400846: Leadership Role in Developing a Performance Improvement Plan
VerifiedAdded on 2023/06/11
|16
|4309
|486
Essay
AI Summary
This essay explores the critical role of leadership in developing and implementing a performance improvement plan within the healthcare sector, focusing on patient safety and hygiene. It examines various leadership styles, such as autocratic, participative, delegative, and corporate culture-driven approaches, and their effectiveness in driving change. The essay outlines the steps required to implement improved hand-washing techniques to reduce patient infections, emphasizing the importance of data collection, staff involvement, and education. It also addresses the impact of workplace culture, potential barriers and facilitators in the change process, and management strategies for motivating staff and engaging stakeholders. The significance of benchmarking best practices in patient safety and hygiene is highlighted, emphasizing the leader's responsibility in creating a safe and high-quality care environment. Desklib offers a platform for students to access this essay and other resources to aid in their studies.

Running head: LEADERSHIP ROLE 1
Leadership Role in Developing a Performance Improvement Plan
Name
Institution
Leadership Role in Developing a Performance Improvement Plan
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LEADERSHIP ROLE 2
Leadership Role in Developing a Performance Improvement Plan
It is no doubt that there has been an increased need for a quality and performance
improvement in the healthcare industry across the globe for the last couple of decades now.
Apparently, the safety of an individual patient in the healthcare industry is a huge determinant of
quality of care and therefore emerges as one of the main priority of any healthcare organization
(Edwards, 2017). In this light, patient safety is often taken to be a rather heart of healthcare
practice as well as nursing throughout the entire history of medicine. Nonetheless, there are those
nondeliberate accidents that often occur to patients and should never be overlooked. One of the
safety cares is the prevention of infection and many hospitals have taken various initiatives to
make sure that there are minimum infections in their patients. In essence, the joint commission
has as well listed this practice as one of the national patient goals in every healthcare facility
particularly in Australia (Engle et al., 217). Under this focus, there is a need to improve the
overall hygiene particularly hands hygiene through the use of clean guidelines that comes from
the Centres for Disease Control and Prevention also referred to as the World Health
Organization. With the increase of patient infections in hospitals, it is quite evident that
healthcare workers often fail to consistently wash their hands either before or rathe after caring
for a particular patient. This has become one of the main causes of patient infections and needs to
be resolved across the healthcare industry.
Primarily, cleaning of hands is no doubt one of the most effective measures of preventing
and minimizing the overall transmission of healthcare-related infections. Essentially, the practice
of hands cleaning across the healthcare present an important apprehension especially in patient’s
safety as a result of ever-increasing rates of Clostridium difficile in hospitals. Apparently, such
bacterium infection is difficult to do away with by the use of antiseptic hand preparation.
Leadership Role in Developing a Performance Improvement Plan
It is no doubt that there has been an increased need for a quality and performance
improvement in the healthcare industry across the globe for the last couple of decades now.
Apparently, the safety of an individual patient in the healthcare industry is a huge determinant of
quality of care and therefore emerges as one of the main priority of any healthcare organization
(Edwards, 2017). In this light, patient safety is often taken to be a rather heart of healthcare
practice as well as nursing throughout the entire history of medicine. Nonetheless, there are those
nondeliberate accidents that often occur to patients and should never be overlooked. One of the
safety cares is the prevention of infection and many hospitals have taken various initiatives to
make sure that there are minimum infections in their patients. In essence, the joint commission
has as well listed this practice as one of the national patient goals in every healthcare facility
particularly in Australia (Engle et al., 217). Under this focus, there is a need to improve the
overall hygiene particularly hands hygiene through the use of clean guidelines that comes from
the Centres for Disease Control and Prevention also referred to as the World Health
Organization. With the increase of patient infections in hospitals, it is quite evident that
healthcare workers often fail to consistently wash their hands either before or rathe after caring
for a particular patient. This has become one of the main causes of patient infections and needs to
be resolved across the healthcare industry.
Primarily, cleaning of hands is no doubt one of the most effective measures of preventing
and minimizing the overall transmission of healthcare-related infections. Essentially, the practice
of hands cleaning across the healthcare present an important apprehension especially in patient’s
safety as a result of ever-increasing rates of Clostridium difficile in hospitals. Apparently, such
bacterium infection is difficult to do away with by the use of antiseptic hand preparation.
