Limb-Girdle Muscular Dystrophy 2B: Pathophysiology and Clinical Impact
VerifiedAdded on 2023/06/16
|9
|1585
|430
Report
AI Summary
This report provides a comprehensive overview of Limb-Girdle Muscular Dystrophy type 2B (LGMD 2B), a rare genetic muscular dystrophy affecting the arms and legs. It explores the similarities and differences between LGMD 2B and other LGMD types, focusing on the genetic mutations, clinical symptoms, and disease progression. The report also examines the role of dysferlin, a protein crucial for muscle fiber function, and how its reduction or absence leads to muscle damage and the characteristic symptoms of LGMD 2B. The analysis includes insights into diagnosis, potential treatments, and the impact of the disease on affected individuals, highlighting the need for further research to develop effective therapies.

Running head: BIOLOGICAL SCIENCES
Limb Girdle Muscular Dystrophies
Name of the Student:
Name of the University:
Author Note:
Limb Girdle Muscular Dystrophies
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1BIOLOGICAL SCIENCES
Table of contents
Introduction......................................................................................................................................2
Limb-girdle muscular dystrophy type 2b........................................................................................2
LGMD 2B and other LGMDs..........................................................................................................3
Similarities...................................................................................................................................3
Differences...................................................................................................................................4
Dysferlin reduction and its effects...................................................................................................4
Conclusion.......................................................................................................................................5
Reference.........................................................................................................................................6
Table of contents
Introduction......................................................................................................................................2
Limb-girdle muscular dystrophy type 2b........................................................................................2
LGMD 2B and other LGMDs..........................................................................................................3
Similarities...................................................................................................................................3
