Importance of Leadership Style on Healthcare Quality: A Review
VerifiedAdded on 2022/11/15
|17
|9111
|169
Report
AI Summary
This systematic review, published in Healthcare (2017), examines the association between various leadership styles and healthcare quality measures. The study, based on Medline and EMBASE databases from 2004 to 2015, analyzed eighteen relevant articles. The review highlights the strong correlation between leadership styles, including transformational and transactional approaches, and quality of care, emphasizing leadership's crucial role in coordinating and integrating care for both patients and healthcare professionals. The research identifies key quality measures such as patient satisfaction, reduced adverse effects, and improved patient outcomes, underscoring the importance of effective leadership in establishing high-productivity, high-quality healthcare organizations. The review also discusses the characteristics of high-quality care (safe, effective, reliable, patient-centered, efficient, and equitable) and the impact of leadership on these elements. The study's findings suggest that leadership styles significantly influence patient outcomes and overall healthcare quality, thereby contributing to the ongoing discourse on evidence-based medicine and nursing.

healthcare
Review
Importance of Leadership Style towards Quality of
Care Measures in Healthcare Settings:
A Systematic Review
Danae F. Sfantou1,†, Aggelos Laliotis2,† ID , Athina E. Patelarou3, Dimitra Sifaki- Pistolla4,
Michail Matalliotakis5 ID and Evridiki Patelarou6,*
1 2nd Department of Cardiology, Attikon University Hospital, National and Kapodistrian University of
Athens Medical School, Athens 12462, Greece; danaes230@gmail.com
2 Department of Upper Gastrointestinal and Bariatric Surgery, St. Georges, NHS Foundation Hospitals,
London SE170QT, UK; laliotisac@gmail.com
3 Department of Anesthesiology, University Hospital of Heraklion, Crete 71500, Greece;
athina.patelarou@gmail.com
4 Clinic of Social and Family Medicine, School of Medicine, University of Crete, Crete 71500, Greece;
spdimi11@gmail.com
5 Department of Obstretics and Gynaecology, Venizeleio General Hospital, Heraklion, 71409, Greece;
mihalismat@hotmail.com
6 Florence Nightingale Faculty of Nursing and Midwifery, King’s College, London SE18WA, UK
* Correspondence: evridiki.patelarou@kcl.ac.uk; Tel.: +44-7596-434-780
† These authors have equally contributed to the manuscript.
Academic Editor: Sampath Parthasarathy
Received: 1 August 2017; Accepted: 25 September 2017; Published: 14 October 2017
Abstract:Effective leadership of healthcare professionals is critical for strengthening quality and
integration of care. This study aimed to assess whether there exist an association between different
leadership styles and healthcare quality measures.The search was performed in the Medline
(NationalLibrary of Medicine,PubMed interface) and EMBASE databases for the time period
2004–2015. The research question that guided this review was posed as: “Is there any relationship
between leadership style in healthcare settings and quality of care?” Eighteen articles were found
relevant to our research question. Leadership styles were found to be strongly correlated with quality
care and associated measures. Leadership was considered a core element for a well-coordinated and
integrated provision of care, both from the patients and healthcare professionals.
Keywords: leadership; leadership style; quality of care; nursing
Review
Importance of Leadership Style towards Quality of
Care Measures in Healthcare Settings:
A Systematic Review
Danae F. Sfantou1,†, Aggelos Laliotis2,† ID , Athina E. Patelarou3, Dimitra Sifaki- Pistolla4,
Michail Matalliotakis5 ID and Evridiki Patelarou6,*
1 2nd Department of Cardiology, Attikon University Hospital, National and Kapodistrian University of
Athens Medical School, Athens 12462, Greece; danaes230@gmail.com
2 Department of Upper Gastrointestinal and Bariatric Surgery, St. Georges, NHS Foundation Hospitals,
London SE170QT, UK; laliotisac@gmail.com
3 Department of Anesthesiology, University Hospital of Heraklion, Crete 71500, Greece;
athina.patelarou@gmail.com
4 Clinic of Social and Family Medicine, School of Medicine, University of Crete, Crete 71500, Greece;
spdimi11@gmail.com
5 Department of Obstretics and Gynaecology, Venizeleio General Hospital, Heraklion, 71409, Greece;
mihalismat@hotmail.com
6 Florence Nightingale Faculty of Nursing and Midwifery, King’s College, London SE18WA, UK
* Correspondence: evridiki.patelarou@kcl.ac.uk; Tel.: +44-7596-434-780
† These authors have equally contributed to the manuscript.
Academic Editor: Sampath Parthasarathy
Received: 1 August 2017; Accepted: 25 September 2017; Published: 14 October 2017
Abstract:Effective leadership of healthcare professionals is critical for strengthening quality and
integration of care. This study aimed to assess whether there exist an association between different
leadership styles and healthcare quality measures.The search was performed in the Medline
(NationalLibrary of Medicine,PubMed interface) and EMBASE databases for the time period
2004–2015. The research question that guided this review was posed as: “Is there any relationship
between leadership style in healthcare settings and quality of care?” Eighteen articles were found
relevant to our research question. Leadership styles were found to be strongly correlated with quality
care and associated measures. Leadership was considered a core element for a well-coordinated and
integrated provision of care, both from the patients and healthcare professionals.
Keywords: leadership; leadership style; quality of care; nursing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare 2017, 5, 73 2 of 17
In transactional leadership the leader acts as a manager of change, making exchanges with employees
that lead to an improvement in production [3]. An autocratic leadership style is considered ideal
in emergencies situation as the leader makes all decisions without taking into account the opinion
of staff. Moreover,mistakes are not tolerated within the blame put on individuals.In contrary,
the laissez-faire leadership style involves a leader who does not make decisions, staff acts without
direction or supervision but there is a hands-off approach resulting in rare changes [4]. Task-oriented
leadership style involves planning of work activities, clarification of roles within a team or a group
of people, objectives set as well as the continuing monitoring and performance of processes. Lastly,
relationship-oriented leadership style incorporates support, development and recognition [ 5].
Quality of care is a vitalelementfor achieving high productivity levels within healthcare
organizations, and is defined as the degree to which the probability of achieving the expected health
outcomes is increased and in line with updated professional knowledge and skills within health
services [6]. The Institute of Medicine OM has described six characteristics of high-quality care
that must be:(1) safe,(2) effective,(3) reliable,(4) patient-centred,(5) efficient,and (6) equitable.
Measuring health outcomes is a core component of assessing quality of care.Quality measures
are: structure,process,outcome,and patient satisfaction [6]. According to the National Quality
Measures Clearing House (USA), a clinical outcome refers to the health state of a patient resulting
from healthcare. Measures on patient outcomes and satisfaction constitute: shorter patient length of
stay, hospital mortality level, health care-associated infections, failure to rescue ratio, restraint use,
medication errors, inadequate pain management, pressure ulcers rate, patient fall rate, falls with injury,
medical errors, and urinary tract infections [7].
There are numerous publications recognizing leadership style as a key element for quality of
healthcare.Effective leadership is among the most critical components that lead an organization
to effective and successful outcomes.Significant positive associations between effective styles of
leadership and high levels of patient satisfaction and reduction of adverse effects have been reported [8].
Furthermore, several studies have stressed the importance of leadership style for quality of healthcare
provision in nursing homes [9]. Transformational leadership is strongly related to the implementation
of effective management that establishes a culture of patient safety [10]. In addition, the literature
stresses that empowering leadership is related to patient outcomes by promoting greater nursing
expertise through increased staff stability,and reduced turnout [11]. Effective leadership has an
indirect impact on reducing mortality rates, by inspiring, retaining and supporting experienced staff.
Although there are many published studies that indicate the importance of leadership, few of these
studies have attempted to correlate a certain leadership style with patient outcomes and healthcare
quality indicators.
Therefore, the aim of this review was to identify the association between leadership styles with
healthcare quality measures.
2. Materials and Methods
In transactional leadership the leader acts as a manager of change, making exchanges with employees
that lead to an improvement in production [3]. An autocratic leadership style is considered ideal
in emergencies situation as the leader makes all decisions without taking into account the opinion
of staff. Moreover,mistakes are not tolerated within the blame put on individuals.In contrary,
the laissez-faire leadership style involves a leader who does not make decisions, staff acts without
direction or supervision but there is a hands-off approach resulting in rare changes [4]. Task-oriented
leadership style involves planning of work activities, clarification of roles within a team or a group
of people, objectives set as well as the continuing monitoring and performance of processes. Lastly,
relationship-oriented leadership style incorporates support, development and recognition [ 5].
Quality of care is a vitalelementfor achieving high productivity levels within healthcare
organizations, and is defined as the degree to which the probability of achieving the expected health
outcomes is increased and in line with updated professional knowledge and skills within health
services [6]. The Institute of Medicine OM has described six characteristics of high-quality care
that must be:(1) safe,(2) effective,(3) reliable,(4) patient-centred,(5) efficient,and (6) equitable.
Measuring health outcomes is a core component of assessing quality of care.Quality measures
are: structure,process,outcome,and patient satisfaction [6]. According to the National Quality
Measures Clearing House (USA), a clinical outcome refers to the health state of a patient resulting
from healthcare. Measures on patient outcomes and satisfaction constitute: shorter patient length of
stay, hospital mortality level, health care-associated infections, failure to rescue ratio, restraint use,
medication errors, inadequate pain management, pressure ulcers rate, patient fall rate, falls with injury,
medical errors, and urinary tract infections [7].
There are numerous publications recognizing leadership style as a key element for quality of
healthcare.Effective leadership is among the most critical components that lead an organization
to effective and successful outcomes.Significant positive associations between effective styles of
leadership and high levels of patient satisfaction and reduction of adverse effects have been reported [8].
Furthermore, several studies have stressed the importance of leadership style for quality of healthcare
provision in nursing homes [9]. Transformational leadership is strongly related to the implementation
of effective management that establishes a culture of patient safety [10]. In addition, the literature
stresses that empowering leadership is related to patient outcomes by promoting greater nursing
expertise through increased staff stability,and reduced turnout [11]. Effective leadership has an
indirect impact on reducing mortality rates, by inspiring, retaining and supporting experienced staff.
Although there are many published studies that indicate the importance of leadership, few of these
studies have attempted to correlate a certain leadership style with patient outcomes and healthcare
quality indicators.
Therefore, the aim of this review was to identify the association between leadership styles with
healthcare quality measures.
2. Materials and Methods
Healthcare 2017, 5, 73 3 of 17
Access and Evaluation”; and “Quality Assurance, Healthcare”.References used by each identified
study were also checked and included in the study according to the eligibility criteria.
Five major inclusion criteria were adopted:
• Papers published in peer-reviewed journal
• Papers written in the English language
• Papers published from 2004 to 2015 (focus on more recent knowledge)
• Human epidemiological studies
• Studiesused a quantitative methodology reporting the leadership style and healthcare
quality measures
Studies that did not meet the above criteria were excluded, while those that complied with the
inclusion criteria were listed and further reviewed.