LEADERSHIP ROLE 3
Additionally, this ailment has indicated that it can indeed be a detrimental especially to a patient
in the healthcare establishments across the globe. Notably, such organism is known to produce
spores that are only removable by a rather proper hygiene which is through the use of soap as
well as water. In this light, there are plenty of methods that can be used to remove and reduce the
level of infections that are caused by these organisms. Such preventative measures include
infection control measures, hand washing as well as environmental decontamination. This paper
intends to focus on the role of the leader in this particular improvement, the type of leadership
style that effect change, the steps required to implement this aspect of workplace performance,
the overall impact of the workplace culture, the main barriers and facilitators in the change
process and management strategies, the importance of benchmarking best practices related to
patient safety, and strategies for motivating an engaging stakeholders or the staff in performance
improvement.
The Role of the Leader in Patient Safety Performance Improvement
In essence, leaders in the healthcare industry are granted a legal as well as a moral
obligation of ensuring that there is a high-quality patient care and to focus on the overall
improvement of patient care. In this light, the main priorities of leaders in healthcare firms are to
be accountable for a particular effective care while still protecting the entire components that
constitute to the overall patient care not forgetting that of its employees (Bogner, 2018). The art
of a set of thoughtful as well as competent leaders is to make sure that they contribute to the
improvement in the firm’s culture and safety. Such leaders are always aware that there can be the
existence of systemic flaws and therefore each procedure in the healthcare industry has a
potential of failing because of hazards and weakness. It is, therefore, the role of these leaders to
identify the existing problems and make sure that they find a meaningful solution before patients
Additionally, this ailment has indicated that it can indeed be a detrimental especially to a patient
in the healthcare establishments across the globe. Notably, such organism is known to produce
spores that are only removable by a rather proper hygiene which is through the use of soap as
well as water. In this light, there are plenty of methods that can be used to remove and reduce the
level of infections that are caused by these organisms. Such preventative measures include
infection control measures, hand washing as well as environmental decontamination. This paper
intends to focus on the role of the leader in this particular improvement, the type of leadership
style that effect change, the steps required to implement this aspect of workplace performance,
the overall impact of the workplace culture, the main barriers and facilitators in the change
process and management strategies, the importance of benchmarking best practices related to
patient safety, and strategies for motivating an engaging stakeholders or the staff in performance
improvement.
The Role of the Leader in Patient Safety Performance Improvement
In essence, leaders in the healthcare industry are granted a legal as well as a moral
obligation of ensuring that there is a high-quality patient care and to focus on the overall
improvement of patient care. In this light, the main priorities of leaders in healthcare firms are to
be accountable for a particular effective care while still protecting the entire components that
constitute to the overall patient care not forgetting that of its employees (Bogner, 2018). The art
of a set of thoughtful as well as competent leaders is to make sure that they contribute to the
improvement in the firm’s culture and safety. Such leaders are always aware that there can be the
existence of systemic flaws and therefore each procedure in the healthcare industry has a
potential of failing because of hazards and weakness. It is, therefore, the role of these leaders to
identify the existing problems and make sure that they find a meaningful solution before patients
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LEADERSHIP ROLE 4
are affected. Latent hazards that healthcare leaders can solve include poor design, lack of overall
supervision of medical works as well as manufacturing or rather maintenance defects. in this
context, leaders can, therefore, make sure that there is a clear and thorough supervision of
workers in the healthcare facilities to ensure that patients are safeguarded from any infections
and that they are given a reputable healthcare services all through their recovery process.
Leaders are therefore called to the creation and an apparent maintenance of a culture of
safety towards their patients and their workers. Leaders supposed to be committed to the creation
of a safe environment to the patient as this is equally important to the whole resources that have
been injected in the firm. The commitment by leaders to maintain a safe environment and
conditions to the patient is often measured by what they do instead of what they normally say
should be done. Beyond healthcare, there is an apparent and clear evidence of leadership impact
on the safety of workplace (Sherwood & Barnsteiner, J2017). Noteworthy, there are indeed non-
empirical articles that provide a proposition as well as a description on the attitude of leadership
and efforts of safety improvement within the literature on healthcare.