Differences...................................................................................................................................4
Dysferlin reduction and its effects...................................................................................................4
Conclusion.......................................................................................................................................5
Reference.........................................................................................................................................6
2BIOLOGICAL SCIENCES
Introduction
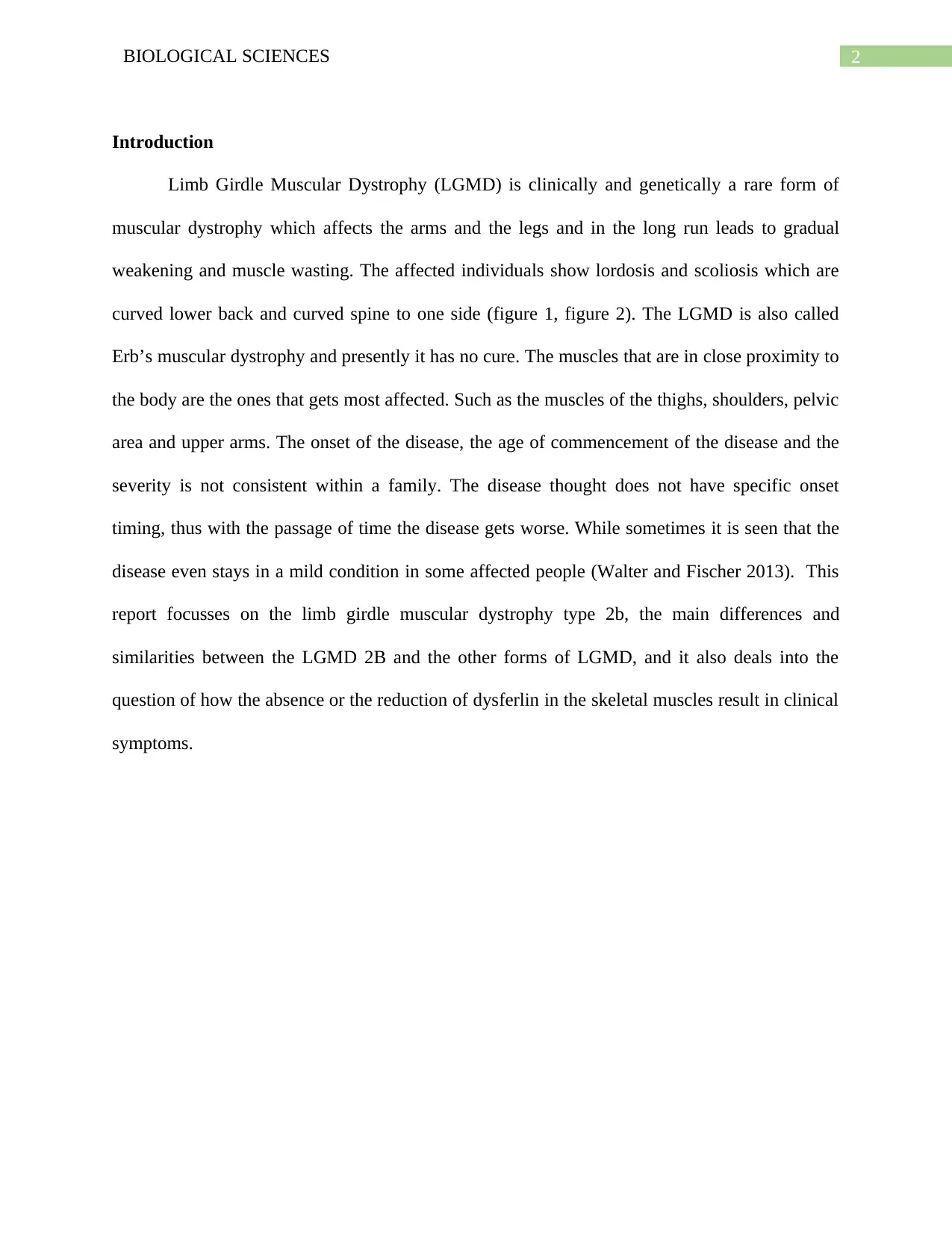
Limb Girdle Muscular Dystrophy (LGMD) is clinically and genetically a rare form of
muscular dystrophy which affects the arms and the legs and in the long run leads to gradual
weakening and muscle wasting. The affected individuals show lordosis and scoliosis which are
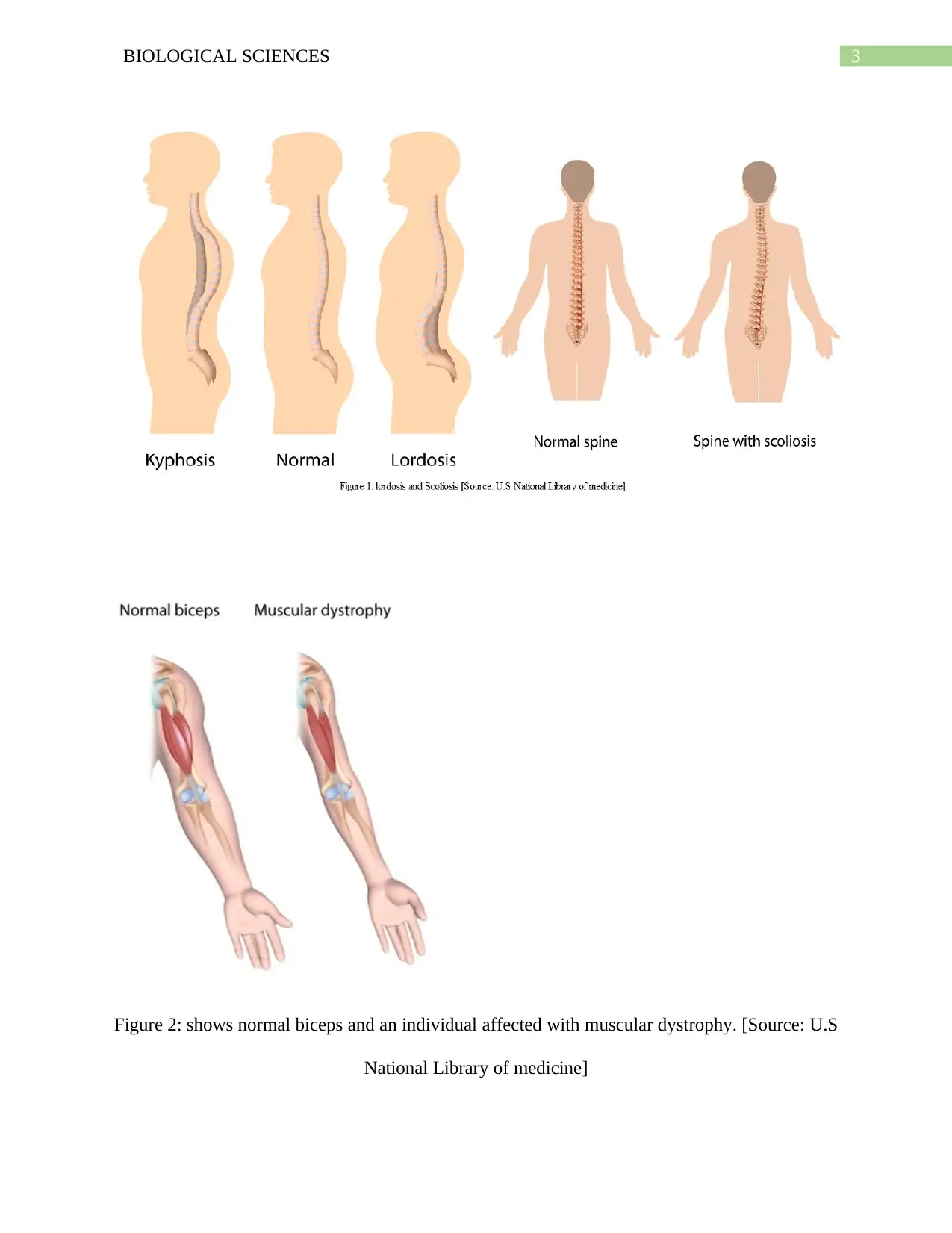
curved lower back and curved spine to one side (figure 1, figure 2). The LGMD is also called
Erb’s muscular dystrophy and presently it has no cure. The muscles that are in close proximity to
the body are the ones that gets most affected. Such as the muscles of the thighs, shoulders, pelvic
area and upper arms. The onset of the disease, the age of commencement of the disease and the
severity is not consistent within a family. The disease thought does not have specific onset
timing, thus with the passage of time the disease gets worse. While sometimes it is seen that the
disease even stays in a mild condition in some affected people (Walter and Fischer 2013). This
report focusses on the limb girdle muscular dystrophy type 2b, the main differences and
similarities between the LGMD 2B and the other forms of LGMD, and it also deals into the
question of how the absence or the reduction of dysferlin in the skeletal muscles result in clinical
symptoms.
Introduction
Limb Girdle Muscular Dystrophy (LGMD) is clinically and genetically a rare form of
muscular dystrophy which affects the arms and the legs and in the long run leads to gradual
weakening and muscle wasting. The affected individuals show lordosis and scoliosis which are
curved lower back and curved spine to one side (figure 1, figure 2). The LGMD is also called
Erb’s muscular dystrophy and presently it has no cure. The muscles that are in close proximity to
the body are the ones that gets most affected. Such as the muscles of the thighs, shoulders, pelvic
area and upper arms. The onset of the disease, the age of commencement of the disease and the
severity is not consistent within a family. The disease thought does not have specific onset