Studies were evaluated and critically appraised (Aveyard criticalappraisaltool) by two
independent reviewers. Literature screening (a three-stage approach-exclusion by reading the title, the
abstract, and the full text) and extraction of the data were conducted by two reviewers, independently.
In cases of uncertainty, a discussion was held among the members of the team to reach a common
consensus. Data were extracted systematically from each retrieved study, using a predesigned standard
data collection form (extraction table). The following information was extracted from each one of the
included studies (Table 1): authors, year of conduction, country, study design, subjects, population,
research purpose, leadership style definition, outcome definition, and main findings.
Access and Evaluation”; and “Quality Assurance, Healthcare”.References used by each identified
study were also checked and included in the study according to the eligibility criteria.
Five major inclusion criteria were adopted:
• Papers published in peer-reviewed journal
• Papers written in the English language
• Papers published from 2004 to 2015 (focus on more recent knowledge)
• Human epidemiological studies
• Studiesused a quantitative methodology reporting the leadership style and healthcare
quality measures
Studies that did not meet the above criteria were excluded, while those that complied with the
inclusion criteria were listed and further reviewed.
Studies were evaluated and critically appraised (Aveyard criticalappraisaltool) by two
independent reviewers. Literature screening (a three-stage approach-exclusion by reading the title, the
abstract, and the full text) and extraction of the data were conducted by two reviewers, independently.
In cases of uncertainty, a discussion was held among the members of the team to reach a common
consensus. Data were extracted systematically from each retrieved study, using a predesigned standard
data collection form (extraction table). The following information was extracted from each one of the
included studies (Table 1): authors, year of conduction, country, study design, subjects, population,
research purpose, leadership style definition, outcome definition, and main findings.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Healthcare 2017, 5, 73 4 of 17
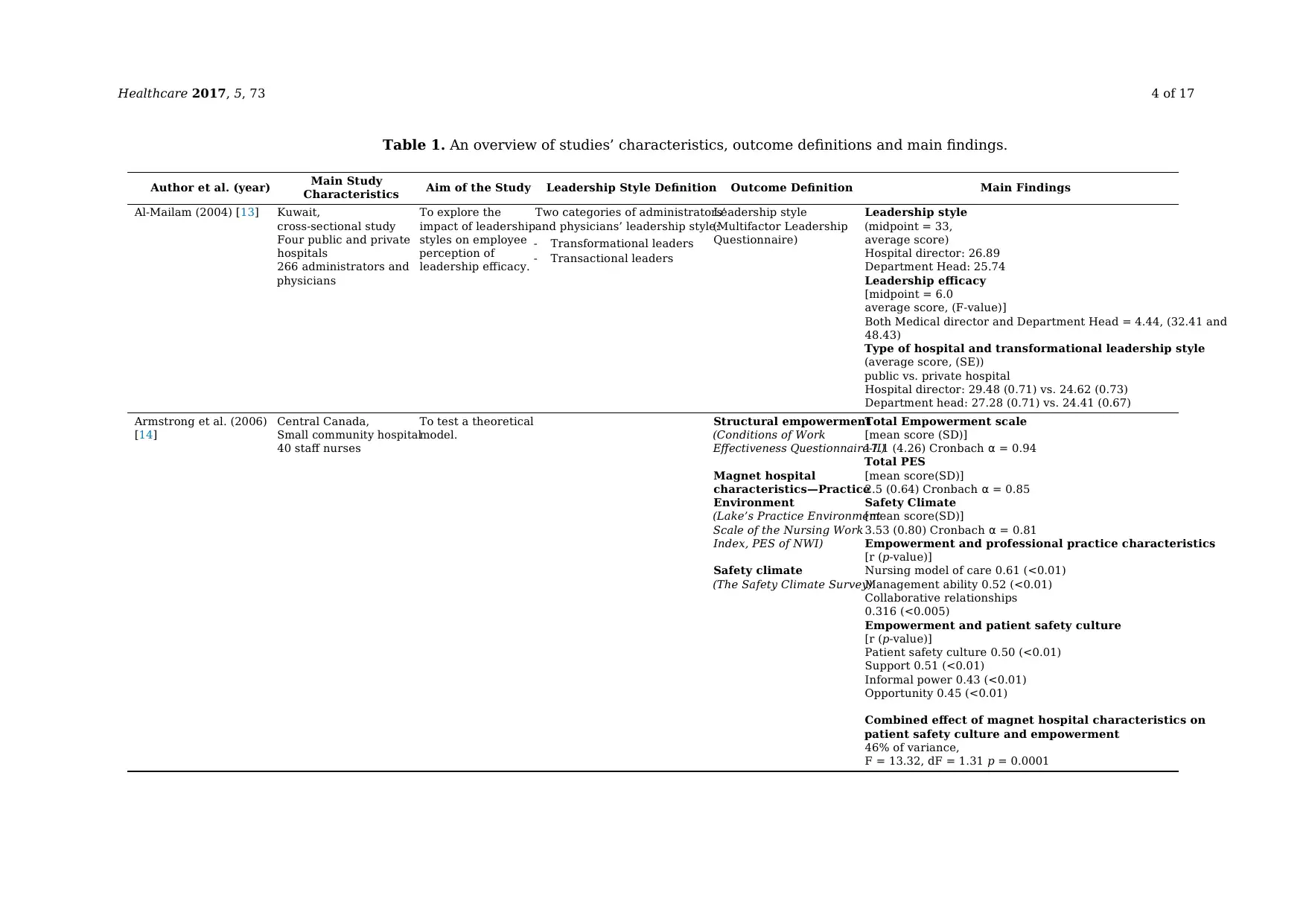
Table 1. An overview of studies’ characteristics, outcome definitions and main findings.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Al-Mailam (2004) [13] Kuwait,
cross-sectional study
Four public and private
hospitals
266 administrators and
physicians
To explore the
impact of leadership
styles on employee
perception of
leadership efficacy.
Two categories of administrators’
and physicians’ leadership style:
- Transformational leaders
- Transactional leaders
Leadership style
(Multifactor Leadership
Questionnaire)
Leadership style
(midpoint = 33,
average score)
Hospital director: 26.89
Department Head: 25.74
Leadership efficacy
[midpoint = 6.0
average score, (F-value)]
Both Medical director and Department Head = 4.44, (32.41 and
48.43)
Type of hospital and transformational leadership style
(average score, (SE))
public vs. private hospital
Hospital director: 29.48 (0.71) vs. 24.62 (0.73)
Department head: 27.28 (0.71) vs. 24.41 (0.67)
Armstrong et al. (2006)
[14]
Central Canada,
Small community hospital
40 staff nurses
To test a theoretical
model.
Structural empowerment
(Conditions of Work
Effectiveness Questionnaire-II)
Magnet hospital
characteristics—Practice
Environment
(Lake’s Practice Environment
Scale of the Nursing Work
Index, PES of NWI)
Safety climate
(The Safety Climate Survey)
Total Empowerment scale
[mean score (SD)]
17.1 (4.26) Cronbach α = 0.94
Total PES
[mean score(SD)]
2.5 (0.64) Cronbach α = 0.85
Safety Climate
[mean score(SD)]
3.53 (0.80) Cronbach α = 0.81
Empowerment and professional practice characteristics
[r (p-value)]
Nursing model of care 0.61 (<0.01)
Management ability 0.52 (<0.01)
Collaborative relationships
0.316 (<0.005)
Empowerment and patient safety culture
[r (p-value)]
Patient safety culture 0.50 (<0.01)
Support 0.51 (<0.01)
Informal power 0.43 (<0.01)
Opportunity 0.45 (<0.01)
Combined effect of magnet hospital characteristics on
patient safety culture and empowerment
46% of variance,
F = 13.32, dF = 1.31 p = 0.0001
Table 1. An overview of studies’ characteristics, outcome definitions and main findings.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Al-Mailam (2004) [13] Kuwait,
cross-sectional study
Four public and private
hospitals
266 administrators and
physicians
To explore the
impact of leadership
styles on employee
perception of
leadership efficacy.
Two categories of administrators’
and physicians’ leadership style:
- Transformational leaders
- Transactional leaders
Leadership style
(Multifactor Leadership
Questionnaire)
Leadership style
(midpoint = 33,
average score)
Hospital director: 26.89
Department Head: 25.74
Leadership efficacy
[midpoint = 6.0
average score, (F-value)]
Both Medical director and Department Head = 4.44, (32.41 and
48.43)
Type of hospital and transformational leadership style
(average score, (SE))
public vs. private hospital
Hospital director: 29.48 (0.71) vs. 24.62 (0.73)
Department head: 27.28 (0.71) vs. 24.41 (0.67)
Armstrong et al. (2006)
[14]
Central Canada,
Small community hospital
40 staff nurses
To test a theoretical
model.