Leaders have the attribute of recognizing rather good catches in which a particular
adverse event can be avoided in the hospitals and therefore share these thoughts with the entire
team members in the healthcare facility. There are therefore important ways in which these set of
leaders can report back to the team members who tend to raise safety issues in the hospital. Some
of these methods are through a shift of the overall unit huddles as well as the visual management
borders. In this manner, there is a need for the concentration of a high-quality leadership
attributes to foster a safety environmental care in the healthcare industry and particularly the
overall hygiene of a particular patient in the hospital.
are affected. Latent hazards that healthcare leaders can solve include poor design, lack of overall
supervision of medical works as well as manufacturing or rather maintenance defects. in this
context, leaders can, therefore, make sure that there is a clear and thorough supervision of
workers in the healthcare facilities to ensure that patients are safeguarded from any infections
and that they are given a reputable healthcare services all through their recovery process.
Leaders are therefore called to the creation and an apparent maintenance of a culture of
safety towards their patients and their workers. Leaders supposed to be committed to the creation
of a safe environment to the patient as this is equally important to the whole resources that have
been injected in the firm. The commitment by leaders to maintain a safe environment and
conditions to the patient is often measured by what they do instead of what they normally say
should be done. Beyond healthcare, there is an apparent and clear evidence of leadership impact
on the safety of workplace (Sherwood & Barnsteiner, J2017). Noteworthy, there are indeed non-
empirical articles that provide a proposition as well as a description on the attitude of leadership
and efforts of safety improvement within the literature on healthcare.
Leaders have the attribute of recognizing rather good catches in which a particular
adverse event can be avoided in the hospitals and therefore share these thoughts with the entire
team members in the healthcare facility. There are therefore important ways in which these set of
leaders can report back to the team members who tend to raise safety issues in the hospital. Some
of these methods are through a shift of the overall unit huddles as well as the visual management
borders. In this manner, there is a need for the concentration of a high-quality leadership
attributes to foster a safety environmental care in the healthcare industry and particularly the
overall hygiene of a particular patient in the hospital.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LEADERSHIP ROLE 5
It is therefore evident that the art of leadership in the contemporary healthcare industry
has turned out to be a rather complex responsibility. Despite the importance of a quality and
mindful leadership in a particular organization it is important to put more attention to what these
set of leaders are contributing to the sustainability of a safer patient environment. In this regards,
understanding the role of leadership and the impact they could bring to a particular organization
needs a detailed knowledge on the way leaders and leadership system is capable of shaping a
firm’s strategy and behavior towards an improvement of patient care.
The Type(S) Of Leadership Style(S) That Can Effect Change
The debate on the overall impact of leadership styles in various business organizations
and particularly in the healthcare sector has been a debated issue for the past couple of decades
now. Apparently, the kind of style that is incorporated to any particular organization often affect
everyone in that firm right from the senior leadership to the intern in a placement. These styles
are fond of creating a certain culture that influences the organization and its overall performance.
Some of the leadership styles that are tipped to influence change in any given health institutions
include:
Autocratic Style Effects
Primarily, this type of leadership is also known as the authoritarian style and it clearly
defines the overall division that lies between the leaders and the entire set or workers.
Apparently, this type of style requires a rather little involvement from the employees in a given
organization. In this regards, leaders involved in this type of style are often very comfortable
with every decision making steps regarding a certain plan or project. However, research indicates
that this type of leadership style does not encourage innovativeness something that the
contemporary world puts a lot of emphasis on. Nonetheless, this style is useful when there is a
It is therefore evident that the art of leadership in the contemporary healthcare industry
has turned out to be a rather complex responsibility. Despite the importance of a quality and
mindful leadership in a particular organization it is important to put more attention to what these
set of leaders are contributing to the sustainability of a safer patient environment. In this regards,
understanding the role of leadership and the impact they could bring to a particular organization
needs a detailed knowledge on the way leaders and leadership system is capable of shaping a
firm’s strategy and behavior towards an improvement of patient care.
The Type(S) Of Leadership Style(S) That Can Effect Change
The debate on the overall impact of leadership styles in various business organizations
and particularly in the healthcare sector has been a debated issue for the past couple of decades
now. Apparently, the kind of style that is incorporated to any particular organization often affect
everyone in that firm right from the senior leadership to the intern in a placement. These styles
are fond of creating a certain culture that influences the organization and its overall performance.
Some of the leadership styles that are tipped to influence change in any given health institutions
include:
Autocratic Style Effects
Primarily, this type of leadership is also known as the authoritarian style and it clearly
defines the overall division that lies between the leaders and the entire set or workers.
