Comparative Analysis: Mammogram vs. Ultrasound for Breast Cancer
VerifiedAdded on 2022/11/16
|12
|3865
|463
Report
AI Summary
This report provides a comprehensive review of mammography and ultrasound as imaging techniques for breast cancer diagnosis. It compares the two methods, discussing their physics, working principles, sensitivity, specificity, advantages, disadvantages, and limitations. The review highlights the importance of age and breast density in determining the most appropriate imaging technique, with ultrasound being particularly useful in complementing mammography, especially for women with dense breasts. The report also explores the benefits of mammography in early cancer detection and the advantages of ultrasound in detecting lesions and assessing soft tissues. It also addresses the potential for overdiagnosis and the limitations of each technique, considering the need for additional examinations and the dependence on equipment and experience. Additionally, the report analyzes a cross-sectional study comparing the results obtained from both techniques, concluding that ultrasound is a better diagnostic tool for patients with high breast density and is more accurate in determining tumor size before surgery. The study shows that mammography is not reliable in breast cancer diagnosis alone.
A REVIEW OF THE USE OF MAMMOGRAM AND ULTRASOUND IN BREAST CANCER
By(name)
Class Name
Tutor
Institution
City and State
Date
By(name)
Class Name
Tutor
Institution
City and State
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Abstract
Breast cancer is one of the most common forms of cancer in women. Mammography and
ultrasound are the common imaging techniques used in breast cancer diagnosis. The choice on
the best imaging technique in breast cancer diagnosis is dependent on age. A review of the two
methods reveal that ultrasound is useful in complementing mammography. It can however not
entirely replace mammography. Because if its properties, mammography is more useful in breast
cancer diagnosis among women with a relatively high dense breasts.
Introduction.
Breast cancer is one of the most common cancer type infecting women in the contemporary
society. In terms of mortality as a resulting from, breast cancer closely follows skin cancer. It
accounts for about 33% of the diagnosed cancer (Devolli Disha et al., 2011). According to Zhang
(2012) the chances of a woman developing breast cancer is about 12%. Epidemiological studies
have revealed that various risk factors expose women to breast cancer. The common risk factors
are late age, first pregnancy after 30 years, premenopausal breast cancer history among others.
Historically, mammography has been employed breast cancer diagnosis in its early stages. This
concept has been used in the diagnosis of over 75% of breast cancer within 12 months prior to
detection (Devolli Disha et al., 2011). Mammography examinations are of two type, diagnostic
and screening. This essay reviews the use of mammogram and ultrasound in breast cancer by
comparing the two techniques in with an objective of finding which technique is relevant under
which circumstances.
Summary of Physics
Mammography refers to the procedure that uses a low dose X-rays of about 0.7mSV in
examining human breast. Just like other types of X-rays, mammograms employs ionization
radiation doses in image creation. The created image is then analyzed in order to identify
abnormal growths. This forms the basis of cancer diagnosis. Normally longer wavelength X-rays
compared to those used in bones radiography are employed (Draghi, Calliada, Ferrozzi,
Mandrioli, & Campani, 2017).
The screening mammograms are used in looking breast cancer signs in women who lack breast
problems. This involves taking the breast pictures at two different angles. Diagnostic
Breast cancer is one of the most common forms of cancer in women. Mammography and
ultrasound are the common imaging techniques used in breast cancer diagnosis. The choice on
the best imaging technique in breast cancer diagnosis is dependent on age. A review of the two
methods reveal that ultrasound is useful in complementing mammography. It can however not
entirely replace mammography. Because if its properties, mammography is more useful in breast
cancer diagnosis among women with a relatively high dense breasts.
Introduction.
Breast cancer is one of the most common cancer type infecting women in the contemporary
society. In terms of mortality as a resulting from, breast cancer closely follows skin cancer. It
accounts for about 33% of the diagnosed cancer (Devolli Disha et al., 2011). According to Zhang
(2012) the chances of a woman developing breast cancer is about 12%. Epidemiological studies
have revealed that various risk factors expose women to breast cancer. The common risk factors
are late age, first pregnancy after 30 years, premenopausal breast cancer history among others.
Historically, mammography has been employed breast cancer diagnosis in its early stages. This
concept has been used in the diagnosis of over 75% of breast cancer within 12 months prior to
detection (Devolli Disha et al., 2011). Mammography examinations are of two type, diagnostic
and screening. This essay reviews the use of mammogram and ultrasound in breast cancer by
comparing the two techniques in with an objective of finding which technique is relevant under
which circumstances.
Summary of Physics
Mammography refers to the procedure that uses a low dose X-rays of about 0.7mSV in
examining human breast. Just like other types of X-rays, mammograms employs ionization
radiation doses in image creation. The created image is then analyzed in order to identify
abnormal growths. This forms the basis of cancer diagnosis. Normally longer wavelength X-rays
compared to those used in bones radiography are employed (Draghi, Calliada, Ferrozzi,
Mandrioli, & Campani, 2017).
The screening mammograms are used in looking breast cancer signs in women who lack breast
problems. This involves taking the breast pictures at two different angles. Diagnostic
mammograms are however used if a woman’s breast shows if a variation is observed in the
screening mammogram. This often include extra vies which are not part of the screening
mammogram.
Working principles of mammogram. Mammograms are machines used in imaging breasts. It
takes X-rays on relatively lesser doses compared to the normal X-rays. Since X-ray are not
capable of penetrating human tissue, mammograms have two plates that compresses breast in
order to increase tissue surface. This forms the basis of the good pictures and gives a room less
radiation usage.
Ultrasound technique is another common imaging procedure. In this technology, breast is
subjected to a sound wave of high frequency forming images. This scanning process involves
placing a sound emitting probe on human breast. This does not involve any form of radiation.
Women showing symptoms of breast cancer or those with palpable findings upon clinical
examination are usually subjected to clinical examination via breast imaging. The breast imaging
techniques generally consist of either ultrasound or mammography or both.
