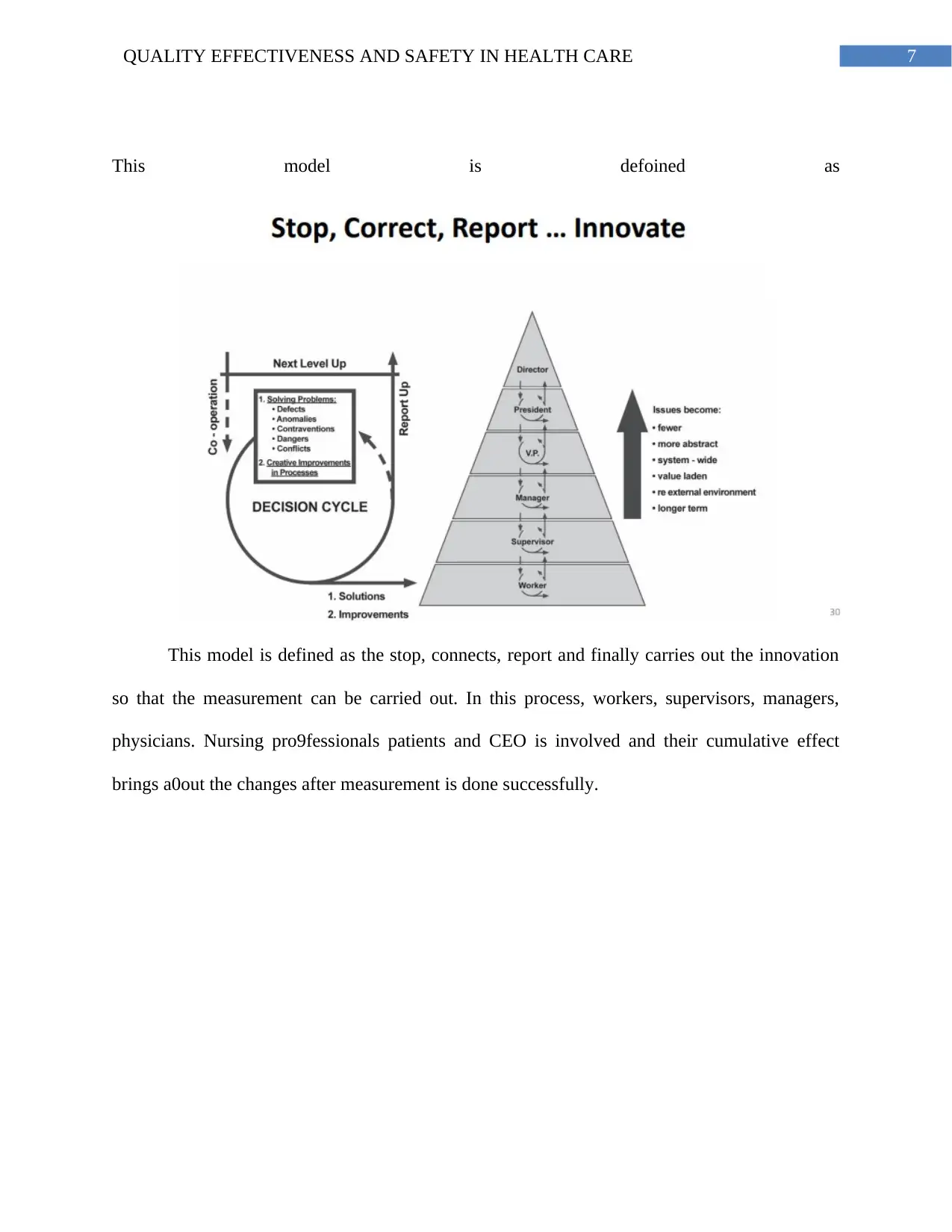
This model is defoined as
This model is defined as the stop, connects, report and finally carries out the innovation
so that the measurement can be carried out. In this process, workers, supervisors, managers,
physicians. Nursing pro9fessionals patients and CEO is involved and their cumulative effect
brings a0out the changes after measurement is done successfully.
This model is defoined as
This model is defined as the stop, connects, report and finally carries out the innovation
so that the measurement can be carried out. In this process, workers, supervisors, managers,
physicians. Nursing pro9fessionals patients and CEO is involved and their cumulative effect
brings a0out the changes after measurement is done successfully.
8QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
References:
Bates, D. W., Saria, S., Ohno-Machado, L., Shah, A., & Escobar, G. (2014). Big data in health
care: using analytics to identify and manage high-risk and high-cost patients. Health
Affairs, 33(7), 1123-1131.
Chartier, Y. (Ed.). (2014). Safe management of wastes from health-care activities. World Health
Organization.
