Lifestyle Approaches to Parkinson's Disease: A Literature Review
VerifiedAdded on 2022/10/10
|12
|3364
|303
Report
AI Summary
This report provides a comprehensive literature review on lifestyle approaches to Parkinson's disease, addressing the research question of the effectiveness of these methods for the treatment of the disease. The report begins with an introduction to Parkinson's disease, its prevalence, and the current treatment options, including pharmacological and surgical interventions. The author then explores the limitations of these conventional treatments, highlighting the need for alternative and complementary approaches. The core of the report focuses on various lifestyle modalities, including nutrition, exercise, mind-body practices, and natural products. It examines the evidence for the efficacy of these approaches, drawing on research from databases such as PubMed, Medline, PsycInfo, and Google Scholar. The report discusses the benefits of natural products, such as fruits, vegetables, and herbs, and the role of antioxidants and specific foods in managing the disease. It also reviews the effectiveness of mind-body interventions, such as tai chi, qigong, and meditation-based exercise programs. The report concludes by emphasizing the potential of lifestyle medicine as a complementary therapy, while acknowledging the need for further research to determine the mechanisms of action and disease-modifying effects of these approaches. The report emphasizes the importance of ongoing research to improve patient outcomes and quality of life.

Running head: LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
Lifestyle Approaches To Parkinson’s disease
Name of the Student
Name of the University
Author Note
Lifestyle Approaches To Parkinson’s disease
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
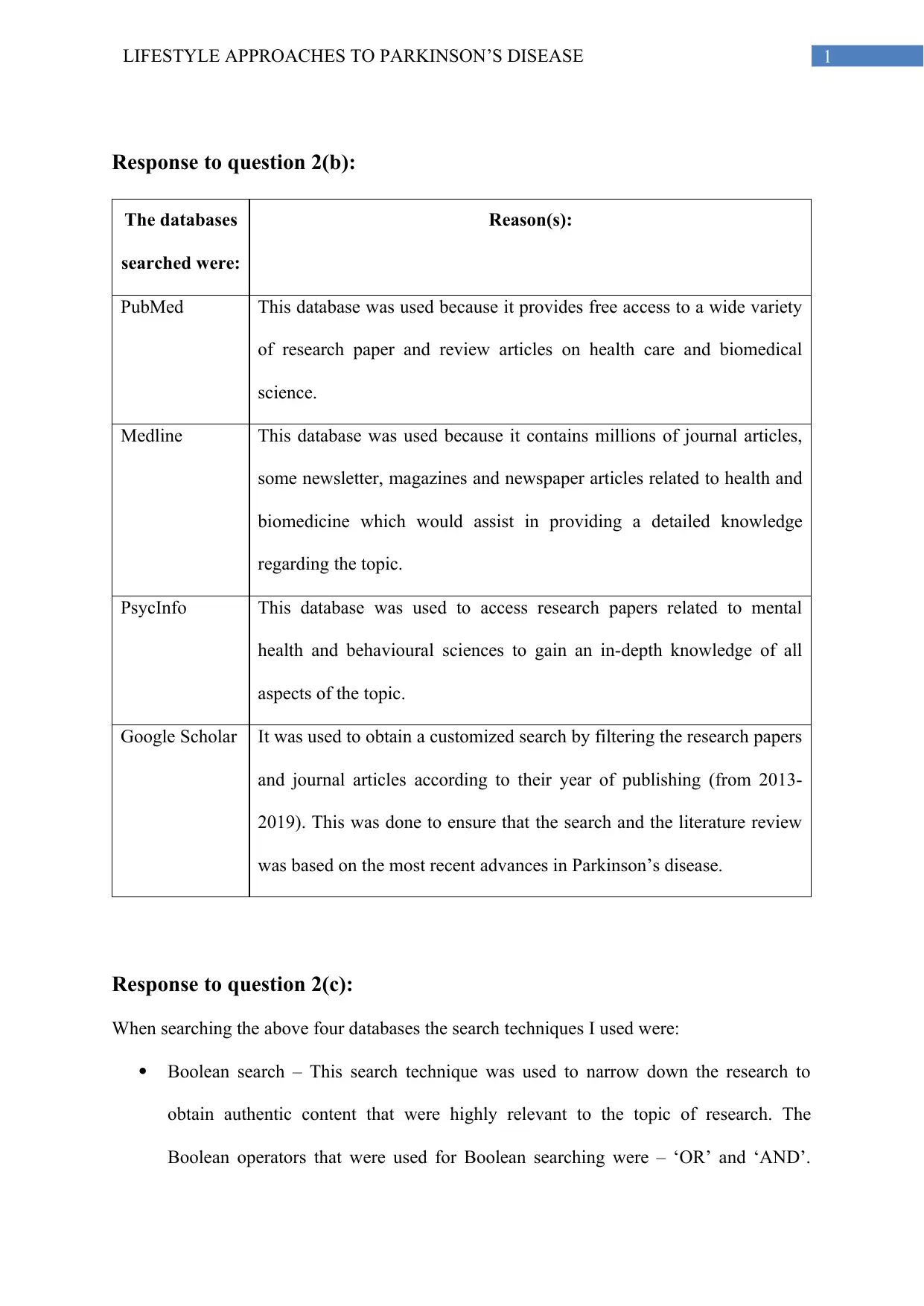
Response to question 2(b):
The databases
searched were:
Reason(s):
PubMed This database was used because it provides free access to a wide variety
of research paper and review articles on health care and biomedical
science.