Structural empowerment
(Conditions of Work
Effectiveness Questionnaire-II)
Magnet hospital
characteristics—Practice
Environment
(Lake’s Practice Environment
Scale of the Nursing Work
Index, PES of NWI)
Safety climate
(The Safety Climate Survey)
Total Empowerment scale
[mean score (SD)]
17.1 (4.26) Cronbach α = 0.94
Total PES
[mean score(SD)]
2.5 (0.64) Cronbach α = 0.85
Safety Climate
[mean score(SD)]
3.53 (0.80) Cronbach α = 0.81
Empowerment and professional practice characteristics
[r (p-value)]
Nursing model of care 0.61 (<0.01)
Management ability 0.52 (<0.01)
Collaborative relationships
0.316 (<0.005)
Empowerment and patient safety culture
[r (p-value)]
Patient safety culture 0.50 (<0.01)
Support 0.51 (<0.01)
Informal power 0.43 (<0.01)
Opportunity 0.45 (<0.01)
Combined effect of magnet hospital characteristics on
patient safety culture and empowerment
46% of variance,
F = 13.32, dF = 1.31 p = 0.0001
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare 2017, 5, 73 5 of 17
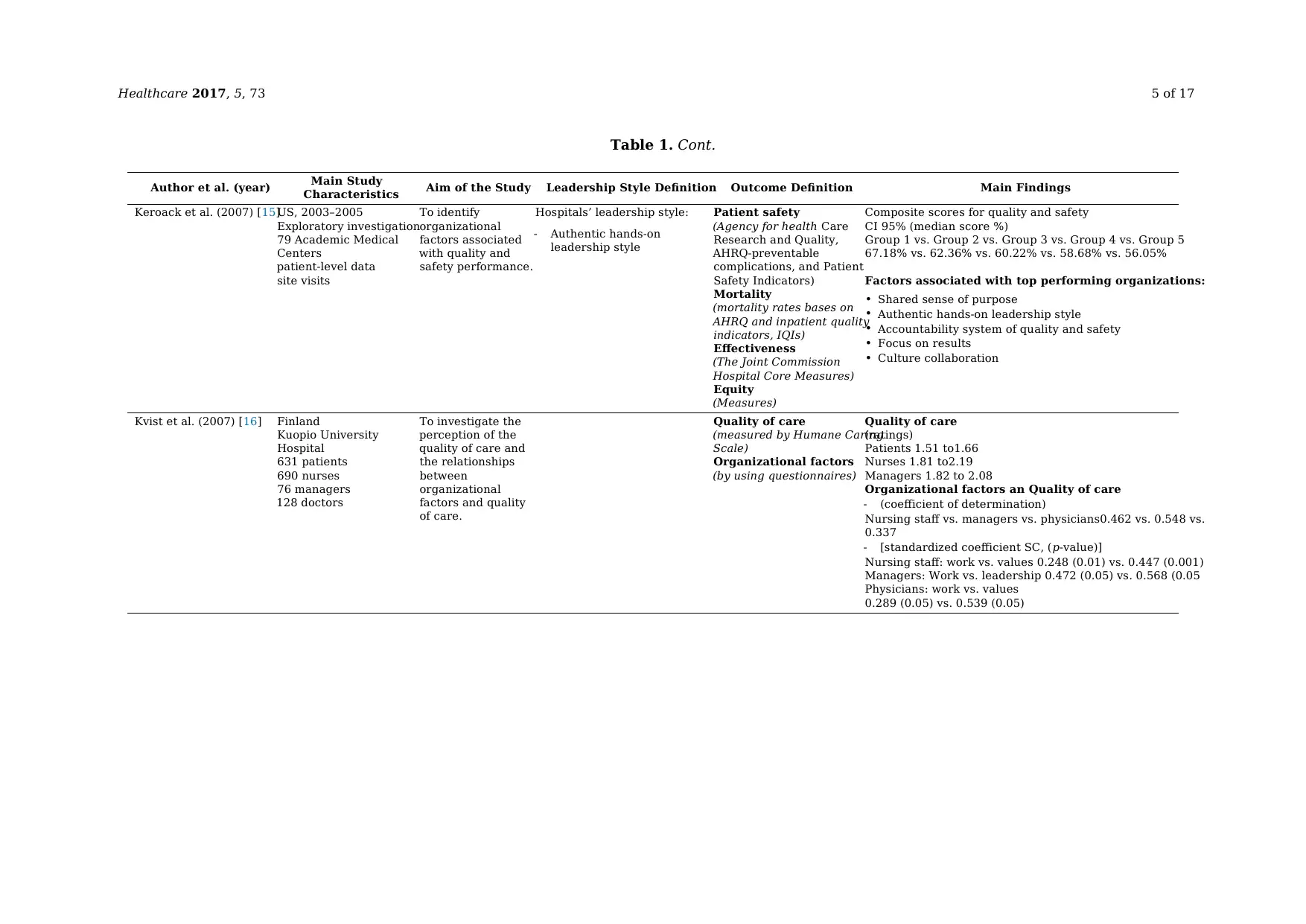
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Keroack et al. (2007) [15]US, 2003–2005
Exploratory investigation
79 Academic Medical
Centers
patient-level data
site visits
To identify
organizational
factors associated
with quality and
safety performance.
Hospitals’ leadership style:
- Authentic hands-on
leadership style
Patient safety
(Agency for health Care
Research and Quality,
AHRQ-preventable
complications, and Patient
Safety Indicators)
Mortality
(mortality rates bases on
AHRQ and inpatient quality
indicators, IQIs)
Effectiveness
(The Joint Commission
Hospital Core Measures)
Equity
(Measures)
Composite scores for quality and safety
CI 95% (median score %)
Group 1 vs. Group 2 vs. Group 3 vs. Group 4 vs. Group 5
67.18% vs. 62.36% vs. 60.22% vs. 58.68% vs. 56.05%
Factors associated with top performing organizations:
• Shared sense of purpose
• Authentic hands-on leadership style
• Accountability system of quality and safety
• Focus on results
• Culture collaboration
Kvist et al. (2007) [16] Finland
Kuopio University
Hospital
631 patients
690 nurses
76 managers
128 doctors
To investigate the
perception of the
quality of care and
the relationships
between
organizational
factors and quality
of care.
Quality of care
(measured by Humane Caring
Scale)
Organizational factors
(by using questionnaires)
Quality of care
(ratings)
Patients 1.51 to1.66
Nurses 1.81 to2.19
Managers 1.82 to 2.08
Organizational factors an Quality of care
- (coefficient of determination)
Nursing staff vs. managers vs. physicians0.462 vs. 0.548 vs.
0.337
- [standardized coefficient SC, (p-value)]
Nursing staff: work vs. values 0.248 (0.01) vs. 0.447 (0.001)
Managers: Work vs. leadership 0.472 (0.05) vs. 0.568 (0.05
Physicians: work vs. values
0.289 (0.05) vs. 0.539 (0.05)
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Keroack et al. (2007) [15]US, 2003–2005
Exploratory investigation
79 Academic Medical
Centers
patient-level data
site visits
To identify
organizational
factors associated
with quality and
safety performance.
Hospitals’ leadership style:
- Authentic hands-on
leadership style
Patient safety
(Agency for health Care
Research and Quality,
AHRQ-preventable
complications, and Patient
Safety Indicators)
Mortality
(mortality rates bases on
AHRQ and inpatient quality
indicators, IQIs)
Effectiveness
(The Joint Commission
Hospital Core Measures)
Equity
(Measures)
Composite scores for quality and safety
CI 95% (median score %)
Group 1 vs. Group 2 vs. Group 3 vs. Group 4 vs. Group 5
67.18% vs. 62.36% vs. 60.22% vs. 58.68% vs. 56.05%
Factors associated with top performing organizations:
• Shared sense of purpose
• Authentic hands-on leadership style
• Accountability system of quality and safety
• Focus on results
• Culture collaboration
Kvist et al. (2007) [16] Finland
Kuopio University
Hospital
631 patients
690 nurses
76 managers
128 doctors
To investigate the
perception of the
quality of care and
the relationships
between
organizational
factors and quality
of care.
Quality of care
(measured by Humane Caring
Scale)
Organizational factors
(by using questionnaires)
Quality of care
(ratings)
Patients 1.51 to1.66
Nurses 1.81 to2.19
Managers 1.82 to 2.08
Organizational factors an Quality of care
- (coefficient of determination)
Nursing staff vs. managers vs. physicians0.462 vs. 0.548 vs.
0.337
- [standardized coefficient SC, (p-value)]
Nursing staff: work vs. values 0.248 (0.01) vs. 0.447 (0.001)
Managers: Work vs. leadership 0.472 (0.05) vs. 0.568 (0.05
Physicians: work vs. values
0.289 (0.05) vs. 0.539 (0.05)
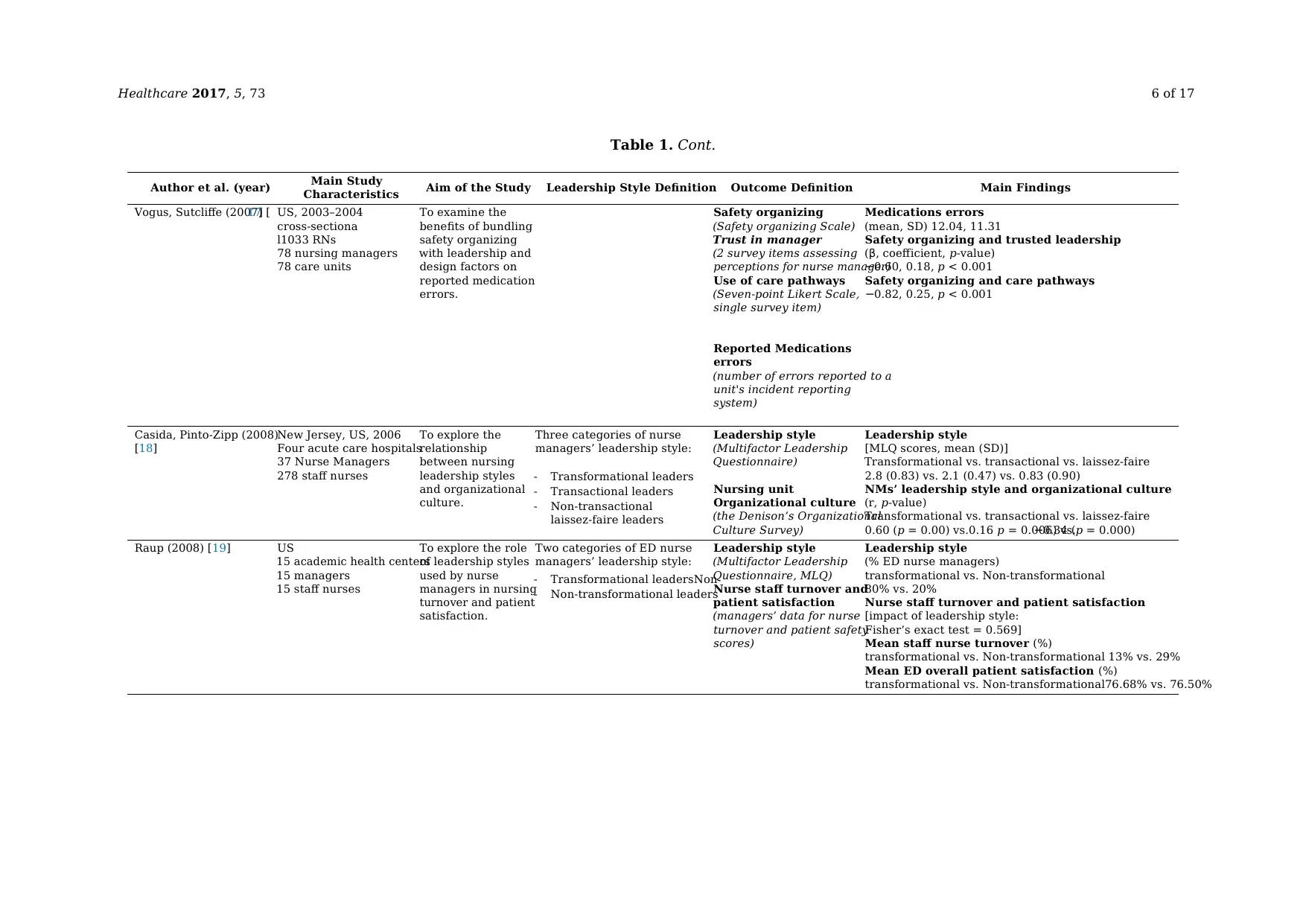
Healthcare 2017, 5, 73 6 of 17
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Vogus, Sutcliffe (2007) [17] US, 2003–2004
cross-sectiona
l1033 RNs
78 nursing managers
78 care units
To examine the
benefits of bundling
safety organizing
with leadership and
design factors on
reported medication
errors.