Apparently, this type of style requires a rather little involvement from the employees in a given
organization. In this regards, leaders involved in this type of style are often very comfortable
with every decision making steps regarding a certain plan or project. However, research indicates
that this type of leadership style does not encourage innovativeness something that the
contemporary world puts a lot of emphasis on. Nonetheless, this style is useful when there is a
LEADERSHIP ROLE 6
need for an urgent decision making in a certain organization as it does not involve complex
process and avoids employee involvement who may be opposed to a particular decision made.
Participative Leadership Effects
In essence, this leadership style is also called the Democratic leadership attribute and is
usually considered as the best option in various companies. Apparently, this style is as well
considered to be the opposite of the autocratic leadership as leaders make decisions and still
accepts inputs from the employee regarding decision making and any other process in a
particular organization. In this way, leaders reserve the overall rights of arriving at the final
decision while still encouraging feedbacks as well as ideas from all the employees. These types
of leaders are always tipped to have more content workforce because each individual has at least
input into the decision making.
Delegative Leadership Effects
This kind of leadership is considered by many people to be the least effective option of
leadership style in the managerial world. Contrary to other managerial styles, this kind of method
of leadership does not make a decision but rather leaves a particular group with the duty of
deciding what to do regarding a certain plan or process. These leaders do not often give guidance
to the workers but instead decides to leave this part to the trusted members of a certain group
(Shanafelt & Noseworthy, 2017).
Corporate Culture Effects
This managerial leadership style is also referred to as the organizational culture and
therefore all things done is defined by the cooperate culture. Apparently, the leadership style in
this context has often a strong impact on the cooperate culture, therefore, making employees to
need for an urgent decision making in a certain organization as it does not involve complex
process and avoids employee involvement who may be opposed to a particular decision made.
Participative Leadership Effects
In essence, this leadership style is also called the Democratic leadership attribute and is
usually considered as the best option in various companies. Apparently, this style is as well
considered to be the opposite of the autocratic leadership as leaders make decisions and still
accepts inputs from the employee regarding decision making and any other process in a
particular organization. In this way, leaders reserve the overall rights of arriving at the final
decision while still encouraging feedbacks as well as ideas from all the employees. These types
of leaders are always tipped to have more content workforce because each individual has at least
input into the decision making.
Delegative Leadership Effects
This kind of leadership is considered by many people to be the least effective option of
leadership style in the managerial world. Contrary to other managerial styles, this kind of method
of leadership does not make a decision but rather leaves a particular group with the duty of
deciding what to do regarding a certain plan or process. These leaders do not often give guidance
to the workers but instead decides to leave this part to the trusted members of a certain group
(Shanafelt & Noseworthy, 2017).
Corporate Culture Effects
This managerial leadership style is also referred to as the organizational culture and
therefore all things done is defined by the cooperate culture. Apparently, the leadership style in
this context has often a strong impact on the cooperate culture, therefore, making employees to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LEADERSHIP ROLE 7
do things that reflects their leaders. Additionally, staff often aims at pleasing the management
and the supervisors while doing their daily duties.
The Steps Required (And Their Relevant Change Theory Support) To Implement This
Aspect of Workplace Performance
Noteworthy, to initiate a better hand washing technique in any health care facility to
reduce the level of patient infections effectively requires a proper assessment in determining the
best learning style. Apparently, there should be a relevant collection of data procedure in
determining and supporting a proposed solution. In this way, the Joint Commission (JC) have for
long suggested that:
One should understand the importance of investigating an apparent reason for the
increased of non-adherence to the guidelines surrounding the patient hygiene before kick-
starting an improvement plan. In this regards, it is possible to determine whether the
adherence is affected by the organization physical facility in making a certain product
available or rather the level of accountability among the workers.
It is therefore important to note the effect of a patient acquiring a certain infection as it may lead
to overstay in the hospital (Flin & O'Connor, 2017). Additionally, there would be an increase in
the hours of patient care required by the staff member, therefore, increasing the hospitalization
cost in the long run. This, therefore, triggers the importance of informing the healthcare workers
of the effect of an increased operational cost.
After analyzing the needs and assessment plan, the health care leadership should then
conduct a meeting involving the safety committee to enable a viable discussion while supporting
data collection that would facilitate the implementation of the hand hygiene. With the acquired
do things that reflects their leaders. Additionally, staff often aims at pleasing the management
and the supervisors while doing their daily duties.
