Nursing Case Study: Leonard's Risk Factors and Interventions
VerifiedAdded on 2021/04/17
|11
|2660
|50
Case Study
AI Summary
This case study analyzes the health risks of Leonard, a 73-year-old man with a history of mild cognitive impairment, anemia, and other health issues, who was admitted to the emergency department after a fall. The assignment identifies three key risk factors: potential for Alzheimer's disease, risk of serious fall injuries, and severe anemia. It outlines the clinical reasoning cycle, including patient situation, information collection, issue identification, goal establishment, action planning, and outcome evaluation. The study evaluates the Mini-Mental State Examination (MMSE), Falls Risk Assessment Tool (FRAT), and Body Mass Index (BMI) as best-practice assessment tools. Furthermore, it details nursing interventions to support Leonard, including strategies for managing Alzheimer's symptoms, preventing falls, and addressing weight management, linking these interventions to the responsibilities of health professionals. The interventions include promoting self-care, social interaction, physical therapy, and nutritional support. Finally, it proposes evaluation methods such as weight charts, fall incidence tracking, and the MMSE scale to assess the effectiveness of the interventions.

NURSING CASE STUDY
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Criteria – 1........................................................................................................................... 3
Identification of Leonards three health risk factors using Clinical Reasoning
Cycle....................................................................................................................................... 3
Patient situation and collecting information...................................................................3
Collecting and processing information.............................................................................. 3
Identification of issues............................................................................................................ 4
Establishing goals..................................................................................................................... 4
Taking action............................................................................................................................. 4
Evaluating outcomes............................................................................................................... 4
Criteria -2............................................................................................................................. 5
Evaluating three best-practice assessment tools for Leonard case..................5
Criteria – 3........................................................................................................................... 6
Identification and discussion of interventions that will support Leonard
and analyse the relation of these interventions with duties of health
professional........................................................................................................................ 6
For Alzheimer’s disease.......................................................................................................... 6
Fall Management...................................................................................................................... 7
Weight management................................................................................................................ 7
References........................................................................................................................... 9
Criteria – 1........................................................................................................................... 3
Identification of Leonards three health risk factors using Clinical Reasoning
Cycle....................................................................................................................................... 3
Patient situation and collecting information...................................................................3
Collecting and processing information.............................................................................. 3
Identification of issues............................................................................................................ 4
Establishing goals..................................................................................................................... 4
Taking action............................................................................................................................. 4
Evaluating outcomes............................................................................................................... 4
Criteria -2............................................................................................................................. 5
Evaluating three best-practice assessment tools for Leonard case..................5
Criteria – 3........................................................................................................................... 6
Identification and discussion of interventions that will support Leonard
and analyse the relation of these interventions with duties of health
professional........................................................................................................................ 6
For Alzheimer’s disease.......................................................................................................... 6
Fall Management...................................................................................................................... 7
Weight management................................................................................................................ 7
References........................................................................................................................... 9
Criteria – 1
Identification of Leonards three health risk factors using Clinical Reasoning
Cycle
Patient situation and collecting information
In the provided case study, Leonard is a 73 years old male living alone without
any family in the community. His wife died a few years back and he has no children.
He had left his job few years’ back and is not working right now. He has a medical
history of mild cognitive impairment, anaemia, industrial deafness, decubitus ulcer on
left leg shin, and arthritis in lower back, mild hypotension and urinary incontinence.
He was diagnosed with mild cognitive impairment around 3 years ago but his Mini-
Mental State Examination (MMSE) score was 25/30 12 months ago, which is a
normal cognitive score.
However, from last 6 months, Leonard is getting socially isolated spending most of
the time at home. He is showing lack of interest in his usual activities, feeling tired
and sleeping most of the day. Further, in these last 6 months, his daily functioning is
also deteriorated and he had two falls incidence with this duration. In the present
situation, Leonard is admitted to the emergency department after third fall incidence.
He is having bruising on face and hip, mild confusion, low body weight and anxiety.
He is unable to walk and stand properly in hospital observations. Leonard also needs
help with transfers and self-care activities. He is also facing difficulty in planning
personal tasks.
Collecting and processing information
As per provided information, Leonard was a victim of mild cognitive
impairment that risk to Alzheimer’s disease. His MMSE was normal around 1 year
ago as per his MMSE score of 25/30 but his recent symptoms from past 6 months are
not proper that involves mild confusion, social isolation, problem planning task,
improper self-management (Dong et al. 2012). Further, he had two major fall
incidence in past that involves fall from stairs and fall from bed in the night. His
recent fall incidence was also a serious one where he falls at a local shop and admitted
to the emergency department. This fall incidence increases his risk of serious injury
Identification of Leonards three health risk factors using Clinical Reasoning
Cycle
Patient situation and collecting information
In the provided case study, Leonard is a 73 years old male living alone without
any family in the community. His wife died a few years back and he has no children.
