University: Diagnostic Algorithm of CF Lower Respiratory Infections
VerifiedAdded on 2022/09/29
|8
|1681
|28
Report
AI Summary
This report provides a diagnostic algorithm for the microbiological diagnosis of lower respiratory tract infections (LRTIs) in patients with cystic fibrosis (CF). It begins with an introduction highlighting the challenges in diagnosing these infections due to the complexity of the disease and the diversity of pathogens involved. The report then details various diagnostic methods, including Gram staining of sputum to identify common pathogens like Streptococcus pneumoniae and Staphylococcus aureus, and quantitative culture techniques using broncho-alveolar lavage (BAL) and other specimens. The report also discusses the detection of acute exacerbations of chronic bronchitis and the evaluation of pulmonary tuberculosis, emphasizing the role of both direct and indirect microbial diagnosis. Furthermore, it covers the significance of detecting opportunistic pathogens and the use of molecular methods like PCR for accurate diagnosis. The report concludes with a summary of the diagnostic algorithm, incorporating symptoms, direct and indirect microbial diagnosis, and quantitative culture results to guide effective management of CF-related LRTIs.

Running Head: DIAGNOSTIC ALGORITHM OF LOWER RESPIRATORY TRACT
INFECTION WITH CYSTIC FIBROSIS
Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
Name of the Student:
Name of the University:
Author Note:
INFECTION WITH CYSTIC FIBROSIS
Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
Introduction
Literature studies reveal that 5% to 10 % deaths occur worldwide due to the lower
respiratory tract infection. A vital role is played by the clinical laboratory in diagnosis of the
disease but it combats a lot of challenges as well because of the complexity of the disease
(Campbell and Forbes, 2011). The complexities include diversity and quality of the
specimen, contamination with oropharyngeal flora, and diversity of the pathogen population
which may include viruses, bacteria and fungi and the complexity of the pathophysiology of
the respiratory tract infections.
The collection of the specimen is done usually by collecting the nasopharyngeal swab and
aspirates, oropharyngeal swab, nasal swab, throat swab and BAL fluid.
Gram staining of expectorated sputum
Gram staining of the expectorated sputum is a standard preliminary procedure executed in
clinical microbiology. It is exploited to assess the quality of the specimen for the initial, rapid
diagnostic information and for the quality assurance of the laboratory. Samples detected by
Gram stain may contain predominant amount of upper respiratory tract material are rejected
for the routine bacterial culture. Gram stain of the expectorated sputum checks for the
presence of Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus sp, and
Pseudomonas sp. Gram stain is a valuable tool for reporting several clinically useful
information.
Quantitative culture techniques
Quantitative culture techniques on broncho-alveolar lavage (BAL) and mini-BAL
specimens, endotracheal (ET) aspirates and trans-bronchial biopsy specimens. This is
obtained during bronchoscopic procedures. In general the colony count of <104/ml indicates
Introduction
Literature studies reveal that 5% to 10 % deaths occur worldwide due to the lower
respiratory tract infection. A vital role is played by the clinical laboratory in diagnosis of the
disease but it combats a lot of challenges as well because of the complexity of the disease
(Campbell and Forbes, 2011). The complexities include diversity and quality of the
specimen, contamination with oropharyngeal flora, and diversity of the pathogen population
which may include viruses, bacteria and fungi and the complexity of the pathophysiology of
the respiratory tract infections.
The collection of the specimen is done usually by collecting the nasopharyngeal swab and
aspirates, oropharyngeal swab, nasal swab, throat swab and BAL fluid.
Gram staining of expectorated sputum
Gram staining of the expectorated sputum is a standard preliminary procedure executed in
clinical microbiology. It is exploited to assess the quality of the specimen for the initial, rapid
diagnostic information and for the quality assurance of the laboratory. Samples detected by
Gram stain may contain predominant amount of upper respiratory tract material are rejected
for the routine bacterial culture. Gram stain of the expectorated sputum checks for the
presence of Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus sp, and
Pseudomonas sp. Gram stain is a valuable tool for reporting several clinically useful
information.
Quantitative culture techniques
Quantitative culture techniques on broncho-alveolar lavage (BAL) and mini-BAL
specimens, endotracheal (ET) aspirates and trans-bronchial biopsy specimens. This is
obtained during bronchoscopic procedures. In general the colony count of <104/ml indicates
2Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
the presence of infection. A count of 104 to 105 CFU /ml represents the grey zone result and
counts >105 CFU /ml indicates the presence of a potential pathogen. The bronchial brushings
are present in approximately 1ml of saline and this step is followed by quantitative culture
that is executed by plating 10 ul of the specimen. If the count is >103 CFU/ml it is suspected
as pneumonia (Langelier et al., 2018).