Comparison between Mammography and Ultrasound.
The choice of a more suitable imaging technique of the two or their combination is partially
dependent on age. Age is known to delineate initial diagnosis choice of the breast imaging in
symptomatic women. According to Stindl (2016) there is little evidence to support the assertion
that age is a key determinant in choosing between ultrasound and mammogram in diagnosing
breast cancer in women. Devolli Disha et al. (2011) however suggest that women who are aged
35 or younger can be easily examined using ultrasound technique because of the high dense
tissue breast. Gaffer Sadist, Janani Shoran, Jafarnejad, & Esmaily, (2018) showed that there is a
progressive improvement in mammography sensitivity for women who are 60 and above years
older compared to ultrasound.
Difference in sensitivity of the two technologies is also a key determinant in choosing between
the two technologies. Generally, based on previous studies on mammography and ultrasound
techniques in breast cancer diagnosis, the difference in sensitivity of the two technologies is
statistically significant. According to Zhang (2012), ultrasound is found to be significantly more
sensitive in women who are 45 years and below than mammography. Besides the two techniques
screening mammogram. This often include extra vies which are not part of the screening
mammogram.
Working principles of mammogram. Mammograms are machines used in imaging breasts. It
takes X-rays on relatively lesser doses compared to the normal X-rays. Since X-ray are not
capable of penetrating human tissue, mammograms have two plates that compresses breast in
order to increase tissue surface. This forms the basis of the good pictures and gives a room less
radiation usage.
Ultrasound technique is another common imaging procedure. In this technology, breast is
subjected to a sound wave of high frequency forming images. This scanning process involves
placing a sound emitting probe on human breast. This does not involve any form of radiation.
Women showing symptoms of breast cancer or those with palpable findings upon clinical
examination are usually subjected to clinical examination via breast imaging. The breast imaging
techniques generally consist of either ultrasound or mammography or both.
Comparison between Mammography and Ultrasound.
The choice of a more suitable imaging technique of the two or their combination is partially
dependent on age. Age is known to delineate initial diagnosis choice of the breast imaging in
symptomatic women. According to Stindl (2016) there is little evidence to support the assertion
that age is a key determinant in choosing between ultrasound and mammogram in diagnosing
breast cancer in women. Devolli Disha et al. (2011) however suggest that women who are aged
35 or younger can be easily examined using ultrasound technique because of the high dense
tissue breast. Gaffer Sadist, Janani Shoran, Jafarnejad, & Esmaily, (2018) showed that there is a
progressive improvement in mammography sensitivity for women who are 60 and above years
older compared to ultrasound.
Difference in sensitivity of the two technologies is also a key determinant in choosing between
the two technologies. Generally, based on previous studies on mammography and ultrasound
techniques in breast cancer diagnosis, the difference in sensitivity of the two technologies is
statistically significant. According to Zhang (2012), ultrasound is found to be significantly more
sensitive in women who are 45 years and below than mammography. Besides the two techniques
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

have a difference in specificity. Ultrasound imaging technique has greater specificity compared
to mammography. This explains the variations in study findings of various studies with some
studies recording higher specificity in ultrasound compared to mammography.
Historically, ultrasound is employed in as tool of diagnosis that helps in evaluating abnormalities
and mammography. Ultrasound screening is relatively more sensitive compared to
mammography in cases where the breasts have denser tissues.
Advantages, disadvantages of mammogram and ultra sound in the diagnosis of breast cancer.
Advantages
Mammogram reduces the risk of succumbing to breast cancer. According to Gøtzsche &
Jørgensen (2013) out of 1000 women who undergo for mammogram in every 2 years for
20years, about 7 deaths have been avoided.
Mammography also lessens the risk of undergoing chemotherapy. The screening process
involved in mammogram helps in cancer detection at early development stages. This makes it
conceivable to have a treatment program at an early stage.
Mammography gives women a chance to be aware their breast health. About 98% of women do
not experience cancer if the mammogram and additional examination shows that they do not
have cancer.
Disadvantages.
Possibility of over diagnosis. Over diagnosis in this case3 refers to cancer detection that would
have not been identified were it not for the screening process. As a result, women are exposed to
diagnosis of cancers that would have had no impact on their health. This happens because
mammogram detects cancer at an early stage. According to Welch, Prorok, O’Malley, & Kramer
(2016) out of 77 breast cancer diagnosis using mammogram, 10 are cases of overdose.
Periods of anxiety and waiting whenever additional examination are involved. Nearly a half of
mammogram screening participants for 20 years (453 in 1000 women) are subjected to at least 1
additional examination (Ohuchi et al., 2016). This causes unrest and anxiety because the patients
are unsure whether they have breast cancer or not.
Limitations.
to mammography. This explains the variations in study findings of various studies with some
studies recording higher specificity in ultrasound compared to mammography.
Historically, ultrasound is employed in as tool of diagnosis that helps in evaluating abnormalities
and mammography. Ultrasound screening is relatively more sensitive compared to
mammography in cases where the breasts have denser tissues.
Advantages, disadvantages of mammogram and ultra sound in the diagnosis of breast cancer.
Advantages
Mammogram reduces the risk of succumbing to breast cancer. According to Gøtzsche &
Jørgensen (2013) out of 1000 women who undergo for mammogram in every 2 years for
20years, about 7 deaths have been avoided.
Mammography also lessens the risk of undergoing chemotherapy. The screening process
involved in mammogram helps in cancer detection at early development stages. This makes it
conceivable to have a treatment program at an early stage.
Mammography gives women a chance to be aware their breast health. About 98% of women do
not experience cancer if the mammogram and additional examination shows that they do not
have cancer.
Disadvantages.
Possibility of over diagnosis. Over diagnosis in this case3 refers to cancer detection that would
have not been identified were it not for the screening process. As a result, women are exposed to
diagnosis of cancers that would have had no impact on their health. This happens because
mammogram detects cancer at an early stage. According to Welch, Prorok, O’Malley, & Kramer
(2016) out of 77 breast cancer diagnosis using mammogram, 10 are cases of overdose.