The Steps Required (And Their Relevant Change Theory Support) To Implement This
Aspect of Workplace Performance
Noteworthy, to initiate a better hand washing technique in any health care facility to
reduce the level of patient infections effectively requires a proper assessment in determining the
best learning style. Apparently, there should be a relevant collection of data procedure in
determining and supporting a proposed solution. In this way, the Joint Commission (JC) have for
long suggested that:
One should understand the importance of investigating an apparent reason for the
increased of non-adherence to the guidelines surrounding the patient hygiene before kick-
starting an improvement plan. In this regards, it is possible to determine whether the
adherence is affected by the organization physical facility in making a certain product
available or rather the level of accountability among the workers.
It is therefore important to note the effect of a patient acquiring a certain infection as it may lead
to overstay in the hospital (Flin & O'Connor, 2017). Additionally, there would be an increase in
the hours of patient care required by the staff member, therefore, increasing the hospitalization
cost in the long run. This, therefore, triggers the importance of informing the healthcare workers
of the effect of an increased operational cost.
After analyzing the needs and assessment plan, the health care leadership should then
conduct a meeting involving the safety committee to enable a viable discussion while supporting
data collection that would facilitate the implementation of the hand hygiene. With the acquired
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LEADERSHIP ROLE 8
data the committee would then suggest various solutions that might fit the current problem in the
healthcare organization.
The organizers of the meetings should make sure that the proposed solutions are
conveyed to the general staff in rather clear as well as honest manner. Essentially, in case the
hand hygiene program is accepted by the majority of the participant then there is a need for a fro
planning for an educational meeting to enable the discussion of the process of infection,
transmission, the protection of patient and employees, and a proper technique for making sure
that the hands are clean. The staff is then required to observe a proper hand washing method
following the educational meeting. In this light, the required supplies and equipment’s include
sinks, a germ kit, clean water, and a paper towels (Rothwell, Hohne, & King, 2018).
Participative leadership should be used by the nurse leader to make sure that the change
is implemented. In this regards, there is an aspect of assuming that a particular change can be
effected by providing new knowledge that can result in a rather positive attitude. Apparently, this
is because the entire participants are given the chance of giving in the ideas as well as supporting
new ideas (Mathews et al., 2017). The leadership is often tipped to contain empirical-rational as
well as a normative strategy. The nurse leader should then come up with a way of making sure
that a committee is set to implement a detailed protocol for the hand washing program for the
improvement of the overall hygiene.
Change Theory
According to Anders and Hawkins (2006), Lippitt articulates that there is an important
emphasis on an active participation by a key section of a given member of a system in the entire
process of change. This theory, therefore, establishes the basis for the apparent development of a
set staff member and committee in the implementation of the approved solution. With this kind
data the committee would then suggest various solutions that might fit the current problem in the
healthcare organization.
The organizers of the meetings should make sure that the proposed solutions are
conveyed to the general staff in rather clear as well as honest manner. Essentially, in case the
hand hygiene program is accepted by the majority of the participant then there is a need for a fro
planning for an educational meeting to enable the discussion of the process of infection,
transmission, the protection of patient and employees, and a proper technique for making sure
that the hands are clean. The staff is then required to observe a proper hand washing method
following the educational meeting. In this light, the required supplies and equipment’s include
sinks, a germ kit, clean water, and a paper towels (Rothwell, Hohne, & King, 2018).
Participative leadership should be used by the nurse leader to make sure that the change
is implemented. In this regards, there is an aspect of assuming that a particular change can be
effected by providing new knowledge that can result in a rather positive attitude. Apparently, this
is because the entire participants are given the chance of giving in the ideas as well as supporting
new ideas (Mathews et al., 2017). The leadership is often tipped to contain empirical-rational as
well as a normative strategy. The nurse leader should then come up with a way of making sure
that a committee is set to implement a detailed protocol for the hand washing program for the
improvement of the overall hygiene.
Change Theory
According to Anders and Hawkins (2006), Lippitt articulates that there is an important
emphasis on an active participation by a key section of a given member of a system in the entire
process of change. This theory, therefore, establishes the basis for the apparent development of a
set staff member and committee in the implementation of the approved solution. With this kind
LEADERSHIP ROLE 9
of theory, there is a room of involving the staff and allow them to make a contribution to a
solution that can be accepted by their co-workers. Additionally, there is the likelihood of peer
motivation and an apparent role modeling for a rather long-term compliance.