timing, thus with the passage of time the disease gets worse. While sometimes it is seen that the
disease even stays in a mild condition in some affected people (Walter and Fischer 2013). This
report focusses on the limb girdle muscular dystrophy type 2b, the main differences and
similarities between the LGMD 2B and the other forms of LGMD, and it also deals into the
question of how the absence or the reduction of dysferlin in the skeletal muscles result in clinical
symptoms.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3BIOLOGICAL SCIENCES
Figure 2: shows normal biceps and an individual affected with muscular dystrophy. [Source: U.S
National Library of medicine]
Figure 2: shows normal biceps and an individual affected with muscular dystrophy. [Source: U.S
National Library of medicine]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4BIOLOGICAL SCIENCES
Limb-girdle muscular dystrophy type 2b
LGMD 2B is also known as Dysferlinopathy is one of the various forms of limb girdle
muscular dystrophy, which affects the muscles of the hips and the shoulders. LGMD 2B affects
at a very young age which has symptoms like atrophy (wasting) and weakness of the shoulder
and pelvic muscles. This disease generally affects at the within the age group of 15 to 36 years,
the legs primarily gets affected first. The other symptoms of this disease include the difficulty in
running and walking and also difficulty in tiptoeing. The respiratory patterns and the cardiac
muscles also behave abnormally. The disease though affects at a very young age, it progresses
gradually and the affected person after a period of 11 to 21 years get confined to wheelchair for
mobility. According to Takahashi et al. (2012), LGMD 2B is caused due to a mutation in the
dysferlin (DYSF) gene, the gene contains the information for the production of a protein which is
vital for muscle fibres. LGMD 2B or dysferlinopathy has two subtypes; one is Miyoshi (distal)
and the other is LGMD 2B (proximal). Both of the complications are caused due to the mutation
of the dysferlin gene, while Miyoshi myopathy shows symptoms of weakness in the calf muscles
of the lower limbs. LGMD 2B is inherited in autosomal recessive form. The disease has no
distinct treatment and involves stretching exercises and physical therapy, and for other
orthopedic complexities surgeries are required. LGMD 2B can be diagnosed by a muscle biopsy,
and also by a serum creatinine kinase (CK) blood test which after the test if shows elevated
levels of 100 times more than the normal confirms a problem in the muscles (Nigro and Savarese
2014). The other diagnosis also involves the confirmation of dysferlin mutation by doing a DNA