Safety organizing
(Safety organizing Scale)
Trust in manager
(2 survey items assessing
perceptions for nurse manager)
Use of care pathways
(Seven-point Likert Scale,
single survey item)
Reported Medications
errors
(number of errors reported to a
unit's incident reporting
system)
Medications errors
(mean, SD) 12.04, 11.31
Safety organizing and trusted leadership
(β, coefficient, p-value)
−0.60, 0.18, p < 0.001
Safety organizing and care pathways
−0.82, 0.25, p < 0.001
Casida, Pinto-Zipp (2008)
[18]
New Jersey, US, 2006
Four acute care hospitals
37 Nurse Managers
278 staff nurses
To explore the
relationship
between nursing
leadership styles
and organizational
culture.
Three categories of nurse
managers’ leadership style:
- Transformational leaders
- Transactional leaders
- Non-transactional
laissez-faire leaders
Leadership style
(Multifactor Leadership
Questionnaire)
Nursing unit
Organizational culture
(the Denison’s Organizational
Culture Survey)
Leadership style
[MLQ scores, mean (SD)]
Transformational vs. transactional vs. laissez-faire
2.8 (0.83) vs. 2.1 (0.47) vs. 0.83 (0.90)
NMs’ leadership style and organizational culture
(r, p-value)
Transformational vs. transactional vs. laissez-faire
0.60 (p = 0.00) vs.0.16 p = 0.006) vs.−0.34 (p = 0.000)
Raup (2008) [19] US
15 academic health centers
15 managers
15 staff nurses
To explore the role
of leadership styles
used by nurse
managers in nursing
turnover and patient
satisfaction.
Two categories of ED nurse
managers’ leadership style:
- Transformational leadersNon
- Non-transformational leaders
Leadership style
(Multifactor Leadership
Questionnaire, MLQ)
Nurse staff turnover and
patient satisfaction
(managers’ data for nurse
turnover and patient safety
scores)
Leadership style
(% ED nurse managers)
transformational vs. Non-transformational
80% vs. 20%
Nurse staff turnover and patient satisfaction
[impact of leadership style:
Fisher’s exact test = 0.569]
Mean staff nurse turnover (%)
transformational vs. Non-transformational 13% vs. 29%
Mean ED overall patient satisfaction (%)
transformational vs. Non-transformational76.68% vs. 76.50%
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Vogus, Sutcliffe (2007) [17] US, 2003–2004
cross-sectiona
l1033 RNs
78 nursing managers
78 care units
To examine the
benefits of bundling
safety organizing
with leadership and
design factors on
reported medication
errors.
Safety organizing
(Safety organizing Scale)
Trust in manager
(2 survey items assessing
perceptions for nurse manager)
Use of care pathways
(Seven-point Likert Scale,
single survey item)
Reported Medications
errors
(number of errors reported to a
unit's incident reporting
system)
Medications errors
(mean, SD) 12.04, 11.31
Safety organizing and trusted leadership
(β, coefficient, p-value)
−0.60, 0.18, p < 0.001
Safety organizing and care pathways
−0.82, 0.25, p < 0.001
Casida, Pinto-Zipp (2008)
[18]
New Jersey, US, 2006
Four acute care hospitals
37 Nurse Managers
278 staff nurses
To explore the
relationship
between nursing
leadership styles
and organizational
culture.
Three categories of nurse
managers’ leadership style:
- Transformational leaders
- Transactional leaders
- Non-transactional
laissez-faire leaders
Leadership style
(Multifactor Leadership
Questionnaire)
Nursing unit
Organizational culture
(the Denison’s Organizational
Culture Survey)
Leadership style
[MLQ scores, mean (SD)]
Transformational vs. transactional vs. laissez-faire
2.8 (0.83) vs. 2.1 (0.47) vs. 0.83 (0.90)
NMs’ leadership style and organizational culture
(r, p-value)
Transformational vs. transactional vs. laissez-faire
0.60 (p = 0.00) vs.0.16 p = 0.006) vs.−0.34 (p = 0.000)
Raup (2008) [19] US
15 academic health centers
15 managers
15 staff nurses
To explore the role
of leadership styles
used by nurse
managers in nursing
turnover and patient
satisfaction.
Two categories of ED nurse
managers’ leadership style:
- Transformational leadersNon
- Non-transformational leaders
Leadership style
(Multifactor Leadership
Questionnaire, MLQ)
Nurse staff turnover and
patient satisfaction
(managers’ data for nurse
turnover and patient safety
scores)
Leadership style
(% ED nurse managers)
transformational vs. Non-transformational
80% vs. 20%
Nurse staff turnover and patient satisfaction
[impact of leadership style:
Fisher’s exact test = 0.569]
Mean staff nurse turnover (%)
transformational vs. Non-transformational 13% vs. 29%
Mean ED overall patient satisfaction (%)
transformational vs. Non-transformational76.68% vs. 76.50%
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
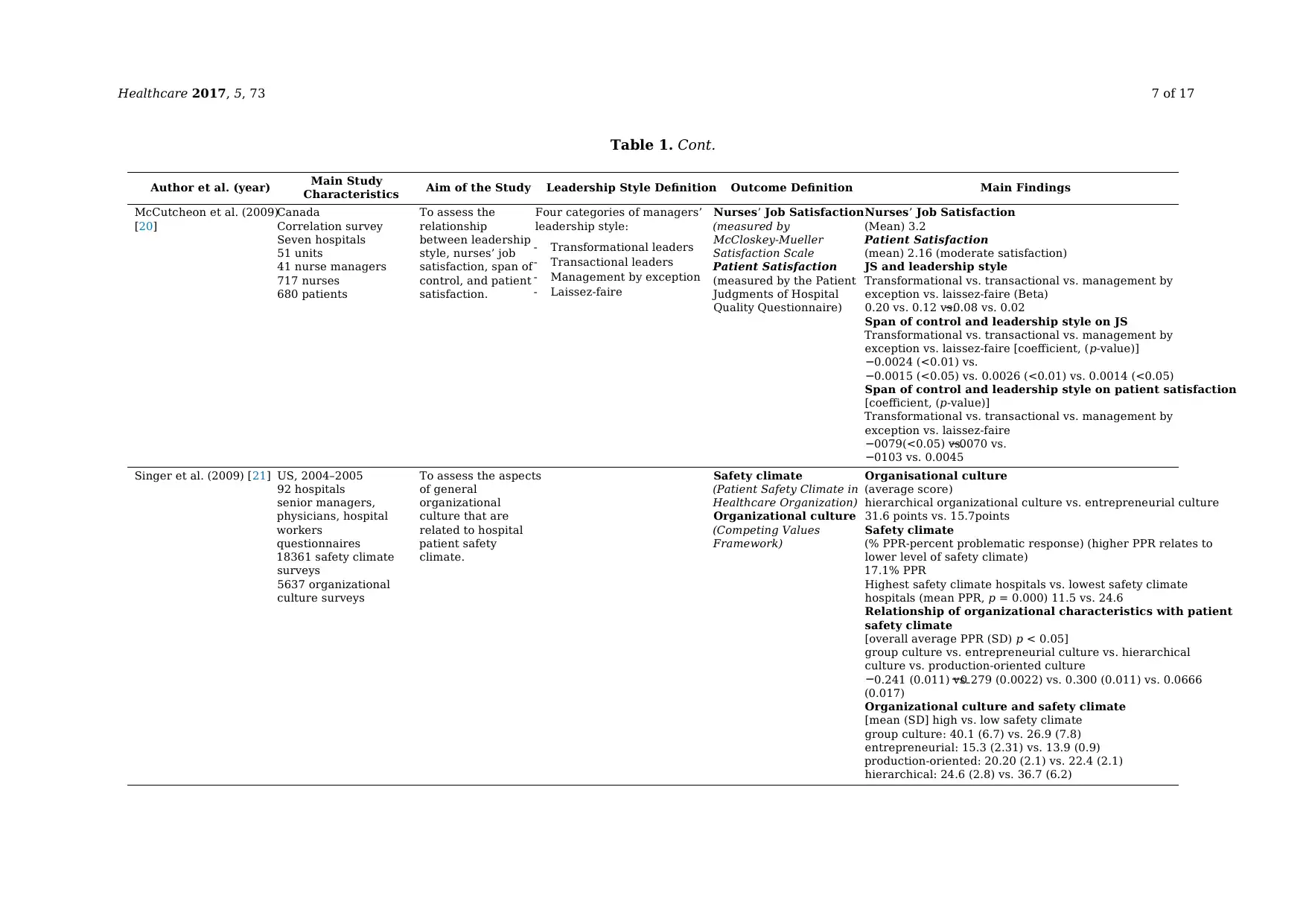
Healthcare 2017, 5, 73 7 of 17
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
McCutcheon et al. (2009)
[20]
Canada
Correlation survey
Seven hospitals
51 units
41 nurse managers
717 nurses
680 patients
To assess the
relationship
between leadership
style, nurses’ job
satisfaction, span of
control, and patient
satisfaction.
Four categories of managers’
leadership style:
- Transformational leaders
- Transactional leaders
- Management by exception
- Laissez-faire
Nurses’ Job Satisfaction
(measured by
McCloskey-Mueller
Satisfaction Scale
Patient Satisfaction
(measured by the Patient
Judgments of Hospital
Quality Questionnaire)
Nurses’ Job Satisfaction
(Mean) 3.2
Patient Satisfaction
(mean) 2.16 (moderate satisfaction)
JS and leadership style
Transformational vs. transactional vs. management by
exception vs. laissez-faire (Beta)
0.20 vs. 0.12 vs.−0.08 vs. 0.02
Span of control and leadership style on JS
Transformational vs. transactional vs. management by
exception vs. laissez-faire [coefficient, (p-value)]
−0.0024 (<0.01) vs.
−0.0015 (<0.05) vs. 0.0026 (<0.01) vs. 0.0014 (<0.05)
Span of control and leadership style on patient satisfaction
[coefficient, (p-value)]
Transformational vs. transactional vs. management by
exception vs. laissez-faire
−0079(<0.05) vs.−0070 vs.
−0103 vs. 0.0045
Singer et al. (2009) [21] US, 2004–2005
92 hospitals
senior managers,
physicians, hospital
workers
questionnaires
18361 safety climate
surveys
5637 organizational
culture surveys
To assess the aspects
of general
organizational
culture that are
related to hospital
patient safety
climate.
Safety climate
(Patient Safety Climate in
Healthcare Organization)
Organizational culture
(Competing Values
Framework)
Organisational culture
(average score)
hierarchical organizational culture vs. entrepreneurial culture
31.6 points vs. 15.7points
Safety climate
(% PPR-percent problematic response) (higher PPR relates to
lower level of safety climate)
17.1% PPR
Highest safety climate hospitals vs. lowest safety climate
hospitals (mean PPR, p = 0.000) 11.5 vs. 24.6
Relationship of organizational characteristics with patient
safety climate
[overall average PPR (SD) p < 0.05]
group culture vs. entrepreneurial culture vs. hierarchical
culture vs. production-oriented culture
−0.241 (0.011) vs.−0.279 (0.0022) vs. 0.300 (0.011) vs. 0.0666
(0.017)
Organizational culture and safety climate
[mean (SD] high vs. low safety climate
group culture: 40.1 (6.7) vs. 26.9 (7.8)
entrepreneurial: 15.3 (2.31) vs. 13.9 (0.9)
production-oriented: 20.20 (2.1) vs. 22.4 (2.1)
hierarchical: 24.6 (2.8) vs. 36.7 (6.2)
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
McCutcheon et al. (2009)
[20]
Canada
Correlation survey
Seven hospitals
51 units
41 nurse managers
717 nurses
680 patients
To assess the
relationship
between leadership
style, nurses’ job
satisfaction, span of
control, and patient
satisfaction.