Detection of acute exacerbations of chronic bronchitis
The worsening of COPD symptoms which typically includes shortness of breath, quantity
and colour of phlegm which lasts for several days. The inflammation of the airway is
increased during the exacerbation that results in elevated hyperinflation, reduced expiratory
air flow and decreased exchange of gases. It is also characterised by elevated dyspea. This
occurs mainly by the intervention of bacteria and viruses. Potential pathogen like
Haemophilus influenza, Streptococcus pneumoniae and Moraxella catarrhalis contributes to
exacerbations (Nepal et al., 2018).
Evaluation of cystic fibrosis
Patients combating COPD, Chronic Obstructive Pulmonary Disease, often face
complications with cystic fibrosis as well. It is observed that Staphylococcus aureus and
Haemophilus influenzae typically infest early in the life and is considered to be the most
common bacterial pathogen that is recovered from the respiratory tract of people combating
cystic fibrosis (De Boeck et al., 2006). The prevalence of the infection that is caused by
Pseudomonas aeruginosa may vary based on the age, it affects 80% of the individual aged
between 25 to 34 years of age. Other opportunistic bacterial pathogens may also be present
apart from these common ones. Certain fungi like Aspergillus sp, Scedosporium sp, and
Exophiala dermatids have been observed to have colonised in the airways.
the presence of infection. A count of 104 to 105 CFU /ml represents the grey zone result and
counts >105 CFU /ml indicates the presence of a potential pathogen. The bronchial brushings
are present in approximately 1ml of saline and this step is followed by quantitative culture
that is executed by plating 10 ul of the specimen. If the count is >103 CFU/ml it is suspected
as pneumonia (Langelier et al., 2018).
Detection of acute exacerbations of chronic bronchitis
The worsening of COPD symptoms which typically includes shortness of breath, quantity
and colour of phlegm which lasts for several days. The inflammation of the airway is
increased during the exacerbation that results in elevated hyperinflation, reduced expiratory
air flow and decreased exchange of gases. It is also characterised by elevated dyspea. This
occurs mainly by the intervention of bacteria and viruses. Potential pathogen like
Haemophilus influenza, Streptococcus pneumoniae and Moraxella catarrhalis contributes to
exacerbations (Nepal et al., 2018).
Evaluation of cystic fibrosis
Patients combating COPD, Chronic Obstructive Pulmonary Disease, often face
complications with cystic fibrosis as well. It is observed that Staphylococcus aureus and
Haemophilus influenzae typically infest early in the life and is considered to be the most
common bacterial pathogen that is recovered from the respiratory tract of people combating
cystic fibrosis (De Boeck et al., 2006). The prevalence of the infection that is caused by
Pseudomonas aeruginosa may vary based on the age, it affects 80% of the individual aged
between 25 to 34 years of age. Other opportunistic bacterial pathogens may also be present
apart from these common ones. Certain fungi like Aspergillus sp, Scedosporium sp, and
Exophiala dermatids have been observed to have colonised in the airways.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
The microbiology laboratory plays a crucial role in management of the cystic fibrosis
patients. The complex bacterial flora requires the usage of selective media and complex
protocols for the isolation of the pathogens. It is almost rare to eradicate the colonizing
pathogens like Pseudomonas sp and Staphylococcus aureus. Inhaled therapies are exploited
for chronic suppression and for treatment of the exacerbations. The antibiotic
pharmacokinetics are altered in the patients with cystic fibrosis. Unusual or altered strains of
the common bacteria as well as uncommon pathogen like Pseudomonas aeruginosa and
Burkholderia cepacia is a challenge to the routine antibiotic susceptibility testing and for
bacterial identification.
Evaluation of pulmonary tuberculosis
The diagnosis of pulmonary tuberculosis is a complex process that is slow, uncertain and
expensive. The laboratory diagnosis requires sampling of the specimens at multiple times for
acid-fast staining to detect the presence of Mycobacterium tuberculosis, then cultured in rapid
broth and on solid medium followed by subsequent identification exploiting either
phenotypic or molecular methods as well as antimicrobial susceptibility testing. The acid fast
stain provides a diagnostic method which is comparatively less expensive and has an impact
on the overall diagnostic yield and the public health (Ieven et al., 2018).