test from the blood sample.
Limb-girdle muscular dystrophy type 2b
LGMD 2B is also known as Dysferlinopathy is one of the various forms of limb girdle
muscular dystrophy, which affects the muscles of the hips and the shoulders. LGMD 2B affects
at a very young age which has symptoms like atrophy (wasting) and weakness of the shoulder
and pelvic muscles. This disease generally affects at the within the age group of 15 to 36 years,
the legs primarily gets affected first. The other symptoms of this disease include the difficulty in
running and walking and also difficulty in tiptoeing. The respiratory patterns and the cardiac
muscles also behave abnormally. The disease though affects at a very young age, it progresses
gradually and the affected person after a period of 11 to 21 years get confined to wheelchair for
mobility. According to Takahashi et al. (2012), LGMD 2B is caused due to a mutation in the
dysferlin (DYSF) gene, the gene contains the information for the production of a protein which is
vital for muscle fibres. LGMD 2B or dysferlinopathy has two subtypes; one is Miyoshi (distal)
and the other is LGMD 2B (proximal). Both of the complications are caused due to the mutation
of the dysferlin gene, while Miyoshi myopathy shows symptoms of weakness in the calf muscles
of the lower limbs. LGMD 2B is inherited in autosomal recessive form. The disease has no
distinct treatment and involves stretching exercises and physical therapy, and for other
orthopedic complexities surgeries are required. LGMD 2B can be diagnosed by a muscle biopsy,
and also by a serum creatinine kinase (CK) blood test which after the test if shows elevated
levels of 100 times more than the normal confirms a problem in the muscles (Nigro and Savarese
2014). The other diagnosis also involves the confirmation of dysferlin mutation by doing a DNA
test from the blood sample.
5BIOLOGICAL SCIENCES
LGMD 2B and other LGMDs
Similarities
When comparing LGMD 2B and other LGMDs there are several similarities which are
found and are mention as under:
Increased serum creatinine kinase in the blood is the first major symptom which is noticed in all
the major forms of LGMD. The progress of LGMD 2B along with LGMD 1C and LGMD 1B
shows a slow progress. Both the LGMD 2B and LGMD 2A and LGMD 1C does not affect the
heart and the breathing patterns (Iyadurai and Kassar 2014). The LGMD 2B and LGMD 1C
affects the calves which causes pain and swelling. In both LGMD 2B and LGMD 1A the age of
onset is around the adult stage (15 to 25 years). The pattern of inheritance of LGMD 2B is
autosomal recessive which is similar to LGMD 2A, LGMD 2C, LGMD 2D, LGMD 2E, LGMD
2F, LGMD 2G, LGMD 2H, LGMD 2I, LGMD 2J, LGMD 2K, LGMD 2L (Mohassel and
Bönnemann 2014).