He had left his job few years’ back and is not working right now. He has a medical
history of mild cognitive impairment, anaemia, industrial deafness, decubitus ulcer on
left leg shin, and arthritis in lower back, mild hypotension and urinary incontinence.
He was diagnosed with mild cognitive impairment around 3 years ago but his Mini-
Mental State Examination (MMSE) score was 25/30 12 months ago, which is a
normal cognitive score.
However, from last 6 months, Leonard is getting socially isolated spending most of
the time at home. He is showing lack of interest in his usual activities, feeling tired
and sleeping most of the day. Further, in these last 6 months, his daily functioning is
also deteriorated and he had two falls incidence with this duration. In the present
situation, Leonard is admitted to the emergency department after third fall incidence.
He is having bruising on face and hip, mild confusion, low body weight and anxiety.
He is unable to walk and stand properly in hospital observations. Leonard also needs
help with transfers and self-care activities. He is also facing difficulty in planning
personal tasks.
Collecting and processing information
As per provided information, Leonard was a victim of mild cognitive
impairment that risk to Alzheimer’s disease. His MMSE was normal around 1 year
ago as per his MMSE score of 25/30 but his recent symptoms from past 6 months are
not proper that involves mild confusion, social isolation, problem planning task,
improper self-management (Dong et al. 2012). Further, he had two major fall
incidence in past that involves fall from stairs and fall from bed in the night. His
recent fall incidence was also a serious one where he falls at a local shop and admitted
to the emergency department. This fall incidence increases his risk of serious injury
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
(Robinson et al. 2014). Leonard was anaemic as per his past medical history. In recent
symptom at the hospital he is considered underweight. Further, Leonard requires help
in work like shopping and cleaning because he took help from his Home and
Community Care (HACC) services. This indicates a risk of severe anaemia that can
cause complication with growing age.
Identification of issues
As per provided information analysis, the three risk factors or issues in
Leonard case involves risk to Alzheimer’s disease, serious fall injuries and severe
anaemia as per his growing age.
Establishing goals
For the identified risk factors the nursing goals involve: -
Minimizing the complication of Alzheimer’s disease
Providing support services to control fall incidence
Provide proper fluid and food intake to enhance better health and overcome
low body weight condition.
Taking action
The fulfilment of these goals would require proper nursing interventions that
should be performed by the healthcare professional to overcome risk conditions in
Mr. Leonard’s case. These nursing interventions are discussed in the below-provided
section of this essay.
Evaluating outcomes
The fulfilment of mentioned nursing goals could be evaluated using specific
evaluation tools and monitoring strategies. For detecting betterment in weight and
health, a proper monitoring chart (weight management chart) should be developed
where the weight of every week should be noted till 6 months to achieve targeted
goal. Further, control over fall incidence can be determined using an observation chart
for 6 months time duration where the number of fall incidence should be noted and
this observation should continue till the fall incidence stop completely. Lastly, the
MMSE scale is perfect to evaluate control over cognitive condition minimising the
risk of Alzheimer’s disease.
symptom at the hospital he is considered underweight. Further, Leonard requires help
in work like shopping and cleaning because he took help from his Home and
Community Care (HACC) services. This indicates a risk of severe anaemia that can
cause complication with growing age.
Identification of issues
As per provided information analysis, the three risk factors or issues in
Leonard case involves risk to Alzheimer’s disease, serious fall injuries and severe
anaemia as per his growing age.
Establishing goals
For the identified risk factors the nursing goals involve: -
Minimizing the complication of Alzheimer’s disease
Providing support services to control fall incidence
Provide proper fluid and food intake to enhance better health and overcome
low body weight condition.
Taking action
The fulfilment of these goals would require proper nursing interventions that
should be performed by the healthcare professional to overcome risk conditions in
Mr. Leonard’s case. These nursing interventions are discussed in the below-provided
section of this essay.
Evaluating outcomes
The fulfilment of mentioned nursing goals could be evaluated using specific
evaluation tools and monitoring strategies. For detecting betterment in weight and
health, a proper monitoring chart (weight management chart) should be developed
where the weight of every week should be noted till 6 months to achieve targeted
goal. Further, control over fall incidence can be determined using an observation chart
for 6 months time duration where the number of fall incidence should be noted and
this observation should continue till the fall incidence stop completely. Lastly, the
MMSE scale is perfect to evaluate control over cognitive condition minimising the
risk of Alzheimer’s disease.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Criteria -2
Evaluating three best-practice assessment tools for Leonard case
The first identified issue in Leonard case is the risk to Alzheimer’s disease as
his medical history states mild cognition impairment with risk to Alzheimer’s disease.