Periods of anxiety and waiting whenever additional examination are involved. Nearly a half of
mammogram screening participants for 20 years (453 in 1000 women) are subjected to at least 1
additional examination (Ohuchi et al., 2016). This causes unrest and anxiety because the patients
are unsure whether they have breast cancer or not.
Limitations.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The breast cancer screening using mammogram does not guarantee that that all the cases of
breast cancer will be detected. According to Henriksen, Carlsen, Vejborg, Nielsen, & Lauridsen
(2018) out of 1000 female subjected to mammogram in every two years for 20 years, 77 still be
diagnosed with cancer despite their mammogram results being normal. Such scenarios are
attributed to the possibility of the cancer not being visible to the mammogram and the possibility
of the cancer not being developed at the time of mammography.
Mammography does not guarantee that all the participants tested with breast cancer will survive.
Out of 1000 women subjected to mammography in every 2 years for 20 years 13 participants die
of breast cancer (Ohuchi et al., 2016).
Ultrasound
Benefits.
The majority of ultrasound scanning process is noninvasive. The procedure does not involve the
use of needles or injection. Ultrasound imaging process provides a real time image rendering it a
relevant tool in complementing lesser invasive procedures such as fluid aspiration.
Compared to mammography, ultrasound process is capable of detecting lesions in cases where
breast tissues are dense. Ultrasound also provides clear pictures of soft tissues which are not
shown by X-ray. Ultrasound do not use ionized radiation making it comparatively safer. It is also
more cost friendly. Besides, the use of ultrasound makes it possible for the physicians to
determine the various regions of clinical concerns because of the normal tissue properties for
example; benign cysts. For the majority of women aged 30 years and above a combination of
mammogram and ultrasound are used in determining the need of biopsy in a concerned area
(Mainiero et al., 2016).
Disadvantage.
The standard diagnostic ultrasound is known to have harmful effect on human health. The
interpretation of breast ultrasound scan often necessitates additional procedure such at the
follow-up ultrasound and biopsy. According to Berg et al. (2015) some of these procedures have
reveled cases of non-cancerous cases where ultrasound technique had shown positive results.
Limitations.
breast cancer will be detected. According to Henriksen, Carlsen, Vejborg, Nielsen, & Lauridsen
(2018) out of 1000 female subjected to mammogram in every two years for 20 years, 77 still be
diagnosed with cancer despite their mammogram results being normal. Such scenarios are
attributed to the possibility of the cancer not being visible to the mammogram and the possibility
of the cancer not being developed at the time of mammography.
Mammography does not guarantee that all the participants tested with breast cancer will survive.
Out of 1000 women subjected to mammography in every 2 years for 20 years 13 participants die
of breast cancer (Ohuchi et al., 2016).
Ultrasound
Benefits.
The majority of ultrasound scanning process is noninvasive. The procedure does not involve the
use of needles or injection. Ultrasound imaging process provides a real time image rendering it a
relevant tool in complementing lesser invasive procedures such as fluid aspiration.
Compared to mammography, ultrasound process is capable of detecting lesions in cases where
breast tissues are dense. Ultrasound also provides clear pictures of soft tissues which are not
shown by X-ray. Ultrasound do not use ionized radiation making it comparatively safer. It is also
more cost friendly. Besides, the use of ultrasound makes it possible for the physicians to
determine the various regions of clinical concerns because of the normal tissue properties for
example; benign cysts. For the majority of women aged 30 years and above a combination of
mammogram and ultrasound are used in determining the need of biopsy in a concerned area
(Mainiero et al., 2016).
Disadvantage.
The standard diagnostic ultrasound is known to have harmful effect on human health. The
interpretation of breast ultrasound scan often necessitates additional procedure such at the
follow-up ultrasound and biopsy. According to Berg et al. (2015) some of these procedures have
reveled cases of non-cancerous cases where ultrasound technique had shown positive results.
Limitations.
Despite the aforementioned merits of ultrasound imaging technique in breast cancer diagnosis,
this procedure does not replace the annual mammography procedure. Besides, majority of
cancers are not visible on ultrasound scans. Majority of the calcifications reveled in the
mammogram are not visible in ultrasound scan. Similarly, the MRI findings as a result of cancer
are often not seen in ultrasound scans.
The biopsy procedure is thus recommending in determining if a suspicious abnormality is
cancerous or not. The majority of such suspicious ultrasound findings turns out to be non-
cancerous. Ultrasound technique is not common in most health facilities. Ultrasound screening is
often not covered in majority of the insurance plans. Ultrasound scanning is dependent on the
abnormality that is being recognized at the time of examination (Freer, 2015). The procedure
thus requires experience and good equipment which are not common in developing nations.