Medline This database was used because it contains millions of journal articles,
some newsletter, magazines and newspaper articles related to health and
biomedicine which would assist in providing a detailed knowledge
regarding the topic.
PsycInfo This database was used to access research papers related to mental
health and behavioural sciences to gain an in-depth knowledge of all
aspects of the topic.
Google Scholar It was used to obtain a customized search by filtering the research papers
and journal articles according to their year of publishing (from 2013-
2019). This was done to ensure that the search and the literature review
was based on the most recent advances in Parkinson’s disease.
Response to question 2(c):
When searching the above four databases the search techniques I used were:
Boolean search – This search technique was used to narrow down the research to
obtain authentic content that were highly relevant to the topic of research. The
Boolean operators that were used for Boolean searching were – ‘OR’ and ‘AND’.
Response to question 2(b):
The databases
searched were:
Reason(s):
PubMed This database was used because it provides free access to a wide variety
of research paper and review articles on health care and biomedical
science.
Medline This database was used because it contains millions of journal articles,
some newsletter, magazines and newspaper articles related to health and
biomedicine which would assist in providing a detailed knowledge
regarding the topic.
PsycInfo This database was used to access research papers related to mental
health and behavioural sciences to gain an in-depth knowledge of all
aspects of the topic.
Google Scholar It was used to obtain a customized search by filtering the research papers
and journal articles according to their year of publishing (from 2013-
2019). This was done to ensure that the search and the literature review
was based on the most recent advances in Parkinson’s disease.
Response to question 2(c):
When searching the above four databases the search techniques I used were:
Boolean search – This search technique was used to narrow down the research to
obtain authentic content that were highly relevant to the topic of research. The
Boolean operators that were used for Boolean searching were – ‘OR’ and ‘AND’.
2LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
Search was conducted using these operators as follows – levodopa and Parkinson’s
disease, lifestyle approaches and Parkinson’s disease, levodopa or dopaminergic
medications, complementary or alternative approaches to Parkinson’s disease.
Search limiters – This search technique was used to filter the research to the latest
articles in order to obtain matter based on the recent and current findings in the field
of Parkinson’s disease. This search was conducted by limiting the year of publishing
in Google scholars from 2013 to 2019.
Response to question 3 (Literature review):
Parkinson’s disease and its prevalence
Parkinson’s disease (PD) may be described as a progressive neurodegenerative
disease which results in impairment of both motor and non-motor functions in the body (Lee
et al., 2018). Rizek, Kumar & Jog (2016) have explained that Parkinson’s disease primarily
occurs due to disorder of the extrapyramidal motor system, which leads to decreased motor
function because of loss of function of the dopaminergic neurons in the substantia nigra
region. Furthermore, it is often accompanied by formation of Lewy bodies and accumulation
of Lewy neuritis (intraneuronal aggregates of α-synuclein) due to mutation in the synuclein
alpha gene (PARK 1). They have also described that the exhibition of non-motor symptoms
is because of the degeneration of serotonergic, cholinergic, adrenergic, peptidergic and
histaminergic neurons. Hence, this disorder is characterized by a complex array of symptoms
that include motor symptoms (such as tremors, bradykinesia/akinesia, rigidity and postural
instability) and non-motor symptoms (such as autonomic disabilities, cognitive impairment,
sensory abnormalities and psychiatric disorders (Tibar et al., 2018).
Search was conducted using these operators as follows – levodopa and Parkinson’s
disease, lifestyle approaches and Parkinson’s disease, levodopa or dopaminergic
medications, complementary or alternative approaches to Parkinson’s disease.
Search limiters – This search technique was used to filter the research to the latest
articles in order to obtain matter based on the recent and current findings in the field
of Parkinson’s disease. This search was conducted by limiting the year of publishing
in Google scholars from 2013 to 2019.