His present social and medical conditions from last 6 months indicate a risk to
Alzheimer’s disease. As per Dong et al. (2012) study, the best assessment tool for
Alzheimer’s disease is Mini-Mental State Examination (MMSE). This test was
previously performed for Leonard 12 months ago but his condition from last 6 months
indicate towards the consequences of mild cognition impairment risking Alzheimer’s
disease. According to Paillard et al. (2015), early diagnosis of Alzheimer’s disease
can help to support and medicate reversing the effect of the disease. However, there is
no single assessment tool to detect cognitive impairment yet MMSE is most widely
used tool that is used to detect cognitive situation within 10-15 minutes of duration
with detailed analysis using 30 questions.
The second tool appropriate to assess and prevent fall incidence in case of
Leonard is Falls Risk Assessment Tool (FRAT) (Hempel et al. 2013). This tool was
developed in 1999 and is considered the most reliable tool for fall incidence
management and prevention till date (Moorhead et al. 2014). According to Hnizdo et
al. (2013) study, FRAT involves a three-part assessment where Part -1 determined
falls risk status, Part-2 detects risk factor checklist and Part-3 is the action plan for
recovery. Lastly, a review chart is constructed to revise the care plan as per detected
risk status each time FRAT assessment is performed for the patient.
Lastly, the third risk issue involves low body weight and risk of anaemia in
Leonard’s case. For this issue, the most suitable assessment tool is Body Mass Index
ratio (BMI) because this tool determines body weight as well as estimate health risk
related to body weight (Moorhead et al. 2014). The BMI tool measure as analyses
body weight as per height and mass (muscle or fat) that help to detect health risk if
there is extra fat in the body. Any patient can perform BMI using machine available
that automatically determines the health condition (Herdman, 2011). In case of
Leonard, BMI tool will work to maintain a healthy body weight assuring no risk of
anaemia.
Evaluating three best-practice assessment tools for Leonard case
The first identified issue in Leonard case is the risk to Alzheimer’s disease as
his medical history states mild cognition impairment with risk to Alzheimer’s disease.
His present social and medical conditions from last 6 months indicate a risk to
Alzheimer’s disease. As per Dong et al. (2012) study, the best assessment tool for
Alzheimer’s disease is Mini-Mental State Examination (MMSE). This test was
previously performed for Leonard 12 months ago but his condition from last 6 months
indicate towards the consequences of mild cognition impairment risking Alzheimer’s
disease. According to Paillard et al. (2015), early diagnosis of Alzheimer’s disease
can help to support and medicate reversing the effect of the disease. However, there is
no single assessment tool to detect cognitive impairment yet MMSE is most widely
used tool that is used to detect cognitive situation within 10-15 minutes of duration
with detailed analysis using 30 questions.
The second tool appropriate to assess and prevent fall incidence in case of
Leonard is Falls Risk Assessment Tool (FRAT) (Hempel et al. 2013). This tool was
developed in 1999 and is considered the most reliable tool for fall incidence
management and prevention till date (Moorhead et al. 2014). According to Hnizdo et
al. (2013) study, FRAT involves a three-part assessment where Part -1 determined
falls risk status, Part-2 detects risk factor checklist and Part-3 is the action plan for
recovery. Lastly, a review chart is constructed to revise the care plan as per detected
risk status each time FRAT assessment is performed for the patient.
Lastly, the third risk issue involves low body weight and risk of anaemia in
Leonard’s case. For this issue, the most suitable assessment tool is Body Mass Index
ratio (BMI) because this tool determines body weight as well as estimate health risk
related to body weight (Moorhead et al. 2014). The BMI tool measure as analyses
body weight as per height and mass (muscle or fat) that help to detect health risk if
there is extra fat in the body. Any patient can perform BMI using machine available
that automatically determines the health condition (Herdman, 2011). In case of
Leonard, BMI tool will work to maintain a healthy body weight assuring no risk of
anaemia.