Differences
The first major difference is that the main cause of LGMD 2B is because dysferlin gene
gets mutated. Although the rate of progress of the disease is slow in LGMD 2B, however rate is
extremely variable in LGMD 2C, 2D, 2E, 2F, 2I. Even in the course of the disease the heart and
breathing patterns are not affected in the LGMD 2B while in other LGMD types like LGMD 2C,
2D, 2E, 2F, 2I, 1B both breathing pattern and heart is affected. Compared to the other LGMD
types, fiber spilling and necrotic changes are observed in LGMD 2B. Another, a major difference
is the occurrence of subtypes of LGMD type 2B in the form of proximal and distal myopathy
which is not found in any other type of LGMD (Mercuri and Muntoni 2013).
LGMD 2B and other LGMDs
Similarities
When comparing LGMD 2B and other LGMDs there are several similarities which are
found and are mention as under:
Increased serum creatinine kinase in the blood is the first major symptom which is noticed in all
the major forms of LGMD. The progress of LGMD 2B along with LGMD 1C and LGMD 1B
shows a slow progress. Both the LGMD 2B and LGMD 2A and LGMD 1C does not affect the
heart and the breathing patterns (Iyadurai and Kassar 2014). The LGMD 2B and LGMD 1C
affects the calves which causes pain and swelling. In both LGMD 2B and LGMD 1A the age of
onset is around the adult stage (15 to 25 years). The pattern of inheritance of LGMD 2B is
autosomal recessive which is similar to LGMD 2A, LGMD 2C, LGMD 2D, LGMD 2E, LGMD
2F, LGMD 2G, LGMD 2H, LGMD 2I, LGMD 2J, LGMD 2K, LGMD 2L (Mohassel and
Bönnemann 2014).
Differences
The first major difference is that the main cause of LGMD 2B is because dysferlin gene