Response to question 3 (Literature review):
Parkinson’s disease and its prevalence
Parkinson’s disease (PD) may be described as a progressive neurodegenerative
disease which results in impairment of both motor and non-motor functions in the body (Lee
et al., 2018). Rizek, Kumar & Jog (2016) have explained that Parkinson’s disease primarily
occurs due to disorder of the extrapyramidal motor system, which leads to decreased motor
function because of loss of function of the dopaminergic neurons in the substantia nigra
region. Furthermore, it is often accompanied by formation of Lewy bodies and accumulation
of Lewy neuritis (intraneuronal aggregates of α-synuclein) due to mutation in the synuclein
alpha gene (PARK 1). They have also described that the exhibition of non-motor symptoms
is because of the degeneration of serotonergic, cholinergic, adrenergic, peptidergic and
histaminergic neurons. Hence, this disorder is characterized by a complex array of symptoms
that include motor symptoms (such as tremors, bradykinesia/akinesia, rigidity and postural
instability) and non-motor symptoms (such as autonomic disabilities, cognitive impairment,
sensory abnormalities and psychiatric disorders (Tibar et al., 2018).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
According to Reeve, Simcox & Turnbull (2014), it is the 2nd most prevailing
neurodegenerative disease in the world, which impacts 1% of all individuals over 60 years in
developed countries. This disease generally occurs in the elderly however, a small proportion
of the population may present with the symptoms of this disease at around 40 years of age
(DeMaagd & Philip, 2015). According to (Nag & Jelinek, 2019), a few pharmacological,
surgical and complementary/supportive therapies may diminish the effects of the disease and
treat it symptomatically. However, the researchers have stated that there is no effective cure
for this disease at present. Hence, there exists a need for extensive research to find a cure that
can prevent the occurrence of this disease or permanently cure it.
Treatment of Parkinson’s disease
Two main approaches that have been used for the treatment of this disease include
drug therapy and surgery (Gazewood & Clebak, 2013). According to Rizek, Kumar & Jog
(2016), dopaminergenic medications are primarily used to provide symptomatic relief for
motor symptoms in Parkinson’s patients. They have explained that this is because many
motor symptoms are because of the lack/deficiency of the endogenous neurotransmitter,
dopamine and hence, the motor function control may be improved by providing drugs that
can temporarily increase dopamine levels in the brain. According to Salat & Tolosa (2013),
levodopa is a drug that is generally used for treating Parkinson’s patients. They have
explained that after intravenous administration of this drug, it crosses the blood-brain barrier
and improves the motor function by getting converted to dopamine. However, they have
stated that levodopa has a short life span and frequent administration leads to cardiac
stimulation (arrhythmia and tachycardia), nausea and vomiting. Moreover, with progression
of the disease, the central nervous system’s capacity to store levodopa and dopamine
declines, which leads to motor fluctuations. Hence, the patients undergoing sustained
treatments of levodopa inevitably experience the on-off phenomenon (On: normal
According to Reeve, Simcox & Turnbull (2014), it is the 2nd most prevailing
neurodegenerative disease in the world, which impacts 1% of all individuals over 60 years in
developed countries. This disease generally occurs in the elderly however, a small proportion
of the population may present with the symptoms of this disease at around 40 years of age
(DeMaagd & Philip, 2015). According to (Nag & Jelinek, 2019), a few pharmacological,
surgical and complementary/supportive therapies may diminish the effects of the disease and
treat it symptomatically. However, the researchers have stated that there is no effective cure
for this disease at present. Hence, there exists a need for extensive research to find a cure that
can prevent the occurrence of this disease or permanently cure it.
Treatment of Parkinson’s disease
Two main approaches that have been used for the treatment of this disease include
drug therapy and surgery (Gazewood & Clebak, 2013). According to Rizek, Kumar & Jog
(2016), dopaminergenic medications are primarily used to provide symptomatic relief for
motor symptoms in Parkinson’s patients. They have explained that this is because many
motor symptoms are because of the lack/deficiency of the endogenous neurotransmitter,
dopamine and hence, the motor function control may be improved by providing drugs that
can temporarily increase dopamine levels in the brain. According to Salat & Tolosa (2013),
levodopa is a drug that is generally used for treating Parkinson’s patients. They have
explained that after intravenous administration of this drug, it crosses the blood-brain barrier
and improves the motor function by getting converted to dopamine. However, they have
stated that levodopa has a short life span and frequent administration leads to cardiac
stimulation (arrhythmia and tachycardia), nausea and vomiting. Moreover, with progression
of the disease, the central nervous system’s capacity to store levodopa and dopamine
declines, which leads to motor fluctuations. Hence, the patients undergoing sustained
treatments of levodopa inevitably experience the on-off phenomenon (On: normal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
movements when the levels are sufficient; Off: akinesia when the levels are low or
insufficient). In order to overcome this limitation, levodopa is now used in a combination
with other substances to increase its effectiveness by preventing its early conversion before it
reaches the brain or by decreasing its side effects. These include COMT-inhibitors (such as
tolcapone or entacapone), peripheral inhibitors (such as carbidopa and benserazide) and
MAO-B inhibitors (such as rasagiline or selegiline) (Stoker, Torsneym & Barker, 2018).