Four categories of managers’
leadership style:
- Transformational leaders
- Transactional leaders
- Management by exception
- Laissez-faire
Nurses’ Job Satisfaction
(measured by
McCloskey-Mueller
Satisfaction Scale
Patient Satisfaction
(measured by the Patient
Judgments of Hospital
Quality Questionnaire)
Nurses’ Job Satisfaction
(Mean) 3.2
Patient Satisfaction
(mean) 2.16 (moderate satisfaction)
JS and leadership style
Transformational vs. transactional vs. management by
exception vs. laissez-faire (Beta)
0.20 vs. 0.12 vs.−0.08 vs. 0.02
Span of control and leadership style on JS
Transformational vs. transactional vs. management by
exception vs. laissez-faire [coefficient, (p-value)]
−0.0024 (<0.01) vs.
−0.0015 (<0.05) vs. 0.0026 (<0.01) vs. 0.0014 (<0.05)
Span of control and leadership style on patient satisfaction
[coefficient, (p-value)]
Transformational vs. transactional vs. management by
exception vs. laissez-faire
−0079(<0.05) vs.−0070 vs.
−0103 vs. 0.0045
Singer et al. (2009) [21] US, 2004–2005
92 hospitals
senior managers,
physicians, hospital
workers
questionnaires
18361 safety climate
surveys
5637 organizational
culture surveys
To assess the aspects
of general
organizational
culture that are
related to hospital
patient safety
climate.
Safety climate
(Patient Safety Climate in
Healthcare Organization)
Organizational culture
(Competing Values
Framework)
Organisational culture
(average score)
hierarchical organizational culture vs. entrepreneurial culture
31.6 points vs. 15.7points
Safety climate
(% PPR-percent problematic response) (higher PPR relates to
lower level of safety climate)
17.1% PPR
Highest safety climate hospitals vs. lowest safety climate
hospitals (mean PPR, p = 0.000) 11.5 vs. 24.6
Relationship of organizational characteristics with patient
safety climate
[overall average PPR (SD) p < 0.05]
group culture vs. entrepreneurial culture vs. hierarchical
culture vs. production-oriented culture
−0.241 (0.011) vs.−0.279 (0.0022) vs. 0.300 (0.011) vs. 0.0666
(0.017)
Organizational culture and safety climate
[mean (SD] high vs. low safety climate
group culture: 40.1 (6.7) vs. 26.9 (7.8)
entrepreneurial: 15.3 (2.31) vs. 13.9 (0.9)
production-oriented: 20.20 (2.1) vs. 22.4 (2.1)
hierarchical: 24.6 (2.8) vs. 36.7 (6.2)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
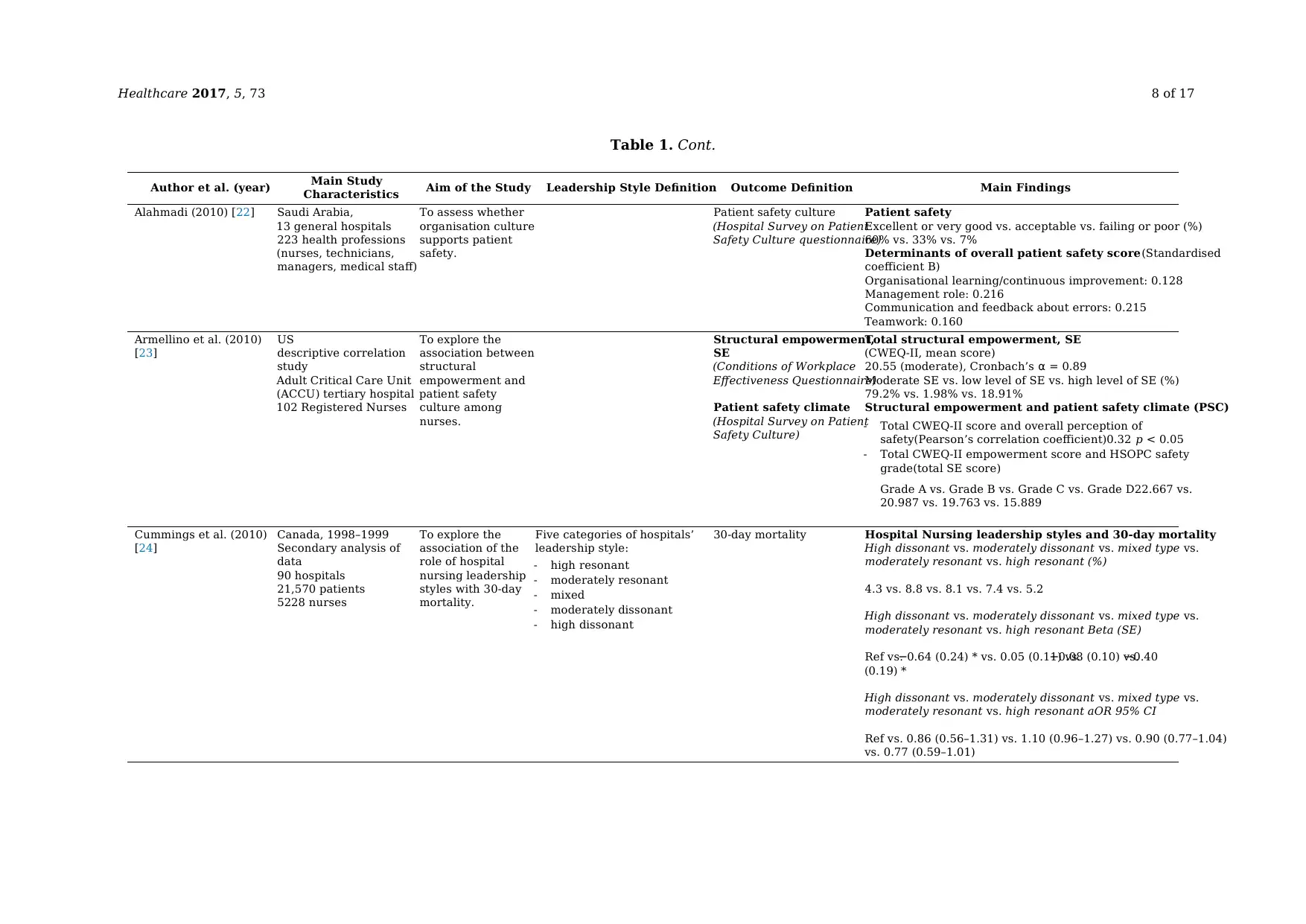
Healthcare 2017, 5, 73 8 of 17
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Alahmadi (2010) [22] Saudi Arabia,
13 general hospitals
223 health professions
(nurses, technicians,
managers, medical staff)
To assess whether
organisation culture
supports patient
safety.
Patient safety culture
(Hospital Survey on Patient
Safety Culture questionnaire)
Patient safety
Excellent or very good vs. acceptable vs. failing or poor (%)
60% vs. 33% vs. 7%
Determinants of overall patient safety score(Standardised
coefficient B)
Organisational learning/continuous improvement: 0.128
Management role: 0.216
Communication and feedback about errors: 0.215
Teamwork: 0.160
Armellino et al. (2010)
[23]
US
descriptive correlation
study
Adult Critical Care Unit
(ACCU) tertiary hospital
102 Registered Nurses
To explore the
association between
structural
empowerment and
patient safety
culture among
nurses.
Structural empowerment,
SE
(Conditions of Workplace
Effectiveness Questionnaire)
Patient safety climate
(Hospital Survey on Patient
Safety Culture)
Total structural empowerment, SE
(CWEQ-II, mean score)
20.55 (moderate), Cronbach’s α = 0.89
Moderate SE vs. low level of SE vs. high level of SE (%)
79.2% vs. 1.98% vs. 18.91%
Structural empowerment and patient safety climate (PSC)
- Total CWEQ-II score and overall perception of
safety(Pearson’s correlation coefficient)0.32 p < 0.05
- Total CWEQ-II empowerment score and HSOPC safety
grade(total SE score)
Grade A vs. Grade B vs. Grade C vs. Grade D22.667 vs.
20.987 vs. 19.763 vs. 15.889
Cummings et al. (2010)
[24]
Canada, 1998–1999
Secondary analysis of
data
90 hospitals
21,570 patients
5228 nurses
To explore the
association of the
role of hospital
nursing leadership
styles with 30-day
mortality.
Five categories of hospitals’
leadership style:
- high resonant
- moderately resonant
- mixed
- moderately dissonant
- high dissonant
30-day mortality Hospital Nursing leadership styles and 30-day mortality
High dissonant vs. moderately dissonant vs. mixed type vs.
moderately resonant vs. high resonant (%)
4.3 vs. 8.8 vs. 8.1 vs. 7.4 vs. 5.2
High dissonant vs. moderately dissonant vs. mixed type vs.
moderately resonant vs. high resonant Beta (SE)
Ref vs.−0.64 (0.24) * vs. 0.05 (0.11) vs.−0.08 (0.10) vs.−0.40
(0.19) *
High dissonant vs. moderately dissonant vs. mixed type vs.
moderately resonant vs. high resonant aOR 95% CI
Ref vs. 0.86 (0.56–1.31) vs. 1.10 (0.96–1.27) vs. 0.90 (0.77–1.04)
vs. 0.77 (0.59–1.01)
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Alahmadi (2010) [22] Saudi Arabia,
13 general hospitals
223 health professions
(nurses, technicians,
managers, medical staff)
To assess whether
organisation culture
supports patient
safety.
Patient safety culture
(Hospital Survey on Patient
Safety Culture questionnaire)
Patient safety
Excellent or very good vs. acceptable vs. failing or poor (%)
60% vs. 33% vs. 7%
Determinants of overall patient safety score(Standardised
coefficient B)
Organisational learning/continuous improvement: 0.128
Management role: 0.216
Communication and feedback about errors: 0.215
Teamwork: 0.160
Armellino et al. (2010)
[23]
US
descriptive correlation
study
Adult Critical Care Unit
(ACCU) tertiary hospital
102 Registered Nurses
To explore the
association between
structural
empowerment and
patient safety
culture among
nurses.