gets mutated. Although the rate of progress of the disease is slow in LGMD 2B, however rate is
extremely variable in LGMD 2C, 2D, 2E, 2F, 2I. Even in the course of the disease the heart and
breathing patterns are not affected in the LGMD 2B while in other LGMD types like LGMD 2C,
2D, 2E, 2F, 2I, 1B both breathing pattern and heart is affected. Compared to the other LGMD
types, fiber spilling and necrotic changes are observed in LGMD 2B. Another, a major difference
is the occurrence of subtypes of LGMD type 2B in the form of proximal and distal myopathy
which is not found in any other type of LGMD (Mercuri and Muntoni 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6BIOLOGICAL SCIENCES
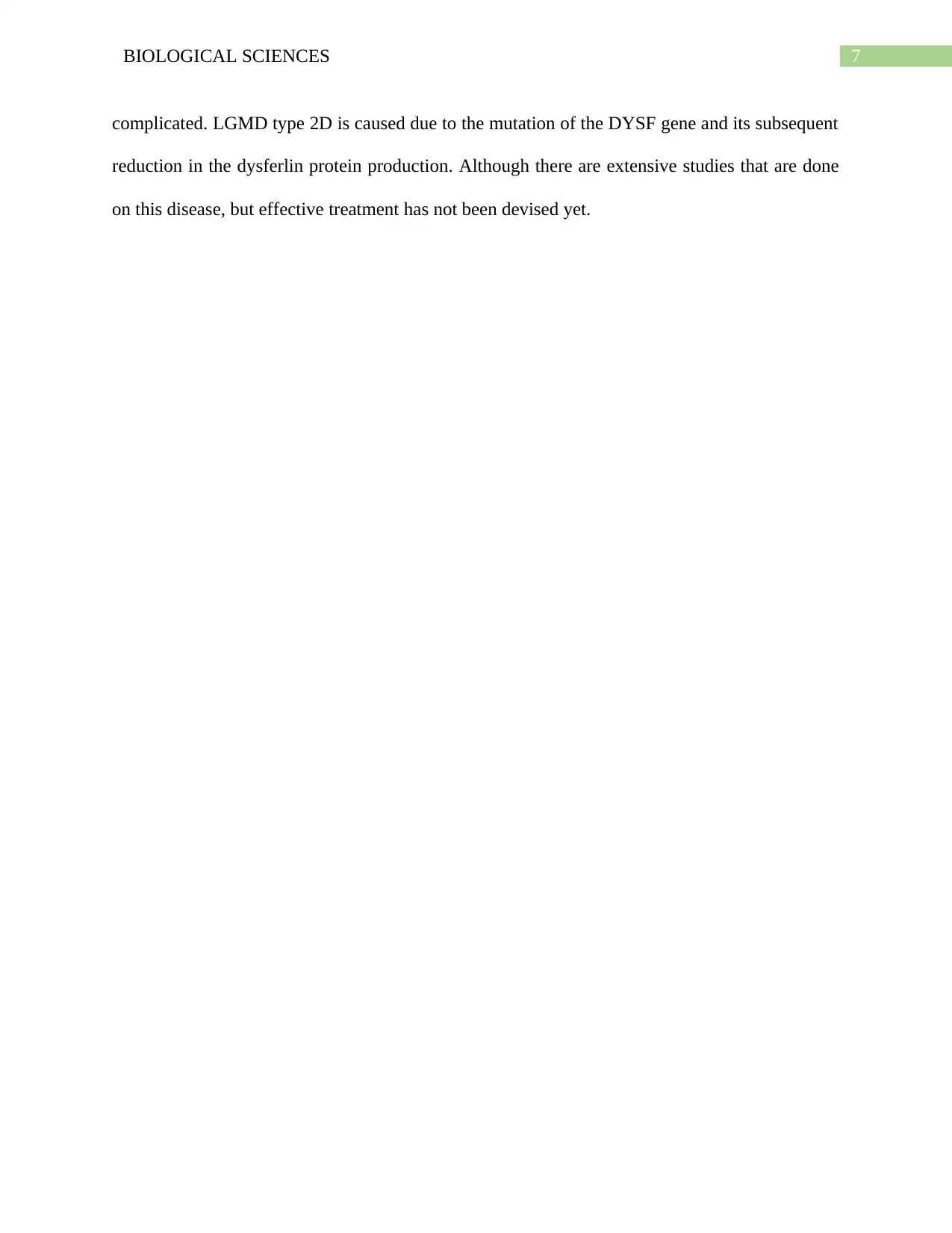
Dysferlin reduction and its effects
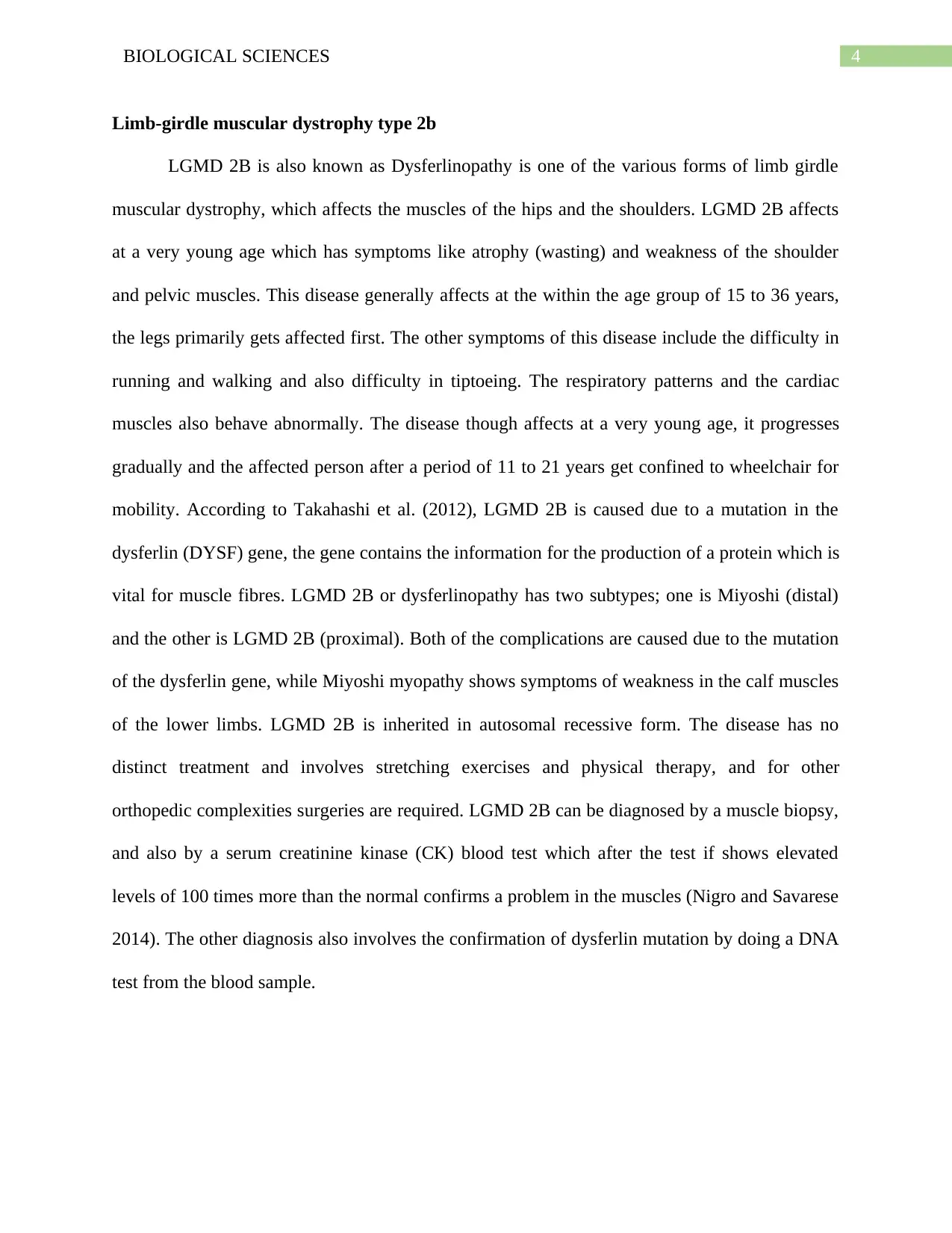
Figure 3: The location of DYSF gene that encodes dysferlin protein [Source: U.S National
Library of medicine]
Dysferlin is produced by the DYSF gene which is located in 2p12-14 chromosome (figure 3).
The muscle fiber that is deficient in dysferlin shows high incidence of vesicle accumulation near
the membrane lesions, which depicts that less levels of dysferlin reduces the chances of repair
and fusion of the plasma membrane with the vesicles. It has been found during a laser induced
experiment on the muscle fibers in vitro, the muscle fibres lacking the dysferlin took more
extracellular dyes than the normal muscle fibres. Which consolidated and proved the fact that
due to dysferlin deficiency vesicles are produced. Also, due to reduced levels of dysferlin the
damages to the plasma membrane of the skeletal muscles is not repaired which lead to cell death