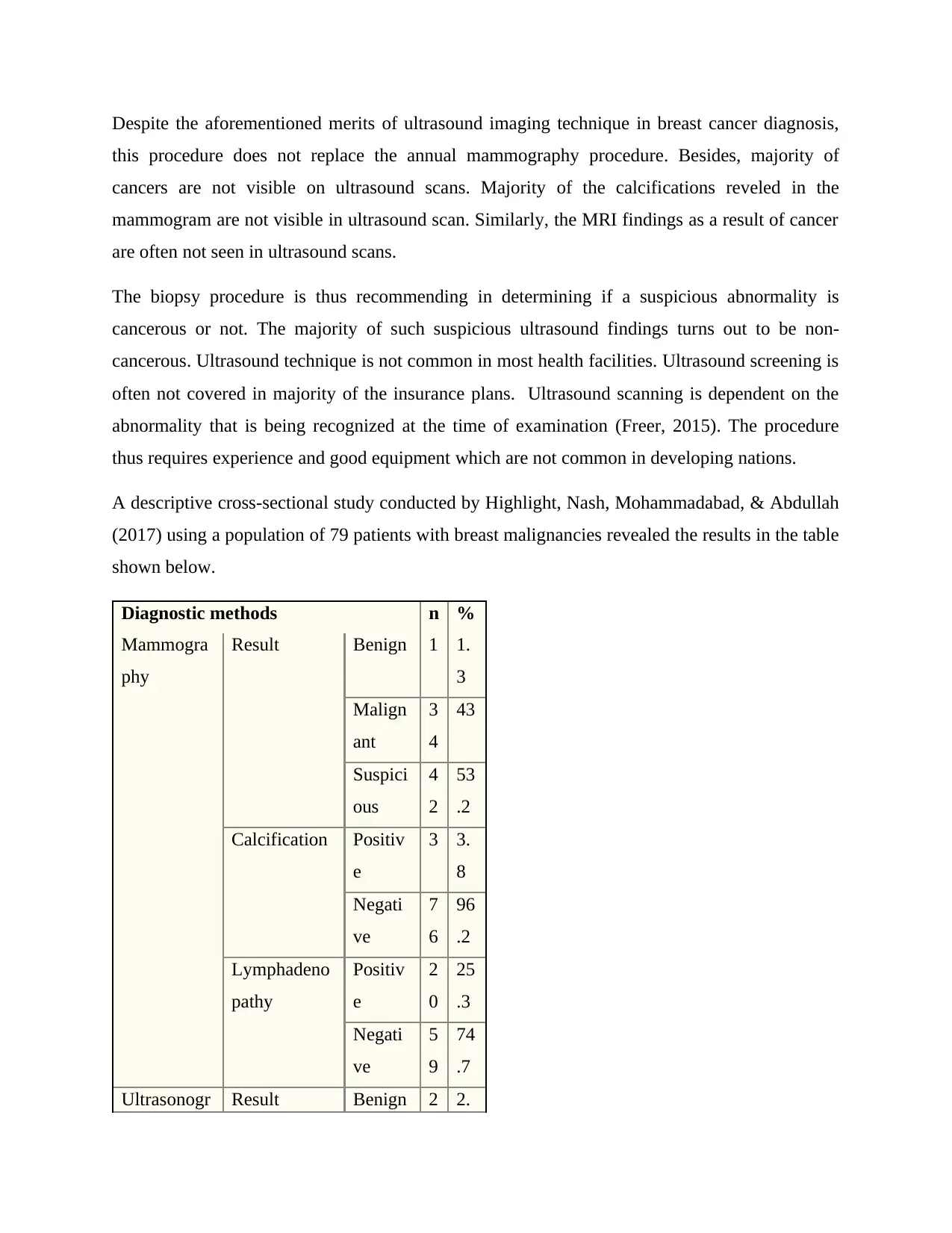
A descriptive cross-sectional study conducted by Highlight, Nash, Mohammadabad, & Abdullah
(2017) using a population of 79 patients with breast malignancies revealed the results in the table
shown below.
Diagnostic methods n %
Mammogra
phy
Result Benign 1 1.
3
Malign
ant
3
4
43
Suspici
ous
4
2
53
.2
Calcification Positiv
e
3 3.
8
Negati
ve
7
6
96
.2
Lymphadeno
pathy
Positiv
e
2
0
25
.3
Negati
ve
5
9
74
.7
Ultrasonogr Result Benign 2 2.
this procedure does not replace the annual mammography procedure. Besides, majority of
cancers are not visible on ultrasound scans. Majority of the calcifications reveled in the
mammogram are not visible in ultrasound scan. Similarly, the MRI findings as a result of cancer
are often not seen in ultrasound scans.
The biopsy procedure is thus recommending in determining if a suspicious abnormality is
cancerous or not. The majority of such suspicious ultrasound findings turns out to be non-
cancerous. Ultrasound technique is not common in most health facilities. Ultrasound screening is
often not covered in majority of the insurance plans. Ultrasound scanning is dependent on the
abnormality that is being recognized at the time of examination (Freer, 2015). The procedure
thus requires experience and good equipment which are not common in developing nations.
A descriptive cross-sectional study conducted by Highlight, Nash, Mohammadabad, & Abdullah
(2017) using a population of 79 patients with breast malignancies revealed the results in the table
shown below.
Diagnostic methods n %
Mammogra
phy
Result Benign 1 1.
3
Malign
ant
3
4
43
Suspici
ous
4
2
53
.2
Calcification Positiv
e
3 3.