Structural empowerment,
SE
(Conditions of Workplace
Effectiveness Questionnaire)
Patient safety climate
(Hospital Survey on Patient
Safety Culture)
Total structural empowerment, SE
(CWEQ-II, mean score)
20.55 (moderate), Cronbach’s α = 0.89
Moderate SE vs. low level of SE vs. high level of SE (%)
79.2% vs. 1.98% vs. 18.91%
Structural empowerment and patient safety climate (PSC)
- Total CWEQ-II score and overall perception of
safety(Pearson’s correlation coefficient)0.32 p < 0.05
- Total CWEQ-II empowerment score and HSOPC safety
grade(total SE score)
Grade A vs. Grade B vs. Grade C vs. Grade D22.667 vs.
20.987 vs. 19.763 vs. 15.889
Cummings et al. (2010)
[24]
Canada, 1998–1999
Secondary analysis of
data
90 hospitals
21,570 patients
5228 nurses
To explore the
association of the
role of hospital
nursing leadership
styles with 30-day
mortality.
Five categories of hospitals’
leadership style:
- high resonant
- moderately resonant
- mixed
- moderately dissonant
- high dissonant
30-day mortality Hospital Nursing leadership styles and 30-day mortality
High dissonant vs. moderately dissonant vs. mixed type vs.
moderately resonant vs. high resonant (%)
4.3 vs. 8.8 vs. 8.1 vs. 7.4 vs. 5.2
High dissonant vs. moderately dissonant vs. mixed type vs.
moderately resonant vs. high resonant Beta (SE)
Ref vs.−0.64 (0.24) * vs. 0.05 (0.11) vs.−0.08 (0.10) vs.−0.40
(0.19) *
High dissonant vs. moderately dissonant vs. mixed type vs.
moderately resonant vs. high resonant aOR 95% CI
Ref vs. 0.86 (0.56–1.31) vs. 1.10 (0.96–1.27) vs. 0.90 (0.77–1.04)
vs. 0.77 (0.59–1.01)
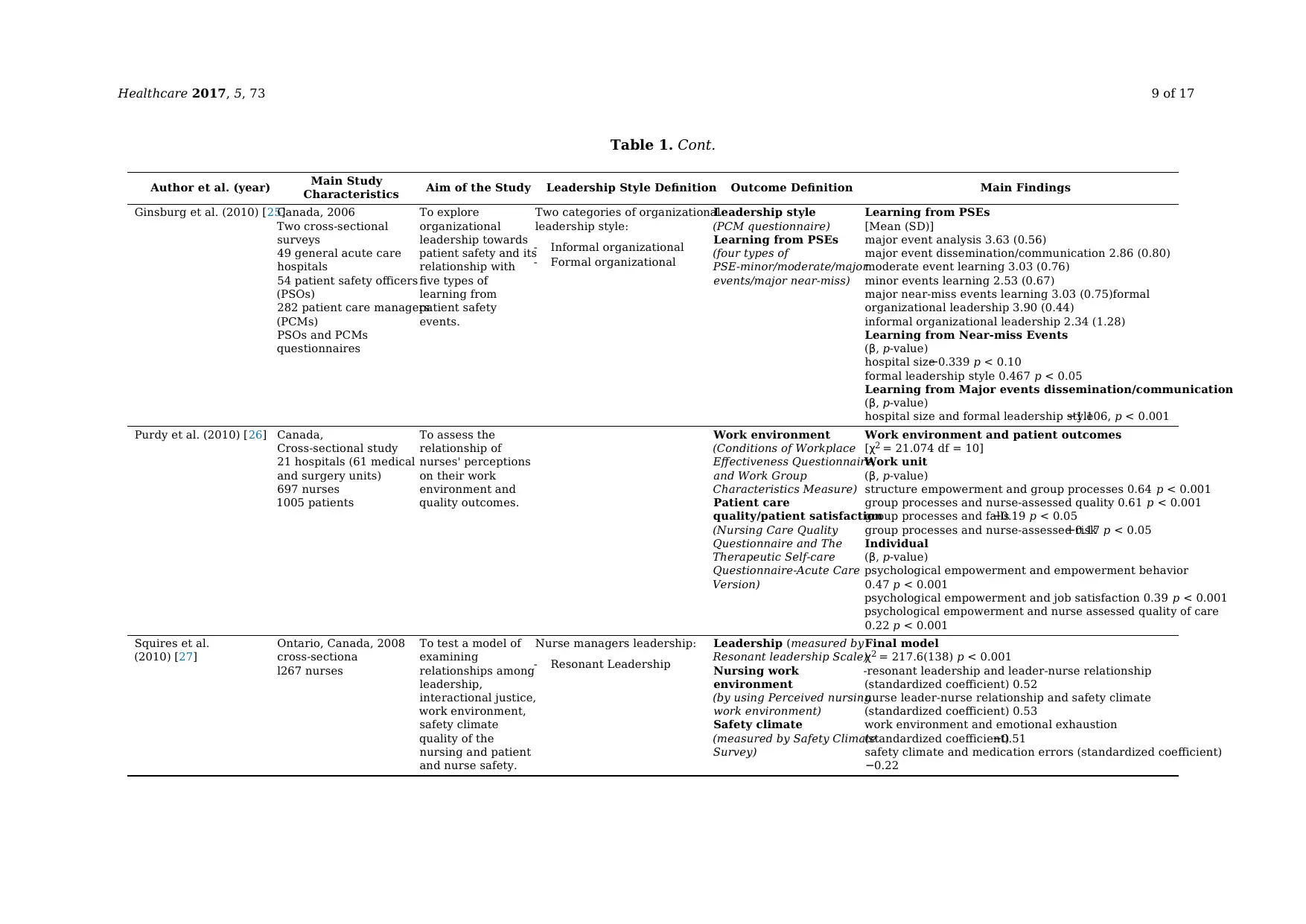
Healthcare 2017, 5, 73 9 of 17
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Ginsburg et al. (2010) [25]Canada, 2006
Two cross-sectional
surveys
49 general acute care
hospitals
54 patient safety officers
(PSOs)
282 patient care managers
(PCMs)
PSOs and PCMs
questionnaires
To explore
organizational
leadership towards
patient safety and its
relationship with
five types of
learning from
patient safety
events.
Two categories of organizational
leadership style:
- Informal organizational
- Formal organizational
Leadership style
(PCM questionnaire)
Learning from PSEs
(four types of
PSE-minor/moderate/major
events/major near-miss)
Learning from PSEs
[Mean (SD)]
major event analysis 3.63 (0.56)
major event dissemination/communication 2.86 (0.80)
moderate event learning 3.03 (0.76)
minor events learning 2.53 (0.67)
major near-miss events learning 3.03 (0.75)formal
organizational leadership 3.90 (0.44)
informal organizational leadership 2.34 (1.28)
Learning from Near-miss Events
(β, p-value)
hospital size−0.339 p < 0.10
formal leadership style 0.467 p < 0.05
Learning from Major events dissemination/communication
(β, p-value)
hospital size and formal leadership style−1.106, p < 0.001
Purdy et al. (2010) [26] Canada,
Cross-sectional study
21 hospitals (61 medical
and surgery units)
697 nurses
1005 patients
To assess the
relationship of
nurses' perceptions
on their work
environment and
quality outcomes.
Work environment
(Conditions of Workplace
Effectiveness Questionnaire,
and Work Group
Characteristics Measure)
Patient care
quality/patient satisfaction
(Nursing Care Quality
Questionnaire and The
Therapeutic Self-care
Questionnaire-Acute Care
Version)
Work environment and patient outcomes
[χ2 = 21.074 df = 10]
Work unit
(β, p-value)
structure empowerment and group processes 0.64 p < 0.001
group processes and nurse-assessed quality 0.61 p < 0.001
group processes and falls−0.19 p < 0.05
group processes and nurse-assessed risk−0.17 p < 0.05
Individual
(β, p-value)
psychological empowerment and empowerment behavior
0.47 p < 0.001
psychological empowerment and job satisfaction 0.39 p < 0.001
psychological empowerment and nurse assessed quality of care
0.22 p < 0.001
Squires et al.
(2010) [27]
Ontario, Canada, 2008
cross-sectiona
l267 nurses
To test a model of
examining
relationships among
leadership,
interactional justice,
work environment,
safety climate
quality of the
nursing and patient
and nurse safety.
Nurse managers leadership:
- Resonant Leadership
Leadership (measured by
Resonant leadership Scale)
Nursing work
environment
(by using Perceived nursing
work environment)
Safety climate
(measured by Safety Climate
Survey)
Final model
χ2 = 217.6(138) p < 0.001
-resonant leadership and leader-nurse relationship
(standardized coefficient) 0.52
nurse leader-nurse relationship and safety climate
(standardized coefficient) 0.53
work environment and emotional exhaustion
(standardized coefficient)−0.51
safety climate and medication errors (standardized coefficient)
−0.22
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Ginsburg et al. (2010) [25]Canada, 2006
Two cross-sectional
surveys
49 general acute care
hospitals
54 patient safety officers
(PSOs)
282 patient care managers
(PCMs)
PSOs and PCMs
questionnaires
To explore
organizational
leadership towards
patient safety and its
relationship with
five types of
learning from
patient safety
events.
Two categories of organizational
leadership style:
- Informal organizational
- Formal organizational
Leadership style
(PCM questionnaire)
Learning from PSEs
(four types of
PSE-minor/moderate/major
events/major near-miss)
Learning from PSEs
[Mean (SD)]
major event analysis 3.63 (0.56)
major event dissemination/communication 2.86 (0.80)
moderate event learning 3.03 (0.76)
minor events learning 2.53 (0.67)
major near-miss events learning 3.03 (0.75)formal
organizational leadership 3.90 (0.44)
informal organizational leadership 2.34 (1.28)
Learning from Near-miss Events
(β, p-value)
hospital size−0.339 p < 0.10
formal leadership style 0.467 p < 0.05
Learning from Major events dissemination/communication
(β, p-value)
hospital size and formal leadership style−1.106, p < 0.001
Purdy et al. (2010) [26] Canada,
Cross-sectional study
21 hospitals (61 medical
and surgery units)
697 nurses
1005 patients
To assess the
relationship of
nurses' perceptions
on their work
environment and
quality outcomes.
Work environment
(Conditions of Workplace
Effectiveness Questionnaire,
and Work Group
Characteristics Measure)
Patient care
quality/patient satisfaction
(Nursing Care Quality
Questionnaire and The
Therapeutic Self-care
Questionnaire-Acute Care
Version)
Work environment and patient outcomes
[χ2 = 21.074 df = 10]
Work unit
(β, p-value)
structure empowerment and group processes 0.64 p < 0.001
group processes and nurse-assessed quality 0.61 p < 0.001
group processes and falls−0.19 p < 0.05
group processes and nurse-assessed risk−0.17 p < 0.05
Individual
(β, p-value)
psychological empowerment and empowerment behavior
0.47 p < 0.001
psychological empowerment and job satisfaction 0.39 p < 0.001
psychological empowerment and nurse assessed quality of care
0.22 p < 0.001
Squires et al.
(2010) [27]
Ontario, Canada, 2008
cross-sectiona
l267 nurses
To test a model of
examining
relationships among
leadership,
interactional justice,
work environment,
safety climate
quality of the
nursing and patient
and nurse safety.