The Impact of the Workplace Culture
In many instances, a certain organization culture is responsible for providing the overall
framework with respect to the workers' behaviors in their respective workplaces, particularly in
the healthcare industry. Apparently, an organizational culture can, therefore, impact the
employees’ performance either negatively or positively. A particular healthcare organization in
which the workers are considered as the main part of the growth process often encourages the
employees’ commitment towards the goal of the selected healthcare institution. Additionally,
these set of employees often align their goals as well as objects to fit those of the companies they
work in and therefore feel much responsible of the entire well-being of the firm (Frankel &
PGCMS, 2018). Noteworthy, they feel satisfied with their role and work in a certain organization
when their efforts are rewarded and appreciated by the management. In such environment, an
employee is always committed to attaining their goals and therefore poses a positive effect on the
performance particularly of service delivery to the patients.
To a larger extent, the overall performance of a particular set of workers is determined by
the available organization culture. It is, therefore, the ultimate interest of any organization to
make sure that it has eliminated all possible negative factors that can lead to lower performance
deliverance by the employees. This always fosters a positive workplace environment and thus
facilitates a safety patient adherence by the workers in a particular healthcare organization.
of theory, there is a room of involving the staff and allow them to make a contribution to a
solution that can be accepted by their co-workers. Additionally, there is the likelihood of peer
motivation and an apparent role modeling for a rather long-term compliance.
The Impact of the Workplace Culture
In many instances, a certain organization culture is responsible for providing the overall
framework with respect to the workers' behaviors in their respective workplaces, particularly in
the healthcare industry. Apparently, an organizational culture can, therefore, impact the
employees’ performance either negatively or positively. A particular healthcare organization in
which the workers are considered as the main part of the growth process often encourages the
employees’ commitment towards the goal of the selected healthcare institution. Additionally,
these set of employees often align their goals as well as objects to fit those of the companies they
work in and therefore feel much responsible of the entire well-being of the firm (Frankel &
PGCMS, 2018). Noteworthy, they feel satisfied with their role and work in a certain organization
when their efforts are rewarded and appreciated by the management. In such environment, an
employee is always committed to attaining their goals and therefore poses a positive effect on the
performance particularly of service delivery to the patients.
To a larger extent, the overall performance of a particular set of workers is determined by
the available organization culture. It is, therefore, the ultimate interest of any organization to
make sure that it has eliminated all possible negative factors that can lead to lower performance