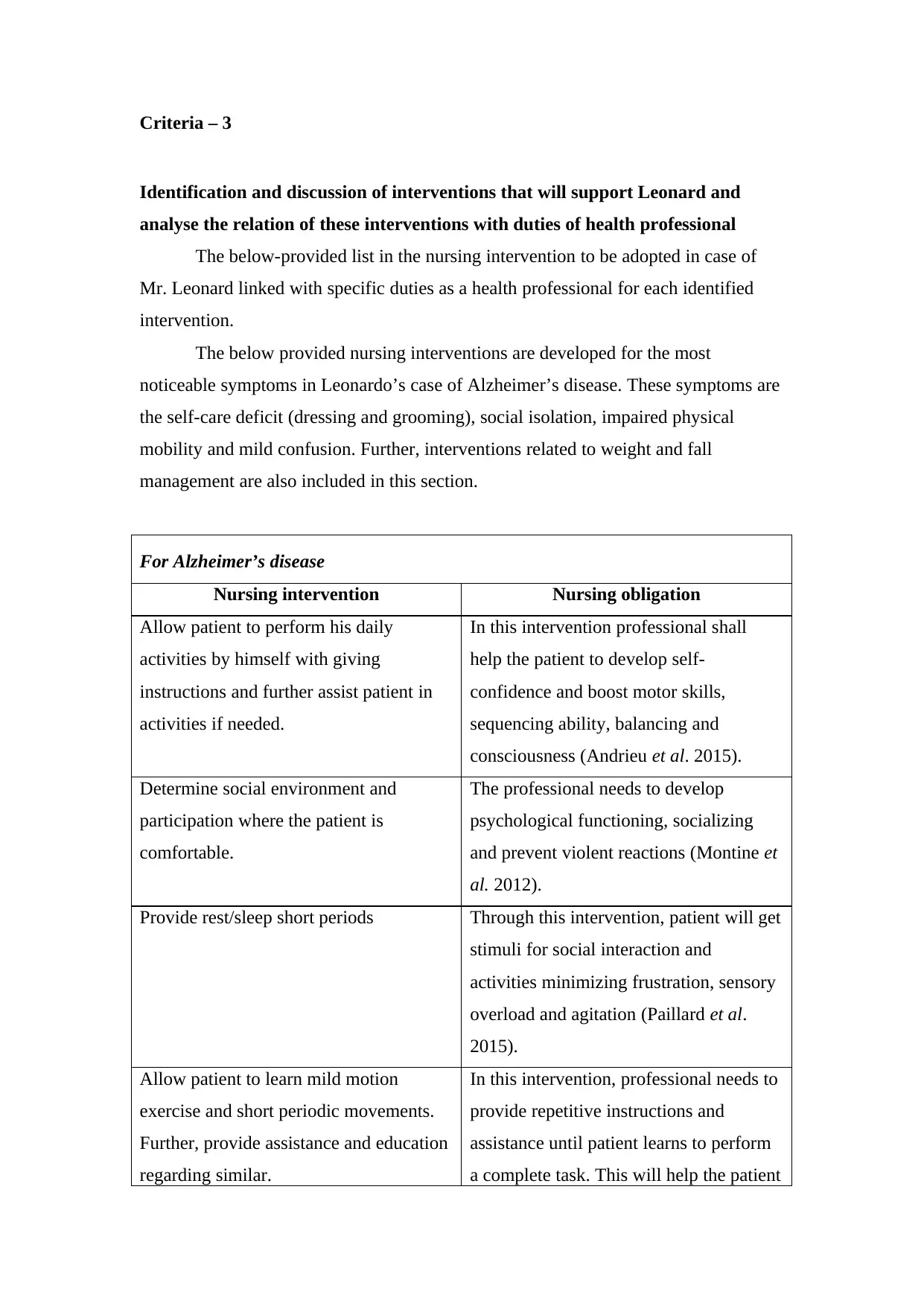
Criteria – 3
Identification and discussion of interventions that will support Leonard and
analyse the relation of these interventions with duties of health professional
The below-provided list in the nursing intervention to be adopted in case of
Mr. Leonard linked with specific duties as a health professional for each identified
intervention.
The below provided nursing interventions are developed for the most
noticeable symptoms in Leonardo’s case of Alzheimer’s disease. These symptoms are
the self-care deficit (dressing and grooming), social isolation, impaired physical
mobility and mild confusion. Further, interventions related to weight and fall
management are also included in this section.
For Alzheimer’s disease
Nursing intervention Nursing obligation
Allow patient to perform his daily
activities by himself with giving
instructions and further assist patient in
activities if needed.
In this intervention professional shall
help the patient to develop self-
confidence and boost motor skills,
sequencing ability, balancing and
consciousness (Andrieu et al. 2015).
Determine social environment and
participation where the patient is
comfortable.
The professional needs to develop
psychological functioning, socializing
and prevent violent reactions (Montine et
al. 2012).
Provide rest/sleep short periods Through this intervention, patient will get
stimuli for social interaction and
activities minimizing frustration, sensory
overload and agitation (Paillard et al.
2015).
Allow patient to learn mild motion
exercise and short periodic movements.
Further, provide assistance and education
regarding similar.
In this intervention, professional needs to
provide repetitive instructions and
assistance until patient learns to perform
a complete task. This will help the patient
Identification and discussion of interventions that will support Leonard and
analyse the relation of these interventions with duties of health professional
The below-provided list in the nursing intervention to be adopted in case of
Mr. Leonard linked with specific duties as a health professional for each identified
intervention.
The below provided nursing interventions are developed for the most
noticeable symptoms in Leonardo’s case of Alzheimer’s disease. These symptoms are
the self-care deficit (dressing and grooming), social isolation, impaired physical
mobility and mild confusion. Further, interventions related to weight and fall
management are also included in this section.
For Alzheimer’s disease
Nursing intervention Nursing obligation
Allow patient to perform his daily
activities by himself with giving
instructions and further assist patient in
activities if needed.
In this intervention professional shall
help the patient to develop self-
confidence and boost motor skills,
sequencing ability, balancing and
consciousness (Andrieu et al. 2015).
Determine social environment and
participation where the patient is
comfortable.
The professional needs to develop
psychological functioning, socializing
and prevent violent reactions (Montine et
al. 2012).