Nurse managers leadership:
- Resonant Leadership
Leadership (measured by
Resonant leadership Scale)
Nursing work
environment
(by using Perceived nursing
work environment)
Safety climate
(measured by Safety Climate
Survey)
Final model
χ2 = 217.6(138) p < 0.001
-resonant leadership and leader-nurse relationship
(standardized coefficient) 0.52
nurse leader-nurse relationship and safety climate
(standardized coefficient) 0.53
work environment and emotional exhaustion
(standardized coefficient)−0.51
safety climate and medication errors (standardized coefficient)
−0.22
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
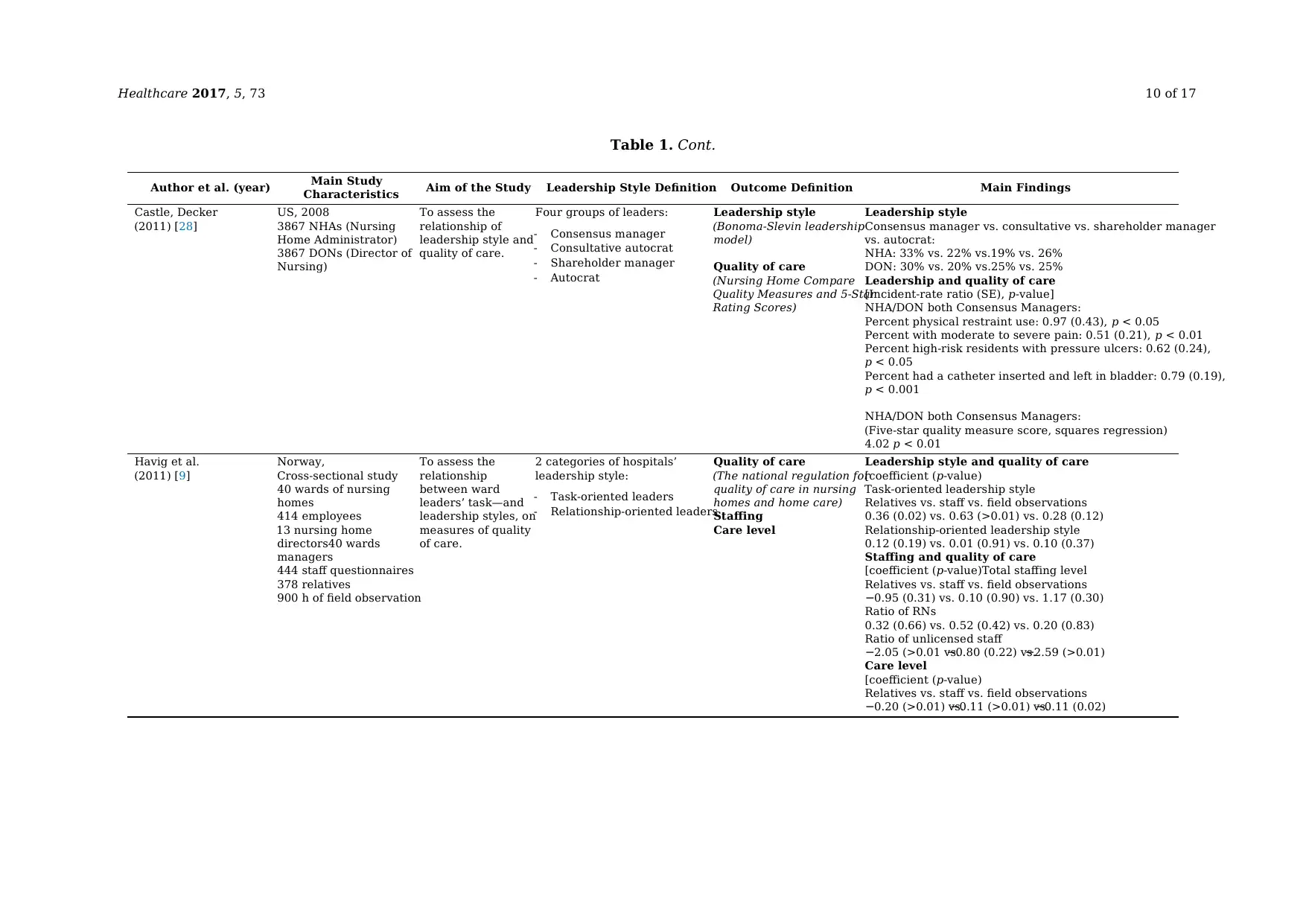
Healthcare 2017, 5, 73 10 of 17
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Castle, Decker
(2011) [28]
US, 2008
3867 NHAs (Nursing
Home Administrator)
3867 DONs (Director of
Nursing)
To assess the
relationship of
leadership style and
quality of care.
Four groups of leaders:
- Consensus manager
- Consultative autocrat
- Shareholder manager
- Autocrat
Leadership style
(Bonoma-Slevin leadership
model)
Quality of care
(Nursing Home Compare
Quality Measures and 5-Star
Rating Scores)
Leadership style
Consensus manager vs. consultative vs. shareholder manager
vs. autocrat:
NHA: 33% vs. 22% vs.19% vs. 26%
DON: 30% vs. 20% vs.25% vs. 25%
Leadership and quality of care
[Incident-rate ratio (SE), p-value]
NHA/DON both Consensus Managers:
Percent physical restraint use: 0.97 (0.43), p < 0.05
Percent with moderate to severe pain: 0.51 (0.21), p < 0.01
Percent high-risk residents with pressure ulcers: 0.62 (0.24),
p < 0.05
Percent had a catheter inserted and left in bladder: 0.79 (0.19),
p < 0.001
NHA/DON both Consensus Managers:
(Five-star quality measure score, squares regression)
4.02 p < 0.01
Havig et al.
(2011) [9]
Norway,
Cross-sectional study
40 wards of nursing
homes
414 employees
13 nursing home
directors40 wards
managers
444 staff questionnaires
378 relatives
900 h of field observation
To assess the
relationship
between ward
leaders’ task—and
leadership styles, on
measures of quality
of care.
2 categories of hospitals’
leadership style:
- Task-oriented leaders
- Relationship-oriented leaders
Quality of care
(The national regulation for
quality of care in nursing
homes and home care)
Staffing
Care level
Leadership style and quality of care
[coefficient (p-value)
Task-oriented leadership style
Relatives vs. staff vs. field observations
0.36 (0.02) vs. 0.63 (>0.01) vs. 0.28 (0.12)
Relationship-oriented leadership style
0.12 (0.19) vs. 0.01 (0.91) vs. 0.10 (0.37)
Staffing and quality of care
[coefficient (p-value)Total staffing level
Relatives vs. staff vs. field observations
−0.95 (0.31) vs. 0.10 (0.90) vs. 1.17 (0.30)
Ratio of RNs
0.32 (0.66) vs. 0.52 (0.42) vs. 0.20 (0.83)
Ratio of unlicensed staff
−2.05 (>0.01 vs.−0.80 (0.22) vs.−2.59 (>0.01)
Care level
[coefficient (p-value)
Relatives vs. staff vs. field observations
−0.20 (>0.01) vs.−0.11 (>0.01) vs.−0.11 (0.02)
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Castle, Decker
(2011) [28]
US, 2008
3867 NHAs (Nursing
Home Administrator)
3867 DONs (Director of
Nursing)
To assess the
relationship of
leadership style and
quality of care.
Four groups of leaders:
- Consensus manager
- Consultative autocrat
- Shareholder manager
- Autocrat
Leadership style
(Bonoma-Slevin leadership
model)
Quality of care
(Nursing Home Compare
Quality Measures and 5-Star
Rating Scores)
Leadership style
Consensus manager vs. consultative vs. shareholder manager
vs. autocrat:
NHA: 33% vs. 22% vs.19% vs. 26%
DON: 30% vs. 20% vs.25% vs. 25%
Leadership and quality of care
[Incident-rate ratio (SE), p-value]
NHA/DON both Consensus Managers:
Percent physical restraint use: 0.97 (0.43), p < 0.05
Percent with moderate to severe pain: 0.51 (0.21), p < 0.01
Percent high-risk residents with pressure ulcers: 0.62 (0.24),
p < 0.05
Percent had a catheter inserted and left in bladder: 0.79 (0.19),
p < 0.001
NHA/DON both Consensus Managers:
(Five-star quality measure score, squares regression)
4.02 p < 0.01
Havig et al.
(2011) [9]
Norway,
Cross-sectional study
40 wards of nursing
homes
414 employees
13 nursing home
directors40 wards
managers
444 staff questionnaires
378 relatives
900 h of field observation
To assess the
relationship
between ward
leaders’ task—and
leadership styles, on
measures of quality
of care.