However, in-vitro studies have observed the toxicity of levodopa on dopaminergic neurons
and in-vivo studies have postulated that its use could lead to oxidative stress, which may
further aggravate the disease by causing damage to remaining dopaminergic neurons (Muller,
2013). Gazewood, Richards & Clebak (2013) have stated that dopamine agonists (ergoline
and non-ergoline agonists) may be used alone or in combination with the drug, levodopa, in
such patients. They have explained that these drugs act directly on the dopamine receptors
(D2-type) and mimic dopamine. Hence, they may significantly reduce complications and
improve the motor functions when used in combination with levodopa. It may also be given
as a first-line treatment to de novo patients to delay the levodopa treatment and hence,
postpone the onset of various complications. However, Borovac (2016) have argued that
ergoline agonists may act on other receptors (5-HT, D1-type or adrenergic receptors) and
increase the risk factor for developing pulmonary, peritoneal or cardiac fibrosis. He has also
stated that the use of non-ergoline agonists may lead to hypotension, somnolence, nausea and
worsening of dyskinesia. Furthermore, Pedrosa & Timmermann (2013) have stated that
although the use of dopaminergic medications may treat motor symptoms and prevent
aggravation of Parkinson’s disease, it may be ineffective in treating certain motor and all the
non-motor symptoms. Oertel (2017) have further supported this perspective by stating that
though certain drugs exist for treating specific non-motor symptoms (such as 5HT2A inverse
agonist for treating psychosis, L-threo-DOPS for treating autonomic symptoms such as
movements when the levels are sufficient; Off: akinesia when the levels are low or
insufficient). In order to overcome this limitation, levodopa is now used in a combination
with other substances to increase its effectiveness by preventing its early conversion before it
reaches the brain or by decreasing its side effects. These include COMT-inhibitors (such as
tolcapone or entacapone), peripheral inhibitors (such as carbidopa and benserazide) and
MAO-B inhibitors (such as rasagiline or selegiline) (Stoker, Torsneym & Barker, 2018).
However, in-vitro studies have observed the toxicity of levodopa on dopaminergic neurons
and in-vivo studies have postulated that its use could lead to oxidative stress, which may
further aggravate the disease by causing damage to remaining dopaminergic neurons (Muller,
2013). Gazewood, Richards & Clebak (2013) have stated that dopamine agonists (ergoline
and non-ergoline agonists) may be used alone or in combination with the drug, levodopa, in
such patients. They have explained that these drugs act directly on the dopamine receptors
(D2-type) and mimic dopamine. Hence, they may significantly reduce complications and
improve the motor functions when used in combination with levodopa. It may also be given
as a first-line treatment to de novo patients to delay the levodopa treatment and hence,
postpone the onset of various complications. However, Borovac (2016) have argued that
ergoline agonists may act on other receptors (5-HT, D1-type or adrenergic receptors) and
increase the risk factor for developing pulmonary, peritoneal or cardiac fibrosis. He has also
stated that the use of non-ergoline agonists may lead to hypotension, somnolence, nausea and
worsening of dyskinesia. Furthermore, Pedrosa & Timmermann (2013) have stated that
although the use of dopaminergic medications may treat motor symptoms and prevent
aggravation of Parkinson’s disease, it may be ineffective in treating certain motor and all the
non-motor symptoms. Oertel (2017) have further supported this perspective by stating that
though certain drugs exist for treating specific non-motor symptoms (such as 5HT2A inverse
agonist for treating psychosis, L-threo-DOPS for treating autonomic symptoms such as
5LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
neurogenic orthostatic hypotension), very few clinical trials exist for the treatment of non-
symptomatic symptoms. According to Lee et al. (2018), certain surgical procedures such as
ablative surgery (thalamotomy and pallidotomy) and deep brain stimulation may be used to
treat this disease by reducing the excess inhibitory output from the pars reticulata of the
substantia nigra and internal paleostriatum. However, as these procedures are invasive, they
are generally reserved for severely afflicted patients who do not benefit from the medications.
At present, the existing therapies provide symptomatic relief by delaying the progression of
the disease rather than permanently curing it.
Lifestyle modalities for treating Parkinson’s disease
According to Oertel (2017), the course of research has changed as attempts are being
made to develop therapies (such as gene therapy or regenerative cell-based therapy) that can
exhibit a disease modifying effect rather than just postponing the advancement of Parkinson’s
disease. However, these studies are in the preliminary stages and require extensive research
before being introduced in the market (Stoker, Torsneym & Barker, 2018). Rabin et al.