Provide rest/sleep short periods Through this intervention, patient will get
stimuli for social interaction and
activities minimizing frustration, sensory
overload and agitation (Paillard et al.
2015).
Allow patient to learn mild motion
exercise and short periodic movements.
Further, provide assistance and education
regarding similar.
In this intervention, professional needs to
provide repetitive instructions and
assistance until patient learns to perform
a complete task. This will help the patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
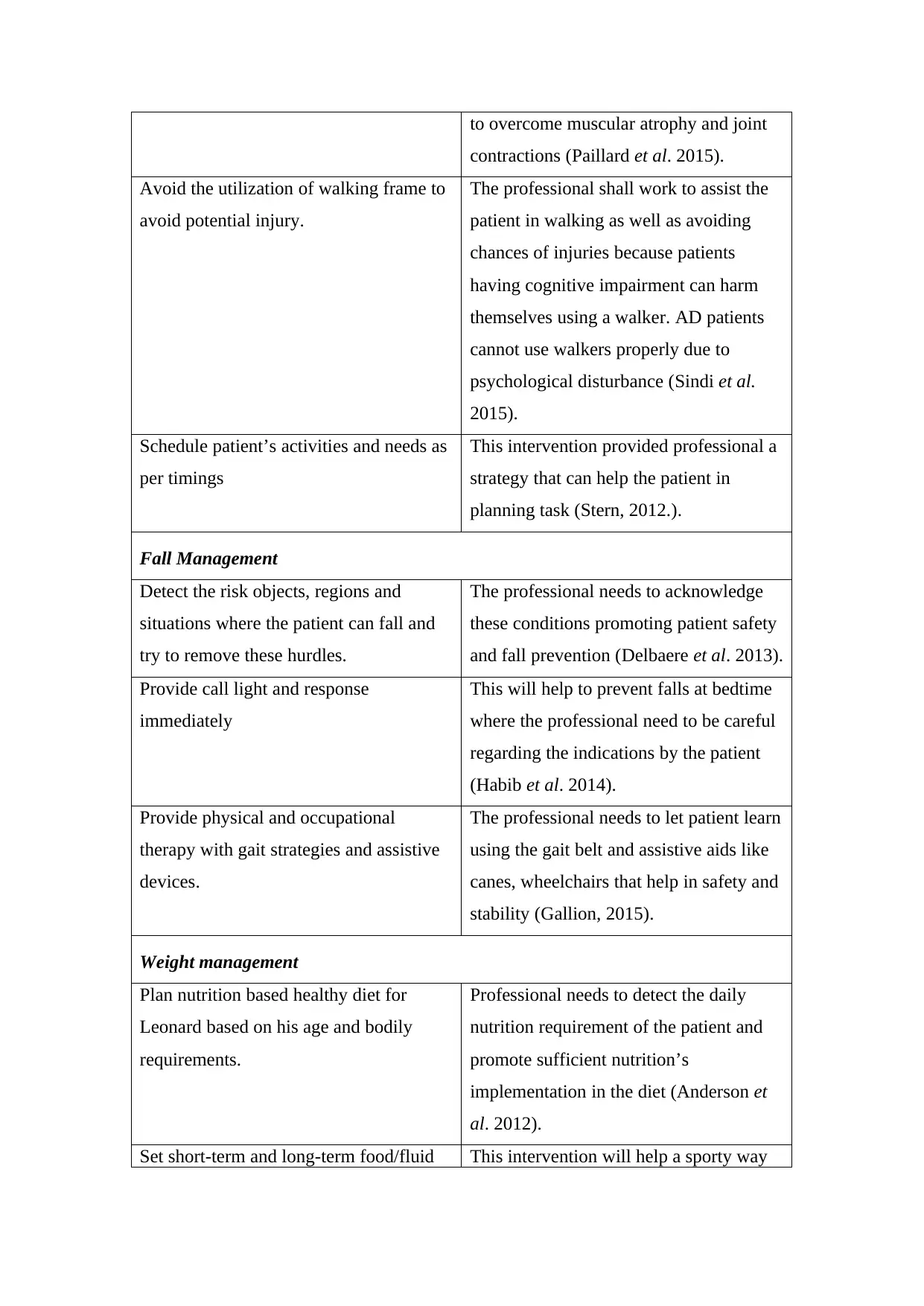
to overcome muscular atrophy and joint
contractions (Paillard et al. 2015).
Avoid the utilization of walking frame to
avoid potential injury.
The professional shall work to assist the
patient in walking as well as avoiding
chances of injuries because patients
having cognitive impairment can harm
themselves using a walker. AD patients
cannot use walkers properly due to
psychological disturbance (Sindi et al.
2015).
Schedule patient’s activities and needs as
per timings
This intervention provided professional a
strategy that can help the patient in
planning task (Stern, 2012.).
Fall Management
Detect the risk objects, regions and
situations where the patient can fall and
try to remove these hurdles.