The other direct methods may include non-culture based methods. This non-culture based
methods can be further categorised into two types, they are- detection on the basis of antigen
and second is on the basis of molecular methods. The antigen dependant methods exploited
are immunofluorescence, immune-chromatography and enzyme linked immunoassay. The
molecular methods exploit DNA and RNA detection. The molecular techniques exploit PCR
techniques (Ogawa et al., 2019). The disadvantages of exploiting the PCR (Polymerase Chain
reaction) is that it cannot be exploited to quantitate and has high risks of cross contamination.
RT-PCR permits quantitation or semi-quantitation of viruses. But the newer PCR
The microbiology laboratory plays a crucial role in management of the cystic fibrosis
patients. The complex bacterial flora requires the usage of selective media and complex
protocols for the isolation of the pathogens. It is almost rare to eradicate the colonizing
pathogens like Pseudomonas sp and Staphylococcus aureus. Inhaled therapies are exploited
for chronic suppression and for treatment of the exacerbations. The antibiotic
pharmacokinetics are altered in the patients with cystic fibrosis. Unusual or altered strains of
the common bacteria as well as uncommon pathogen like Pseudomonas aeruginosa and
Burkholderia cepacia is a challenge to the routine antibiotic susceptibility testing and for
bacterial identification.
Evaluation of pulmonary tuberculosis
The diagnosis of pulmonary tuberculosis is a complex process that is slow, uncertain and
expensive. The laboratory diagnosis requires sampling of the specimens at multiple times for
acid-fast staining to detect the presence of Mycobacterium tuberculosis, then cultured in rapid
broth and on solid medium followed by subsequent identification exploiting either
phenotypic or molecular methods as well as antimicrobial susceptibility testing. The acid fast
stain provides a diagnostic method which is comparatively less expensive and has an impact
on the overall diagnostic yield and the public health (Ieven et al., 2018).
The other direct methods may include non-culture based methods. This non-culture based
methods can be further categorised into two types, they are- detection on the basis of antigen
and second is on the basis of molecular methods. The antigen dependant methods exploited
are immunofluorescence, immune-chromatography and enzyme linked immunoassay. The
molecular methods exploit DNA and RNA detection. The molecular techniques exploit PCR
techniques (Ogawa et al., 2019). The disadvantages of exploiting the PCR (Polymerase Chain
reaction) is that it cannot be exploited to quantitate and has high risks of cross contamination.