8
Negati
ve
7
6
96
.2
Lymphadeno
pathy
Positiv
e
2
0
25
.3
Negati
ve
5
9
74
.7
Ultrasonogr Result Benign 2 2.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
aphy 5
Malign
ant
2
1
26
.6
Suspici
ous
5
6
70
.9
Calcification Positiv
e
9 11
.4
Negati
ve
7
0
88
.6
Lymphadeno
pathy
Positiv
e
2
5
31
.6
Negati
ve
5
3
67
.1
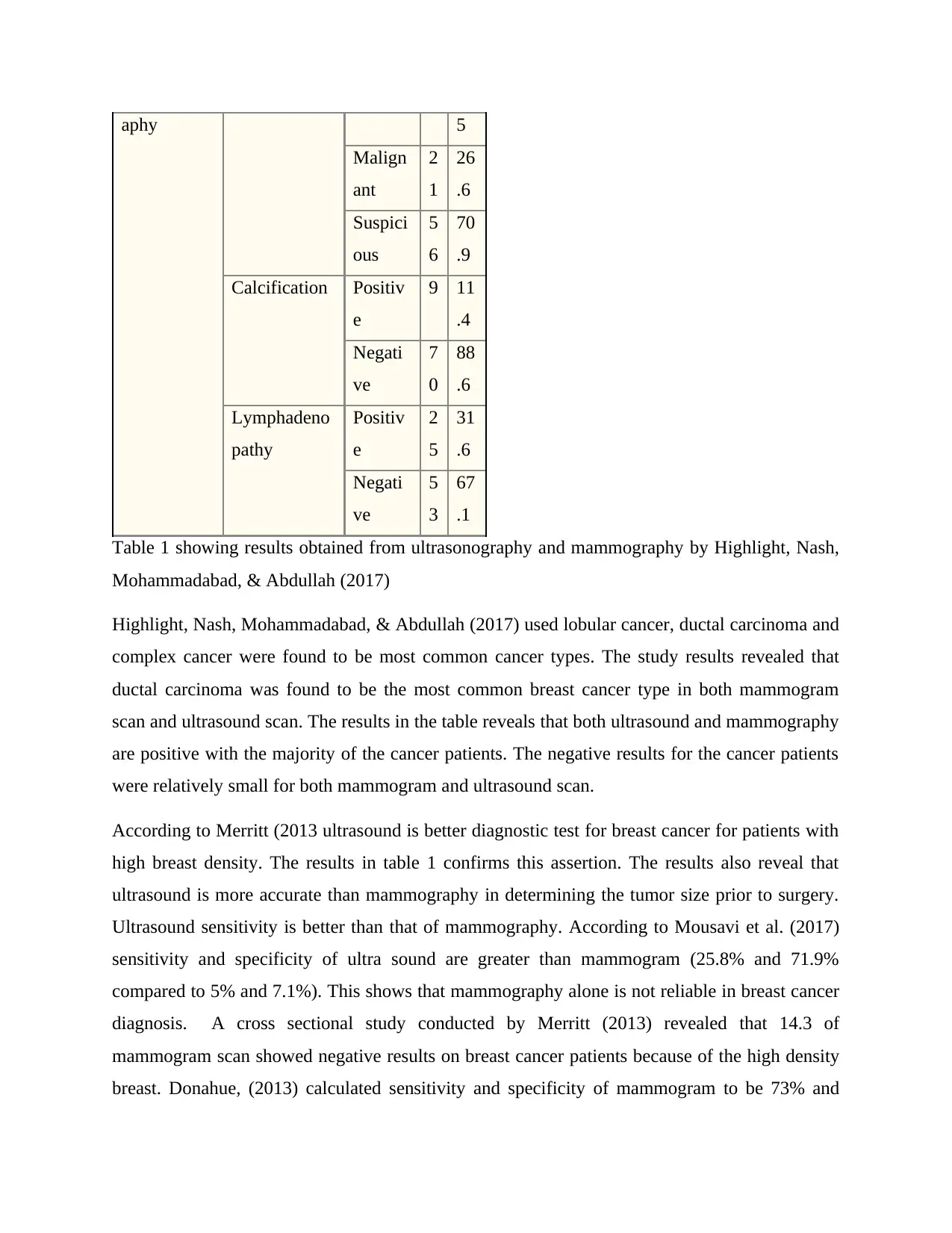
Table 1 showing results obtained from ultrasonography and mammography by Highlight, Nash,
Mohammadabad, & Abdullah (2017)
Highlight, Nash, Mohammadabad, & Abdullah (2017) used lobular cancer, ductal carcinoma and
complex cancer were found to be most common cancer types. The study results revealed that
ductal carcinoma was found to be the most common breast cancer type in both mammogram
scan and ultrasound scan. The results in the table reveals that both ultrasound and mammography
are positive with the majority of the cancer patients. The negative results for the cancer patients
were relatively small for both mammogram and ultrasound scan.
According to Merritt (2013 ultrasound is better diagnostic test for breast cancer for patients with
high breast density. The results in table 1 confirms this assertion. The results also reveal that
ultrasound is more accurate than mammography in determining the tumor size prior to surgery.
Ultrasound sensitivity is better than that of mammography. According to Mousavi et al. (2017)
sensitivity and specificity of ultra sound are greater than mammogram (25.8% and 71.9%
compared to 5% and 7.1%). This shows that mammography alone is not reliable in breast cancer
diagnosis. A cross sectional study conducted by Merritt (2013) revealed that 14.3 of
mammogram scan showed negative results on breast cancer patients because of the high density
breast. Donahue, (2013) calculated sensitivity and specificity of mammogram to be 73% and
Malign
ant
2
1
26
.6
Suspici
ous
5
6
70
.9
Calcification Positiv
e
9 11
.4
Negati
ve
7
0
88
.6
Lymphadeno
pathy
Positiv
e
2
5
31
.6
Negati
ve
5
3
67
.1
Table 1 showing results obtained from ultrasonography and mammography by Highlight, Nash,
Mohammadabad, & Abdullah (2017)
Highlight, Nash, Mohammadabad, & Abdullah (2017) used lobular cancer, ductal carcinoma and
complex cancer were found to be most common cancer types. The study results revealed that
ductal carcinoma was found to be the most common breast cancer type in both mammogram
scan and ultrasound scan. The results in the table reveals that both ultrasound and mammography
are positive with the majority of the cancer patients. The negative results for the cancer patients
were relatively small for both mammogram and ultrasound scan.
According to Merritt (2013 ultrasound is better diagnostic test for breast cancer for patients with
high breast density. The results in table 1 confirms this assertion. The results also reveal that
ultrasound is more accurate than mammography in determining the tumor size prior to surgery.
Ultrasound sensitivity is better than that of mammography. According to Mousavi et al. (2017)
sensitivity and specificity of ultra sound are greater than mammogram (25.8% and 71.9%
compared to 5% and 7.1%). This shows that mammography alone is not reliable in breast cancer
diagnosis. A cross sectional study conducted by Merritt (2013) revealed that 14.3 of
mammogram scan showed negative results on breast cancer patients because of the high density
breast. Donahue, (2013) calculated sensitivity and specificity of mammogram to be 73% and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
55% respectively with a false rate of 17.3%. The same study showed that the sensitivity and
specificity of ultrasound are 99% and 70% correspondingly with a false proportion of 17.7%.
This study also revealed a significant difference in sensitivity and specificity.