(2014) have discussed the significance of complementary and alternative lifestyle approaches
for reducing the prevalence of this disease and improving the health outcome of patients
suffering from this disease. They have explained that the alternative medicine interventions
may be classified into two groups that include natural product (herbals, vitamins, minerals
and other nutrients) and mind-body practices (hydrotherapy, exercise, physiotherapy, yoga,
expression therapy and massage). Various researches have been conducted to investigate the
effectiveness of these approaches for treating Parkinson’s patients.
According to Essa et al. (2014), natural products (such as fruits, vegetables, herbs and
spices) are beneficial in the treatment of this disease because of their ability to prevent
oxidative stress, reduce neuroinflammation and modify cellular signaling pathways. This is
neurogenic orthostatic hypotension), very few clinical trials exist for the treatment of non-
symptomatic symptoms. According to Lee et al. (2018), certain surgical procedures such as
ablative surgery (thalamotomy and pallidotomy) and deep brain stimulation may be used to
treat this disease by reducing the excess inhibitory output from the pars reticulata of the
substantia nigra and internal paleostriatum. However, as these procedures are invasive, they
are generally reserved for severely afflicted patients who do not benefit from the medications.
At present, the existing therapies provide symptomatic relief by delaying the progression of
the disease rather than permanently curing it.
Lifestyle modalities for treating Parkinson’s disease
According to Oertel (2017), the course of research has changed as attempts are being
made to develop therapies (such as gene therapy or regenerative cell-based therapy) that can
exhibit a disease modifying effect rather than just postponing the advancement of Parkinson’s
disease. However, these studies are in the preliminary stages and require extensive research
before being introduced in the market (Stoker, Torsneym & Barker, 2018). Rabin et al.
(2014) have discussed the significance of complementary and alternative lifestyle approaches
for reducing the prevalence of this disease and improving the health outcome of patients
suffering from this disease. They have explained that the alternative medicine interventions
may be classified into two groups that include natural product (herbals, vitamins, minerals
and other nutrients) and mind-body practices (hydrotherapy, exercise, physiotherapy, yoga,
expression therapy and massage). Various researches have been conducted to investigate the
effectiveness of these approaches for treating Parkinson’s patients.
According to Essa et al. (2014), natural products (such as fruits, vegetables, herbs and
spices) are beneficial in the treatment of this disease because of their ability to prevent
oxidative stress, reduce neuroinflammation and modify cellular signaling pathways. This is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
because they possess various phytonutrients such as stilbenoids, zingerone, lycopene,
catechols, flavonoids, isoflavonoids, anthocyanins, S-Allylcysteine and eugenol. Recently,
extensive research has been done to determine the efficacy of antioxidants in treating
Parkinson’s disease. However, Filograna et al. (2016) have stated that though antioxidants
such as Vitamin E, coenzyme Q10, mitoquinone and creatine have shown positive effects on
mice, these antioxidants are found to be ineffective in treating Parkinson’s disease in humans.
Seidl et al. (2014), have further explained the significance of nutrition in Parkinson’s disease.
They have stated that certain foods (such as milk) increase the risk of neurodegeneration
whereas other foods (such as omega-3 fatty acids, fruits, vegetables, red wine and tea) may
exhibit neuroprotection. The latter may be due to the ability of the nutrients to maintain
oxidative balance and prevent mitochondrial dysfunction, thereby, improving the health
conditions of Parkinson’s patients.
According to Bega & Zadikoff (2014), mind-body interventions may be used to as a
holistic approach for treating this disease. They have stated the effectiveness of tai chi and
qigong, music, dance, expressive therapy, relaxation therapy, massage and Alexander therapy
and the ineffectiveness of yoga for treating Parkinson’s patients. However, Van et al. (2018)
offer a different perspective by stating the effectiveness of yoga in improving gait and
postural stability in Parkinson’s patients. The contradictory statements may be due to the
availability of limited literature, which emphasizes the need for extensive research.
Furthermore, de Carvalho et al. (2018) have stated the effectiveness of physical activity in
treating motor symptoms, improving postural stability and mental health by restoring
previously affected neuronal pathways. According to Son & Choi (2018), meditation-based
exercise program is highly functional in improving the non-motor and motor symptoms in the
Parkinson’s patients. Carroll et al. (2017) had observed the effectiveness of aquatic exercise
therapy in Parkinson’s patients. They had concluded that by utilizing the physical properties
because they possess various phytonutrients such as stilbenoids, zingerone, lycopene,
catechols, flavonoids, isoflavonoids, anthocyanins, S-Allylcysteine and eugenol. Recently,
extensive research has been done to determine the efficacy of antioxidants in treating
Parkinson’s disease. However, Filograna et al. (2016) have stated that though antioxidants
such as Vitamin E, coenzyme Q10, mitoquinone and creatine have shown positive effects on
mice, these antioxidants are found to be ineffective in treating Parkinson’s disease in humans.