RT-PCR permits quantitation or semi-quantitation of viruses. But the newer PCR
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
instrumentations involve multiplex PCR linked in liquid array and rapid diagnostic PCR
instrument which are relatively expensive. Quantitative methods like real time PCR offers
additional diagnostic values in comparison to the non-quantitative methods (Kumar et al.,
2016).
instrumentations involve multiplex PCR linked in liquid array and rapid diagnostic PCR
instrument which are relatively expensive. Quantitative methods like real time PCR offers
additional diagnostic values in comparison to the non-quantitative methods (Kumar et al.,
2016).
5Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
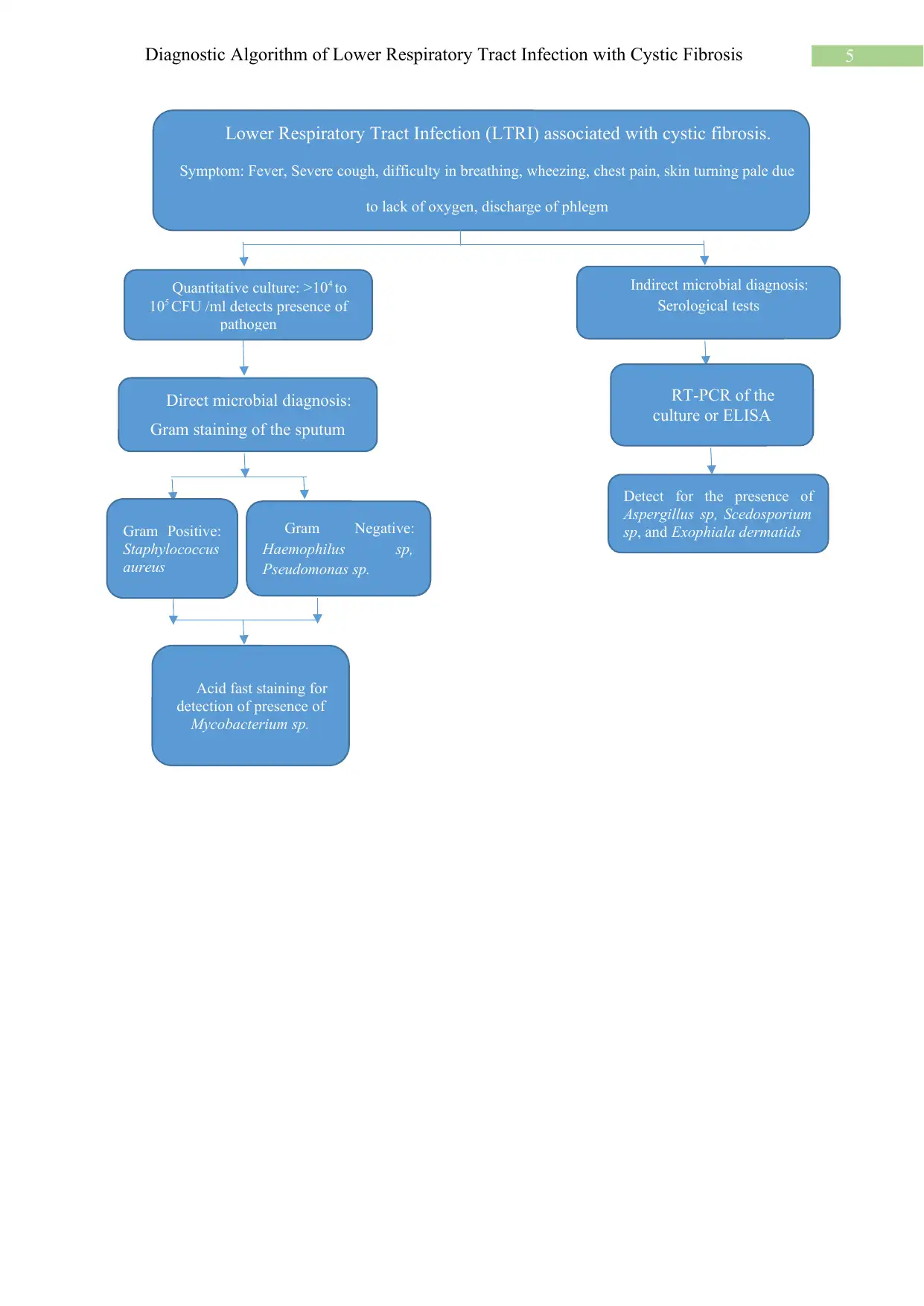
Lower Respiratory Tract Infection (LTRI) associated with cystic fibrosis.
Symptom: Fever, Severe cough, difficulty in breathing, wheezing, chest pain, skin turning pale due
to lack of oxygen, discharge of phlegm
Direct microbial diagnosis:
Gram staining of the sputum
Indirect microbial diagnosis:
Serological tests
Gram Positive:
Staphylococcus
aureus
Gram Negative:
Haemophilus sp,
Pseudomonas sp.
RT-PCR of the
culture or ELISA
Quantitative culture: >104 to
105 CFU /ml detects presence of
pathogen
Detect for the presence of
Aspergillus sp, Scedosporium
sp, and Exophiala dermatids
Acid fast staining for
detection of presence of
Mycobacterium sp.
Lower Respiratory Tract Infection (LTRI) associated with cystic fibrosis.
Symptom: Fever, Severe cough, difficulty in breathing, wheezing, chest pain, skin turning pale due
to lack of oxygen, discharge of phlegm
Direct microbial diagnosis:
Gram staining of the sputum
Indirect microbial diagnosis:
Serological tests
Gram Positive:
Staphylococcus
aureus
Gram Negative:
Haemophilus sp,
Pseudomonas sp.
RT-PCR of the
culture or ELISA
Quantitative culture: >104 to
105 CFU /ml detects presence of
pathogen
Detect for the presence of
Aspergillus sp, Scedosporium
sp, and Exophiala dermatids
Acid fast staining for
detection of presence of
Mycobacterium sp.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
References
Kumar, S., Saigal, S.R., Sethi, G.R. and Kumar, S., 2016. Application of serology and nested
polymerase chain reaction for identifying Chlamydophila pneumoniae in community-
acquired lower respiratory tract infections in children. Indian Journal of Pathology and
Microbiology, 59(4), p.499.
De Boeck, K., Wilschanski, M., Castellani, C., Taylor, C., Cuppens, H., Dodge, J. and
Sinaasappel, M., 2006. Cystic fibrosis: terminology and diagnostic algorithms. Thorax, 61(7),
pp.627-635.