Besides breastfeeding history and pregnancies are also key determinant of the breast cancer
diagnosis method. The specificity and sensitivity of both power Doppler and color Doppler are
often employed in differentiating between the malignant and benign lesion. This entire process
helps in avoiding unnecessary lesions. According to Devolli Disha et al., (2011) mammogram
sensitivity is used in non-palpable cancer diagnosis. The findings of Pellegrino & Mansi (2014)
reveals that mammogram is comparatively better in diagnosis of non-palpable cancers within
stages 1 to 4 compared to ultrasound but not within stage 1 to 2. Clinical study conducted by
Vercauteren et al. (2008) reveals that ultrasound is not an ultimate substitute for mammography
in breast cancer diagnosis.
There are other complementary imaging technologies that can be used alongside mammogram
other ultrasound. A study by Martin & Boyd (2014) revealed that magnetic imaging is a better
technology in clinical screening of residual tumor diagnosis after a chemotherapy of carcinoma
extent. Magnetic resonance imaging technique is also relatively cheaper compared to the two
technologies. Despite its merits over mammography, this technology is still incapable of
substituting mammography. This is because the magnetic resonance imaging has a lower
specificity compared to mammography. All the breast cancer screening processes are however
characterized by anxiety and possible faulty results that indicates that participants have breast
cancer when in reality they do not have cancer. According to Mousavi et al. (2017) a large
proportion of the screen-detected invasive breast cancer are node negative. The risk of false
results in however significantly decreased by the use of sonographic screening alongside
mammography and the magnetic resonance imaging as proposed by Yaghjyan, Colditz, Rosner,
& Tamimi (2015).
Situation when ultrasound is useful.
There are scenarios where ultrasound is necessary in breast cancer screening. Such cases
include a scenario where a patient feel a palpable lump while the mammogram is normal. This is
particularly common in cases where the lump is far away from the breast surface making the
mammogram to miss it. In such cases, a breast ultrasound is important in detecting cancer
specificity of ultrasound are 99% and 70% correspondingly with a false proportion of 17.7%.
This study also revealed a significant difference in sensitivity and specificity.
Besides breastfeeding history and pregnancies are also key determinant of the breast cancer
diagnosis method. The specificity and sensitivity of both power Doppler and color Doppler are
often employed in differentiating between the malignant and benign lesion. This entire process
helps in avoiding unnecessary lesions. According to Devolli Disha et al., (2011) mammogram
sensitivity is used in non-palpable cancer diagnosis. The findings of Pellegrino & Mansi (2014)
reveals that mammogram is comparatively better in diagnosis of non-palpable cancers within
stages 1 to 4 compared to ultrasound but not within stage 1 to 2. Clinical study conducted by
Vercauteren et al. (2008) reveals that ultrasound is not an ultimate substitute for mammography
in breast cancer diagnosis.
There are other complementary imaging technologies that can be used alongside mammogram
other ultrasound. A study by Martin & Boyd (2014) revealed that magnetic imaging is a better
technology in clinical screening of residual tumor diagnosis after a chemotherapy of carcinoma
extent. Magnetic resonance imaging technique is also relatively cheaper compared to the two
technologies. Despite its merits over mammography, this technology is still incapable of
substituting mammography. This is because the magnetic resonance imaging has a lower
specificity compared to mammography. All the breast cancer screening processes are however
characterized by anxiety and possible faulty results that indicates that participants have breast
cancer when in reality they do not have cancer. According to Mousavi et al. (2017) a large
proportion of the screen-detected invasive breast cancer are node negative. The risk of false
results in however significantly decreased by the use of sonographic screening alongside
mammography and the magnetic resonance imaging as proposed by Yaghjyan, Colditz, Rosner,
& Tamimi (2015).
Situation when ultrasound is useful.
There are scenarios where ultrasound is necessary in breast cancer screening. Such cases
include a scenario where a patient feel a palpable lump while the mammogram is normal. This is
particularly common in cases where the lump is far away from the breast surface making the
mammogram to miss it. In such cases, a breast ultrasound is important in detecting cancer
compared to mammogram. In this case, imaging is done for diagnosis rather than a mere
screening procedure. As previously mentioned, in cases of dense breast tissue, a combination of
the two methods are more appropriate in breast cancer screening procedure. Again this is
attributed to mammogram sensitivity which drops from about 85% in average women to between
48% and 64% in women who have dense breast (Merritt, 2013).
Radiation concerns of mammography and ultrasound breast cancer screening.
There are often radiation concerns about mammogram usage. This is because mammograms
expose patients to radiation. Ultrasound on the other hand does not expose patients to any form
of radiation. Given the possibility of annual screening there are often fear of accumulated
radiation as a result of being subjected to mammogram scans which might one day result in
caner. The radiation levels in mammograms are however extremely low. According to Yaghjyan,
Colditz, Rosner, & Tamimi (2015) the radiation levels in mammograms are nearly the same as
those used in the dental X-rays and less than the radiation required in standard chest X-ray.
Conclusion.
In consideration breast cancer incidents among the young women, the proportion of young
women with dense breasts, ultrasound is suitable as an additional imaging method in breast
cancer diagnosis. Ultrasound imaging is thus preferred as supplementary technique in breast
cancer imaging process. This is attributed to the fact that ultrasound imaging will help in
improving the both the sensitivity and specificity of the diagnosis process. The two technologies
also vary significantly in their procedures. Generally, mammography is preferred in breast cancer
screening. For young female patients, mammography should be however supplemented with
ultrasound scanning for the diagnosis of benign lesions and in scenarios where the patients have
large breast density in order to improve the detection speed. Complementing mammography with
ultrasound scan also reduces the cost of the entire procedure and minimizes the high risk women
from succumbing to breast cancer. Mammogram accuracy improves when the breast is less dense
and fattier. Ultrasound appears superior to mammography in young women who have dense
breast. Ultrasound is more appropriate at the initial imaging test.
screening procedure. As previously mentioned, in cases of dense breast tissue, a combination of
the two methods are more appropriate in breast cancer screening procedure. Again this is
attributed to mammogram sensitivity which drops from about 85% in average women to between
48% and 64% in women who have dense breast (Merritt, 2013).