(Nilsson et al. 2013). Although, skeletal muscles have the capability to regenerate new cells but
in the long run, it gets exhausted and the myocytes that are lost are substituted by fibrosis and fat
which further facilitates muscular dystrophy.
Conclusion
Therefore, from the above study it can be concluded that Limb Girdle Muscular
Dystrophy is a serious orthopedic complication which impairs a person’s mobility. However,
among all the other types of Limb Girdle Muscular Dystrophy, LGMD type 2D is more
Dysferlin reduction and its effects
Figure 3: The location of DYSF gene that encodes dysferlin protein [Source: U.S National
Library of medicine]
Dysferlin is produced by the DYSF gene which is located in 2p12-14 chromosome (figure 3).
The muscle fiber that is deficient in dysferlin shows high incidence of vesicle accumulation near
the membrane lesions, which depicts that less levels of dysferlin reduces the chances of repair
and fusion of the plasma membrane with the vesicles. It has been found during a laser induced
experiment on the muscle fibers in vitro, the muscle fibres lacking the dysferlin took more
extracellular dyes than the normal muscle fibres. Which consolidated and proved the fact that
due to dysferlin deficiency vesicles are produced. Also, due to reduced levels of dysferlin the
damages to the plasma membrane of the skeletal muscles is not repaired which lead to cell death
(Nilsson et al. 2013). Although, skeletal muscles have the capability to regenerate new cells but
in the long run, it gets exhausted and the myocytes that are lost are substituted by fibrosis and fat
which further facilitates muscular dystrophy.