Campbell, S. and Forbes, B.A., 2011. The clinical microbiology laboratory in the diagnosis of
lower respiratory tract infections. Journal of clinical microbiology, 49(9 Supplement),
pp.S30-S33.
Langelier, C., Kalantar, K.L., Moazed, F., Wilson, M.R., Crawford, E.D., Deiss, T., Belzer,
A., Bolourchi, S., Caldera, S., Fung, M. and Jauregui, A., 2018. Integrating host response and
unbiased microbe detection for lower respiratory tract infection diagnosis in critically ill
adults. Proceedings of the National Academy of Sciences, 115(52), pp.E12353-E12362.
Ieven, M., Coenen, S., Loens, K., Lammens, C., Coenjaerts, F., Vanderstraeten, A.,
Henriques-Normark, B., Crook, D., Huygen, K., Butler, C.C. and Verheij, T.J., 2018.
Aetiology of lower respiratory tract infection in adults in primary care: a prospective study in
11 European countries. Clinical Microbiology and Infection, 24(11), pp.1158-1163.
Nepal, R., Shrestha, B., Joshi, D.M., Joshi, R.D., Shrestha, S. and Singh, A., 2018. Antibiotic
Susceptibility Pattern of Gram-negative Isolates of Lower Respiratory Tract
Infection. Journal of Nepal Health Research Council, 16(1), pp.22-26.
References
Kumar, S., Saigal, S.R., Sethi, G.R. and Kumar, S., 2016. Application of serology and nested
polymerase chain reaction for identifying Chlamydophila pneumoniae in community-
acquired lower respiratory tract infections in children. Indian Journal of Pathology and
Microbiology, 59(4), p.499.
De Boeck, K., Wilschanski, M., Castellani, C., Taylor, C., Cuppens, H., Dodge, J. and
Sinaasappel, M., 2006. Cystic fibrosis: terminology and diagnostic algorithms. Thorax, 61(7),
pp.627-635.
Campbell, S. and Forbes, B.A., 2011. The clinical microbiology laboratory in the diagnosis of
lower respiratory tract infections. Journal of clinical microbiology, 49(9 Supplement),
pp.S30-S33.
Langelier, C., Kalantar, K.L., Moazed, F., Wilson, M.R., Crawford, E.D., Deiss, T., Belzer,
A., Bolourchi, S., Caldera, S., Fung, M. and Jauregui, A., 2018. Integrating host response and
unbiased microbe detection for lower respiratory tract infection diagnosis in critically ill
adults. Proceedings of the National Academy of Sciences, 115(52), pp.E12353-E12362.
Ieven, M., Coenen, S., Loens, K., Lammens, C., Coenjaerts, F., Vanderstraeten, A.,
Henriques-Normark, B., Crook, D., Huygen, K., Butler, C.C. and Verheij, T.J., 2018.
Aetiology of lower respiratory tract infection in adults in primary care: a prospective study in
11 European countries. Clinical Microbiology and Infection, 24(11), pp.1158-1163.
Nepal, R., Shrestha, B., Joshi, D.M., Joshi, R.D., Shrestha, S. and Singh, A., 2018. Antibiotic
Susceptibility Pattern of Gram-negative Isolates of Lower Respiratory Tract
Infection. Journal of Nepal Health Research Council, 16(1), pp.22-26.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Diagnostic Algorithm of Lower Respiratory Tract Infection with Cystic Fibrosis
Ogawa, M., Hoshina, T., Haro, K., Kumadaki, T., Ishii, M., Fujino, Y., Fukuda, K. and
Kusuhara, K., 2019. The microbiological characteristics of lower respiratory tract infection in
patients with neuromuscular disorders: An investigation based on a multiplex polymerase
chain reaction to detect viruses and a clone library analysis of the bacterial 16S rRNA gene
sequence in sputum samples. Journal of Microbiology, Immunology and Infection.
Ogawa, M., Hoshina, T., Haro, K., Kumadaki, T., Ishii, M., Fujino, Y., Fukuda, K. and
Kusuhara, K., 2019. The microbiological characteristics of lower respiratory tract infection in
patients with neuromuscular disorders: An investigation based on a multiplex polymerase
chain reaction to detect viruses and a clone library analysis of the bacterial 16S rRNA gene
sequence in sputum samples. Journal of Microbiology, Immunology and Infection.
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.