Radiation concerns of mammography and ultrasound breast cancer screening.
There are often radiation concerns about mammogram usage. This is because mammograms
expose patients to radiation. Ultrasound on the other hand does not expose patients to any form
of radiation. Given the possibility of annual screening there are often fear of accumulated
radiation as a result of being subjected to mammogram scans which might one day result in
caner. The radiation levels in mammograms are however extremely low. According to Yaghjyan,
Colditz, Rosner, & Tamimi (2015) the radiation levels in mammograms are nearly the same as
those used in the dental X-rays and less than the radiation required in standard chest X-ray.
Conclusion.
In consideration breast cancer incidents among the young women, the proportion of young
women with dense breasts, ultrasound is suitable as an additional imaging method in breast
cancer diagnosis. Ultrasound imaging is thus preferred as supplementary technique in breast
cancer imaging process. This is attributed to the fact that ultrasound imaging will help in
improving the both the sensitivity and specificity of the diagnosis process. The two technologies
also vary significantly in their procedures. Generally, mammography is preferred in breast cancer
screening. For young female patients, mammography should be however supplemented with
ultrasound scanning for the diagnosis of benign lesions and in scenarios where the patients have
large breast density in order to improve the detection speed. Complementing mammography with
ultrasound scan also reduces the cost of the entire procedure and minimizes the high risk women
from succumbing to breast cancer. Mammogram accuracy improves when the breast is less dense
and fattier. Ultrasound appears superior to mammography in young women who have dense
breast. Ultrasound is more appropriate at the initial imaging test.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Bibliography
Berg, W. A., Bandos, A. I., Mendelson, E. B., Lehrer, D., Jong, R. A., & Pisano, E. D. (2015).
Ultrasound as the Primary Screening Test for Breast Cancer: Analysis From ACRIN
6666. Journal of the National Cancer Institute, 108(4), djv367.
Devolli Disha, E., Manxhuka Kerliu, S., Baruti Gafurri, Z., Topciu, V., Zhubi, B., & Paqarizi, H.
(2011). Evaluation of breast symptoms with mammography and ultrasonography.
Journal of Health Sciences, 1(3).
Donahue, E. J. (2013). Ultrasound-Guided Breast Biopsy Tissue Sampling: Technique and
Breast Ultrasound Characteristics of Benign and Malignant Lesions. Breast Cancer, 133-
148.
Draghi, F., Calliada, F., Ferrozzi, G., Mandrioli, R., & Campani, R. (2017). Ascessual breast
cancer and non-puerperal breast abscesses: Diagnosis and follow-up with mammography,
B-mode and color Doppler ultrasonography. European Journal of Ultrasound, 7, S13.
Freer, P. E. (2015). Mammographic Breast Density: Impact on Breast Cancer Risk and
Implications for Screening. RadioGraphics, 35(2), 302-315.
Berg, W. A., Bandos, A. I., Mendelson, E. B., Lehrer, D., Jong, R. A., & Pisano, E. D. (2015).
Ultrasound as the Primary Screening Test for Breast Cancer: Analysis From ACRIN
6666. Journal of the National Cancer Institute, 108(4), djv367.
Devolli Disha, E., Manxhuka Kerliu, S., Baruti Gafurri, Z., Topciu, V., Zhubi, B., & Paqarizi, H.
(2011). Evaluation of breast symptoms with mammography and ultrasonography.
Journal of Health Sciences, 1(3).
Donahue, E. J. (2013). Ultrasound-Guided Breast Biopsy Tissue Sampling: Technique and
Breast Ultrasound Characteristics of Benign and Malignant Lesions. Breast Cancer, 133-
148.
Draghi, F., Calliada, F., Ferrozzi, G., Mandrioli, R., & Campani, R. (2017). Ascessual breast
cancer and non-puerperal breast abscesses: Diagnosis and follow-up with mammography,
B-mode and color Doppler ultrasonography. European Journal of Ultrasound, 7, S13.
Freer, P. E. (2015). Mammographic Breast Density: Impact on Breast Cancer Risk and
Implications for Screening. RadioGraphics, 35(2), 302-315.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Ghaffari Sardasht, F., Jahani Shourab, N., Jafarnejad, F., & Esmaily, H. (2018). Communication
Skills of Health Personnel During Reproductive Ages in Pre-Conception Care. Journal of
Holistic Nursing and Midwifery, 28(2), 109-114.
Gøtzsche, P. C., & Jørgensen, K. J. (2013). Screening for breast cancer with mammography.
Cochrane Database of Systematic Reviews.
Haghighi, F., Naseh, G., Mohammadifard, M., & Abdollahi, N. (2017). Comparison of
mammography and ultrasonography findings with pathology results in patients with
breast cancer in Birjand, Iran. Electronic Physician, 9(10), 5494-5498.
Henriksen, E. L., Carlsen, J. F., Vejborg, I. M., Nielsen, M. B., & Lauridsen, C. A. (2018). The
efficacy of using computer-aided detection (CAD) for detection of breast cancer in
mammography screening: a systematic review. Acta Radiologica, 60(1), 13-18.
Mainiero, M. B., Lourenco, A., Mahoney, M. C., Newell, M. S., Bailey, L., Barke, L. D., …
Haffty, B. G. (2016). ACR Appropriateness Criteria Breast Cancer Screening. Journal of
the American College of Radiology, 13(11), R45-R49.
Martin, L. J., & Boyd, N. F. (2014). Mammographic density. Potential mechanisms of breast
cancer risk associated with mammographic density: hypotheses based on epidemiological
evidence. Breast Cancer Research, 10(S1).
Merritt, C. (2013). Combined Screening With Ultrasound and Mammography vs Mammography
Alone in Women at Elevated Risk of Breast Cancer. Breast Diseases: A Year Book
Quarterly, 20(4), 401-402.