deliverance by the employees. This always fosters a positive workplace environment and thus
facilitates a safety patient adherence by the workers in a particular healthcare organization.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LEADERSHIP ROLE 10
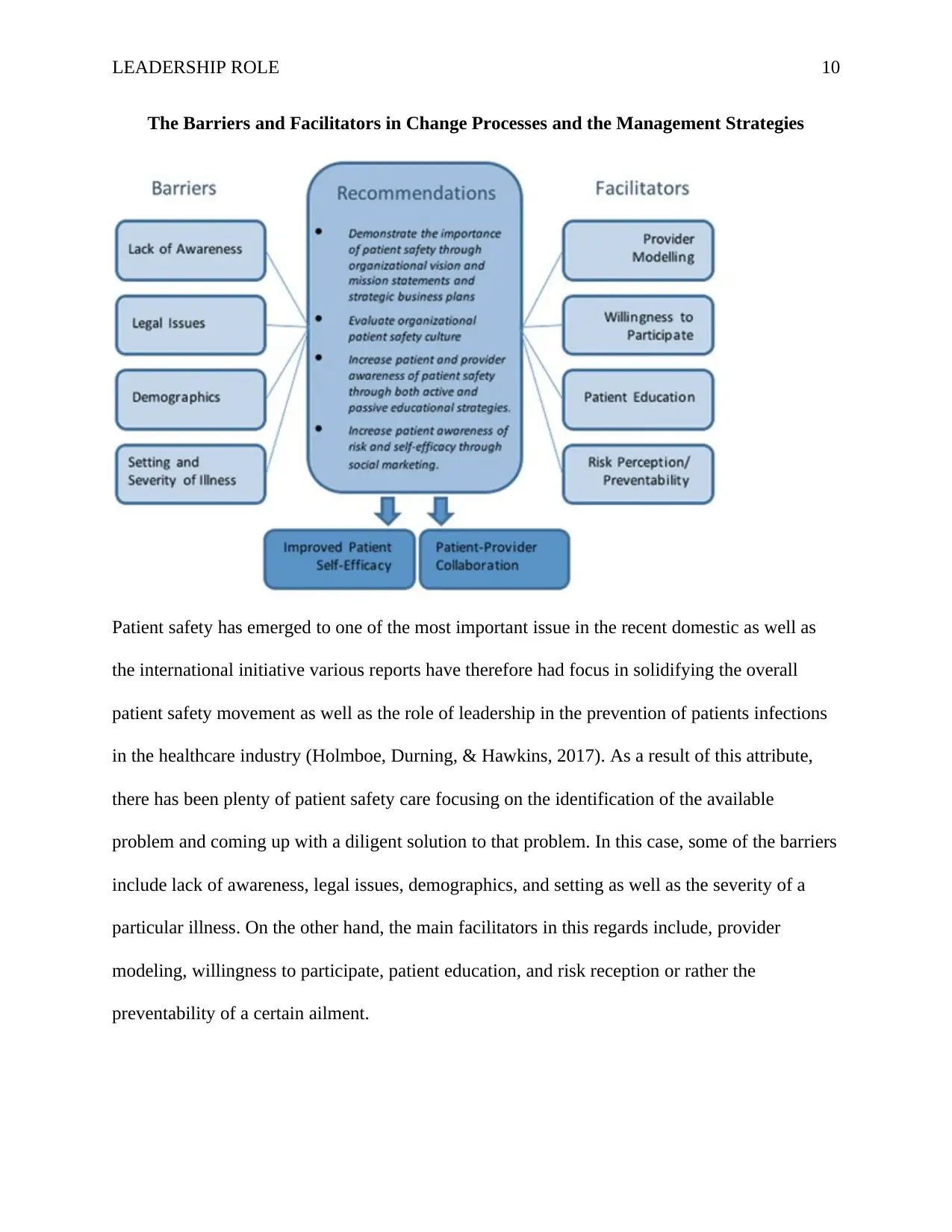
The Barriers and Facilitators in Change Processes and the Management Strategies
Patient safety has emerged to one of the most important issue in the recent domestic as well as
the international initiative various reports have therefore had focus in solidifying the overall
patient safety movement as well as the role of leadership in the prevention of patients infections
in the healthcare industry (Holmboe, Durning, & Hawkins, 2017). As a result of this attribute,
there has been plenty of patient safety care focusing on the identification of the available
problem and coming up with a diligent solution to that problem. In this case, some of the barriers
include lack of awareness, legal issues, demographics, and setting as well as the severity of a
particular illness. On the other hand, the main facilitators in this regards include, provider
modeling, willingness to participate, patient education, and risk reception or rather the
preventability of a certain ailment.
The Barriers and Facilitators in Change Processes and the Management Strategies
Patient safety has emerged to one of the most important issue in the recent domestic as well as
the international initiative various reports have therefore had focus in solidifying the overall
patient safety movement as well as the role of leadership in the prevention of patients infections
in the healthcare industry (Holmboe, Durning, & Hawkins, 2017). As a result of this attribute,
there has been plenty of patient safety care focusing on the identification of the available
problem and coming up with a diligent solution to that problem. In this case, some of the barriers
include lack of awareness, legal issues, demographics, and setting as well as the severity of a
particular illness. On the other hand, the main facilitators in this regards include, provider
modeling, willingness to participate, patient education, and risk reception or rather the
preventability of a certain ailment.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LEADERSHIP ROLE 11
Barriers
Lack of awareness, in essence, lack of awareness is cited as one of the main barriers to
the patient engagement as well as patient safety practices. Apparently, the overall lack of a
detailed understanding of what patient safety engagement has become a problem especially in
the provision of the hygienic environment by health care workers across the globe and
particularly in Australia.
Demographics primarily, recent researches have indicated some of the effects patient
demographic factors can have on the prevention strategies of infections. In this way, most of the
health workers do not have the required knowledge of the composition of the patient population
and therefore cannot come up with a decisive solution to a certain infection.
Legality There has been an increasing uncertainty regarding the overall patient
involvement in their own care as well as error prevention of infections in the healthcare system.