Seidl et al. (2014), have further explained the significance of nutrition in Parkinson’s disease.
They have stated that certain foods (such as milk) increase the risk of neurodegeneration
whereas other foods (such as omega-3 fatty acids, fruits, vegetables, red wine and tea) may
exhibit neuroprotection. The latter may be due to the ability of the nutrients to maintain
oxidative balance and prevent mitochondrial dysfunction, thereby, improving the health
conditions of Parkinson’s patients.
According to Bega & Zadikoff (2014), mind-body interventions may be used to as a
holistic approach for treating this disease. They have stated the effectiveness of tai chi and
qigong, music, dance, expressive therapy, relaxation therapy, massage and Alexander therapy
and the ineffectiveness of yoga for treating Parkinson’s patients. However, Van et al. (2018)
offer a different perspective by stating the effectiveness of yoga in improving gait and
postural stability in Parkinson’s patients. The contradictory statements may be due to the
availability of limited literature, which emphasizes the need for extensive research.
Furthermore, de Carvalho et al. (2018) have stated the effectiveness of physical activity in
treating motor symptoms, improving postural stability and mental health by restoring
previously affected neuronal pathways. According to Son & Choi (2018), meditation-based
exercise program is highly functional in improving the non-motor and motor symptoms in the
Parkinson’s patients. Carroll et al. (2017) had observed the effectiveness of aquatic exercise
therapy in Parkinson’s patients. They had concluded that by utilizing the physical properties
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
of water, this therapy can effectively reduce disability Parkinson’s patients. Moreover, Volpe
et al. (2014) have stated that hydrotherapy is more effective in treating balance dysfunction in
individuals suffering from this disease as compared to land-based therapy. Hence,
complementary and alternative lifestyle medicines may be beneficial in improving the health
outcome and the quality of living in Parkinson’s patients.
Currently, the lifestyle medicine approaches are being used as
complementary/supportive therapies along with drug therapy in order to improve
performance and provide symptomatic relief to Parkinson’s patients. The success of most of
the lifestyle modalities has been attributed to the effectiveness of the scientific evidence-
based trials. However, the existing randomized trials are based on small sample size.
Moreover, limited literature is available on the mechanism of action of these approaches.
Hence, extensive research is required to determine the mechanism of action and the disease
modifying effects of the lifestyle approaches in reducing the prevalence of the disease and
improving the health outcomes in Parkinson’s patients (Nag & Jelinek, 2019).
of water, this therapy can effectively reduce disability Parkinson’s patients. Moreover, Volpe
et al. (2014) have stated that hydrotherapy is more effective in treating balance dysfunction in
individuals suffering from this disease as compared to land-based therapy. Hence,
complementary and alternative lifestyle medicines may be beneficial in improving the health
outcome and the quality of living in Parkinson’s patients.
Currently, the lifestyle medicine approaches are being used as
complementary/supportive therapies along with drug therapy in order to improve
performance and provide symptomatic relief to Parkinson’s patients. The success of most of
the lifestyle modalities has been attributed to the effectiveness of the scientific evidence-
based trials. However, the existing randomized trials are based on small sample size.
Moreover, limited literature is available on the mechanism of action of these approaches.
Hence, extensive research is required to determine the mechanism of action and the disease
modifying effects of the lifestyle approaches in reducing the prevalence of the disease and
improving the health outcomes in Parkinson’s patients (Nag & Jelinek, 2019).
8LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
References
Bega, D., & Zadikoff, C. (2014). Complementary & alternative management of Parkinson’s
disease: an evidence-based review of eastern influenced practices. Journal of
movement disorders, 7(2), 57.
Borovac, J. A. (2016). Focus: The Aging Brain: Side effects of a dopamine agonist therapy
for Parkinson’s disease: a mini-review of clinical pharmacology. The Yale journal of
biology and medicine, 89(1), 37.
Carroll, L. M., Volpe, D., Morris, M. E., Saunders, J., & Clifford, A. M. (2017). Aquatic
exercise therapy for people with Parkinson disease: a randomized controlled
trial. Archives of physical medicine and rehabilitation, 98(4), 631-638.
de Carvalho, A. O., Sá Filho, A. S., Murillo-Rodriguez, E., Rocha, N. B., Carta, M. G., &
Machado, S. (2018). Physical exercise for parkinson’s disease: clinical and
experimental evidence. Clinical practice and epidemiology in mental health: CP &
EMH, 14, 89.
DeMaagd, G., & Philip, A. (2015). Parkinson’s disease and its management: part 1: disease
entity, risk factors, pathophysiology, clinical presentation, and diagnosis. Pharmacy
and therapeutics, 40(8), 504.