2 categories of hospitals’
leadership style:
- Task-oriented leaders
- Relationship-oriented leaders
Quality of care
(The national regulation for
quality of care in nursing
homes and home care)
Staffing
Care level
Leadership style and quality of care
[coefficient (p-value)
Task-oriented leadership style
Relatives vs. staff vs. field observations
0.36 (0.02) vs. 0.63 (>0.01) vs. 0.28 (0.12)
Relationship-oriented leadership style
0.12 (0.19) vs. 0.01 (0.91) vs. 0.10 (0.37)
Staffing and quality of care
[coefficient (p-value)Total staffing level
Relatives vs. staff vs. field observations
−0.95 (0.31) vs. 0.10 (0.90) vs. 1.17 (0.30)
Ratio of RNs
0.32 (0.66) vs. 0.52 (0.42) vs. 0.20 (0.83)
Ratio of unlicensed staff
−2.05 (>0.01 vs.−0.80 (0.22) vs.−2.59 (>0.01)
Care level
[coefficient (p-value)
Relatives vs. staff vs. field observations
−0.20 (>0.01) vs.−0.11 (>0.01) vs.−0.11 (0.02)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare 2017, 5, 73 11 of 17
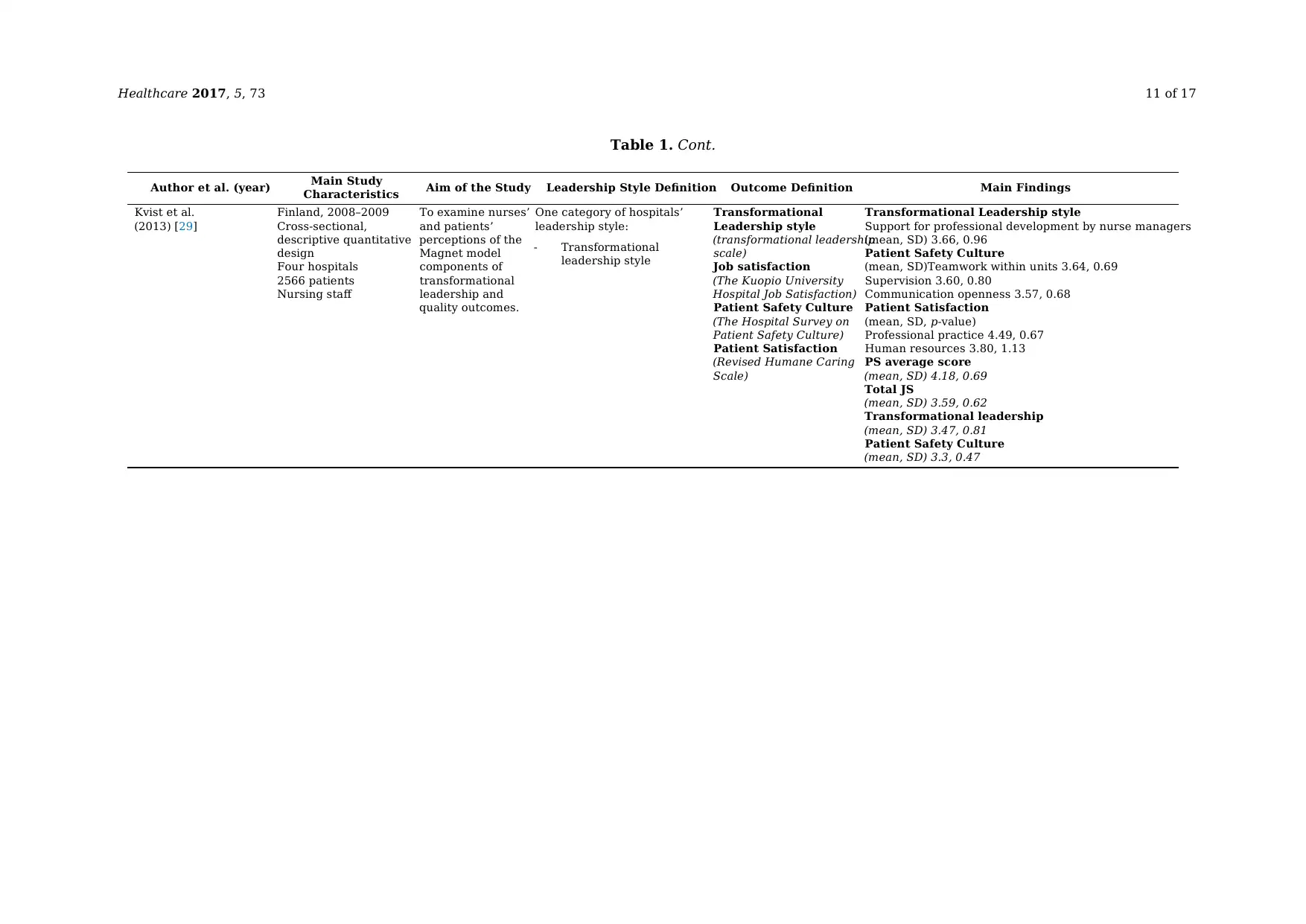
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Kvist et al.
(2013) [29]
Finland, 2008–2009
Cross-sectional,
descriptive quantitative
design
Four hospitals
2566 patients
Nursing staff
To examine nurses’
and patients’
perceptions of the
Magnet model
components of
transformational
leadership and
quality outcomes.
One category of hospitals’
leadership style:
- Transformational
leadership style
Transformational
Leadership style
(transformational leadership
scale)
Job satisfaction
(The Kuopio University
Hospital Job Satisfaction)
Patient Safety Culture
(The Hospital Survey on
Patient Safety Culture)
Patient Satisfaction
(Revised Humane Caring
Scale)
Transformational Leadership style
Support for professional development by nurse managers
(mean, SD) 3.66, 0.96
Patient Safety Culture
(mean, SD)Teamwork within units 3.64, 0.69
Supervision 3.60, 0.80
Communication openness 3.57, 0.68
Patient Satisfaction
(mean, SD, p-value)
Professional practice 4.49, 0.67
Human resources 3.80, 1.13
PS average score
(mean, SD) 4.18, 0.69
Total JS
(mean, SD) 3.59, 0.62
Transformational leadership
(mean, SD) 3.47, 0.81
Patient Safety Culture
(mean, SD) 3.3, 0.47
Table 1. Cont.
Author et al. (year) Main Study
Characteristics Aim of the Study Leadership Style Definition Outcome Definition Main Findings
Kvist et al.
(2013) [29]
Finland, 2008–2009
Cross-sectional,
descriptive quantitative
design
Four hospitals
2566 patients
Nursing staff
To examine nurses’
and patients’
perceptions of the
Magnet model
components of
transformational
leadership and
quality outcomes.
One category of hospitals’
leadership style:
- Transformational
leadership style
Transformational
Leadership style
(transformational leadership
scale)
Job satisfaction
(The Kuopio University
Hospital Job Satisfaction)
Patient Safety Culture
(The Hospital Survey on
Patient Safety Culture)
Patient Satisfaction
(Revised Humane Caring
Scale)
Transformational Leadership style
Support for professional development by nurse managers
(mean, SD) 3.66, 0.96
Patient Safety Culture
(mean, SD)Teamwork within units 3.64, 0.69
Supervision 3.60, 0.80
Communication openness 3.57, 0.68
Patient Satisfaction
(mean, SD, p-value)
Professional practice 4.49, 0.67
Human resources 3.80, 1.13
PS average score
(mean, SD) 4.18, 0.69
Total JS
(mean, SD) 3.59, 0.62
Transformational leadership
(mean, SD) 3.47, 0.81
Patient Safety Culture
(mean, SD) 3.3, 0.47
Healthcare 2017, 5, 73 12 of 17
3. Results
3.1. Bibliographic Search
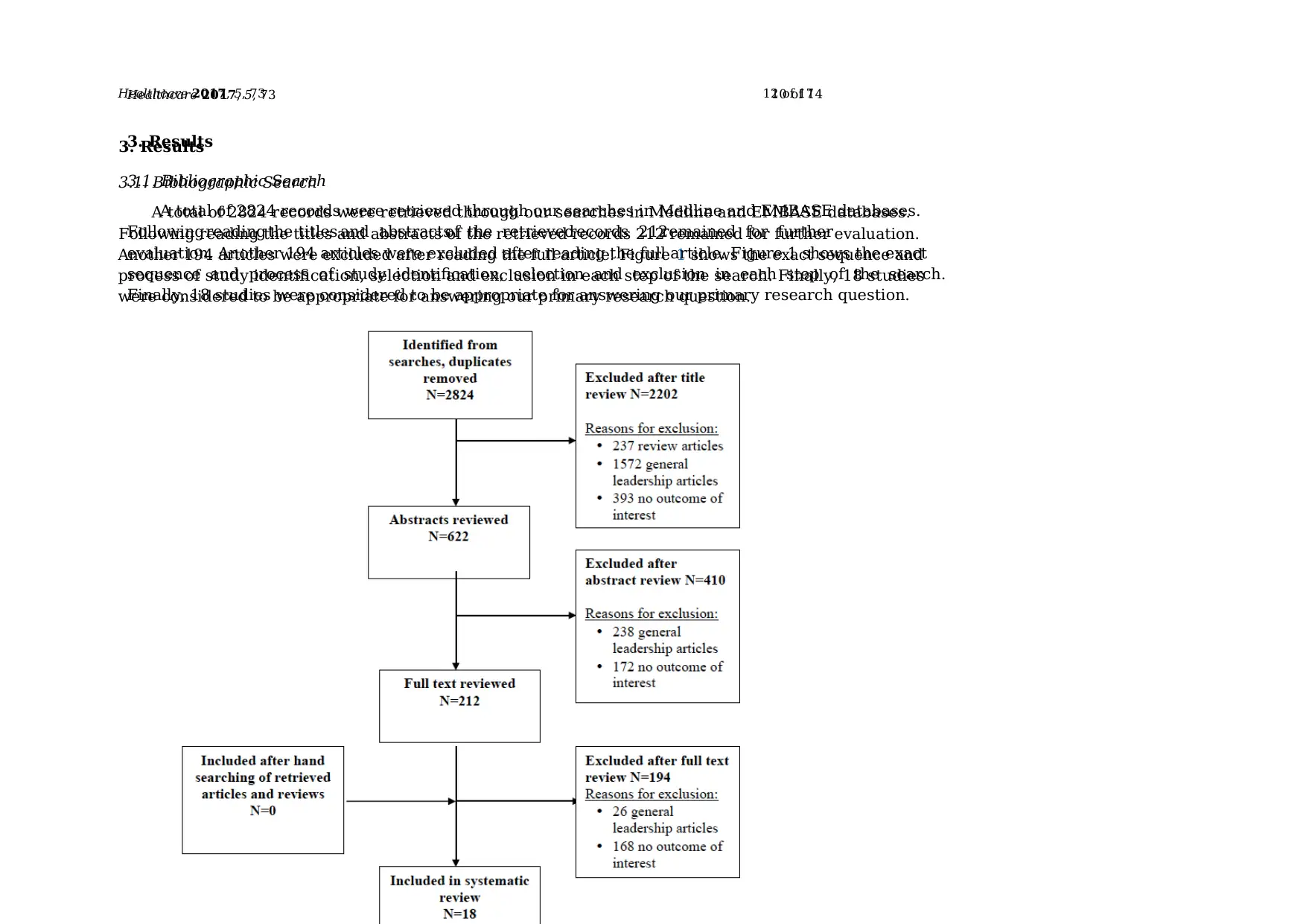
A total of 2824 records were retrieved through our searches in Medline and EMBASE databases.
Following reading the titles and abstracts of the retrieved records 212 remained for further evaluation.
Another 194 articles were excluded after reading the full article. Figure 1 shows the exact sequence and
process of study identification, selection and exclusion in each step of the search. Finally, 18 studies
were considered to be appropriate for answering our primary research question.
Healthcare 2017, 5, 73 10 of 14
3. Results
3.1. Bibliographic Search
A total of 2824 records were retrieved through our searches in Medline and EMBASE databases.
Following reading the titles and abstractsof the retrievedrecords 212remained for further
evaluation. Another 194 articles were excluded after reading the full article. Figure 1 shows the exact
sequence and process of study identification, selection and exclusion in each step of the search.
Finally, 18 studies were considered to be appropriate for answering our primary research question.
3. Results
3.1. Bibliographic Search
A total of 2824 records were retrieved through our searches in Medline and EMBASE databases.
Following reading the titles and abstracts of the retrieved records 212 remained for further evaluation.
Another 194 articles were excluded after reading the full article. Figure 1 shows the exact sequence and
process of study identification, selection and exclusion in each step of the search. Finally, 18 studies
were considered to be appropriate for answering our primary research question.
Healthcare 2017, 5, 73 10 of 14
3. Results
3.1. Bibliographic Search
A total of 2824 records were retrieved through our searches in Medline and EMBASE databases.
Following reading the titles and abstractsof the retrievedrecords 212remained for further
evaluation. Another 194 articles were excluded after reading the full article. Figure 1 shows the exact
sequence and process of study identification, selection and exclusion in each step of the search.
Finally, 18 studies were considered to be appropriate for answering our primary research question.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