Clement, S. A. (2017). Feasibility of Remote Management of Uncomplicated Urinary Tract
Infection: A Quality Improvement Project.
Dumont, A., Fournier, P., Abrahamowicz, M., Traoré, M., Haddad, S., Fraser, W. D., &
QUARITE Research Group. (2013). Quality of care, risk management, and technology in
obstetrics to reduce hospital-based maternal mortality in Senegal and Mali (QUARITE):
a cluster-randomised trial. The Lancet, 382(9887), 146-157.
Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., ... & Haines, A. (2013). The
effectiveness of mobile-health technology-based health behaviour change or disease
management interventions for health care consumers: a systematic review. PLoS
medicine, 10(1), e1001362.
Gittell, J. H., Godfrey, M., & Thistlethwaite, J. (2013). Interprofessional collaborative practice
and relational coordination: improving healthcare through relationships.
Hunter, C. L., Goodie, J. L., Oordt, M. S., & Dobmeyer, A. C. (2017). Integrated behavioral
health in primary care: Step-by-step guidance for assessment and intervention. American
Psychological Association.
References:
Bates, D. W., Saria, S., Ohno-Machado, L., Shah, A., & Escobar, G. (2014). Big data in health
care: using analytics to identify and manage high-risk and high-cost patients. Health
Affairs, 33(7), 1123-1131.
Chartier, Y. (Ed.). (2014). Safe management of wastes from health-care activities. World Health
Organization.
Clement, S. A. (2017). Feasibility of Remote Management of Uncomplicated Urinary Tract
Infection: A Quality Improvement Project.
Dumont, A., Fournier, P., Abrahamowicz, M., Traoré, M., Haddad, S., Fraser, W. D., &
QUARITE Research Group. (2013). Quality of care, risk management, and technology in
obstetrics to reduce hospital-based maternal mortality in Senegal and Mali (QUARITE):
a cluster-randomised trial. The Lancet, 382(9887), 146-157.
Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., ... & Haines, A. (2013). The
effectiveness of mobile-health technology-based health behaviour change or disease
management interventions for health care consumers: a systematic review. PLoS
medicine, 10(1), e1001362.
Gittell, J. H., Godfrey, M., & Thistlethwaite, J. (2013). Interprofessional collaborative practice
and relational coordination: improving healthcare through relationships.
Hunter, C. L., Goodie, J. L., Oordt, M. S., & Dobmeyer, A. C. (2017). Integrated behavioral
health in primary care: Step-by-step guidance for assessment and intervention. American
Psychological Association.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9QUALITY EFFECTIVENESS AND SAFETY IN HEALTH CARE
Iacob, C., & Constantin, C. (2014). Correlation Analysis of the quality of medical quality
economic and financial management using correlation coefficients based on
nonparametric data.
Iuga, A. O., & McGuire, M. J. (2014). Adherence and health care costs. Risk management and
healthcare policy, 7, 35.
Shekelle, P. G., Wachter, R. M., Pronovost, P. J., Schoelles, K., McDonald, K. M., Dy, S. M., ...
& Larkin, J. W. (2013). Making health care safer II: an updated critical analysis of the
evidence for patient safety practices. Evidence report/technology assessment, (211), 1.
Wager, K. A., Lee, F. W., & Glaser, J. P. (2017). Health care information systems: a practical
approach for health care management. John Wiley & Sons,pp 245
Zornoza, R., Acosta, J. A., Bastida, F., Domínguez, S. G., Toledo, D. M., & Faz, A. (2015).
Identification of sensitive indicators to assess the interrelationship between soil quality,
management practices and human health. Soil, 1(1), 173-185.
Iacob, C., & Constantin, C. (2014). Correlation Analysis of the quality of medical quality
economic and financial management using correlation coefficients based on
nonparametric data.
Iuga, A. O., & McGuire, M. J. (2014). Adherence and health care costs. Risk management and
healthcare policy, 7, 35.
Shekelle, P. G., Wachter, R. M., Pronovost, P. J., Schoelles, K., McDonald, K. M., Dy, S. M., ...
& Larkin, J. W. (2013). Making health care safer II: an updated critical analysis of the
evidence for patient safety practices. Evidence report/technology assessment, (211), 1.
Wager, K. A., Lee, F. W., & Glaser, J. P. (2017). Health care information systems: a practical
approach for health care management. John Wiley & Sons,pp 245
Zornoza, R., Acosta, J. A., Bastida, F., Domínguez, S. G., Toledo, D. M., & Faz, A. (2015).
Identification of sensitive indicators to assess the interrelationship between soil quality,
management practices and human health. Soil, 1(1), 173-185.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