Conclusion
Therefore, from the above study it can be concluded that Limb Girdle Muscular
Dystrophy is a serious orthopedic complication which impairs a person’s mobility. However,
among all the other types of Limb Girdle Muscular Dystrophy, LGMD type 2D is more
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7BIOLOGICAL SCIENCES
complicated. LGMD type 2D is caused due to the mutation of the DYSF gene and its subsequent
reduction in the dysferlin protein production. Although there are extensive studies that are done
on this disease, but effective treatment has not been devised yet.
complicated. LGMD type 2D is caused due to the mutation of the DYSF gene and its subsequent
reduction in the dysferlin protein production. Although there are extensive studies that are done
on this disease, but effective treatment has not been devised yet.
8BIOLOGICAL SCIENCES
Reference
Iyadurai, S.J.P. and Kassar, D., 2014. Limb-girdle muscular dystrophies. In Neuromuscular
Disorders in Clinical Practice(pp. 1231-1249). Springer New York.
Mercuri, E. and Muntoni, F., 2013. Muscular dystrophies. The Lancet, 381(9869), pp.845-860.
Mohassel, P. and Bönnemann, C.G., 2014. Limb-girdle Muscular Dystrophies.
In Neuromuscular Disorders of Infancy, Childhood, and Adolescence (Second Edition) (pp. 635-
666).
Nigro, V. and Savarese, M., 2014. Genetic basis of limb-girdle muscular dystrophies: the 2014
update. Acta Myologica, 33(1), p.1.
Nilsson, M.I., Laureano, M.L., Saeed, M. and Tarnopolsky, M.A., 2013. Dysferlin aggregation in
limb‐girdle muscular dystrophy type 2B/myoshi myopathy necessitates mutational screen for
diagnosis. Muscle & nerve, 47(5), pp.740-747.
Takahashi, T., Aoki, M., Suzuki, N., Tateyama, M., Yaginuma, C., Sato, H., Hayasaka, M.,
Sugawara, H., Ito, M., Abe-Kondo, E. and Shimakura, N., 2012. Clinical features and a mutation
with late onset of limb girdle muscular dystrophy 2B. J Neurol Neurosurg Psychiatry, pp.jnnp-
2011.
Walter, M.C. and Fischer, D., 2013. Limb Girdle Muscular Dystrophies. In Neuromuscular
Imaging (pp. 227-245). Springer New York.
Reference
Iyadurai, S.J.P. and Kassar, D., 2014. Limb-girdle muscular dystrophies. In Neuromuscular
Disorders in Clinical Practice(pp. 1231-1249). Springer New York.
Mercuri, E. and Muntoni, F., 2013. Muscular dystrophies. The Lancet, 381(9869), pp.845-860.
Mohassel, P. and Bönnemann, C.G., 2014. Limb-girdle Muscular Dystrophies.
In Neuromuscular Disorders of Infancy, Childhood, and Adolescence (Second Edition) (pp. 635-
666).
Nigro, V. and Savarese, M., 2014. Genetic basis of limb-girdle muscular dystrophies: the 2014
update. Acta Myologica, 33(1), p.1.
Nilsson, M.I., Laureano, M.L., Saeed, M. and Tarnopolsky, M.A., 2013. Dysferlin aggregation in
limb‐girdle muscular dystrophy type 2B/myoshi myopathy necessitates mutational screen for
diagnosis. Muscle & nerve, 47(5), pp.740-747.
Takahashi, T., Aoki, M., Suzuki, N., Tateyama, M., Yaginuma, C., Sato, H., Hayasaka, M.,
Sugawara, H., Ito, M., Abe-Kondo, E. and Shimakura, N., 2012. Clinical features and a mutation
with late onset of limb girdle muscular dystrophy 2B. J Neurol Neurosurg Psychiatry, pp.jnnp-
2011.
Walter, M.C. and Fischer, D., 2013. Limb Girdle Muscular Dystrophies. In Neuromuscular
Imaging (pp. 227-245). Springer New York.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