The professional needs to acknowledge
these conditions promoting patient safety
and fall prevention (Delbaere et al. 2013).
Provide call light and response
immediately
This will help to prevent falls at bedtime
where the professional need to be careful
regarding the indications by the patient
(Habib et al. 2014).
Provide physical and occupational
therapy with gait strategies and assistive
devices.
The professional needs to let patient learn
using the gait belt and assistive aids like
canes, wheelchairs that help in safety and
stability (Gallion, 2015).
Weight management
Plan nutrition based healthy diet for
Leonard based on his age and bodily
requirements.
Professional needs to detect the daily
nutrition requirement of the patient and
promote sufficient nutrition’s
implementation in the diet (Anderson et
al. 2012).
Set short-term and long-term food/fluid This intervention will help a sporty way
contractions (Paillard et al. 2015).
Avoid the utilization of walking frame to
avoid potential injury.
The professional shall work to assist the
patient in walking as well as avoiding
chances of injuries because patients
having cognitive impairment can harm
themselves using a walker. AD patients
cannot use walkers properly due to
psychological disturbance (Sindi et al.
2015).
Schedule patient’s activities and needs as
per timings
This intervention provided professional a
strategy that can help the patient in
planning task (Stern, 2012.).
Fall Management
Detect the risk objects, regions and
situations where the patient can fall and
try to remove these hurdles.
The professional needs to acknowledge
these conditions promoting patient safety
and fall prevention (Delbaere et al. 2013).
Provide call light and response
immediately
This will help to prevent falls at bedtime
where the professional need to be careful
regarding the indications by the patient
(Habib et al. 2014).
Provide physical and occupational
therapy with gait strategies and assistive
devices.
The professional needs to let patient learn
using the gait belt and assistive aids like
canes, wheelchairs that help in safety and
stability (Gallion, 2015).
Weight management
Plan nutrition based healthy diet for
Leonard based on his age and bodily
requirements.
Professional needs to detect the daily
nutrition requirement of the patient and
promote sufficient nutrition’s
implementation in the diet (Anderson et
al. 2012).
Set short-term and long-term food/fluid This intervention will help a sporty way
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
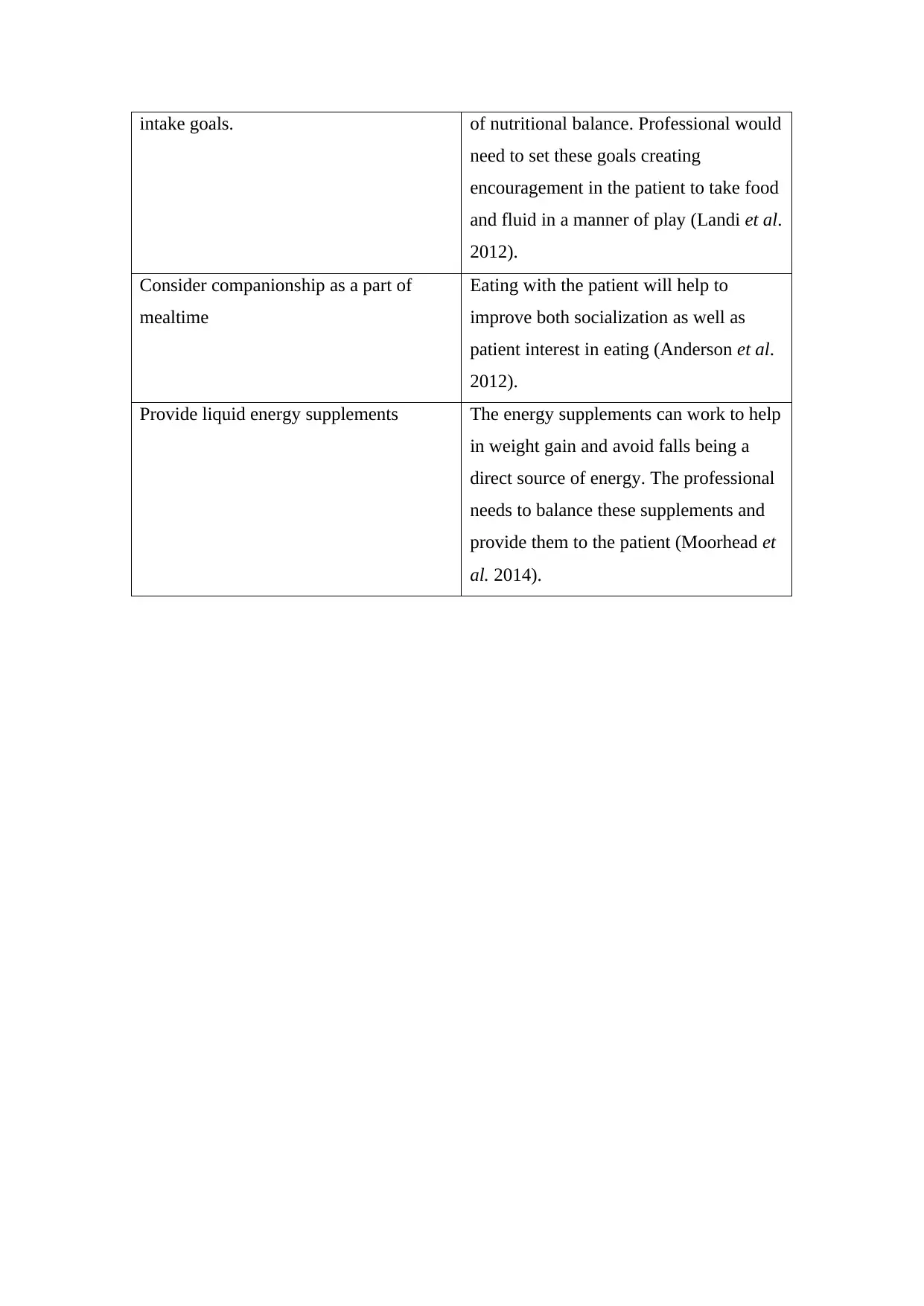
intake goals. of nutritional balance. Professional would
need to set these goals creating
encouragement in the patient to take food
and fluid in a manner of play (Landi et al.