Essa, M. M., Braidy, N., Bridge, W., Subash, S., Manivasagam, T., Vijayan, R. K., Al-
Adawi, S. & Guillemin, G. J. (2014). Review of natural products on Parkinson’s
disease pathology. J Aging Res Clin Pract, 3(1), 1-8.
References
Bega, D., & Zadikoff, C. (2014). Complementary & alternative management of Parkinson’s
disease: an evidence-based review of eastern influenced practices. Journal of
movement disorders, 7(2), 57.
Borovac, J. A. (2016). Focus: The Aging Brain: Side effects of a dopamine agonist therapy
for Parkinson’s disease: a mini-review of clinical pharmacology. The Yale journal of
biology and medicine, 89(1), 37.
Carroll, L. M., Volpe, D., Morris, M. E., Saunders, J., & Clifford, A. M. (2017). Aquatic
exercise therapy for people with Parkinson disease: a randomized controlled
trial. Archives of physical medicine and rehabilitation, 98(4), 631-638.
de Carvalho, A. O., Sá Filho, A. S., Murillo-Rodriguez, E., Rocha, N. B., Carta, M. G., &
Machado, S. (2018). Physical exercise for parkinson’s disease: clinical and
experimental evidence. Clinical practice and epidemiology in mental health: CP &
EMH, 14, 89.
DeMaagd, G., & Philip, A. (2015). Parkinson’s disease and its management: part 1: disease
entity, risk factors, pathophysiology, clinical presentation, and diagnosis. Pharmacy
and therapeutics, 40(8), 504.
Essa, M. M., Braidy, N., Bridge, W., Subash, S., Manivasagam, T., Vijayan, R. K., Al-
Adawi, S. & Guillemin, G. J. (2014). Review of natural products on Parkinson’s
disease pathology. J Aging Res Clin Pract, 3(1), 1-8.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
Filograna, R., Beltramini, M., Bubacco, L., & Bisaglia, M. (2016). Anti-oxidants in
Parkinson’s disease therapy: a critical point of view. Current
neuropharmacology, 14(3), 260-271.
Lee, D. J., Dallapiazza, R. F., De Vloo, P., & Lozano, A. M. (2018). Current surgical
treatments for Parkinson's disease and potential therapeutic targets. Neural
regeneration research, 13(8), 1342.
Nag, N., & Jelinek, G. A. (2019). More research is needed on lifestyle behaviours that
influence progression of Parkinson’s Disease. Frontiers in neurology, 10, 452.
Oertel, W. H. (2017). Recent advances in treating Parkinson’s disease. F1000Research, 6.
Rabin, M. L., Stevens Haas, C., Havrilla, E., Rosenstein, A., Toffey, B., Devi, T., Earnhardt,‐
M.C. & Kurlan, R. (2015). Complementary Therapies for Parkinson's Disease: What's
Promoted, Rationale, Potential Risks and Benefits. Movement disorders clinical
practice, 2(3), 205-212.
Reeve, A., Simcox, E., & Turnbull, D. (2014). Ageing and Parkinson's disease: why is
advancing age the biggest risk factor?. Ageing research reviews, 14, 19-30.
Rizek, P., Kumar, N., & Jog, M. S. (2016). An update on the diagnosis and treatment of
Parkinson disease. Cmaj, 188(16), 1157-1165.
Seidl, S. E., Santiago, J. A., Bilyk, H., & Potashkin, J. A. (2014). The emerging role of
nutrition in Parkinson's disease. Frontiers in aging neuroscience, 6, 36.
Son, H. G., & Choi, E. O. (2018). The Effects of Mindfulness Meditation-Based Complex
Exercise Program on Motor and Nonmotor Symptoms and Quality of Life in Patients
with Parkinson's Disease. Asian nursing research, 12(2), 145-153.
Filograna, R., Beltramini, M., Bubacco, L., & Bisaglia, M. (2016). Anti-oxidants in
Parkinson’s disease therapy: a critical point of view. Current
neuropharmacology, 14(3), 260-271.
Lee, D. J., Dallapiazza, R. F., De Vloo, P., & Lozano, A. M. (2018). Current surgical
treatments for Parkinson's disease and potential therapeutic targets. Neural
regeneration research, 13(8), 1342.
Nag, N., & Jelinek, G. A. (2019). More research is needed on lifestyle behaviours that
influence progression of Parkinson’s Disease. Frontiers in neurology, 10, 452.
Oertel, W. H. (2017). Recent advances in treating Parkinson’s disease. F1000Research, 6.
Rabin, M. L., Stevens Haas, C., Havrilla, E., Rosenstein, A., Toffey, B., Devi, T., Earnhardt,‐
M.C. & Kurlan, R. (2015). Complementary Therapies for Parkinson's Disease: What's
Promoted, Rationale, Potential Risks and Benefits. Movement disorders clinical
practice, 2(3), 205-212.