Mousavi, S. M., Montazeri, A., Mohagheghi, M. A., Jarrahi, A. M., Harirchi, I., Najafi, M., &
Ebrahimi, M. (2017). Breast Cancer in Iran: An Epidemiological Review. The Breast
Journal, 13(4), 383-391.
Ohuchi, N., Suzuki, A., Sobue, T., Kawai, M., Yamamoto, S., Zheng, Y., … Ishida, T. (2016).
Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for
breast cancer in the Japan Strategic Anti-cancer Randomized Trial (J-START): a
randomised controlled trial. The Lancet, 387(10016), 341-348.
Pellegrino, S., & Mansi, L. (2014). Andrea Rockall, Andrew Hatrick, Peter Armstrong, Martin
Wastie (Eds.): Diagnostic Imaging (7th edn.). European Journal of Nuclear Medicine
and Molecular Imaging, 41(12), 2357-2357.
Skills of Health Personnel During Reproductive Ages in Pre-Conception Care. Journal of
Holistic Nursing and Midwifery, 28(2), 109-114.
Gøtzsche, P. C., & Jørgensen, K. J. (2013). Screening for breast cancer with mammography.
Cochrane Database of Systematic Reviews.
Haghighi, F., Naseh, G., Mohammadifard, M., & Abdollahi, N. (2017). Comparison of
mammography and ultrasonography findings with pathology results in patients with
breast cancer in Birjand, Iran. Electronic Physician, 9(10), 5494-5498.
Henriksen, E. L., Carlsen, J. F., Vejborg, I. M., Nielsen, M. B., & Lauridsen, C. A. (2018). The
efficacy of using computer-aided detection (CAD) for detection of breast cancer in
mammography screening: a systematic review. Acta Radiologica, 60(1), 13-18.
Mainiero, M. B., Lourenco, A., Mahoney, M. C., Newell, M. S., Bailey, L., Barke, L. D., …
Haffty, B. G. (2016). ACR Appropriateness Criteria Breast Cancer Screening. Journal of
the American College of Radiology, 13(11), R45-R49.
Martin, L. J., & Boyd, N. F. (2014). Mammographic density. Potential mechanisms of breast
cancer risk associated with mammographic density: hypotheses based on epidemiological
evidence. Breast Cancer Research, 10(S1).
Merritt, C. (2013). Combined Screening With Ultrasound and Mammography vs Mammography
Alone in Women at Elevated Risk of Breast Cancer. Breast Diseases: A Year Book
Quarterly, 20(4), 401-402.
Mousavi, S. M., Montazeri, A., Mohagheghi, M. A., Jarrahi, A. M., Harirchi, I., Najafi, M., &
Ebrahimi, M. (2017). Breast Cancer in Iran: An Epidemiological Review. The Breast
Journal, 13(4), 383-391.
Ohuchi, N., Suzuki, A., Sobue, T., Kawai, M., Yamamoto, S., Zheng, Y., … Ishida, T. (2016).
Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for
breast cancer in the Japan Strategic Anti-cancer Randomized Trial (J-START): a
randomised controlled trial. The Lancet, 387(10016), 341-348.
Pellegrino, S., & Mansi, L. (2014). Andrea Rockall, Andrew Hatrick, Peter Armstrong, Martin
Wastie (Eds.): Diagnostic Imaging (7th edn.). European Journal of Nuclear Medicine
and Molecular Imaging, 41(12), 2357-2357.
Stindl, R. (2016). Telomere-driven karyotypic and molecular convergence mimics the
transmissibility of cancer in the Tasmanian devil. The Winnower.
Vercauteren, L. D., Kessels, A. G., Van der Weijden, T., Koster, D., Severens, J. L., Van
Engelshoven, J. M., & Flobbe, K. (2008). Clinical impact of the use of additional
ultrasonography in diagnostic breast imaging. European Radiology, 18(10), 2076-2084.
Welch, H. G., Prorok, P. C., O’Malley, A. J., & Kramer, B. S. (2016). Breast-Cancer Tumor
Size, Overdiagnosis, and Mammography Screening Effectiveness. New England Journal
of Medicine, 375(15), 1438-1447.
Yaghjyan, L., Colditz, G. A., Rosner, B., & Tamimi, R. M. (2015). Mammographic breast
density and breast cancer risk: interactions of percent density, absolute dense, and non-
dense areas with breast cancer risk factors. Breast Cancer Research and Treatment,
150(1), 181-189.
Zhang, Z. (2012). Detection of Breast Cancer With Addition of Annual Screening Ultrasound or
a Single Screening MRI to Mammography in Women With Elevated Breast Cancer Risk.
JAMA, 307(13), 13-94.
transmissibility of cancer in the Tasmanian devil. The Winnower.
Vercauteren, L. D., Kessels, A. G., Van der Weijden, T., Koster, D., Severens, J. L., Van
Engelshoven, J. M., & Flobbe, K. (2008). Clinical impact of the use of additional
ultrasonography in diagnostic breast imaging. European Radiology, 18(10), 2076-2084.
Welch, H. G., Prorok, P. C., O’Malley, A. J., & Kramer, B. S. (2016). Breast-Cancer Tumor
Size, Overdiagnosis, and Mammography Screening Effectiveness. New England Journal
of Medicine, 375(15), 1438-1447.
Yaghjyan, L., Colditz, G. A., Rosner, B., & Tamimi, R. M. (2015). Mammographic breast
density and breast cancer risk: interactions of percent density, absolute dense, and non-
dense areas with breast cancer risk factors. Breast Cancer Research and Treatment,
150(1), 181-189.
Zhang, Z. (2012). Detection of Breast Cancer With Addition of Annual Screening Ultrasound or
a Single Screening MRI to Mammography in Women With Elevated Breast Cancer Risk.
JAMA, 307(13), 13-94.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