2012).
Consider companionship as a part of
mealtime
Eating with the patient will help to
improve both socialization as well as
patient interest in eating (Anderson et al.
2012).
Provide liquid energy supplements The energy supplements can work to help
in weight gain and avoid falls being a
direct source of energy. The professional
needs to balance these supplements and
provide them to the patient (Moorhead et
al. 2014).
need to set these goals creating
encouragement in the patient to take food
and fluid in a manner of play (Landi et al.
2012).
Consider companionship as a part of
mealtime
Eating with the patient will help to
improve both socialization as well as
patient interest in eating (Anderson et al.
2012).
Provide liquid energy supplements The energy supplements can work to help
in weight gain and avoid falls being a
direct source of energy. The professional
needs to balance these supplements and
provide them to the patient (Moorhead et
al. 2014).
References
Books
Herdman, T.H. ed., 2011. Nursing diagnoses 2012-14: definitions and classification.
John Wiley & Sons.
Moorhead, S., Johnson, M., Maas, M.L. and Swanson, E., 2014. Nursing Outcomes
Classification (NOC)-E-Book: Measurement of Health Outcomes. Elsevier Health
Sciences.
Journals
Anderson, G.H., Foreyt, J., Sigman-Grant, M. and Allison, D.B., 2012. The Use of
Low-Calorie Sweeteners by Adults: Impact on Weight Management–3. The Journal
of nutrition, 142(6), pp.1163s-1169s.
Andrieu, S., Coley, N., Lovestone, S., Aisen, P.S. and Vellas, B., 2015. Prevention of
sporadic Alzheimer's disease: lessons learned from clinical trials and future
directions. The Lancet Neurology, 14(9), pp.926-944.
Delbaere, K., Sherrington, C. and Lord, S.R., 2013. Falls prevention interventions.
In Osteoporosis (Fourth Edition) (pp. 1649-1666).
Dong, Y., Lee, W.Y., Basri, N.A., Collinson, S.L., Merchant, R.A.,
Venketasubramanian, N. and Chen, C.L.H., 2012. The Montreal Cognitive
Assessment is superior to the Mini–Mental State Examination in detecting patients at
higher risk of dementia. International Psychogeriatrics, 24(11), pp.1749-1755.
Gallion, A.D., 2015. Improving a Fall Prevention and Management Program in an
Acute Care Setting.
Habib, M.A., Mohktar, M.S., Kamaruzzaman, S.B., Lim, K.S., Pin, T.M. and Ibrahim,
F., 2014. Smartphone-based solutions for fall detection and prevention: challenges
and open issues. Sensors, 14(4), pp.7181-7208.
Books
Herdman, T.H. ed., 2011. Nursing diagnoses 2012-14: definitions and classification.
John Wiley & Sons.
Moorhead, S., Johnson, M., Maas, M.L. and Swanson, E., 2014. Nursing Outcomes
Classification (NOC)-E-Book: Measurement of Health Outcomes. Elsevier Health
Sciences.
Journals
Anderson, G.H., Foreyt, J., Sigman-Grant, M. and Allison, D.B., 2012. The Use of
Low-Calorie Sweeteners by Adults: Impact on Weight Management–3. The Journal
of nutrition, 142(6), pp.1163s-1169s.
Andrieu, S., Coley, N., Lovestone, S., Aisen, P.S. and Vellas, B., 2015. Prevention of
sporadic Alzheimer's disease: lessons learned from clinical trials and future
directions. The Lancet Neurology, 14(9), pp.926-944.
Delbaere, K., Sherrington, C. and Lord, S.R., 2013. Falls prevention interventions.