Apparently, this has led to the change in the responsibility of both the patient and the healthcare
providers.
Health care settings and illness It is no doubt that the setting, as well as the nature of a
particular disease, can hugely impact the way patients are supposed to be engaged in the error
prevention strategies.
Facilitators
Provide modeling one of the main facilitators towards a successful patient engagement is
to come up with a suitable provider behavior and physician modeling. In this case, patients are
often opposed to those behaviors that are perceived to be challenging as well as confrontational.
Barriers
Lack of awareness, in essence, lack of awareness is cited as one of the main barriers to
the patient engagement as well as patient safety practices. Apparently, the overall lack of a
detailed understanding of what patient safety engagement has become a problem especially in
the provision of the hygienic environment by health care workers across the globe and
particularly in Australia.
Demographics primarily, recent researches have indicated some of the effects patient
demographic factors can have on the prevention strategies of infections. In this way, most of the
health workers do not have the required knowledge of the composition of the patient population
and therefore cannot come up with a decisive solution to a certain infection.
Legality There has been an increasing uncertainty regarding the overall patient
involvement in their own care as well as error prevention of infections in the healthcare system.
Apparently, this has led to the change in the responsibility of both the patient and the healthcare
providers.
Health care settings and illness It is no doubt that the setting, as well as the nature of a
particular disease, can hugely impact the way patients are supposed to be engaged in the error
prevention strategies.
Facilitators
Provide modeling one of the main facilitators towards a successful patient engagement is
to come up with a suitable provider behavior and physician modeling. In this case, patients are
often opposed to those behaviors that are perceived to be challenging as well as confrontational.
LEADERSHIP ROLE 12
Perception and risk preventability making patient aware of the possible risks they are
likely to face because of certain actions and preventative issues can be one of the most
encouraging as well as facilitators in finding a viable solution in patient care.
Willingness to participate the general interest by the patient in engaging in a particular
preventative measure can be considered to be one of the main facilitators in the creation of a
suitable strategy of safety improvement.
Patient education it is definitely crucial for any health care organization to set aside a
program that would ensure that is a vibrant patient education regarding a certain illness and how
it can be prevented. This is a good way of ensuring that patients are aware of the risks they might
be involved in.
The Importance of Benchmarking Best Practice Related To Patient Safety Performance
Improvement
Primarily, it is always important of any organization particularly the healthcare industry
introduce a strategy that engages all the stakeholders in with an aim of providing a technique that
would improve the safety and quality of patient care. In the healthcare settings as it involves not
only the care providers but also the patient. Additionally, this method encourages innovation as it
involves incorporation of various ideas from other healthcare institutions (Hollnagel, 2017).
Strategies for Motivating and Engaging the Stakeholders/Staff in the Performance
Improvement at All Stages
In the current business world where the nature of the market is defined by the level of
competition, there is a need to come up with a better way of motivating and engaging
stakeholders in your business particularly in the healthcare sector. The following are the main
ways of encouraging stakeholders’ engagement in an institution (Jorsal et al., 2017).
Perception and risk preventability making patient aware of the possible risks they are
likely to face because of certain actions and preventative issues can be one of the most
encouraging as well as facilitators in finding a viable solution in patient care.
Willingness to participate the general interest by the patient in engaging in a particular
preventative measure can be considered to be one of the main facilitators in the creation of a
suitable strategy of safety improvement.
Patient education it is definitely crucial for any health care organization to set aside a
program that would ensure that is a vibrant patient education regarding a certain illness and how
it can be prevented. This is a good way of ensuring that patients are aware of the risks they might
be involved in.
The Importance of Benchmarking Best Practice Related To Patient Safety Performance
Improvement
Primarily, it is always important of any organization particularly the healthcare industry
introduce a strategy that engages all the stakeholders in with an aim of providing a technique that
would improve the safety and quality of patient care. In the healthcare settings as it involves not
only the care providers but also the patient. Additionally, this method encourages innovation as it
involves incorporation of various ideas from other healthcare institutions (Hollnagel, 2017).
Strategies for Motivating and Engaging the Stakeholders/Staff in the Performance
Improvement at All Stages
In the current business world where the nature of the market is defined by the level of
competition, there is a need to come up with a better way of motivating and engaging
stakeholders in your business particularly in the healthcare sector. The following are the main
ways of encouraging stakeholders’ engagement in an institution (Jorsal et al., 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