Reeve, A., Simcox, E., & Turnbull, D. (2014). Ageing and Parkinson's disease: why is
advancing age the biggest risk factor?. Ageing research reviews, 14, 19-30.
Rizek, P., Kumar, N., & Jog, M. S. (2016). An update on the diagnosis and treatment of
Parkinson disease. Cmaj, 188(16), 1157-1165.
Seidl, S. E., Santiago, J. A., Bilyk, H., & Potashkin, J. A. (2014). The emerging role of
nutrition in Parkinson's disease. Frontiers in aging neuroscience, 6, 36.
Son, H. G., & Choi, E. O. (2018). The Effects of Mindfulness Meditation-Based Complex
Exercise Program on Motor and Nonmotor Symptoms and Quality of Life in Patients
with Parkinson's Disease. Asian nursing research, 12(2), 145-153.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
Stoker, T. B., Torsney, K. M., & Barker, R. A. (2018). Emerging treatment approaches for
Parkinson's disease. Frontiers in Neuroscience, 12, 693.
Tibar, H., El Bayad, K., Bouhouche, A., Haddou, A. B., Hachmia, E., Benomar, A.,
Benazzouz, A. & Regragui, W. (2018). Non-Motor symptoms of Parkinson’s Disease
and Their impact on Quality of life in a cohort of Moroccan Patients. Frontiers in
neurology, 9, 170.
Van Puymbroeck, M., Walter, A., Hawkins, B. L., Sharp, J. L., Woschkolup, K., Urrea-
Mendoza, E., Revilla, F., Adams, E.V. & Schmid, A. A. (2018). Functional
improvements in Parkinson’s disease following a randomized trial of yoga. Evidence-
Based Complementary and Alternative Medicine, 2018.
Volpe, D., Giantin, M. G., Maestri, R., & Frazzitta, G. (2014). Comparing the effects of
hydrotherapy and land-based therapy on balance in patients with Parkinson’s disease:
a randomized controlled pilot study. Clinical rehabilitation, 28(12), 1210-1217.
Pedrosa, D. J., & Timmermann, L. (2013). Management of Parkinson’s
disease. Neuropsychiatric disease and treatment, 9, 321.
Gazewood, J. D., Richards, D. R., & Clebak, K. (2013). Parkinson disease: an update. Am
Fam Physician, 87(4), 267-73.
Muller, T. (2013). Detoxification and antioxidative therapy for levodopa-induced
neurodegeneration in Parkinson’s disease. Expert review of neurotherapeutics, 13(6),
707-718.
Salat, D., & Tolosa, E. (2013). Levodopa in the treatment of Parkinson's disease: current
status and new developments. Journal of Parkinson's disease, 3(3), 255-269.
Stoker, T. B., Torsney, K. M., & Barker, R. A. (2018). Emerging treatment approaches for
Parkinson's disease. Frontiers in Neuroscience, 12, 693.
Tibar, H., El Bayad, K., Bouhouche, A., Haddou, A. B., Hachmia, E., Benomar, A.,
Benazzouz, A. & Regragui, W. (2018). Non-Motor symptoms of Parkinson’s Disease
and Their impact on Quality of life in a cohort of Moroccan Patients. Frontiers in
neurology, 9, 170.
Van Puymbroeck, M., Walter, A., Hawkins, B. L., Sharp, J. L., Woschkolup, K., Urrea-
Mendoza, E., Revilla, F., Adams, E.V. & Schmid, A. A. (2018). Functional
improvements in Parkinson’s disease following a randomized trial of yoga. Evidence-
Based Complementary and Alternative Medicine, 2018.
Volpe, D., Giantin, M. G., Maestri, R., & Frazzitta, G. (2014). Comparing the effects of
hydrotherapy and land-based therapy on balance in patients with Parkinson’s disease:
a randomized controlled pilot study. Clinical rehabilitation, 28(12), 1210-1217.
Pedrosa, D. J., & Timmermann, L. (2013). Management of Parkinson’s
disease. Neuropsychiatric disease and treatment, 9, 321.
Gazewood, J. D., Richards, D. R., & Clebak, K. (2013). Parkinson disease: an update. Am
Fam Physician, 87(4), 267-73.
Muller, T. (2013). Detoxification and antioxidative therapy for levodopa-induced
neurodegeneration in Parkinson’s disease. Expert review of neurotherapeutics, 13(6),
707-718.
Salat, D., & Tolosa, E. (2013). Levodopa in the treatment of Parkinson's disease: current
status and new developments. Journal of Parkinson's disease, 3(3), 255-269.

11LIFESTYLE APPROACHES TO PARKINSON’S DISEASE
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