In Osteoporosis (Fourth Edition) (pp. 1649-1666).
Dong, Y., Lee, W.Y., Basri, N.A., Collinson, S.L., Merchant, R.A.,
Venketasubramanian, N. and Chen, C.L.H., 2012. The Montreal Cognitive
Assessment is superior to the Mini–Mental State Examination in detecting patients at
higher risk of dementia. International Psychogeriatrics, 24(11), pp.1749-1755.
Gallion, A.D., 2015. Improving a Fall Prevention and Management Program in an
Acute Care Setting.
Habib, M.A., Mohktar, M.S., Kamaruzzaman, S.B., Lim, K.S., Pin, T.M. and Ibrahim,
F., 2014. Smartphone-based solutions for fall detection and prevention: challenges
and open issues. Sensors, 14(4), pp.7181-7208.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Hempel, S., Newberry, S., Wang, Z., Booth, M., Shanman, R., Johnsen, B., Shier, V.,
Saliba, D., Spector, W.D. and Ganz, D.A., 2013. Hospital fall prevention: a
systematic review of implementation, components, adherence, and
effectiveness. Journal of the American Geriatrics Society, 61(4), pp.483-494.
Hnizdo, S., Archuleta, R.A., Taylor, B. and Kim, S.C., 2013. Validity and reliability
of the modified John Hopkins Fall Risk Assessment Tool for elderly patients in home
health care. Geriatric nursing, 34(5), pp.423-427.
Landi, F., Liperoti, R., Fusco, D., Mastropaolo, S., Quattrociocchi, D., Proia, A.,
Tosato, M., Bernabei, R. and Onder, G., 2012. Sarcopenia and mortality among older
nursing home residents. Journal of the American Medical Directors
Association, 13(2), pp.121-126.
Montine, T.J., Phelps, C.H., Beach, T.G., Bigio, E.H., Cairns, N.J., Dickson, D.W.,
Duyckaerts, C., Frosch, M.P., Masliah, E., Mirra, S.S. and Nelson, P.T., 2012.
National Institute on Aging–Alzheimer’s Association guidelines for the
neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta
neuropathologica, 123(1), pp.1-11.
Paillard, T., Rolland, Y. and de Souto Barreto, P., 2015. Protective effects of physical
exercise in Alzheimer's disease and Parkinson's disease: a narrative review. Journal of
clinical neurology, 11(3), pp.212-219.
Robinson, L., Newton, J.L., Jones, D. and Dawson, P., 2014. Self-management and
adherence with exercise-based falls prevention programmes: a qualitative study to
explore the views and experiences of older people and physiotherapists. Disability
and rehabilitation, 36(5), pp.379-386.
Sindi, S., Mangialasche, F. and Kivipelto, M., 2015. Advances in the prevention of
Alzheimer's Disease. F1000prime reports, 7.
Stern, Y., 2012. Cognitive reserve in ageing and Alzheimer's disease. The Lancet
Saliba, D., Spector, W.D. and Ganz, D.A., 2013. Hospital fall prevention: a
systematic review of implementation, components, adherence, and
effectiveness. Journal of the American Geriatrics Society, 61(4), pp.483-494.
Hnizdo, S., Archuleta, R.A., Taylor, B. and Kim, S.C., 2013. Validity and reliability
of the modified John Hopkins Fall Risk Assessment Tool for elderly patients in home
health care. Geriatric nursing, 34(5), pp.423-427.
Landi, F., Liperoti, R., Fusco, D., Mastropaolo, S., Quattrociocchi, D., Proia, A.,
Tosato, M., Bernabei, R. and Onder, G., 2012. Sarcopenia and mortality among older
nursing home residents. Journal of the American Medical Directors
Association, 13(2), pp.121-126.
Montine, T.J., Phelps, C.H., Beach, T.G., Bigio, E.H., Cairns, N.J., Dickson, D.W.,
Duyckaerts, C., Frosch, M.P., Masliah, E., Mirra, S.S. and Nelson, P.T., 2012.
National Institute on Aging–Alzheimer’s Association guidelines for the
neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta
neuropathologica, 123(1), pp.1-11.
Paillard, T., Rolland, Y. and de Souto Barreto, P., 2015. Protective effects of physical
exercise in Alzheimer's disease and Parkinson's disease: a narrative review. Journal of
clinical neurology, 11(3), pp.212-219.
Robinson, L., Newton, J.L., Jones, D. and Dawson, P., 2014. Self-management and
adherence with exercise-based falls prevention programmes: a qualitative study to
explore the views and experiences of older people and physiotherapists. Disability
and rehabilitation, 36(5), pp.379-386.
Sindi, S., Mangialasche, F. and Kivipelto, M., 2015. Advances in the prevention of
Alzheimer's Disease. F1000prime reports, 7.
Stern, Y., 2012. Cognitive reserve in ageing and Alzheimer's disease. The Lancet
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Neurology, 11(11), pp.1006-1012.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




